ABSTRACT
Herpes simplex virus 1 (HSV-1) glycoprotein B (gB)-specific CD8+ T cells protect mice from herpes infection and disease. However, whether and which HSV-1 gB-specific CD8+ T cells play a key role in the “natural” protection seen in HSV-1-seropositive healthy asymptomatic (ASYMP) individuals (who have never had clinical herpes disease) remain to be determined. In this study, we have dissected the phenotypes and the functions of HSV-1 gB-specific CD8+ T cells from HLA-A*02:01 positive, HSV-1 seropositive ASYMP and symptomatic (SYMP) individuals (with a history of numerous episodes of recurrent ocular herpes disease). We found the following. (i) Healthy ASYMP individuals maintained a significantly higher proportion of differentiated HSV-1 gB-specific effector memory CD8+ T cells (TEM cells) (CD45RAlow CCR7low CD44high CD62Llow). In contrast, SYMP patients had frequent less-differentiated central memory CD8+ T cells (TCM cells) (CD45RAlow CCR7high CD44low CD62Lhigh). (ii) ASYMP individuals had significantly higher proportions of multifunctional effector CD8+ T cells which responded mainly to gB342–350 and gB561–569 “ASYMP” epitopes, and simultaneously produced IFN-γ, CD107a/b, granzyme B, and perforin. In contrast, effector CD8+ T cells from SYMP individuals were mostly monofunctional and were directed mainly against nonoverlapping gB17–25 and gB183–191 “SYMP” epitopes. (iii) Immunization of an HLA-A*02:01 transgenic mouse model of ocular herpes with “ASYMP” CD8+ TEM cell epitopes, but not with “SYMP” CD8+ TCM cell epitopes, induced a strong CD8+ T cell-dependent protective immunity against ocular herpes infection and disease. Our findings provide insights into the role of HSV-specific CD8+ TEM cells in protection against herpes and should be considered in the development of an effective vaccine.
IMPORTANCE A significantly higher proportion of differentiated and multifunctional HSV-1 gB-specific effector memory CD8+ T cells (TEM cells) (CD45RAlow CCR7low CD44high CD62Llow) were found in healthy ASYMP individuals who are seropositive for HSV-1 but never had any recurrent herpetic disease, while there were frequent less-differentiated and monofunctional central memory CD8+ T cells (TCM cells) (CD45RAlow CCR7high CD44low CD62Lhigh) in SYMP patients. Immunization with “ASYMP” CD8+ TEM cell epitopes, but not with “SYMP” CD8+ TCM cell epitopes, induced a strong protective HSV-specific CD8+ T cell response in HLA-A*02:01 transgenic mice. These findings are important for the development of a safe and effective T cell-based herpes vaccine.
INTRODUCTION
Over a billion individuals worldwide carry herpes simplex virus 1 (HSV-1), which causes a wide range of mild to life-threatening diseases (1–3). Although the virus reactivates from latency and is shed multiple times each year in body fluids (i.e., tears, saliva, and nasal and vaginal secretions), most reactivations are subclinical due to an efficient immune-mediated containment of the infection and disease (4–7). Thus, most infected individuals are asymptomatic (ASYMP) and do not present any apparent recurrent herpetic disease (e.g., cold sores, genital, or ocular herpetic disease). However, a small proportion of individuals experience endless recurrences of herpetic disease, usually multiple times a year, often necessitating continuous antiviral therapy (i.e., with acyclovir and derivatives) (8, 9). In those symptomatic (SYMP) individuals, HSV-1 frequently reactivates from latency, reinfects the eyes, and may trigger recurrent and severe corneal herpetic disease, a leading cause of infectious corneal blindness in the industrialized world (10–12). In the United States, up to 450,000 individuals have a history of recurrent herpetic stromal keratitis (HSK), a T cell-mediated immunopathological lesion of the cornea (10–12). Thus, a better understanding of the immune mechanisms that protect against HSV-1 infection and disease is highly desirable for the development of more efficacious vaccines and immunotherapies to reduce HSV-1-related diseases.
In animal models of herpes infection and disease, HSV-specific CD8+ T cells play a critical role in aborting attempts of virus reactivation from latency and in clearing herpetic disease (3, 5, 13–16). However, herpetic corneal disease is also associated with HSV-specific CD8+ T cell responses (17, 18). While the HSV-1 glycoprotein B (gB) is a major target of CD8+ T cells in seropositive ASYMP individuals (7, 19), it produced only a transient protective immunity in vaccine clinical trials (12, 20, 21). In B6 mice, an immunodominant CD8+ T cell epitope, gB498–505, achieved at least partial protection against herpes infection and disease (8, 12, 22, 23). Considering the wealth of data addressing the phenotype and function of HSV-1 gB498–505 epitope-specific CD8+ T cells in mice (4–6, 24, 25), it is surprising how few reports exist characterizing the phenotype and function of human epitope-specific “protective” CD8+ T cells from HSV-seropositive healthy ASYMP individuals, who appear to have acquired a “natural” protection (13, 26). This information is necessary for the successful design of an effective T cell-based therapeutic vaccine strategy.
While memory CD8+ T cell subpopulations are heterogeneous in terms of phenotype, function, and anatomical distribution, they can generally be divided into two major subsets: effector memory CD8+ T cells (TEM cells) and central memory CD8+ T cells (TCM cells) (26, 27). The different characteristics of TCM and TEM cells suggest that they play different roles in recall responses and containment of herpes infection and disease (26, 28–30). We hypothesize that ASYMP individuals develop more of the protective HSV-specific CD8+ TEM cells, while SYMP patients develop more of the nonprotective (or maybe pathogenic) HSV-specific CD8+ TCM cells (31, 32).
In this study, we found two distinct phenotypic and functional patterns of protective and nonprotective HSV-1 gB-specific CD8+ T cells that are associated with ASYMP versus SYMP ocular herpes, respectively. A significantly higher proportion of differentiated HSV-1 gB-specific CD45RAlow CCR7low CD44high CD62Llow CD8+ TEM cells were detected in ASYMP individuals. In contrast, a significantly higher proportion of less-differentiated HSV-1 gB-specific CD45RAlow CCR7high CD44low CD62Lhigh CD8+ TCM cells were detected in SYMP patients. Moreover, the HLA-A*02:01-restricted ASYMP HSV-1 gB epitopes, which specifically recalled polyfunctional CD8+ TEM cell responses in HLA-A*02:01-positive ASYMP individuals, induced a CD8+ T cell-dependent protective immunity against ocular herpes infection and disease in “humanized” HLA-A*02:01 transgenic (Tg) mice. In contrast, HLA-A*02:01-restricted SYMP gB epitopes, which tended to recall more monofunctional CD8+ TCM cell responses in HLA-A*02:01-positive SYMP patients, were unable to protect HLA-A*02:01 Tg mice from ocular herpes.
Our findings delineate the quantitative and qualitative features of a protective HSV-specific CD8+ T cell response that should be taken into consideration during herpes vaccine development.
MATERIALS AND METHODS
Human study population.
During the last decade (i.e., January 2003 to August 2014), we have screened 693 individuals for HSV-1 and HSV-2 seropositivity (Table 1). Four hundred eighty-eight individuals were white, 205 were nonwhite (African, Asian, Hispanic, and others), 355 were females, and 338 were males. Among these, a cohort of 261 immunocompetent individuals, with an age range of 18 to 65 (median, 32) and who were seropositive for HSV-1 and seronegative for HSV-2, were enrolled in the present study. All patients were negative for HIV and hepatitis B virus (HBV) and had no history of immunodeficiency. Six hundred seven patients were HSV-1, HSV-2, or HSV-1/HSV-2 seropositive, among whom 575 patients were healthy and ASYMP (individuals who, in the absence of therapy, have never had any recurrent herpes disease [ocular, genital, or elsewhere], based on their self-report and physician examination; even a single episode of any herpetic disease in his or her life span will exclude the individual from this group). The remaining 32 patients were defined as HSV-seropositive symptomatic patients and had frequent and severe recurrent genital, ocular, and/or oro-facial lesions, with two patients having had clinically well-documented repetitive herpes stromal keratitis (HSK) including one patient with ∼20 episodes over 20 years that necessitated several corneal transplantations.
TABLE 1.
