Abstract
Objective
To assess pediatric resident and preceptor environmental tobacco smoke (ETS)-reduction practices and attitudes to inform the development of resident tobacco intervention training.
Study design
Pediatricians in a teaching hospital anonymously completed a 65-item survey.
Results
Residents’ and preceptors’ (n = 93) ETS actions were generally similar. Pediatricians inconsistently intervened across treatment settings and when treating different ETS-related illnesses (eg, 60% “always” assessed during asthma visits, 13% during otitis visits). Less than 50% “always” explained ETS risks to smoking parents and less than 33% “always” advised about creating smoke-free homes. Most pediatricians reported negative attitudes toward smoking parents; however, attitudes were not related to actions. Most frequently cited barriers to ETS action were lack of time and low confidence in effectiveness.
Conclusion
Understanding barriers to ETS intervention could promote transdisciplinary (TD) training and intervention approaches that effectively promote pediatrician advice while offloading the time burden of intensive smoking intervention. ETS intervention training should foster pediatrician confidence and TD relationships with affiliated health professionals who could facilitate intervention, referral, and follow-up necessary to sustain smoking behavior change.
Almost 60% of US children 3 to 11 years of age (approximately 22 million children) are exposed to environmental tobacco smoke (ETS) daily–with urban children suffering the highest rates of exposure.1,2 Although research suggests slightly lower rates of exposure when considering broader child age ranges,3 younger children are more susceptible to ETS-related consequences than older age groups.4,5 Children exposed to ETS have higher rates of lower respiratory infections, asthma, middle ear effusions, behavior problems, and sudden infant death syndrome.2,6–8 Moreover, a child with a parent who smokes has a threefold higher risk of becoming a smoker.9 ETS exposure is a leading cause of childhood morbidity and mortality, and an estimated $4.6 billion in direct medical costs are expensed annually to treat children with ETS-related illnesses and disease.10 Recent evidence suggests that complete development of the lungs continues through 6 to 8 years of age.11 Exposure to ETS during infancy can modify the formation, structure, and maturity of the lungs—an important factor in the development of asthma, to which researchers attribute 40% to 60% of the cases to ETS exposure.12,13 Children exposed to environmental toxins (eg, ETS) may accrue half of their total lifetime cancer risk because of this exposure by 6 years of age.14 ETS also significantly increases cardiovascular disease risk as much as 20%.15,16
Pediatricians recognize the harmful effects of children’s exposure to ETS and have been encouraged by the American Academy of Pediatrics and the US Surgeon General to directly address ETS with parents and provide guidance on smoking cessation.1,6,17 Moreover, numerous studies indicate that even brief advice about smoking and reducing ETS facilitates parent action toward smoking behavior change.18 For example, a recent meta-analysis showed that brief physician advice provided in primary care, hospital wards, and outpatient clinics significantly increased the odds of quitting smoking by approximately 2.5% compared with no advice.19
A broad, multidisciplinary literature suggests that a combination of physician and healthcare worker advice, referrals to behavioral counseling programs with or without pharmacotherapies, and ongoing follow-up are necessary components to motivate smoking behavior change and sustain long-term abstinence.20–21 However, pediatricians have yet to embrace fully their role in ETS reduction and in helping parents quit smoking, even when patients present with diagnoses directly affected by ETS and despite parental interest in the topic.22,23
We developed the present assessment to determine physician training needs to improve ETS-reduction efforts. As such, we wanted to explore the extent to which pediatric residents and their primary care preceptors currently addressed ETS. We also sought to determine the frequency of resident intervention with smoking parents across different settings (eg, emergency department [ED] and inpatient units). Finally, we wanted to explore pediatrician attitudes about ETS intervention and their role in helping parents change their smoking behavior. Knowledge of these attitudes and how they relate to physician practices would serve as a guide for our ETS training approach.
