Introduction
Cancer-related fatigue (CRF) is the most commonly reported side effect of cancer treatment [1]. It is defined by the National Comprehensive Cancer Network as “a distressing, persistent, subjective sense of physical, emotional, and cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity.” Patients feel tired even after resting, have reduced capacity to carry out normal activities, experience slow physical recovery from tasks, and report diminished concentration. Most patients experience CRF during their treatment and many continue to experience CRF long after all treatment has ended. In our research with survivors of hematopoietic stem cell transplantation (HSCT) 1-3 years off treatment, 40% of those interviewed reported clinically significant CRF.
Various pharmacological and non-pharmacological interventions have been studied to treat CRF with generally mild to moderate effect sizes [1]. An alternative intervention may be systematic bright white light (BWL) exposure, which is far less costly and involves less patient burden than other interventions. Reviews and meta-analyses have [2] reported that BWL is effective in reducing sleep and circadian rhythm problems associated with other disorders (e.g., depression, jet lag), but has not been previously tested for the effect on fatigue. Recent research from our group has shown that, when given during chemotherapy, BWL compared to dim red light (DRL) keeps CRF from getting worse [3]. However, to date, the impact of BWL on fatigue among cancer survivors has not been examined.
This preliminary efficacy trial sought to determine the impact of BWL on CRF among survivors of breast and gynecologic cancers who had completed all cancer treatment, and survivors of hematological malignancy who had completed HSCT. We tested the hypothesis that the BWL condition would result in a significant reduction in CRF compared to the DRL condition.
Methods
Participants
Thirty-six cancer survivors from the Mount Sinai Hospital in New York, NY participated in the study (CONSORT Flow Diagram) across all four seasons. Inclusion criteria were: up to 3.5 years post HSCT, up to 3 years post completion of chemotherapy or chemotherapy and radiation for breast cancer, or any time post completion of treatment for gynecologic cancer; 18 years of age or older; and reporting clinically significant fatigue as measured by the Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-Fatigue) scale. Exclusion criteria were: pregnancy; confounding underlying medical illnesses such as significant pre-existing anemia; history of mania (which is a contra-indication for light treatment) or current clinical depression; and any other physical or psychological impairment including a sleep disorder which would limit participation. The study was approved by the Program for the Protection of Human Subjects at Mount Sinai Hospital.
Procedure
Cancer survivors were approached by study personnel during their regular follow-up clinical visits at Mount Sinai. The study was described, signed consent obtained, and the screening/eligibility measures administered. Participants who qualified were then randomized to either the BWL (n=18) or the DRL (n=18) group. All participants completed questionnaires on fatigue at four time points: baseline, during the second week of the intervention, at the end of the 4-week intervention, and three weeks after the completion of the intervention.
Light treatment
The BWL condition was compared to the DRL condition. Traditionally, DRL has been used as a comparison for BWL as the biological clock is less sensitive to wavelengths in the red light area [4]. Both BWL and DRL treatment were administered via a Litebook 1.2 (Litebook®, Ltd. Medicine Hat, Canada). For the BWL condition, the Litebook® used 60 premium white light emitting diode (LED) lights which mimic the visible spectrum of sunlight (full spectrum white light) for minimum glare and maximum eye comfort. An identical-appearing device utilizing red LEDs emitting <50 lux was used for the DRL comparison group. Participants were instructed to self-administer the light treatment in their homes by placing the light box at a 45 degree angle, 18 inches from their face, for 30 minutes every morning within 30 minutes of waking throughout the four week intervention period.
Measures
Cancer-related fatigue was measured with the FACIT-Fatigue scale A FACIT-Fatigue score ≤30 constitutes clinically significant fatigue [5]. Since depression is a known correlate of fatigue, the Brief Symptom Inventory depression scale was also used [6].
Results
Participant Characteristics
Table 1 contains descriptive medical and demographic information for the sample. The General Linear Model analysis of baseline fatigue indicated no significant (p=0.4840) difference between the DRL and BWL groups at baseline. There was also no significant (F(1,23)=0.95; p=0.3389) difference between the two light conditions at baseline in participants’ belief that the treatment to which they had been assigned would successfully reduce their fatigue.
Table 1.