Cohorts of HLA-A*02:01-positive, HSV-seropositive symptomatic and asymptomatic individuals enrolled in the study
| Subject-level characteristic | Value for subjects (n = 693) |
|---|---|
| Gender, no. (%) | |
| Female | 355 (52) |
| Male | 338 (48) |
| Race, no. (%) | |
| White | 488 (71) |
| Nonwhite | 205 (29) |
| Median age, yr (range) | 32 (18–65) |
| HSV status, no. (%) | |
| HSV-1 positive | 261 (38) |
| HSV-2 positive | 323 (46) |
| HSV-1 and -2 positive | 23 (3) |
| HSV negative | 86 (12) |
| HLA-A*02:01, no. (%) | |
| Positive | 363 (52) |
| Negative | 330 (48) |
| Herpes disease status, no. (%) | |
| Asymptomatic | 575 (94) |
| Symptomatic | 32 (6) |
Signs of recurrent disease in SYMP patients were defined as herpetic lid lesions, herpetic conjunctivitis, dendritic or geographic keratitis, stromal keratitis, and iritis consistent with HSK, with one or more episodes per year for the past 2 years. However, at the time of blood collection, SYMP patients had no recurrent disease (other than corneal scarring) and had had no recurrences during the past 30 days. They had no ocular disease other than HSK, had no history of recurrent genital herpes, and were HSV-1 seropositive and HSV-2 seronegative. Because the spectrum of recurrent ocular herpetic disease is wide, our emphasis is mainly on the number of recurrent episodes and not on the severity of the recurrent disease. No attempt was made to assign specific T cell epitopes to specific severity of recurrent lesions. Patients were also excluded if they (i) had an active ocular (or elsewhere) herpetic lesion or one in the past 30 days, (ii) were seropositive for HSV-2, (iii) were pregnant or breastfeeding, or (iv) were on acyclovir or other related antiviral drugs or any immunosuppressive drugs at time of blood draw. SYMP and ASYMP groups were matched for age, gender, serological status, and race. Eighty-six healthy control individuals were seronegative for both HSV-1 and HSV-2 and had no history of ocular herpes, genital lesions, or oro-facial herpes disease. All subjects were enrolled at the University of California, Irvine (UCI), under Institutional Review Board-approved protocols (IRB number 2003-3111 and IRB number 2009-6963). Written informed consent was received from all participants prior to inclusion in the study.
HLA typing.
HLA-A2 subtyping was performed using a commercial sequence-specific primer (SSP) kit and following the manufacturer's instructions (SSPR1-A2; One Lambda, Canoga Park, CA). Briefly, genomic DNA extracted from peripheral blood mononuclear cells (PBMC) of HSV-seropositive SYMP and ASYMP individuals was analyzed using a Tecan DNA workstation from a 96-well plate with a 2-μl volume per well, as we previously described (13). The yield and purity of each DNA sample were tested using a UV spectrophotometer. The integrity of DNA samples was ascertained by electrophoresis on agarose gels. Each DNA sample was then subjected to multiple small-volume PCRs using primers specific to areas of the genome surrounding the single point mutations associated with each allele. Only primers that matched the specific sequence of a particular allele would amplify a product. The PCR products were subsequently electrophoresed on a 2.5% agarose gel with ethidium bromide, and the pattern of amplicon generation was analyzed using HLA Fusion software (One Lambda, Inc., Canoga Park, CA). In addition, the HLA-A2 status was confirmed by staining PBMC with anti-HLA-A2 monoclonal antibody (MAb) BB7.2 (BD Pharmingen, USA) at 4°C for 30 min. The cells were washed, acquired on a BD LSR II, and analyzed using FlowJo software version 9.7.5 (TreeStar).
PBMC isolation.
Individuals (negative for HIV and HBV and with or without any HSV infection history) were recruited at the Gavin Herbert Eye Institute and the UCI Institute for Clinical and Translational Science (ICTS). Between 40 and 100 ml of blood was drawn into yellow-top Vacutainer tubes (Becton Dickinson, USA). The serum was isolated and stored at −80°C for detection of anti-HSV-1 and -HSV-2 antibodies, as we previously described (9). PBMC were isolated by gradient centrifugation using leukocyte separation medium (Cellgro, USA). The cells were washed in phosphate-buffered saline (PBS) and resuspended in complete culture medium consisting of RPMI 1640 and 10% fetal bovine serum (FBS) (Bio-Products, Woodland, CA, USA) supplemented with 1× penicillin–l-glutamine–streptomycin, 1× sodium pyruvate, 1× nonessential amino acids, and 50 μM 2-mercaptoethanol (Life Technologies, Rockville, MD, USA). Freshly isolated PBMC were also cryopreserved in 90% fetal calf serum (FCS) and 10% dimethyl sulfoxide (DMSO) in liquid nitrogen for future testing.
Flow cytometry analysis.
PBMC were analyzed by flow cytometry after staining with fluorochrome-conjugated human- and mouse-specific monoclonal antibodies (MAbs). The following anti-human antibodies were used: CD3 (clone SK7)–phycoerythrin (PE)-Cy7, CD44 (clone G44-26) A700, CD8 (clone SK1)–allophycocyanin (APC)-Cy7, CCR7 (clone 150503)-Alexa Fluor 700, CD45RO–PE-Cy5, CD45RA-fluorescein isothiocyanate (FITC), CD62L-APC, gamma interferon (IFN-γ)-Alexa Fluor 647, and T-bet (clone O4-46)-Alexa Fluor 488 (BD Pharmingen); granzyme B (GzmB) (clone GB11)-A647, CD107a (clone H4A3)-FITC, and CD107b (clone H4B4)-FITC (BioLegend); and Ki-67 (clone 20Raj1)–PE-Cy7, Granzyme K (clone G3H69)-peridinin chlorophyll protein (PerCP) eFluor 710, perforin (clone d69)-FITC, and Eomes (clone WD1928) eFluor 660 (eBioscience). Cell surface staining was used for CD107a/b. The following anti-mouse antibodies were used: CD8 (clone 53-6.7)–PE-Cy7, CD44 (clone IM7)–APC-Cy7, and CD62L (MEL-14)-A700 (BD Pharmingen).
For surface staining, MAbs against various cell markers were added to a total of 1 × 106 PBMC in phosphate-buffered saline containing 1% FBS and 0.1% sodium azide (fluorescence-activated cell sorter [FACS] buffer) and left for 45 min at 4°C. After washing with FACS buffer, cells were permeabilized for 20 min on ice using the Cytofix/Cytoperm kit (BD Biosciences) and then washed twice with Perm/Wash buffer (BD Bioscience). Intracellular cytokine/intranuclear transcription factor-staining MAbs were then added to the cells and incubated for 45 min on ice in the dark. Cells were washed again with Perm/Wash and FACS buffer and fixed in PBS containing 2% paraformaldehyde (Sigma-Aldrich, St. Louis, MO). For each sample, 200,000 total events were acquired on a BD LSRII. Antibody capture beads (BD Biosciences) were used as individual compensation tubes for each fluorophore in the experiment. To define positive and negative populations, we employed fluorescence-minus controls for each fluorophore used in this study, when initially developing staining protocols. In addition, we further optimized gating by examining known negative cell populations for background level expression. The gating strategy was similar to that used in our previous work (6). Briefly, we gated on single cells, dump− cells, viable cells (Aqua Blue), lymphocytes, CD3+ cells, and CD8+ cells before finally gating human epitope-specific CD8+ T cells using gB epitope-specific tetramers. The gB tetramers were prepared and provided by the NIH Tetramer Core Facility, Emory University, Atlanta, GA. Briefly, tetramers, were linked to streptavidin-PE (PJRS25; Prozyme) and adjusted to a concentration of 1 mg/ml. At a 1:1 ratio of streptavidin to phycobiliprotein, the addition of streptavidin to the biotinylated monomers was performed at room temperature. Data analysis was performed using FlowJo version 9.7.5 (TreeStar, Ashland, OR). Statistical analyses were done using GraphPad Prism version 5 (GraphPad, La Jolla, CA).
mRNA isolation and real-time reverse transcription-PCR (RT-PCR) analysis.
Total RNA was isolated from fresh PBMC using the Direct-zol RNA MiniPrep kit (Zymo Research) and reverse transcribed with a high-capacity cDNA reverse transcription kit (Applied Biosystems) according to the manufacturer's instructions. Quantitative real-time PCR was carried out on a Rotor-Gene 3000 (Corbett Research) using the LightCycler 480 SYBR green 1 Master (Roche). The data were normalized to GAPDH (glyceraldehyde-3-phosphate dehydrogenase) for transcription factor analysis. Relative mRNA expression levels were calculated using the following formula, and data are expressed as fold increase:
CD107 cytotoxicity assay.
