Abstract
Objective: This study aimed to compare the stability of Tile C pelvic fractures fixed with two iliosacral (IS) screws, tension band plate (TBP), and minimally invasive adjustable plate (MIAP). Methods: Six embalmed specimens of adult pelvis were used. The soft tissue was removed from the specimens, but spines from the fourth lumbar vertebra to the proximal one-third of both femurs were retained. The pubic symphysis, bilateral sacroiliac joints and ligaments, bilateral hip joints, bilateral sacrotuberous ligaments, and bilateral sacrospinous ligaments were intact. Tile C pelvic fractures were created on the specimens. The symphysis pubis was fixed with a plate, and the fracture on the posterior pelvic ring was fixed with three types of internal fixation in a randomized block design. The specimens were placed in a biomechanical machine at a standing neutral posture. A cyclic vertical load of up to 500N was applied, and displacement was recorded. Shifts in the fracture gap were measured by a grating displacement sensor. Results: Under different vertical loads, the shift in the fracture gap and displacement of the pelvic fractures fixed with two IS screws were similar to those in fractures fixed with MIAP. However, the shift in the fracture gap and displacement of fractures fixed with MIAP was significantly smaller than those of fractures fixed with TBP. Conclusion: The stability of the Tile C pelvic fractures fixed with MIAP was similar to that of fractures fixed with IS screws. MIAP performed better than TBP under vertical load.
Keywords: Pelvis, biomechanics, unstable, internal fixation
Introduction
Pelvic fractures are common injuries that account for 3.64% of fractures in adults [1]. Approximately 68.3% of pelvic fractures are unstable fractures, which are complex and serious injuries with a mortality rate of up to 19% [2-4]. Selecting appropriate treatment for unstable pelvic fractures remains a challenging problem for orthopedic physicians. The stability of the pelvis is mainly related to the integrity of the posterior pelvic ring [5]. Therefore, treatment of an unstable pelvic fracture must restore the continuity and stability of the posterior pelvic ring. Internal fixation is the definitive method used in treating pelvic fractures [6]. Iliosacral (IS) screws and tension band plates (TBPs) are commonly used in clinics, and proven to achieve good results in the treatment of pelvic fractures [7-12]. However, the use of IS screws and TBP has some limitations.
IS screw fixation is one of the most frequently used methods with satisfactory results. How-ever, IS screw fixation is a highly technical procedure that requires extensive surgical experience [13]. In addition, doctors and patients are exposed to large amounts of radiation during IS screw fixation because continuous fluoroscopic or computed tomography (CT) guidance is required for appropriate screw insertion [14,15]. Studies reported that the average fluoroscopy time for IS screw fixation ranges from 26s to 5.7 min using a C-arm [16-18]. Improper position, length, and direction of the IS screws can lead to iatrogenic neural, vascular, or visceral injuries; pressurized IS screws may also damage the sacral nerve roots and cauda equina [19-21]. The widespread clinical application of IS screw fixation is limited by the aforementioned disadvantages.
Pre-bending of TBP to adapt to the structure of the posterior pelvic ring can reduce the strength of the plate or damage the threads of screw holes, which can affect the stability of pelvic fractures fixed with TBP [22]. Krappinger et al. treated 23 patients with vertically unstable pelvic injury using TBP fixation, and found that the average residual displacement of fracture remained at 6.1 mm [23]. Moreover, skin infections were found to be common postoperative complications in TBP fixation. Ayoub et al. reported a skin infection rate of 12.5% when TBP fixation was used for the unstable vertical fractures of the sacrum [24]. Suzuki treated 19 patients with vertical fractures of the sacrum, of which two patients had skin infections [25].
To address these limitations, we introduced a novel minimally invasive adjustable plate (MIAP), which was based on the structural characteristics of the posterior pelvic ring (Patent NO. ZL201010130312.6). Chen et al. constructed zone I vertical sacral fracture models, which were fastened to an Electroforce 3520-AT Bose biomechanical testing machine in sitting position and fixed with three types of internal fixation under both vertical and torsional loads; they demonstrated that these fractures fixed with MIAP were as stable as those fixed with two IS screws, and fractures fixed with MIAP and two IS screws were more stable than those fixed with TBP [26]. However, Chen et al. only compared the stability of vertical fractures of the posterior pelvic ring fixed with three types of internal fixation in sitting position. Clinically, to avoid long-term complications associated with bed rest, patients treated with internal fixation were asked to walk earlier because of strong fixation. Therefore, a biomechanical experiment using the type C zone II pelvic fracture model in standing position was designed to compare the stability of posterior pelvic ring disruptions fixed with three types of internal fixation, and provide a basis for the clinical application of MIAP.
