Abstract
Background:
In Malaysia, contraceptive prevalence rate (CPR) during past three decades has been steady, with only 34% of women practicing modern contraception. The aim of this study was to determine the factors associated with modern contraceptive practices with a focus on spousal communication and perceived social support among married women working in the university.
Materials and Methods:
A cross-sectional study was carried out using self-administered structured questionnaire. The association between variables were assessed using Chi-square test, independent sample t-test, and logistic regression.
Results:
Overall, 36.8% of women used modern contraceptive methods. Significant association was found between contraceptive practice and ethnicity (P = 0.003), number of pregnancies (P < 0.001), having child (P = 0.003), number of children (P < 0.001), positive history of mistimed pregnancy (P = 0.006), and experience of unwanted pregnancy (P = 0.003). The final model showed Malay women were 92% less likely to use modern contraception as compared to non-Malay women. Women who discussed about family planning with their spouses were more likely to practice modern contraception than the women who did not [odds ratio (OR): 2.2, Confidence Interval (CI): 1.3–3.7]. Those women with moderate (OR: 4.9, CI: 1.6–10.8) and strong (OR: 14, CI: 4.5–26.4) perception of social support for contraceptive usage were more likely to use modern contraception than the women with poor perception of social support.
Conclusion:
Spousal communication regarding family planning would be an effective way to motivate men for supporting and using contraceptives. Family planning education initiatives should target both men and women, particularly high-risk cases, for promoting healthy timing and spacing of pregnancies. Ethnic disparities need to be considered in planning reproductive health programs.
Keywords: Contraceptive practices, family planning, social support, spousal communication
INTRODUCTION
According to the World Health Organization estimates, about 210 million pregnancies occur each year, one-third of which are unintended. Most of them end in still births, miscarriages, and induced abortions.[1] Five million women are hospitalized each year for treatment of abortion complications such as hemorrhages and sepsis.[2] When abortion is restricted by law and women have limited access to safe abortion, the rate of unsafe abortion increases.[3] In Malaysia, abortion is permitted to save the woman's life or to preserve her physical or mental health.[4] It lacks implementation and there is restricted access to abortion care in the public health care system.[5] Doctors are reluctant to provide abortion services, even to women who are legally qualified.[6] A high proportion (98%) of unsafe abortions occurs in the developing countries. Unsafe abortion is said to cause 13% of the maternal deaths or 68,000 deaths each year.[1,7]
Promoting family planning contributes substantially to improving maternal health, reducing child mortality, and for women's empowerment.[8,9] This requires that women have access to safe and effective contraceptive methods. Promoting family planning can help avoid unwanted pregnancy among reproductive women. Thus, improving maternal health is the core to achieving the Millennium Development Goal (MDG).[10]
Family planning also has potential to prevent high-risk pregnancies. Studies have shown significant association between parity, maternal age, and pregnancy outcomes such as obstetric complications, perinatal death, and neonatal morbidity, after adjusting for socioeconomic and demographic confounders.[11,12,13,14] An important aspect of family planning is Healthy Timing and Spacing of Pregnancy (HTSP) which helps women and couples space or delay their desired pregnancies, in order to achieve the healthiest outcomes for mothers and babies within the context of free and informed choice.[15]
It is estimated that 90% of abortion-related and 20% of pregnancy-related morbidity and mortality, along with 32% of maternal deaths, could be avoided by effective contraceptive practices.[8] In developing countries, about one in every six married women faces an “unmet need” for family planning. Demographic Health Survey (DHS) defined a woman to have an unmet need for contraception if she is fecund, sexually active, not using any form of contraception, and does not want a child for at least 2 years (spacers) or wants no more children (limiters).[16]
The importance of the unmet need for family planning was clearly restated by the Programme of the Action of the International Conference on Population and Development (ICPD) as “Government goals for family planning should be defined in terms of unmet needs for information and services” and that all countries should, over the next several years, assess the extent of national unmet need for good-quality family planning services.[17] One of the goals of ICPD includes 50% reduction in the unmet need for contraception by 2005 and its total reduction by 2015. A revitalization of the agenda is required and political willingness is also required to incorporate family planning into the development arena.[9]
Studies have shown that family planning information availability and proper counseling, demographic characteristics, cultural and religious beliefs, and economic and education level of the women can also affect the selection of a modern contraceptive method.[18,19,20] Husbands’ opposition to the use, fear of side effects, health concerns, and dissatisfaction with sexual sensation when using them have been identified as obstacles to the use of modern contraceptives.[21,22,23]
Lack of knowledge of modern contraceptive methods and their mechanism of action has been cited as one of the major reasons for the non-use of contraception by women.[24,25,26] Due to lack of knowledge on reproductive physiology and fertile period among women, especially adolescent girls, they may not be effectively assessing their risk of getting pregnant when they have occasional or infrequent sex.[27]
Furthermore, the importance of cooperation and support from men as partners is undeniable. Studies have shown that involving men in family planning counseling does increase contraceptive adoption, satisfaction of clients, effective use of contraception, and contraceptive continuation.[28,29] Husband's opposition has been reported as the main factor for not using any contraceptive methods among Turkish married women.[30] In South Asia, apart from husbands, the role of peers, mothers-in-law, and elders in contraceptive decision-making is well documented.[31,32,33] Urban women in Pakistan are more likely to use family planning if their mothers-in-law have discussed it with them as an option for their families.[31]
Several studies demonstrated strong positive association between spousal communication and use of contraceptive methods. The communication between husband and wife about family planning and the desired number of children is closely linked to successful contraceptive use.[34,35,36]
In Malaysia, the use of modern contraceptive method among married women is low. Contraceptive prevalence rate (CPR) during past three decades has been steady at about 50% for any method. In terms of modern contraception, only 34% of women practice these methods.[37] The Reproductive Rights Advocacy Alliance Malaysia (RRAAM) reported that unwanted pregnancies are increasing due to low contraceptive practice among Malaysian women.[38] Reports from Confidential Enquiries into Maternal Death (CEMD) Malaysia 2001–2005 revealed that in up to 70% of the maternal deaths, any form of family planning was not followed.[39] Maternal mortality due to postpartum hemorrhage (PPH) was greater among mothers with high parity, short birth intervals, with lack of antenatal care, and higher maternal age.[40]
There is a lack of published data in Malaysia about the factors influencing modern contraceptive use with a view on women's spousal communication and their perceived social support for using modern contraception. This study was planned to determine the factors associated with modern contraceptive practices among married female women working in a university. Findings of the study can provide health policymakers with the information needed to develop strategies to improve contraceptive practices among couples, especially among women in a university.
