Abstract
Background:
Pregnancy with anxious or depressive symptoms might be associated with worse birth outcomes. The aim of this study was to determine the demographic predictors of anxiety and depression symptoms in pregnant women.
Materials and Methods:
We assessed pregnancy anxiety and depression levels among 142 women in three trimesters. All subjects completed two questionnaires: Demographic scale and the 21-item Depression Anxiety Stress Scale (DASS-21) questionnaire. Chi-square test and regression analysis were used to assess the association between anxiety and depression symptoms with maternal age, maternal education, family income, gestational age, body mass index, parity, and pregnancy risk.
Results:
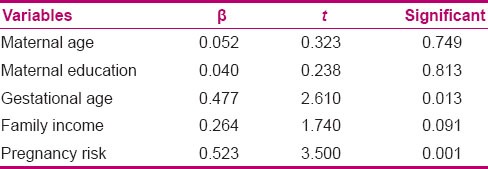
25.3% of the pregnant women reported having depressive symptoms. Also, 49.3% of the subjects reported having anxiety symptoms. There was positive correlation between body mass index, gestational age, and pregnancy risk with depression symptom. Also, there was negative correlation between family income and maternal education level with anxiety symptom. In linear regression model, the variables of maternal age, maternal education, parity, abortion, gestational age, family income, body mass index, and pregnancy risk predicted 44.7% anxiety (F = 1.903, P = 0.006) and 68.1% depression (F = 2.101, P = 0.003). The strongest predictors of depression in pregnant women were pregnancy risk (β = 0.361, P = 0.001) and maternal education (β = −0.297, P = 0.006). Also, pregnancy risk (β = 0.523, P = 0.001) and gestational age (β = 0.477, P = 0.01) were the important predictors of maternal anxiety in the pregnancy period.
Conclusions:
Pregnancy risk, gestational age, and education level are the strongest predictors of mental health in the pregnancy period. This result suggests that psychological support is needed for pregnant women with high risk and low education, especially in the third trimester, to improve their mental health.
Keywords: Anxiety, depression, pregnancy
INTRODUCTION
Depression and anxiety are the most prevalent psychiatric disorders during pregnancy, and several studies have reported their prevalence ranging from 4 to 25%.[1,2] Both anxiety and depression have been linked to increased risk of preeclampsia and other high-risk conditions.[3] Also, antenatal depression is a strong predictor of postnatal depression.[4] Increased hospital admissions have also been linked to maternal depression.[5]
Past studies have shown that pregnancy-related stress or anxiety,[6] life events,[7] and anxious[8] or depressive[9] symptoms might be associated with worse birth outcomes such as preterm birth, smaller birth weight, and smaller head circumference.[10] Glover reported that prenatal anxiety or depression may contribute 10–15% of the attributable load for emotional and behavioral outcomes, including emotional problems, symptoms of attention deficit hyperactivity disorder, and impaired cognitive development.[11] Pearson et al. investigated the association between symptoms of antenatal and postnatal parental depression with offspring depression at age 18. They reported that offspring were 1.28 times more likely to have depression at age 18 in maternal depression score antenatally, independent of maternal depression at a later stage.[12]
Several factors predispose to depression during pregnancy. Benute et al. reported that unplanned pregnancy in women with a medical disorder was a risk factor for major depression during pregnancy.[13] Pereira et al. noted that previous history of depression and any psychiatric treatment, serious physical illness, and casual jobs were the risk factors of depression during pregnancy.[14] A systemic review by Lancaster et al. showed that maternal anxiety, life stress, history of depression, lack of social support, unintended pregnancy, Medicaid insurance, domestic violence, lower income, lower education, smoking, single status, and poor relationship quality were associated with a greater likelihood of antepartum depressive symptoms.[15] Other risk factors include age, marital status, gravidity, unplanned pregnancy, previous history of stillbirth, abortions, past instrumental or operative delivery, and level of social support.[16]
Studies in the developing world have found that the risk factors of depression during pregnancy are often culturally determined. As there is little information on the predictors of depression or anxiety in the Iranian population, the aim of this study was to investigate some predictor factors of mental health (depression/anxiety) in pregnant women.
