Abstract
Chronic inflammation is frequently associated with malignant growth and is thought to promote and enhance tumor progression, although the mechanisms which regulate this relationship remain elusive. We reported previously that interleukin (IL)-1β promoted tumor progression by enhancing the accumulation of myeloid-derived suppressor cells (MDSC), and hypothesized that inflammation leads to cancer through the production of MDSC which inhibit tumor immunity. If inflammation-induced MDSC promote tumor progression by blocking antitumor immunity, then a reduction in inflammation should reduce MDSC levels and delay tumor progression, whereas an increase in inflammation should increase MDSC levels and hasten tumor progression. We have tested this hypothesis using the 4T1 mammary carcinoma and IL-1 receptor (IL-1R)–deficient mice which have a reduced potential for inflammation, and IL-1R antagonist–deficient mice, which have an increased potential for inflammation. Consistent with our hypothesis, IL-1R–deficient mice have a delayed accumulation of MDSC and reduced primary and metastatic tumor progression. Accumulation of MDSC and tumor progression are partially restored by IL-6, indicating that IL-6 is a downstream mediator of the IL-1β–induced expansion of MDSC. In contrast, excessive inflammation in IL-1R antagonist–deficient mice promotes the accumulation of MDSC and produces MDSC with enhanced suppressive activity. These results show that immune suppression by MDSC and tumor growth are regulated by the inflammatory milieu and support the hypothesis that the induction of suppressor cells which down-regulate tumor immunity is one of the mechanisms linking inflammation and cancer.
Introduction
Epidemiologic and experimental evidence supports the concept that chronic inflammation promotes the development and progression of cancers (1, 2). Because inflammation is a complex process involving many effector cells and mediators, it is likely that inflammation facilitates tumor progression through multiple mechanisms. We have recently proposed that immune suppression may be one of these mechanisms, and have hypothesized that chronic inflammation causes immune suppression, which inhibits immune surveillance and/or tumor immunity thereby enhancing the proliferation of malignant cells (3, 4). This hypothesis was based on findings that chronic inflammation, through the production of the proinflammatory cytokine, interleukin (IL)-1β, facilitated tumor progression and simultaneously elevated a population of suppressor cells called myeloid-derived suppressor cells (MDSC; refs. 3, 5). MDSC are a heterogeneous mixture of immature myeloid cells that are potent inhibitors of antitumor immunity. They mediate their effects by inhibiting CD4+ and CD8+ T cell proliferation (6–10), by blocking natural killer cell activation (11, 12), by limiting dendritic cell maturation (13), and by polarizing immunity towards a type 2 phenotype (14). MDSC are found in many patients and experimental animals with cancer (3, 5–11, 13, 15–18), and their induction, expansion, and retention are driven by factors produced by tumor cells and tumor stroma, including potent inflammatory mediators, such as prostaglandin E2 (PGE2; ref. 4) and IL-1β (3, 5).
If inflammation-induced MDSC are a significant factor linking inflammation and cancer, then down-regulating inflammation should reduce MDSC levels and delay tumor progression. We are testing this hypothesis by perturbing the IL-1β signaling pathway in tumor-bearing mice and thereby manipulating the extent of inflammation. The agonists IL-1β and IL-1α bind to the IL-1 receptor (IL-1R) to induce inflammation, whereas the IL-1R antagonist (IL-1Ra), attenuates inflammation by inhibiting signal transduction through the IL-1R (19). The balance between IL-1β and IL-1Ra plays an important role in normal physiology, and a disruption of this balance may predispose to or enhance disease, as seen in chronic inflammatory bowel disease (20). An imbalance between IL-1β and IL-1Ra may be due to either overproduction of IL-1β or a deficiency in IL-1Ra, both leading to increased inflammation, as mice deficient for the IL-1Ra show a propensity for spontaneous inflammation (21). In contrast, deletion of the IL-1R reduces inflammation as shown by an increased susceptibility to infection with Listeria monocytogenes and the absence of IL-6, a downstream mediator of IL-1β (22).
We now show that IL-1R–deficient mice with 4T1 mammary carcinoma tumors have a delayed accumulation of MDSC and slower growing tumors as compared with wild-type 4T1 tumor–bearing mice. Conversely, MDSC in tumor-bearing mice deficient for the IL-1Ra accumulate more rapidly and are more potent suppressor cells. Because IL-6 is a key downstream mediator of the IL-1β–induced inflammation pathway, we also show that IL-6 restores the early accumulation of MDSC and facilitates tumor progression in IL-1R–deficient mice. These findings support the hypothesis that inflammation promotes malignant cell growth by inducing immune suppression, and show that decreased accumulation of MDSC is one of the mechanisms by which reducing inflammation delays tumor progression.
Materials and Methods
Mice
BALB/c mice were purchased from The Jackson Laboratory. TS1 and clone 4 mice on a BALB/c background and transgenic for T cell receptors reactive to influenza hemagglutinin peptides 110 to 119 restricted to I-Ed (23) and peptides 518 to 526 restricted to Kd (24, 25), respectively, were provided by Dr. E. Fuchs (Johns Hopkins University, Baltimore, MD). IL-1R−/− (22) and IL-1Ra−/− (26) mice, backcrossed to BALB/c mice for 10 to 12 generations, were provided by Drs. M. Kopf (Swiss Federal Institute of Technology, Switzerland) and J. Stuart (University of Tennessee Health Science Center, Memphis, TN), respectively. Transgenic and knockout mice were bred in the University of Maryland Baltimore County animal facility. Female mice <6 months of age were used for all experiments. All animal procedures were approved by the University of Maryland Baltimore County Institutional Animal Care and Use Committee.
Plasmids and nucleofection
4T1 cells were transfected with the BCMG/Neo/hIL-6 plasmid containing the human IL-6 gene (4T1/IL-6; ref. 27) using an Amaxa nucleofector instrument, the Nucleofector Solution V, and protocol T-24, according to the manufacturer’s protocols. Following transfection, cells were cultured for 48 h, washed with sterile PBS, and placed on G418 selection. 4T1/IL-6 transfectants stably secrete 1.5 ng/mL/5 × 105/24 h of human IL-6 (4T1/IL-6) as quantified by ELISA.
Cell lines
The 4T1 mammary carcinoma and 4T1/IL-1β cell lines were maintained as described (3, 28). The 4T1/IL-6 transfectants were grown in the same medium as the parental cells supplemented with 400 μg/mL of G418 (Sigma/Aldrich).
Reagents and antibodies
HA110–119 and HA518–526 peptides were synthesized in the Biopolymer Core Facility at the University of Maryland, Baltimore. Monoclonal antibodies Gr1-PE, CD11b-FITC, CD126-PE (IL-6R), rat IgG2α-PE isotype control, and rat IgG2α-FITC isotype control were from BD PharMingen. The arginase inhibitor, Nw-hydroxy-nor-L-arginine (nor-NOHA), and the nitric oxide (NO) inhibitor, NG-monomethyl-L-arginine (L-NMMA) were from Calbiochem.