MATERIALS AND METHODS
A cross-sectional study was carried out among married female staff in the university. The list of married women between the ages of 20 and 49 years was obtained from the Registrar's office according to each faculty. Out of 15 faculties in the university, 9 faculties were selected randomly. The academic and non-academic staff of each faculty were selected using stratified random sampling. All married female staff (576) in selected faculties were invited to participate in this study. The women who were pregnant, infertile, menopausal women, medical lecturers as well as nurses were excluded from the study. The data for the study were collected using validated, reliable self-administered questionnaire which was written in Malay. Reproductive health knowledge scale was developed by researchers based on the World Health Organization guideline, Decision-Making Tool for Family Planning Clients and Providers (2005), and was divided into modern contraceptive knowledge (17 items) and reproductive system and sexually transmitted infection (STI) knowledge (9 items). Knowledge on modern contraceptive methods investigated included general awareness about contraceptive methods, indication, mode of action, and side effects of the methods. Knowledge on reproductive system and STI included physiology of human reproductive organs and STIs including HIV and its prevention. For the knowledge questions, the respondents were requested to respond to individual statements using the options “Yes,” “No,” or “Do not know.” For scoring of knowledge items, the respondents were given one point for answering correctly and no points for answering wrongly or that they did not know the answer. Respondents’ knowledge scores were summed up and then categorized as good (>75th percentile), moderate (50th–75th percentile), and poor (<50th percentile). Participants’ perceived social support from husbands and peers for contraceptive use was measured by seven items adopted and modified from a previous study.[33] All items related to this scale were scored on 5-point Likert scale from 1 (strongly disagree) to 5 (fully agree). Total score for perceived social support ranged from 7 to 35. Respondents’ perceived social support scores for modern contraceptive practice were categorized as follows: Poor if they obtained <50th percentile, moderate for 50th–75th percentile, and strong for >75th percentile.
Content validity of the questionnaire was ascertained by two medical doctors and a midwife. Pretesting of the questionnaire was carried out among 40 married female staff working in the administration building of the university to ensure that the respondents understood the items and to measure the reliability (internal consistency) of the scales in the questionnaire.
The Cronbach's alpha coefficient was 0.78 for modern contraceptive knowledge, 0.71 for knowledge on reproductive system and STI, and 0.86 for perceived social support. The Cronbach's alpha coefficient for all scales was above 0.70, indicating that the questionnaire had adequate reliability.[41]
Outcome variable in this study was modern contraceptive practice. A positive response was recorded if the woman or her husband was using any form of modern contraceptive methods within past 1 month. Oral contraceptive pills (OCP), injectables, condom, intrauterine device (IUD), implant, male sterilization (vasectomy), and female sterilization (tubal ligation) were considered as modern contraceptives. The independent variables studied were socio-demographic and reproductive health variables, reproductive health knowledge, having discussion with spouse about family planning methods, and perceived social support for contraceptive practice. Unintended pregnancy was classified as mistimed and unwanted. In this study, mistimed pregnancy was defined when pregnancy occurred sooner than the desire time and an unwanted pregnancy was defined when the woman reported that she did not want a child at the time of conception or any time in the future.[42] In the study, high-risk women for pregnancy were considered those aged >35 years, having high parity (≥5 pregnancies), or having a child younger than 2 years.
Statistical analysis
Data were analyzed using IBM, SPSS Inc., Chicago, USA. Significance level was set at P < 0.05. Descriptive analysis was presented in terms of frequency, percentage, means, and standard deviations. Chi-square test was used to determine the associations between categorical variables. Fisher's exact test was used to examine the association among categorical variables since the study sample size and cell sizes were relatively small. Independent sample t-test was used to compare the means of the two groups of an interval or the ratio of variables. The variables that were significant in the bivariate analysis were re-examined in the multivariate analysis. Binary logistic regression was conducted to identify the significant predictors after controlling other variables.
Ethical considerations
The Ethics Committee of the Faculty Medicine and Health Sciences, Universiti Putra Malaysia reviewed and approved the study protocol. From all married female staff who agreed to participate in the study, informed consent was obtained prior to their involvement in the research.
