Abstract
Study Objective:
The trend in sleep duration in the United States population remains uncertain. Our objective was to examine changes in sleep duration from 1985 to 2012 among US adults.
Design:
Trend analysis.
Setting:
Civilian noninstitutional population of the United States.
Participants:
324,242 US adults aged ≥ 18 y of the National Health Interview Survey (1985, 1990, and 2004–2012).
Measurements and Results:
Sleep duration was defined on the basis of the question “On average, how many hours of sleep do you get in a 24-h period?” The age-adjusted mean sleep duration was 7.40 h (standard error [SE] 0.01) in 1985, 7.29 h (SE 0.01) in 1990, 7.18 h (SE 0.01) in 2004, and 7.18 h (SE 0.01) in 2012 (P 2012 versus 1985 < 0.001; P trend 2004–2012 = 0.982). The age-adjusted percentage of adults sleeping ≤ 6 h was 22.3% (SE 0.3) in 1985, 24.4% (SE 0.3) in 1990, 28.6% (SE 0.3) in 2004, and 29.2% (SE 0.3) in 2012 (P 2012 versus 1985 < 0.001; P trend 2004–2012 = 0.050). In 2012, approximately 70.1 million US adults reported sleeping ≤ 6 h.
Conclusions:
Since 1985, age-adjusted mean sleep duration has decreased slightly and the percentage of adults sleeping ≤ 6 h increased by 31%. Since 2004, however, mean sleep duration and the percentage of adults sleeping ≤ 6 h have changed little.
Citation:
Ford ES, Cunningham TJ, Croft JB. Trends in self-reported sleep duration among US adults from 1985 to 2012. SLEEP 2015;38(5):829–832.
Keywords: health surveys, sleep, trends
INTRODUCTION
Sleep duration is thought to have declined in many modern-day societies.1,2 In the United States, for example, limited data indicate that the prevalence of adults who sleep ≤ 6 h may have increased over time.3–6 However, a review of studies from the United States concluded that the available information painted an uncertain picture.7
Because the impetus for public health interventions to address sleep health depends on a thorough knowledge of its epidemiology, additional information about trends in sleep duration in the United States population is desirable. Consequently, our objective was to examine the trend in self-reported sleep duration among US adults from 2004 to 2012. To provide a longer-term perspective, we also compared data from 2004– 2012 to that for 1985.
METHODS
This analysis is based on data from the National Health Interview Survey for the years 1985, 1990, and 2004–2012.8 Potential participants were selected using a multistage area probability design and were representative of the civilian noninstitutionalized US population. During the first stage, a sample of primary sampling units (PSUs) consisting of a county, a small group of contiguous counties, or a metropolitan statistical area was drawn from the universe of PSUs. During the second stage, a sample of area segments comprising eight, 12, or 16 addresses and permit segments composed of housing units built after a census is drawn from the selected PSUs. One adult was randomly selected from each family. Interviews were conducted in participants' homes. The response rates for adult sample persons were 90% in 1985 and 83.4% in 1990, and ranged from 60.8% in 2010 to 72.5% in 2004. Detailed information about the designs of the surveys and changes to the designs can be found elsewhere.9–11
Sleep duration was assessed with the question “On average, how many hours of sleep do you get in a 24-h period?” Answers were given in whole hours. We included age, sex, and race or ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other) as covariates.
Only adults aged ≥ 18 y were included in the analyses. We calculated age-adjusted estimates using the direct method with the year 2000 projected US population as the standard (18–24 y, 25–34 y, 35–44 y, 45–54 y, 55–64 y, 65–74 y, and ≥ 75 y). Tests for linear trends were calculated by using orthogonal linear contrast coefficients. Prevalence ratios (PR) and 95% confidence interval (CI) were calculated by using log-linear regression that included all covariates. The statistical software programs SAS (SAS Institute Inc., Cary, NC) and SUDAAN (RTI International, Research Triangle Park, NC) were used to conduct the analyses to account for the complex sampling design of the surveys.
RESULTS
Of the 33,630 and 41,104 participants in 1985 and 1990, respectively, 33,239 and 40,892 had a value for sleep duration. For the years 2004–2012, a total of 254,630 participants aged ≥ 18 y were asked about their sleep duration, and 250,111 had a useable value. Mean age increased significantly (P trend < 0.001), the percentage of non-Hispanic white participants declined significantly (P trend < 0.001), and the percentage of men remained stable.