MATERIALS AND METHODS
This cross-sectional study was conducted between November 2012 and December 2013 in pregnant women of two teaching hospitals of Babol University of Medical Sciences. One hundred and forty-two pregnant women participated in the study (47 in the first trimester, 47 in the second trimester, and 48 in the third trimester). Available sampling was utilized to recruit the pregnant women based on their gestational age. Inclusion criteria for the women were: Having education of at least 5 years and willingness to participate in the study. Ethical approval was granted by the Medical Education Ethics Committee at Babol University of Medical Sciences.
A midwife interviewed the subjects. She took the history, measured the height, and completed the checklist of Pregnancy Risk. She collected demographic data including age, education, and family income. Also, she took the weight of the women before pregnancy to calculate the body mass index (BMI) at the beginning of the pregnancy. The women were classified according to their BMI values as normal weight (18.0–24.9 kg/m2), overweight/obese (>25.0 kg/m2), and underweight (<18.0 kg/m2).[17] Then the midwife distributed the mental health questionnaires [21-item Depression Anxiety Stress Scale (DASS-21)] to the respondents during prenatal visit. She gave a brief explanation regarding the purpose of the plan, reminded the subjects of their rights to not answer any question if they wished so, and how to fill in the questionnaires. The pregnant women were also told that their response would be treated with utmost confidentiality. The questionnaires took only 10 min to be completed.
Scales and measurement
DASS-21: The DASS-21 is a 21-item self-reported questionnaire designed to measure a range of three subscales (depression, anxiety, and stress). The scale contains three subscales that cover depression (7 items), anxiety (7 items), and stress (7 items). Each item is scored from 0 (at all) to 3 (very much). Therefore, the total score of each subscale ranged 0–21. Because the DASS-21 is short form version of DASS (the long form has 42 items), the final score of each subscale needs to be multiplied by two (x2). The following cutoff score is used to assess the presence of the symptoms: Depression ≥10, anxiety ≥8, and stress ≥15.[18] A valid Persian version of DASS-21 was used in the study.[19]
Pregnancy Risk: The checklist was based on Prenatal Risk Assessment System of the Ministry of Health and Medical Education of Iran.[20] The items cover six categories: Unusual features of pregnancy, gynecological/obstetrical history, past pregnancy complications, medical history, family history, and current pregnancy complaints. Items are scored as present (1) or absent (0). The presence of any item is considered as high-risk pregnancy. Also, high mark of risk shows the severity of complicated pregnancy.
We determined the univariate association between all demographic variables (maternal age, maternal education, gestational age, family income, pregnancy risk, and BMI) with depression or anxiety symptoms using Chi-square. Then, each of the variables whose association reached statistical significance in the univariate analysis (P < 0.05) was included in a multiple linear regression model. After investigating the assumptions to analysis of regression (linearity of the relationship between dependent and independent variables, independence of the errors, homoscedasticity of the errors, and normality of the error distribution), we carried out two series regression analyses. In the first model, five variables (maternal education, gestational age, family income, pregnancy risk, and BMI) were used as independent variables and depression symptoms formed the independent variable. In the second model, five variables (maternal education, maternal age, gestational age, family income, and pregnancy risk) were used as independent variable and anxiety symptoms formed the independent variable. We applied the Statistical Package for Social Sciences SPSS Version 18.0 (Inc., Chicago, IL, USA) for data analysis. A value of P < 0.05 was considered significant.
RESULTS
The mean age of the participants was 24.38 ± 5.07 years (range 15–41 years). 71.1% of the pregnant women were in the age group of 21–30 years. 33.1% of subjects were in the first trimester, 33.1% in the second trimester, and 33.8% were in the third trimester. 31.7% of the population was classified as high-risk pregnancy.
Pearson correlation test showed that there was positive correlation between BMI, gestational age, and pregnancy risk with the depression symptom. Also, there was negative correlation between family income and maternal education level with the anxiety symptom.