IL-6 ELISA and cytokine analysis
Supernatants from 5 × 105 cells cultured in 3 mL of medium for 24 h were frozen at −80°C until assayed using a hIL-6 DuoSet ELISA kit according to the manufacturer’s instructions (R&D Systems). Plates were read at 420 nm on a Bio-Tek 311 microplate reader and quantified using a standard curve. Data are the mean ± SD of triplicate wells. Multiplex cytokine analysis for IFNγ, IL-12p70, monocyte chemoattractant protein (MCP-1), IL-6, IL-1β, tumor necrosis factor α (TNFα), and transforming growth factor-β (TGFβ) was done by the Cytokine Core Laboratory at University of Maryland, Baltimore.
Tumor inoculations, tumor tissue dissections, and metastasis assay
Tumor inoculations and tumor measurements were as described previously (3, 28). Briefly, 6- to 10-week-old female BALB/c IL-1R−/− or IL-1Ra−/− mice were inoculated in the mammary fat pad with 7 ×103 tumor cells in 50 μL of PBS. Mice were euthanized when moribund or at the indicated time points. For tumor tissue dissections, primary tumors were surgically removed when tumors were 8 to 10 mm in diameter. The tumor tissue was minced with scissors and teased apart, incubated at 37°C in DMEM for 24 h, and supernatants were collected for cytokine analysis. For metastasis assays, lungs were harvested at the indicated times and metastatic disease was quantified using the clonogenic assay by plating cells in 6-thioguanine–supplemented media (28).
Blood MDSC
Blood Gr1+CD11b+ MDSC were obtained as previously described (4). Briefly, mice were tail-bled and the percentage of Gr1+CD11b+ cells was analyzed by flow cytometry. If >90% of the WBCs were Gr1+CD11b+, then the mice were euthanized, blood was collected, and RBCs were lysed. The resulting cells were >90% Gr1+CD11b+ and were used in the subsequent assays.
T cell proliferation assays
The CD8+ and CD4+ T cell proliferation assays were done as described (6). Briefly, TS1 or clone 4 splenocytes were cocultured with their respective hemagglutinin peptides and irradiated blood MDSC from BALB/c, IL-1R−/−, or IL-1Ra−/− mice inoculated with 4T1 tumor cells. Cultures were pulsed with 3H-thymidine on day 4, harvested 24 h later, and the samples counted by scintillation counter. Arginase or NO inhibitors were added to some wells. Data are expressed as the average ± SD of triplicate wells.
Flow cytometry
Cells were labeled for direct immunofluorescence as described (28) and analyzed on an Epics XL flow cytometer using Expo32 ADC software (Beckman Coulter).
Bone marrow chimeras
IL-1R−/− mice containing BALB/c bone marrow (BALB/c → IL-1R−/−) and BALB/c mice containing IL-1R−/− bone marrow (IL-1R−/− → BALB/c) were constructed as described (29). Briefly, femurs of donor mice were flushed with PBS using a 30 mL syringe fitted with a 27-gauge needle. Bone marrow cells were washed twice with PBS and resuspended in RPMI at 200 μL per donor mouse. Recipient mice were lethally irradiated at 850 rad and bone marrow (one donor for two recipients) was inoculated into recipient mice through the tail vein using a 1-mL syringe fitted with a 27-gauge needle. Reconstituted mice received daily injections of gentamicin sulfate i.p. (100 μL of 5 mg/mL) for 7 days beginning 1 day before bone marrow reconstitution. Reconstituted mice were maintained on 0.02% tetracycline drinking water starting 1 week before bone marrow transfer and continuing for 6 to 8 weeks after reconstitution. Six to 8 weeks after bone marrow reconstitution, chimeras were bled from the tail vein, and tested by PCR to ascertain hemopoietic genotype and reconstitution. PCR primers IL-1R-s 5′-ATTCTCCATCATCTCTGCTGGTA and IL-1R-as 5′-ATCTCAGTTGTCAAGTGTGTCCC were used to detect the ~350 bp amplicon of the IL-1R gene, present only in wild-type BALB/c mice. PCR primers Neo-s 5′-TGAATGAACTGCAGGACGAGGCA and Neo-as 5′-TCAGCCCATTCGCC GCCAAGCTC were used to detect the 543 bp amplicon of the neomycin insertion gene, present only in the IL-1R−/− mice. PCR annealing temperatures were 56°C and 63°C, respectively, for 30 cycles.
Statistical analyses
Student’s two-tailed t test for unequal variance was done using Microsoft Excel 2003. For Figs. 2 and 6A, differences in tumor diameter in the inoculated mice were tested using a repeated measures profile ANOVA (30, 31) using the procedure in SAS V 9.1 (SAS Institute, Inc.).
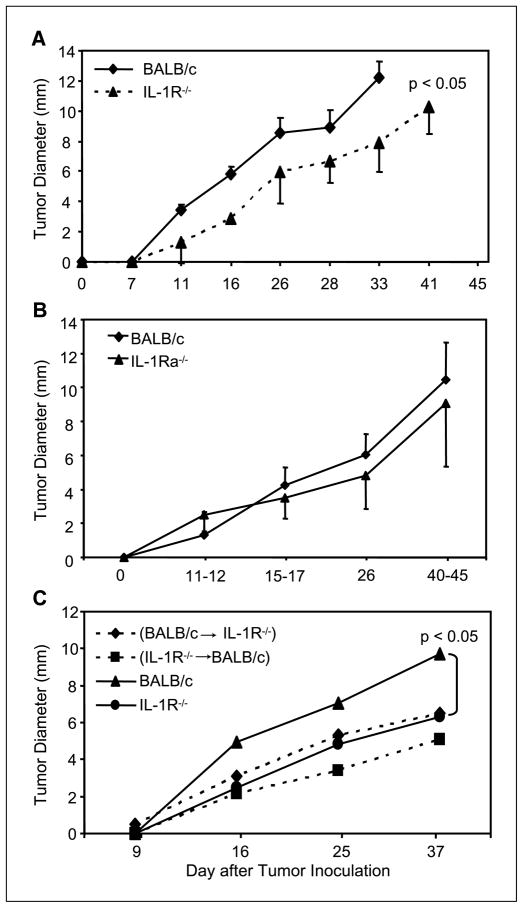
Figure 2.
Tumor progression is delayed in IL-1R−/− mice but not in IL-1Ra−/− mice. A, BALB/c and IL-1R−/− mice were inoculated with 7,000 4T1 tumor cells in the abdominal mammary gland and monitored for primary tumor growth. Tumor progression was delayed in IL-1R−/− mice relative to BALB/c mice (P < 0.05). B, 4T1 tumor growth did not differ in BALB/c and IL-1Ra−/− mice. C, BALB/c, IL-1R−/−, and BALB/c → IL-1R−/− and IL-1R−/− → BALB/c bone marrow chimeras were inoculated with 4T1 tumor cells and monitored for primary tumor growth. Tumor progression in both chimeras was delayed compared with BALB/c mice (P < 0.05). Points, averages of 10 to 15, 10 to 15, and 7 to 15 mice per group (for A, B, and C, respectively); bars, SD. Data are pooled from two to three experiments.
