ABSTRACT
The spontaneous control of human and simian immunodeficiency viruses (HIV/SIV) is typically associated with specific major histocompatibility complex (MHC) class I alleles and efficient CD8+ T-cell responses, but many controllers maintain viral control despite a nonprotective MHC background and weak CD8+ T-cell responses. Therefore, the contribution of this response to maintaining long-term viral control remains unclear. To address this question, we transiently depleted CD8+ T cells from five SIV-infected cynomolgus macaques with long-term viral control and weak CD8+ T-cell responses. Among them, only one carried the protective MHC allele H6. After depletion, four of five controllers experienced a transient rebound of viremia. The return to undetectable viremia was accompanied by only modest expansion of SIV-specific CD8+ T cells that lacked efficient SIV suppression capacity ex vivo. In contrast, the depletion was associated with homeostatic activation/expansion of CD4+ T cells that correlated with viral rebound. In one macaque, viremia remained undetectable despite efficient CD8+ cell depletion and inducible SIV replication from its CD4+ T cells in vitro. Altogether, our results suggest that CD8+ T cells are not unique contributors to the long-term maintenance of low viremia in this SIV controller model and that other mechanisms, such as weak viral reservoirs or control of activation, may be important players in control.
IMPORTANCE Spontaneous control of HIV-1 to undetectable levels is associated with efficient anti-HIV CD8+ T-cell responses. However, in some cases, this response fades over time, although viral control is maintained, and many HIV controllers (weak responders) have very low frequencies of HIV-specific CD8+ T cells. In these cases, the importance of CD8 T cells in the maintenance of HIV-1 control is questionable. We developed a nonhuman primate model of durable SIV control with an immune profile resembling that of weak responders. Transient depletion of CD8+ cells induced a rise in the viral load. However, viremia was correlated with CD4+ T-cell activation subsequent to CD8+ cell depletion. Regain of viral control to predepletion levels was not associated with restoration of the anti-SIV capacities of CD8+ T cells. Our results suggest that CD8+ T cells may not be involved in maintenance of viral control in weak responders and highlight the fact that additional mechanisms should not be underestimated.
INTRODUCTION
A rare subset of human immunodeficiency virus type 1 (HIV-1)-infected patients called HIV controllers (HIC) are naturally able to maintain durable, tight control of the infection in the absence of therapy (1, 2). These cases are often considered examples in the search for a functional HIV cure (3). Most HIC are infected by replication-competent viruses (4–6), indicating that host mechanisms actively restrain HIV-1 infection. An efficient HIV-specific CD8+ T-cell response is thought to play a decisive role in natural control. Some HLA class I molecules (especially HLA-B*5701 and -B*2705) are associated with lower viral loads (VL) (7) and are overrepresented in HIC (8, 9). Many HIC (strong responders [SR]) possess high frequencies of HIV-specific CD8+ T cells that are highly functional in response to HIV antigens (9–11). These HIV-specific CD8+ T cells can suppress ex vivo HIV infection of autologous CD4+ T cells (9, 12), probably due to their ability to upregulate the cytotoxic-granule content (11, 13, 14).
However, HIC exhibit immunological heterogeneity; many of them (weak responders [WR]) are able to maintain viremia at undetectable levels despite displaying weak HIV-specific CD8+ T-cell responses (12, 15, 16). Differences in T-cell responses between SR and WR cannot be explained by their expression of HLA class I alleles because they are overrepresented to the same extent in both groups (17). This raises the question of the real contribution of CD8+ T-cell responses to the maintenance of long-term viral control in these patients. In WR, it is possible that highly reactive HIV-specific memory CD8+ T cells expand and acquire effector functions in response to relapses in viral replication, thereby controlling the virus when necessary. In fact, a recent report showed that CD8+ T cells from WR HIC can gain the capacity to suppress HIV replication after a short period of in vitro stimulation with HIV peptides (18). However, cells from antiretroviral-treated patients have also been shown to acquire similar properties following peptide stimulation (19) but cannot prevent viral rebound following treatment interruption.
Cases of spontaneous control of viral replication have been reported in some macaques infected with simian immunodeficiency virus (SIV) (20–22). As in humans, these cases are mostly associated with a favorable genetic background (e.g., Mamu B*08 or B*17 in rhesus macaques [RM] or the H6 haplotype in cynomolgus macaques [CyM]) (20, 23–26). CD8+ T cell-mediated control of infection in RM has been demonstrated through in vivo CD8+ cell depletion experiments (21, 27) or by the occurrence of major histocompatibility complex (MHC) escape mutations in viruses from progressor macaques (28). However, these studies have focused mainly on animals carrying protective MHC alleles, and this may be a confounding factor when evaluating the roles of mechanisms other than T-cell responses.
Here, we report a high frequency of spontaneous set point viral control in 6 CyM intrarectally infected with low doses (5 50% animal infectious doses [AID50]) of SIVmac251. Five CyM displayed a long-term-controller profile. Four had an MHC haplotype distinct from the H6 haplotype that is usually associated with this phenotype, and they all displayed a strong decrease in CD8+ T-cell antiviral activities over years of viral control. To our knowledge, this is the first report of an animal model that resembles the WR phenotype sometimes observed in HIC. We used this model to explore the contribution of CD8+ T-cell responses in WR by transiently depleting CD8-expressing cells. Next, we performed phenotypic analyses and directly assessed the anti-SIV activity of CD8+ T cells on superinfected autologous CD4+ T cells, a function known to correlate with protection in HIV controllers. As previously reported, CD8+ depletion induced transient viral escape, but unexpectedly, the CD8-mediated anti-HIV immunity was not strongly recalled and no increase in ex vivo antiviral activity could be detected at the time of the reestablishment of viral control.
MATERIALS AND METHODS
Ethics statement.
Adult CyM (Macaca fascicularis) were imported from Mauritius and housed in the facilities of the Commissariat à l'Energie Atomique et aux Energies Alternatives (CEA) (Fontenay-aux-Roses, France). CyMs are used at the CEA in accordance with French national regulations and under the supervision of national veterinary inspectors (CEA permit number A 92-032-02). The CEA complies with the Standards for Human Care and Use of Laboratory Animals of the Office for Laboratory Animal Welfare (OLAW) (USA) under OLAW Assurance number A5826-01. All experimental procedures were conducted according to European guidelines for animal care. This experiment was approved by the ethics committee Comite d'Ethique en Experimentation Animale de la Direction des Sciences du Vivant au CEA under reference number 10-006.
Animals, infection, and CD8+ depletion.
The MHC haplotype was determined as previously described (23). Six animals were intrarectally inoculated with 5 AID50 of an uncloned SIVmac251 isolate (provided by A. M. Aubertin, Université Louis Pasteur, Strasbourg, France). These animals were followed for up to 6 years postinfection (p.i.). For CD8+ depletion, animals were intravenously treated with a single dose of the anti-human CD8 monoclonal antibody CM-T807 (50 mg/kg of body weight) provided by the National Institutes of Health nonhuman primate reagent resources. These animals were compared to another group of 11 animals infected intrarectally with 50 AID50 of the same isolate.
Sample collection and processing.
Blood sampling (days −15, −8, 3, 7, 10, 13, 17, 21, 28, 35, 42, 65, and 177), bronchoalveolar lavages (BAL) (days −15, 14, 44, and 177), lymph node (LN) biopsies (days −15, 13, and 35, 42, or 177, depending on the kinetics of the reconstitution of CD8+ T cells), and rectal biopsies (RB) (days −20, 15, and 35, 43, or 177, depending on the kinetics of the reconstitution of CD8+ T cells) were performed after ketamine anesthesia. Blood samples were collected in BD Vacutainer Plus Plastic K3 EDTA tubes (BD Biosciences, France). Tissue samples were collected in phosphate-buffered saline (PBS) or snap-frozen in liquid nitrogen for storage at −80°C.
Plasma was isolated from EDTA blood samples by centrifugation for 10 min at 1,500 × g and cryopreserved. Whole blood, peripheral blood leukocytes (PBLs), peripheral blood mononuclear cells (PBMCs), BAL fluid, LN, RB cell suspensions, and purified CD4+ and CD8+ T cells were used for experiments. Peripheral LN cells were obtained using a GentleMACS dissociator (Miltenyi Biotech). Cell suspensions from RB were obtained by a protocol used for humans (29) that was adapted in house for macaques. Briefly, several 1-mm2 punches of mucosa were collected and digested for 45 min with collagenase II (Sigma-Aldrich), mechanically disrupted with a syringe equipped with an 18-gauge blunt-end needle, and passaged through a 70-μm-pore-size cell strainer. Finally, cell suspensions were isolated using a 30%-70% Percoll gradient. BAL fluid was passed through a 100-μm-pore-size cell strainer and washed with PBS to obtain the final cell suspension.
CD4+ and CD8+ T cells were purified from cell suspensions with antibody-coated magnetic beads in a Robosep instrument (Stemcell Technologies). CD4+ T cells were obtained with a custom positive nonhuman primate CD4+ T-cell selection kit, and untouched CD8+ T cells were obtained subsequently with a custom negative nonhuman primate CD8+ T-cell selection kit (Stemcell Technologies).
T-cell phenotypic characterizations by flow cytometry.
Analyses were performed on whole blood, PBLs, or cell suspensions. A list of the antibodies used is provided in Table S1 in the supplemental material. Naive cells were defined as CD95− CD28+, central memory (CM) cells as CD95+ CD28+ CCR5− CCR7+, transitional memory (TM) cells as CD95+ CD28+ CCR5+, and effector memory (EM) cells as CD95+ CD28−. Antibodies were added to 50 μl of blood or 2 × 106 cells from tissues and, after 15 min of incubation, red blood cells were lysed with fluorescence-activated cell sorter (FACS) lysing solution (BD Biosciences). Ki67 staining was performed after permeabilization with the IntraStain kit (Dako). The cells were washed and resuspended in CellFix prior to acquisition.
ICS.
For intracellular cytokine staining (ICS), cell preparation, culture, stimulation, staining, acquisition, and analysis were performed as described previously (30). Peptide pools consisting of 15-mer overlapping peptides (11-amino-acid overlap, 1 μM each, covering the Gag, Vif, Rev, and Nef proteins of SIVmac251 [Proteogenix, Strasbourg, France]) were used for stimulation. Gag was covered by two peptide pools, one encompassing p6 to p8 and the other p15 to p27.
Measurement of CD8+ T-cell-mediated SIV suppression.