Materials and methods
Preparation and preservation of specimens
Six embalmed adult male cadaver pelvises (provided by the Department of Anatomy of Hebei Medical University) were used for biomechanical investigations. The average age of the specimens was 40.8 years (range 27 to 50 years). The inclusion criteria for pelvis specimens were as follows: (1) Specimens from patients with tuberculosis, rheumatism, cancer and other diseases, and anatomic variations were excluded. (2) Specimens that were proven to have osteoporosis using an osteocore 3 dual energy X-ray osteodensitometer (Medilink Company, Parc de la Mediterranee, France) were excluded. (3) The fourth and fifth lumbar vertebrae must be intact, and both femurs must be amputated at the transition of the upper to the middle third. All specimens were prepared by removing the soft tissues. Ligaments (anterior, posterior, interosseal sacroiliac ligament, sacrospinous ligament, and sacrotuberous ligament) were left intact. (4) Hip joints and pubic symphysis must be intact. The specimens were packaged and stored at -20°C. The frozen specimens were melted at room temperature 12 h before the experiment. This study was conducted in accordance with the declaration of Helsinki. This study was approved by the Hospital Ethics Committee of the Third Hospital of Hebei Medical University (Shijiazhuang, Hebei, China). Written informed consent was obtained from all participants.
Structure of MIAP
The MIAP (Tianjin Zhengtian Medical Instrument Company Ltd., Tianjin, P.R.C.) is composed of two Z-shaped brackets and an adjustable connection bar (Figure 1). Each Z-shaped bracket consists of an upper wing, web plate, and lower wing. The connection is made up of a hexagonal tube and two custom-made eye bolts, which can be stretched or shortened by rotating the hexagonal tube. The Z-shaped bracket was positioned with the upper wing on the dorsal surface of the posterior superior iliac spines and the lower wing close to the dorsal surface of the sacrum. Some long cancellous screws were inserted through the holes of the upper and lower wings to secure the Z-shaped bracket on the ilium and sacrum, respectively.
Figure 1.

Structure of MIAP for posterior pelvic ring injury.
Modeling type C pelvic ring injury and fixation of specimens
The anterior and posterior pelvic rings are disrupted in Tile C fractures, leading to translation and rotation instability. Anteriorly, a symphysis pubis rupture was manipulated by cutting through the symphysis pubis, which was stabilized with a five- or four-hole plate placed on the cranial aspect of the symphysis. Posteriorly, a Denis type II fracture was created by an oscillating saw passing through the left sacral foramen (Figure 2). After the reduction of sacral fractures, three types of internal fixation were implanted (Table 1) to reduce the experimental error.
Figure 2.

Image of the specimen after creating an unstable type C zone II vertically oriented injury with incision on the symphysis pubis.
Table 1.
Specimen information and sequence of internal fixation
| Sequence number | Age (years) | Bone mineral density (T score) | sequence of internal fixation |
|---|---|---|---|
| 1 | 27 | 0.7 | ISS--TBP--MIAP |
| 2 | 36 | 0.5 | TBP--MIAP--ISS |
| 3 | 42 | 0.8 | MIAP--ISS--TBP |
| 4 | 45 | 0.3 | ISS--MIAP--TBP |
| 5 | 45 | 0.2 | TBP--ISS--MIAP |
| 6 | 50 | 0.3 | MIAP--TBP--ISS |
ISS: iliosacral screw; TBP: tension band plate; MIAP: minimally invasive adjustable plate.
Three types of internal fixation were used in this study as follows:
① IS screw group: Two 2.0 mm Kirschner wires were inserted through the ipsilateral external surface of the ilium and into the first sacral vertebral body. Fluoroscopy (anteroposterior, inlet, and outlet views) was used to confirm appropriate screw placement. Two 7.3 mm cannulated, partially threaded, and cancellous IS screws (Tianjin Zhengtian Medical Instrument Company Ltd., Tianjin, P.R.C.) were inserted into the first sacral vertebral body with Kirschner wires (Figure 3). CT scan was used to confirm appropriate screw placement.
