Abstract
Objective: In this study, we evaluated parent and child characteristics as predictors and moderators of response in the four-site Treatment of Severe Childhood Aggression (TOSCA) study.
Methods: A total of 168 children with severe aggression, disruptive behavior disorder, and attention-deficit/hyperactivity disorder (ADHD) were enrolled in a 9-week trial of basic treatment (n=84, stimulant+parent training+placebo) versus augmented treatment (n=84, stimulant+parent training+risperidone). In the initial report, augmented treatment surpassed basic treatment in reducing the primary outcome of disruptive behavior (D-Total) scores. In the current study, we evaluated parent (income, education, family functioning, employment) and child variables (intelligence quotient [IQ], aggression type, comorbid symptomatology) as predictors or moderators, using linear mixed models and the MacArthur guidelines.
Results: Higher scores on ADHD symptom severity and callous/unemotional traits predicted better outcome on D-Total regardless of treatment assignment. Two moderators of D-Total were found: Higher anger/irritability symptoms and lower mania scores were associated with faster response, although not better overall effect at endpoint, in the augmented but not the basic group. Several variables moderated response on secondary outcomes (ADHD severity and prosocial behavior), and were characterized by faster response, although not better outcome, in the augmented but not in the basic group. Maternal education moderated outcome on the measure of positive social behavior; children of mothers with less education benefited more from augmented treatment relative to basic than those with more education.
Conclusion: Although these findings require validation, they tentatively suggest that augmented treatment works equally well across the entire sample. Nevertheless, certain child characteristics may be useful indicators for the speed of response to augmented treatment.
Introduction
The disruptive behavior disorders (DBD) oppositional defiant disorder (ODD) and conduct disorder (CD), especially in combination with severe aggression, are a significant public health concern. Children who engage in these behaviors are at increased risk of later psychopathology, substance abuse, criminal behavior, and incarceration, and are also more likely themselves to be victims of violent crimes (Stattin and Magnusson 1989; Fergusson and Horwood 1998; Tremblay et al. 2004).
Pharmacotherapy, especially with antipsychotic agents, is effective in the treatment of disruptive behavior in children (for review, see Zuddas et al. 2011), although studies have typically focused on children with a subaverage intelligence quotient [IQ] (McKinney and Renk 2011). Concomitant pharmacotherapy (psychostimulant plus antipsychotic), an approach frequently used in clinical settings, has had little empirical evidence until recently (Bussing and Winterstein 2012). In a 9 week, double-blind, placebo-controlled study, the Treatment of Severe Childhood Aggression (TOSCA) network explored the effectiveness of adding risperidone to ongoing stimulant (STIM) and parent training in behavior management (PT) (Aman et al. 2014). Participants had average IQ and a clinically significant level of physical or object aggression and Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) diagnoses of attention-deficit hyperactivity disorder (ADHD, any subtype), and ODD or CD (American Psychiatric Association 1994; see Farmer et al. 2011 for complete design details). A sizeable decrease (Cohen's d=1.25) in disruptive behaviors, as measured by the primary outcome (Nisonger Child Behavior Rating Form Disruptive Total [NCBRF D-Total]), was observed after 3 weeks of PT+STIM. However, most children remained impaired at 3 weeks, and began treatment with risperidone (augmented treatment) or placebo (basic treatment) (n=8; did not receive second drug). At 9 weeks, a moderate and statistically significant effect was observed in favor of augmented treatment on the D-Total.
Although augmented treatment was effective in further reducing NCBRF D-Total scores, ∼ 20% of the augmented group remained nonresponders (compared with ∼ 30% of the basic group; Aman et al. 2014). Moderator analyses can help to explain the variation in response to treatment, and may suggest mechanisms of treatment. As psychiatry moves toward a more individualized approach to treatment, and psychiatric research moves toward research domain criteria with identification of biomarkers, the identification of probable responders and nonresponders becomes more important than ever. Although most studies are not designed to evaluate moderators and predictors of response, the post-hoc analysis of such variables is a worthy endeavor that can provide hints for treatment refinement as well as further study (Kraemer et al. 2002). The identification of subgroups or of factors that relate to treatment response inform both clinical and research practice, particularly in contributing to patient selection for future trials. Several studies of ADHD and DBD have identified moderators of response to treatment.
The richest source of moderator analyses pertaining to response to treatments for ADHD has been the Multimodal Treatment Study of Children with Attention-Deficit/Hyperactivity Disorder (MTA Cooperative Group 1999a; for review, see Hinshaw 2007), and many moderator analyses have been performed on psychosocial treatment trials for children with conduct problems (e.g., Lundahl et al. 2006; La Greca et al. 2009). Initial severity of presenting symptoms has mixed evidence as a moderator; ADHD severity was linked to worse outcomes in the MTA study (Owens et al. 2003), but level of child problem behavior at baseline has consistently been related to enhanced psychosocial intervention effectiveness, with a few exceptions. This may be because the MTA, but not usually studies of psychosocial intervention alone, included children with more extreme problem behaviors (Shelleby and Kolko 2013). In children with ADHD, comorbid symptoms, such as anxiety (MTA Cooperative Group 1999b), DBD, and double comorbidity with DBD and anxiety (Jensen et al. 2001) were also found to moderate response to treatment. It is worth noting that although many of the MTA moderator studies conceptualized response dimensionally as amount of improvement from baseline, at least one (Owens et al. 2003) defined response as categorical (responder vs. nonresponder). The categorical approach defines response as normalization, and is therefore more likely to yield an association between lower baseline severity and higher rate of response (as in Owens et al. 2003). The use of a dimensional response variable, on the other hand, tends to result in greater baseline severity being associated with greater response.
Studies other than the MTA have also found evidence for the moderating effect of comorbidity in children with ADHD; Ghuman et al. (2007) reported that children with ADHD and fewer than three comorbid diagnoses responded more favorably to psychostimulant treatment than did children with three or more comorbidities. In a review of the literature, Ollendick et al. (2008) found that comorbidity was reported to be a predictor or moderator of response to several treatment modalities across several internalizing (e.g., mood/anxiety) and externalizing (e.g., ADHD, DBD) childhood disorders. Some demographic characteristics, such as parental education (Rieppi et al. 2002) and ethnicity (Arnold et al. 2003) were also found to moderate response to treatment in the MTA. It is not surprising, then, that at least one study found psychosocial intervention effects on child behavior to be greater in those with higher baseline cumulative risk scores (e.g., measures of conduct problems, parental conflict, negative life events, maternal distress, reduced father contact, financial hardship; Zhou et al. 2008). However, other studies on these parental and family factors have reported nonsignificant moderating effects when comparing psychosocial treatment to control groups in children with conduct problems (Van Zeijl et al. 2006; McTaggart and Sanders 2007; Lavigne et al. 2008; Gardner et al. 2009).
Therefore, there is some inconsistency across studies in the level of moderation reported for both child and parent variables, perhaps influenced by study design (e.g., wait-list control vs. active control condition) and sample characteristics (e.g., severity of initial behavior). An important advance prompted by this literature is to explore other baseline clinical characteristics beyond sociodemographics, to potentially identify subgroups of patients who may show differential response to a combined psychosocial/medication treatment regimen.
The goal of the present analyses was to evaluate potential predictors and moderators of response in the TOSCA study. Based on previous findings in the ADHD and DBD literature summarized, we included several family characteristics (income, education, employment, family functioning) as well as patient-level variables (parent-rated scales of aggression type and comorbid symptoms, IQ, body mass index [BMI]). We hypothesized that high scores on the Reactive Aggression subscale of the Antisocial Behavior Scale (ABS) would be associated with improvement on the D-Total subscale, whereas we expected high scores on the Proactive Aggression subscale to be associated with less improvement (Farmer et al. 2011). This hypothesis was driven by the generally unsubstantiated clinical lore that reactive aggression is more amenable to psychotropic intervention than is proactive aggression (Vitiello and Stoff 1997). Beyond this, we were largely agnostic about which variables might moderate or predict improvement, and analyses should be considered exploratory.