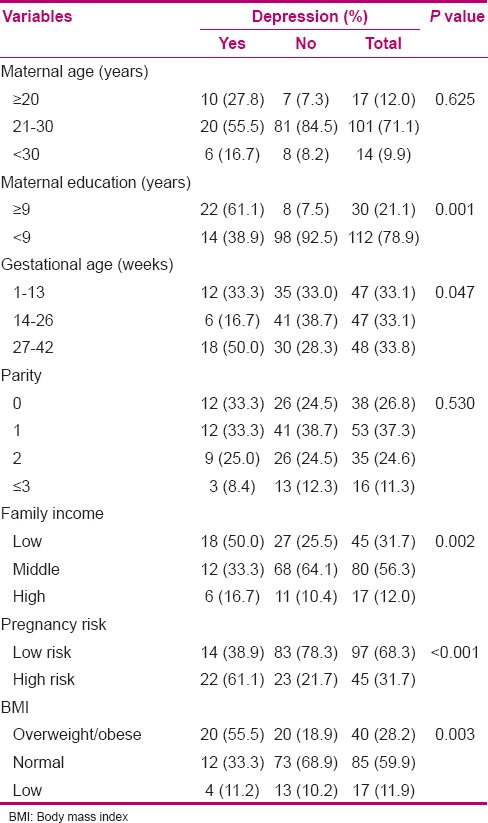
Thirty-six pregnant women (25.3%) reported having depressive symptoms. Characteristics of the pregnant women according to their status of depressive symptoms are given in Table 1. There was statistically no difference between depressive and non-depressive groups in maternal age and parity (P > 0.05). There were significant differences between depressive and non-depressive groups in maternal education, gestational age, BMI, family income, and pregnancy risk (P < 0.05). The frequency of low maternal education, obese/overweight/low family income, and high-risk pregnancy was significantly more in depressive group than in non-depressive group. Also, the frequency of depressive symptom was significantly more in third trimester than in second or first trimester.
Table 1.
Demographic factors of the population with/without depressive symptoms
Seventy pregnant women (49.3%) reported having anxious symptoms. Characteristics of the pregnant women according to their status of anxiety symptoms are shown in Table 2. There was statistically no difference between anxious and non-anxious groups in BMI and parity (P > 0.05). There were significant differences between anxious and non-anxious groups in maternal education, maternal age, gestational age, family income, and pregnancy risk (P < 0.05). The frequency of low maternal education, maternal age less than 20 years, low family income, and high-risk pregnancy was significantly more in anxious group than in non-anxious group. Also, the frequency of anxious symptom was significantly more in third trimester than in second or first trimester.
Table 2.
Demographic factors of the population with/without anxiety symptoms
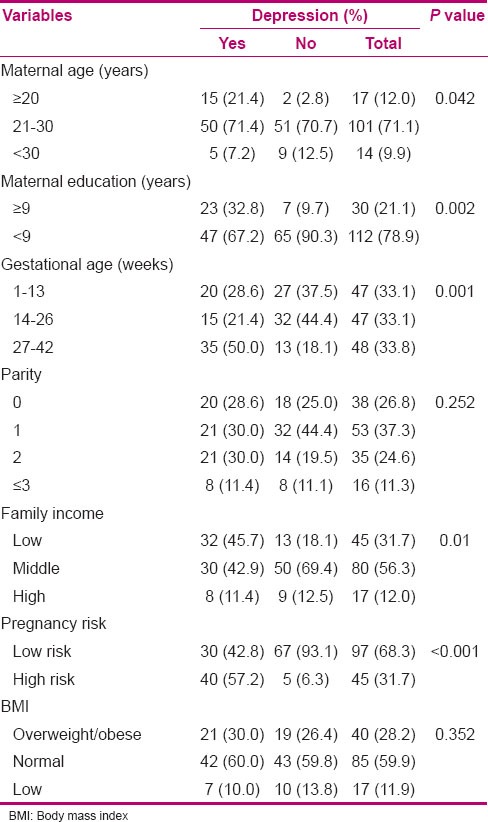
Bivariate analysis results [Tables 1 and 2] revealed significant differences between pregnant women with depressive/anxious symptoms and without depressive/anxious symptoms in the following factors: Maternal age, maternal education, gestational age, family income, pregnancy risk, and BMI. Then, inter-linear regression analysis was performed with the above 10 factors.