RESULTS
Socio-demographic and reproductive health characteristics
Out of 576 eligible women, 386 responded giving a response rate of 67%. The overall mean age of respondents was 34.53 years (SD = 7.27). Most of the participants were aged between 31 and 40 years. Minimum age was 24 years and maximum age was 49 years. Overall mean age of participants’ husbands was 37.10 years (SD = 8.37) with a range of 24–58 years. The mean working experience in years was 10.99 (SD = 7.81). Majority (61.7%) of the respondents had working experience of less than 10 years. The mean total household income was Malaysian Ringgit (RM) 5561 (SD = 3871). The mean age at marriage and duration of marriage was 25.1 (SD = 2.95) and 9.37 (SD = 7.75), respectively. The mean number of children was 2.49 (SD = 1.41) with a minimum of 1 and a maximum of 11. Overall, 51% of women used any of the contraceptive methods, of which 36.8% used modern and 14.2% practiced traditional contraceptive methods. Among the modern contraceptive users, OCP was reported as the most prevalent contraceptive method (51%), which was followed by IUD (19%), condom (17%), and injection (5.1%) [Figure 1]. Figure 2 shows the modern contraceptive practices among high-risk women, who were above 35 years, with high parity (≥5 pregnancies), and those with a child younger than 2 years. A majority (87%) of the respondents had heard about modern contraception. Awareness of specific modern contraception was as follows: For OCP (92%), IUD (83.4%), injectable (89%), implant (78.5%), male condom (93.5%), and female sterilization (85.5%); only 46% of the participants knew about vasectomy. Regarding modern contraceptive knowledge, overall, 15% of the participants had poor knowledge, 45% had moderate knowledge, and 40% had good knowledge.
Figure 1.
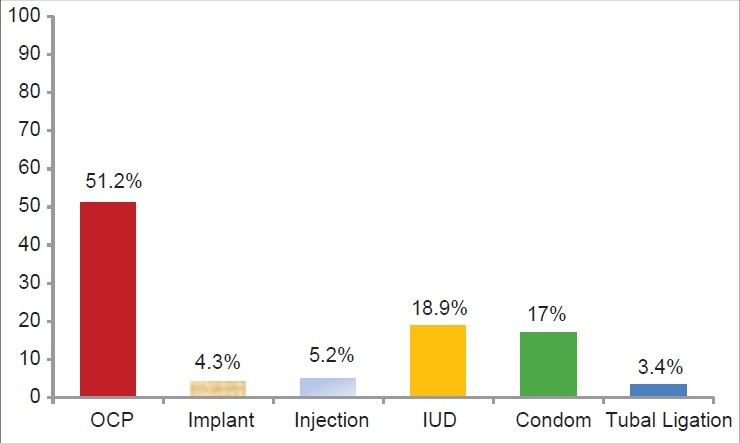
Distribution of modern contraceptive methods’ use among participants (n = 142)
Figure 2.
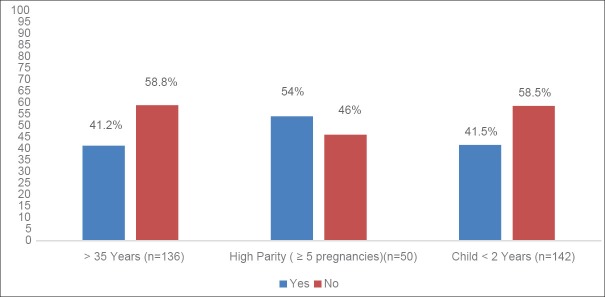
Modern contraceptive practices among high-risk women for pregnancy
Respondents’ knowledge on reproductive system and STI was poor in 53%, moderate in 35%, and good in 12% of the participants. Out of 386 respondents, 48% had discussed about family planning with their spouse while 52% had not. About one-third (32%) of the participants had strong, 52% had moderate, and 16% had poor perceived social support for modern contraceptive use.
Table 1 shows the association between use of modern contraceptives and background variables such as age, husband's age, income, ethnicity, and religion. Significant association was found only between ethnicity and modern contraceptive practice. The proportion of non-Malay women was more (7.7%) among contraceptive users compared to non-users (1.6%, P = 0.003). Table 2 shows the association between reproductive health factors and modern contraceptive practice. The mean number of pregnancies was significantly higher among modern contraceptive users (M = 3.04, SD = 1.70) compared to non-users of the methods (M = 2.32, SD = 1.86) [t (384) =1.59, P < 0.001]. Those women who had child more likely practiced modern contraception compared to childless women [χ2 = (1, 386) =8.75, P = 0.003]. The relation between number of children and modern contraceptive use was significant [χ2 = (2, 338) =17.26, P < 0.001]. A large majority (90.2%) of contraceptive users had between one and four children and only a small proportion (9.8%) of women with more than four children practiced modern contraception.
Table 1.
Association between socio-demographic variables and use of modern contraception (n=386)
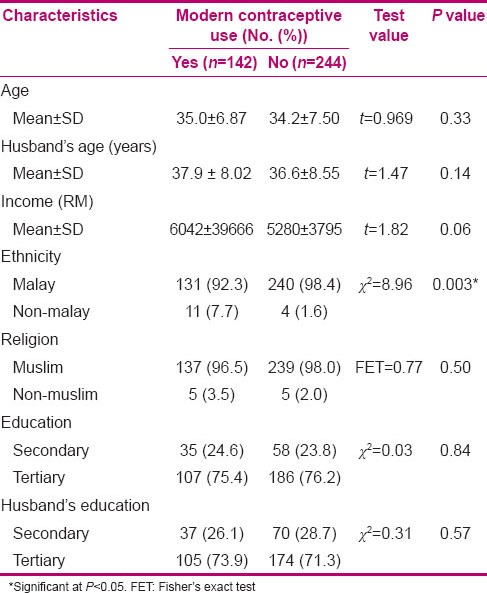
Table 2.