Methods
Participants
The design, assessment, and results of this study are reported in greater detail elsewhere (Farmer et al. 2011; Aman et al. 2014;). Informed consent was obtained from the legal guardian of the child, and assent was obtained from the child prior to study participation. Participants were 168 children, 129 male (77%), with a mean age of 8.89±2.01 years. In addition to significant physical or property aggression, participants were required to have ADHD and average IQ (mean±SD=97.1±14.1), and ODD (n=124, 74%) or CD (n=44, 26%).
Study design
This study was 3 weeks of open-label STIM and PT followed by 6 weeks of a double-blind, placebo controlled comparison of added risperidone (augmented treatment) versus placebo (basic treatment). Children were randomized at baseline to receive either risperidone (n=84) or placebo (n=84) in addition to STIM (n=84) if response to STIM and PT was not optimal at the end of 3 weeks. Both clinicians and participants were unaware of treatment assignment. All medications were titrated according to a weight-based schedule, adjusted for clinical response or adverse events (AEs).
Measures
Outcomes
The primary outcome measure in the study was the NCBRF Typical IQ version (Aman et al. 2008) Disruptive Total Score (D-Total). The NCBRF is a parent-report measure with excellent psychometric properties and demonstrated sensitivity to drug effects. Five problem subscales plus a Positive Social subscale result from this instrument; the current analyses used the D-Total (sum of Oppositional Behavior and Conduct Problem; range 0–64), ADHD Total (sum of Hyperactive and Inattentive; range 0–30), and the Positive Social (range 0–30) subscales as outcomes. The Positive Social subscale is a mix of prosocial actions (e.g., “Shared with or helped others”), compliance-related behaviors (e.g., “Accepted redirection”), and other miscellaneous behaviors shown by factor analysis to be related to the construct (e.g., “Expressed ideas clearly”). D-Total scores >12 are considered high (mean±SD in the normative sample, n=471, was 10.09±11.44); a score >27 (90th percentile) was required for study entry. The mean normative score on the ADHD Total subscale was 6.82±7.06 (n=479), and the mean normative score for the Positive Social subscale was 19.96±6.28 (n=485) (Aman et al. 2008).
Putative predictors and moderators
Potential predictors and moderators were drawn from several parent- and clinician-completed instruments gathered at screening and baseline. To confirm study eligibility, IQ was assessed at screen using the Kaufmann Brief Intelligence Test, 2nd ed. (Kaufman and Kaufman 2004). An adapted version of the Overt Aggression Scale-Modified (Coccaro et al. 1991) was used at screening and baseline to confirm the degree of aggression required for study eligibility. The version used in this study omitted the Verbal Aggression question, which was not relevant to the eligibility criteria, and required actual physical violence to a person or property. Therefore, three unweighted items were retained: Aggression toward objects, others, and self. Clinicians selected one rating on a 0 (no event) to 5 (severe events) point scale, based on parent and child report. A score of at least 3 on at least one item was required for study entry (see Gadow et al. 2014).
The Child Adolescent Symptom Inventory-4 Revised (CASI-4R, Gadow and Sprafkin 2005) was completed by parents, and reflects symptom severity in several domains of psychopathology. The mean item scores (range 0–3) from the following subscales were used in the current study: Generalized Anxiety, Separation Anxiety, Anxiety Composite, Schizophrenia Spectrum Disorder, Major Depressive Episode (Depression), Manic Episode (Mania), Pervasive Developmental Disorder, ADHD, ODD (Anger and Irritability Symptoms [AIS] comprises three items of this subscale, “loses temper,” “is angry and resentful,” and “is touchy or easily annoyed by others”), CD, and the Peer Conflict Scale. The CASI-4R items correspond to the Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision (DSM-IV-TR) criteria for each disorder; for example, the Mania subscale queries whether the child is more cheerful, irritable, active, talkative, distractible, and/or reckless than usual, in addition to whether the child needs less sleep than usual and believes that (s)he has special abilities (American Psychiatric Association 2000).
The MacMaster Family Assessment Device (FAD) (Epstein et al. 1983) was used to evaluate family conflict. The version used in this study has three parent-rated subscales, in which higher scores on a scale of 1–4 indicate greater conflict: Problem Solving (six items), Communication (nine items), and General Functioning (12 items). Proactive (10 items) and reactive (6 items) aggression behaviors were rated on a scale of 1–3 by parents on the ABS (Brown et al. 1996). The Proactive Aggression subscale comprised items tapping planned and instrumental aggression (e.g., “picks on kids,” “does sneaky things,” “gets others to gang up”). The Reactive Aggression items reflect behaviors that occur in response to provocation (e.g., “mad when corrected,” “blames others,” “poor loser”). Although the ABS is traditionally used for teacher ratings, confirmatory factor analysis of the parent-rated data collected in this study indicated acceptable fit, supporting the construct validity of the instrument with parent reporters (Kaat et al., 2014).
An ad hoc callous/unemotional (C/U) composite variable was created using relevant items from the NCBRF (cruelty or meanness to others; does not feel guilty), CASI-4R (physically cruel; does not care about causing pain/suffering; physically cruel to animals; emotionally cold; no interest in others' feelings), and the Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime (Kaufman et al. 1997) (physically cruel; cruel to animals). Items were selected based on item content that reflected planned and/or intentional aggression without apparent remorse or concern for others. We explored the usefulness of three different composites, but they rendered essentially the same results for all comparisons. Therefore, only one C/U composite is presented.
Analyses
Putative moderators were first entered into a Spearman correlation matrix to evaluate collinearity. The threshold was set at r=0.7; one member of any pair with a correlation >0.7 was excluded. The MacArthur guidelines for prediction and moderation (Kraemer et al. 2002, 2008) were used, requiring the potential moderator's temporal precedence and independence from treatment assignment. All potential predictors and moderators were baseline characteristics, and, therefore, satisfied these criteria.
The variables were median centered and square-root transformed as appropriate, and then entered into a linear mixed model that slightly altered from the original constrained longitudinal data analysis (cLDA) model described by Aman et al. (2014). The cLDA model assumed that treatment groups did not differ at baseline; therefore, they were modeled as one. With the addition of the putative moderator into the model, we were no longer able to make this assumption. Therefore, we instead employed the same linear mixed model for repeated measures (unstructured covariance matrix), with fixed effects for time, group, and time-by-group interaction, but analyzed only postbaseline data while controlling for the baseline level of the dependent variable. Stratification/balance factors (site and disorder) were also entered as fixed effects, as in the original analyses. The primary outcome was NCBRF D-Total (square-root transformed, as in the primary analysis); secondary outcomes were the NCBRF ADHD Total and Positive Social subscale.
Predictors were variables that exerted an effect over time (significant moderator by visit interaction) on outcome that did not differ by treatment group. Moderation was indicated by a significant three-way interaction of time, treatment, and moderator. Because lower-order terms are difficult to interpret in the presence of a significant higher-order term, variables with both significant predictor and moderator terms were considered only as moderators.
In order to visually examine and interpret significant prediction and moderation, analyses were rerun with the moderator held constant at high (∼85th percentile) and low (∼15th percentile) values (Farmer 2012). This allowed for all data to be used without dichotomization. Figures show the treatment by time interaction at the high and low levels of the moderator. Except for one hypothesized effect (reactive versus proactive aggression), all analyses were exploratory and, therefore, no correction was made for multiple comparisons (two tailed α=0.05). SAS Version 9.3 was used for all analyses.
Results
Several variables were excluded because of collinearity (Table 1): FAD Communication, CASI-4R Generalized Anxiety Disorder (GAD) and Schizophrenia Spectrum, CASI-4R CD, and CASI-4R ODD (respectively, the retained member of the pairs were FAD General Functioning, CASI-4R Anxiety Composite, C/U Composite, and CASI-4R AIS). The results of the linear mixed models with the remaining variables are presented in Table 2. Significant predictors and moderators are summarized in Table 3.
Table 1.