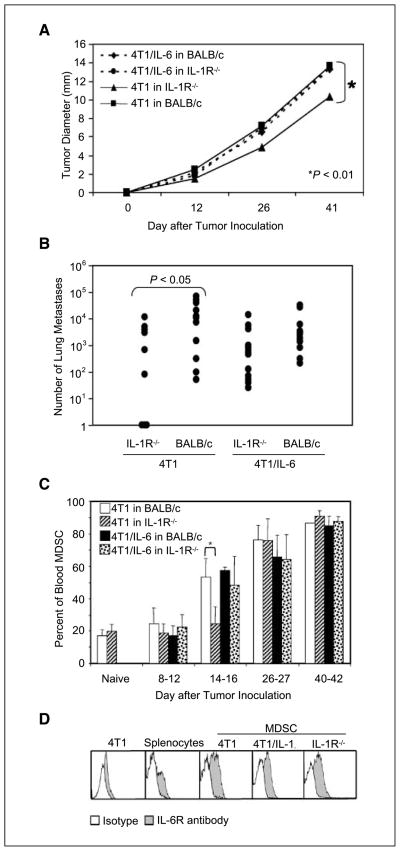
Figure 6.
IL-6 compensates for tumor progression and MDSC accumulation in IL-1R−/− mice. BALB/c and IL-1R−/− mice were inoculated with 7,000 4T1 or 4T1/IL-1β tumor cells in the abdominal mammary gland on day 0 and monitored for primary tumor growth, lung metastases, and blood MDSC. A, tumor diameter was measured at the indicated time points. Points, averages of 15 to 17 mice per group; bars, SD. B, mice were sacrificed and lungs were harvested when BALB/c mice were moribund (days 35–40). Metastatic cells (●) in individual mice were quantified using the clonogenic assay. C, the percentage of blood CD11b+Gr1+ MDSC was measured by flow cytometry at the indicated time points. Columns, averages of 15 to 17 mice per group and are pooled from three independent experiments; bars, SD. D, blood CD11b+Gr1+ MDSC from tumor-bearing BALB/c or IL-1R−/− mice with 4T1 or 4T1/IL-1β were stained with IL-6R antibody or isotype control antibody. 4T1 tumor cells and BALB/c splenocytes were stained as negative and positive controls, respectively. All MDSC express the IL-6R. Data are pooled from two to three experiments.
Results
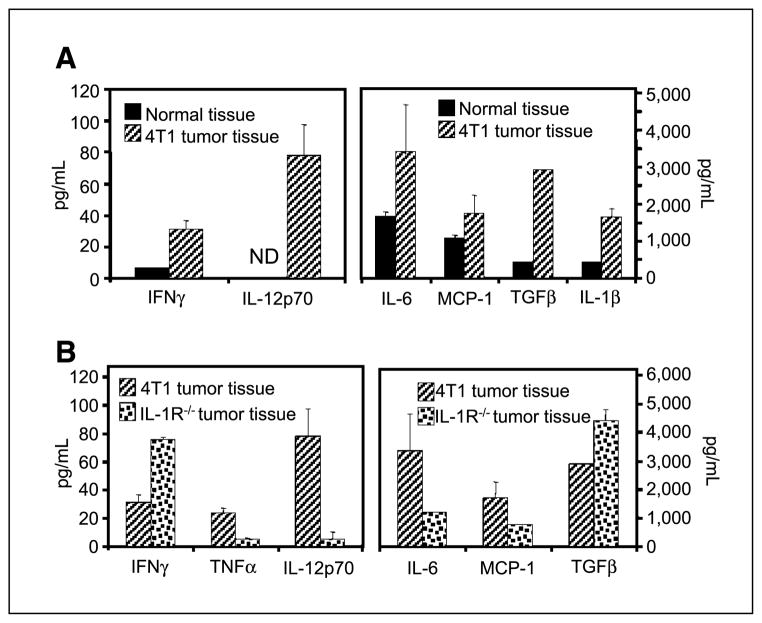
Tumor-associated inflammation is reduced in IL-1R−/− mice
Tumor progression is often accompanied by the presence of inflammation (2). To establish if inflammation accompanies the growth of 4T1 mammary carcinomas, we examined the production of inflammatory cytokines that are hallmarks of inflammatory responses (1, 2). BALB/c mice were inoculated in the abdominal mammary gland with 4T1 tumor cells, primary tumors were removed when tumors reached 8 to 10 mm in diameter, and the presence of inflammatory cytokines in dissociated 4T1 tumor tissue was compared with normal mammary tissue by multiplex analysis (Fig. 1A). Canonical proinflammatory cytokines, such as IL-6, MCP-1, TGFβ, and IL-1β were significantly elevated in 4T1 tumor tissue. The presence of other cytokines associated with inflammation, such as IFNγ and IL-12p70, typically secreted by activated T cells and macrophages, respectively, were also significantly higher in 4T1 tumor tissue. These results show that the growth of 4T1 primary tumor is associated with an inflammatory microenvironment.
Figure 1.
Inflammation-associated cytokines are higher in 4T1 primary tumors of BALB/c mice than in 4T1 tumors of IL-1R–deficient mice. BALB/c and IL-1R−/− mice were inoculated with 7,000 4T1 tumor cells in the abdominal mammary gland on day 0, and primary tumors were surgically removed when their diameters reached 8 to 10 mm. The resulting tumor tissue and control mammary tissue from tumor-free mice was minced, incubated at 37°C for 24 h, and the resulting supernatants were assayed for cytokines by multiplex analysis. A, 4T1 tumor tissue versus normal mammary tissue from BALB/c mice. B, 4T1 tumor tissue from BALB/c mice compared with 4T1 tumor tissue from IL-1R−/− mice. Columns, average of triplicates of individual mice; bars, SD.
Because IL-1β and several cytokines induced by IL-1β were significantly elevated in 4T1 tumor tissue, we questioned whether a deficiency in the IL-1R would limit tumor-associated inflammation. BALB/c and BALB/c IL-1R−/− mice were inoculated with 4T1 cells, and tumors were removed when they were 8 to 10 mm in diameter and analyzed by multiplex analysis for proinflammatory cytokines (Fig. 1B). Cytokines typically induced by IL-1β, such as IL-6, TNFα, and MCP-1 (19), were significantly reduced in the tumor tissue from IL-1R−/− mice compared with tumor tissue from wild-type BALB/c mice. Additionally, IL-1R−/− tumor tissue had less IL-12p70 and more TGFβ and IFNγ than tumor tissue from wild-type BALB/c mice. Therefore, loss of IL-1 activity leads to a reduction in inflammation in the tumor and significantly alters the tumor microenvironment.
Tumor progression is delayed in IL-1R–deficient mice
If inflammation drives tumor progression, then tumors may grow more slowly in IL-1R−/− mice as compared with BALB/c mice. To test this hypothesis, BALB/c and IL-1R−/− BALB/c mice were inoculated with 4T1 cells on day 0 and tumor growth was followed. For both groups, tumors were palpable by day 10, and tumor diameters were measured at the indicated time points (Fig. 2A). The time of tumor onset did not differ between BALB/c and IL-1R−/− mice; however, tumor progression was significantly delayed in IL-1R−/− mice as compared with BALB/c mice (P < 0.05). These data show that the absence of IL-1 signaling and a reduction in inflammation in the tumor environment reduce the growth of 4T1 primary tumors.