Patient demographics and medical variables
| n = 36 |
|
|---|---|
| Gender | |
| Male | 7 (19)1 |
| Female | 29 (81) |
| Race/Ethnicity | |
| Black | 11(31) |
| White | 12(33) |
| Other | 13(36) |
| Living Arrangement | |
| Live Alone | 4(13) |
| Live with spouse/partner | 12(40) |
| Live with parents | 2(7) |
| Other | 12(40) |
| Marital status | |
| Single | 4 (13) |
| Married/Partnered | 14(47) |
| Separated | 5 (17) |
| Divorced | 5 (17) |
| Other | 2 (6) |
| Children | |
| Yes | 22(76) |
| No | 7(24) |
| Education | |
| High School Graduate | 4(14) |
| Some College/Post-College | 7 (24) |
| College Graduate | 10(34) |
| Graduate Degree | 8(28) |
| Employed | |
| No | 16(62) |
| Yes | 10(38) |
| Annual Income (in Dollars) | |
| 0 - 9999 | 4(15) |
| 10,000-19,999 | 3(12) |
| 30,000-39,999 | 1(4) |
| 40,000-49,999 | 3(11) |
| 50,000-59,999 | 1(4) |
| 60,000-69,999 | 1(4) |
| 70,000-79,999 | 1(4) |
| Above 80,000 | 12(46) |
| Diagnosis | |
| Acute Myeloid Leukemia | 4(10) |
| Follicular non-Hodgkin's | |
| Lymphoma | 2(6) |
| Hodgkin's Lymphoma | 1(3) |
| Multiple Myeloma | 10(28) |
| Myelofibrosis | 1(3) |
| Breast Cancer | 15(41) |
| Endometrial Cancer | 2(6) |
| Ovarian cancer | 1(3) |
| Months Post Diagnosis | 17.22(10.11)2 |
n(percentage)
mean(SD)
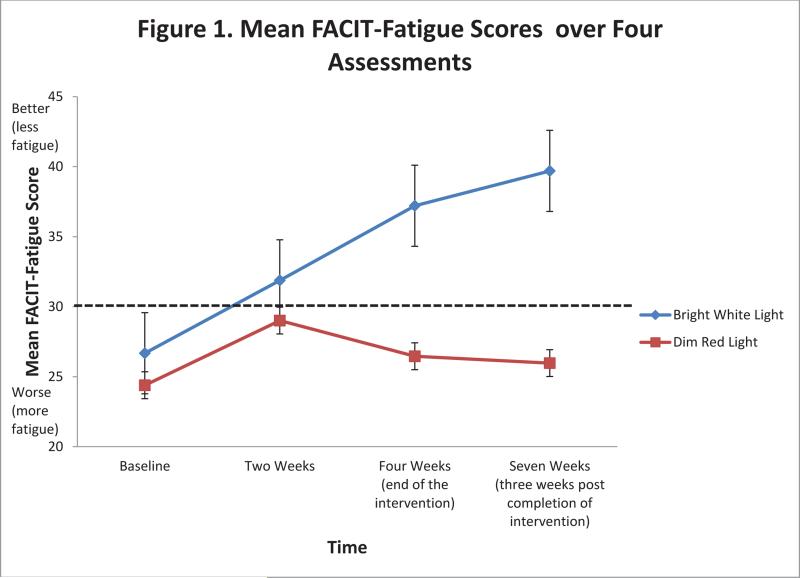
Effect of light on CRF
Using a linear mixed model repeated measures analysis (SAS Proc MIXED), there was a significant time effect (F(3(68)=5.93; p=0.0012) suggesting that fatigue levels changed over time. There was a significant group effect (F(1,28)=7.12; p=0.0125) suggesting that across all time points, the BWL group had less fatigue than the DRL group. In addition, there was a significant time x treatment effect (F(3,68)=5.27; p=0.0025) indicating that the groups differed with respect to change in fatigue over time. As can be seen in Fig 1, there was a significant improvement in fatigue over time for those in the BWL condition while, in the DRL condition, fatigue improved at two weeks but became worse at 4-weeks and at follow-up. There was a large effect size (d) at 0.98 [7]. When depression was added to the model as a control variable with assessment time and the treatment variable, depression was not a statistically significant (p = 0.3322) predictor of CRF and BWL remained a statistically significant predictor of fatigue.
Figure 1.
Mean FACIT-Fatigue scores for Bright White Light and Dim Red Light conditions over four assessment time points. Higher FACIT-Fatigue score corresponds to less fatigue. FACIT-Fatigue score equal to or less than 30 constitutes clinically significant fatigue. Standard errors are given.
At the end of the 4-week intervention, no patients in the BWL condition were still clinically fatigued (FACIT-Fatigue score >30) whereas 55% of patients in the DRL condition were still clinically fatigued.
Discussion
This preliminary efficacy trial showed that CRF among clinically fatigued cancer survivors was significantly reduced among those who were exposed to BWL but not among those exposed to DRL. To our knowledge, this is the first study to show beneficial effects of BWL exposure on fatigue in cancer survivors.
Although other studies have examined non-pharmacologic treatments of fatigue, the effect size (d = 0.98) in this study was larger than the small to moderate effects seen in other interventions [1]. Three weeks following the completion of the intervention, none of the participants in the BWL condition reported clinical levels of fatigue whereas most of the participants in the DRL condition continued to report clinical levels of fatigue. It is important to note that the BWL intervention is a low cost and low burden intervention compared with alternative approaches (most of which require travel to meet with a clinician and intensive clinician involvement).