A previously described assay for measuring the capacity of human CD8+ T cells to suppress HIV infection of autologous CD4+ T cells (31) was adapted to the CyM-SIVmac251 model. Briefly, purified CD4+ cells were stimulated for 3 days with 10 μg/ml concanavalin A (ConA) in the presence of interleukin 2 (IL-2) (Chiron) at 100 IU/ml. CD8+ T cells were maintained in culture in the absence of mitogens and cytokines. Then, CD4+ T cells (105) in 96-well plates were superinfected with SIVmac251 (multiplicity of infection [MOI], 10−2) using a spinoculation protocol (32) in the presence or absence of CD8+ T cells (CD8/CD4 ratio, 1:1). After challenge, the cells were washed and cultured for 14 days. The capacity of CD8+ T cells to suppress infection was calculated as the log10 drop in p27 levels registered at the peak of viral replication in CD4+ T cells when CD8+ T cells were present in the culture.
Detection of viral production in culture supernatants.
Reverse transcriptase activity was measured by using the Lenti-RT Activity Assay (Cavidi Tech), and p27 protein concentrations were assayed with the Retro-Tek SIV p27 Antigen ELISA (enzyme-linked immunosorbent assay) kit (ZeptoMetrix), both following the manufacturer's instructions.
vRNA quantification in tissues and plasma.
Absolute concentrations of plasma viral RNA (vRNA) and tissue vDNA were determined as previously described (33, 34). The SIV Gag primers and probe used were as follows: Forward, GCAGAGGAGGAAATTACCCAGTAC; Reverse, CAATTTTACCCAGGCATTTAATGTT; and Probe, TGTCCACCTGCCATTAAGCCCGA. The GAPDH (glyceraldehyde-3-phosphate dehydrogenase) primers and probe used were as follows: Forward, GAAGGTGAAGGTCGGAGTC; Reverse, GAAGATGGTGATGGGATTTC; and Probe, CAAGCTTCCCGTTCTCAGCC.
The quantification limit (QL) for vRNA in the classical assay was estimated to be 111 copies/ml, and the detection limit (DL) was estimated to be 37 copies/ml. A more sensitive method was applied for the follow-up of the CD8 depletion phase, as previously described (35). In this case, the QL and DL were 37 and 12.3 copies of vRNA/ml, respectively.
Cytokine quantification.
Cytokine concentrations in plasma were assayed with Luminex (23-plex nonhuman primate kit; Merck Millipore) with a MagPix instrument. Plasma IL-7 levels were determined using a Human IL-7 ELISA kit (R&D Systems), as previously described (36).
Western blot analysis.
Western blots were performed using a commercial SIV Western Blot Assay kit (ZeptoMetrix) following the manufacturer's instructions.
Statistical analysis.
The nonparametric Spearman rank correlation test was used to investigate the relationship between variables. The nonparametric Mann-Whitney test was used to compare data sets between groups, and the paired nonparametric Wilcoxon signed-rank test was used to compare data from the same macaques at different time points. All statistical analyses were performed using GraphPad Prism 5.03 software (GraphPad Software, La Jolla, CA, USA). In the 2-tailed tests, P values of 0.05 or lower were considered to be significant.
RESULTS
A high proportion of controllers among cynomolgus macaques exposed intrarectally to 5 AID50 of SIVmac251.
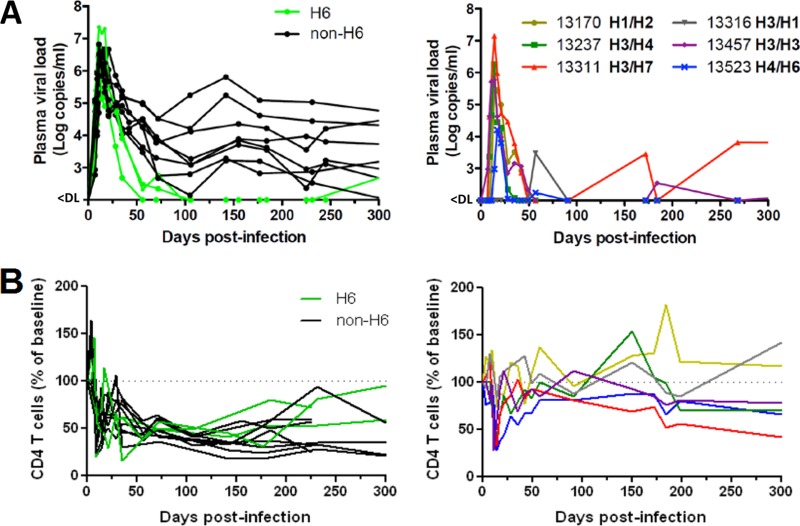
Atraumatic intrarectal exposure of 11 CyM to high doses (50 AID50) of an uncloned SIVmac251 isolate resulted in relatively similar peaks of plasma viremia in all animals. The peaks were observed on day 11 p.i., with viral loads ranging from 7 × 105 to 6 × 107 RNA copies/ml (median, 3 × 106 RNA copies/ml) (Fig. 1A). Three CyM bearing the protective H6 haplotype (23, 24) demonstrated control of plasma viremia below 100 copies/ml at the set point (3 months). In contrast, none of the non-H6 macaques controlled their viremia to such a low level at this time (median, 3 × 104 RNA copies/ml), and their CD4+ T-cell counts declined during the first year of infection (Fig. 1B).
FIG 1.
MHC H6 haplotype and low-dose intrarectal infection are both associated with spontaneous control of SIVmac251 infection in CyM. (A) Longitudinal evolution of plasma viral loads in macaques exposed intrarectally to 50 AID50 (n = 11) (left) or 5 AID50 (n = 6) (right) of SIVmac251. In the 50-AID50 group, MHC H6-bearing animals are shown in green and non-H6 animals in black. Animals in the 5-AID50 group are color coded, and MHC haplotypes are indicated for each animal. The viral-RNA QL and DL were 111 and 37 copies of vRNA/ml, respectively. (B) Longitudinal evolution of CD4+ T-cell blood counts in the 50-AID50 group (n = 11) (left) and in the 5-AID50 group (n = 6) (right). CD4+ T-cell counts are expressed as a percentage of the mean preinfection value for each macaque.
In comparison, the exposure of six macaques to 10-fold-lower doses (5 AID50) of the same virus isolate by the same route was associated with diverse peaks of plasma viremia, ranging from 5 × 101 to 1.42 × 107 RNA copies/ml (median, 4.41 × 105 RNA copies/ml) (Fig. 1A). Early spontaneous control below 100 RNA copies/ml at the set point (3 months) was observed in all six macaques, although only one (no. 13523) possessed the H6 haplotype. One macaque (13311) lost control of the infection shortly after, between 3 and 6 months p.i. The remaining five macaques remained below 400 RNA copies/ml for >5 years. One macaque (13316) did not seroconvert and displayed only blips of viremia early during the course of the infection. The CD4+ T-cell count declined during acute infection in four of the five controllers in the 5-AID50 group and recovered almost completely at the set point with no major changes afterward (Fig. 1B).
These observations revealed a high proportion of long-term SIV controllers (SIC) in a group of CyM exposed intrarectally to a relatively low dose (5 AID50) of SIVmac251 that could not be related solely to a favorable MHC haplotype.
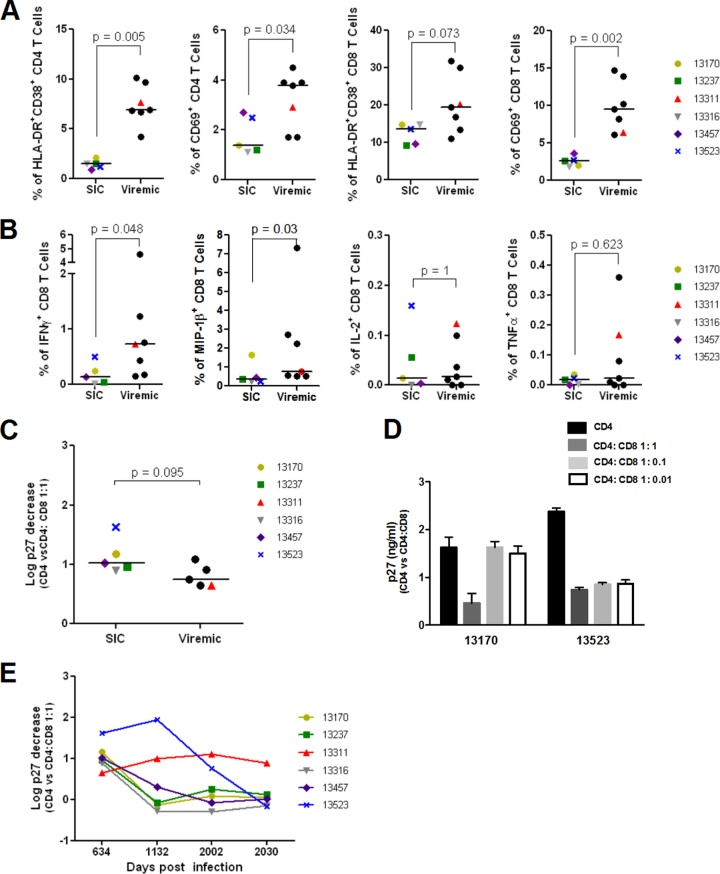
SIV controllers displayed weak CD8+ T-cell activation, cytokine production, and SIV-suppressive capacity during the chronic phase of infection.
Because the 5-AID50 CyM were not initially dedicated to the analysis of T-cell immunity during primary infection, we could explore the CD8+ T-cell response in the five SIC only after 2 years p.i. We compared the CD8+ T-cell responses to those of the animal that had lost viral control (13311) and six other CyM with uncontrolled viremia (median VL, 5 × 104 copies/ml) that were infected at the same time with a higher dose of the same virus stock. T-cell activation, measured as either CD69 expression or CD38–HLA-DR coexpression, was lower in controllers than in noncontrollers (Fig. 2A). ICS revealed that Gag-specific CD8+ T-cell responses (especially the gamma interferon [IFN-γ]- and MIP-1β-producing cells that constituted the largest proportion of the response) were generally lower in controllers than in noncontrollers (Fig. 2B).
FIG 2.