METHODS
We conducted a cross-sectional study of pediatric residents and primary care preceptors at Children’s Hospital of Philadelphia using an anonymous, self-report questionnaire. The survey was distributed to all pediatric residents’ and primary care preceptors’ mail boxes, during one grand rounds presentation and a routine primary care training session. Respondents voluntarily completed the survey in approximately 10 minutes based on observations during pilot testing of the instrument. Then, residents returned the surveys to an investigator’s (KPL) office mail box. E-mail reminders encouraged participation. Duplicate responses were possible, but very unlikely, given the length of the survey and the lack of any monetary or other incentive for completion. The survey consisted of 65 items assessing pediatrician tobacco intervention practices and attitudes. Item selection blended previous published research, primary care practice guidelines for smoking cessation,22,24 and our goal of determining ETS intervention training issues at Children’s Hospital of Philadelphia. The survey included 40 forced-choice questions about pediatrician ETS practices for different patient visit types (eg, well child vs asthma or lower respiratory tract infection [LRTI]) and different treatment settings, (eg, primary care vs inpatient). Forced-choice questions used a 4-point Likert-type response scale (“none,” “occasionally,” “often,” and “always”) for assessing (1) how often pediatricians ask about ETS exposure for different visit types and settings; (2) how often they advise and assist parents to create a smoke-free home; and (3) how often they assess parents’ willingness to quit, advise them to quit, assist them in their quit attempt, and monitor their smoking behavior through follow-up. Ten open-ended questions were included to assess pediatrician attitudes about ETS intervention, for example: “Think about the last time you walked into an exam room and smelled tobacco smoke on a parent. What were your thoughts and feelings? What did you say to the parent? If you said nothing, what were your reasons?” To classify open-ended responses, a panel of three, study-blind tobacco researchers independent of the coding investigators created response codes into these subsequent categories: (1) visceral negative reactions (eg, “disgusted,” “Yuck!”); (2) frustration, anger, or disappointment with a parent; (3) helplessness; and (4) motivation to actively address ETS. Coders achieved an average intra-item agreement of 87%. Responses coded with <75% reliability were recoded as (5) “other” for analyses. Primary analyses were descriptive and included χ2 tests to