Significant (p<0.05) Spearman Correlations Among Continuous Putative Moderators
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ABS | |||||||||||||||||||||
| 1.Proactive | 0.43 | 0.75 | 0.55 | 0.38 | 0.29 | 0.38 | 0.17 | 0.16 | 0.31 | 0.40 | 0.56 | 0.64 | 0.43 | 0.68 | |||||||
| 2.Reactive | −0.18 | 0.40 | 0.17 | 0.39 | 0.33 | 0.39 | 0.20 | 0.26 | 0.35 | 0.56 | 0.33 | 0.55 | 0.3 | ||||||||
| 3.Pro:Rea Ratio | 0.34 | 0.16 | 0.19 | 0.22 | 0.45 | 0.56 | |||||||||||||||
| 4.C/U Composite | 0.25 | 0.41 | 0.39 | 0.41 | 0.27 | 0.23 | 0.57 | 0.37 | 0.51 | 0.75 | 0.42 | 0.57 | |||||||||
| 5.OAS Total | 0.19 | 0.22 | 0.17 | 0.16 | 0.2 | 0.27 | 0.21 | 0.27 | |||||||||||||
| FAD | |||||||||||||||||||||
| 6.Prob.Solv. | 0.55 | 0.64 | |||||||||||||||||||
| 7.Comm. | 0.72 | −0.20 | −0.16 | −0.18 | |||||||||||||||||
| 8.Gen. Func. | −0.17 | ||||||||||||||||||||
| CASI-4R | |||||||||||||||||||||
| 9.GAD | 0.30 | 0.86 | 1.0 | 0.46 | 0.21 | 0.41 | 0.47 | 0.42 | 0.4 | 0.42 | 0.34 | ||||||||||
| 10.Sep. Anx. | 0.48 | 0.30 | 0.44 | 0.32 | 0.28 | −0.17 | |||||||||||||||
| 11.Anx. Comp. | 0.86 | 0.56 | 0.35 | 0.55 | 0.36 | 0.28 | 0.36 | 0.28 | 0.29 | ||||||||||||
| 12.Schizo. | 0.46 | 0.21 | 0.41 | 0.47 | 0.42 | 0.40 | 0.42 | 0.34 | |||||||||||||
| 13.Dep. | 0.45 | 0.48 | 0.24 | 0.26 | 0.29 | 0.30 | 0.21 | 0.19 | −0.18 | ||||||||||||
| 14.Mania | 0.52 | 0.33 | 0.25 | 0.24 | −0.30 | ||||||||||||||||
| 15.PDD | 0.36 | 0.26 | 0.46 | 0.22 | 0.32 | −0.21 | |||||||||||||||
| 16.ADHD | 0.45 | 0.32 | 0.36 | 0.30 | |||||||||||||||||
| 17.ODD | 0.53 | 0.92 | 0.63 | ||||||||||||||||||
| 18.CD | 0.41 | 0.69 | |||||||||||||||||||
| 19.AIS | 0.53 | ||||||||||||||||||||
| 20.Peer Conflict | |||||||||||||||||||||
| 21.BMI | |||||||||||||||||||||
| 22.IQ | |||||||||||||||||||||
Correlations above the a priori are bolded.
ABS, Antisocial Behavior Scale; Pro:Rea Ratio, ratio of proactive score to reactive score; C/U, callous/unemotional; OAS, Overt Aggression Scale; FAD, Family Assessment Device; CASI-4R, Child and Adolescent Symptom Inventory-4R; PDD, pervasive developmental disorder; ADHD, attention-deficit/hyperactivity disorder; AIS, anger irritability symptoms; BMI, body mass index; IQ, intelligence quotient.
Table 2.
Results of Linear Mixed Models Analysis for Prediction and for Moderation of NCBRF D-Total, ADHD-Total, and Positive Social Subscale
| Predictor, F(p) | Moderator, F(p) | |||||
|---|---|---|---|---|---|---|
| D-Total | ADHD-Total | Positive Social | D-Total | ADHD-Total | Positive Social | |
| ABS Proactive | 1.83(0.10) | 1.19(0.32) | 1.29(0.26) | 0.78(0.59) | 2.18(0.047) | 1.04(0.40) |
| ABS Reactivea | 0.95(0.46) | 0.66(0.68) | 0.85(0.53) | 0.87(0.52) | 0.55(0.77) | 2.08(0.06) |
| C/U Composite | 3.17(0.01)b | 1.37(0.23) | 1.78(0.11) | 1.20(0.31) | 1.10(0.36) | 1.33(0.25) |
| OAS Total Score | 0.96(0.45) | 1.19(0.31) | 0.43(0.86) | 0.56(0.76) | 0.86(0.53) | 1.57(0.16) |
| FAD Problem Solving | 1.16(0.33) | 0.60(0.73) | 1.12(0.35) | 0.64(0.70) | 0.41(0.87) | 0.68(0.67) |
| FAD General Function | 0.22(0.97) | 0.16(0.99) | 1.89(0.09) | 1.56(0.16) | 0.62(0.72) | 0.89(0.50) |
| CASI-4R Subscales | ||||||
| Depressiona | 1.75(0.11) | 1.08(0.38) | 0.38(0.89) | 0.91(0.49) | 1.02(0.41) | 0.97(0.45) |
| Maniaa | 0.76(0.60) | 1.34(0.24) | 0.66(0.68) | 2.29(0.04) | 1.77(0.11) | 0.52(0.79) |
| PDDa | 0.67(0.68) | 0.20(0.98) | 0.34(0.92) | 0.85(0.53) | 0.56(0.76) | 0.21(0.97) |
| ADHDa | 3.00(0.01)b | 1.84(0.09) | 1.43(0.21) | 0.91(0.49) | 0.64(0.70) | 2.93(0.01) |
| Anxiety Compositea | 1.53(0.17) | 0.48(0.83) | 1.37(0.23) | 0.83(0.55) | 0.55(0.77) | 0.52(0.79) |
| Separation Anxietya | 0.74(0.62) | 0.92(0.49) | 1.40(0.22) | 0.45(0.84) | 0.89(0.51) | 0.82(0.55) |
| AISa | 3.38(0.004) | 1.59(0.15) | 2.72(0.02) | 2.98(0.01) | 2.01(0.07) | 2.58(0.02) |
| Peer Conflict Scalea | 1.20(0.31) | 0.56(0.76) | 0.62(0.72) | 0.92(0.48) | 0.75(0.61) | 0.9(0.50) |
| BMIa | 1.87(0.09) | 0.92(0.48) | 0.66(0.68) | 1.26(0.28) | 1.50(0.18) | 0.97(0.45) |
| IQa | 0.23(0.97) | 0.49(0.82) | 1.10(0.37) | 0.58(0.75) | 1.38(0.23) | 0.97(0.45) |
| Maternal Employmentc | 1.08(0.38) | 0.50(0.81) | 1.77(0.11) | 0.98(0.44) | 0.53(0.78) | 0.95(0.46) |
| Maternal Educationd | 0.40(0.88) | 1.85(0.09) | 1.36(0.23) | 1.65(0.14) | 1.28(0.27) | 3.28(0.004) |
| Household Incomee | 1.00(0.43) | 0.71(0.64) | 1.25(0.28) | 0.46(0.84) | 0.44(0.85) | 0.60(0.73) |
Results of a linear mixed model that includes fixed effects for stratification factors (disorder and site), as well as the baseline value of the outcome as a covariate. DF are (6, 149). Predictor refers to variable×time term; Moderator refers to the variable×treatment×time term. A statistically significant predictor term in a model where there was also a significant moderator term was not considered. Triple interactions are illustrated in Figures 2 and 3.
Statistically Significant effects are bolded.
Variable was square-root transformed for analysis.
Higher values of predictor are associated with more and faster improvement, regardless of treatment assignment. See Figure 1.
Not employed versus employed full or part time.
High school diploma or less versus some college or more.
≤$40,000 or less versus >$40,000.