SIV controllers display low T-cell activation and low CD8+ T-cell responses during the chronic phase. Two years p.i., the five long-term controllers of the 5-AID50 group were compared to the only viremic animal in the group (13311) and six other noncontroller macaques. (A) The coexpression of HLA-DR and CD38 and the expression of CD69 by CD4+ (left) and CD8+ (right) T cells were assessed to evaluate chronic T-cell activation. (B) SIV Gag-specific CD8+ T-cell responses were assessed by ICS after stimulation with a pool of overlapping SIV Gag p15-p27 peptides. Shown are (from left to right) the percentages of IFN-γ+, MIP-1β+, IL-2+, and tumor necrosis factor alpha-positive (TNF-α+) cells. (C) The SIV-suppressive activity of blood CD8+ T cells from SIC and noncontroller animals was measured on autologous activated CD4+ T cells superinfected in vitro with SIVmac251. SIV suppression is reported as the log decline in p27 titers in CD4+ T cell supernatants when autologous ex vivo unstimulated CD8+ T cells were added at a 1:1 ratio to the culture. (A to C) Each symbol represents one animal, and horizontal lines represent the median value for the group. (D) SIV replication in culture supernatants of CD4+ T cells from SIC 13170 and 13523 in the absence of CD8+ T cells or at various CD4+/CD8+ T-cell ratios. The error bars indicate standard deviations. (E) Longitudinal follow-up of CD8+ T-cell-dependent SIV-suppressive antiviral activity over 3 years in the six macaques exposed to an inoculum of 5 AID50 of virus.
CD8+ T cells from HIC are endowed ex vivo with a strong capacity to suppress HIV infection of autologous CD4+ T cells (9, 12). We adapted this technique (31) to assess the capacity of CD8+ T cells from CyM to suppress SIV infection of autologous CD4+ T cells. CD8+ T cells from the five SIC collected on day 634 p.i. showed some capacity to suppress SIV infection, although their capacities were not stronger than those from noncontroller CyM (Fig. 2C). However, the CD8+ T cells from the animal with the H6 haplotype (13523) had the strongest suppressive capacity, even at low effector/target cell ratios (Fig. 2D). The suppressive capacities of the five SIC decreased with time, although the anti-SIV activity of the cells from the H6 animal (13523) faded later (Fig. 2E). The SIV-suppressive capacity of the CyM that lost control shortly after the set point (13311) was relatively stable over time, albeit low. CD8+ T cells from the remaining five CyM displayed weak cytotoxic activity 5.5 years p.i. (Fig. 2E). The virus could be isolated in vitro by reactivation of enriched CD4+ T cells from all six macaques. When we evaluated the infectiousness of the viruses from three SICs, we found that they were able to infect CD4+ T cells from uninfected macaques to the same extent as the original SIVmac251 isolate (see Fig. S1 in the supplemental material).
In summary, the SIC displayed lower T-cell activation and lower SIV-specific CD8+ responses than viremic animals during the chronic phase despite the persistence of cells infected with replication-competent viruses. The immune profile of these animals resembles that of the HIC WR that we have described previously (12).
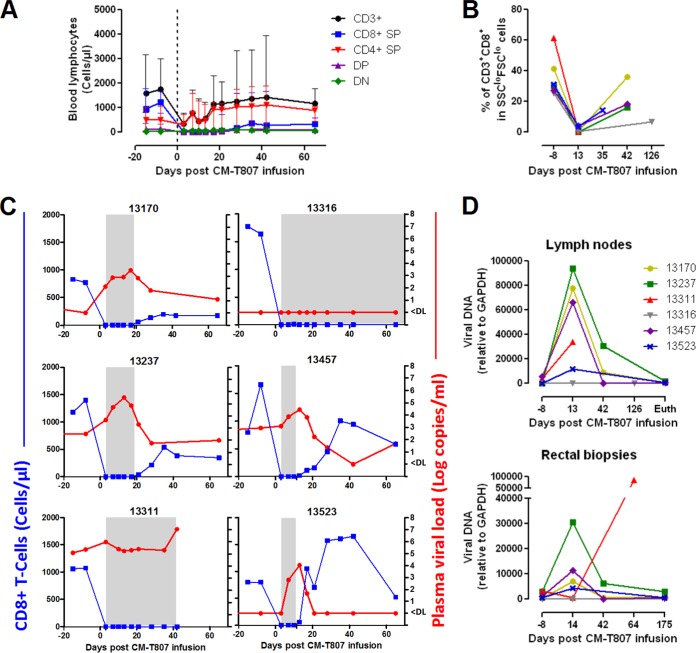
In vivo depletion of CD8+ cells resulted in transient elevation of viral loads in four controllers.
We assessed the consequences of in vivo depletion of CD8+ cells in the five SIC. Animal 13311, which lost control of viremia earlier during infection, was included in this study as a reference control. A single injection of the human monoclonal antibody CM-T807 resulted in profound CD8+ T-cell depletion from the blood (Fig. 3A; see Fig. S2 in the supplemental material); the depletion lasted at least 10 days. The CD8+ T-cell pool progressively recovered in all controllers, with kinetics differing between animals in the following order: 13523, 13457 (days 10 to 13), 13237, 13170 (days 17 to 21), and 13316 (days 65 to 177). The health of the progressor animal (13311) quickly degraded 5 weeks after CD8+ depletion, and the animal died of AIDS hours before scheduled euthanasia and before any detectable CD8+ cell recovery was observed.
FIG 3.
In vivo depletion of CD8+ cells after 5 years of chronic infection led to a transient increase in viremia in all but one SIV controller. The consequences of CM-T807 monoclonal antibody (MAb) infusion for T-cell populations and viral loads were monitored by flow cytometry and quantitative PCR (qPCR), respectively. (A) Evolution of circulating T-cell populations, including total CD3+, single-positive (CD4+ or CD8+) (SP), double-positive (CD4+ CD8+) (DP), and double-negative (CD4− CD8−) (DN) T cells. Median values and ranges are reported. (B) Frequencies of CD8+ T cells in peripheral LN before and after CM-T807 MAb infusion. (C) Temporal association between CD8+ T-cell counts (blue) and viral-RNA loads (red) for each macaque. The time period during which CD8+ T cells were undetectable is shaded in gray. The viral-RNA QL and DL were 37 and 12.3 copies of vRNA/ml, respectively. (D) Cell-associated viral-DNA loads in the peripheral LN (top) and rectal mucosa (bottom).
Similar kinetics were observed in the peripheral LN (Fig. 3B; see Fig. S3A in the supplemental material), as well as in RB specimens and BAL samples (see Fig. S3B in the supplemental material) from all animals. Due to the limited tissue availability, we could not determine whether the CD8+ cell depletion was incomplete or lasted for a shorter time in tissues from animals 13523 and 13457, which had detectable CD8+ cells in their LN at day 13 after depletion. Other CD8+ cells, including CD3− CD8+ NK cells (data not shown) and double-positive (CD4+ CD8+) T cells (Fig. 3A), showed amplitudes and kinetics of depletion similar to those of CD8+ T cells. During the depletion, all remaining CD3+ T cells were CD4+ single-positive T cells, and no increase in the numbers of double-negative CD3+ T cells was detected (Fig. 3A).
Upon depletion, four of the five SIC and the viremic CyM experienced a transient increase in their viral-RNA loads in plasma (Fig. 3C) and their levels of cell-associated SIV DNA in lymphoid and mucosal tissues (Fig. 3D). The viremia peaked on day 13 (13523, 13457, and 13237) or 17 (13170) postdepletion. The viremic animal (13311) experienced an earlier peak of viremia (day 7), which then returned to the predepletion level and eventually increased again. Interestingly, the remaining SIC (13316) never lost viral control following depletion, and the viral load in plasma and in tissues remained undetectable throughout the follow-up phase (see below).
The CD8+ T-cell recovery appeared to coincide temporally with the regain of viral control in three controllers (13170, 13523, and 13457) (Fig. 3C), whereas the regain of viral control began despite CD8+ T cells remaining undetectable in blood or tissues in one SIC (13237) (Fig. 3C; see Fig. S2 and S3 in the supplemental material).
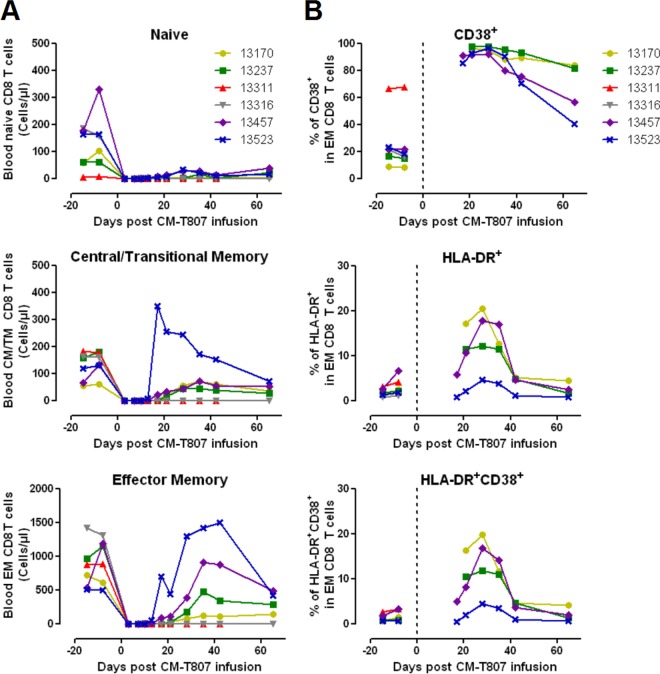
To characterize the CD8+ T-cell recovery after depletion, the naive and memory phenotypes and activation statuses of the cells were assessed by flow cytometry. Most CD8+ T cells returning after the depletion phase possessed an EM phenotype (Fig. 4A) and were much more activated during the reconstitution phase than before depletion (Fig. 4B). EM CD8+ T cell activation peaked on day 28 postdepletion, reaching levels higher than that observed in the progressor (13311) at baseline, and progressively faded with time. The macaque bearing the H6 MHC haplotype (13523) reconstituted EM CD8+ T cells the fastest and to the largest extent, but with the lowest activation levels.
FIG 4.
CD8+ T cells recovering after depletion are mostly activated effector memory cells. CD8+ T-cell subpopulations and activation levels (CD38 and HLA-DR expression) in blood were monitored by flow cytometry. Naive, CM, and EM cells were distinguished on the basis of CD28 and CD95 expression levels. (A) Follow-up of absolute counts of naive, CM/TM, and EM CD8+ T cells in blood at various time points. (B) Expression of the activation markers CD38 (top), HLA-DR (middle), or both (bottom) by EM CD8+ T cells. Note that 13311 did not show any reconstitution of CD8+ cells before death and 13316 exhibited extremely late partial reconstitution of CD8+ cells; this precluded any phenotypic analysis of CD8+ T cells in 50 μl of whole blood for these 2 animals during this period.