4T1 tumor progression does not require the IL-1Ra
IL-1Ra dampens IL-1β signaling by competing with IL-1β for the IL-1R. Its presence therefore reduces the ensuing inflammatory response, and its absence enhances inflammation (18). Because both the receptor agonist (IL-1β) and the receptor antagonist (IL-1Ra) signal through the IL-1R, the decrease in tumor growth rate in IL-1R−/− mice could be due to the absence of either IL-1β or IL-1Ra. To determine which ligand is responsible, BALB/c and IL-1Ra−/− BALB/c mice were inoculated with 4T1 on day 0 and tumor diameters were measured at the indicated time points (Fig. 2B). No difference in tumor onset or rate of tumor progression was observed between BALB/c and IL-1Ra−/− mice. Therefore, loss of the IL-1Ra does not alter tumor growth, indicating that reduced tumor growth in IL-1R−/− mice is due to the absence of IL-1β.
IL-1 nonresponsiveness in either hemopoietic or nonhemopoietic cells is sufficient for delayed tumor progression
IL-1β mediates its effects on a variety of cells. To determine if its ability to promote tumor growth involves hemopoietic and/or non-hemopoietic cells, bone marrow chimeras were created. IL-1R−/− or BALB/c mice were lethally irradiated and reconstituted with BALB/c or IL-1R−/− bone marrow to generate BALB/c → IL-1R−/− and IL-1R−/− → BALB/c chimeras, respectively. The resulting chimeras were inoculated with 4T1 cells and primary tumor growth was measured weekly (Fig. 2C). 4T1 tumor growth was significantly delayed in both BALB/c → IL-1R−/− and IL-1R−/− → BALB/c chimeras relative to wild-type BALB/c mice (P < 0.01 for both); however, tumor progression in the chimeras was not significantly different from tumor growth in IL-1R−/− mice. Therefore, IL-1 nonresponsiveness in either the hemopoietic or nonhemopoietic cells is sufficient for delayed tumor growth.
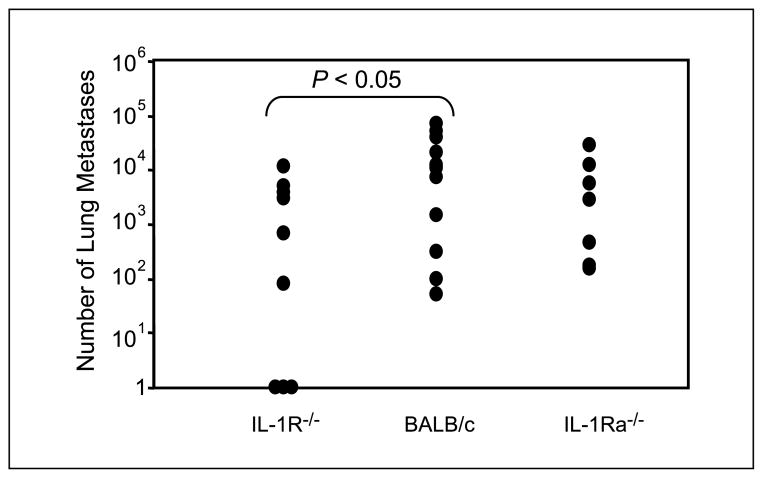
IL-1R−/− mice have reduced numbers of lung metastases
Because loss of the IL-1R slows tumor progression, we examined whether the absence of the IL-1R also reduces the development of lung metastases. BALB/c and IL-1R−/− mice were inoculated on day 0 with 4T1 tumor cells and mice were sacrificed on days 39 to 40 when the BALB/c mice were moribund. Lungs were harvested and the number of lung metastases was quantified using the clonogenic assay (28). Lung metastases were significantly reduced (P < 0.05) in IL-1R−/− mice as compared with BALB/c mice (Fig. 3), indicating that the absence of IL-1 signaling limits metastatic dissemination to the lungs. Therefore, reduced inflammation in the tumor microenvironment is associated with diminished metastatic potential.
Figure 3.
IL-1R−/−, but not IL-1Ra−/−, mice have reduced lung metastases. BALB/c, IL-1R−/−, and IL-1Ra−/− mice were inoculated with 7,000 4T1 tumor cells in the abdominal mammary gland on day 0, and their lungs harvested on days 35 to 40, when BALB/c mice were moribund. Metastatic cells were quantified using the clonogenic assay. Lung metastases are reduced in IL-1R−/− mice relative to BALB/c mice (P < 0.05). ●, number of metastatic cells in the lungs of individual mice. Data are pooled from two to three experiments.
The experiment in Fig. 2B showed that delayed tumor progression in IL-1R−/− mice was due to a deficiency in signaling by IL-1β rather than signaling by IL-1Ra. To determine whether the reduction in lung metastases in the IL-1R−/− mice was also due to the absence of signaling by IL-1β, BALB/c and IL-1Ra−/− mice were inoculated on day 0 with 4T1 tumor cells and the number of lung metastases was determined on days 39 to 40. No differences in the number of lung metastases were observed between BALB/c and IL-1Ra−/− mice (Fig. 3), indicating that the decrease in lung metastasis in IL-1R−/− mice was due to loss of IL-1β and not IL-1Ra signaling.
Because IL-1β mediates tumor progression through both hemopoietic and nonhemopoietic cells (Fig. 2C), we examined which cellular compartment regulates the effects of IL-1β on the development of lung metastases. IL-1R−/− → BALB/c and BALB/c → IL-1R−/− chimeras were inoculated with 4T1 tumor cells on day 0 and the lungs were harvested on days 39 to 40. Lung metastases were significantly reduced in the IL-1R−/− group compared with the BALB/c group; however, neither chimera group had significantly fewer lung metastases compared with BALB/c mice (data not shown). Therefore, both hemopoietic and nonhemopoietic cells respond to IL-1β to promote metastatic disease.
Inhibition of IL-1 signaling delays MDSC accumulation
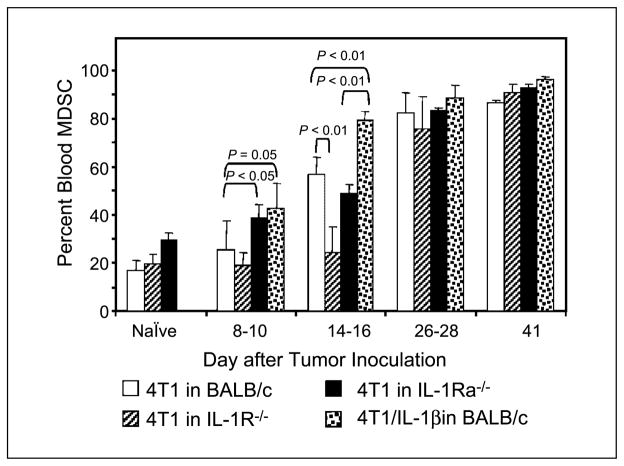
We (3) and others (5) have previously shown that immune suppression driven by MDSC is accentuated by IL-1β–induced inflammation. To determine if the elimination of signaling through IL-1β blocks MDSC accumulation, we examined the levels of MDSC in IL-1R−/−, wild-type BALB/c, and IL-1Ra−/− mice following inoculation with either 4T1 or 4T1/IL-1β tumor cells. Mice were inoculated on day 0 and the percentage of CD11b+Gr1+ MDSC in the blood was measured at various time points by flow cytometry (Fig. 4). MDSC levels in BALB/c mice with 4T1/IL-1β tumors and in IL-1Ra−/− mice with 4T1 tumors increased significantly by days 8 to 10 compared with BALB/c mice with parental 4T1 tumors (P < 0.05). In contrast, MDSC accumulation was significantly delayed in IL-1R−/− mice and did not reach the levels of MDSC in BALB/c mice until days 26 to 28. By days 26 to 40, MDSC levels were >80% of the blood cells in all groups of mice. Therefore, MDSC accumulate more slowly in the early stages of tumor growth in mice that are not responsive to IL-1β.