The results of multiple linear regression analysis are presented in Tables 3 and 4. According to this analysis, maternal education (β = −0.297, P = 0.006) and pregnancy risk (β =0.361, P = 0.01) were significantly important risk factors for depression symptoms in the pregnancy period. Also, gestational age (β =0.477, P = 0.01) and pregnancy risk (β =0.523, P = 0.001) were significantly important predictors for anxiety symptoms in the pregnant women.
Table 3.
Predictors of depression symptom of pregnant women in multiple linear regression analysis
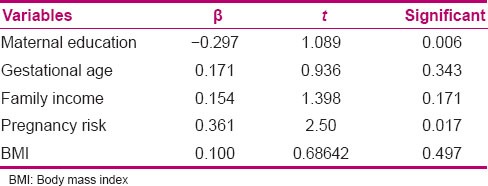
Table 4.
Predictors of anxiety symptom of pregnant women in multiple linear regression analysis
DISCUSSION
We found that the prevalence of depressive symptom during pregnancy was 55.3%. Also, 49.3% of the pregnant women reported having anxiety symptoms. Other studies using a variety of depression assessment tools have reported antenatal depression prevalence of 9–28% for middle-class samples and 25–50% for low-income populations.[21] Rubertsson et al. reported the prevalence of anxiety symptoms as 15.6% in early pregnancy.[22]
The results revealed that the strongest predictor of depressive symptom during pregnancy was high-risk pregnancy. Some study, in line with the present study, has indicated that women with depressive symptom reported having more obstetric risk than those without depression.[3,13] Ajinkya reported that history of obstetric complications, in both present and past pregnancy, is the main predictor of depression in pregnant women.[23]
How can we explain why depressive pregnant people reported more obstetric complications than non-depressive women? It is unclear how depression is related to pregnancy risk. However, the negative consequences of maternal depression might result in higher impulsivity, maladaptive social interactions, and cognitive, behavioral, and emotional difficulties.[24] Also, there is co-morbid between physical and psychological health problems. Perlen et al. reported that pregnant women with five or more physical health problems had a threefold increase in the likelihood of reporting depressive symptoms.[25] Depression appears to be related to poorer adherence to treatment during pregnancy. Depressed women report having feeling of hopelessness. They are more often socially isolated and social support has been related to self-care. Also, depressed pregnant women may not have the energy to follow health care.
The results showed that the second strong predictor of depressive symptom during pregnancy was maternal education. Hein et al. reported that parity status, education status, monthly income, residential property status, and partnership status, as well as interactions were found to be predictive factors for depression during and after pregnancy.[26] Contrast to our results, Miyake et al. reported that there was no relationship between household income or education and the prevalence of depressive symptoms during pregnancy.[27]
The results revealed that the two strong predictors of anxiety symptom during pregnancy were high-risk pregnancy and gestational age. Ding et al., in a meta-analysis, investigated the association between maternal anxiety and preterm birth and/or low birth weight. They suggested that maternal anxiety during pregnancy was positively related to an increased risk of preterm birth and low birth weight.[28] Bödecs et al. reported that the mean scores for depression and anxiety were significantly higher among women who were unemployed, less than 20 years of age, and had low educational or/and socio-economic status.[29] Consistent with our results, a study showed that 54% pregnant women reported anxiety during the first, second, or third trimester. Also, prevalence of anxiety was more and severe in the first and third trimester.[30]
A few study limitations should be mentioned. First, the cross-sectional nature of the study prevents any conclusion being made regarding causality. Prospective cohort studies are a more reliable way of finding the relation between various factors and mental health in pregnant women. Second, it was performed in two teaching hospitals; therefore, the sample may not be representative of all pregnant women. Third, data collection was performed by self-report using questionnaires, which could result in underreporting of the conditions. Future research might include a more detailed and complete view on depression/anxiety, which, in particular, might be obtained by using alternative methods such as psychiatric clinical interviews. The strength of our study lies in the fact it focused on the issue of anxiety/depression during pregnancy in the Iranian population, which has not been yet well studied so far, and determined several obstetric variables that were significantly associated with depression/anxiety during pregnancy.