Figure 3.
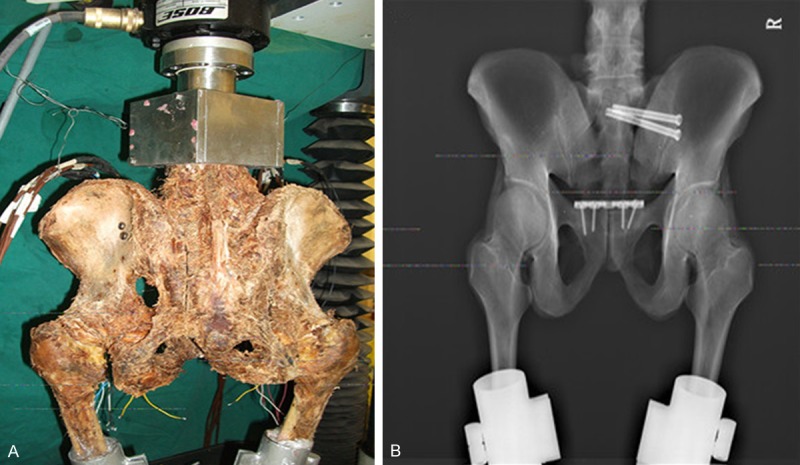
Posterior pelvic ring fixed with two IS screws. A. Posterior view of the specimen. B. Outlet radiograph of the pelvis.
② TBP group: The TBP (Tianjin Zhengtian Medical Instrument Company Ltd., Tianjin, P.R.C.) was bent according to the structural features of the posterior pelvic ring. Suitable screws were inserted into the external surface of the ilium (Figure 4).
Figure 4.
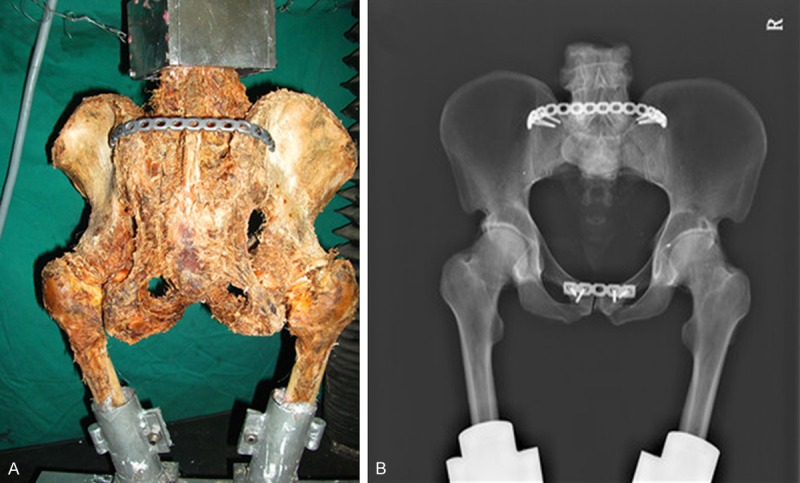
Posterior pelvic ring fixed with TBP. A. Posterior view of the specimen. B. Anteroposterior radiograph of the pelvis.
③ MIAP group: The posterior side of the sacrum and ilium was exposed, and an appropriate MIAP was chosen. Some long cancellous screws were inserted into the ilium and sacrum (Figure 5).
Figure 5.
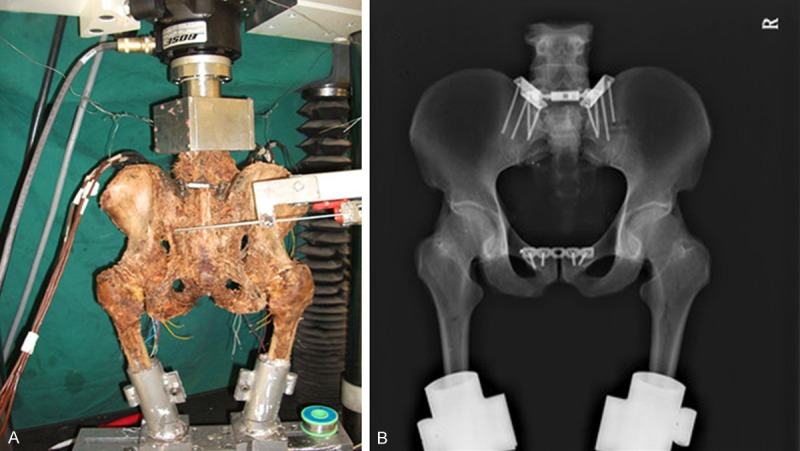
Posterior pelvic ring fixed with MIAP. A. Posterior view of the specimen and grating displacement sensor. B. Anteroposterior radiograph of the pelvis.