assess differences in frequencies of behaviors between residents and preceptors in primary care, across ETS-related visits, and across settings. Pearson correlations were used to assess attitude-behavior relationships. A priori significance was set at P < .05. Results were entered and analyzed using the Statistical Package for the Social Sciences version 11.0 (SPSS Inc., Chicago, Ill). Surveys with incomplete answers were included in the analyses and denominators were adjusted accordingly.
RESULTS
Sixty-six residents across all years of training (approximately 60% of all pediatric residents) and 27 preceptors (70% of all preceptors) responded to the survey. Almost all respondents (93%) reported that they received <2 hours of smoking cessation training during residency.
ETS-Related Practice in Primary Care Clinics
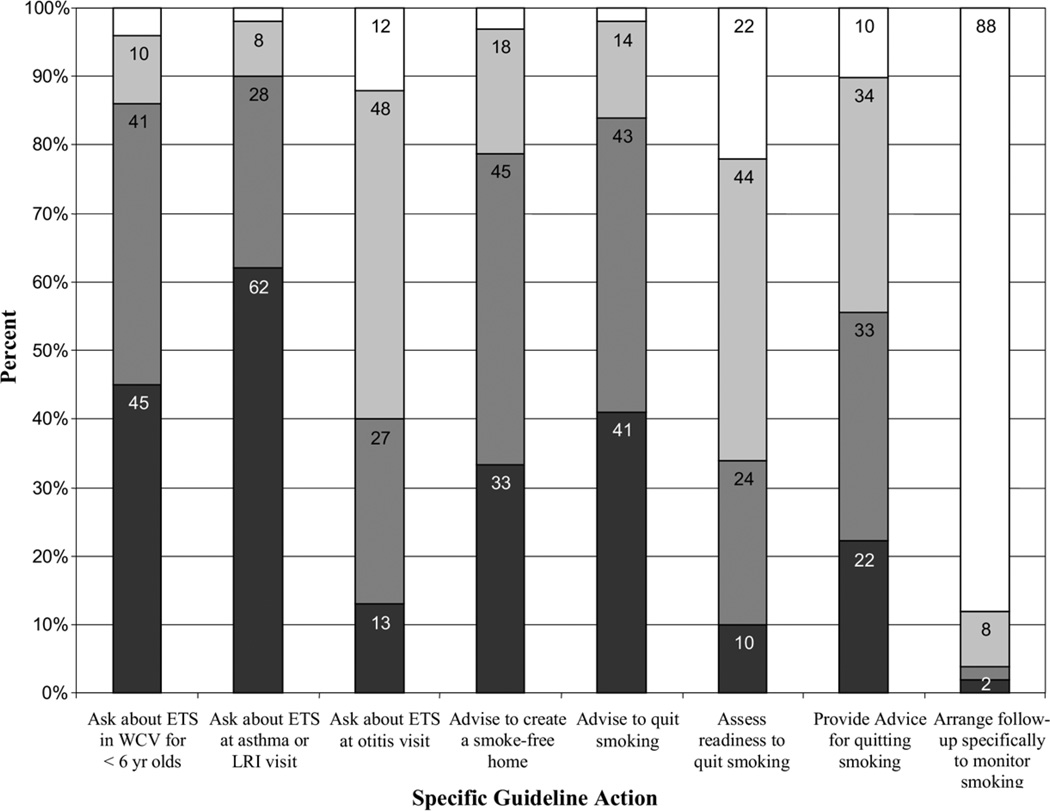
Preceptor and resident reports of ETS practices in clinic were similar across assessment and advice behaviors except for two items. Chi square analyses indicated differences between groups in frequency of ETS exposure assessment during clinic visits for asthma or LRTI (χ2 = 12.41, P < .05). For example, 70% of residents versus 42% of preceptors “always” asked about ETS during these visits. Conversely, for clinic visits in general, there were group differences in advising smoking parents about creating a smoke-free home (χ2 = 23.25, P < .01) with 69% of preceptors versus 19% of residents stating they “always” advise smoking parents to create a smoke-free home. Otherwise, group differences across action categories were not significant, thus, we collapsed data between groups to illustrate in Figure 1 the specific ETS practices of all pediatricians in primary care.
Figure 1.
Percent of pediatric residents’ and preceptors’ ETS practices in primary care clinic.  , Never;
, Never;  Occasionally;
Occasionally;  Often;
Often;  Always.
Always.
Respondents most frequently engaged in four ETS action categories based on the frequencies of “always” or “often” asking about ETS during well child visits and sick visits for asthma or LRTI as well as advising smoking parents about creating a smoke-free home or quitting smoking. However, these frequencies are far below the recommended consistent courses of action. Even when parents were interested in smoking cessation, nearly all respondents reported that they neglected to provide standard advice, (eg, identifying triggers, establishing quit-dates, providing referrals, and arranging follow-up to monitor parents’ smoking behavior). Respondents also reported infrequently asking about ETS during otitis visits.
Resident Practices across Clinical Settings
