Abstract
Background:
Establishment of a consistent bedtime routine (the activities that occur right before lights out) is often recommended as part of healthy sleep habits. However, no studies have investigated the dose-dependent association of a bedtime routine with sleep outcomes, especially in young children for whom they are particularly recommended. Thus, the aim of this study was to examine the associations of a consistent bedtime routine with sleep outcomes in young children (ages 0 through 5 y) in a large global sample and assess whether there is a dose-dependent relationship between the frequency of a bedtime routine both concurrently and retrospectively with sleep outcomes.
Participants:
Mothers of 10,085 children (Australia-New Zealand, Canada, China, Hong Kong, India, Japan, Korea, Malaysia, Philippines, Singapore, Thailand, United Kingdom, United States) completed the Brief Infant/Child Sleep Questionnaire.
Results:
A consistent bedtime routine was associated with better sleep outcomes, including earlier bedtimes, shorter sleep onset latency, reduced night wakings, and increased sleep duration. Decreased parent-perceived sleep problems and daytime behavior problems were also related to institution of a regular bedtime routine. Furthermore, there was a dose-dependent relationship, with better outcomes associated with increased “doses” of having a bedtime routine, both currently and retrospectively, and was found within both predominantly Asian and predominantly Caucasian cultural regions.
Conclusions:
These results indicate that having a regular nightly bedtime routine is associated with improved sleep in young children, and suggests that the more consistently a bedtime routine is instituted and the younger started the better.
Citation:
Mindell JA, Li AM, Sadeh A, Kwon R, Goh DY. Bedtime routines for young children: a dose-dependent association with sleep outcomes. SLEEP 2015;38(5):717–722.
Keywords: bedtime routine, infant, preschooler, sleep, toddler
INTRODUCTION
Sleep problems are one of the most common concerns of parents, occurring in approximately 20–30% of young children,1,2 and one of the most common behavioral issues brought to the attention of pediatricians.3,4 Not only do sleep issues tend to persist,5–7 but there is increasing evidence of the negative consequences of inadequate sleep quality and quantity in children, including cognitive and behavioral deficits that affect daytime functioning,8 as well as psychiatric and health outcomes, such as obesity and metabolic consequences.9,10 A bedtime routine is commonly recommended as part of healthy sleep habits, with more than 90% of pediatricians recommending it for their patients with sleep difficulties.3 However, there is limited research on the importance of a bedtime routine and its effect on outcomes.
Prior research has found that daily routines in general lead to predictable and less stressful environments for young children and are related to greater parenting sense of competence and improved daytime behaviors.11 A bedtime routine is one such daily family routine and consists of parents engaging their child in the same activities in the same order on a nightly basis prior to lights out. It is expected that a bedtime routine, similar to other daily routines, will improve behavior and result in better sleep. A few broader studies on sleep in young children have noted that bedtime routines are associated with less sleep disruption and longer total sleep time.2,12,13 In addition, a study of language-based bedtime routines at age 3 y, that is, one that includes reading, singing, or other verbal communication, was associated with increased nighttime sleep duration and cognitive development at age 5 y.14 This study, however, did not assess the effect of any bedtime routine on future outcomes. Furthermore, one study found that institution of a bedtime routine for infants and toddlers was efficacious in improving sleep disturbances.15 Overall, though, no studies have looked specifically at whether there is a dose-dependent relationship between bedtime routines and sleep outcomes.
Thus, the primary objectives of the current study were to (1) examine the associations of a consistent bedtime routine with sleep outcomes in young children (ages birth through 5 y) in a large global sample, and further to (2) assess whether there is a dose-dependent relationship between the frequency of a bedtime routine both concurrently and retrospectively with sleep outcomes.