ABS, Antisocial Behavior Scale; C/U, callous/unemotional; OAS, Overt Aggression Scale; FAD, Family Assessment Device; CASI-4R, Child and Adolescent Symptom Inventory-4R; PDD, pervasive developmental disorder; ADHD, attention-deficit/hyperactivity disorder; AIS, anger irritability symptoms; BMI, body mass index; IQ, intelligence quotient.
Table 3.
Narrative Description of Significant Predictor and Moderator Effects
| Predictor/Moderator | Effect | Outcome | Description |
|---|---|---|---|
| CASI ADHD | Predictor | D-Total | Subjects with higher ADHD score showed more and faster improvements, regardless of treatment assignment. |
| Callous/Unemotionala | Predictor | D-Total | Subjects with higher Callous/Unemotional scores showed more and faster improvements, regardless of treatment assignment. |
| CASI-4R Anger Irritability Symptoms | Moderator | D-Total | Early on, the advantage of augmented treatment was greater for children with high AIS scores, but this effect was diminished before 9 weeks. Essentially, the augmentation effect was faster for those with high baseline AIS scores. |
| CASI-4R Mania | Moderator | D-Total | Early on, the effect of augmented treatment was greater for children with low Mania scores, but this effect was diminished before 9 weeks. Essentially, the augmentation effect was faster for those with low baseline Mania scores. |
| ABS Proactive Aggression | Moderator | ADHD Total | Early on, the effect of augmented treatment was greater for children with high Proactive Aggression scores, but this effect was diminished before 9 weeks. Essentially, the augmentation effect was faster for those with high proactive aggression scores. |
| CASI ADHD | Moderator | Positive Social | Early on, the effect of augmented treatment was greater for children with high CASI ADHD scores, but this effect was diminished before 9 weeks, by which time those with lower baseline ADHD scores showed greater advantage of augmented treatment. |
| CASI Anger Irritability Symptoms | Moderator | Positive Social | Early on, the effect of augmented treatment was greater for children with high AIS scores, but midway through the trial, the effect of augmented treatment became greater for children with low AIS scores. |
| Maternal education | Moderator | Positive Social | Within the basic treatment group, children of mothers with less education (high school or less) did worse, but there was no relationship between maternal education and outcome within the augmented treatment group. Therefore, the effect of augmented treatment was greater for children of mothers with less education. |
Callous/Unemotional Score was a composite of items selected by authors to reflect lack of remorse when behaving antisocially (scoring algorithm available on request).
CASI-4R, Child and Adolescent Symptom Inventory; ADHD, attention-deficit/hyperactivity disorder; ABS, Antisocial Behavior Scale.
Predictors
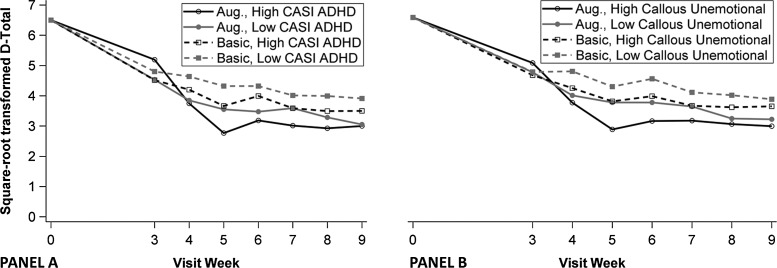
Two variables were predictors of outcome on the primary outcome measure, NCBRF D-Total (Table 2). In both cases, higher scores on the baseline variables (C/U Composite and CASI-4R ADHD) were associated with more and faster improvement in both treatment groups (Fig. 1). The predictor term for the CASI-4R AIS subscale was statistically significant for both D-Total and NCBRF Positive Social; however, AIS was also a moderator of these outcomes and was, therefore, not considered a nonspecific predictor. No other variable was a nonspecific predictor of any outcome.
FIG. 1.
Baseline Child Adolescent Symptom Inventory (CASI) Attention-Deficit/Hyperactivity Disorder (ADHD) Scores (A) and Callous/Unemotional Scores (B) predict Nisonger Child Behavior Rating Form Disruptive Total (NCBRF DTotal). Regardless of treatment assignment, high levels of CASI-4R ADHD and Callous/Unemotional Composite Scores at baseline were associated with more and faster improvement on the primary outcome measure, NCBRF D-Total. Lower scores indicate better behavior.
Moderators
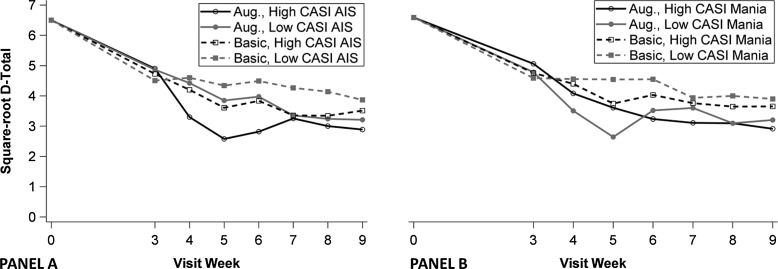
Two CASI-4R variables moderated outcome on NCBRF D-Total (Table 2). Whereas high scores on CASI-4R AIS were associated with better outcome in both the basic and augmented groups (evidenced by the significant predictor term in Table 2), this difference was greater for augmented than for basic for the first several weeks of combined pharmacologic treatment (Fig. 2, panel A). Stated another way, the treatment effect in favor of augmented was stronger for children with high baseline AIS than for children with low AIS. However, this difference was reversed by week 7 such that the effect of treatment was greater for children with low baseline AIS, although evidence of moderation in any direction was scant at endpoint. A similar type of moderated effect was observed with low CASI-4R Mania scores (Fig. 2, panel B). The difference between basic and augmented treatment was greater for children with low Mania scores than for children with high Mania scores until Week 6 or thereabouts, when the difference diminished.
FIG. 2.
Moderating effects of baseline Anger and Irritability Symptoms (AIS) Scores (A) and Mania Scores (B) on primary outcome (Nisonger Child Behavior Rating Form Disruptive Total [NCBRF D-Total]). The effect of treatment at high (black lines) and low (gray lines) values of the moderator are illustrated in the difference between the like-colored solid and dotted lines. A shows that higher baseline Child and Adolescent Symptom Inventory-4R (CASI) AIS Scores were associated with a greater effect of augmented treatment on the primary outcome (NCBRF D-Total) until Week 7 thereabouts, when children with lower baseline CASI AIS Scores demonstrated a greater effect of augmented relative to basic treatment. B shows a greater effect of augmented treatment associated with low baseline CASI Mania Scores up to Week 6, at which point the moderating effect of the Mania Score was diminished or disappeared. Lower scores indicate better behavior.
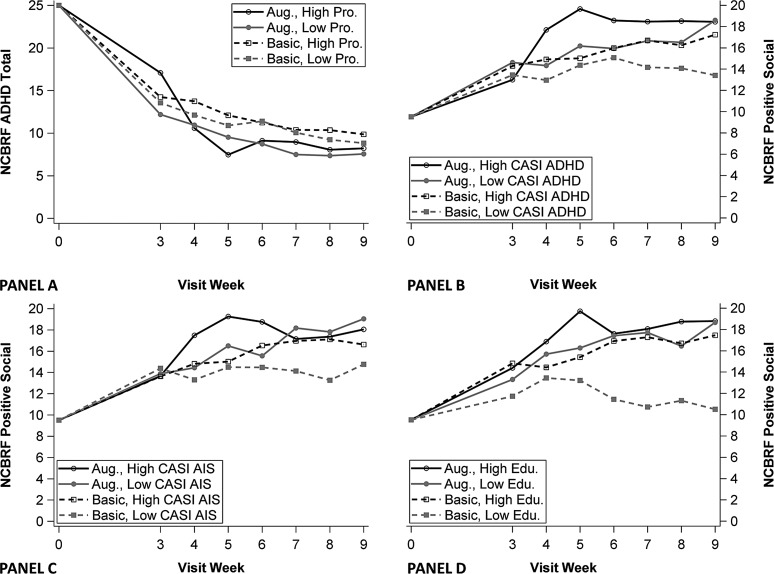
One moderator of NCBRF ADHD-Total was observed (Fig. 3, panel A). Within the basic group, children with high and low scores on the ABS Proactive Aggression subscale responded similarly to the first 3 weeks of treatment (STIM+PT). Within the augmented group, children with low Proactive scores responded better to STIM+PT, as demonstrated by a mean difference of approximately six points at Week 3. This finding has no implications for the effect of augmented treatment, as risperidone had not yet been added. After risperidone was introduced (end of Week 3) until Week 6, the treatment effect in favor of augmented was stronger for children with high Proactive scores than for those with low Proactive scores. After Week 6, there was no appreciable effect of the moderator.