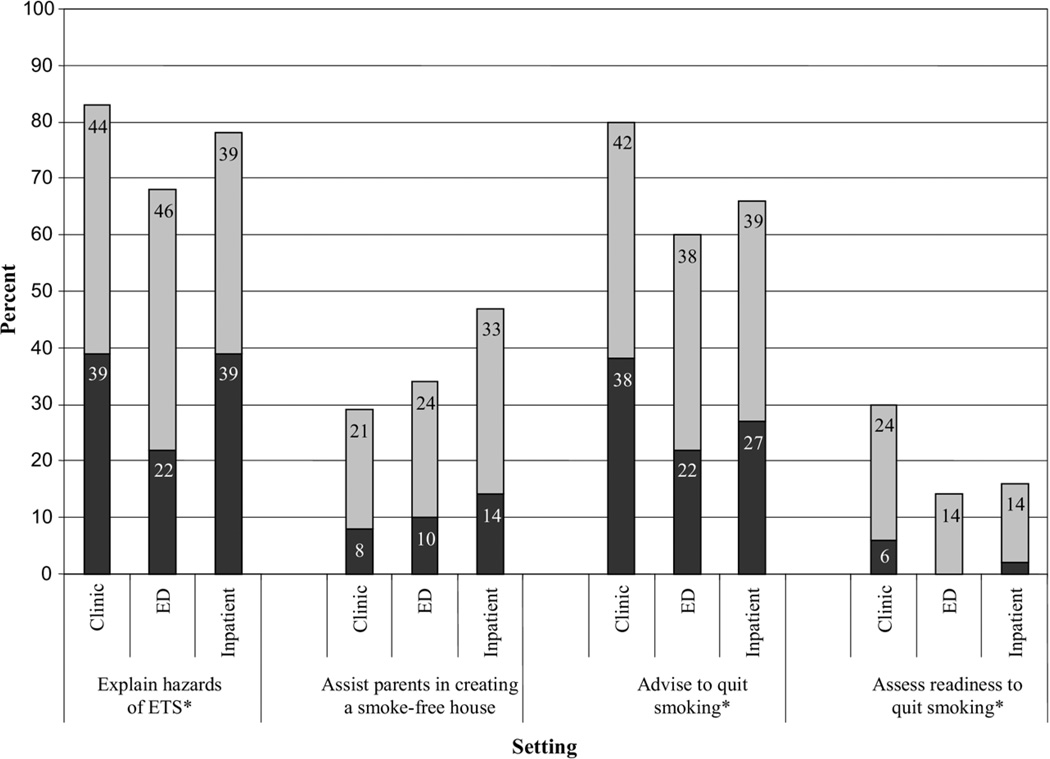
Figure 2 shows residents’ tobacco intervention behaviors across clinic settings (assessing attending physician actions across settings was beyond the scope of this study). Residents “often” or “always” explained hazards of ETS to smoking parents more frequently in primary care versus inpatient (χ2 = 28.94, P < .01) and ED units (χ2 = 23.77, P < .001). Similarly, albeit much less frequently, residents “always” provided smoke-free home advice more often in primary care and inpatient units than in the ED (clinic vs ED, χ2 = 16.48, P < .001). Respondents also advised smoking parents to quit smoking more frequently in primary care versus inpatient settings (χ2 = 37.62, P < .001) and the ED (χ2 = 29.85, P < .001).
Figure 2.
Percent of pediatric residents performing each ETS action “often” or “always” in different settings when learning that a parent smokes.*Statistically significant differences among settings (χ2, P < .01).  Often;
Often;  Always.
Always.
Beliefs and Attitudes
More than 75% of respondents agreed that ETS is “one of the most important health hazards for children,” and 95% believed it is an “extremely serious concern for patients with asthma.” Yet, only 55% agreed that they were “very comfortable” with their “knowledge about the effects of ETS.” Many respondents (51%) also reported believing they were ineffective in reducing their patients’ ETS exposure, in providing advice about how to quit (61%), and in positively influencing a parent’s smoking behavior (54%). None believed they were “very effective” in any of these activities.
Pediatricians also reported a perceived conflict about their role in advising smoking parents about smoking cessation. Most pediatricians (82%) agreed they should “help parents quit smoking;” however, most stated they do not have enough “time” (69%) or “training” (79%) to talk about tobacco issues. Almost all (89%) stated they were “not familiar with the resources available for parents interested in quitting.” Most pediatricians (53%) also believed that “parents are not interested in hearing about smoking cessation from pediatricians.” Pediatricians’ open-ended responses about their thoughts and feelings when entering a room and smelling tobacco smoke fell into four categories: 33% reported visceral negative responses (eg, “Yuck, I can’t breathe”); 37% reported feeling annoyance or anger toward the parent (eg, “I can’t believe that the parent smoked right before coming here”); 9% reported helplessness and dismay (eg, “Wish they would quit … I can’t do anything about it”); and 16% reported actions to intervene (eg, “I need to do something about this ….”).