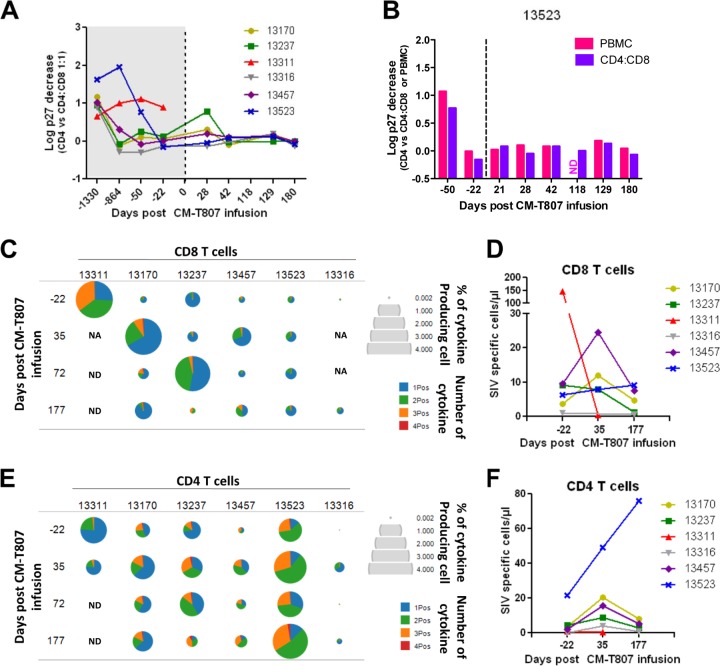
Weak expansion of SIV-specific CD8+ T-cell responses and no increase in SIV-suppressive activity were observed during the CD8+ recovery phase.
Next, we analyzed the evolution of the SIV-specific CD8+ T-cell response in these animals during the CD8+ cell recovery period. We followed the ability of recovered CD8+ T cells to suppress SIV replication in autologous CD4+ T cells in vitro. Activation of CD8+ T cells during reconstitution was not accompanied by an increase in their capacity to suppress SIV infection, which was weak and did not change in the blood of any animal at the time of CD8+ T-cell reconstitution (Fig. 5A). Only cells from macaque 13237 showed slightly higher antiviral activity on day 28. The SIV-suppressive activities of CD8+ T cells isolated from BAL fluid and peripheral LN from SIC were also low at baseline and did not significantly change upon CD8+ T-cell reconstitution (see Fig. S4A in the supplemental material). Total PBMCs could be infected in vitro to the same extent as purified CD4+ T cells (Fig. 5B; see Fig. S4B in the supplemental material), suggesting the absence of other anti-SIV activities in these cultures.
FIG 5.
Regain of viral control in SIV controllers upon CD8+ cell reconstitution was not associated with efficient SIV-suppressive antiviral activities. SIV-specific responses were monitored in peripheral blood by functional assays and ICS. (A) Evolution of the capacity of CD8+ T cells to suppress SIVmac251 replication in autologous CD4 T cells. Predepletion activities (Fig. 2D) are represented in the gray-shaded area for reference. (B) Suppression of SIV replication in PBMCs and in CD4+-CD8+ cocultures (1:1 ratio) from animal 13523 at various time points in comparison to CD4+ T cells cultured alone. ND, not done. (C and E) Cytokine production by CD8+ (C) and CD4+ (E) T cells assayed by ICS. Cumulative responses after stimulation with pools of overlapping peptides from SIV Gag, Rev, Nef, and Vif are represented. The size of each pie is proportional to the percentage of T cells expressing at least one cytokine, including IFN-γ, TNF-α, MIP1β, and IL-2, and the proportions of cells expressing 1 (1Pos), 2 (2Pos), 3 (3Pos), or 4 (4Pos) cytokines are displayed in each pie. NA, not applicable because the samples did not contain enough CD8+ T cells to be analyzed by flow cytometry. ND, not done because 13311 died 2 months after CD8+ cell depletion. (D and F) Absolute counts of circulating SIV-specific T cells expressing at least one cytokine.
ICS after stimulation with pools of overlapping peptides covering the SIV Gag, Nef, Rev, and Vif proteins was used to evaluate the frequency of SIV-specific CD8+ T-cell responses in PBMCs after depletion. A transient relative increase in the percentage of cytokine-producing CD8+ T cells was observed in the five SIC upon CD8+ T-cell reconstitution (Fig. 5C), but these increases were translated into an increase in the absolute numbers of circulating SIV-specific CD8+ T cells in only two animals (13170 and 13457) and remained at low amplitude (Fig. 5C and D). Remarkably, the H6 macaque (13523) displayed the smallest relative increase in the frequency of SIV-specific CD8+ T cells. The polyfunctionality of the cells did not increase following the reconstitution of the CD8+ T-cell compartment, consistent with the weak SIV suppression activities of the CD8+ T cells observed for these animals. Furthermore, no trend toward an increase in a particular SIV antigen-specific response was observed (see Fig. S5 in the supplemental material).
Activated CD8+ T cells can produce soluble factors, such as β-chemokines, that are able to block SIV replication. Therefore, we assessed plasma levels of MIP-1α and MIP-1β. There was an increase in the levels of both β-chemokines that peaked a few days postdepletion and decreased before viremia started to decline (see Fig. S6 in the supplemental material).
ICS analysis revealed the expansion of SIV-specific CD4+ T-cell responses in all controllers upon CD8+ depletion; these cells retained better polyfunctionality than those from the viremic macaque (Fig. 5E). Of note, the highest expansion of SIV-specific CD4+ T cells was observed in the H6 animal (13523) (Fig. 5F). In contrast, the progressor macaque (13311) showed a contraction of the SIV-specific CD4+ T-cell response associated with a severe depletion of CD4+ T cells.
Overall, using a highly effective readout of T-cell functionality (i.e., cytokine production, soluble-suppressive-factor secretion, and direct suppressive ability), we were unable to show evidence of a robust pattern of CD8+ T-cell responses during the return to predepletion viremia levels after viral rebound.
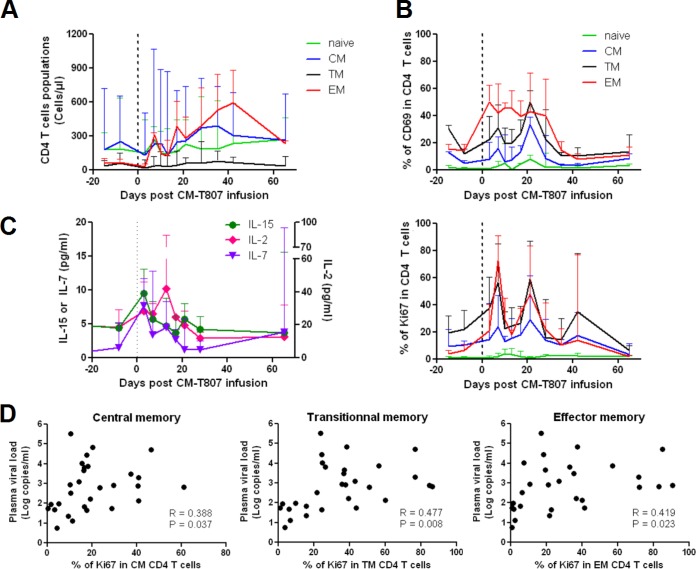
Controllers experienced transient proliferation and activation of transitional memory CD4+ T cells associated with an expansion of effector memory CD4+ T cells and increased viral replication.
It was plausible that the increases in the SIV-specific CD4+ T-cell responses were related to the homeostatic expansion of the CD4+ T-cell compartment, which has been recently reported to occur as a consequence of CD8+ cell depletion in vivo (37, 38). Thus, we monitored changes in the naive/memory subpopulations and the activation and proliferation of CD4+ T cells by flow cytometry. All SIC experienced a progressive increase in the absolute numbers of CD4+ T cells in blood (Fig. 6A). In particular, there was a strong expansion of CD4+ TEM cells (mean increase, 8.47- ± 5.40-fold). CM and TM CD4+ T cell counts also increased, although to a lesser extent (1.95- ± 1.26- and 2.10- ± 1.08-fold mean increases, respectively). During their expansion phase, CD4+ T cells showed a large increase in the expression of the activation markers CD69 (Fig. 6B), CD38, and HLA-DR (data not shown). Two consecutive peaks of proliferation based on Ki67 expression were observed in the 1st and the 3rd weeks after CD8+ cell depletion (Fig. 6B).
FIG 6.
Viral replication in SIV controllers upon CD8+ cell depletion is associated with homeostatic activation levels of the CD4+ T-cell compartment. Flow cytometry and Luminex assays were used to monitor CD4+ T cells and cytokine dynamics in response to CD8+ cell depletion. (A) Absolute blood counts of naive, CM, TM, and EM CD4+ T-cell subpopulations in SIC. (B) Evolution of the activation and proliferation levels of blood CD4+ T-cell subpopulations. Shown are the percentages of activated CD69+ (top) and proliferative Ki67+ (bottom) naive, CM, TM, and EM CD4+ T cells in blood. (C) Plasma IL-2, IL-7, and IL-15 concentrations. (A to C) Median values and ranges are reported. (D) Spearman correlation between Ki67 expression in CM, TM, and EM CD4+ T cells and plasma viral loads after CD8+ cell depletion in SIC. Data pairs for which the viral load was undetectable were excluded.
Transient increases in IL-2 (1.95-fold), IL-7 (2.6-fold), and IL-15 (1.8-fold) concentrations in the plasma were observed following CD8+ cell depletion and coincided with the initial peaks of activation of memory CD4+ T cells (Fig. 6C). The activation and expansion of EM CD4+ T cells coincided with the transient increase in viremia in SIC, and the plasma viral-RNA loads following CD8+ depletion correlated with the percentage of Ki67+ CD4+ memory cells (Fig. 6D). These findings suggest that the transient rebound of viremia in SIC might result from homeostatic CD4+ T-cell activation and proliferation.