FIG. 3.
Moderating effects of Antisocial Behavior Scale (ABS) Proactive Aggression score on Attention-Deficit/Hyperactivity Disorder (ADHD) Total (A), Child and Adolescent Symptom Inventory (CASI) ADHD Score on Positive Social Score (B), Anger and Irritability Symptoms (AIS) Scores on Positive Social Score (C), and maternal education on Positive Social Score (D). The effect of treatment within high (black lines) and low (gray lines) values of the moderator are illustrated in the difference between the like-colored solid and dotted lines. A illustrates the moderating effect of ABS Proactive Aggression ratings on the secondary outcome Nisonger Child Behavior Rating Form (NCBRF) ADHD Total (lower scores indicate better behavior). High Proactive Scores were associated with a greater effect of augmented treatment until Week 6, at which point the moderated effect diminished. B–D illustrate moderated effects on a different secondary outcome, NCBRF Positive Social Score (higher scores indicate better behavior). B and C show that higher baseline CASI ADHD and Anger AIS Scores, respectively, were associated with greater effects of augmented treatment on the Positive Social Score until Week 6 or thereabouts, when the moderator effect diminished (ADHD) or shifted in favor of lower baseline values (AIS). D illustrates that low maternal education (high school diploma or less) was associated with a greater effect of augmented treatment than was higher maternal education (some college or more). This is alternatively stated as a greater effect of basic treatment in families with high maternal education than in those with low maternal education, which was neutralized by the addition of risperidone.
Change in NCBRF Positive Social score was moderated by CASI-4R AIS (Fig. 3, panel C). Again, the moderated effect was inconsistent over time. The advantage of augmented treatment was greater for children with high levels of AIS early on, but the treatment effect was greater for children with low AIS by Week 7 through the end of the trial. Another CASI-4R subscale, ADHD, moderated response on Positive Social in a similar way (Fig. 3, panel B). Two patterns emerged; during the early part of the trial, high ADHD scores at baseline were associated with greater response to augmented treatment (the difference between augmented and basic was greater for those with high baseline ADHD scores than for those with low ADHD scores). However, starting at Week 6 or thereabouts, a greater advantage of augmented treatment emerged for children with low CASI-4R ADHD scores at baseline. At endpoint, a larger effect of treatment (augmented vs. basic) was observed in children with low baseline ADHD scores than in children with high ADHD scores.
Finally, maternal education was also a significant moderator of outcome on the NCBRF Positive Social score. Low maternal education (high school degree or less) was associated with a greater effect of augmented treatment, compared with children of mothers with at least some college coursework (Fig. 3, panel D). Stated another way, children in the basic group whose mothers had more education had outcomes very similar to those observed in the augmented group (where maternal education had no effect on NCBRF Positive Social score). The results of the study are summarized in Table 3.
Discussion
Although the details varied, one pervasive trend emerged, in which greater baseline severity/adversity was associated with better treatment response, either in general or in advantage of augmentation. Two predictors—higher C/U symptoms and higher ADHD symptoms—forecast better D-Total outcome irrespective of whether risperidone adjunctive treatment was employed. In contrast, more baseline AIS and fewer baseline manic symptoms predicted faster response to augmented, but not to basic, treatment (moderation). Higher baseline severity was also associated with better/faster response to augmented treatment on the secondary outcomes; more proactively aggressive children responded faster on the secondary ADHD outcome, and children with more anger/irritability or ADHD symptoms responded faster to augmented treatment on the secondary Positive Social outcome. Finally, children of mothers with less education benefited differentially from augmented treatment. Had they received basic treatment, they likely would have fared worse on the Positive Social outcomes score than the children of mothers with more education. However, the introduction of augmented treatment resulted in no difference between children of mothers with more or less education. Finally, contrary to our hypothesis (and contrary to much conjecture in the literature), we did not find evidence for an effect of reactive aggression scores on augmented D-Total scores. We consider each of these findings in turn.
Predictors
Higher CASI-4R ADHD subscale scores were associated with more rapid improvement on the primary outcome (D-Total) regardless of treatment assignment. All participants were diagnosed with ADHD and all participants received psychostimulant treatment. The observation that patients with greater degrees of ADHD symptoms improve more rapidly on a related symptom domain than those with less severe symptoms is consistent with the phenomenon of “rate dependency” (Branch 1984; Teicher et al. 2003). The phenomenon of rate dependency, in which children with more severe ADHD experience faster improvement in ADHD symptoms with methylphenidate (Teicher et al. 2003), appears to have been replicated here in an associated symptom domain (i.e., disruptive behavior and aggression). Rate dependency would have been more clearly demonstrated if the ADHD outcome had been implicated, but the prediction effect was only at the trend level (p=0.09). A similar finding appeared with C/U traits, which also predicted better D-Total response for both treatment groups. These data contribute to a mixed literature surrounding the treatment resistance of children with C/U traits, at least to behavioral intervention (e.g., Kolko and Pardini 2010; Haas et al. 2011). However, it is important to note that the C/U composite used in this article was not a validated measure, and future research should employ existing measures such as the Antisocial Process Screening Device (Frick and Hare 2001). These two variables, coupled with aggression, captured the most prominent presenting symptoms of this clinically referred sample. Therefore, children with especially severe symptoms may present greater opportunity for improvement with either type of evidence-based treatment (i.e., STIM+PT, or their combination with risperidone).
Moderators
Primary outcome
The significant moderator effects on the primary outcome, NCBRF D-Total, suggested that children with higher baseline AIS and lower baseline Mania scores responded faster to augmented treatment, although these advantages were not sustained over 9 weeks. These findings may be clinically useful, in that the combined treatment may be especially helpful in providing faster relief for children significantly impaired by anger and irritability. Symptoms of anger and irritability map closely onto the recruitment criteria, which may suggest that clinical severity may dispose the best response to added risperidone. These results contribute to the body of literature on differential outcomes associated with clusters of ODD symptoms (e.g., Stringaris and Goodman 2009; Drabick and Gadow 2012). The results of this study may be of particular importance to those studying the new Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-V) diagnosis of Disruptive Mood Dysregulation Disorder, which is characterized by a persistently irritable and angry mood (American Psychiatric Association 2013).
With regard to manic episode symptoms, it warrants repeating that a Kiddie-SADS current diagnosis of bipolar disorder was a TOSCA exclusion criterion. In other words, unlike ADHD and physical aggression, participants were not selected for extreme levels of these symptoms. Given that atypical antipsychotics are currently among the drugs of first choice for the clinical management of pediatric bipolar disorder (McClellan et al. 2007), it seems counterintuitive that children with relatively high Mania scores responded more slowly to augmentation than did children with low Mania scores. At least two other studies of children with ADHD found few or no differences at endpoint in response to STIM plus behavioral treatment between children with manic symptoms and those without (Galanter et al. 2003; Waxmonsky et al. 2008), consistent with our findings in the basic group. It may be that children with high levels of manic symptoms are more impaired by other symptoms, as was found in one long-term study of children with elevated symptoms of mania (Findling et al. 2010). Regardless, elevated manic symptoms may be a clinical marker for persistence of disruptive behavior in the early stages of augmented therapy.