Attitude-Behavior Correlations
We also explored parental smoking and ETS attitude-behavior relationships to guide the development of training materials. Bivariate Pearson r correlations indicated that differences in attitudes toward parental smoking did not relate to a number of tobacco intervention-related behaviors. For example, residents with greater negative attitudes toward parent smokers were not less likely to ask about ETS, advise parents to establish a smoke-free household or to quit smoking, assess willingness to quit smoking, or provide advice on how to quit than residents with less negative attitudes toward parent smokers. However, there was a relationship between intervention-oriented attitudes and reported confidence in helping parents create smoke-free homes (r = .31, P < .01). Pediatricians were less likely to assess readiness to quit smoking if they believed a handout about ETS (r = −.27, P < .01) or literature on how to quit (r = −.22, P < .05) would be helpful to smoking parents. Also, the belief that ETS is “one of the most serious health hazards for children,” was related to interest in learning more about how to help parents quit smoking (r = .31, P < .01). This belief also correlated with beliefs that “it is a pediatrician’s role to help parents quit smoking” (r = .24, P < .05), that “a handout on ETS would be very helpful” (r = .31, P < .01); and that “lack of proper documentation is a big problem in helping parents quit smoking” (r = .26, P < .01). Finally, the concern that one does not have enough training in advising parents to quit smoking was related to feeling uninformed about ETS resources (r = .33, P < .01).
Practice and Tobacco Training—Behavior Relationships
Among all respondents, years of practice ranged from 1 to 25 years (mean = 4.80, SD = 5.61), with mean tobacco training in residency = 1.37 hours (SD = .63). Years of practice was significantly related to frequency of providing smoke-free home advice (r = .22, P = .03); cessation advice (r = .33, P = .002); cessation referrals (r = .33, P = .002); and explanation of ETS hazards (r = .26, P = .04). Years of practice also related to the following attitudes: “It is my role to help smoking parents quit” (r = .33, P = .001); “I am comfortable helping parents create a smoke-free home” (r = .21, P = .04); and “I am familiar with smoking cessation resources” (r = .22, P = .02). No significant correlations emerged between tobacco training and either actions or attitudes, perhaps because of the restricted range of training hours. However, trends emerged between tobacco training and frequency of assessing parent readiness to quit (r = .20, P = .07) and explaining ETS dangers in the ED (r = .22, P = .08).
DISCUSSION
This study provides a distinct view of pediatrician attitudes and actions associated with parent smoking and child ETS exposure. These data suggest an opportunity to improve pediatrician ETS intervention behavior given that too few pediatricians are following best practice guidelines for addressing parental smoking. For example, only 75% of pediatricians in this sample agreed that ETS is one of the most important health hazards for children, and when pediatricians identified a parent smoker, they rarely intervened beyond brief advice to eliminate children’s ETS exposure or to quit smoking— they typically did not assess willingness to quit, provide advice about how to quit, or arrange follow-up. Such omissions occurred across treatment settings. Pediatricians were more likely to assess ETS for patients with asthma or LRTI than for other ETS-related illnesses, as expected. However, it is concerning that only 13% of respondents “always” asked about ETS during otitis visits when ETS is one of the leading causes of otitis.25
Among respondents’ primary reasons for inconsistent ETS intervention was lack of training. This reason suggests that the average of 1.4 hours of tobacco training reported in this sample may be grossly insufficient to promote routine smoking intervention. Even though practice years influenced some specific actions, data indicated that general pediatric experience is not sufficient to promote full adherence to tobacco guidelines. Thus, it appears that preceptors as well as residents would benefit from more thorough tobacco intervention training. Other key barriers to ETS intervention included lack of time, lack of knowledge about appropriate, intensive tobacco intervention resources, and lack of confidence in their tobacco intervention skills. To a degree not documented previously, pediatricians appeared very frustrated with parents who smoke and were pessimistic about their ability to help them change. However, our analyses suggest that negative attitudes toward parent smokers did not significantly affect physician practices.
All barriers described herein can be addressed through comprehensive training. Previous research suggests that training directly relates to physicians’ smoking cessation counseling self-efficacy and effectiveness,26,27 and that self-efficacy can improve pediatrician tobacco guideline adherence.26 Our data support the assertion that tobacco intervention self-confidence may improve the frequency of ETS-related actions. In our sample, pediatricians expressed general interest in learning more about strategies to reduce patients’ ETS exposure and in being able to provide smoking parents with useful information.