Association between marriage reproductive health variables and use of modern contraception (n=386)
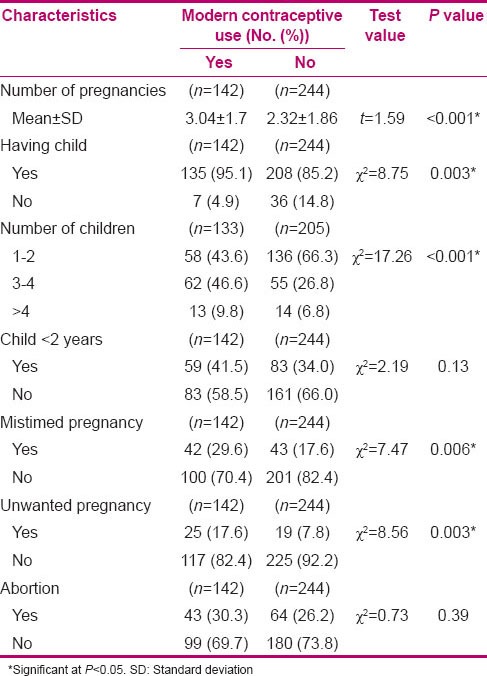
There was significant association between modern contraceptive practice and a past history of mistimed pregnancies [χ2 (1, 386) =7.47, P = 0.006]. Experience of mistimed pregnancies was higher among modern contraceptive users (29.6%) as compared to non-users (17.6%). Similarly, significant association was found between modern contraceptive practice and a positive past history of unwanted pregnancies [χ2 (1, 386) =8.56, P = 0.003]. Experience of unwanted pregnancies was more (17.6%) among modern contraceptive users than among non-users (7.8%).
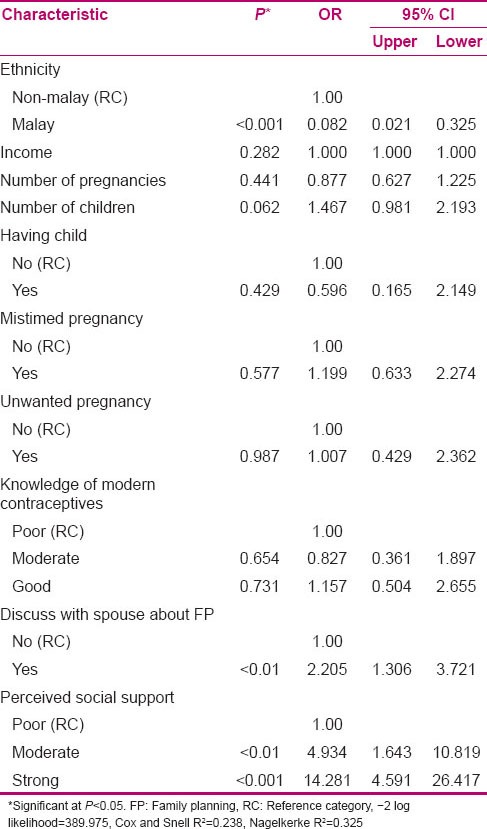
Table 3 shows that women who had good contraceptive knowledge significantly practiced modern contraceptive methods as compared to women with moderate or poor knowledge [χ2 (1, 386) =12.023, P = 0.002], while no significant association was found between knowledge of reproductive system–STI and modern contraceptive practice (P = 0.194). There was significant association between spousal communication and modern contraceptive practice [χ2 (1, 386) =131.5, P < 0.001]. Modern contraceptive users discussed with their spouses about family planning more than non-users (50.5% vs. 24.5%). Furthermore, significant association was found between perceived social support and modern contraceptive practice [χ2 (2, 386) =58.64, P < 0.001]. The observed association in bivariate analysis was further re-examined by logistic regression to identify adjusted association with the probability of using modern contraception [Table 4]. The variables such as ethnicity, discussing with spouse about family planning, and perceived social support are significant predictors of using modern contraceptives after controlling for other variables. Malay women [92%; odds ratio (OR): 0.082, 95% Confidence Interval (CI): 0.01–0.33] were less likely to use modern contraception as compared to non-Malay women. Further, those women who discussed with their spouse about family planning were 2.2 times more likely to practice contraceptive methods than those who did not (OR: 4.9, CI: 1.6–10.8; P < 0.01). Moreover, those women who had moderate (OR: 4.9, CI: 1.9–10.8) and strong (OR: 14.2, CI: 4.5–26.4) perception of social support for using modern contraceptives are more likely to use the contraceptive methods as compared to women with poor perception of social support. Nagelkerke R2 value was 0.325, suggesting that 32.5% of the variation in modern contraceptive practices is explained by the three predictor variables: Ethnicity, spousal communication, and perceived social support [Table 4].
Table 3.