To detect gB-specific cytolytic CD8+ T cells in PBMC, an intracellular CD107a/b cytotoxicity assay was performed as described by Betts et al. (33) with a few modifications. Briefly, 1 × 106 PBMC from patients were transferred into 96-well flat bottom plates and stimulated with immunodominant and subdominant gB peptide epitopes (10 μg/ml in 200 μl complete culture medium) in the presence of anti-CD107a-FITC, CD107b-FITC, and BD Golgi stop (10 μg/ml) for 6 h at 37°C. Phytohemagglutinin (PHA) (10 μg/ml) (Sigma) and no peptide were used as positive and negative controls, respectively. At the end of the incubation period, the cells were transferred to a 96-well round bottom plate and washed once with FACS buffer. Surface staining and intracellular staining were done as described above.
Virus production.
HSV-1 (strain McKrae) was grown and titrated on RS (rabbit skin) cells. UV-inactivated HSV-1 was generated as we previously described (4). HSV inactivation was confirmed by the inability to produce plaques when tested on RS cells.
Immunization of HLA transgenic mice with SYMP and ASYMP epitope peptides, virus challenge and monitoring of ocular infection and disease.
HLA-A*02:01 transgenic mice, previously described (34–36), were kindly provided by Francois Lemonier (Pasteur Institute, Paris, France) and were bred at UCI. These mice represent the F1 generation resulting from a cross between HLA-A*02:01/Kb transgenic mice (expressing a chimeric gene consisting of the 1 and 2 domains of HLA-A*02:01 and the 3 domain of H-2Kb) created on the BALB/c genetic background. The genotype of the HLA transgenic mice used in this study was confirmed as HLA-A*02:01, the most common A*02 subtype, supporting that the immunogenic SYMP versus ASYM peptide epitopes reported here are likely presented by the HLA-A*02:01 molecule. All animal studies were conducted in facilities approved by the Association for Assessment and Accreditation of Laboratory Animal Care and according to Institutional Animal Care and Use Committee-approved animal protocols (IACUC number 2002-2372). Age-matched female HLA-A*0201 transgenic mice (n = 10) were immunized on day 0 and day 21 with either SYMP or ASYMP CD8+ T cell epitopes mixed with CD4+ T-helper PADRE epitope, as we described previously (34, 35). All immunizations were carried out using 100 μM each peptide epitope. After 2 weeks, mice were then challenged ocularly with 2 × 105 PFU of HSV-1 (strain McKrae).
Monitoring of ocular herpes infection and disease.
Animals were examined for signs of ocular disease by slit lamp. Clinical assessments were made immediately before inoculation and on days 1, 4, 7, 10, 14, and 21 thereafter. The examination was performed by investigators blinded to the treatment regimen of the mice and scored according to a standard scale of 0 to 4, as previously described (3): 0, no disease; 1, 25% staining; 2, 50% staining; 3, 75% staining; and 4, 100% staining. Mice were segregated into two groups based on eye disease: ASYMP (without any ocular disease) and SYMP (with ocular disease). To quantify replication and clearance of HSV-1 from the eyes, mice were swabbed daily with moist type 1 calcium alginate swabs. Swabs were placed in 1.0 ml titration medium (media 199, 2% penicillin-streptomycin, 2% newborn calf serum) and frozen at −80°C until titrated on RS cell monolayers as described previously (3). Mice were also examined for survival in a window of 30 days after challenge, as we previously described (3).
Statistical analyses.
Data for each assay were compared by analysis of variance (ANOVA) and Student's t test using GraphPad Prism 5 software (GraphPad, La Jolla, CA). Differences between the groups were identified by ANOVA and multiple-comparison procedures, as we previously described (37). Data are expressed as the mean ± standard deviation (SD). Results were considered statistically significant at a P value of <0.05.
RESULTS
HSV-seropositive symptomatic and asymptomatic individuals have different frequencies of CD8+ T cells specific to some HSV-1 gB epitopes.
The characteristics of the symptomatic (SYMP) and asymptomatic (ASYMP) study populations used in the present study, with respect to gender, age, HLA-A*02:01 frequency distribution, HSV-1/HSV-2 seropositivity, and status of ocular herpetic disease are presented in Table 1 and detailed in Materials and Methods. Since HSV-1 is the main cause of ocular herpes, only individuals who were HSV-1 seropositive and HSV-2 seronegative were enrolled in the present study. The HSV-1-seropositive individuals were segregated into two groups: (i) 10 HLA-A*02:01-positive, HSV-1-infected ASYMP individuals who have never had any clinically detectable herpes disease and (ii) 10 HLA-A*02:01-positive HSV-1-infected SYMP individuals with a history of numerous episodes of well-documented recurrent clinical herpes diseases, such as herpetic lid lesions, herpetic conjunctivitis, dendritic or geographic keratitis, stromal keratitis, and iritis consistent with recurrent HSK, with 1 or more episodes per year for the past 2 years. One patient had over 20 severe recurrent episodes during the last 20 years that necessitated multiple corneal transplantations. Only SYMP patients who were not on acyclovir or other antiviral or anti-inflammatory drug treatments at the time of blood sample collections were enrolled.
To identify potential HLA-A*02:01-binding epitopes from HSV-1 gB, we previously searched the deduced HSV-1 (strain 17) gB amino acid sequence using the BIMAS, SYFPEITHI, and MAPPP predictive computational algorithms (Table 2) (13). Based on these analyses, we selected and synthesized 10 potential gB peptide epitopes with high predicted affinity to HLA-A*02:01, a haplotype that is represented in over 50% of the world's population, irrespective of gender and ethnicity (3, 5, 13). Tetramers specific to each of the 10 HLA-A*02:01-restricted CD8+ T cell epitopes were constructed.
TABLE 2.
Potential HLA-A*02:01-restricted epitopes selected from herpes simplex virus glycoprotein Ba
| Peptide | Sequenceb | Mol wt | No. of amino acids | Predicted binding affinity as calculated byc: |
|||
|---|---|---|---|---|---|---|---|
| BIMAS | SYFPEITHI | MAPPP | MHCPred | ||||
| gB17–25 | ALLGLTLGV | 856.0 | 9 | 257.342 | 31 | 0.5241 | 0.27 |
| gB161–169 | TMYYKDVTV | 1,119.3 | 9 | 160.742 | 23 | 0.8421 | 0.34 |
| gB183–191 | GIFEDRAPV | 1,003.1 | 9 | 145.077 | 24 | 0.5003 | 0.24 |
| gB286–294 | FVLATGDFV | 968.1 | 9 | 279.149 | 17 | 0.09 | |
| gB342–350 | NLLTTPKFT | 1,034.2 | 9 | 151.648 | 15 | ||
| gB343–351 | LLTTPKFTV | 1,019.2 | 9 | 685.783 | 24 | 1 | 0.19 |
| gB441–449 | YLANGGFLI | 967.1 | 9 | 278.347 | 24 | 0.2 | |
| gB447–455 | FLIAYQPLL | 1,077.3 | 9 | 98.267 | 25 | 0.8300 | 0.4 |
| gB561–569 | RMLGDVMAV | 991.2 | 9 | 427.474 | 27 | 0.7222 | 0.37 |
| gB675–683 | TMLEDHEFV | 1,120.2 | 9 | 2,053.642 | 22 | 0.9942 | 0.19 |
The sequence of HSV-1 glycoprotein B was submitted for screening of potential HLA-A*02:01 epitopes using several computer algorithms. Ten peptides selected on the basis of the HLA-A*02:01-binding motif sequence from HSV-1 gB.
The sequences of synthesized peptides are based on the HSV-1 strain 17. Sequences of immunodominant HLA-A02:01-restricted peptides are in bold.
BIMAS, http://www-bimas.cit.nih.gov/molbio/hla_bind; SYFPEITHI, http://www.syfpeithi.de ; MAPPP: http://www.mpiib-berlin.mpg.de/MAPPP; MHCPred, http://www.mhc-pathway.net.