METHODS
Participants
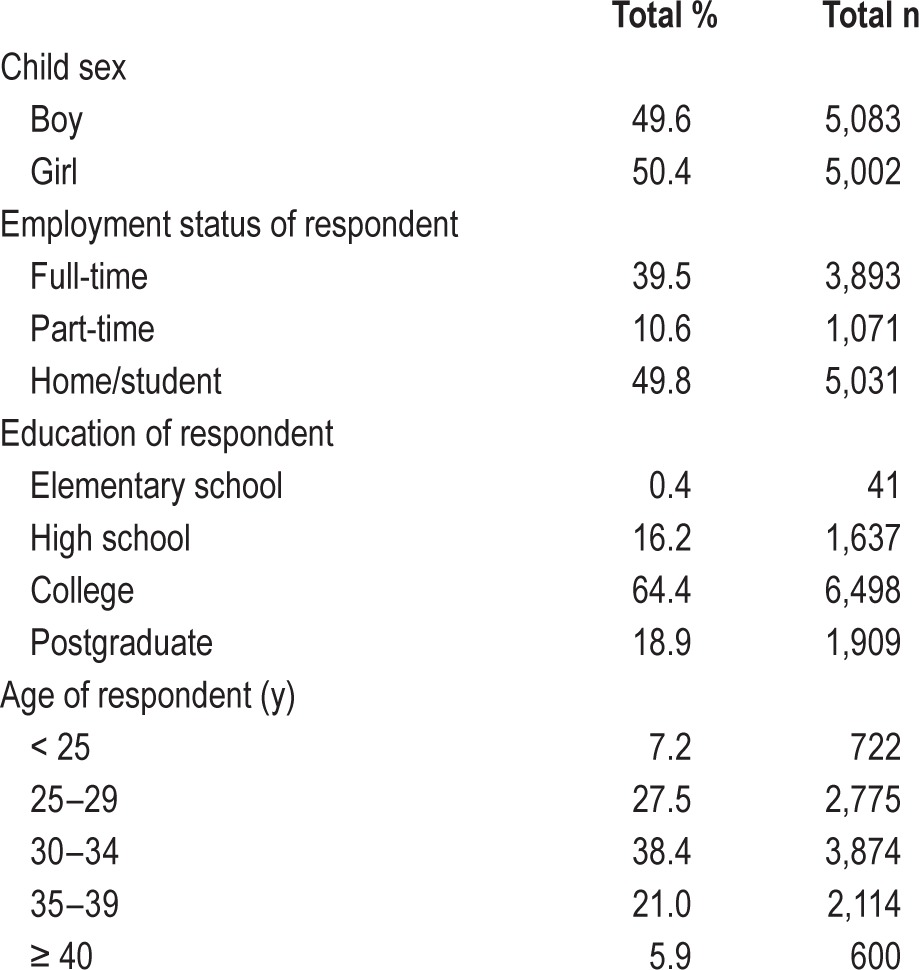
A sample of 10,085 mothers of children ages 0 through 5.11 y (830 Australia-New Zealand/AUNZ, 749 Canada/CA, 1,215 China/CN, 586 Hong Kong/HK, 998 India/IN, 499 Japan/JP, 712 South Korea/KR, 513 Malaysia/MY, 396 Philippines/PH, 449 Singapore/SG, 565 Thailand/TH, 1,238 United Kingdom/UK, and 1,335 United States/US) participated in this study. In the sample, there were 7,499 children ages 0–35 mo (infants/ toddlers) and 2,586 children 36–59 mo (preschoolers). Demographic data for the entire sample are provided in Table 1.
Table 1.
Demographics.