Measurements
Bilateral distal femurs of the specimens were fixed in the homemade clamp by Type II denture-based self-curing denture acrylic (Shanghai Medical Instrument Company Ltd, Shanghai, P.R.C.). The pelvic specimens were placed in the Electroforce 3520-AT Bose biomechanical testing machine (BOSE Corporation, Eden Prairie, USA) at a standing neutral position, and both anterior superior iliac spines and ventral surface of the pubic symphysis were covered by the same plane. The L4 vertebral body was also fixed in the homemade clamp. The positioning pins of a grating displacement sensor (Guangzhou Lokshun CNC Equipment Ltd., Guangzhou, P.R.C.) were set to enclose an angle parallel to the posterior inferior iliac spine (PIIS) and perpendicular to the fracture gap, which was fastened to the testing machine. After internal fixation was implanted, a vertical load of 200 N was applied to eliminate creep. The vertical cyclic load was between 0 and 500N, and increased at a rate of 10 N/s. The cyclic load was applied in 20 cycles. In the last three cycles, the displacement of the specimens was recorded at vertical loads of 100, 200, 300, 400, and 500 N by the testing machine. Shifts in the fracture gap were recorded at a vertical load of 500 N by the grating displacement sensor.
The pelvic fracture model was constructed and fixed by the same surgeon. Designing the location and direction of the internal fixation prior to implantation and using X-ray fluoroscopy after the procedure can reduce the influence of pre-fixation on subsequent operations.
Statistical analysis
Data are presented as mean ± SD. All statistical analyses were performed using SPSS version 16.0 software (SPSS Inc., Chicago, IL, USA). Displacement and shifts in the fracture gap were compared by ANOVA. Significant differences between groups were compared using the Student-Newman-Keuls test. Significance was set at P<0.05.
Results
General situation
During the test period, the specimens were fixed at a standing neutral position without any obvious obliquity or fracture. Breakage, loosening, and evulsion of the internal fixation were not observed. All displacements were recorded by the BOSE biomechanical workstation under vertical load, and shifts in the fracture gap were simultaneously recorded by a surgeon. (Figure 6) shows that the load-displacement scattergraph of the specimens was a smooth straight line, which indicates that the deformation observed in the specimens was elastic.
Figure 6.
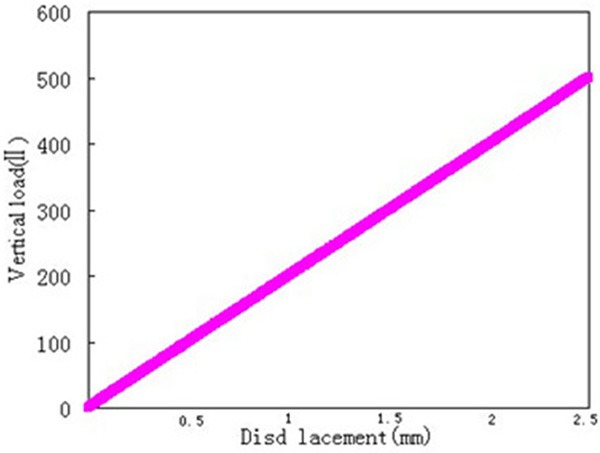
Load-displacement scattergraph of the specimens indicates that the deformation of specimens was elastic.
Displacement of the specimens
Under vertical load, the displacement of the specimens fixed with either MIAP or two IS screws was significantly lower than that of specimens fixed with TBP (P<0.05). The displacement of the pelvis fixed with two IS screws was similar to that of specimens fixed with MIAP (P>0.05) (Table 2).
Table 2.