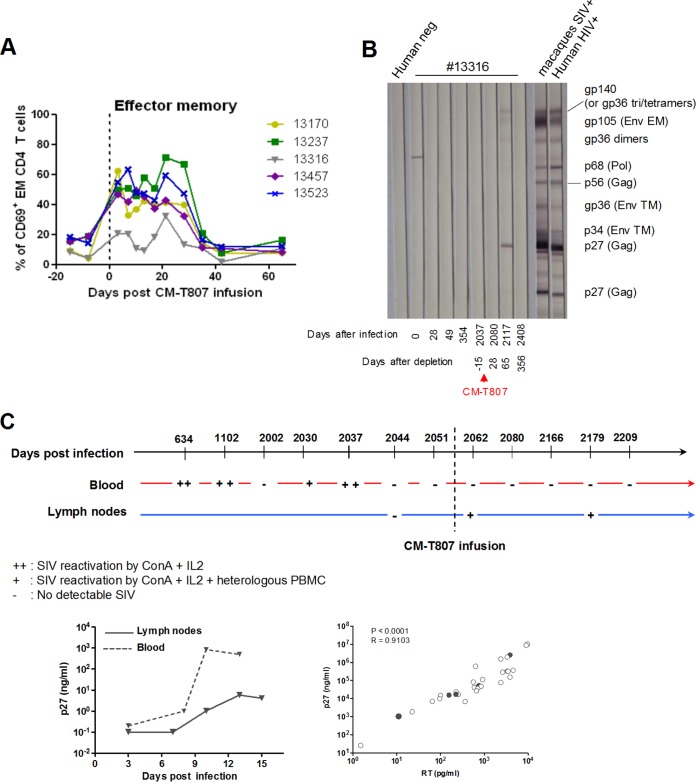
An exceptional profile of one SIV controller with persistently undetectable viral loads despite CD8+ cell depletion.
Macaque 13316 was the only animal that did not experience any detectable increase in viremia following the depletion of CD8+ cells (Fig. 3C and D). This animal showed the lowest levels of CD4+ T-cell activation and expansion following CD8+ cell depletion (Fig. 7A and data not shown). Moreover, only a few blips of detectable plasma viral loads were detected in the animal during the acute phase (Fig. 1), and the viral load remained below 12 copies/ml for 5 years during the chronic stage. Unlike all of the other animals in the 5-AID50 group, macaque 13316 did not seroconvert and showed no detectable reactivity against any SIV proteins before the depletion experiment (Fig. 7B). This macaque had extremely weak T-cell responses upon stimulation with SIV antigens (Fig. 5C and E). The hallmark of persistent infection in this animal included several in vitro reactivations of the virus, evidenced by measuring SIVp27 and reverse transcriptase activity from purified CD4+ T cells collected from both blood and LN (Fig. 7C). The virus isolate was able to infect heterologous CD4+ T cells in vitro, and the sequencing of a region of gag showed a match with the original SIVmac251 sequence (data not shown). Interestingly, the detection of viral replication was easier during the first years of control, when SIV could often be reactivated by mitogenic stimulation of blood CD4+ T cells (Fig. 7C), than at later time points, when it was observed only following stimulation of LN CD4+ T cells. After CD8+ depletion, the viremia remained undetectable, but partial Western blotting reactivity against the Gag and Env proteins was transiently observed (day 65 after depletion) (Fig. 7B). Therefore, macaque 13316 presented an exceptional long-term SIV controller profile that resisted CD8+ cell depletion.
FIG 7.
Macaque 13316 displayed an exceptional profile of control with no detectable increase in plasma viral loads but transient seroconversion after CD8+ cell depletion. (A) Frequencies of CD69+ EM CD4+ T cells from SIV controllers during the CD8+ depletion experiment. (B) Western blot SIV reactivity of plasma collected at various time points from macaque 13316, including pre- and postdepletion time points. (C) (Top) Summary of experiments involving the reactivation of viral replication from purified CD4+ T cells of macaque 13316. Samples were obtained from blood, LN, and purified CD4+ T cells. ++, time points at which SIV was isolated upon ConA activation and culture with IL-2; +, time points at which adjunction of heterologous PBMCs was needed for detectable SIV production; −, time points at which SIV could not be detected. (Bottom left) Two representative examples of SIV reactivation upon stimulation of CD4+ T cells isolated from blood or LN from 13316. (Bottom right) Spearman correlation between p27 concentration and reverse transcriptase (RT) activity in various culture supernatants (different time points in the summary) from macaque 13316 (●) and another CyM (○).
DISCUSSION
In contrast to the rapid-progression macaque models of SIV infection, the SIVmac251 infection model of CyM closely resembles HIV infection in humans in terms of viral load, CD4+ T-cell depletion, and rates of progression (39). Thus, it appears to be an optimal model to study host mechanisms able to naturally control infection. Our work provides further evidence that the H6 haplotype in CyM is associated with the control of infection: following intrarectal inoculation of 11 CyM with 50 AID50 of SIVmac251, the three H6 macaques, but none of the eight non-H6 macaques, were able to control the infection. This association between MHC and the control of infection in CyM seemed to lessen when lower doses of SIVmac251 were used for inoculation: intrarectal inoculation of six CyM with 5 AID50 of SIVmac251 resulted in control of infection in all animals at the set point, despite only one possessing the H6 haplotype. Although one CyM lost control a few months later, the remaining five CyM continued to control SIV viremia for 5 years. This model of CyM controlling infection after intrarectal exposure to low doses of SIVmac251 may be useful for investigating the mechanisms leading to the spontaneous control of HIV/SIV viremia independent of known protective MHC haplotypes, as well as those with MHC-associated control (23, 24, 26, 40–42), in the context of pathogenic-virus infection.
Both a low-dose inoculum and infection through the mucosal route in macaques have been associated with a decreased number of transmitted/founder viruses and lower genetic complexity of the infecting virus (43, 44). This restricted viral diversity may facilitate the control of infection by host mechanisms, possibly due to the lack of necessity for broad-spectrum responses. Although we cannot exclude subtle differences in the fitness of the viruses, all low-dose controllers carried replication-competent viruses that are able to infect heterologous CD4+ T cells to the same extent as the original SIVmac251. Low-dose SIV exposure in macaques has also been associated with lower plasma proinflammatory cytokine levels during the early phases of infection (45), which may provide an optimal context for the development of adaptive responses.
Unfortunately, we were not able to analyze the immune responses during primary infection in our group of CyM exposed to low-dose SIV. After a couple of years of controlling the infection, they exhibited weaker SIV-specific CD8+ T-cell responses and weaker T-cell activation than noncontroller CyM. We analyzed the ex vivo capacities of CD8+ T cells from these macaques to suppress SIV infection of autologous CD4+ T cells using a technique developed for HIV-infected patients to highlight the qualitatively superior HIV-specific CD8+ T-cell response often observed in HIC (9, 12). This activity was not stronger in SIC than in viremic CyM; the exception was macaque 13523, carrying the H6 haplotype, whose CD8+ T cells were able to efficiently suppress SIV infection even at low E/T ratios. Nevertheless, the longitudinal follow-up showed that CD8+ T-cell-mediated SIV suppression waned over time in the SIC. SIV-specific CD8+ T-cell responses were weak and displayed low anti-SIV capacity in blood, BAL fluid, and LN. Only macaque 13311, the animal that lost viral control, maintained almost constant anti-SIV activity ex vivo, albeit at a modest level. Although further analyses including the primary phase of infection are needed, our results are compatible with a scenario in which the CD8+ T-cell response contracts once viremia has been efficiently controlled.
Human HIV controllers are usually characterized after several years of control of the infection. During chronic infection, many HIC show high frequencies of robust HIV-specific CD8+ T cells (9–11). However, many others continue to control their viremia despite low frequencies of HIV-specific CD8+ T cells and a weak suppressive capacity in the blood or rectal mucosa (12, 15, 16, 46). In HIC with weak T-cell responses, an efficient memory CD8+ T-cell response may proliferate in response to viral rebound, rapidly acquire effector functions, and thereby control viral relapses (18), but the quiescent T-cell status in many of these patients suggests that these cells are not actively repressing infection (12). After several years of viral control, our SIC with weak T-cell activation and weak SIV-specific CD8+ T-cell responses resembled these HIC; this finding prompted us to explore the role of their weak CD8+ T-cell responses in the long-term maintenance of SIV control.
The in vivo depletion of CD8+ cells in SIC macaques has been used to highlight the role of CD8+ T-cell response in the control of SIV infection (21, 27), although the interpretation of such experiments deserves discussion. In our study, we observed a transient rebound of viremia in four of the five SIC, which is consistent with previous reports (21, 27). The viral load in one SIC started to decline before we could detect the recovery of CD8+ T cells in the blood or any of the various tissues tested. In the three other SIC who lost control, recovery of their CD8+ T-cell compartments began earlier and coincided with the drop in viremia. The kinetics of the SIV-specific CD8+ T-cell responses indicates that the frequency of these cells expanded very modestly during the CD8+ T-cell recovery phase compared with the baseline levels and the frequency of SIV-specific CD8+ T cells in the viremic CyM. The only exceptions in which a significant expansion of SIV-specific CD8+ T cells were observed corresponded to late time points in animals 13170 and 13237, when viremia was already back to predepletion levels. No differences in CD8+ T-cell polyfunctionality or capacity to suppress SIV infection were found in pre- and postdepletion blood, LN, and BAL fluid samples, including those collected from the H6-bearing CyM (13523), whose cells had the strongest activities at earlier time points. Intriguingly, CD8+ T cells from this macaque, which reconstituted the CD8+ T-cell compartment faster and more strongly than the other animals, expressed by far the lowest levels of HLA-DR and showed the smallest increase in SIV-specific CD8+ T cells during reconstitution. Overall, our findings suggest that other mechanisms may have contributed to the reestablishment of the control of infection in these macaques.
CD8+ T cells can inhibit HIV/SIV infection through noncytolytic soluble factors (47). Several reports have suggested that these mechanisms may play a major role in the CD8-mediated partial control of SIV infection during primary infection in macaques (48–50). In vitro infection of mitogen-activated PBMCs has been widely used to reveal the presence of strong activities of these various soluble antiviral factors. Using this system, we did not observe any significant differences between the levels of SIVmac251 replication in mitogen-activated autologous CD4+ T cells and whole PBMCs. We observed a sharp increase in the plasma MIP-1α and MIP-1β levels a few days after CD8+ depletion, but their peaks preceded the peaks of viremia and their levels subsequently decreased so that they were much lower during the decreasing phase of viremia. Thus, it is unlikely that CD8+ cell-produced soluble factors influenced the viremia during this phase of the study. Although we could not directly analyze the role of NK cells or γδ T cells, our results with PBMCs suggest that no efficient anti-SIV effectors significantly expanded following CD8+ cell depletion and recovery.