Procedure
All participants completed the Brief Infant/Child Sleep Questionnaire (BISQ/BCSQ). The BISQ has been validated against actigraphy and daily logs and its sensitivity in documenting expected developmental changes in infant sleep and the effects of environmental factors has been established.16 The BISQ has been used in previous cross-cultural studies.17 The BCSQ is based on the BISQ, and includes additional age-appropriate questions.18 Both questionnaires include specific questions about daytime and nighttime sleep patterns, as well as sleep related behaviors. The mothers were asked to describe their child's behavior during the previous 2 w. Specific to the aim of this paper, all were asked “In a typical week, how often does your child have a regular bedtime routine?” with answer choices including “never,” “1–2 nights/w,” “3–4 nights/w, “5–6 nights/w,” and “every night.” Additionally, all parents were asked “Do you consider your child's sleep as a problem?” Mothers of preschoolers were also asked “When your child was a baby (3 to 12 mo old), did he/she have a regular bedtime routine?” with answer choices of “yes,” “no,” and “don't remember,” as well as one question regarding their child's daytime behavior (“Does your child have (or is suspected to have) problems of hyperactivity, attention deficit, or difficult behaviors, i.e. either you, a caregiver, teacher or medical professional has suggested or suspected that your child may have a behavior problem?”). Both the BISQ and BCSQ have been validated against sleep diaries and actigraphy.16,19,20
The questionnaire was translated into each language and backtranslated to check for accuracy. All data were collected online. In almost all countries/regions, the questionnaire was set as a pop-up screen at a popular parenting website (Baby-Center) and invited mothers to complete a sleep survey. In two countries (Japan and Korea), recruitment was conducted via email using mailing lists obtained from local marketing firms and online advertising at other parenting sites. Completion of the questionnaire was voluntary and there were no exclusionary criteria. This study was approved by a university-based Institutional Review Board and all participants provided informed consent. No identifying information was collected. A few areas offered incentives for completion (e.g., free samples or gift voucher), and participants were asked to provide their email address at the end of the survey if they were interested. The complete sample was collected between February 2011 and March 2012. A complete description of the methodology can be found in previous reports.18,21
In addition to the BISQ/BCSQ, demographic information was collected, including maternal age, maternal education, and employment status. For quality control, responses were limited to avoid inappropriate or extreme data (e.g., sleep onset before bedtime, total nighttime sleep < 5 h or > 14 h).
Statistical Analyses