Secondary outcomes
Figure 3, Panel A illustrates a moderating effect of ABS Proactive Aggression ratings on the secondary outcome NCBRF ADHD Total. High proactive aggression, or aggression that is driven by instrumental gain or social dominance (Dodge and Coie 1987), was associated with a greater effect of augmented treatment from end of Week 3 through Week 6, at which point the moderated effect diminished. Importantly, Figure 3 also suggested some resistance to the effect of stimulant in children with that type of aggression (end of Week 3). Therefore, the effect may be refractoriness to stimulant therapy, which was then overcome by adjunctive risperidone. In any case, the sole effect ascribed to proactive aggression was on a variable other than disruptive behavior. No explanation for this association with ADHD Total score comes to mind unless we conceptualize ADHD as a proxy for disruptive behavior, which we do not find compelling, even though ADHD was once classified as a DBD.
Stronger symptoms of ADHD and anger/irritability, as measured by the CASI-4R, were both associated with faster initial response to augmented treatment on the prosocial behaviors measured by the NCBRF Positive Social subscale. Ultimately, however, children with less severe baseline ADHD and AIS demonstrated a greater advantage of augmentation on these positive behaviors. The initial advantage to children with higher levels of these symptoms is consistent with our findings that greater ADHD symptoms predicted response to both treatments and greater AIS moderated the effect of augmented treatment. However, in both moderators of prosocial behavior, we observed a reversal of the pattern, showing an advantage of lower ADHD and anger/irritability scores by endpoint. Although these findings appear to be at odds, it is worth consideration that improvements on NCBRF Positive Social subscale constitute the development of positive behaviors, not just elimination of negative behaviors, which is one way of describing improvements in NCBRF D-Total. Therefore, it stands to reason that children with more severe overall behaviors may exhibit better response to treatment when the metric is reduction of bad behavior, whereas children with less severe overall behavior may be more able to develop new prosocial behaviors over the longer term. Another possibility is that children with more severe disruptive behavior symptoms at baseline may be likely to experience impairments in positive social behaviors as a result of the disruptive behaviors, whereas the impairment in positive social behaviors may have been unrelated to disruptive behaviors in those with lower initial ADHD and AIS (baseline Positive Social scores were moderately and negatively correlated with baseline D-Total scores). The impairments in positive social behaviors in the latter group may be less responsive to the ongoing parent training intervention. Finally, it is worth noting that the Positive Social subscale of the NCBRF does have several compliance-related items and may, therefore, not reflect prosocial behaviors as they may be perceived by teachers or peers.
Both reactive and proactive aggression, as measured by the ABS, failed to moderate outcome, even though it was our sole directional hypothesis for this study. It is possible that the CASI-4R Anger Irritability Symptoms subscale does a better job of capturing “hot,” reactive, unplanned hostility than “reactive aggression,” despite the names that were originally assigned to these subscales. It is also possible that the lack of variation in reactive aggression may have impaired our ability to demonstrate an effect. Perhaps unsurprisingly in this sample of children with severe aggression and ADHD, ABS Reactive Aggression scores were generally in the maximum range (ABS Proactive Aggression scores, on the other hand, were more normally distributed). However, these data do not support the clinical lore that children with reactive aggression are more amenable to psychotropic intervention than are those with primarily proactive aggression (Vitiello and Stoff 1997), and further research is needed. Without supportive data, perhaps this theory needs reevaluation.
The final moderator effect concerning Positive Social outcomes was maternal education. Within those who received augmented treatment, children of both less- and more-educated mothers did equally well. However, for those who received only STIM and PT, the children of more-educated mothers did much better than children of less-educated mothers. Hence, augmented treatment made an “equal playing field” for parents with lower education, who for many reasons may be less able than higher-educated parents to successfully implement the lessons of PT. One might also interpret this finding as an endorsement for the efficacy of PT on prosocial behaviors in this subgroup; high maternal education was able to offset any disadvantage on Positive Social outcomes of not receiving augmentation. This also underscores the importance of efforts to enhance the efficacy of psychosocial treatments in families with low maternal education (e.g., Chacko et al. 2009). Importantly, this effect of maternal education appeared to be ongoing at the end of the 9 week trial. The maternal education result is compatible with the MTA results reported by Rieppi et al. (2002), who found that children in high-education but not low-education families responded better to combined treatment versus medication management alone (in the absence of an antipsychotic). Therefore, the finding presented here appears to be robust.
Overall, we are encouraged by the fact that the identified moderators of primary and secondary outcomes did not generally sustain impact through the end of the trial. The treatment literature in the disruptive behavior disorder arena has shown that certain variables moderate behavioral treatment effectiveness in some studies, but not others (Lundahl et al. 2006). These findings suggest that at least within this clinical group of children, our recently published findings of more efficacious augmented treatment for childhood aggression versus STIM plus PT alone (Aman et al. 2014) largely applies across the sample. One speculation regarding the absence of effects may rest with the stringent clinical threshold required for study entry, which may have homogenized the group, compared with the diversity of patients who present for clinical care. For example, in the MTA, only 15% of the sample met diagnostic criteria for CD at baseline (MTA Cooperative Group, 1999), compared with 26% in the current study.
Limitations
The results of this study must be interpreted in the context of several potential limitations. The measure of C/U behaviors was created on an ad-hoc basis for the express purpose of this study, and has not been validated. Although the ABS is a validated measure, the TOSCA study is the first to use it as a parent-report measure. Our preliminary psychometric report on the instrument indicates good construct validity (Kaat et al., 2014), but more research is needed. As with most moderator analyses of clinical trials, this study was not powered for tests of moderation and was significantly smaller than other studies that have reported moderation effects (e.g., MTA, n=579). In this exploratory study, we did not correct for multiple comparisons; therefore, it is important to consider that the few significant findings could potentially be attributed to type 1 error.
Conclusions
The results, summarized in Table 3, indicate the following: More severe ADHD and C/U symptoms are related to better treatment effect with both basic and augmented treatment. Children with higher anger and irritability scores and those with fewer symptoms of mania responded faster to augmentation. Higher Proactive Aggression scores forecast better initial responses to augmented treatment on ADHD-Total. Children with high ADHD scores and high anger and irritability scores had better initial responses to augmented treatment on the prosocial outcome. Finally, augmented treatment ameliorated the deleterious impact of low maternal education on prosocial outcomes. As do all post-hoc moderator analyses, these results require validation in future investigations. However, at this point, these results may point to more expeditious treatment depending upon the profile of the child. If these findings are validated in the future, clinicians in the field will need to equip themselves with appropriate scales for assessing initial and outcome behavior.
Clinical Significance
The value of moderator analyses is to facilitate matching treatment to patient, making treatment more personalized and effective. Clinicians use moderators of treatment in calculating the risk:benefit ratio of a particular course of treatment for a particular individual; the likelihood of response may sway the decision one way or the other. The limited number of moderators in this report is two edged: Disappointing in not finding more markers predicting good response, but heartening in the realization that the augmentation strategy in the study benefits a wide range of clinical and demographic profiles within the sampling definition. Clinicians can have confidence that risperidone augmentation of STIM and PT will show a moderate benefit for a range of outcomes in aggressive children with DBD and ADHD. However, this benefit must be weighed against the side effects associated with risperidone (especially weight gain and, sometimes, neurological issues) (McKinney and Renk 2011).
The moderators that we found were generally time limited; therefore, it is possible that that these moderators will not dramatically impact the clinical decision-making process. The moderators suggest that the added benefit may come more quickly to those with high anger/irritability and without manic symptoms. Conversely, those with low anger/irritability and/or high manic symptoms may require more patience to achieve full benefit. Similarly, the positive social benefit of augmentation comes faster in the presence of high anger/irritability and ADHD symptoms, and the absence of these requires more clinical patience for full benefits. Maternal education has a more persistent moderating effect and should be noted in treatment planning. It appears that more maternal education may improve the ultimate response to STIM and PT sufficiently to make risperidone unnecessary. Conversely, the addition of risperidone eliminated the deleterious effect of low maternal education on positive social outcomes.