Although these results are encouraging, this study is preliminary. Because the follow-up assessment was only three weeks, the long-term effect of BWL on CRF is not yet known. In addition, potential mechanisms underlying the effects of BWL on CRF were not examined. BWL may affect CRF through its effects on circadian activity rhythms (CARs) – a chronobiological mechanism theorized to underlie CRF. CARs serve the function of preparing the body for restful sleep at some times of the day and for active wakefulness at others. CARs are biological cycles that are slightly longer than 24-hours and are entrained to the 24-hour day by environmental Zeitgebers (time cue) such as bright light. Several studies have observed desynchronized CARs among cancer patients and survivors [8] and CARs have been found to be associated with fatigue in cancer patients [9]. A recent study from our group found that BWL prevented CAR deterioration among breast cancer patients undergoing chemotherapy [10]. Other mechanisms involving circadian neuroendocrine regulation and inflammatory dynamics may also be involved. Future studies with larger and more diverse samples are needed to determine the long-term effects of BWL on CRF and to examine the potential mechanisms underlying the effects of BWL on CRF among cancer survivors.
Despite these limitations, the present study suggests that BWL, a safe, inexpensive and easily delivered treatment, may be a clinically effective intervention to treat CRF among cancer survivors who continue to experience CRF long after medical treatment has ended.
Five Key Points.
Cancer related fatigue (CRF) lasts well beyond the end of cancer treatment.
Light has a strong effect on sleep and circadian rhythms in other medical conditions, but the effect of light on CRF has only just begun to be tested.
Preliminary studies in breast cancer suggest that Bright White Light (BWL), compared to Dim Red Light (DRL), kept CRF from worsening during chemotherapy.
The current preliminary study tested BWL vs DRL on 36 patients post hematopoietic stem cell transplantation (HSCT), post chemotherapy or chemotherapy and radiation for breast cancer, or post completion of treatment for gynecologic cancer.
Results suggest that BWL reduced fatigue in these patients while DRL did not. In addition, post light treatment, no patients in the BWL group reported any residual fatigue while 55% of those in the DRL condition still reported fatigue.
Acknowledgements
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers R21CA158954 and K05CA108955. Additional support was provided by grant UL1TR000067 from the National Center for Advancing Translational Sciences, National Institutes of Health.
REFERENCES
- 1.Kangas M, Bovbjerg DH, Montgomery GH. Cancer-related fatigue: a systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychol Bull. 2008;134:700–741. doi: 10.1037/a0012825. doi: 10.1037/a0012825. [DOI] [PubMed] [Google Scholar]
- 2.Golden RN, Gaynes BN, Ekstrom RD, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005 Apr;162(4):656–62. doi: 10.1176/appi.ajp.162.4.656. [DOI] [PubMed] [Google Scholar]
- 3.Ancoli-Israel S, Rissling M, Neikrug A, et al. Light treatment prevents fatigue in women undergoing chemotherapy for breast cancer. Support Care Cancer. 2012;20(6):1211–1219. doi: 10.1007/s00520-011-1203-z. doi: 10.1007/s00520-011-1203-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glickman G, Byrne B, Pineda C, Hauck WW, Brainard GC. Light therapy for seasonal affective disorder with blue narrow-band light-emitting diodes (LEDs). Biol Psychiatry. 2006 Mar 15;59(6):502–7. doi: 10.1016/j.biopsych.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Cella D. The Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) scale: Summary of development and validation. 2013 Sep 3; Update. 2013. [Google Scholar]
- 6.Derogatis L. Brief Symptom Inventory 18: administration, scoring, and procedures manual. Minneapolis: NCS Assessments. 2001 [Google Scholar]
- 7.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 8.Pati AK, Parganiha A, Kar A, Soni R, Roy S, Choudhary V. Alterations of the characteristics of the circadian rest-activity rhythm of cancer in-patients. Chronobiol Int. 2007;24(6):1179–1197. doi: 10.1080/07420520701800868. doi: 10.1080/07420520701800868. [DOI] [PubMed] [Google Scholar]
- 9.Payne JK. Altered circadian rhythms and cancer-related fatigue outcomes. Integr Cancer Ther. 2011;10(3):221–233. doi: 10.1177/1534735410392581. doi: 10.1177/1534735410392581. [DOI] [PubMed] [Google Scholar]
- 10.Neikrug AB, Rissling M, Trofimenko V, et al. Bright light therapy protects women from circadian rhythm desynchronization during chemotherapy for breast cancer. Behav Sleep Med. 2012;10(3):202–216. doi: 10.1080/15402002.2011.634940. doi: 10.1080/15402002.2011.634940. [DOI] [PubMed] [Google Scholar]