Transdisciplinary Training
The multi-determined nature of chronic behavioral health problems, such as smoking, requires that practitioners promote the implementation of broad, comprehensive treatments that blend disciplinary perspectives. Previous articles have described training for transdiciplinary (TD) scientists in approaching public health problems.28 The theses of these articles can be extended to training for practitioners who address public health problems at an idiographic level. Specific to pediatrician ETS training, recent research supports this assertion.29 In a recent study by Collins and colleagues,27 pediatric residents were provided multidimensional training including didactics, problem-solving, patient education materials, and clinical reminders for guideline adherence. Residents who were trained with this approach compared with nontrained residents were more likely to ask parents about their patients’ ETS exposure, to advise parents to cut down or to quit smoking, to help set a quit-date, and to provide ETS-specific follow-up. Moreover, follow-up was facilitated because trained residents were more likely to record history of passive tobacco exposure in the medical record.27 A TD training approach integrating disciplinary approaches could address barriers to effective, brief ETS intervention by suggesting ways to offload the burden of intensive intervention components to specialists and by boosting pediatrician confidence in the effectiveness using brief behavioral advice and follow-up.
Limitations of this study include the lack of respondent demographic data collected through the anonymous survey process. We opted not to include these items in favor of maximizing response validity by protecting the identity of residents, many of whom felt their responses might be evaluated as part of their training program. As a consequence, it is impossible to assess potential biases in resident versus preceptor behaviors. We also were unable to obtain information on nonrespondents. Without these data, it is difficult to determine the generalizability of our results; however, we feel that the issues identified in the survey parallel similar issues that can shape training at other academic pediatric health systems.30 Furthermore, respondents’ recall rates across different settings may be influenced by training status or even by the other questions on the survey in ways that this study could not measure, and our results were vulnerable to respondent bias toward inflating socially desirable responses.20,31 Future studies can address these limitations and better elucidate how pediatricians’ attitudes and behaviors could be influenced by pediatrician versus patient demographic characteristics. Other measurement-related limitations included the typical challenges with open-ended response coding. However, the investigators employed standard coding procedures with high reliability, and these results can inform the construction of future instruments to better ascertain physician attitude-behavior relationships.
Another limitation was that we only collected data related to acute illnesses known to be related to or exacerbated by ETS. Aside from asthma, we did not query actions with ETS-related chronic illness or behavioral presentations (eg, cancers, heart disease, attention deficit hyperactivity disorder), nor did we collect data from pediatric specialty clinics (eg, oncology, otolaryngology, cardiology, etc). To our knowledge, no study has examined such pediatrician tobacco intervention practices, therefore leaving that area open for study. We also did not assess nursing staff adherence, as this information was beyond the scope of the study. Future studies should examine this issue and whether a clinic-team approach to ETS exposure enhances guideline adherence.
A large body of research points to pediatricians’ influence on smoking parents, particularly in helping them seriously consider smoking behavior change. This study demonstrated key areas where pediatricians can improve their tobacco intervention actions with parents, and the results delineated opportunities for training strategies that could maximize pediatricians’ effectiveness with reducing ETS. It is likely that just improving ETS knowledge and intervention skills with smoking parents will not guarantee improved adherence to tobacco intervention guidelines when barriers to action, such as time constraints, exist. However, given the deficits in pediatricians’ ETS knowledge and ETS-reduction actions suggested in this study, improving training to enhance knowledge and tobacco intervention skills is a good starting point that in the end could have a wide, pediatrician-lead public health impact.
Acknowledgments
Supported by National Cancer Institute grants K07 CA-93756 and R01 CA-105183 (Collins, PI), and a Transdisciplinary Tobacco Use Research Center grant, P50CA84718 (Caryn Lerman, PI).
The authors thank Jamie Dahm and Dr Marcie Mitre for their assistance with manuscript editing. The lead author thanks Caryn Lerman for her mentorship during this study.
Glossary
- ED
Emergency department
- ETS
Environmental tobacco smoke
- LRTI
Lower respiratory tract infection
- TD
Transdiciplinary
Footnotes
Data were collected at Children’s Hospital of Philadelphia as part of Dr. Levin’s “Ann E. Dyson Advocacy Training Project” during residency.