Figure 4.
IL-1β or the absence of the IL-1Ra enhances MDSC accumulation, whereas the absence of the IL-1R delays MDSC accumulation. BALB/c, IL-1R−/−, and IL-1Ra−/− mice were inoculated with 7,000 4T1 or 4T1/IL-1β tumor cells in the abdominal mammary gland on day 0. Mice were tail-bled at the indicated time points and the percentage of CD11b+Gr1+ MDSC was quantified by flow cytometry. MDSC are elevated in BALB/c mice with 4T1/IL-1β tumors and in IL-1Ra−/− mice with 4T1 tumors by day 8, and remain elevated up to day 16 (P = 0.05 and P < 0.05, respectively for days 8–10; P < 0.01 for both groups on days 14–16). MDSC are reduced in IL-1R−/− mice (P < 0.01). Columns, average of 5 to 15 mice per group and are pooled from two experiments; bars, SD.
To determine whether MDSC accumulation is driven by IL-1 responsiveness of host hemopoietic or nonhemopoietic cells, bone marrow chimeric mice were inoculated with 4T1 tumor cells and blood MDSC were measured by flow cytometry. Percentages of MDSC in the BALB/c → IL-1R−/− chimeras and in nonchimeric IL-1R−/− mice were not significantly different; and both BALB/c → IL-1R−/− and IL-1R−/− → BALB/c chimeras had significantly reduced levels of MDSC compared with BALB/c mice (P < 0.05; data not shown). Therefore, a deficiency for the IL-1R in either the hemopoietic or nonhemopoietic compartment is sufficient to delay MDSC accumulation.
Reduced inflammation limits the quantity of MDSC but does not alter the suppressive quality of MDSC
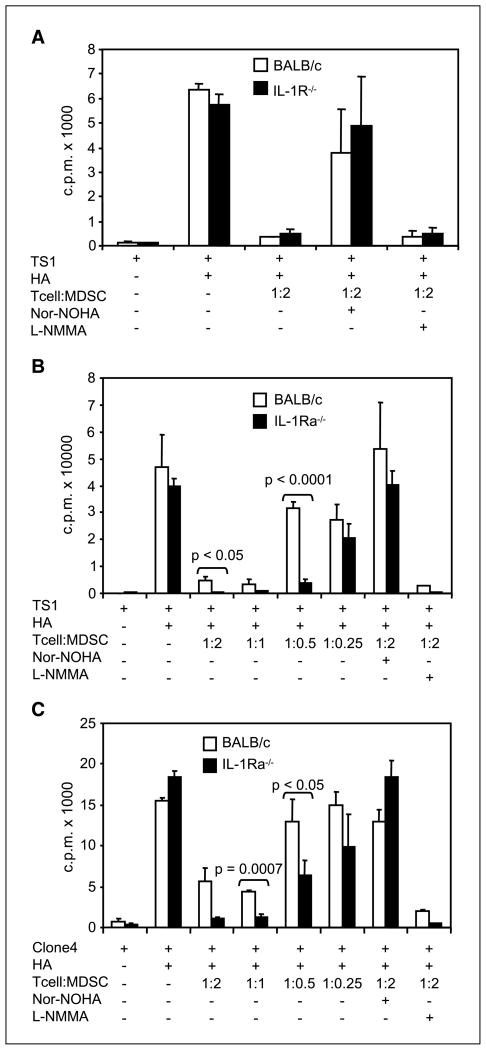
The delay in MDSC accumulation in IL-1R−/− mice shows that a reduction in inflammation alters the quantity of MDSC. We have previously reported that MDSC induced by 4T1/IL-1β tumors are more suppressive than MDSC induced by parental 4T1 tumors (3). If, as these previous experiments suggested, an enhanced proinflamma-tory cytokine milieu affects both the quantity and the quality of MDSC, then MDSC from IL-1R–deficient mice may be less suppressive than MDSC from IL-1β–competent mice. To determine the role of IL-1β in MDSC activity, BALB/c and IL-1R−/− mice were inoculated with 4T1 tumor cells on day 0 and blood MDSC were harvested when MDSC were >90% of cells in the blood (days 35–40). Suppressive activity was tested by coculturing splenocytes from TS1 mice with their respective hemagglutinin peptide in the presence or absence of graded doses of MDSC from BALB/c or IL-1R−/− mice (Fig. 5A). MDSC from BALB/c and IL-1R−/− mice suppressed CD4+ T cell proliferation by >90% as measured by 3H-thymidine uptake. To identify the mechanism of suppression, inhibitors of arginase or NO, nor-NOHA, or L-NMMA, respectively, were added to the TS1 cultures. The addition of nor-NOHA completely reversed the suppression of both BALB/c and IL-1R−/− MDSC, whereas the addition of L-NMMA had no effect. These data show that although the loss of IL-1 and a reduction in the inflammatory environment limits the quantity of MDSC, it does not alter the functional activity of MDSC.
Figure 5.
MDSC from IL-1Ra−/− mice are more suppressive towards CD4+ and CD8+ T cells than MDSC from BALB/c mice. BALB/c, IL-1R−/−, and IL-1Ra−/− mice were inoculated with 7,000 4T1 tumor cells in the abdominal mammary gland, and tail-bled to test for CD11b+Gr1+ MDSC. When MDSC were >90% of the WBCs, mice were sacrificed, blood was collected and RBCs were lysed. The resulting MDSC were used in T cell proliferation assays. CD4+ TS1 or CD8+ clone 4 transgenic splenocytes were stimulated with HA110–119 or HA518–526 peptides, respectively, and cocultured in the presence or absence of graded doses of blood MDSC. Inhibitors of arginase (nor-NOHA) or nitric oxide (L-NMMA) were added to some of the wells. T cell proliferation was measured as counts per minute of [3H]thymidine. A, BALB/c and IL-1R−/− MDSC were equally suppressive. B and C, IL-1Ra−/− MDSC were more suppressive than BALB/c MDSC towards CD4+ T cells (P < 0.05; B) and CD8+ T cells (P < 0.05; C). Data are from one of two to five independent experiments.