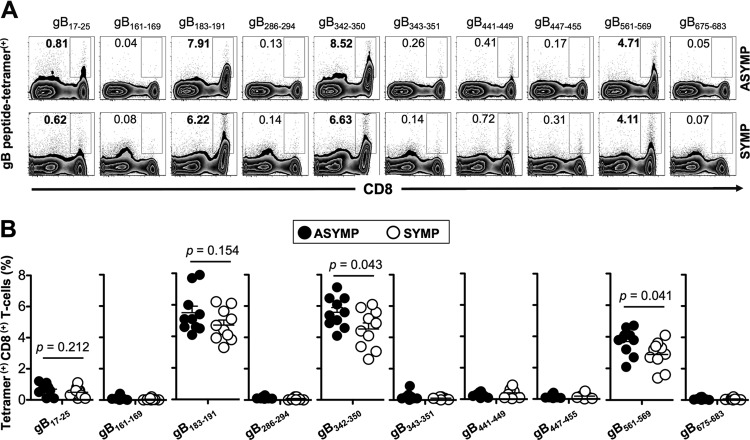
We subsequently compared the frequencies of CD8+ T cells specific to each gB epitope, using HLA-A*02:01-specific tetramers/anti-CD8 MAbs, in the peripheral blood of 10 HLA-A*02:01-positive, HSV-1-seropositive ASYMP and 10 HLA-A*02:01-positive, HSV-1-seropositive SYMP individuals, as described above (Fig. 1). The low frequencies of PBMC-derived HSV-specific CD8+ T cells complicate a direct ex vivo detection with tetramers using a typical number of PBMC (∼106 cells), and a prior expansion of CD8+ T cells by HSV-1 or peptide stimulation in an in vitro culture will hamper a reliable determination of the frequency, phenotype, and function of epitope-specific CD8+ T cells. We therefore opted to measure the frequencies of gB epitope-specific CD8+ T cells ex vivo using a large number of PBMC (∼10 × 106) per tetramer/CD8 MAb panel. The representative dot plots shown in Fig. 1A indicate overall similar frequencies of CD8+ T cells specific to two immunodominant (gB183–191 and gB342–350) and two subdominant (gB17–25 and gB561–569) epitopes detected in one ASYMP individual (top row) and one SYMP individual (bottom row). Figure 1B shows median frequencies detected in 10 SYMP and 10 ASYMP individuals. The highest and most significant frequencies of gB peptide tetramer-positive CD8+ T cells that were consistently detected in both SYMP and ASYMP individuals were recorded for 3 out of 10 gB peptide epitopes: gB183–191, gB342–350, and gB561–569 (4.11% to 8.52%). The frequencies of CD8+ T cells specific to the gB183–191 epitope were similar in SYMP and ASYMP individuals (P = 0.154), while frequencies of CD8+ T cells recorded for gB342–350 and gB561–569 were slightly higher in ASYMP than in SYMP individuals (P = 0.043 and P = 0.041, respectively). Low frequencies of CD8+ T cells against the gB17–25 subdominant epitope were detected in both SYMP and ASYMP individuals. Despite repeated attempts, with and without in vitro expansions, the remaining six gB peptide/HLA-A*02:01 tetramers consistently detected nonsignificant frequencies of CD8+ T cells in both SYMP and ASYMP individuals. We next determined whether there are any differences in the phenotype and function of gB epitope-specific effector and memory CD8+ T cells between SYMP and ASYMP individuals.
FIG 1.
Similar frequencies of CD8+ T cells specific to gB17–25, gB183–191, gB342–350, and gB561–569 epitopes detected in HLA-A*02:01-positive, HSV-seropositive SYMP and ASYMP individuals. PBMC (∼107) derived from ASYMP and SYMP individuals were analyzed ex vivo by FACS for the frequency of gB epitope-specific CD8+ T cells using tetramer complexes representing each of the 10 potential gB epitopes shown in Table 2. (A) Representative FACS data of the frequencies of CD8+ T cells in one HSV-1-seropositive ASYMP individual (upper panels) and one SYMP individual (lower panels) specific to the indicated epitope. (B) Average frequencies of PBMC-derived CD8+ T cells, specific to each of the indicated gB epitopes, from 10 HLA-A*02:01-positive, HSV-1-seropositive ASYMP individuals compared to 10 HLA-A*02:01-positive, HSV-seropositive SYMP individuals. The indicated P values, calculated using one-way ANOVA, show statistical significance of differences between SYMP and ASYMP individuals.
Asymptomatic individuals have a higher frequency of HSV-1 gB epitope-specific CD8+ TEM cells, while symptomatic individuals have a higher frequency of CD8+ TCM cells.
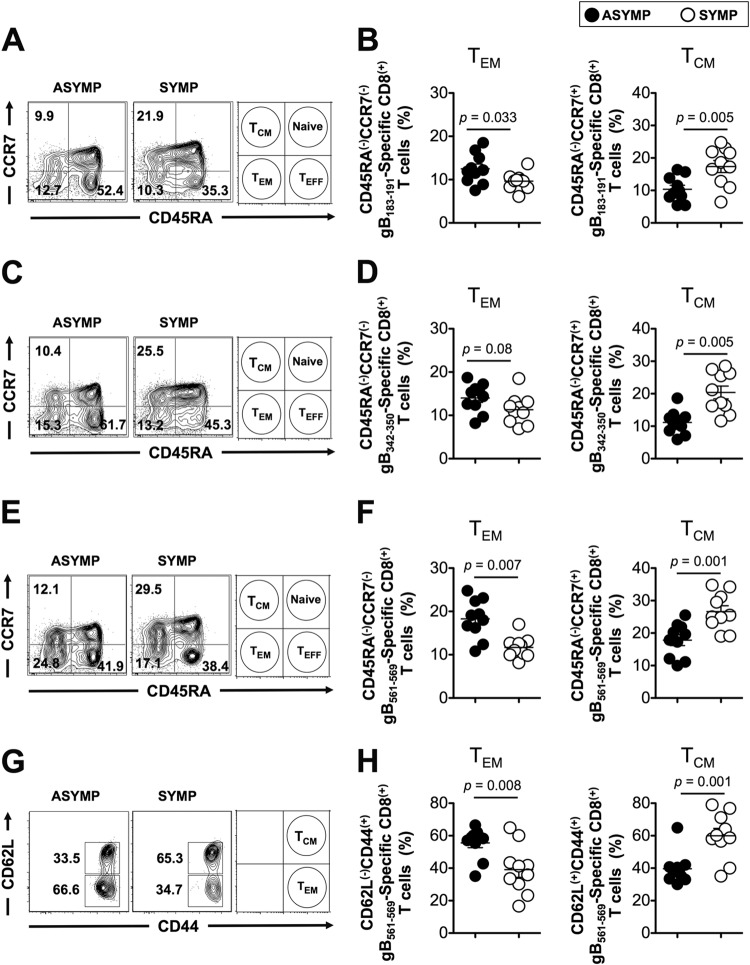
HSV-specific memory CD8+ T cells are categorized into two major phenotypically distinct TEM and TCM subpopulations (3, 5, 13, 38). We investigated whether SYMP and ASYMP individuals had different frequencies of HSV-specific CD8+ TEM and TCM subpopulations. We gated on CD3+ CD8+ T cells that are specific to either the immunodominant (gB183–191 and gB342–350) or the subdominant (gB17–25 and gB561–569) gB epitopes, using the specific tetramers described above. As shown in Fig. 2A, B, C, and D, ASYMP individuals had significantly higher percentages of CD45RAlow CCR7low CD8+ TEM cells specific to gB183–191 and gB342–350 immunodominant epitopes than SYMP individuals (P < 0.05). In contrast, we consistently detected significantly higher percentages of gB183–191 and gB342–350 epitope-specific CD45RAlow CCR7high CD8+ TCM cells in SYMP individuals than in ASYMP individuals (P < 0.05). Similarly, ASYMP individuals had significantly higher percentages of CD45RAlow CCR7low CD8+ TEM cells specific to the subdominant gB561–569 epitope, while significantly higher percentages of CD45RAhigh CCR7high CD8+ TCM cells were consistently detected in SYMP individuals (Fig. 2E and F) (P < 0.005). Moreover, ASYMP individuals had significantly higher percentages of gB561–569 epitope-specific CD44high CD62Llow CD8+ TEM cells than SYMP individuals (Fig. 2G and H) (P = 0.008). In contrast, significantly higher percentages of gB561–569 epitope-specific CD44high CD62Lhigh CD8+ TCM cells were detected in SYMP individuals than in ASYMP individuals (P = 0.001). Similar profiles of memory CD8+ T cell subpopulations were detected for the other subdominant gB17–25 epitope (data not shown).
FIG 2.