Means and frequencies were used for demographic information. Analysis of covariance (ANCOVA), covarying for child age and maternal education, was used for all sleep variables, with effect sizes (partial eta-squared) reported for all comparisons. Maternal education was included as a covariate given demographic differences across countries/regions. Analyses were performed across frequency of bedtime routine (“never,” “1–2 nights/w,” “3–4 nights/w, “5–6 nights/w,” and “every night”) for the following continuous variables as sleep outcomes: (1) bedtime, (2) sleep onset latency, (3) duration and number of night wakings, (4) nighttime sleep, and (5) total sleep time across 24 h. Chi-square analyses were conducted for categorical variables, including parent-perceived sleep problems and daytime behavioral difficulties. Missing data were handled using pairwise deletion, as there were minimal missing data (98.5–100% of data were present across all variables) and data were missing completely at random. Because of the large cohort size and the multiple analyses, findings were considered significant if P < 0.001. All data were analyzed by the first author (JAM) using SPSS version 20 (IBM).
RESULTS
Bedtime Routine
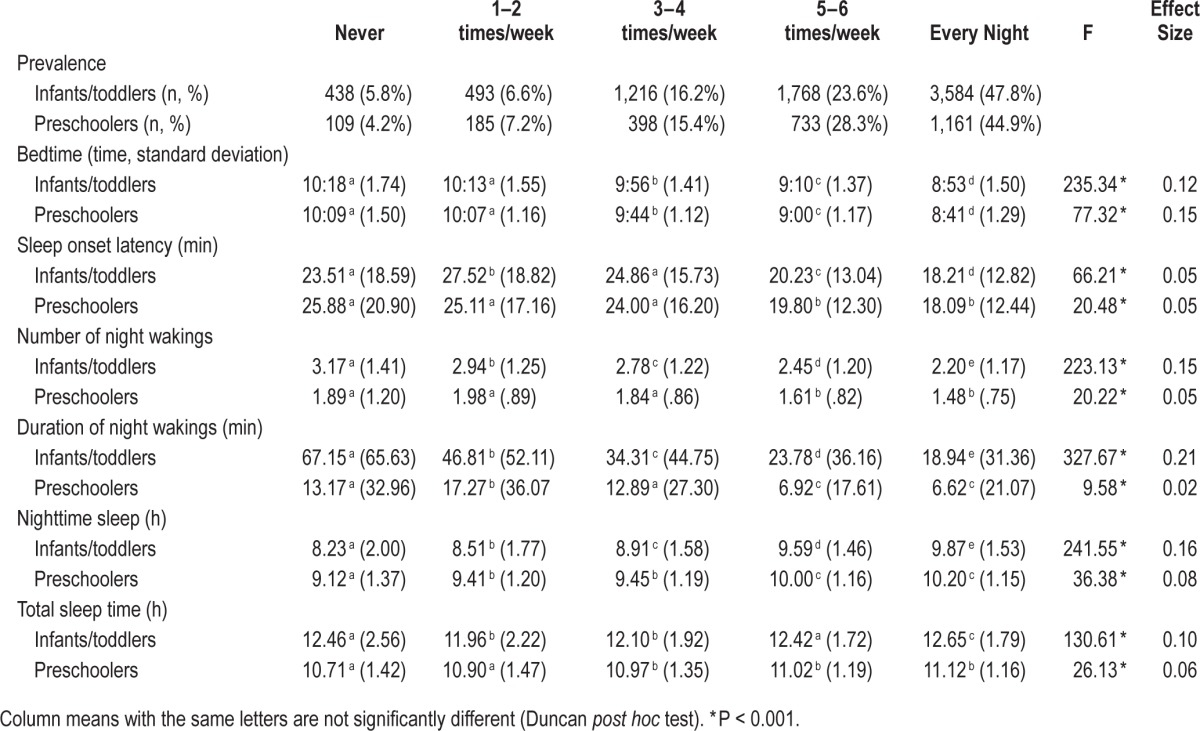
The frequency of mothers reporting a consistent bedtime routine is presented in Table 2, with approximately half of all families reporting a bedtime routine occurring less than every night. Furthermore, mothers of preschoolers reported that 71.9% (n = 1,859) had a regular bedtime routine as an infant, 21.9% (n = 567) did not have a bedtime routine, and 6.1% (n = 159) did not remember. Furthermore, 82.0% of those pre-schoolers with a current bedtime routine also reported having a routine in infancy (0–12 mo), whereas 61.1% of preschoolers without a current routine reported having a routine in infancy, χ2 = 112.38, P < 0.001. Similarly, of those reporting a bedtime routine during infancy, 79.7% have a current bedtime routine compared to 57.5% without a routine during infancy.
Table 2.
Dose-dependency of sleep outcomes by frequency of current bedtime routine.
Having a consistent bedtime routine, as defined by three or more times per week, was more common in predominantly Caucasian countries (82.6%; AUNZ, CA, US, UK) than in predominantly Asian countries (64.4%; CN, HK, IN, JP, KR, MY, PH, SG, TH), although it is important to note that all relationships described in the following paragraphs were found within each of these cultural groups. No differences were found in frequency of current bedtime routine by child gender, χ2 = 2.77, P = 0.597.
Sleep Patterns
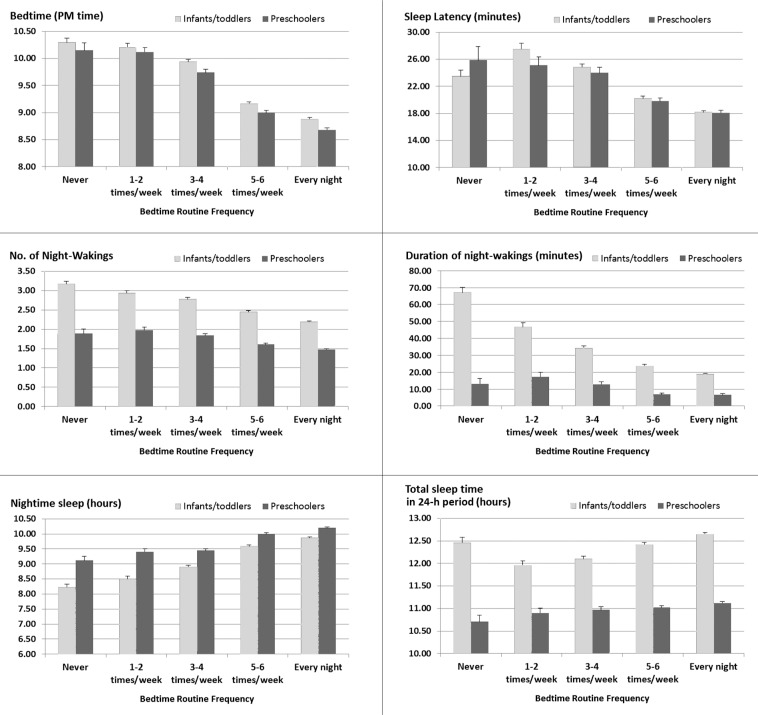
Data for sleep patterns by frequency of a current bedtime routine are presented in Table 2 and Figure 1. Overall, in both age groups, children with a consistent bedtime routine have earlier bedtimes, shorter sleep onset latency, fewer number and duration of night wakings, more nighttime sleep, and more total sleep per 24 h, all P's < 0.001. Post hoc tests indicate that there is a linear relationship between the frequency of a bedtime routine and sleep outcomes, although “one to two times/w” had the worst outcomes for a few variables. Furthermore, the variability of the sleep outcomes decreases with increased frequency of a nightly bedtime routine.