The age-adjusted mean sleep duration was 7.40 h (95% CI: 7.38–7.41) in 1985 and was 7.18 h (95% CI: 7.16–7.20) in 2012 (Table S1, supplemental material). Compared with mean sleep duration in 1985, means in 2012 were significantly (P < 0.001) lower among all adults (−0.22 h), men (−0.19 h), women (−0.25 h), non-Hispanic Whites (−0.20 h), non-Hispanic Blacks (−0.44 h), Hispanics (−0.12 h), and in all age groups except ages ≥ 75 y). In addition, there were significant declines (P < 0.001) among non-Hispanic White men (−0.19 h) and women (−0.21 h), non-Hispanic Black men (−0.35 h) and women (−0.50 h), Hispanic women (−0.16 h), and non-Hispanic other men (−0.22 h) and women (−0.29 h). Assuming a US resident population of approximately 240 million in 2012, an average loss of 0.22 h or 13 min would translate into approximately 52.8 million h of sleep having been lost. Since 2004, however, the age-adjusted mean sleep duration changed little (P trend = 0.982).
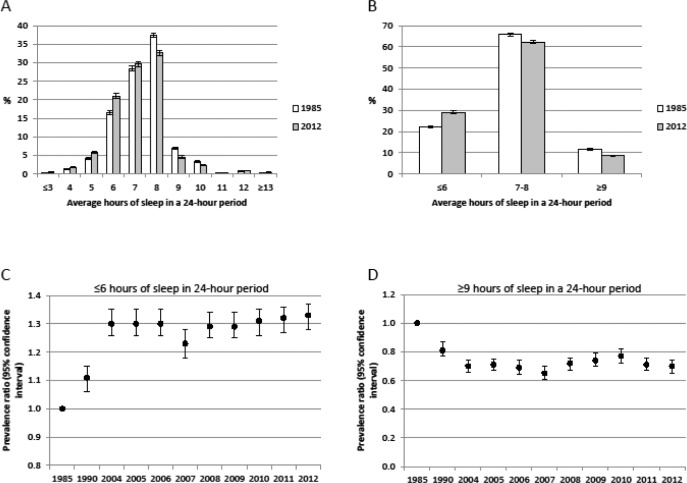
The distribution of sleep duration between 1985 and 2012 differed significantly (P < 0.001) (Figure 1A). Compared with 1985, the increase in the percentage of adults who reported sleeping ≤ 6 h in a 24-h period in 2012 was accompanied by decreases in the percentages of adults who reported sleeping 7–8 and ≥ 9 h in a 24-h period (P < 0.001) (Figure 1B).
Figure 1.
Temporal changes in sleep duration among US adults aged ≥ 18 y, National Health Interview Survey. (A) Shift in the detailed age-adjusted distributions of sleep duration. (B) Shift in the age-adjusted distributions of sleep duration using three categories. (C) The age-adjusted prevalence ratios (95% confidence interval) for sleep ≤ 6 h in a 24-h period. (D) The age-adjusted prevalence ratios (95% confidence interval) for sleep ≥ 9 h in a 24-h period.
The age-adjusted percentages of sleeping ≤ 6 h were 22.3% in 1985, 28.6% in 2004, and 29.2% in 2012 (Table S2, supplemental material). The unadjusted and age-adjusted prevalence ratios for 2012 compared with 1985 were 1.33 (95% CI: 1.28, 1.37) and 1.33 (95% CI: 1.28, 1.37), respectively (Figure 1C), and the prevalence ratio for 2012 compared to 1985 remained similar after adjustment for age, sex, and race or ethnicity (PR = 1.32, 95% CI: 1.27, 1.37). The age-adjusted prevalence ratio for 2012 versus 2004 was 0.98 (95% CI: 0.95, 1.01). The associations between time in years and sleep duration ≤ 6 h varied significantly by sex (P interaction = 0.002) and by race or ethnicity (P interaction = 0.014). The associations of age, sex, and race or ethnicity with short sleep duration for data aggregated from 2004 to 2012 are shown in Figure S1 (supplemental material.
The unadjusted percentage of participants who reported sleeping on average ≤ 6 h in a 24-h period was significantly higher in 2012 (29.2%) than in 1985 (22.0%) (P < 0.001). Thus, approximately 38.6 million US adults, using the resident population, reported sleeping ≤ 6 h in a 24-h period in 1985, and 70.1 million US adults reported sleeping ≤ 6 h in a 24-h period in 2012.
In 2012, 62.3% of adults reported sleeping 7–8 h in a 24-h period after age adjustment compared with 65.9% in 1985 (P < 0.001) and with 62.8% in 2004 (P trend = 0.004). The significant decline between 1985 and 2012 was observed among men, women, most age groups, and non-Hispanic Whites (Table S3, supplemental material). An increase in sleeping 7–8 h was observed among adults aged ≥ 75 y (P = 0.004). Al -though the estimates from 2004 to 2012 showed slight variation in most demographic groups, the tests for trend for several demographic subgroups suggested an overall decline in the percentage during the period.