IL-1Ra−/− MDSC are more suppressive than BALB/c MDSC
Previous studies showed that MDSC from BALB/c mice with 4T1/IL-1β tumors accumulate earlier and at a faster rate, and are a functionally more suppressive population of MDSC (3). If the loss of the IL-1Ra enhances inflammation and promotes MDSC accumulation, then IL-1Ra−/− MDSC may be functionally more suppressive than BALB/c MDSC. To test this hypothesis, BALB/c and IL-1Ra−/− mice were inoculated with 4T1 tumor cells on day 0, and blood MDSC were harvested when MDSC levels were >90% of the cells in the blood (days 35–40). Suppressive activity was tested by coculturing splenocytes from TS1 mice with their respective hemagglutinin peptide in the presence or absence of graded doses of MDSC. MDSC from IL-1Ra−/− mice were more suppressive towards CD4+ TS1 cells on a per cell basis than MDSC from BALB/c mice (Fig. 5B). MDSC from 4T1-inoculated BALB/c and IL-Ra–deficient mice were also tested for suppressive activity against CD8+ T cells using splenocytes from clone 4 mice and their respective hemagglutinin peptide (Fig. 5C). Similar to the results with CD4+ T cells, MDSC from IL-1Ra−/− mice were more suppressive on a per cell basis than MDSC from BALB/c mice (P < 0.05). To determine if MDSC from IL-1Ra–deficient mice were suppressed by the same arginase-dependent mechanism as MDSC derived from BALB/c mice (3, 6), an inhibitor of arginase (nor-NOHA) or nitric oxide (L-NMMA) was added to the TS1 or clone 4 cultures (Fig. 5B and C). MDSC from BALB/c and IL-1Ra−/− mice suppressed CD4+ and CD8+ T cells through an arginase-dependent mechanism, as the addition of the arginase inhibitor, but not the NO inhibitor, reversed MDSC-mediated suppression. Therefore, elimination of the IL-1Ra induced MDSC that are more potent suppressors but use the same suppressive mechanism as MDSC induced by wild-type mice.
IL-6 compensates for the loss of the IL-1R in primary tumor growth
The reduction in tumor growth observed in IL-1R−/− mice may be due to the loss of the direct effects of IL-1β or may be due to the loss of a downstream product of the IL-1 signaling pathway. A potential downstream candidate is the proinflammatory cytokine, IL-6, the production of which is reduced in IL-1R−/− tumor tissue (Fig. 1B). To examine whether IL-6 is involved in IL-1–mediated tumor progression, 4T1 tumor cells were stably transfected with a construct containing the human IL-6 gene to generate 4T1/IL-6 cells. Because murine cells are responsive to human IL-6 (32), the human IL-6 gene was used to differentiate between IL-6 secreted by the 4T1/IL-6 cells and endogenous murine IL-6 present in the serum and tumor environment. 4T1/IL-6 cells have the same in vivo growth rate as 4T1 cells, so human IL-6 does not serve as an alloantigen (Fig. 6A). If IL-6 is a downstream mediator by which IL-1β alters MDSC activity and tumor progression, then IL-6 production should restore elevated MDSC levels and more rapid tumor progression in IL-1R–deficient mice. To test this hypothesis, IL-1R−/− and BALB/c mice were inoculated with 4T1/IL-6 tumor cells and tumor progression was monitored. No delay in tumor growth was observed in IL-1R−/− mice bearing 4T1/IL-6 tumors compared with the significant delay seen in IL-1R−/− mice with 4T1 tumors (Fig. 6A). Additionally, 4T1/IL-6 tumors in IL-1R−/− mice grew at a similar rate to 4T1 and 4T1/IL-6 tumors in BALB/c mice. Therefore, IL-6 compensates for the loss of IL-1R, supporting the hypothesis that IL-6 is a downstream mediator of IL-1β that facilitates tumor progression.
IL-6 compensates for the loss of IL-1R in the development of lung metastases
Because IL-6 restores primary tumor growth in IL-1R–deficient mice, we examined whether IL-6 also eliminates the reduction in lung metastases. BALB/c and IL-1R−/− mice were inoculated with 4T1/IL-6 tumor cells on day 0 and sacrificed on days 39 to 40. Lung metastases were quantified as previously described and compared with the levels of lung metastases in BALB/c and IL-1R−/− mice inoculated with 4T1 parental cells (Fig. 6B). IL-6 restores the number of lung metastases in IL-1R–deficient mice to that seen in BALB/c mice, demonstrating that IL-6 may be a downstream mediator of IL-1 for metastatic dissemination to the lungs.
IL-6 restores MDSC accumulation in IL-1R−/− mice
The delay in MDSC accumulation in IL-1R−/− tumor-bearing mice and the IL-1β–induced induction of MDSC suggest that inflammation through the production of IL-1β promotes the accumulation of MDSC and contributes to tumor progression. However, MDSC do not express the IL-1R (3) and therefore cannot respond directly to IL-1β. Therefore, it is likely that IL-1β indirectly affects MDSC activity via mediators downstream of IL-1β. Because IL-6 compensates for the loss of IL-1 with respect to primary and metastatic tumor growth, we examined whether IL-6 might be a downstream mediator that affects MDSC. If IL-6 is a downstream mediator, then secretion of IL-6 by 4T1 tumor cells could compensate for the delay in MDSC accumulation in IL-1R–deficient mice. To test this possibility, BALB/c and IL-1R−/− mice were inoculated with 4T1 or 4T1/IL-6 tumor cells at day 0, periodically tail-bled, and the percentage of blood MDSC levels were determined by flow cytometry (Fig. 6C). On days 14 to 16, when the delay in MDSC in IL-1R−/− is most pronounced, there is no observed delay in IL-1R−/− mice inoculated with 4T1/IL-6 tumor cells, suggesting that IL-6 production compensates for the loss of IL-1 signaling.
IL-6 could be acting directly on MDSC or it could trigger other downstream factors that directly act on MDSC. For a direct effect, MDSC would need to express the receptor for IL-6. To determine if MDSC express the IL-6 receptor, MDSC from BALB/c mice with 4T1 or 4T1/IL-1β tumors, and MDSC from IL-1R−/− mice with 4T1 tumors were stained for the IL-6R and analyzed by flow cytometry (Fig. 6D). MDSC uniformly express the IL-6R whether they are derived from BALB/c or IL-1R−/− mice or induced by 4T1 or 4T1/IL-1β tumor cells. Therefore, MDSC have the capability to directly respond to IL-6.
Discussion
Although the concept is widely accepted, the pathways by which inflammation lead to tumor progression remain elusive. We have proposed that one of the contributing mechanisms may be the induction of MDSC, which limit antitumor immunity and thereby promote tumor growth (3, 4). This hypothesis was based on studies in which inflammation was exacerbated by increasing proinflammatory mediators. Although these studies showed a strong correlation, they did not eliminate the possibility that immune suppression simply accompanies inflammation, rather than being caused by inflammation. Using two very different experimental approaches to alter the inflammatory milieu, we now report that reducing inflammation by blocking signaling through the IL-1R, or increasing inflammation through loss of the IL-1Ra, alters the accumulation of MDSC and tumor progression in agreement with the concept that inflammation promotes tumor progression by activating immunosuppressive networks.