Disclosures
Dr. Aman has received research contracts, consulted with, or served on advisory boards of Biomarin Pharmaceuticals, Bristol-Myers Squibb, Cog State, Confluence Pharmaceutica, Coronado Biosciences, Forest Research, Hoffman LaRoche, Johnson and Johnson, MedAvante Inc., Novartis, Pfizer, ProPhase LLC, and Supernus Pharmaceuticals. Dr. Gadow is a shareholder in Checkmate Plus, publisher of the Child and Adolescent Symptom Inventory-4R. Dr. Bukstein has received royalties from Routledge Press and acted as a consultant for Ezra Innovations and PRIME CME. Dr. Arnold has received research funding from Curemark, Forest, Lilly, Neuropharm, Novartis, Noven, Shire (as well as NIH and Autism Speaks) and has consulted or been on advisory boards for Gowlings, Neuropharm, Novartis, Noven, Organon, Pfizer, Roche, Seaside Therapeutics, Shire, and Tris Pharma. Dr. McNamara has received research support from Forest Research, GlaxoSmithKline, Eli Lilly and Co., Lundbeck, Merck, the NIH, Novartis, Otsuka, Pfizer, Rhodes Pharmaceuticals, Roche, Shire, Stanley Medical Research Institute, Sunovion, and Supernus Pharmaceuticals. Dr. Rundberg-Rivera has received research support from Covance/Otsuka, GlaxoSmithKline, Merck/Schering Plough, the NIMH, and Pfizer. Dr. Bangalore has received research support from Supernus Pharmaceuticals. Dr. Findling receives or has received research support from, or acted as a consultant and/or served on a speaker's bureau for Alexza Pharmaceuticals, American Academy of Child & Adolescent Psychiatry, American Physician Institute, American Psychiatric Press, AstraZeneca, Bracket, Bristol-Myers Squibb, Clinsys, CogCubed, Cognition Group, Coronado Biosciences, Dana Foundation, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press, Johnson & Johnson, KemPharm, Lilly, Lundbeck, Merck, NIH, Novartis, Noven, Otsuka, Oxford University Press, Pfizer, Physicians Postgraduate Press, Rhodes Pharmaceuticals, Roche, Sage, Seaside Pharmaceuticals, Shire, Stanley Medical Research Institute, Sunovion, Supernus Pharmaceuticals, Transcept Pharmaceuticals, Validus, and WebMD. Drs. Farmer, Molina, Kolko, and Rice; and Ms. Buchan-Page and Ms. Brown report no conflicts of interest.
References
- Aman M, Leone S, Lecavalier L, Park L, Buican B, Coury D: The Nisonger Child Behavior Rating Form: Typical IQ version. Int Clin Psychopharmacol 23:232–242, 2008 [DOI] [PubMed] [Google Scholar]
- Aman MG, Bukstein OG, Gadow KD, Arnold LE, Molina BS, McNamara NK, Rundberg-Rivera EV, Li X, Kipp H, Schneider J, Butter EM, Baker J, Sprafkin J, Rice RR, Jr, Bangalore SS, Farmer CA, Austin AB, Buchan-Page KA, Brown NV, Hurt EA, Grondhuis SN, Findling RL: What does risperidone add to parent training and stimulant for severe aggression in child attention-deficit/hyperactivity disorder? J Am Acad Child Adolesc Psychiatry 53:47–60 e41, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision. Washington, DC: American Psychiatric Association; 2000 [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013 [Google Scholar]
- Arnold LE, Elliott M, Sachs L, Bird H, Kraemer HC, Wells KC, Abikoff HB, Comarda A, Conners CK, Elliott GR, Greenhill LL, Hechtman L, Hinshaw SP, Hoza B, Jensen PS, March JS, Newcorn JH, Pelham WE, Severe JB, Swanson JM, Vitiello B, Wigal T: Effects of ethnicity on treatment attendance, stimulant response/dose, and 14-month outcome in ADHD. Consult Clin Psychol 71:713–727, 2003 [DOI] [PubMed] [Google Scholar]
- Branch M: Rate dependency, behavioral mechanisms, and behavioral pharmacology. J Exp Anal Behav 42:511–522, 1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K, Atkins MS, Osborne ML, Milnamow M. A revised teacher rating scale for reactive and proactive aggression. J Abnorm Child Psychol 24:473–480, 1996 [DOI] [PubMed] [Google Scholar]
- Bussing R, Winterstein A: Polypharmacy in attention deficit hyperactivity disorder treatment: current status, challenges and next steps. Curr Psychiatry Rep 14:447–449, 2012 [DOI] [PubMed] [Google Scholar]
- Chacko A, Wymbs BT, Wymbs FA, Pelham WE, Swanger–Gagne MS, Girio E, Pirvics L, Herbst L, Guzzo J, Phillips C, O'Connor B. Enhancing traditional behavioral parent training for single mothers of children with ADHD. J Am Acad Child Adolesc Psychiatry 38:206–218, 2009 [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Harvey PD, Kupsaw–Lawrence E, Herbert JL, Bernstein D: Development of neuropharmacologically based behavioral assessments of impulsive aggressive behavior. J Neuropsychiatry Clin Neurosc 3:S44–S51, 1991 [PubMed] [Google Scholar]
- Dodge KA, Coie JD: Social-information-processing factors in reactive and proactive aggression in children's peer groups. J Pers Soc Psychol 53: 1146, 1987 [DOI] [PubMed] [Google Scholar]
- Drabick D, Gadow K: Deconstructing oppositional defiant disorder: Clinic-based evidence for an anger/irritability phenotype. J Am Acad Child Adolesc Psychiatry 51:384–393, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS: The McMaster Family Assessment Device. J Marital Fam Ther 9:171–180, 1983 [Google Scholar]
- Farmer C: Demystifying moderators and mediators in intellectual and developmental disabilities research: a primer and review of the literature. J Intellect Disabil Res 56:1148–1160, 2012 [DOI] [PubMed] [Google Scholar]
- Farmer CA, Arnold LE, Bukstein OG, Findling RL, Gadow KD, Li X, Butter EM, Aman MG: The treatment of severe child aggression (TOSCA) study: Design challenges. Child Adolescent Psychiatry Mental Health 5:36, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ: Early conduct problems and later life opportunities. J Child Psychol Psychiatry 39:1097–1108, 1998 [PubMed] [Google Scholar]
- Findling R, Youngstrum E, Fristad M, Birmaher B, Kowach R, Arnold L, Frazier T, Axelson D, Ryand N, Demeter C, Gill M, Fields B, Depew J, Kennedy S, Marsh L, Rowles B, Horwitz S: Characteristics of children with elevated symptoms of mania: The Longitudinal Assessment of Manic Symptoms (LAMS) study. J Clin Psychiatry 71:1664–1672, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frick P, Hare R: The Antisocial Process Screening Device (APSD). Toronto: Multi-Health Systems; 2001 [Google Scholar]
- Gadow K, Sprafkin J: Child and Adolescent Symptom Inventory-4R. Stony Brook, NY: Checkmate Plus; 2005 [Google Scholar]
- Gadow KD, Arnold LE, Molina BSG, Findling RL, Bukstein OG, Brown NV, McNamara NK, Rundberg–Rivera EV, Li X, Kipp HL, Schneider J, Farmer CA, Baker JL, Sprafkin J, Rice RR, Bangalore SS, Butter EM, Buchan–Page KA, Hurt EA, Austin AB, Grondhuis SN, Aman MG: Risperidone added to parent training and stimulant medication: effects on attention-deficit/hyperactivity disorder, oppositional defiant disorder, conduct disorder, and peer aggression. J Am Acad Child Psychol 53:948–959, 959.e1, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanter CA, Carlson GA, Jensen PS, Greenhill LL, Davies M, Li W, Chuang S, Elliott G, Arnold L, March J, Hechtman L, Pelham W, Swanson JM: Response to methylphenidate in children with attention deficit hyperactivity disorder and manic symptoms in the multimodal treatment study of children with attention deficit hyperactivity disorder titration trial. J Child Adolesc Psychopharmacol 13:123–136, 2003 [DOI] [PubMed] [Google Scholar]