REFERENCES
- 1.US Department of Health and Human Services Centers of Disease Control and Prevention Coordinating Center for Health Promotion National Center for Chronic Disease Prevention and Health Promotion, editor. Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Rockville, MD: 2006. [Google Scholar]
- 2.Kurtz ME, Kurtz JC, Johnson SM, Beverly EE. Exposure to environmental tobacco smoke—perceptions of African American children and adolescents. Preventive Med. 1996;25:286–292. doi: 10.1006/pmed.1996.0058. [DOI] [PubMed] [Google Scholar]
- 3.Gehrman CA, Hovell MF. Protecting children from environmental tobacco smoke (ETS) exposure: a critical review. Nicotine Tobacco Res. 2003;5:289–301. doi: 10.1080/1462220031000094231. [DOI] [PubMed] [Google Scholar]
- 4.Gergen PJ, Fowler JA, Maurer KR, Davis WW, Overpeck MD. The burden of environmental tobacco smoke exposure on the respiratory health of children 2 months through 5 years of age in the United States: Third National Health and Nutrition Examination Survey, 1988 to 1994. Pediatrics. 1998;101:E8. doi: 10.1542/peds.101.2.e8. [DOI] [PubMed] [Google Scholar]
- 5.Carmichael SL, Ahluwalia IB. Correlates of postpartum smoking relapse. Results from the Pregnancy Risk Assessment Monitoring System (PRAMS) Am J Prev Med. 2000;19:193–196. doi: 10.1016/s0749-3797(00)00198-7. [DOI] [PubMed] [Google Scholar]
- 6.Committee on Environmental Health Policy Statement. Environmental tobacco smoke: a hazard to children. Pediatrics. 1997;99:639–642. [PubMed] [Google Scholar]
- 7.Klonoff-Cohen HS, Edelstein SL, Lefkowitz ES, Srinivasan IP, Kaegi D, Chang JC, et al. The effect of passive smoking and tobacco exposure through breast milk on sudden infant death syndrome. JAMA. 1995;273:795–798. doi: 10.1001/jama.1995.03520340051035. [DOI] [PubMed] [Google Scholar]
- 8.Weitzman M, Gortmaker S, Sobol A. Maternal smoking and behavior problems of children. Pediatrics. 1992;90:342–349. [PubMed] [Google Scholar]
- 9.Farkas AJ, Gilpin EA, White MM, Pierce JP. Association between household and workplace smoking restrictions and adolescent smoking. JAMA. 2000;284:717–722. doi: 10.1001/jama.284.6.717. [DOI] [PubMed] [Google Scholar]
- 10.Secondhand Smoke Tearing Families Apart: The Health and Economic Burden of Smoking on Children. Washington, DC: American Legacy Foundation; 2004. [Google Scholar]
- 11.Plopper CG, Fanucchi MV. Do urban environmental pollutants exacerbate childhood lung diseases? Environ Health Perspect. 2000;108:A252–A253. doi: 10.1289/ehp.108-a252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perera FP, Illman SM, Kinney PL, Whyatt RM, Kelvin EA, Shepard P, et al. The challenge of preventing environmentally related disease in young children: community-based research in New York City. Environ Health Perspect. 2002;110:197–204. doi: 10.1289/ehp.02110197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheikh S, Goldsmith LJ, Howell L, Parry L, Eid N. Comparison of lung function in infants exposed to maternal smoking and in infants with a family history of asthma. Chest. 1999;116:52–58. doi: 10.1378/chest.116.1.52. [DOI] [PubMed] [Google Scholar]
- 14.Day NE, Brown CC. Multistage models and primary prevention of cancer. J Natl Cancer Inst. 1980;64:977–989. [PubMed] [Google Scholar]
- 15.Burke V, Gracey MP, Milligan RA, Thompson C, Taggart AC, Beilin LJ. Parental smoking and risk factors for cardiovascular disease in 10- to 12-year-old children. J Pediatr. 1998;133:206–213. doi: 10.1016/s0022-3476(98)70221-5. [DOI] [PubMed] [Google Scholar]