Frequent gB-specific CD8+ T cells with effector memory phenotype (CD8+ TEM cells) detected in ASYMP individuals compared to SYMP individuals. The phenotype of CD8+ T cells specific to gB peptide/tetramer complexes representing each of the four gB17–25, gB183–191, gB342–350, and gB561–569 epitopes shown in Fig. 1 was analyzed in term of TEM and TCM cells. (A, C, and E) Representative FACS data of the frequencies of gB-specific CD45RAlow CCR7low CD8+ TEM and CD45RAlow CCR7high TCM cells in one ASYMP individual and one SYMP individual. (G) Representative FACS data of the frequencies of gB-specific CD44high CD62Llow CD8+ TEM and CD44high CD62Lhigh TCM cells in one ASYMP individual and one SYMP individual. (B, D, F, and H) Average frequencies of PBMC-derived gB-specific CD8+ T cells with either the TEM or TCM phenotype analyzed from 10 ASYMP and 10 SYMP individuals. The results are representative of 2 independent experiments for each individual. The indicated P values, calculated using one-way ANOVA, show statistical significance of differences between SYMP and ASYMP individuals.
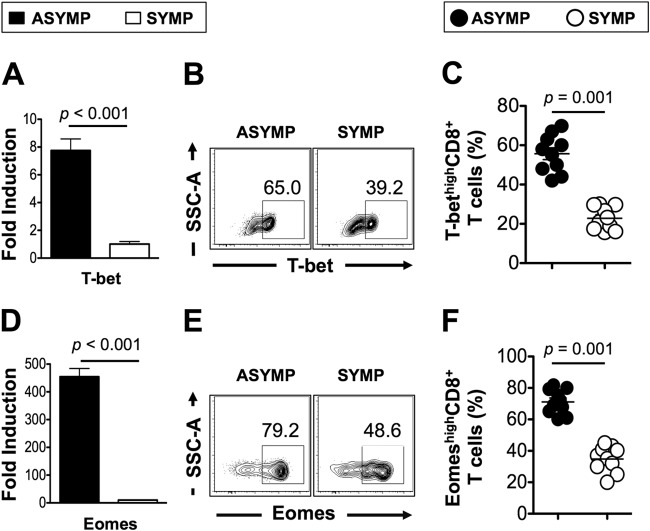
The expression patterns of the T-bet and Eomes transcription factors, which are associated with TCM/TEM balance, were analyzed ex vivo in gB epitope-specific CD8+ T cells from SYMP and ASYMP individuals at both the mRNA (using RT-PCR) and protein (using FACS) levels. As shown in Fig. 3A and D, a significantly higher proportion of CD8+ T cells from ASYMP individuals than from SYMP individuals expressed T-bet and Eomes. In addition, a higher proportion of HSV-1 gB epitope-specific CD8+ TEM cells from ASYMP individuals than from SYMP individuals were T-bethigh (Fig. 3B and C) and Eomeshigh (Fig. 3E and F) (P = 0.001).
FIG 3.
High levels of transcription factors expressed by HSV-1 gB epitope-specific CD8+ T cells from ASYMP individuals. (A and D) The expression patterns of transcription factors T-bet and Eomes were determined ex vivo at the RNA level using RT-PCR from total CD8+ T cells derived from either SYMP (open symbols) or ASYMP (closed symbols) individuals. (B and E) Representative FACS data of the percent expression of T-bet (B) and Eomes (E) in gB561–569 epitope-specific CD8+ TEM cells derived from one SYMP individual (right) and one ASYMP individual (left). (C and F) Average frequencies of the expression of T-bet and Eomes transcription factors analyzed by FACS at the protein level from gB561–569 epitope-specific CD8+ TEM cells derived from 10 SYMP (open circles) and 10 ASYMP (closed circles) individuals. The results are representative of 3 independent experiments for each individual. The indicated P values, calculated using one-way ANOVA, show statistical significance of differences between SYMP and ASYMP individuals.
Altogether, the phenotypic properties of HSV-1 gB epitope-specific memory CD8+ T cells revealed a clear dichotomy in memory CD8+ T cell subpopulations in SYMP versus ASYMP individuals. By maintaining high frequencies of the “experienced” HSV-specific CD8+ TEM cells, the ASYMP individuals should be better protected against infection and/or disease. The higher expression of T-bet and Eomes seen in ASYMP individuals may favor effector-to-memory CD8+ T cell transition (E>>>M) and the formation of a higher percentage of CD8+ TEM cells (39). Thus, the results suggest that at a subsequent pathogen encounter (e.g., following HSV-1 reactivation from latency), the ASYMP individuals, but not SYMP individuals, would mount much faster and stronger protective HSV-specific CD8+ TEM cell responses, allowing a better clearance of herpes infection and disease.
HSV gB epitope-specific effector CD8+ T cells from asymptomatic individuals are multifunctional compared to HSV gB epitope-specific CD8+ T cells from symptomatic individuals.
We next compared the function of HSV gB epitope-specific effector CD8+ T cells from SYMP versus ASYMP individuals. Because the frequency of the subdominant gB17–25 epitope is so low, the functional studies were focused only on three epitopes: the immunodominant gB183–191 and gB342–350 epitopes and the subdominant gB561–569 epitope.
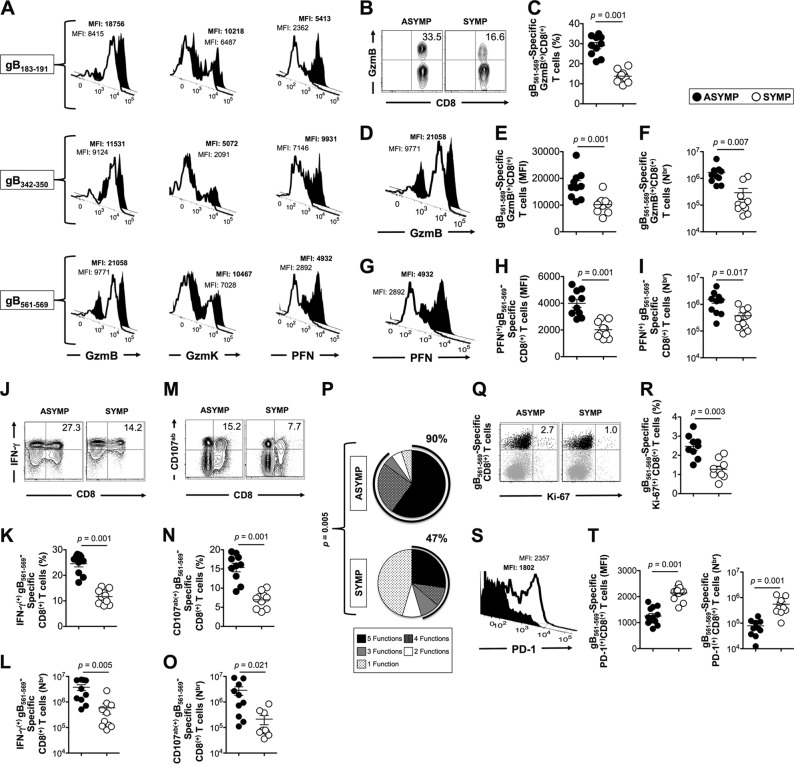
We first compared the expression of granzyme B (GzmB), granzyme K (GzmK), and perforin (PFN) on gated gB183–191, gB342–350, and gB561–569 epitope-specific CD8+ T cells from 10 SYMP and 10 ASYMP individuals (Fig. 4A). We found high levels of GzmB, GzmK, and PFN expressed on gB342–350, gB183–191, and gB561–569 epitope-specific CD8+ T cells from ASYMP individuals compared to SYMP individuals, suggesting a positive correlation of strong HSV-specific CD8+ T cell cytotoxic responses with protection from ocular herpetic disease (Fig. 4A). A significantly higher frequency of GzmB+ CD8+ T cells was detected in 10 ASYMP individuals than in 10 SYMP individuals (Fig. 4B and C) (P = 0.001). A significant increase in the level of expression of GzmB, as determined by mean fluorescence intensity (MFI) (Fig. 4D and E) (P = 0.001), and higher numbers of gB561–569 epitope-specific GzmB+ CD8+ T cells (Fig. 4F) (P = 0.007) were consistently detected in ASYMP individuals than in SYMP individuals. Similar trends were obtained for gB183–191 and gB342–350 epitope-specific GzmB+ CD8+ T cells (data not shown). We then determined the level of expression of perforin by gB epitope-specific CD8+ T cells and the numbers of PFN+ CD8+ T cells from SYMP and ASYMP individuals. Significantly higher levels of PFN, determined by mean fluorescence intensity (Fig. 4G and H) (P = 0.001), and higher numbers of gB561–569 epitope-specific CD8+ T cells producing PFN, determined by tetramer staining (Fig. 4I) (P = 0.017) were detected in ASYMP individuals than in SYMP individuals. We observed similar trends of PFN expression on gB183–191 and gB342–350 epitope-specific PFN+ CD8+ T cells from SYMP and ASYMP individuals (data not shown).