Displacement of the pelvis fixed with three types of internal fixation under vertical load (x̅±s, n = 6)
| Load (N) | ISS (mm) | TBP (mm) | MIAP (mm) | F value/p value | p value | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| ISS vs TBP | ISS vs MIAP | TBP vs MIAP | |||||
| 100 | 0.664±0.256 | 1.553±0.517 | 0.884±0.424 | 7.525/0.005 | 0.002 | 0.372 | 0.013 |
| 200 | 1.106±0.333 | 2.284±0.738 | 1.411±0.697 | 5.891/0.013 | 0.005 | 0.405 | 0.027 |
| 300 | 1.556±0.429 | 2.805±0.863 | 1.783±0.707 | 5.571/0.016 | 0.007 | 0.577 | 0.022 |
| 400 | 2.022±0.609 | 3.508±1.137 | 2.253±0.730 | 5.243/0.019 | 0.009 | 0.647 | 0.023 |
| 500 | 2.423±0.753 | 4.144±1.129 | 2.795±0.893 | 5.592/0.015 | 0.006 | 0.502 | 0.025 |
ISS: iliosacral screw; TBP: tension band plate; MIAP: minimally invasive adjustable plate.
Displacement at the fracture gap
Under the vertical load of 500 N, the shifts in the fracture gap of specimens fixed with two IS screws and MIAP were 0.756±0.233 and 1.074±0.324 mm, respectively, which were significantly smaller than that of specimens fixed with TBP [1.983±0.45 mm (P<0.05)]. However, no significant difference was observed between the IS screw group and MIAP group (P>0.05) (Table 3).
Table 3.
Shifts in the fracture gap of the pelvis fixed with three types of internal fixation under a load of 500 N (x̅±s, n = 6)
| Load (N) | ISS (mm) | TBP (mm) | MIAP (mm) | F value/p value | p value | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| ISS vs TBP | ISS vs MIAP | TBP vs MIAP | |||||
| 500 | 0.756±0.233 | 1.983±0.454 | 1.074±0.324 | 19.957/<0.001 | <0.001 | 0.135 | <0.001 |
ISS: iliosacral screw; TBP: tension band plate; MIAP: minimally invasive adjustable plate.
Discussion
Open reduction or minimally invasive reduction internal fixation is the main method used for the treatment of unstable pelvic fractures. Chen et al. treated patients with Denis type II sacral fractures using MIAP, and yielded satisfactory clinical outcomes [22,27]. MIAP was applied using a minimally invasive procedure, and the incidence of iatrogenic injury involving nerves and blood vessels was low [22,26,27]. IS screws and TBP are commonly used in clinics [7-12]. The aim of our biomechanical experiment was to compare the stability of posterior pelvic ring disruptions fixed with two IS screws, TBP, and MIAP under physiological conditions.
Injury model and biomechanical experiment design
Tile C pelvic fractures are vertically and rotationally unstable injuries that are associated with high energy trauma. Posterior injuries consist of a dislocation or fracture dislocation of the sacroiliac joint or vertical fracture of the sacrum. Anteriorly, the injury may comprise disruption of the symphysis pubis or unilateral or bilateral fractures of the pubic rami. In this study, we constructed a Tile C pelvic fracture, the most frequent sacral fracture, by cutting the symphysis pubis using a scalpel and cutting the sacrum through the sacral foramen using an oscillating saw [28]. Some scholars believe that conservative treatment is most effective when the separation of the symphysis pubis is less than 2.5 cm [29]. However, some scholars advocate open reduction and fixation [30]. In our study, we stabilized the symphysis pubis using a five- or four-hole plate. Given that the sacroiliac complex has an important load-bearing function, it was stabilized by rigid internal fixation after reduction [31] to achieve better effects. In this study, the performances of frequently used IS screws and TBP were compared with that of MIAP. We used a randomized block design to avoid inaccuracies caused by age, bone density of specimens, and implanting sequence of internal fixation.
We fixed the specimens at a standing neutral position and used a peak load of 500 N, which corresponded to the weight of the upper body of an average adult [19,32]. Twenty cycles were examined to determine the stability of the posterior pelvic ring fixed with three types of internal fixation. Sagi [10] only examined ten cycles, whereas Schildhauer performed 10,000 cycles in biomechanical tests [33].