Figure 1.
Dose-dependency of sleep outcomes by frequency of current bedtime routine.
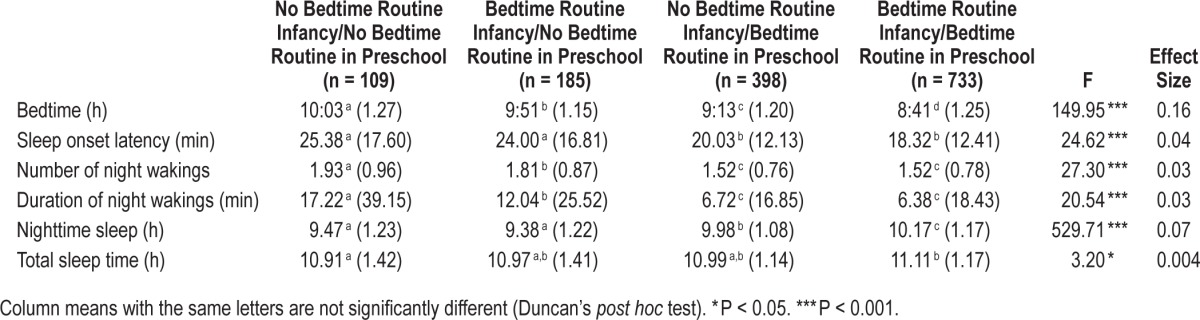
For preschool-aged children we further examined the effect of having a current bedtime routine (defined as having a bedtime routine 3 or more nights/w) in relationship to having reported a bedtime routine as an infant on sleep outcomes (see Table 3). There was a similar dose-dependent relationship in that children with a current routine as well as a routine as an infant were found to have the best sleep outcomes, all P's < 0.001. That is, there was again a linear progression for all sleep outcomes (except total sleep duration) at each step from infant no/current no to infant yes/current no to infant no/ current yes, followed by the best outcomes at infant yes/current yes.
Table 3.
Sleep outcomes by current and past bedtime routine.
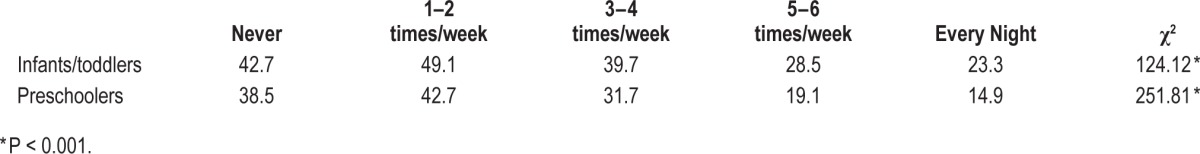
Bedtime Routines and Sleep Problems
In addition to differences in sleep patterns, there were also significant differences in parent-reported sleep problems (see Table 4). For infants/toddlers, parents' perception that their child has a sleep problem ranged from 23.3% for those with a bedtime routine “every night” to 47.2% for those who “never” have a bedtime routine, χ2 = 124.12, P < 0.001, and from 14.9% (“always”) to 38.5% (“never”) for preschoolers, χ2 = 251.81, P < 0.001. Sleep problems increased in a linear progression with decreases in bedtime routine frequency per week. There was a similar relationship in the perception of sleep problems for preschool-aged children in terms of parental report of whether their child currently had a bedtime routine and whether their child had a bedtime routine as an infant. Preschoolers with a current bedtime routine and a routine as an infant were equally likely to report a current sleep problem (16.0%) compared to those with a current bedtime routine and no infant routine (16.3%). However, those with no current bedtime routine were more likely to report a current sleep problem whether (33.6%) or not they had a routine for their child during infancy (36.1%), χ2 = 96.68, P < 0.001.