FIG 4.
Asymptomatic individuals have a significantly higher proportion of polyfunctional HSV-1 gB-epitope-specific CD8+ T cells. (A) gB epitope-primed CD8+ T cells from ASYMP individuals express high levels of lytic granules compared to CD8+ T cells from SYMP individuals. FACS was used to determine the expression levels of GzmB, GzmK, and PFN on tetramer-gated CD8+ T cells specific the to gB183–191, gB342–350, and gB561–569 epitopes, as described in Materials and Methods. The numbers on the top of each histogram represent mean fluorescence intensity (MFI), depicting the level of expression of each cytotoxic molecule. Numbers in bold represent the MFI for ASYMP individuals. (B and C) FACS data showing frequency of gB561–569-specific GzmB+ CD8+ T cells in SYMP and ASYMP individuals. (D to I) Representative histograms (D and G), average MFI (E and H), and absolute numbers (F and I) of gB561–569-specific GzmB+ CD8+ T cells and PFN+ CD8+ T cells from 10 ASYMP and 10 SYMP individuals, respectively. (J to L) Representative FACS data (J), frequencies (K), and absolute numbers (L) of gB561–569-specific IFN-γ+ CD8+ T cells from 10 ASYMP and 10 SYMP individuals. (M to O) Representative FACS data (M), frequencies (N), and absolute numbers (O) of gB561–569-specific CD107a/b+ CD8+ T cells from 10 ASYMP and 10 SYMP individuals. (P) Summary pie charts showing the overall portions of gB epitope-specific CD8+ T cell functions from 10 ASYMP and 10 SYMP individuals. (Q and R) Representative FACS data (Q) and average frequencies (R) of gB561–569-specific Ki-67+ CD8+ T cells from 10 ASYMP and 10 SYMP individuals. (S and T) Representative histogram (S), MFI (T, left panel), and absolute number (T, right panel) of gB561–569-specific PD-1+ CD8+ T cells. Bold number represents the MFI of ASYMP individuals. The results are representative of 2 independent experiments for each individual. The indicated P values, calculated using one-way ANOVA, show statistical significance of differences between SYMP and ASYMP individuals.
We next determined the ability of gB epitope-specific CD8+ T cells from SYMP versus ASYMP individuals to produce IFN-γ and degranulation marker CD107a/b following in vitro stimulation. Freshly isolated CD8+ T cells from SYMP and ASYMP individuals were stimulated in vitro for 6 h with individual immunodominant (gB183–191 and gB342–350) or subdominant (gB561–569) epitope peptides, as described in Materials and Methods. The percentages and numbers of IFN-γ+ CD8+ T and CD107a/b+ CD8+ T cells from SYMP and ASYMP individuals were compared by intracellular FACS staining. Significantly higher percentages (Fig. 4J and K) (P = 0.001) and numbers (Fig. 4L) (P = 0.007) of gB561–569 epitope-specific CD8+ T cells producing IFN-γ were detected in ASYMP individuals than in SYMP individuals. A similar trend was obtained when CD8+ T cells from SYMP and ASYMP individuals were stimulated by gB183–191 or gB342–350 peptide epitopes (data not shown). The level of CD107a/b expression on the surface of CD8+ T cells was used to determine epitope-specific cytotoxic function (33). We observed significantly higher percentages (Fig. 4M and N) (P = 0.001) and numbers (Fig. 4O) (P = 0.021) of gB561–569 epitope-specific CD8+ T cells expressing CD107a/b in ASYMP individuals than in SYMP individuals. A similar trend of CD107a/b expression was observed when CD8+ T cells from SYMP and ASYMP individuals were stimulated by gB183–191 or gB342–350 peptide epitopes (data not shown).
We compared the polyfunctionality of gB561–569-specific CD8+ T cells from ASYMP and SYMP individuals based on concurrent production of IFN-γ and high expression levels of GzmB, GzmK, PFN, and CD107a/b lytic granules. We found that 90% of ASYMP individuals had gB561–569-specific CD8+ T cells with 3 to 5 functions, indicating their polyfunctional ability. In contrast, only 47% of SYMP individuals had gB561–569-specific CD8+ T cells with 3 functions, while the majority had just one function, suggesting that CD8+ T cells from SYMP patients tended to be monofunctional (Fig. 4P) (P = 0.005). Moreover, a significantly higher percentage of gB561–569-specific CD8+ T cells from ASYMP individuals than from SYMP individuals upregulated Ki-67, indicative of increased proliferation (Fig. 4Q and R) (P = 0.003). To determine the exhaustion status of HSV-specific effector CD8+ T cells from SYMP versus ASYMP individuals, we analyzed the expression of PD-1, a marker of T cell exhaustion (40). SYMP patients had higher expression of PD-1 than ASYMP individuals as shown by mean fluorescence intensity and numbers of gB561–569-specific PD1+ CD8+ T cells (Fig. 4S and T) (P = 0.001), suggesting phenotypic exhaustion of HSV-specific CD8+ T cells derived from SYMP patients.
Altogether, these results indicate the following. (i) HSV-gB-specific effector CD8+ T cells from ASYMP individuals are multifunctional. In contrast, HSV-specific effector CD8+ T cells from SYMP individuals are mostly monofunctional. (ii) High expression of PD-1 on HSV-1 gB-specific CD8+ T cells from SYMP individuals also suggests more exposure to antigen than in ASYMP individuals, leading to dysfunction. (iii) The functional results suggest that, compared to SYMP individuals, ASYMP individuals are better prepared to mount protective cytotoxic and IFN-γ-producing CD8+ T cells, two effector arms of immunity that protect against herpes.
Immunization with asymptomatic CD8+ TEM epitopes, but not with symptomatic CD8+ TCM epitopes, elicits a strong CD8+ T cell-dependent protective immunity against ocular herpes in the “humanized” HLA-A*02:01 transgenic mouse model of ocular herpes.
Among the four gB epitopes identified in this study (gB17–25, gB183–191, gB342–350, and gB561–569), the most frequent, robust, and polyfunctional CD8+ TEM cell responses detected in 10 ASYMP individuals were directed mainly against gB342–350 and gB561–569 epitopes, and these are hence designated ASYMP CD8+ TEM epitopes (Fig. 2, 3, and 4) (13). In contrast, frequent, but less robust, CD8+ TCM cell responses detected in 10 SYMP individuals were directed mainly against gB17–25 and gB183–191 epitopes, and these are hence designated SYMP CD8+ TCM epitopes (Fig. 2, 3, and 4) (13). We next set up a preclinical vaccine trial, using our established susceptible “humanized” HLA-A*02:01 transgenic mouse model (BALB/c genetic background) (13), to evaluate whether immunization with ASYMP CD8+ TEM epitopes confers protection against ocular herpes infection and disease.
Groups of susceptible HLA Tg mice (n = 10 mice per group) were immunized subcutaneously twice, 21 days apart, with two ASYMP CD8+ TEM cell epitope peptides (gB342–350 and gB561–569) (group 1) or with two SYMP TCM epitope peptides (gB17–25 and gB183–191) (group 2). The CD8+ T cell epitope peptides were delivered with the CD4+ T helper PADRE epitope peptide mixed together and emulsified in CpG1826 adjuvant, as we previously described (13). As a negative control, mock-immunized mice received CpG1826 adjuvant alone (group 3). Two weeks after the second and final immunization, animals from all groups received an ocular HSV-1 challenge (2 × 105 PFU, McKrae strain) without scarification. The mice were then assessed for up to 30 days postchallenge for ocular herpes pathology, ocular viral titers, and survival.