In conclusion, our results showed that pregnancy risk, gestational age, and education level are the strongest predictors of mental health in pregnancy period. We recommend that screening for depression and anxiety should be a part of the routine during antenatal care. Also, these results suggest that healthcare providers should give close attention to anxiety and depression in pregnant women and provide appropriate mental health care in order to improve the outcomes for both mothers and infants.
ACKNOWLEDGMENTS
We thank all the pregnant women who participated in the study. Also, we thank Ms. Abdolahzadeh who gathered patients’ information. The research project number is 1363.
Footnotes
Source of Support: Babol University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Teixeira C, Figueiredo B, Conde A, Pacheco A, Costa R. Anxiety and depression during pregnancy in women and men. J Affect Disord. 2009;119:142–8. doi: 10.1016/j.jad.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Pereira PK, Lovisi GM, Pilowsky DL, Lima LA, Legay LF. Depression during pregnancy: Prevalence and risk factors among women attending a public health clinic in Rio de Janeiro, Brazil. Cad Saude Publica. 2009;25:2725–36. doi: 10.1590/s0102-311x2009001200019. [DOI] [PubMed] [Google Scholar]
- 3.Kharaghani R, Geranmaye M, Janani L, Hantooshzade S, Arbabi M, Rahmani Bilandi R, et al. Preeclampsia and depression: A case-control study in Tehran. Arch Gynecol Obstet. 2012;286:249–53. doi: 10.1007/s00404-012-2260-3. [DOI] [PubMed] [Google Scholar]
- 4.Faisal-Cury A, Menezes PR. Antenatal depression strongly predicts postnatal depression in primary health care. Rev Bras Psiquiatr. 2012;34:446–50. doi: 10.1016/j.rbp.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Andersson L, Sundström-Poromaa I, Wulff M, Aström M, Bixo M. Implications of antenatal depression and anxiety for obstetric outcome. Obstet Gynecol. 2004;104:467–76. doi: 10.1097/01.AOG.0000135277.04565.e9. [DOI] [PubMed] [Google Scholar]
- 6.Kramer MS, Lydon J, Seguin L, Goulet L, Kahn SR, McNamara H, et al. Stress path ways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. Am J Epidemiol. 2009;169:1319–26. doi: 10.1093/aje/kwp061. [DOI] [PubMed] [Google Scholar]
- 7.Khashan AS, McNamee R, Abel KM, Mortensen PB, Kenny LC, Pedersen MG, et al. Rates of preterm birth following antenatal maternal exposure to severe life events: A population-based cohort study. Hum Reprod. 2009;24:429–37. doi: 10.1093/humrep/den418. [DOI] [PubMed] [Google Scholar]
- 8.Mancuso RA, Schetter CD, Rini CM, Roesch SC, Hobel CJ. Maternal prenatal anxiety and corticotropin-releasing hormone associated with timing of delivery. Psychosom Med. 2004;66:762–9. doi: 10.1097/01.psy.0000138284.70670.d5. [DOI] [PubMed] [Google Scholar]
- 9.Dayan J, Creveuil C, Marks MN, Conroy S, Herlicoviez M, Dreyfus M, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: A prospective cohort study among women with early and regular care. Psychosom Med. 2006;68:938–46. doi: 10.1097/01.psy.0000244025.20549.bd. [DOI] [PubMed] [Google Scholar]
- 10.Hobel CJ, Goldstein A, Barrett ES. Psychosocial stress and pregnancy outcome. Clin Obstet Gynecol. 2008;51:333–48. doi: 10.1097/GRF.0b013e31816f2709. [DOI] [PubMed] [Google Scholar]
- 11.Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28:25–35. doi: 10.1016/j.bpobgyn.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 12.Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, et al. Maternal depression during pregnancy and the postnatal period: Risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. 2013;70:1312–9. doi: 10.1001/jamapsychiatry.2013.2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benute GR, Nomura RM, Reis JS, Fraguas R, Junior, Lucia MC, et al. Depression during pregnancy in women with a medical disorder: Risk factors and perinatal outcomes. Clinics (Sao Paulo) 2010;65:1127–31. doi: 10.1590/S1807-59322010001100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pereira PK, Lovisi GM, Pilowsky DL, Lima LA, Legay LF. Depression during pregnancy: Prevalence and risk factors among women attending a public health clinic in Rio de Janeiro, Brazil. Cad Saude Publica. 2009;25:2725–36. doi: 10.1590/s0102-311x2009001200019. [DOI] [PubMed] [Google Scholar]