Table 4.
Percent parent-defined sleep problem by frequency of current bedtime routine.
Bedtime Routines and Daytime Problems
Parents of preschoolers with a current bedtime routine were less likely to report current daytime behavior problems (including problems of hyperactivity, attention deficit, or difficult behaviors) than those without a bedtime routine (10.1% versus 17.9%, respectively), χ2 = 28.56, P < 0.001. A dose-dependent relationship between daytime behaviors and a bedtime routine was again found (never = 22.9%, one to two times/w = 18.4%, three to four times/w = 16.3%, five to six times/w = 11.9%, and every night = 9.1%), χ2 = 35.10, P < 0.001. Similarly, parents who reported having a bedtime routine for their child as an infant were less likely to report current behavior problems (10.1%) than those without a routine during infancy (15.7%), χ2 = 13.70, P < 0.001. The relationship between having a routine as an infant and a current routine was again dose-dependent, with decreasing report of behavior problems with institution of a bedtime routine at an early age (infant no/current no = 19.9%, infant yes/current no = 14.6%, infant no/current yes = 12.6%, and infant yes/current yes = 8.9%), χ2 = 30.59, P < 0.001.
DISCUSSION
The results of this study suggest that having a consistent nightly bedtime routine is associated with better sleep in young children, as manifested in earlier bedtimes, shorter sleep onset latency, decreased wakefulness after sleep onset, more total sleep, and decreased parent-perceived sleep problems, as well as report of decreased daytime behavior problems. The frequency of having a bedtime routine is also important and demonstrates a dose-dependent relationship, with better sleep outcomes associated with the more nights a week that a routine is implemented. Furthermore, instituting a bedtime routine during infancy also demonstrates a dose-dependent relationship in sleep outcomes at a later age, with those having a bedtime routine as an infant and later in childhood demonstrating the best sleep and behavioral outcomes, although it is not associated with parental report of a current sleep problem.
This is the first study that we know of that demonstrates that there is a dose-dependent relationship between bedtime routines and better sleep outcomes. As discussed earlier, previous studies have noted a relationship between bedtime routines and sleep outcomes. In one study of 5,006 infants and toddlers, a bedtime routine was found to negatively predict night wakings and positively predict longest continuous sleep period.2 Another study found that for children ages 3 to 10 y, but not for the younger infants and toddlers, that those with a consistent bedtime routine were reported to obtain more sleep.12 A final study noted that instituting a bedtime routine for infants and toddlers resulted in improved sleep, both at bedtime and throughout the night, compared to controls.15 It is important to note that these relationships were found in our study across all age groups, including infants, toddlers, and preschoolers, and also were found in a large global sample representing diverse cultures. However, in a few instances sleep outcomes were slightly better for those who “never” have a sleep routine compared to those with a bedtime routine just one to two times per week, although both scenarios resulted in the poorest outcomes for all variables. It may be that such inconsistency in instituting a bedtime routine results in more disturbed sleep, although this finding was apparent for only a few variables. Similarly, for older children, instituting a bedtime routine as an infant predicted better sleep outcomes in later ages, but our findings suggest that having a current routine is what is most important.
Interestingly, not only was having a bedtime routine associated with earlier bedtimes and shorter sleep onset latency as would be expected, but it was also associated with a decrease in night wakings. Thus, there is a question as to the mechanism for the association between bedtime routines and overall improved sleep. One possibility may be that bedtime routines in and of themselves are beneficial, decreasing bedtime stress (e.g., separation stress, fears) and arousal levels that affect both bedtime and throughout the night. Another possibility is that bedtime routines are a marker of overall parent behavior management, with those parents having a regular bedtime routine more likely to engage in other positive sleep practices, such as early bedtimes, encouragement of independent sleep, and engaging in parental limit-setting. Other studies have shown that daily routines are efficacious in decreasing overall behavior problems.11 Lack of a consistent bedtime routine may also be a marker of chaotic households, which would also have an effect on bedtimes and sleep duration. There is support for this hypothesis, given that there was significantly higher variability for all sleep measures for those with less frequent bedtime routines. Finally, a child with an easy temperament, who is more likely to be able to self-regulate and self-soothe, may also be more compliant with a bedtime routine. In contrast, a child with attention-deficit/hyperactivity disorder or a disruptive behavior disorder could affect the ability for parents to successfully implement routines at bedtime.