The age-adjusted percentages of adults who reported sleeping ≥ 9 h in a 24-h period were 11.9% in 1985, 8.6% in 2004, and 8.6% in 2012 (Table S4, supplemental material). The estimate for 2012 was significantly lower than that for 1985 in all participants (P < 0.001) and in most subgroups. No signifi-cant trend from 2004 to 2012 was observed (Figure 1D). The associations between time and sleep duration varied significantly by sex (P interaction = 0.647) and by race or ethnicity (P interaction < 0.001).
Trends in sleep duration by educational status are shown in Table S5, supplemental material.
DISCUSSION
Our analyses indicate that the mean reported sleep duration and the percentage sleeping ≤ 6 h in a 24-h period changed little during the period from 2004 to 2012. White men reported sleeping on average 3 min more in 2012 than in 2004, and non-Hispanic Black men reported sleeping on average 8 fewer min than in 2004. Compared to 1985, however, mean sleep duration and the percentage of adults who reported sleeping ≤ 6 h in a 24-h period declined significantly.
Limited information about trends in sleep duration in the US population has been published. Previous studies have provided mixed findings about the trend in sleep duration in the United States.7 Infographics using data from the National Health Interview Survey (NHIS) showed that the percentage of adults sleeping ≤ 6 h was higher in 2004 or 2006 than in 1985.3,4 Our results showing an increase in the percentage of adults who reported sleeping ≤ 6 h in a 24-h period in each year from 2004 to 2012 compared to 1985 are consistent with those findings and build on those findings by expanding the time horizon. From 2004 to 2012, however, sleep duration generally changed little. Because participants in the NHIS were asked to report the time spent sleeping during a 24-h period, it is conceivable that participants may have included the time spent napping in their responses. A subsequent study from 1975 to 2006 examined data from eight national datasets that contained information from time diaries.5 Based on all available data, no significant linear trend was observed, but some periods had a higher percentage of adults who slept ≤ 6 h than adults in 1975. When the data were stratified by employment status, the percentage of full-time workers who slept ≤ 6 h was higher during 1998–1999 and later years. Thus, this study did not yield convincing evidence that the percentage of short sleepers had changed between 1975 and 2006. In Alameda County, the percentage of participants who slept < 7 h per night increased from 15% in 1965 to 25% in 1999 among white participants, from 26% to 54% among African American participants, and from 12% to 37% among Hispanic participants.12 More recently, an analysis of time-use surveys showed a decrease in the percentage of short sleep duration from 1985 (11.7%) to 2007 (9.2%).6
In light of the many adverse associations between insufficient sleep and health outcomes, the loss of sleep in many modern-day societies has caused considerable consternation. These decreases have been attributed to a host of reasons including competing interests for time with the advent of the electronic age and the many electronic toys and technology, increasing demands from work, increasingly harried lifestyles, and possible increases in perceived stress. It is unclear whether the recession of 2007 to 2009 and its lingering effects may have affected sleep duration. The age-adjusted mean sleep duration varied little from 2004 to 2012 as did the age-adjusted percentage of adults reporting sleeping < 7 h. Noteworthy is that the age-adjusted percentage reporting sleeping ≥ 9 h increased from 2007 to 2010 (P 2010 versus 2007 < 0.001) and then declined through 2012. Although the mean change in self-reported sleep duration comprised about 0.22 h or 13 min since 1985, the change in the prevalence of adults sleeping ≤ 6 h was more pronounced. Whether such changes are sufficient to adversely affect population health is unknown.
Our results show that the prevalence of long sleep duration decreased from 1985 to 2004 and subsequently changed little through 2012. Long sleep duration has been associated with poor health outcomes.13–17 If long sleep duration is causally related to adverse health outcomes, our results could suggest that the risk associated with long sleep duration may have decreased from 1985 to 2004. However, an analysis of time-use surveys showed that long sleep duration (> 9 h) in the United States had increased from 26.3% in 1985 to 37.5% in 2007.6
Large sample sizes and the representative nature of the data are important strengths of this study. The self-reported information about sleep duration is the chief limitation of this study. Although the question used in the NHIS has not been validated with tests such as polysomnography or actigraphy, similar questions have been routinely used in observational studies. Some efforts to examine the validity and reliability of simple self-reported questions about sleep duration have been made.18–23 Furthermore, sleep duration in the NHIS was not assessed from 1986 to 1989 and from 1991 to 2003, and thus pinpointing the exact survey year or time period when sleep duration may have changed was not feasible. Although the questions about sleep duration remained the same in the surveys included in our study, the redesigns of the NHIS including revisions to the questionnaire in 1997 may have affected the estimates.