Under vertical load, the shifts in the fracture gap in Tile C injuries were not limited to vertical (z-axis) shifts but also included rotational (x-axis) and translational (y-axis) shifts [34]. Shifts arising along the three axes were calculated, and the shifts in the fracture gap on the level of the PIIS were measured using the grating displacement sensor, which was used to reflect the stability of pelvic fractures fixed with three types of internal fixation. Although the vertical displacement recorded by the biomechanical testing machine reflected the total displacement of the entire structure, three types of internal fixation were fixed in the same specimen in sequence, so our data were comparable.
Stability of the posterior pelvic ring fixed with three types of internal fixation
The results of this study indicate that using two IS screws, TBP, and MIAP in the treatment of Tile C pelvic ring injuries restored most of the stability of the pelvic ring. Two IS screws placed in the first sacral vertebral body to stabilize the posterior pelvic ring were considered to be the strongest fixation among the three types of fixation [7]. Yinger et al. [35] and Padalkar et al. [36] showed that two IS screws are stiffer than TBP in stabilizing the posterior pelvic ring, which was consistent with the results obtained in our experiment. TBP can effectively stabilize posterior pelvic ring disruptions [11,12], but it also reduces the strength of the plate and may even damage the threads of screw holes because of pre-bending of TBP [12]. Compared with IS screws and MIAP simultaneously fixed in the ilium and sacrum, TBP was used to stabilize the posterior pelvic ring by being fixed in the ilium. Therefore, the stability of the posterior pelvic ring fixed with two IS screws and MIAP was significantly better than that fixed with TBP in our study.
Biomechanical studies suggested that two IS screws provide better fixation than only one screw in stabilizing the posterior pelvic ring [11,35]. IS screw fixation is considered as a “two point” fixation technique that provides strong fixation because IS screw placement into the S1 body penetrates through three layers of cortical bone [37,38]. MIAP was designed according to the structure of the posterior pelvic ring, and functioned as a suspension bridge structure similar to the sacroiliac complex [22]. MIAP was attached to the dorsal part of sacroiliac joints without pre-bending, and fixed the ilium and sacrum through long cancellous screws. MIAP was used to reduce separated or compressed fractures by rotating the connection bar. In this study, we found that the stability of the posterior pelvic ring fixed by two IS screws was better than that fixed by MIAP, but the difference was not statistically significant.
Our study had several limitations. We implanted three types of internal fixation in the same specimen in sequence to reduce the influence caused by bone and skeletal age, but the implantation and removal of pre-fixation was bound to affect the holding power of subsequent fixation and strength of the posterior pelvic ring. Therefore, when we implanted each internal fixation, we accurately located the position and direction of the screws to minimize the interference between screw channels. Only six specimens were used in our study because the acquisition of a large number of specimens was difficult. In future studies, we should increase the sample size and compare the stability of the posterior pelvic ring fixed with three types of internal fixation.
In conclusion, the stability of Tile C pelvic fractures fixed with MIAP was similar to that of fractures fixed with two SI screws, and better than that of fractures fixed with TBP under vertical load. MIAP could be used in the clinical treatment of longitudinal fractures in the posterior pelvic ring.
Acknowledgements
The study was funded by the Nature Science Foundation of China (Grant No. 81271975).
Disclosure of conflict of interest
None.