- 16.Weiss ST. Cardiovascular effects of environmental tobacco smoke. Circulation. 1996;94:599. doi: 10.1161/01.cir.94.4.599. [DOI] [PubMed] [Google Scholar]
- 17.Koop CE. The pediatrician’s obligation in smoking education. Am J Dis Child. 1985;5:38–48. doi: 10.1001/archpedi.1985.02140120019017. [DOI] [PubMed] [Google Scholar]
- 18.Rustin TA. Techniques for smoking cessation: what really works? Tex Med. 2001;97:63–67. [PubMed] [Google Scholar]
- 19.Lancaster T, Stead L. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2004:CD000165. doi: 10.1002/14651858.CD000165.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Collins B, Dahm J, Wilder A, McGarrah A, Audrain-McGovern J, Lerman C, et al. Philadelphia Fresh: Family Rules for Establishing Smoke-Free Homes. An Integrated Behavioral Smoking Trial Tailored to Urban African Americans; Paper presented at the Annual Conference of the Eastern Psychological Association; March 2003; Baltimore, MD. [Google Scholar]
- 21.Tong EK, Ong MK, Vittinghoff E, Perez-Stable EJ. Nondaily smokers should be asked and advised to quit. Am J Preventive Med. 2006;30:23–30. doi: 10.1016/j.amepre.2005.08.048. [DOI] [PubMed] [Google Scholar]
- 22.Perez-Stable EJ, Juarez-Reyes M, Kaplan C, Fuentes-Afflick E, Gildengorin V, Millstein S. Counseling smoking parents of young children: comparison of pediatricians and family physicians. Arch Pediatr Adolescent Med. 2001;155:25–31. doi: 10.1001/archpedi.155.1.25. [DOI] [PubMed] [Google Scholar]
- 23.Tanski SE, Klein JD, Winickoff JP, Auinger P, Weitzman M. Tobacco counseling at well-child and tobacco-influenced illness visits: opportunities for improvement. Pediatrics. 2003;111:E162–E167. doi: 10.1542/peds.111.2.e162. [DOI] [PubMed] [Google Scholar]
- 24.Fiore MC. Treating tobacco use and dependence: an introduction to the US Public Health Service Clinical Practice Guideline. Respiratory Care. 2000;45:1196–1199. [PubMed] [Google Scholar]
- 25.Stenstrom R, Bernard PA, Ben-Simhon H. Exposure to environmental tobacco smoke as a risk factor for recurrent acute otitis media in children under the age of five years. Int J Pediatric Otorhinolaryngol. 1993;27:127–136. doi: 10.1016/0165-5876(93)90128-p. [DOI] [PubMed] [Google Scholar]
- 26.Cabana MD, Rand C, Slish K, Nan B, Davis MM, Clark N. Pediatrician self-efficacy for counseling parents of asthmatic children to quit smoking. Pediatrics. 2004;113(1 Pt 1):78–81. doi: 10.1542/peds.113.1.78. [DOI] [PubMed] [Google Scholar]
- 27.Collins RL, D’Angelo S, Stearns SD, Campbell LR. Training pediatric residents to provide smoking cessation counseling to parents. Sci World J. 2005;5:410–419. doi: 10.1100/tsw.2005.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nash JM, Collins BN, Loughlin SE, Solbrig M, Harvey R, Krishnan-Sarin S, et al. Training the transdisciplinary scientist: a general framework applied to tobacco use behavior. Nicotine Tobacco Res. 2003;5(suppl 1):S41–S53. doi: 10.1080/14622200310001625528. [DOI] [PubMed] [Google Scholar]
- 29.Scal P, Hennrikus D, Ehrlich L, Ireland M, Borowsky I. Preparing residents to counsel about smoking. Clin Pediatr (Phila) 2004;43:703–708. doi: 10.1177/000992280404300803. [DOI] [PubMed] [Google Scholar]
- 30.Zapka JG, Fletcher K, Pbert L, Druker SK, Ockene JK, Chen L. The perceptions and practices of pediatricians: tobacco intervention. Pediatrics. 1999;103:e65. doi: 10.1542/peds.103.5.e65. [DOI] [PubMed] [Google Scholar]
- 31.Hymowitz N, Schwab J, Eckholdt H. Pediatric residency training on tobacco. Pediatrics. 2001;108:E8. doi: 10.1542/peds.108.1.e8. [DOI] [PubMed] [Google Scholar]