Association between contraceptive practices and reproductive health knowledge, spousal communication, and social support
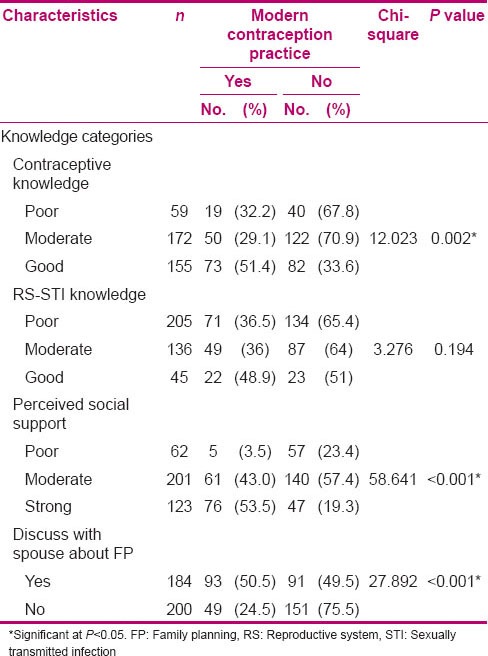
Table 4.
Logistic regression estimates of odds ratios of factors associated with modern contraceptive practices among married women in the university (n=386)
DISCUSSION
This study assessed the contraceptive practices and factors associated with modern contraceptive practices among married women at a public university in Malaysia. The CPR was almost the same as the recently reported figure (in 2004) by National Population and Family Development Board, i.e. 51.7%. In the current study, about 37% of the subjects practiced modern contraceptive methods. The study revealed that a majority (>60%) of women in reproductive age did not practice modern contraception. Poor contraceptive practice placed women at risk of unintended pregnancy and its negative health outcomes. The contraceptive practice among married female staff in the university was found to be relatively low in comparison with modern contraceptive practice in neighboring countries like Singapore (55%), Thailand (70%), and Vietnam (67%).[43] In this study, the Muslim majority Malay women were less likely to practice modern contraceptives as compared to non-Malay women. The low usage of contraception, particularly permanent methods, may reflect the women's religious belief that contraceptive practice is not permitted by Islam and putting a stop to pregnancy is considered a sin.[30,44] It should be noted that Islam generally permits reversible contraceptive methods and Islamic guiding principle for using contraception is safety of the method, legality, and only should be used in the context of marriage.[45,46,47,48] From the Islamic perspective, any contraception that is reversible and does not induce abortion can be used.[49,50] Muslim women were more likely to discontinue using contraception due to bleeding and pain than Protestant women. Because of the problems caused by some contraceptive method and inability to follow the religious rituals, Muslim women were more likely to stop the use of contraceptive.[51,52]
The findings of this study showed that about one-quarter of the respondents had experienced mistimed pregnancy and 11% had a positive history of unwanted pregnancy. This reflects that a higher proportion of unintended pregnancies occurred among those women who desired to delay their childbearing than those who wanted to limit their fertility.
Studies have shown that unintended pregnancy is associated with risky prenatal behaviors that increase poor pregnancy outcomes such as low birth weight, prematurity, and abuse among children born of unintended pregnancy.[53,54,55]
Prevention of pregnancy is more important among high-risk groups, namely subjects who are in postpartum period, breastfeeding women, those with high parity (≥5 pregnancies), >35-year-old women, and those approaching menopause. Globally, delayed childbearing and decline in birth rate are becoming general phenomena. The risk of adverse obstetric and perinatal outcome is increased by advancing maternal age.[14] Therefore, the physicians and health staff should explain the risk of advancing maternal age to clients who are planning a pregnancy. In the present study, more than half (58.5% out of 142) of the women who had a child below 2 years and also more than half (59% out of 136) of the women who were above 35 years old did not use modern contraceptive, which increases the chance of unintended and risky pregnancies. Studies have shown that inter-pregnancies interval of 3–5 years could raise the chance of infant and maternal survival by 2.5 times compared to children born at an interval of ≤2 years.[56,57]
Although a majority of participants were aware of modern contraception, their specific knowledge about modern contraception was inadequate. More than half (60%) of the participants had poor and moderate knowledge about the methods. Majority of the participants also lacked adequate knowledge about reproductive system and STI, whereas only 12% were found to have good knowledge. The importance of spousal communication for the use of contraception has been highlighted in several studies.[58,59,60] Investigation of the influence of spousal communication on the use of family planning methods in rural Nepal and Myanmar showed a strong positive impact of spousal communication on contraceptive use.[61,62]
It was found in the present study that women who had discussion with their spouses about family planning were 2.2 times more likely to practice modern contraception than the women who did not.
Studies have shown that exposure of women to physical abuse within their marriage significantly decreased contraceptive use among them.[63,64,65,66] It may be related to women's low power in abusive marriages to negotiate contraceptive methods’ usage with their husbands and are captured in a violent relationship with fewer options including autonomous family planning decisions.
Involving influential community members in family planning program can positively change couples’ contraceptive behaviors. A community-based intervention conducted among young couples in India and influential people such as parents, in-laws, and those who have a role in shaping family planning decision-making of young people was able to positively influence contraceptive behavior change of young couples.[67] The result of this study indicated that those women who had moderate or strong perception of social support for using modern contraceptives were more likely to use the contraceptive methods as compared to women with poor perception of social support. This finding is in agreement with Samandari et al.'s findings which showed that those women who believed that their husbands had a positive attitude toward contraception were more likely to use a method than those who did not (OR: 3.4, P < 0.001), while the women who were nervous about discussing contraception with their husbands were less likely than others to use a method (OR: 0.6, P < 0.05).