References
- 1.Zhang Y. Clinical epidemiology of orthopedic trauma. Theme. 2012;10:548. [Google Scholar]
- 2.Tachibana T, Yokol H, Kirits M, Marukawa S, Yoshiya S. Instability of the pelvic ring and injury severity can be predictors of death in patients with pelvic ring fractures: a retrospective study. J Orthop Traumatol. 2009;10:79–82. doi: 10.1007/s10195-009-0050-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou ZD, Hu SB, Tang ZH, Wang SG, Yang GP, Xu EC. 60 cases of pelvic fracture. J Bone Joint Injury. 1999;14:397–8. [Google Scholar]
- 4.White CE, Hsu JR, Holcomb JB. Haemodynamically unstable pelvic fractures. Injury. 2009;40:1023–30. doi: 10.1016/j.injury.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 5.Culemann U, Seelig M, Lange U, Gänsslen A, Tosounidis G, Pohlemann T. [Biomechanical comparson of different stabilization devices for transforaminal sacral fracture. Is an interlocking device advantageous?] . Unfallchirurg. 2007;110:528–36. doi: 10.1007/s00113-007-1236-4. [DOI] [PubMed] [Google Scholar]
- 6.Kellam JF, McMurtry RY, Paley D, Tile M. The unstable pelvic fracture. Operative treatment. Orthop Clin North Am. 1987;18:25–41. [PubMed] [Google Scholar]
- 7.van Zwienen CM, van den Bosch EW, Hoek van Dijke GA, Snijders CJ, van Vugt AB. Cyclic loading of sacroiliac screws in Tile C pelvic fractures. J Trauma. 2005;58:1029–34. doi: 10.1097/01.ta.0000158515.58494.11. [DOI] [PubMed] [Google Scholar]
- 8.Moed BR, Geer BL. S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: a report of 49 cases. J Orthop Trauma. 2006;20:378–83. doi: 10.1097/00005131-200607000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Schweitzer D, Zylberberg A, Córdova M, Gonzalez J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury. 2008;39:869–74. doi: 10.1016/j.injury.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 10.Sagi HC, Ordway NR, DiPasquale T. Biomechanical analysis of fixation for ventically unstable sacroiliac dislocations with iliosacral screws and symphyseal plating. J Orthop Trauma. 2004;18:138–43. doi: 10.1097/00005131-200403000-00002. [DOI] [PubMed] [Google Scholar]
- 11.van Zwienen CM, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB. Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma. 2004;18:589–95. doi: 10.1097/00005131-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Hao T, Changwei Y, Qiulin Z. Treatment of posterior pelvic ring injuries with minimally invasive percutaneous plate osteosynthesis. Int Orthop. 2009;33:1435–9. doi: 10.1007/s00264-009-0756-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hou Z, Zhang Q, Chen W, Zhang P, Jiao Z, Li Z, Smith WR, Pan J, Zhang Y. The application of the axial view projection of the S1 pedicel for sacroiliac screw. J Trauma. 2010;69:122–7. doi: 10.1097/TA.0b013e3181ccba66. [DOI] [PubMed] [Google Scholar]
- 14.Grützner PA, Rose E, Vock B, Holz F, Nolte LP, Wentzensen A. Computer-assisted screw osteosynthesis of the posterior pelvic ring. Initial experiences with an image reconstruction based optoelectronic navigation system. Unfallchirurg. 2002;105:254–60. doi: 10.1007/s001130100339. [DOI] [PubMed] [Google Scholar]
- 15.Sagi HC, Lindvall EM. Inadvertent intraforaminal iliosacral screw placement despite apparent appropriate positioning on intraoperative fluoroscopy. J Orthop Trauma. 2005;19:130–3. doi: 10.1097/00005131-200502000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Collinge C, Coons D, Tornetta P, Aschenbrenner J. Standard multiplanar fluoroscopy versus a fluoroscopically based navigation system for the percutaneous insertion of iliosacral screws: a cadaver model. J Orthop Trauma. 2005;19:254–8. doi: 10.1097/01.bot.0000151821.79827.fb. [DOI] [PubMed] [Google Scholar]
- 17.Peng KT, Huang KC, Chen MC, Li YY, Hsu RW. Percutaneous placement of iliosacral screws for unstable pelvic ring injuries: comparison between one and two C-arm fluoroscopic techniques. J Trauma. 2006;60:602–8. doi: 10.1097/01.ta.0000200860.01931.9a. [DOI] [PubMed] [Google Scholar]
- 18.Zwingmann J, Konrad G, Kotter E, Südkamp NP, Oberst M. Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res. 2009;467:1833–8. doi: 10.1007/s11999-008-0632-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berber O, Amis AA, Day AC. Biomechanical testing of a concept of posterior pelvic reconstruction in rotationally and vertically unstable fractures. J Bone Joint Surg Br. 2011;93:237–244. doi: 10.1302/0301-620X.93B2.24567. [DOI] [PubMed] [Google Scholar]