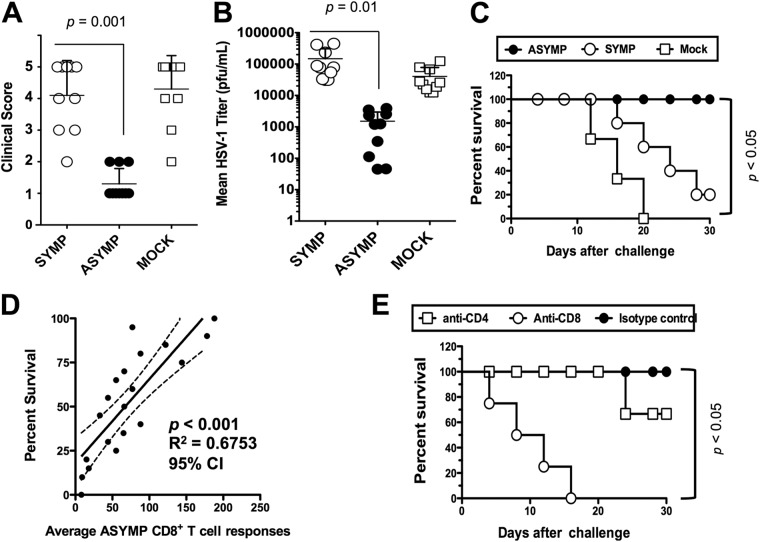
As shown in Fig. 5A, on day 10 postinfection, the pathology clinical scores observed in the ASYMP group were significantly lower than those recorded in the SYMP group or the mock-immunized group (P = 0.001 for all). Furthermore, significantly less virus was detected on day 7 postinfection (the peak of viral replication) in eye swabs of the ASYMP group than in the SYMP and mock-immunized groups (P = 0.01) (Fig. 5B). All animals in the ASYMP group survived lethal infection (100%), compared to only 10% survival in the SYMP group and 0% in the mock-immunized group (P < 0.005) (Fig. 5C). Overall, there was a positive correlation between survival and the number of ASYMP CD8+ TEM cells detected in the draining lymph nodes (DLN) of vaccinated mice (Fig. 5D) (P < 0.001, r2 = 0.6753, 95% confidence interval [CI]).
FIG 5.
CD8+ T cell-dependent protective immunity against ocular herpes induced by ASYMP CD8+ TEM epitopes in “humanized” HLA-A*02:01 transgenic mice. Three groups of age-matched female HLA-A*02:01 Tg mice (n = 10 each) were immunized subcutaneously, on days 0 and 21, with the human CD8+ TEM cell epitope peptides (gB342–350 and gB561–569) delivered with the CD4+ T cell PADRE epitope peptide emulsified in CpG1826 adjuvant (ASYMP), with the human CD8+ TCM cell epitope peptides (gB17–25 and gB183–191) delivered with the CD4+ T cell PADRE epitope peptide emulsified in CpG1826 adjuvant (SYMP), or with the CpG1826 adjuvant alone (mock). Two weeks after the final immunization, all animals were challenged ocularly with 2 × 105 PFU of HSV-1 (strain McKrae). (A) The eye disease was detected and scored 2 weeks after immunization as described in Materials and Methods. (B) Viral titrations were determined from eye swabs on day 7 postinfection, as described in Materials and Methods. (C) Survival was determined in a window of 30 days postchallenge, as described in Materials and Methods. (D) Scatter diagram and linear regression analysis of mouse survival (%) and HSV-specific CD8+ T cell responses after challenge with HSV-1. Correlation was performed using the Pearson test with two-tailed P value analysis (r2 = 0.6753; P < 0.001) (r2 = correlation coefficient). (E) The protective immunity against ocular herpes induced by immunization with the ASYMP CD8+ TEM cell human epitopes is abrogated following depletion of CD8+ T cells but not of CD4+ T cells. Following the second immunization, and before challenge with HSV-1, mice were injected intraperitoneally with six doses (i.e., 1 every other day) of 100 μl of saline containing anti-CD4, anti-CD8, or isotype control. Flow cytometry analysis confirmed a decrease in spleen CD4+ and CD8+ T cells in treated mice to consistently less than 2% after MAb treatment. The P values compare protection achieved in MAb-treated versus untreated mice using ANOVA. Immunized, MAb-treated, and infected mice were examined for survival in a window of 30 days postchallenge. The indicated P values, calculated using one-way ANOVA, show statistically significant differences between protected “ASYMP” and nonprotected “SYMP” mice.
To verify the implication of CD8+ T cells in the observed protection induced following immunization with the ASYMP CD8+ TEM cell epitopes, we performed an in vivo depletion of either CD4+ or CD8+ T cells in immunized mice before virus challenge, using specific MAbs. As shown in Fig. 5E, depletion of CD8+ T cells, but not of CD4+ T cells, significantly abrogated protection against death induced by immunization with the ASYMP CD8+ T cell epitopes (P < 0.005), suggesting that, in this system, CD8+ T cells, but not CD4+ T cells, provided most of the protection against lethal ocular herpes.
Overall, these results indicate that immunization with ASYMP CD8+ TEM cell epitope peptides, but not with SYMP TCM epitope peptides, decreased ocular herpes disease, decreased virus replication, and resulted in protection against lethal ocular herpes in susceptible HLA-A*02:01 Tg mice.
Frequent gB-specific CD8+ TEM cells are detected in the corneas of HSV-1-infected “ASYMP” HLA-A*02:01 transgenic mouse.
We next determined the frequency, phenotype, and function of CD8+ T cells in the cornea of protected “ASYMP” and nonprotected “SYMP” HLA-A*02:01 Tg mice that were vaccinated and challenged with HSV-1, as described above. For simplicity only the extremes of ASYMP and SYMP mice were used for phenotypic and functional characterization of cornea-resident CD8+ T cells. ASYMP mice had a clinical score of 1.0, while SYMP mice had a clinical score of 4 to 5.
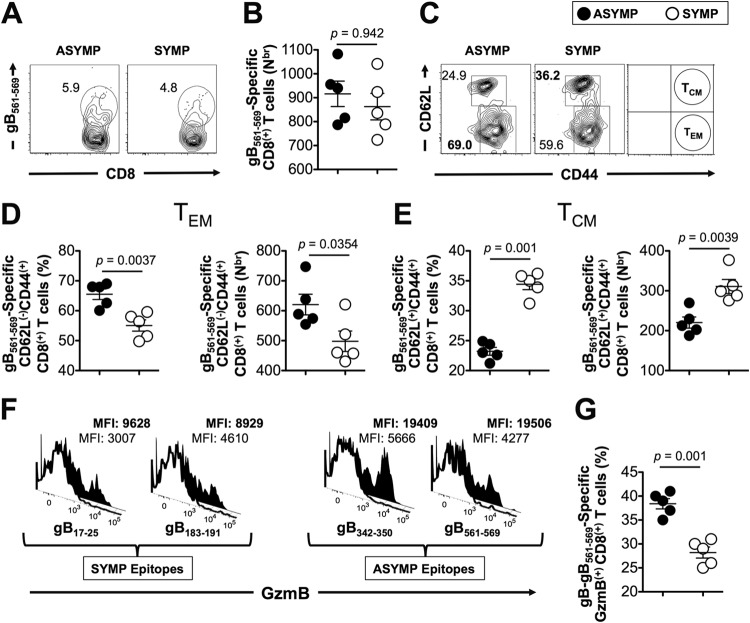
We looked at the frequencies and numbers of gB561–569-specific CD8+ T cells in corneas of ASYMP and SYMP mice. There were no significant differences in the frequencies and numbers of gB561–569-specific CD8+ T cells in the two groups of mice (Fig. 6A and B) (P = 0.942). As shown in Fig. 6C and D, ASYMP mice had a significantly higher percentage and number of cornea-resident gB561–569-specific CD44high CD62Llow CD8+ T cells with the TEM phenotype, compared to SYMP mice (65.2% ± 4% versus 54.14% ± 3%, P = 0.0037). In contrast, significantly higher percentages and numbers of cornea-resident gB561–569-specific CD44high CD62Lhigh CD8+ TCM cells were detected in SYMP mice than in ASYMP mice (Fig. 6C and E) (P = 0.001). Next, we determined the level of expression of GzmB, as determined by mean fluorescence intensity (MFI), in all four types of gB epitope-specific CD8+ T cells. There was significantly higher expression of GzmB in ASYMP gB epitope-specific CD8+ T cells than in SYMP gB epitope-specific CD8+ T cells (Fig. 6F). In addition, a higher percentage of gB epitope-specific CD8+ T cells expressing GzmB was also detected in ASYMP corneas than in SYMP corneas, suggesting that there are more functional effector gB-specific CD8+ T cells in ASYMP corneas (Fig. 6G) (P = 0.001).