Similarly, Agha in Pakistan demonstrated the perception of women that their in-laws’ support in contraception use was the strongest determinant of their intentions to use hormonal contraceptive methods (OR: 2.12, CI: 1.68–2.68; P < 0.001), IUD (OR: 2.18, CI: 1.60–2.98; P < 0.001), and female sterilization (OR: 2.19; CI: 1.78–2.70; P < 0.001) in the next 12 months.[68] In Malaysia, men's role in family planning program and their contribution were not acknowledged.[69] Men need to be more involved in health educational programs for support and family planning practices. This study was carried out among married educated women in a public university, who may not be a representative sample of Malaysian women. More investigations need to be conducted in the actual community. The study showed that modern contraceptive use was low among married women in the university. Ethnicity, family planning spousal communication, and perceived social support were the most important predictors of modern contraceptive practices among married women in the university. Majority of the reproductive age women were at risk of unintended pregnancy, which can lead to poor maternal and child health outcomes. Serious attention should be paid to women with risk factors for high-risk pregnancies. Family planning education programs should target all the women in reproductive age, especially those who are in breastfeeding period, those with high parity, of advanced age, and approaching menopause, for promoting HTSP. Therefore, educating women can contribute to improve maternal and child health that is the central goal of the MDG four and five.
ACKNOWLEDGMENT
The authors wish to thank the deans of all faculties in University Putra Malaysia for their permission to conduct this study and all the staff for their participation in this research.
Footnotes
Source of Support: This study financially has been supported by Research Management Center, University Putra Malaysia (Grant No: 9337800).
Conflict of Interest: The authors have no conflicts of interest to disclose.
REFERENCES
- 1.6th ed. Geneva: World Health Organization; 2011. World Health Organization, Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. [Google Scholar]
- 2.Singh S. Hospital admissions resulting from unsafe abortion: Estimates from 13 developing countries. Lancet. 2006;368:1887–92. doi: 10.1016/S0140-6736(06)69778-X. [DOI] [PubMed] [Google Scholar]
- 3.Geneva: World Health Organization; 1998. World Health Organization, Unsafe Abortion: Global and regional estimates of incidence of and mortality due to unsafe abortion with a listing of available country data. [Google Scholar]
- 4.Center for reproductive rights. The World's Abortion Laws. 2007. Available from: http//www.reproductiverights.org . Last accessed on 2012 Oct 20.
- 5.Abdullah R. Malaysia: Arrows for Change; 2009. Abortion in Malaysia: Legal yet still inaccessible. 15 (2/3) pp. 8–9. [Google Scholar]
- 6.Whittaker A. Vol. 20. New York: Berghahn Books; 2010. Abortion in Asia: Local dilemmas, global politics. [Google Scholar]
- 7.5th ed. Geneva: World Health Organization; 2007. World Health Organization, Unsafe abortion, Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003. [Google Scholar]
- 8.Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: The unfinished agenda. Lancet. 2006;368:1810–27. doi: 10.1016/S0140-6736(06)69480-4. [DOI] [PubMed] [Google Scholar]
- 9.New York: 2004. United Nations Population Fund. State of the world population. The Cairo Consensus at Ten: Population, Reproductive Health and the Global Effort to End Poverty. [Google Scholar]
- 10.World Health Organisation, Making Pregnancy Safer: Annual Report 2007 Geneva. 2008 [Google Scholar]
- 11.Ananth CV, Wilcox AJ, Savitz DA, Bowes JW, Luther ER. Effect of maternal age and parity on the risk of uteroplacental bleeding disorders in pregnancy. Obstet Gynecol. 1996;88:511–6. doi: 10.1016/0029-7844(96)00236-0. [DOI] [PubMed] [Google Scholar]
- 12.Bai J, Wong FW, Bauman A, Mohsin M. Arity and pregnancy outcomes. Am J Obstet Gynecol. 2002;186:274–8. doi: 10.1067/mob.2002.119639. [DOI] [PubMed] [Google Scholar]
- 13.Al-Farsi Y, Brooks D, Werler M, Cabral H, Al-Shafei M, Wallenburg H. Effect of high parity on occurrence of anemia in pregnancy: A cohort study. BMC Pregnancy Childbirth. 2011;11:7. doi: 10.1186/1471-2393-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koo YJ, Ryu HM, Yang JH, Lim JH, Lee JE, Kim MY, et al. Pregnancy outcomes according to increasing maternal age. Taiwan J Obstet Gynecol. 2012;51:60–5. doi: 10.1016/j.tjog.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Geneva, Switzerland: 2006. World Health Organisation, Report of a WHO Technical consultation on birthspacing. [Google Scholar]
- 16.Hossain SM, Khan ME, Rahman M, Sebastian MP. New Delhi, India; 2005. South East Asia Regional Training Manual. [Google Scholar]
- 17.United Nations Population Fund, Programme of action of the international conference on population and development. 1994 [Google Scholar]