In contrast to SIV-specific CD8+ T-cell responses, SIV-specific CD4+ T cells from SIC (which retained better polyfunctionality than those from the viremic macaque) expanded after CD8+ cell depletion, especially in the case of the H6-bearing CyM, 13523. Antigen-specific CD4+ T cells provide help for the generation of functional CD8+ T-cell responses (51). Over the last few years, various reports have suggested that HIV/SIV-specific CD4+ T-cell responses may themselves be endowed with cytotoxic potential (52–54), although it is not clear how this activity is exerted in vivo (40). We cannot rule out the possibility that these cells may have contributed to the reestablishment of the control of infection in SIC, although no direct activities were detected in cultures of purified CD4+ T cells from the SIC before or after CD8+ depletion; indeed, these cultures could be infected in vitro to levels similar to those of cells from healthy macaques (data not shown).
In agreement with previous reports, the expansion of SIV-specific CD4+ T cells was associated with the activation and expansion of the memory CD4+ T-cell compartment and, in particular, of EM cells (37, 38). Indeed, CD8+ cell depletion was followed by an increase in the number of memory CD4+ T cells upregulating the early activation marker CD69, a subsequent increase in the frequency of Ki67+ proliferating CD4+ T cells, and an expansion in the number of memory cells at later time points. It has been suggested that there is an expansion of EM CD4+ T cells in CD8+ cell-depleted macaques in response to the increased IL-15 concentrations in plasma, but the viral dynamics in primary infection are not affected by this expansion (38). We observed two peaks of CD4+ T-cell activation following CD8+ cell depletion in our group of SIC, reminiscent of an early depletion study in SIV-infected RM (55). These peaks coincided with peaks in plasma levels of IL-15, but also of IL-2 and IL-7. All of these cytokines are regulators of T-cell homeostasis (56). Therefore, it is possible that memory CD4+ T cells were activated in response to transient increases in the levels of these interleukins. CD4+ T-cell activation in SIC may increase the number of target cells for SIV replication, and IL-2, IL-7, and IL-15 have been shown in vitro to increase the susceptibility of cells to infection (57, 58) and to reactivate latent provirus from CD4+ T cells (59, 60), including those from HIC with extremely small viral reservoirs (5). We found significant correlations between the levels of plasma viremia and the levels of Ki67+ CD4+ T cells in SIC following CD8+ cell depletion. Our results agree well with the report by Mueller et al. of a correlation between plasma viremia and the number of proliferating CD4+ T cells in CD8+ cell-depleted CyM chronically infected with SHIV89.6P (37). These observations suggest that the homeostatic activation of CD4+ T cells may have played an important role in the loss of the control of viremia in four of our SIC.
Finally, one CyM (13316) represented an exceptional case of control of infection. This macaque did not show a real peak of viremia during acute infection, experienced only two viral blips, and did not seroconvert. Viral RNA and cell-associated DNA were undetectable in either LN or the rectal mucosa at all time points analyzed during chronic infection. Although this profile was evocative of transient or defective infection, the virus could be successfully reactivated in vitro from CD4+ T cells purified from this animal at various time points during the follow-up of the study (up to 6 years after infection), confirming that the animal was infected. Viral reactivation from blood samples was easier at earlier time points, and later, the virus could be rescued only from larger quantities of LN cells. These results suggest that the viral reservoir in this CyM was small and shrank further during the study. This type of occult infection is not unknown; a few similar cases have been reported in various macaque models of SIV infection (61, 62) and even among highly HIV-exposed seronegative individuals (63–65). Remarkably, in vivo CD8+ cell depletion in this animal lasted for several months, during which SIV replication remained undetectable in either plasma or tissues. Thus, the extreme control of SIV infection in the macaque was independent of the CD8+ T-cell response, further arguing for the existence of additional mechanisms contributing to maintaining control of the infection.
Although it is likely that the CD8+ T-cell response makes an important contribution to establishing natural control of SIV infection, our results suggest that its role may be less important for the maintenance of viral control. Several results from this study support this hypothesis: (i) the anti-SIV CD8+ T-cell responses appear to wane over time, while the viremia remains controlled; (ii) although in vivo CD8+ depletion in the SIC was accompanied by a transient loss of control, the viremia was correlated with the activation of CD4+ T cells; (iii) the control of viremia in macaque 13237 started before CD8+ T cells were detected in the blood or tissues; (iv) the regain of viral control was not accompanied by a boost in the SIV-specific CD8+ T-cell response, and 13523 achieved the fastest and deepest control of infection while maintaining extremely low frequencies of SIV-specific CD8+ T cells; and (v) one animal with an extreme phenotype of control maintained an undetectable viremia despite the absence of CD8+ T cells for more than 3 months.
In conclusion, once control of viremia has been established, other mechanisms, perhaps including control of small viral reservoirs, regulation of T-cell activation, or robust specific CD4+ T-cell responses, may overtake the CD8+ T-cell response, at least partially, to maintain control of the infection in the long term. Future longitudinal studies in CyM exposed to a low-dose viral inoculum may provide information about these mechanisms.
Supplementary Material
ACKNOWLEDGMENTS
This study received financial support from the French National Agency of AIDS and Viral Hepatitis Research (ANRS). C.H. was a Ph.D. student funded by the Université Pierre et Marie Curie and Sidaction.
We thank C. Torres, B. Delache, S. Even, S. Guenounou, and the TIPIV staff at CEA for excellent technical assistance; I. Mangeot-Méderlé, CEA, for helpful project management; and C. Joubert and the animal facility staff of the CEA. We acknowledge A. Aarninck and A. Blancher (University Paul Sabatier, Toulouse, France) for MHC genotyping, A.-L. Bauchet (CEA-Mircen) for support in anatomopathology, and the Center for Human Immunology (CIH) at Institut Pasteur for technical support in conducting this study. We are also indebted to Keith Reimann (Beth Israel Deaconess Medical Center Nonhuman Primate Reagent Resource, Boston, MA, USA) for useful advice about the in vivo use of the CM-T807 monoclonal antibody for CD8 cell depletion.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JVI.03723-14.
REFERENCES
- 1.Saez-Cirion A, Pancino G. 2013. HIV controllers: a genetically determined or inducible phenotype? Immunol Rev 254:281–294. doi: 10.1111/imr.12076. [DOI] [PubMed] [Google Scholar]
- 2.Lambotte O, Boufassa F, Madec Y, Nguyen A, Goujard C, Meyer L, Rouzioux C, Venet A, Delfraissy JF. 2005. HIV controllers: a homogeneous group of HIV-1-infected patients with spontaneous control of viral replication. Clin Infect Dis 41:1053–1056. doi: 10.1086/433188. [DOI] [PubMed] [Google Scholar]
- 3.Deeks SG, Autran B, Berkhout B, Benkirane M, Cairns S, Chomont N, Chun TW, Churchill M, Di Mascio M, Katlama C, Lafeuillade A, Landay A, Lederman M, Lewin SR, Maldarelli F, Margolis D, Markowitz M, Martinez-Picado J, Mullins JI, Mellors J, Moreno S, O'Doherty U, Palmer S, Penicaud MC, Peterlin M, Poli G, Routy JP, Rouzioux C, Silvestri G, Stevenson M, Telenti A, Van Lint C, Verdin E, Woolfrey A, Zaia J, Barre-Sinoussi F. 2012. Towards an HIV cure: a global scientific strategy. Nat Rev Immunol 12:607–614. doi: 10.1038/nri3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blankson JN, Bailey JR, Thayil S, Yang HC, Lassen K, Lai J, Gandhi SK, Siliciano JD, Williams TM, Siliciano RF. 2007. Isolation and characterization of replication-competent human immunodeficiency virus type 1 from a subset of elite suppressors. J Virol 81:2508–2518. doi: 10.1128/JVI.02165-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lamine A, Caumont-Sarcos A, Chaix ML, Saez-Cirion A, Rouzioux C, Delfraissy JF, Pancino G, Lambotte O. 2007. Replication-competent HIV strains infect HIV controllers despite undetectable viremia (ANRS EP36 study). AIDS 21:1043–1045. doi: 10.1097/QAD.0b013e3280d5a7ac. [DOI] [PubMed] [Google Scholar]
- 6.Miura T, Brockman MA, Brumme CJ, Brumme ZL, Carlson JM, Pereyra F, Trocha A, Addo MM, Block BL, Rothchild AC, Baker BM, Flynn T, Schneidewind A, Li B, Wang YE, Heckerman D, Allen TM, Walker BD. 2008. Genetic characterization of human immunodeficiency virus type 1 in elite controllers: lack of gross genetic defects or common amino acid changes. J Virol 82:8422–8430. doi: 10.1128/JVI.00535-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrington M, O'Brien SJ. 2003. The influence of HLA genotype on AIDS. Annu Rev Med 54:535–551. doi: 10.1146/annurev.med.54.101601.152346. [DOI] [PubMed] [Google Scholar]