It is important to emphasize that all these associations between bedtime routine and sleep measures were found while controlling for the child's age and maternal education. Higher maternal education has been linked to higher socioeconomic status and increased parenting skills and knowledge.22,23 Furthermore, higher education and socioeconomic status have been linked to higher adoption of bedtime routines and better sleep.24,25 The fact that, in our study, the links between bedtime routines and sleep outcomes remain valid after controlling for maternal education supports the interpretation that there are underlying basic, perhaps physiological, links between these domains. Although causal interpretation cannot be made from our correlational findings, intervention studies strongly support the causal link between bedtime routines and sleep outcomes.15
There are a number of limitations to this study. First, this study was based on parental report without an objective measure of sleep, such as actigraphy. Future studies should include such additional measures. Second, there may have been perceptual differences in the interpretation of what constitutes a consistent bedtime routine that may have affected the results. Furthermore, asking about whether a bedtime routine was instituted during infancy relied on parental report of past behaviors, and there may be biases in recall. That is, parents of children with current sleep problems may report lack of routines in the past, although this may not be the case. However, if biased recall was an issue it is unlikely that such dose-dependent outcomes would have been observed. To further test this question, longitudinal studies should be conducted to eliminate the possibility of biased recall. An additional limitation was that the mothers were not asked about the specifics of their bedtime routine, so we are not able to comment on whether any bedtime routine would be associated with improved sleep or whether there are specific aspects of a routine that may result in better outcomes, such as inclusion of a bath (which may affect core body temperature). Further evaluation of specific components of bedtime routines would help elucidate whether there are specific aspects that are associated with more or less improvement in sleep. Finally, as with all Internet-based surveys, the cohort in this study is skewed toward higher education but was likely consistent across all countries and we believe that we obtained similar segments of the population within each country/ region. In addition, these results are likely not representative of all families within each country. We expect that this sample represents more urban-based populations, especially in the predominantly Asian countries, given the need for internet access to participate.
Overall, this study found that a consistent nightly bedtime routine is associated with better sleep outcomes in infants, toddlers, and preschool-aged children. Furthermore, there appears to be a dose-dependent relationship, in that the more often a bedtime routine occurs the better the outcomes, and instituting it early on during infancy results in better outcomes at an older age. The recommendation of a consistent bedtime routine can be easily adopted by pediatric providers. There appears to be no negative cost to a bedtime routine, and such a recommendation is a simple message that parents can easily implement and one that requires minimal practitioner time.
DISCLOSURE STATEMENT
This study was supported by Asia Pacific Pediatric Sleep Alliance (APPSA) and sponsored by Johnson & Johnson Consumer & Personal Products Worldwide, a division of Johnson & Johnson Consumer Companies, Inc. Dr. Mindell has served as a consultant and speaker for Johnson & Johnson. Dr. Sadeh has served as a consultant for Johnson & Johnson. Dr. Goh has served as a speaker for Johnson & Johnson. Robert Kwon is an employee of Johnson & Johnson. Dr. Li has indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was supported by Asia Pacific Pediatric Sleep Association (APPSA) and sponsored by Johnson & Johnson Consumer & Personal Products Worldwide, a division of Johnson & Johnson Consumer Companies, Inc. Dr. Mindell has served as a consultant and speaker for Johnson & Johnson. Dr. Sadeh has served as a consultant for Johnson & Johnson. Dr. Goh has served as a speaker for Johnson & Johnson. Mr. Kwon is an employee of Johnson & Johnson. Dr. Mindell had full access to all the data in the study and takes responsibility for the integrity of the data and was responsible for all data analyses.