- 18.Salter C, Johnston HB, Hengen N. Care for postabortion complications: Saving women's lives. Population Reports 1997, Series L: Issues in World Health. (10):1–31. [PubMed] [Google Scholar]
- 19.McCauley AP, Robey B, Blanc AK, Geller JS. Washington, DC: 1994. Opportunities for women through reproductive choice. Population reports. Series M. Special topics; p. 12. [PubMed] [Google Scholar]
- 20.Sathar ZA, Chidambaram VC. Netherlands: Voorburg; 1984. Differentials in contraceptive use. [Google Scholar]
- 21.Bongaarts J, Bruce J. The causes of unmet need for contraception and the social content of services. Stud Fam Plann. 1995;26:57–75. [PubMed] [Google Scholar]
- 22.Casterline JB, Perez AE, Biddlecom AE. Factors underlying unmet need for family planning in the Philippines. Stud Fam Plann. 1997;28:173–91. [PubMed] [Google Scholar]
- 23.Nagase T, Kunii O, Wakai S, Khaleel A. Obstacles to modern contraceptive use among married women in southern urban Maldives. Contraception. 2003;68:125–34. doi: 10.1016/s0010-7824(03)00113-6. [DOI] [PubMed] [Google Scholar]
- 24.Kham MH, Shah H, Saba N. Study of contraceptive user women in Dikhan, Pakistan. Biomedica. 2007;23:24–6. [Google Scholar]
- 25.Sajid A, Malik S. Vol. 4. Lahore: Annals of King Edward Medical University; 2010. Knowledge, Attitude and Practice of Contraception among Multiparous Women at Lady Aitchison Hospital; p. 16. [Google Scholar]
- 26.Wu L. A survey on the knowledge, attitude, and behaviour regarding contraception use among pregnant teenagers in Beijing, China. Clin Nurs Res. 2010;19:403–15. doi: 10.1177/1054773810375982. [DOI] [PubMed] [Google Scholar]
- 27.Sedgh G, Hussain R, Bankole A, Singh S. United States: Alan Guttmacher Institute; 2007. Women with an unmet need for contraception in developing countries and their reasons for not using a method. [Google Scholar]
- 28.Terefe A, Larson CP. Modern contraception use in Ethiopia: Does involving husbands make a difference? Am J Public Health. 1993;83:1567–71. doi: 10.2105/ajph.83.11.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang CC, Vittinghoff E, Hua LS, Yun WH, Rong ZM. Reducing pregnancy and induced abortion rates in China: Family planning with husband participation. Am J Public Health. 1998;88:646–8. doi: 10.2105/ajph.88.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sahin HA, Sahin HG. Reasons for not using family planning methods in Eastern Turkey. Eur J Contracept Reprod Health Care. 2003;8:11–6. [PubMed] [Google Scholar]
- 31.Kadir MM, Fikree FF, Khan A, Sajan F. Do mothers-in-law matter? Family dynamics and fertility decision-making in urban squatter settlements of Karachi, Pakistan. J Biosoc Sci. 2003;35:545–58. doi: 10.1017/s0021932003005984. [DOI] [PubMed] [Google Scholar]
- 32.Kansal A, Kandpal SD, Mishra P. Reasons for not practicing contraception in a rural population of Dehradun District. J Commun Dis. 2006;38:97. [PubMed] [Google Scholar]
- 33.Samandari G, Speizer IS, O’Connell K. The role of social support and parity on contraceptive use in Cambodia. Int Perspect Sex Reprod Health. 2010;36:122–31. doi: 10.1363/ipsrh.36.122.10. [DOI] [PubMed] [Google Scholar]
- 34.Balaiah D, Naik DD, Ghule M, Tapase P. Determinants of spacing contraceptive use among couples in Mumbai: A male perspective. J Biosoc Sci. 2005;37:689–704. doi: 10.1017/S0021932005007145. [DOI] [PubMed] [Google Scholar]
- 35.Klomegah R. Spousal communication, power, and contraceptive use in Burkina Faso, West Africa. Marriage Fam Rev. 2006;40:89–105. [Google Scholar]
- 36.Kaggwa EB, Diop N, Storey JD. The role of individual and community normative factors: A multilevel analysis of contraceptive use among women in union in Mali. Int Fam Plan Perspec. 2008;34:79–88. doi: 10.1363/ifpp.34.079.08. [DOI] [PubMed] [Google Scholar]
- 37.United Nations Population Fund, Country Profile for Population and Reproductive Health: Policy Developments and Indicators. 2004 [Google Scholar]
- 38.Asian Pacific Resource and Research Center, Women's gender and rights perspectives in health policies and programmes. ARROW. 2006;12(3):7. [Google Scholar]
- 39.Kuala Lumpur, Malaysia: Ministry of Health; 2008. Ministry of Health Malaysia, Report on the confidential enquiries into maternal deaths in Malaysia 2001 -2005. [Google Scholar]
- 40.Achanna KS. Postpartum Haemorrhage: A Continuing Tragedy in Malaysia. Med J Malaysia. 2011;66:1–3. [PubMed] [Google Scholar]
- 41.DeVellis R. Scale development: Theory and applications. Applied Social Research Methods Series. In: Bickman L, Rog DJ, editors. Thousand Oaks. Calif: SAGE Publications, Inc; 2003. [Google Scholar]
- 42.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Vol. 25. Maryland, USA: 2005. Fertility, family planning, and reproductive health of US women: Data from the 2002 National Survey of Family Growth. Vital and health statistics. Series 23, Data from the National Survey of Family Growth; p. 1. [PubMed] [Google Scholar]
- 43.Sciortino R. Bangkok, Thailand: Asia Pacific Alliance for Sexual and Reproductive Health and Rights; 2010. Achieving contraceptive security and meeting reproductive health needs in Southeast Asia. [Google Scholar]