- Gardner F, Connell A, Trentacosta CJ, Shaw DS, Dishion TJ, Wilson MN: Moderators of outcome in a brief family-centered intervention for preventing early problem behavior. J Consult Clin Psychol 77:543–553, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghuman JK, Riddle MA, Vitiello B, Greenhill LL, Chuang SZ, Wigal SB, Kollins SH, Abikoff HB, McCracken JT, Kastelic E, Scharko AM, McGough JJ, Murray DW, Evan L, Swanson JM, Wigal T, Posner K, Cunningham C, Davies M, Skrobala AM: Comorbidity moderates response to methylphenidate in the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS). J Child Adolesc Psychopharmacol 17:563–580, 2007 [DOI] [PubMed] [Google Scholar]
- Haas S, Waschbusch D, Pelham W, Jr, King S, Andrade B, Carrey N: Treatment response in CP/ADHD children with callous/unemotional traits. J Abnorm Child Psychol 39:541–552, 2011 [DOI] [PubMed] [Google Scholar]
- Hinshaw SP: Moderators and mediators of treatment outcome for youth with ADHD: Understanding for whom and how interventions work. Ambul Pediatr 7Suppl. 1:91–100, 2007 [DOI] [PubMed] [Google Scholar]
- Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, March JS, Arnold L E, Cantwell DP, Conners CK, Elliott GR, Greenhill LL, Hechtman L, Hoza B, Pelham WE, Severe JB, Swanson JM, Wells KC, Wigal T, Vitiello B: ADHD comorbidity findings from the MTA study: Comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry 40:147–158, 2001 [DOI] [PubMed] [Google Scholar]
- Kaat A, Farmer C, Gadow K, Findling R, Bukstein O, Arnold E, Bangalore S, McNamara N, Aman M: Factor validity of a proactive and reactive aggression rating scale. J Child Fam Stud. November27, 2014. Epub ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman A, Kaufman N: Kaufman Brief Intelligence Test, 2nd ed. Bloomington, MN: Pearson, Inc.; 2004 [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N: Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988, 1997 [DOI] [PubMed] [Google Scholar]
- Kolko DJ, Pardini DA: ODD dimensions, ADHD, and callous–unemotional traits as predictors of treatment response in children with disruptive behavior disorders. J. Abnorm Psychol 119:713–725, 2010 [DOI] [PubMed] [Google Scholar]
- Kraemer H, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychol 27:S101, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer H, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry 59:877–883, 2002 [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Lochman JE: Moving beyond efficacy and effectiveness in child and adolescent intervention research. J Consult Clin Psychol 77:373–382, 2009 [DOI] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Gouze KR, Cicchetti C, Jessup BW, Arend R, Pochyly J, Binns HJ: Predictor and moderator effects in the treatment of oppositional defiant disorder in pediatric primary care. J Pediatr Psychol 33:462–472, 2008 [DOI] [PubMed] [Google Scholar]
- Lundahl B, Risser HJ, Lovejoy MC: A meta-analysis of parent training: Moderators and follow-up effects. Clin Psychol Rev 26:86–104, 2006 [DOI] [PubMed] [Google Scholar]
- McClellan J, Kowatch R, Findling RL: Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 46:107–125, 2007 [DOI] [PubMed] [Google Scholar]
- McKinney C, Renk K: Atypical antipsychotic medications in the management of disruptive behaviors in children: Safety guidelines and recommendations. Clin Psychol Rev 31:465–471, 2011 [DOI] [PubMed] [Google Scholar]
- McTaggart P, Sanders M: Mediators and moderators of change in dysfunctional parenting in a school-based universal application of the Triple-P Positive Parenting Programme. J Child Serv 2:4–17, 2007 [Google Scholar]
- MTA Cooperative Group: A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 56:1073–1086, 1999a [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group: Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: The multimodal treatment study of children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 56:1088–1096, 1999b [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Jarrett MA, Grills–Taquechel AE, Hovey LD, Wolff JC: Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clin Psychol Rev 28:1447–1471, 2008 [DOI] [PubMed] [Google Scholar]
- Owens E B, Hinshaw SP, Kraemer HC, Arnold LE, Abikoff HB, Cantwell DP, Conners CK, Elliott G, Greenhill LL, Hechtman L, Hoza B, Jensen PS, March JS, Newcorn JH, Pelham WE, Severe JB, Swanson JM, Vitiello B, Wells KC, Wigal T: Which treatment for whom for ADHD? Moderators of treatment response in the MTA. J Consult Clin Psychol 71:540–552, 2003 [DOI] [PubMed] [Google Scholar]
- Rieppi R, Greenhill LL, Ford RE, Chuang S, Wu M, Davies M, Abikoff HB, Arnold LE, Conners CK, Elliott GR, Hechtman L, Hinshaw SP, Hoza B, Jensen PS, Kraemer HC, March JS, Newcorn JH, Pelham WE, Severe JB, Swanson JM, Vitiello B, Wells KC, Wigal T. Socioeconomic status as a moderator of ADHD treatment outcomes. J Am Acad Child Adolesc Psychiatry 41:269–277, 2002 [DOI] [PubMed] [Google Scholar]
- Shelleby EC, Kolko DJ: Predictors, moderators, and treatment parameters of community and clinic-based treatment for child disruptive behavior disorders. J Child Fam Stud 1–15, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stattin H, Magnusson D: The role of early aggressive behavior in the frequency, seriousness, and types of later crime. J Consult Clin Psychol 57:710–718, 1989 [DOI] [PubMed] [Google Scholar]
- Stringaris A, Goodman R: Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinct predictions. J Am Acad Child Adolesc Psychiatry 48:404–412, 2009 [DOI] [PubMed] [Google Scholar]
- Teicher MH, Polcari A, Anderson CM, Andersen SL, Lowen SB, Navalta CP: Rate dependency revisited understanding the effects of methylphenidate in children with attention deficit hyperactivity disorder. J Child Adolesc Psychopharmacol 13:41–51, 2003 [DOI] [PubMed] [Google Scholar]
- Tremblay RE, Nagin DS, Séguin JR, Zoccolillo M, Zelazo PD, Boivin M, Pérusse D, Japel C: Physical aggression during early childhood: Trajectories and predictors. Pediatrics, 114:e43–e50, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Zeijl J, Mesman J, Van Ijzendoorn MH, Bakermans–Kranenburg MJ, Juffer F, Stolk MN, Koot HM, Alink LRA: Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: A randomized controlled trial. J Consult Clin Psychol 74:994–1005, 2006 [DOI] [PubMed] [Google Scholar]
- Vitiello B, Stoff DM: Subtypes of aggression and their relevance to child psychiatry. J Am Acad Child Adolesc Psychiatry 36:307–315, 1997 [DOI] [PubMed] [Google Scholar]
- Waxmonsky J, Pelham WE, Gnagy E, Cummings MR, O'Connor B, Majumdar A, Verley J, Hoffman M, Massetti G, Burrows–MacLean L, Fabiano G, Waschbusch D, Chakco A, Arnold F, Walker K, Garefino A, Robb JA: The efficacy and tolerability of methylphenidate and behavior modification in children with attention-deficit/hyperactivity disorder and severe mood dysregulation. J Child Adolesc Psychopharmacol 18:573–588, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Q, Sandler IN, Millsap RE, Wolchik SA, Dawson–McClure SR: Mother-child relationship quality and effective discipline as mediators of the 6-year effects of the New Beginnings Program for children from divorced families. J Consult Clin Psychol 76:579, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuddas A, Zanni R, Usala T: Second generation antipsychotics (SGAs) for non-psychotic disorders in children and adolescents: A review of the randomized controlled studies. Eur Neuropsychopharmacol 21:600–620, 2011 [DOI] [PubMed] [Google Scholar]