Interestingly, the increase in MDSC is dramatic during early tumor growth, and diminishes at later stages, indicating that the effect of inflammation on MDSC accumulation is an early event in tumor progression. Because many of the factors that produce MDSC are also secreted by tumor cells [e.g., IL-6, IL-10, vascular endothelial growth factor (VEGF); refs. 1, 2, 33] the bolus induction of MDSC by inflammation may only be detectable at the early stages because as tumors increase in mass, they are producing proportionately more MDSC induction factors which override the local inflammatory environment. Alternatively, the effects of inflammation may only be detectable early because MDSC levels reach their maximum at later stages and there is no “space” for additional MDSC in the blood or spleen. Indeed, many of the agents known to induce MDSC are associated with and/or are induced by inflammation, suggesting that the inflammatory environment of progressively growing tumors promotes MDSC accumulation through multiple effector molecules. For example, VEGF, an essential molecule for neoangiogenesis, is induced by inflammation (1) and is correlated with the presence of MDSC in the peripheral blood (34, 35). Likewise, IL-6 (33, 36, 37), another proinflammatory mediator, and PGE2 (4, 38), a product of inflammation, induce MDSC accumulation. MDSC may also enhance inflammation as their production of VEGF, IL-10, and reactive oxygen species, which mediate their suppressive function, may contribute to the inflammatory milieu (14, 33, 35). Whether there are MDSC that are induced by inflammation-independent factors, or whether the extent of inflammation governs the quality and quantity of MDSC is unclear. The studies reported here using the IL-1Ra knockout mice and earlier studies using IL-1β–secreting tumor cells (3) show that heightened inflammation induces more MDSC with more suppressive activity. These observations do not necessarily indicate that inflammation induces a novel population of MDSC, because the tumor microenvironment itself is an inflammatory microenvironment and the added inflammation could simply be an amplification effect. However, the quantity and quality of MDSC may be differentially regulated because excessive inflammation, through tumor cell production of IL-1β or loss of the IL-1Ra, increases both the quantity and the suppressive activity of MDSC, whereas a reduction in inflammation, as seen in the IL-1R−/− mice, only affects MDSC quantity. Further complicating this issue is the observation that MDSC are not a homogeneous population of cells, but are a heterogeneous mixture of immature myeloid cells. Indeed, inflammation and noninflammatory mediators may affect subpopulations of MDSC differently.
As shown in previous studies, IL-1β induces the expansion of MDSC indirectly because MDSC do not have the IL-1R (3). This earlier observation led us to examine other potential downstream mediators of IL-1β for their effects on the accumulation of MDSC. IL-6 was a prime candidate because it has previously been implicated in the accumulation of MDSC (33), and because hyperactivation of its transcription factor, signal transducers and activators of transcription 3, promotes abnormal differentiation of dendritic cells (37). Our finding that MDSC express the IL-6R and that tumor-secreted IL-6 at least partially restores MDSC accumulation and enhanced tumor progression in IL-1R–deficient mice, confirms that IL-6 is likely to be a relevant IL-1β downstream mediator. Although tumor-secreted IL-6 increases tumor growth and MDSC levels in IL-1R−/− mice, it does not fully restore enhanced tumor growth or MDSC accumulation to that seen in wild-type mice with 4T1/IL-1β tumors. There are several possibilities for this apparent discrepancy. The quantity of IL-6 produced by the transfectants may not be equivalent to the in vivo amount of IL-6 induced by the IL-1β transductants. Alternatively, IL-6 might be only one of several downstream mediators induced by IL-1β, and maximal induction of MDSC and tumor growth may require additive or synergistic action with other downstream mediators. Previous studies showed that PGE2 also induces the accumulation of MDSC and hastens tumor progression (4). Because PGE2 is also induced by IL-1β (19), it may be another downstream mediator that acts in conjunction with IL-6.
Novel immune-based therapies for the treatment of cancer are currently under development. Many of these approaches involve active immunization and are likely to be most effective in immunocompetent tumor-bearing individuals who are minimally immunosuppressed. Given the causal relationship between inflammation and the induction of MDSC, adjunctive therapies that reduce inflammation prior to immunotherapy, might significantly enhance the efficacy of any active immunotherapy.
Acknowledgments
Grant support: NIH grants R01 CA115880 and R01 CA84232, and Susan G. Komen for the Cure grant BCTR0503885 (S. Ostrand-Rosenberg); and Department of Defense Breast Cancer Research Program Predoctoral Fellowship W81XWH-05-1-0276 (S.K. Bunt).
We thank Dr. Drew Pardoll for providing the hIL-6 construct, Drs. M. Kopf and J. Stuart for providing the IL-1R and IL-1Ra-deficient mice, respectively, and Dr. E. Fuchs for providing the TS1 and clone 4 mice. We appreciate the excellent care of our mouse colony by Sandy Mason.
References
- 1.Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357:539–45. doi: 10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- 2.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bunt SK, Sinha P, Clements VK, Leips J, Ostrand-Rosenberg S. Inflammation induces myeloid-derived suppressor cells that facilitate tumor progression. J Immunol. 2006;176:284–90. doi: 10.4049/jimmunol.176.1.284. [DOI] [PubMed] [Google Scholar]
- 4.Sinha P, Clements VK, Fulton AM, Ostrand-Rosenberg S. Prostaglandin e2 promotes tumor progression by inducing myeloid-derived suppressor cells. Cancer Res. 2007;67:4507–13. doi: 10.1158/0008-5472.CAN-06-4174. [DOI] [PubMed] [Google Scholar]
- 5.Song X, Krelin Y, Dvorkin T, et al. CD11b+/Gr-1+ immature myeloid cells mediate suppression of T cells in mice bearing tumors of IL-1β-secreting cells. J Immunol. 2005;175:8200–8. doi: 10.4049/jimmunol.175.12.8200. [DOI] [PubMed] [Google Scholar]
- 6.Sinha P, Clements VK, Ostrand-Rosenberg S. Reduction of myeloid-derived suppressor cells and induction of M1 macrophages facilitate the rejection of established metastatic disease. J Immunol. 2005;174:636–45. doi: 10.4049/jimmunol.174.2.636. [DOI] [PubMed] [Google Scholar]
- 7.Bronte V, Chappell DB, Apolloni E, et al. Unopposed production of granulocyte-macrophage colony-stimulating factor by tumors inhibits CD8+ T cell responses by dysregulating antigen-presenting cell maturation. J Immunol. 1999;162:5728–37. [PMC free article] [PubMed] [Google Scholar]