- 44.Shah MA, Shah NM, Chowdhury RI, Menon I. Unmet need for contraception in Kuwait: Issues for health care providers. Soc Sci Med. 2004;59:1573–80. doi: 10.1016/j.socscimed.2004.01.033. [DOI] [PubMed] [Google Scholar]
- 45.Paksima SM, Madanat HN, Hawks SR. A contextual model for reproductive health education: Fertility and family planning in Jordan. Promot Educ. 2002;9:89–95. [PubMed] [Google Scholar]
- 46.Pennachio D. Caring for your Muslim patients. Stereotypes and misunderstandings affect the care of patients from the Middle East and other parts of the Islamic World. Med Econ. 2005;82:46. [PubMed] [Google Scholar]
- 47.Schenker JG, Rabenou V. Family planning: Cultural and religious perspectives. Hum Reprod. 1993;8:969–76. doi: 10.1093/oxfordjournals.humrep.a138176. [DOI] [PubMed] [Google Scholar]
- 48.Siraj H. Family planning and contraception. Removing the religious and sociocultural barriers among Malaysian women. Presented at 9th World Congress of International Association for Maternal and Neonatal Health (IAMANEH)-Cairo Marriot, Egypt on Nov, 3th. 2006 [Google Scholar]
- 49.Christianity. In: LoPresti AF, editor; Manning C, Zuckerman P, editors. Sex and religion. Toronto: Thomson Wadsworth; 2005. pp. 117–41. [Google Scholar]
- 50.Omran AR. New York: Psychology Press; 2004. Family planning in the legacy of Islam. [Google Scholar]
- 51.Fathizadeh N, Salemi P, Ehsanpour S. Dissatisfaction with contraceptive methods. Iran J Nurs Midwifery Res. 2011;16:79–82. [PMC free article] [PubMed] [Google Scholar]
- 52.Rivera R, Chen-Mok M, McMullen S. Analysis of client characteristics that may affect early discontinuation of the TCu-380A IUD. Contraception. 1999;60:155–60. doi: 10.1016/s0010-7824(99)00077-3. [DOI] [PubMed] [Google Scholar]
- 53.Hulsey TM. Association between early prenatal care and mother's intention of and desire for the pregnancy. J Obstet Gynecol Neonatal Nurs. 2001;30:275–82. [PubMed] [Google Scholar]
- 54.Orr ST, James SA, Reiter JP. Unintended pregnancy and prenatal behaviors among urban, black women in Baltimore, Maryland: The Baltimore preterm birth study. Ann Epidemiol. 2008;18:545–51. doi: 10.1016/j.annepidem.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 55.Goto A, Yasumura S, Yabe J, Anazawa Y, Hashimoto Y. Association of pregnancy intention with parenting difficulty in Fukushima, Japan. J Epidemiol. 2005;15:244–6. doi: 10.2188/jea.15.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Setty-Venugopal V, Upadhyay UD. Birth spacing: Three to five saves lives. Pop Rep. 2002;50:1–23. [PubMed] [Google Scholar]
- 57.Whitworth A, Stephenson R. Birth spacing, sibling rivalry and child mortality in India. Soc Sci Med. 2006;55:2107–19. doi: 10.1016/s0277-9536(02)00002-3. [DOI] [PubMed] [Google Scholar]
- 58.Mahmood N, Ringheim K. Factors affecting contraceptive use in Pakistan. The Pak Dev Rev. 1996;35:1–22. [PubMed] [Google Scholar]
- 59.Salem RM, Bernstein J, Sullivan TM, Lande R. Communication for Better Health Pop Rep 2008 [Google Scholar]
- 60.Mostafavi SF, Mehryar AH, Agha H. Socio-Cultural Factors Affecting Men's Use of Family Planning Methods in Iran. Journal of Social Sciences and Humanities of Shiraz University; 2006;24:9–15. [Google Scholar]
- 61.Link CF. Spousal Communication and Contraceptive Use in Rural Nepal: An Event History Analysis. Stud Fam Plann. 2011;42:83–92. doi: 10.1111/j.1728-4465.2011.00268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mon MM, Liabsuetrakul T. Predictors of contraceptive use among married youths and their husbands in a rural area of Myanmar. Asia Pac J Public Health. 2010;24:151–60. doi: 10.1177/1010539510381918. [DOI] [PubMed] [Google Scholar]
- 63.Gharaibeh MK, Oweis A, Shakhatreh F, Froelicher ES. Factors Associated with Contraceptive Use among Jordanian Muslim Women: Implications for Health and Social Policy. J Int Womens Stud. 2013;12:168–84. [Google Scholar]
- 64.Heise LL, Ellsberg M, Gottemoeller M. Ending violence against women. Baltimore: John Hopkins University School of Public Health. Population Information Program 1999. Series L, No. 1. [Google Scholar]
- 65.Kishor S, Johnson K. Calverton, Maryland: 2004. Profiling domestic violence: A multi-country study. Measure DHS+, ORC Macro. [Google Scholar]
- 66.Williams CM, Larsen U, McCloskey LA. Intimate partner violence and women's contraceptive use. Violence Against Women. 2008;14:1382–96. doi: 10.1177/1077801208325187. [DOI] [PubMed] [Google Scholar]
- 67.Daniel EE, Masilamani R, Rahman M. The effect of community-based reproductive health communication interventions on contraceptive use among young married couples in Bihar, India. Int Fam Plan Perspect. 2008;34:189–97. doi: 10.1363/ifpp.34.189.08. [DOI] [PubMed] [Google Scholar]
- 68.Agha S. Intentions to use contraceptives in Pakistan: Implications for behavior change campaigns. BMC Public Health. 2010;10:450. doi: 10.1186/1471-2458-10-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abdul Manaf R, Manaf M. Male participation and sharing of responsibility in strengthening family planning activities in Malaysia. Malays J Public Health Med. 2010;10:23–7. [Google Scholar]