- 8.Migueles SA, Sabbaghian MS, Shupert WL, Bettinotti MP, Marincola FM, Martino L, Hallahan CW, Selig SM, Schwartz D, Sullivan J, Connors M. 2000. HLA B*5701 is highly associated with restriction of virus replication in a subgroup of HIV-infected long term nonprogressors. Proc Natl Acad Sci U S A 97:2709–2714. doi: 10.1073/pnas.050567397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saez-Cirion A, Lacabaratz C, Lambotte O, Versmisse P, Urrutia A, Boufassa F, Barre-Sinoussi F, Delfraissy JF, Sinet M, Pancino G, Venet A. 2007. HIV controllers exhibit potent CD8 T cell capacity to suppress HIV infection ex vivo and peculiar cytotoxic T lymphocyte activation phenotype. Proc Natl Acad Sci U S A 104:6776–6781. doi: 10.1073/pnas.0611244104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Betts MR, Nason MC, West SM, De Rosa SC, Migueles SA, Abraham J, Lederman MM, Benito JM, Goepfert PA, Connors M, Roederer M, Koup RA. 2006. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 107:4781–4789. doi: 10.1182/blood-2005-12-4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Migueles SA, Laborico AC, Shupert WL, Sabbaghian MS, Rabin R, Hallahan CW, Van Baarle D, Kostense S, Miedema F, McLaughlin M, Ehler L, Metcalf J, Liu S, Connors M. 2002. HIV-specific CD8+ T cell proliferation is coupled to perforin expression and is maintained in nonprogressors. Nat Immunol 3:1061–1068. doi: 10.1038/ni845. [DOI] [PubMed] [Google Scholar]
- 12.Saez-Cirion A, Sinet M, Shin SY, Urrutia A, Versmisse P, Lacabaratz C, Boufassa F, Avettand-Fenoel V, Rouzioux C, Delfraissy JF, Barre-Sinoussi F, Lambotte O, Venet A, Pancino G. 2009. Heterogeneity in HIV suppression by CD8 T cells from HIV controllers: association with Gag-specific CD8 T cell responses. J Immunol 182:7828–7837. doi: 10.4049/jimmunol.0803928. [DOI] [PubMed] [Google Scholar]
- 13.Hersperger AR, Pereyra F, Nason M, Demers K, Sheth P, Shin LY, Kovacs CM, Rodriguez B, Sieg SF, Teixeira-Johnson L, Gudonis D, Goepfert PA, Lederman MM, Frank I, Makedonas G, Kaul R, Walker BD, Betts MR. 2010. Perforin expression directly ex vivo by HIV-specific CD8 T-cells is a correlate of HIV elite control. PLoS Pathog 6:e1000917. doi: 10.1371/journal.ppat.1000917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Migueles SA, Osborne CM, Royce C, Compton AA, Joshi RP, Weeks KA, Rood JE, Berkley AM, Sacha JB, Cogliano-Shutta NA, Lloyd M, Roby G, Kwan R, McLaughlin M, Stallings S, Rehm C, O'Shea MA, Mican J, Packard BZ, Komoriya A, Palmer S, Wiegand AP, Maldarelli F, Coffin JM, Mellors JW, Hallahan CW, Follman DA, Connors M. 2008. Lytic granule loading of CD8+ T cells is required for HIV-infected cell elimination associated with immune control. Immunity 29:1009–1021. doi: 10.1016/j.immuni.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Emu B, Sinclair E, Hatano H, Ferre A, Shacklett B, Martin JN, McCune JM, Deeks SG. 2008. HLA class I-restricted T-cell responses may contribute to the control of human immunodeficiency virus infection, but such responses are not always necessary for long-term virus control. J Virol 82:5398–5407. doi: 10.1128/JVI.02176-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pereyra F, Addo MM, Kaufmann DE, Liu Y, Miura T, Rathod A, Baker B, Trocha A, Rosenberg R, Mackey E, Ueda P, Lu Z, Cohen D, Wrin T, Petropoulos CJ, Rosenberg ES, Walker BD. 2008. Genetic and immunologic heterogeneity among persons who control HIV infection in the absence of therapy. J Infect Dis 197:563–571. doi: 10.1086/526786. [DOI] [PubMed] [Google Scholar]
- 17.Lecuroux C, Saez-Cirion A, Girault I, Versmisse P, Boufassa F, Avettand-Fenoel V, Rouzioux C, Meyer L, Pancino G, Lambotte O, Sinet M, Venet A. 2014. Both HLA-B*57 and plasma HIV RNA levels contribute to the HIV-specific CD8+ T cell response in HIV controllers. J Virol 88:176–187. doi: 10.1128/JVI.02098-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ndhlovu ZM, Proudfoot J, Cesa K, Alvino DM, McMullen A, Vine S, Stampouloglou E, Piechocka-Trocha A, Walker BD, Pereyra F. 2012. Elite controllers with low to absent effector CD8+ T cell responses maintain highly functional, broadly directed central memory responses. J Virol 86:6959–6969. doi: 10.1128/JVI.00531-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shan L, Deng K, Shroff NS, Durand CM, Rabi SA, Yang HC, Zhang H, Margolick JB, Blankson JN, Siliciano RF. 2012. Stimulation of HIV-1-specific cytolytic T lymphocytes facilitates elimination of latent viral reservoir after virus reactivation. Immunity 36:491–501. doi: 10.1016/j.immuni.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Loffredo JT, Maxwell J, Qi Y, Glidden CE, Borchardt GJ, Soma T, Bean AT, Beal DR, Wilson NA, Rehrauer WM, Lifson JD, Carrington M, Watkins DI. 2007. Mamu-B*08-positive macaques control simian immunodeficiency virus replication. J Virol 81:8827–8832. doi: 10.1128/JVI.00895-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandrea I, Gaufin T, Gautam R, Kristoff J, Mandell D, Montefiori D, Keele BF, Ribeiro RM, Veazey RS, Apetrei C. 2011. Functional cure of SIVagm infection in rhesus macaques results in complete recovery of CD4+ T cells and is reverted by CD8+ cell depletion. PLoS Pathog 7:e1002170. doi: 10.1371/journal.ppat.1002170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schultheiss T, Schulte R, Sauermann U, Ibing W, Stahl-Hennig C. 2011. Strong mucosal immune responses in SIV infected macaques contribute to viral control and preserved CD4+ T-cell levels in blood and mucosal tissues. Retrovirology 8:24. doi: 10.1186/1742-4690-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aarnink A, Dereuddre-Bosquet N, Vaslin B, Le Grand R, Winterton P, Apoil PA, Blancher A. 2011. Influence of the MHC genotype on the progression of experimental SIV infection in the Mauritian cynomolgus macaque. Immunogenetics 63:267–274. doi: 10.1007/s00251-010-0504-6. [DOI] [PubMed] [Google Scholar]
- 24.Mee ET, Berry N, Ham C, Sauermann U, Maggiorella MT, Martinon F, Verschoor EJ, Heeney JL, Le Grand R, Titti F, Almond N, Rose NJ. 2009. Mhc haplotype H6 is associated with sustained control of SIVmac251 infection in Mauritian cynomolgus macaques. Immunogenetics 61:327–339. doi: 10.1007/s00251-009-0369-8. [DOI] [PubMed] [Google Scholar]
- 25.Takahashi N, Nomura T, Takahara Y, Yamamoto H, Shiino T, Takeda A, Inoue M, Iida A, Hara H, Shu T, Hasegawa M, Sakawaki H, Miura T, Igarashi T, Koyanagi Y, Naruse TK, Kimura A, Matano T. 2013. A novel protective MHC-I haplotype not associated with dominant Gag-specific CD8+ T-cell responses in SIVmac239 infection of Burmese rhesus macaques. PLoS One 8:e54300. doi: 10.1371/journal.pone.0054300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yant LJ, Friedrich TC, Johnson RC, May GE, Maness NJ, Enz AM, Lifson JD, O'Connor DH, Carrington M, Watkins DI. 2006. The high-frequency major histocompatibility complex class I allele Mamu-B*17 is associated with control of simian immunodeficiency virus SIVmac239 replication. J Virol 80:5074–5077. doi: 10.1128/JVI.80.10.5074-5077.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friedrich TC, Valentine LE, Yant LJ, Rakasz EG, Piaskowski SM, Furlott JR, Weisgrau KL, Burwitz B, May GE, Leon EJ, Soma T, Napoe G, Capuano SV III, Wilson NA, Watkins DI. 2007. Subdominant CD8+ T-cell responses are involved in durable control of AIDS virus replication. J Virol 81:3465–3476. doi: 10.1128/JVI.02392-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mudd PA, Ericsen AJ, Burwitz BJ, Wilson NA, O'Connor DH, Hughes AL, Watkins DI. 2012. Escape from CD8(+) T cell responses in Mamu-B*00801(+) macaques differentiates progressors from elite controllers. J Immunol 188:3364–3370. doi: 10.4049/jimmunol.1102470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shacklett BL, Critchfield JW, Lemongello D. 2009. Isolating mucosal lymphocytes from biopsy tissue for cellular immunology assays. Methods Mol Biol 485:347–356. doi: 10.1007/978-1-59745-170-3_23. [DOI] [PubMed] [Google Scholar]
- 30.Guenounou S, Bosquet N, Dembek CJ, Le Grand R, Cosma A. 2013. OMIP-016: Characterization of antigen-responsive macaque and human T-cells. Cytometry A 83:182–184. doi: 10.1002/cyto.a.22233. [DOI] [PubMed] [Google Scholar]
- 31.Saez-Cirion A, Shin SY, Versmisse P, Barre-Sinoussi F, Pancino G. 2010. Ex vivo T cell-based HIV suppression assay to evaluate HIV-specific CD8+ T-cell responses. Nat Protoc 5:1033–1041. doi: 10.1038/nprot.2010.73. [DOI] [PubMed] [Google Scholar]
- 32.O'Doherty U, Swiggard WJ, Malim MH. 2000. Human immunodeficiency virus type 1 spinoculation enhances infection through virus binding. J Virol 74:10074–10080. doi: 10.1128/JVI.74.21.10074-10080.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karlsson I, Malleret B, Brochard P, Delache B, Calvo J, Le Grand R, Vaslin B. 2007. Dynamics of T-cell responses and memory T cells during primary simian immunodeficiency virus infection in cynomolgus macaques. J Virol 81:13456–13468. doi: 10.1128/JVI.01619-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mannioui A, Bourry O, Sellier P, Delache B, Brochard P, Andrieu T, Vaslin B, Karlsson I, Roques P, Le Grand R. 2009. Dynamics of viral replication in blood and lymphoid tissues during SIVmac251 infection of macaques. Retrovirology 6:106. doi: 10.1186/1742-4690-6-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernard-Stoecklin S, Gommet C, Corneau AB, Guenounou S, Torres C, Dejucq-Rainsford N, Cosma A, Dereuddre-Bosquet N, Le Grand R. 2013. Semen CD4+ T cells and macrophages are productively infected at all stages of SIV infection in macaques. PLoS Pathog 9:e1003810. doi: 10.1371/journal.ppat.1003810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Muthukumar A, Wozniakowski A, Gauduin MC, Paiardini M, McClure HM, Johnson RP, Silvestri G, Sodora DL. 2004. Elevated interleukin-7 levels not sufficient to maintain T-cell homeostasis during simian immunodeficiency virus-induced disease progression. Blood 103:973–979. doi: 10.1182/blood-2003-03-0874. [DOI] [PubMed] [Google Scholar]