- 15.Lancaster CA, Gold KJ, Flynn HA, Yooh H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: A systematic review. Am J Obstet Gynecol. 2010;202:5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.King NM, Chambers J, O’Donnell K, Jayaweera SR, Williamson C, Glover VA. Anxiety, depression and saliva cortisol in women with a medical disorder during pregnancy. Arch Womens Ment Health. 2010;13:339–45. doi: 10.1007/s00737-009-0139-5. [DOI] [PubMed] [Google Scholar]
- 17.Vol. 894. Geneva: World Health Organ Tech Rep Ser; 2000. World Health Organization. Obesity: Preventing and managing the global epidemic Report of a WHO consultation on obesity. Technical report series, No 894; pp. 1–253. [PubMed] [Google Scholar]
- 18.Lovibond PE, Lovibond PF. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Therap. 1995;33:335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 19.Sahebi A, Asghari J, Salari Validation of Depression Anxiety and Stress Scale (DAS-21) for an Iranian population. J Iran Psychol. 2004;1:299–312. [Google Scholar]
- 20.Revised. 3rd ed. New York: Spring; 2006. The Ministry of Health and Medical Education of Iran. Family Health and Population Office of Maternal Health. National safe motherhood program. Integrated maternal health care. [Google Scholar]
- 21.Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W. Depression and anxiety during pregnancy: A risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20:189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- 22.Rubertsson C, Hellström J, Cross M, Sydsjö G. Anxiety in early pregnancy: Prevalence and contributing factors. Arch Womens Ment Health. 2014;17:221–8. doi: 10.1007/s00737-013-0409-0. [DOI] [PubMed] [Google Scholar]
- 23.Ajinkya S, Jadhav PR, Srivastava NN. Depression during pregnancy: Prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J. 2013;22:37–40. doi: 10.4103/0972-6748.123615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bonari L, Pinto N, Ahn E, Einarson A, Steiner M, Koren G. Perinatal risks of untreated depression during pregnancy. Can J Psychiatry. 2004;49:726–35. doi: 10.1177/070674370404901103. [DOI] [PubMed] [Google Scholar]
- 25.Perlen S, Woolhouse H, Gartland D, Brown SJ. Maternal depression and physical health problems in early pregnancy: Findings of an Australian nulliparous pregnancy cohort study. Midwifery. 2013;29:233–9. doi: 10.1016/j.midw.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 26.Hein A, Rauh C, Engel A, Häberle L, Dammer U, Voigt F, et al. Socioeconomic status and depression during and after pregnancy in the Franconian Maternal Health Evaluation Studies (FRAMES) Arch Gynecol Obstet. 2014;289:755–63. doi: 10.1007/s00404-013-3046-y. [DOI] [PubMed] [Google Scholar]
- 27.Miyake Y, Tanaka K, Arakawa M. Employment, income, and education and prevalence of depressive symptoms during pregnancy: The Kyushu Okinawa Maternal and Child Health Study. BMC Psychiatry. 2012;12:117. doi: 10.1186/1471-244X-12-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ding XX, Wu YL, Xu SJ, Zhu RP, Jia XM, Zhang SF, et al. Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103–10. doi: 10.1016/j.jad.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 29.Bödecs T, Szilágyi E, Cholnoky P, Sándor J, Gonda X, Rihmer Z, et al. Prevalence and psychosocial background of anxiety and depression emerging during the first trimester of pregnancy: Data from a Hungarian population-based sample. Psychiatr Danub. 2013;25:352–8. [PubMed] [Google Scholar]
- 30.Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, Fong DY. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. 2007;110:1102–12. doi: 10.1097/01.AOG.0000287065.59491.70. [DOI] [PubMed] [Google Scholar]