- 8.Serafini P, De Santo C, Marigo I, et al. Derangement of immune responses by myeloid suppressor cells. Cancer Immunol Immunother. 2004;53:64–72. doi: 10.1007/s00262-003-0443-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kusmartsev S, Nefedova Y, Yoder D, Gabrilovich DI. Antigen-specific inhibition of CD8+ T cell response by immature myeloid cells in cancer is mediated by reactive oxygen species. J Immunol. 2004;172:989–99. doi: 10.4049/jimmunol.172.2.989. [DOI] [PubMed] [Google Scholar]
- 10.Gabrilovich DI, Velders MP, Sotomayor EM, Kast WM. Mechanism of immune dysfunction in cancer mediated by immature Gr-1+ myeloid cells. J Immunol. 2001;166:5398–406. doi: 10.4049/jimmunol.166.9.5398. [DOI] [PubMed] [Google Scholar]
- 11.Suzuki E, Kapoor V, Jassar AS, Kaiser LR, Albelda SM. Gemcitabine selectively eliminates splenic Gr-1+/CD11b+ myeloid suppressor cells in tumor-bearing animals and enhances antitumor immune activity. Clin Cancer Res. 2005;11:6713–21. doi: 10.1158/1078-0432.CCR-05-0883. [DOI] [PubMed] [Google Scholar]
- 12.Liu C, Yu S, Kappes J, et al. Expansion of spleen myeloid suppressor cells represses NK cell cytotoxicity in tumor-bearing host. Blood. 2007;109:4336–42. doi: 10.1182/blood-2006-09-046201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Almand B, Clark JI, Nikitina E, et al. Increased production of immature myeloid cells in cancer patients: a mechanism of immunosuppression in cancer. J Immunol. 2001;166:678–89. doi: 10.4049/jimmunol.166.1.678. [DOI] [PubMed] [Google Scholar]
- 14.Sinha P, Clements V, Bunt S, Albelda S, Ostrand-Rosenber S. Cross-talk between myeloid-derived suppressor cells and macrophages subverts tumor immunity towards a type 2 response. J Immunol. 2007;179:977–83. doi: 10.4049/jimmunol.179.2.977. [DOI] [PubMed] [Google Scholar]
- 15.Mirza N, Fishman M, Fricke I, et al. All-transretinoic acid improves differentiation of myeloid cells and immune response in cancer patients. Cancer Res. 2006;66:9299–307. doi: 10.1158/0008-5472.CAN-06-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmielau J, Finn OJ. Activated granulocytes and granulocyte-derived hydrogen peroxide are the underlying mechanism of suppression of T-cell function in advanced cancer patients. Cancer Res. 2001;61:4756–60. [PubMed] [Google Scholar]
- 17.Young MR, Petruzzelli GJ, Kolesiak K, et al. Human squamous cell carcinomas of the head and neck chemoattract immune suppressive CD34(+) progenitor cells. Hum Immunol. 2001;62:332–41. doi: 10.1016/s0198-8859(01)00222-1. [DOI] [PubMed] [Google Scholar]
- 18.Yang L, DeBusk LM, Fukuda K, et al. Expansion of myeloid immune suppressor Gr+CD11b+ cells in tumor-bearing host directly promotes tumor angiogenesis. Cancer Cell. 2004;6:409–21. doi: 10.1016/j.ccr.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 19.Dinarello CA. Biologic basis for interleukin-1 in disease. Blood. 1996;87:2095–147. [PubMed] [Google Scholar]
- 20.Arend WP. The balance between IL-1 and IL-1Ra in disease. Cytokine Growth Factor Rev. 2002;13:323–40. doi: 10.1016/s1359-6101(02)00020-5. [DOI] [PubMed] [Google Scholar]
- 21.Fantuzzi G. Lessons from interleukin-deficient mice: the interleukin-1 system. Acta Physiol Scand. 2001;173:5–9. doi: 10.1046/j.1365-201X.2001.00879.x. [DOI] [PubMed] [Google Scholar]
- 22.Glaccum MB, Stocking KL, Charrier K, et al. Phenotypic and functional characterization of mice that lack the type I receptor for IL-1. J Immunol. 1997;159:3364–71. [PubMed] [Google Scholar]
- 23.Kirberg J, Baron A, Jakob S, et al. Thymic selection of CD8+ single positive cells with a class II major histocompatibility complex-restricted receptor. J Exp Med. 1994;180:25–34. doi: 10.1084/jem.180.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morgan DJ, Kreuwel HT, Fleck S, et al. Activation of low avidity CTL specific for a self epitope results in tumor rejection but not autoimmunity. J Immunol. 1998;160:643–51. [PubMed] [Google Scholar]
- 25.Morgan DJ, Liblau R, Scott B, et al. CD8(+) T cell-mediated spontaneous diabetes in neonatal mice. J Immunol. 1996;157:978–83. [PubMed] [Google Scholar]
- 26.Hirsch E, Irikura VM, Paul SM, Hirsh D. Functions of interleukin 1 receptor antagonist in gene knockout and overproducing mice. Proc Natl Acad Sci U S A. 1996;93:11008–13. doi: 10.1073/pnas.93.20.11008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tohyama N, Karasuyama H, Tada T. Growth autonomy and tumorigenicity of interleukin 6-dependent B cells transfected with interleukin 6 cDNA. J Exp Med. 1990;171:389–400. doi: 10.1084/jem.171.2.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pulaski BA, Ostrand-Rosenberg S. Reduction of established spontaneous mammary carcinoma metastases following immunotherapy with major histocompatibility complex class II and B7. 1 cell-based tumor vaccines. Cancer Res. 1998;58:1486–93. [PubMed] [Google Scholar]
- 29.Ostrand-Rosenberg S, Clements VK, Terabe M, et al. Resistance to metastatic disease in STAT6-deficient mice requires hemopoietic and nonhemopoietic cells and is IFN-γ dependent. J Immunol. 2002;169:5796–804. doi: 10.4049/jimmunol.169.10.5796. [DOI] [PubMed] [Google Scholar]
- 30.Simms ELaDSB. Profile analysis of variance as a tool for analyzing correlated responses in experimental ecology. Biometrical journal. 1988;30:229–42. [Google Scholar]
- 31.Zar JH. Biostatistical Analysis. Upper Saddle River: Prentice Hall; 1999. [Google Scholar]
- 32.Van Damme J, Opdenakker G, Simpson RJ, et al. Identification of the human 26-kD protein, interferon β2 (IFN-β2), as a B cell hybridoma/plasmacytoma growth factor induced by interleukin 1 and tumor necrosis factor. J Exp Med. 1987;165:914–9. doi: 10.1084/jem.165.3.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kusmartsev S, Gabrilovich DI. Immature myeloid cells and cancer-associated immune suppression. Cancer Immunol Immunother. 2002;51:293–8. doi: 10.1007/s00262-002-0280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Almand B, Resser JR, Lindman B, et al. Clinical significance of defective dendritic cell differentiation in cancer. Clin Cancer Res. 2000;6:1755–66. [PubMed] [Google Scholar]
- 35.Melani C, Chiodoni C, Forni G, Colombo MP. Myeloid cell expansion elicited by the progression of spontaneous mammary carcinomas in c-erbB-2 transgenic BALB/c mice suppresses immune reactivity. Blood. 2003;102:2138–45. doi: 10.1182/blood-2003-01-0190. [DOI] [PubMed] [Google Scholar]
- 36.Menetrier-Caux C, Montmain G, Dieu MC, et al. Inhibition of the differentiation of dendritic cells from CD34(+) progenitors by tumor cells: role of interleukin-6 and macrophage colony-stimulating factor. Blood. 1998;92:4778–91. [PubMed] [Google Scholar]
- 37.Nefedova Y, Huang M, Kusmartsev S, et al. Hyper-activation of STAT3 is involved in abnormal differentiation of dendritic cells in cancer. J Immunol. 2004;172:464–74. doi: 10.4049/jimmunol.172.1.464. [DOI] [PubMed] [Google Scholar]
- 38.Rodriguez PC, Hernandez CP, Quiceno D, et al. Arginase I in myeloid suppressor cells is induced by COX-2 in lung carcinoma. J Exp Med. 2005;202:931–9. doi: 10.1084/jem.20050715. [DOI] [PMC free article] [PubMed] [Google Scholar]