REFERENCES
- 1.Mindell JA, Kuhn BR, Lewin DS, Meltzer LJ, Sadeh A, Owens JA. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep. 2006;29:1263–76. [PubMed] [Google Scholar]
- 2.Sadeh A, Mindell JA, Luedtke K, Wiegand B. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18:60–73. doi: 10.1111/j.1365-2869.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 3.Mindell JA, Moline ML, Zendell SM, Brown LW, Fry JM. Pediatricians and sleep disorders: training and practice. Pediatrics. 1994;94:194–200. [PubMed] [Google Scholar]
- 4.Owens JA. The practice of pediatric sleep medicine: results of a community survey. Pediatrics. 2001;108:e51. doi: 10.1542/peds.108.3.e51. [DOI] [PubMed] [Google Scholar]
- 5.Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics. 2012;129:e276–84. doi: 10.1542/peds.2011-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jenni OG, Fuhrer HZ, Iglowstein I, Molinari L, Largo RH. A longitudinal study of bed sharing and sleep problems among Swiss children in the first 10 years of life. Pediatrics. 2005;115:233–40. doi: 10.1542/peds.2004-0815E. [DOI] [PubMed] [Google Scholar]
- 7.Roberts RE, Roberts CR, Duong HT. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42:294–302. doi: 10.1016/j.jadohealth.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011;58:649–65. doi: 10.1016/j.pcl.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Arch Pediatr Adolesc Med. 2010;164:840–5. doi: 10.1001/archpediatrics.2010.143. [DOI] [PubMed] [Google Scholar]
- 10.Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev. 2012;16:231–41. doi: 10.1016/j.smrv.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiese BH, Tomcho TJ, Douglas M, Josephs K, Poltrock S, Baker T. A review of 50 years of research on naturally occurring family routines and rituals: cause for celebration? J Fam Psychol. 2002;16:381–90. doi: 10.1037//0893-3200.16.4.381. [DOI] [PubMed] [Google Scholar]
- 12.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10:771–9. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 13.Koulouglioti C, Cole R, Moskow M, McQuillan B, Carno MA, Grape A. The longitudinal association of young children's everyday routines to sleep duration. J Pediatr Health Care. 2014;28:80–7. doi: 10.1016/j.pedhc.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Hale L, Berger L, Lebourgeois MK, Brooks-Gunn J. A longitudinal study of preschoolers' language-based bedtime routines, sleep duration, and well-being. J Fam Psychol. 2011;25:423–33. doi: 10.1037/a0023564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mindell JA, Telofski LS, Wiegand B, Kurtz E. A nightly bedtime routine: impact on sleep problems in young children and maternal mood. Sleep. 2009;32:599–606. doi: 10.1093/sleep/32.5.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113:e570–7. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 17.Mindell JA, Sadeh A, Wiegand B, How TH, Goh DY. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010;11:274–80. doi: 10.1016/j.sleep.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 18.Mindell JA, Sadeh A, Kwon R, Goh DY. Cross-cultural differences in the sleep of preschool children. Sleep Med. 2013;14:1283–9. doi: 10.1016/j.sleep.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Tikotzky L, Sadeh A. Sleep patterns and sleep disruptions in kindergarten children. J Clin Child Psychol. 2001;30:581–91. doi: 10.1207/S15374424JCCP3004_13. [DOI] [PubMed] [Google Scholar]
- 20.Kushnir J, Sadeh A. Correspondence between reported and actigraphic sleep measures in preschool children: the role of a clinical context. J Clin Sleep Med. 2013;9:1147–51. doi: 10.5664/jcsm.3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mindell JA, Sadeh A, Kwon R, Goh DY. Cross-cultural comparison of maternal sleep. Sleep. 2013;36:1699–706. doi: 10.5665/sleep.3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carr A, Pike A. Maternal scaffolding behavior: links with parenting style and maternal education. Dev Psychol. 2012;48:543–51. doi: 10.1037/a0025888. [DOI] [PubMed] [Google Scholar]
- 23.Tamis-Lemonda CS, Briggs RD, McClowry SG, Snow DL. Maternal control and sensitivity, child gender, and maternal education in relation to children's behavioral outcomes in African American families. J Appl Dev Psychol. 2009;30:321–31. doi: 10.1016/j.appdev.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children's sleep problems: multiple indicators and moderation of effects. Health Psychol. 2013;32:849–59. doi: 10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. Social and demographic predictors of preschoolers' bedtime routines. J Dev Behav Pediatr. 2009;30:394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]