- 20.Marmor M, Lynch T, Matityahu A. Superior gluteal artery injury during iliosacral screw placement due to aberrant anatomy. Orthopedics. 2010;33:117–20. doi: 10.3928/01477447-20100104-26. [DOI] [PubMed] [Google Scholar]
- 21.Reilly MC, Bono CM, Litkouhi B, Sirkin M, Behrens FF. The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma. 2006;2:S37–43. [PubMed] [Google Scholar]
- 22.Chen W, Hou Z, Su Y, Smith WR, Liporace FA, Zhang Y. Treatment of posterior pelvic ring disruptions using a minimally invasive adjustable plate. Injury. 2013;44:975–80. doi: 10.1016/j.injury.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 23.Krappinger D, Larndorfer R, Struve P, Rosenberger R, Arora R, Blauth M. Minimally invasive transiliac plate osteosynthesis for type C injuries of the pelvic ring: a clinical and radiological follow-up. J Orthop Trauma. 2007;21:595–602. doi: 10.1097/BOT.0b013e318158abcf. [DOI] [PubMed] [Google Scholar]
- 24.Ayoub MA. Vertically unstable sacral fractures with neurological insult: outcomes of surgical decompression and reconstruction plate internal fixation. Int Orthop. 2009;33:261–7. doi: 10.1007/s00264-007-0468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suzuki T, Hak DJ, Ziran BH, Adams SA, Stahel PF, Morgan SJ, Smith WR. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury. 2009;40:405–9. doi: 10.1016/j.injury.2008.06.039. [DOI] [PubMed] [Google Scholar]
- 26.Chen W, Wang MY, Zhang Q, Li ZY, Wang B, Wang J. Biomechanical comparison of the stability of posterior pelvic ring disruptions fixed with three kinds of internal fixator. Chin J Orthop. 2011;31:1232–8. [Google Scholar]
- 27.Chen W, Zhang Q, Lu Y, Ma LJ, Wu XB, Wang MY. Denis type II sacral fractures treated with minimally invasive adjustable plate. Chin J Orthop Trauma. 2012;14:385–90. [Google Scholar]
- 28.Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma. 2003;17:399–405. doi: 10.1097/00005131-200307000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Matta JM, Tornetta P 3rd. Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996;329:129–140. doi: 10.1097/00003086-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 30.Chen W, Zhang Q, Zheng ZL, Zhang YY, Qin D, Han CL. Biomechanical study of the influence of different degrees of pubic symphysis diastasis on stress distribution of the posterior pelvic ring. Chin J Trauma. 2010;90:531–4. [Google Scholar]
- 31.Kobbe P, Hockertz I, Sellei RM, Reilmann H, Hockertz T. Minimally invasive stabilisation of posterior pelvic-ring instabilities with a transiliac locked compression plate. Int Orthop. 2012;36:159–64. doi: 10.1007/s00264-011-1279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li SZ, Su W, Zhao JM, Xie NF. Biomechanical comparison of pedicle screw-rod system and pelvic external fixator in models of rotatory unstable pelvic injury. Chin J Orthop Trauma. 2013;15:517–20. [Google Scholar]
- 33.Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt ML Jr. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic load. J Orthop Trauma. 2003;17:22–31. doi: 10.1097/00005131-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Bodzay T, Szita J, Manó S, Kiss L, Jónás Z, Frenyó S, Csernátony Z. Biomechanical comparison of two stabilization techniques for unstable sacral fractures. J Orthop Sci. 2012;17:574–9. doi: 10.1007/s00776-012-0246-4. [DOI] [PubMed] [Google Scholar]
- 35.Yinger K, Scalise J, Olson SA, Bay BK, Finkemeier CG. Biomechanical comparison of posterior pelvic ring fixation. J Orthop Trauma. 2003;17:481–7. doi: 10.1097/00005131-200308000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Padalkar P, Pereira BP, Kathare A, Sun KK, Kagda F, Joseph T. Trans-iliosacral plating for vertically unstable fractures of sacral spine associated with spinopelvic dissociation: A cadaveric study. Indian J Orthop. 2012;46:274–8. doi: 10.4103/0019-5413.96376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hinsche AF, Giannoudis PV, Smith RM. Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res. 2002;395:135–44. doi: 10.1097/00003086-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 38.Collinge C, Coons D, Aschenbrenner J. Risks to the superior gluteal neurovascular bundle during percutaneous iliosacral screw insertion: an anatomical cadaver study. J Orthop Trauma. 2005;19:96–101. doi: 10.1097/00005131-200502000-00005. [DOI] [PubMed] [Google Scholar]