In conclusion, self-reported sleep duration decreased from 1985 into the 2000s but changed little from 2004 to 2012. Additional data about sleep duration in the United States using other assessment methods would be helpful in gauging past and future changes in sleep duration. The National Institutes of Health suggest that healthy adults should sleep 7–8 h,24 and Healthy People 2020 includes an objective for ≥ 8 h of sleep for adults aged 18–21 y and ≥ 7 h for adults aged 22 y and older.25 Thus, reducing the percentage of adults who are not sleeping sufficiently remains an important public health objective.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. There was no off-label or investigational drug use.
SUPPLEMENTAL MATERIAL
Prevalence ratios (95% confidence limits) for associations of sleep duration ≤6 h in a 24-h period with age, gender, and race or ethnicity among adults aged ≥18 years, National Health Interview Survey 2004-2012. Prevalence ratios were adjusted for other two variables.
Visit www.journalsleep.org for supplemental tables Table S1–S5 (Microsoft Word format).
REFERENCES
- 1.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10:S3–6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Ferrie JE, Kumari M, Salo P, Singh-Manoux A, Kivimaki M. Sleep epidemiology--a rapidly growing field. Int J Epidemiol. 2011;40:1431–7. doi: 10.1093/ije/dyr203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Percentage of adults who reported an average of < 6 hours of sleep per 24-gour period, by sex and age group --- United States, 1985 and 2004. MMWR Morb Mortal Wkly Rep. 2005;54:933. [Google Scholar]
- 4.Centers for Disease Control and Prevention. QuickStats: percentage of adults aged > 18 tears who reported an average of < 6 hours of sleep† per 24-hour period, by sex and age group --- National Health Interview Survey, United States, 1985 and 2006. MMWR Morb Mortal Wkly Rep. 2008;57:209. [Google Scholar]
- 5.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975-2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bin YS, Marshall NS, Glozier N. Sleeping at the limits: the changing prevalence of short and long sleep durations in 10 countries. Am J Epidemiol. 2013;177:826–33. doi: 10.1093/aje/kws308. [DOI] [PubMed] [Google Scholar]
- 7.Bin YS, Marshall NS, Glozier N. Secular trends in adult sleep duration: a systematic review. Sleep Med Rev. 2012;16:223–30. doi: 10.1016/j.smrv.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. About the National Health Interview Survey. [Accessed 26 June 2014]. http://www.cdc.gov/nchs/nhis/about_nhis.htm.
- 9.National Center for Health Statistics. Design and estimation for National Health Interview Survey, 1985-1994. Vital Health Stat. 1989;2:1–33. [Google Scholar]
- 10.Centers for Disease Control and Prevention. 2004 National Health Interview Survey (NHIS) Public Use Data Release. [Accessed 26 June 2014]. http://www.cdc.gov/nchs/data/nhis/srvydesc.pdf.
- 11.Centers for Disease Control and Prevention. Design and Estimation for the National Health Interview Survey, 2006–2015. [Accessed 26 June 2014]. http://www.cdc.gov/nchs/data/series/sr_02/sr02_165.pdf.
- 12.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17:948–55. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 14.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33:414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 17.Guo X, Zheng L, Wang J, et al. Epidemiological evidence for the link between sleep duration and high blood pressure: a systematic review and meta-analysis. Sleep Med. 2013;14:324–32. doi: 10.1016/j.sleep.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Chen JC, Brunner RL, Ren H, et al. Sleep duration and risk of ischemic stroke in postmenopausal women. Stroke. 2008;39:3185–92. doi: 10.1161/STROKEAHA.108.521773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 20.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8:175–83. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]
- 21.Levine DW, Kripke DF, Kaplan RM, et al. Reliability and validity of the Women's Health Initiative Insomnia Rating Scale. Psychol Assess. 2003;15:137–48. doi: 10.1037/1040-3590.15.2.137. [DOI] [PubMed] [Google Scholar]
- 22.Signal TL, Gale J, Gander PH. Sleep measurement in flight crew: comparing actigraphic and subjective estimates to polysomnography. Aviat Space Environ Med. 2005;76:1058–63. [PubMed] [Google Scholar]
- 23.Girschik J, Heyworth J, Fritschi L. Reliability of a sleep quality questionnaire for use in epidemiologic studies. J Epidemiol. 2012;22:244–50. doi: 10.2188/jea.JE20110107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Institutes of Health, National Heart, Lung, and Blood Institute. How Much Sleep Is Enough? [Accessed 13 August 2013]. http://www.nhlbi.nih.gov/health/health-topics/topics/sdd/howmuch.html.
- 25.U.S. Department of Health and Human Serices. Sleep Health. [Accessed 26 June 2014]. http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=38.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Prevalence ratios (95% confidence limits) for associations of sleep duration ≤6 h in a 24-h period with age, gender, and race or ethnicity among adults aged ≥18 years, National Health Interview Survey 2004-2012. Prevalence ratios were adjusted for other two variables.