- 37.Mueller YM, Do DH, Boyer JD, Kader M, Mattapallil JJ, Lewis MG, Weiner DB, Katsikis PD. 2009. CD8+ cell depletion of SHIV89.6P-infected macaques induces CD4+ T cell proliferation that contributes to increased viral loads. J Immunol 183:5006–5012. doi: 10.4049/jimmunol.0900141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Okoye A, Park H, Rohankhedkar M, Coyne-Johnson L, Lum R, Walker JM, Planer SL, Legasse AW, Sylwester AW, Piatak M Jr, Lifson JD, Sodora DL, Villinger F, Axthelm MK, Schmitz JE, Picker LJ. 2009. Profound CD4+/CCR5+ T cell expansion is induced by CD8+ lymphocyte depletion but does not account for accelerated SIV pathogenesis. J Exp Med 206:1575–1588. doi: 10.1084/jem.20090356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ten Haaft P, Almond N, Biberfeld G, Cafaro A, Cranage M, Ensoli B, Hunsmann G, Polyanskaya N, Stahl-Hennig C, Thortensson R, Titti F, Heeney J. 2001. Comparison of early plasma RNA loads in different macaque species and the impact of different routes of exposure on SIV/SHIV infection. J Med Primatol 30:207–214. doi: 10.1034/j.1600-0684.2001.d01-54.x. [DOI] [PubMed] [Google Scholar]
- 40.Mudd PA, Ericsen AJ, Price AA, Wilson NA, Reimann KA, Watkins DI. 2011. Reduction of CD4+ T cells in vivo does not affect virus load in macaque elite controllers. J Virol 85:7454–7459. doi: 10.1128/JVI.00738-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muhl T, Krawczak M, Ten Haaft P, Hunsmann G, Sauermann U. 2002. MHC class I alleles influence set-point viral load and survival time in simian immunodeficiency virus-infected rhesus monkeys. J Immunol 169:3438–3446. doi: 10.4049/jimmunol.169.6.3438. [DOI] [PubMed] [Google Scholar]
- 42.O'Connor DH, Mothe BR, Weinfurter JT, Fuenger S, Rehrauer WM, Jing P, Rudersdorf RR, Liebl ME, Krebs K, Vasquez J, Dodds E, Loffredo J, Martin S, McDermott AB, Allen TM, Wang C, Doxiadis GG, Montefiori DC, Hughes A, Burton DR, Allison DB, Wolinsky SM, Bontrop R, Picker LJ, Watkins DI. 2003. Major histocompatibility complex class I alleles associated with slow simian immunodeficiency virus disease progression bind epitopes recognized by dominant acute-phase cytotoxic-T-lymphocyte responses. J Virol 77:9029–9040. doi: 10.1128/JVI.77.16.9029-9040.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greenier JL, Miller CJ, Lu D, Dailey PJ, Lu FX, Kunstman KJ, Wolinsky SM, Marthas ML. 2001. Route of simian immunodeficiency virus inoculation determines the complexity but not the identity of viral variant populations that infect rhesus macaques. J Virol 75:3753–3765. doi: 10.1128/JVI.75.8.3753-3765.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu J, Keele BF, Li H, Keating S, Norris PJ, Carville A, Mansfield KG, Tomaras GD, Haynes BF, Kolodkin-Gal D, Letvin NL, Hahn BH, Shaw GM, Barouch DH. 2010. Low-dose mucosal simian immunodeficiency virus infection restricts early replication kinetics and transmitted virus variants in rhesus monkeys. J Virol 84:10406–10412. doi: 10.1128/JVI.01155-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Durudas A, Chen HL, Gasper MA, Sundaravaradan V, Milush JM, Silvestri G, Johnson W, Giavedoni LD, Sodora DL. 2011. Differential innate immune responses to low or high dose oral SIV challenge in Rhesus macaques. Curr HIV Res 9:276–288. doi: 10.2174/157016211797635928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ferre AL, Hunt PW, Critchfield JW, Young DH, Morris MM, Garcia JC, Pollard RB, Yee HF Jr, Martin JN, Deeks SG, Shacklett BL. 2009. Mucosal immune responses to HIV-1 in elite controllers: a potential correlate of immune control. Blood 113:3978–3989. doi: 10.1182/blood-2008-10-182709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gulzar N, Copeland KF. 2004. CD8+ T-cells: function and response to HIV infection. Curr HIV Res 2:23–37. doi: 10.2174/1570162043485077. [DOI] [PubMed] [Google Scholar]
- 48.Bosinger SE, Jochems SP, Folkner KA, Hayes TL, Klatt NR, Silvestri G. 2013. Transcriptional profiling of experimental CD8(+) lymphocyte depletion in rhesus macaques infected with simian immunodeficiency virus SIVmac239. J Virol 87:433–443. doi: 10.1128/JVI.01746-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klatt NR, Shudo E, Ortiz AM, Engram JC, Paiardini M, Lawson B, Miller MD, Else J, Pandrea I, Estes JD, Apetrei C, Schmitz JE, Ribeiro RM, Perelson AS, Silvestri G. 2010. CD8+ lymphocytes control viral replication in SIVmac239-infected rhesus macaques without decreasing the lifespan of productively infected cells. PLoS Pathog 6:e1000747. doi: 10.1371/journal.ppat.1000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dioszeghy V, Benlhassan-Chahour K, Delache B, Dereuddre-Bosquet N, Aubenque C, Gras G, Le Grand R, Vaslin B. 2006. Changes in soluble factor-mediated CD8+ cell-derived antiviral activity in cynomolgus macaques infected with simian immunodeficiency virus SIVmac251: relationship to biological markers of progression. J Virol 80:236–245. doi: 10.1128/JVI.80.1.236-245.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Swain SL, McKinstry KK, Strutt TM. 2012. Expanding roles for CD4(+) T cells in immunity to viruses. Nat Rev Immunol 12:136–148. doi: 10.1038/nri3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sacha JB, Giraldo-Vela JP, Buechler MB, Martins MA, Maness NJ, Chung C, Wallace LT, Leon EJ, Friedrich TC, Wilson NA, Hiraoka A, Watkins DI. 2009. Gag- and Nef-specific CD4+ T cells recognize and inhibit SIV replication in infected macrophages early after infection. Proc Natl Acad Sci U S A 106:9791–9796. doi: 10.1073/pnas.0813106106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Soghoian DZ, Jessen H, Flanders M, Sierra-Davidson K, Cutler S, Pertel T, Ranasinghe S, Lindqvist M, Davis I, Lane K, Rychert J, Rosenberg ES, Piechocka-Trocha A, Brass AL, Brenchley JM, Walker BD, Streeck H. 2012. HIV-specific cytolytic CD4 T cell responses during acute HIV infection predict disease outcome. Sci Transl Med 4:123ra25. doi: 10.1126/scitranslmed.3003165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zheng N, Fujiwara M, Ueno T, Oka S, Takiguchi M. 2009. Strong ability of Nef-specific CD4+ cytotoxic T cells to suppress human immunodeficiency virus type 1 (HIV-1) replication in HIV-1-infected CD4+ T cells and macrophages. J Virol 83:7668–7677. doi: 10.1128/JVI.00513-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jin X, Bauer DE, Tuttleton SE, Lewin S, Gettie A, Blanchard J, Irwin CE, Safrit JT, Mittler J, Weinberger L, Kostrikis LG, Zhang L, Perelson AS, Ho DD. 1999. Dramatic rise in plasma viremia after CD8(+) T cell depletion in simian immunodeficiency virus-infected macaques. J Exp Med 189:991–998. doi: 10.1084/jem.189.6.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leone A, Picker LJ, Sodora DL. 2009. IL-2, IL-7 and IL-15 as immuno-modulators during SIV/HIV vaccination and treatment. Curr HIV Res 7:83–90. doi: 10.2174/157016209787048519. [DOI] [PubMed] [Google Scholar]
- 57.Ducrey-Rundquist O, Guyader M, Trono D. 2002. Modalities of interleukin-7-induced human immunodeficiency virus permissiveness in quiescent T lymphocytes. J Virol 76:9103–9111. doi: 10.1128/JVI.76.18.9103-9111.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Unutmaz D, KewalRamani VN, Marmon S, Littman DR. 1999. Cytokine signals are sufficient for HIV-1 infection of resting human T lymphocytes. J Exp Med 189:1735–1746. doi: 10.1084/jem.189.11.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Al-Harthi L, Roebuck KA, Landay A. 1998. Induction of HIV-1 replication by type 1-like cytokines, interleukin (IL)-12 and IL-15: effect on viral transcriptional activation, cellular proliferation, and endogenous cytokine production. J Clin Immunol 18:124–131. doi: 10.1023/A:1023246800353. [DOI] [PubMed] [Google Scholar]
- 60.Smithgall MD, Wong JG, Critchett KE, Haffar OK. 1996. IL-7 up-regulates HIV-1 replication in naturally infected peripheral blood mononuclear cells. J Immunol 156:2324–2330. [PubMed] [Google Scholar]
- 61.McChesney MB, Collins JR, Lu D, Lu X, Torten J, Ashley RL, Cloyd MW, Miller CJ. 1998. Occult systemic infection and persistent simian immunodeficiency virus (SIV)-specific CD4(+)-T-cell proliferative responses in rhesus macaques that were transiently viremic after intravaginal inoculation of SIV. J Virol 72:10029–10035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhu T, Hu SL, Feng F, Polacino P, Liu H, Hwangbo Y, Learn GH, Mullins JI, Corey L. 2004. Persistence of low levels of simian immunodeficiency virus in macaques that were transiently viremic by conventional testing. Virology 323:208–219. doi: 10.1016/j.virol.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 63.Delwart E, Bernardin F, Lee TH, Winkelman V, Liu C, Sheppard H, Liu A, Greenblatt R, Anastos K, DeHovitz J, Nowicki M, Cohen M, Golub ET, Barbour J, Buchbinder S, Busch MP. 2011. Absence of reproducibly detectable low-level HIV viremia in highly exposed seronegative men and women. AIDS 25:619–623. doi: 10.1097/QAD.0b013e3283440269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sahu GK, McNearney T, Evans A, Turner A, Weaver S, Huang JC, Baron S, Paar D, Cloyd MW. 2005. Transient or occult HIV infections may occur more frequently than progressive infections: changing the paradigm about HIV persistence. Arch Virol Suppl 19:131–145. doi: 10.1007/3-211-29981-5_11. [DOI] [PubMed] [Google Scholar]
- 65.Zhu T, Corey L, Hwangbo Y, Lee JM, Learn GH, Mullins JI, McElrath MJ. 2003. Persistence of extraordinarily low levels of genetically homogeneous human immunodeficiency virus type 1 in exposed seronegative individuals. J Virol 77:6108–6116. doi: 10.1128/JVI.77.11.6108-6116.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.