FIG 6.
The corneas of HSV-1 infected “ASYMP” HLA-A*02:01 transgenic mice contain frequent gB-specific CD8+ TEM cells. The corneas of SYMP and ASYMP mice were analyzed for gB-specific CD8+ T cells on day 9 postinfection. ASYMP mice had a clinical score of 1.0, whereas SYMP mice had a score of 4 to 5. We used 1 × 106 cells for each assay. (A and B) Representative FACS data of the frequency (A) and absolute number (B) of gB561–569-specific CD8+ T cells in pooled corneas from SYMP and ASYMP mice. (C) Representative FACS data of the frequencies of CD44high CD62Llow CD8+ TEM and CD44high CD62Lhigh CD8+ TCM cells specific to gB561–569 tetramer in ASYMP and SYMP mice. (D) Average frequencies (left panel) and absolute number (right panel) of cornea-derived CD8+ T cells specific to gB561–569 tetramer in ASYMP and SYMP mice with the TEM phenotype, analyzed from 5 ASYMP and 5 SYMP mice. (E) Average frequencies (left panel) and absolute numbers (right panel) of cornea-derived CD8+ T cells specific to gB561–569 tetramer in ASYMP and SYMP mice with the TCM phenotype, analyzed from 5 ASYMP and 5 SYMP mice. (F and G) Representative histograms of levels of GzmB expression in SYMP gB-specific CD8+ T cell epitopes (gB17–25 and gB183–191) and ASYMP gB-specific CD8+ T epitopes (gB342–350 and gB561–569) (F) and frequencies of gB561–569 epitope-specific GzmB+ CD8+ T cells (G) from 5 ASYMP and 5 SYMP mice. The indicated P values, calculated using one-way ANOVA, show statistically significant differences between SYMP and ASYMP mice.
Altogether, these results indicate that, similar to HLA-A*02:01-positive ASYMP individuals, “ASYMP” HLA-A*02:01 Tg mice had frequent HSV-specific CD8+ TEM cells retained in the cornea, poised to act as an early line of defense against future virus encounter. The results also support HLA-A*02:01 Tg mice as a useful animal model for investigating the underlying immune mechanisms by which CD8+ T cells specific to HLA-restricted HSV-1 epitopes mediate control of ocular herpes infection and disease.
DISCUSSION
Characterizing the phenotype and function of HSV-specific effector and memory CD8+ T cells associated with ASYMP herpes infection is critical for the logical design of a T cell epitope-based herpes vaccine. The results presented in this report should yield new insights into the nature of protective HSV-specific CD8+ T cells in humans and provide a framework for the rational design of vaccines that elicit long-term CD8+ T cell protective immunity. We report that two major subpopulations of HSV-1 gB-specific CD8+ T cells, which possessed remarkably different phenotypes and functions, are maintained in SYMP versus ASYMP individuals. (i) ASYMP individuals had a significantly higher proportion of differentiated polyfunctional HSV-1 gB-specific CD8+ TEM cells. In contrast, SYMP patients had significantly higher frequencies of less-differentiated monofunctional HSV-1 gB-specific CD8+ TCM cells. (ii) Polyfunctional and robust TEM CD8+ T cells from ASYMP individuals recognized mainly gB342–350 and gB561–562 T cell epitopes. In contrast, monofunctional and less robust TCM CD8+ T cells in SYMP patients recognized mainly gB17–25 and gB183–191 epitopes. (iii) Immunization with ASYMP gB342–350 and gB561–562 TEM epitopes, but not with SYMP gB17–25 and gB183–191 TCM epitopes, protected susceptible HLA-A*02:01 transgenic mice from a highly pathogenic ocular herpes infection. To the best of our knowledge, this is the first report of phenotypic and functional differences of HSV-1-specific effector and memory CD8+ T cells from SYMP and ASYMP individuals with ocular herpes. It is hoped that our findings will guide a successful design of effective T cell-based vaccine strategies.
Our understanding of the population size, the specificity, the phenotype, and the function of HSV-specific CD8+ T cell populations derives mainly from mouse models of herpes infection (11, 23, 32, 41–43). To gain insight into the nature of human HSV-specific CD8+ T cell subpopulations, we used several human-focused immunological assays to characterize protective versus nonprotective HSV-1 gB-specific CD8+ T cells at both effector and memory levels (13). Our findings indicate that SYMP and ASYMP individuals have similar frequencies of HSV-1 gB epitope-specific CD8+ T cells, suggesting that herpetic disease is not a consequence of a clonal deletion of specific repertoires of CD8+ T cells in SYMP individuals. This result is in agreement with a recent study showing that once the clonal repertoire of HSV-specific CD8+ T cells is established, it is kept constant for several years (44). However, there were differences in T cells between SYMP and ASYMP individuals at the phenotypic and functional levels. The HSV-specific effector CD8+ T cell subpopulations in HSV-1 seropositive SYMP and ASYMP individuals were categorized in two major phenotypes: phenotype 1 appeared predominantly in most SYMP individuals, was least effector-like, and had low expression of GzmB/perforin, low expression of Ki-67, and less production of IFN-γ and CD107a/b, while phenotype 2 appeared predominantly in most ASYMP individuals, was most effector-like, and had high expression of GzmB/perforin and Ki-67 and high production of IFN-γ and CD107a/b. Moreover, the majority of HSV-1 gB-specific memory CD8+ T cells from ASYMP individuals and SYMP HLA-A*02:01 Tg mice were mainly of the TEM subpopulation, whileHSV-1 gB-specific CD8+ T cells from SYMP individuals and SYMP HLA-A*02:01 Tg mice were mainly of the TCM subpopulation. Although the information gained from PBMC-derived CD8+ T cells may not be completely reflective of tissue-resident CD8+ T cells, because of the obvious ethical and practical considerations of obtaining tissue-resident CD8+ T cells (i.e., from the human cornea and trigeminal ganglia [TG], the sites of acute and latent infections, respectively), our investigations in humans were limited to human PBMC-derived CD8+ T cells. Nevertheless, we were able to characterize T cells from corneas removed from HSV-1-infected SYMP and ASYMP “humanized” HLA Tg mice. HSV-specific CD8+ T cells from SYMP patients and SYMP mice had a greater frequency of monofunctional gB epitope-specific CD8+ TCM cells, while HSV-specific CD8+ T cells from ASYMP individuals and ASYMP mice had more polyfunctional gB epitope-specific CD8+ TTM cells. This suggests that the phenotype and function of CD8+ T cells from human PBMC likely reflect the phenotype and function of human cornea-resident T cells. These results suggest that at a second pathogen encounter (e.g., following HSV-1 reactivation from latency), ASYMP individuals would mount faster and stronger protective HSV-specific CD8+ TEM cell responses, allowing a better clearance of herpes infection and disease. In contrast, at a second pathogen encounter, SYMP individuals would not develop timely protective tissue-resident HSV-specific CD8+ TEM cell responses and hence would have more disease. This is supported by in vivo HLA-A*02:01 Tg mouse experiments demonstrating that the predicted ASYMP epitopes generated protective immunity against primary ocular herpes infection and disease. This suggests that these CD8+ T cells do recognize HLA-A*02:01-positive target cells, in which “native” epitopes have been generated and presented naturally by the endogenous major histocompatibility complex (MHC) class I processing pathway. Since mice do not undergo spontaneous reactivation, shedding of virus in tears, and recurrent eye disease, this study is focused on the protective efficacy of ASYMP epitopes against primary infection and disease. However, we will investigate therapeutic efficacy in the future using either (i) our HLA transgenic rabbit model, in which spontaneous reactivation and recurrent eye disease occur, or (ii) the UV-B mouse model of induced reactivation and recurrent eye disease. The results will be the subject of future reports.
Within the overall memory CD8+ T cell population, two distinct major subpopulations have been described and can be recognized by the differential expression of chemokine receptor CCR7 and L-selectin (CD62L). Central memory TCM cells express CD62L and CCR7 and secrete interleukin-2 (IL-2) but not IFN-γ or IL-4. Effector memory TEM cells do not express CD62L or CCR7 but produce effector cytokines such as IFN-γ and IL-4, consistent with our findings. Lack of CCR7 expression, which is required for T cell egress and recirculation, impairs the capacity of TEM cells for homing to lymphoid tissues (45). Beside TEM and TCM cells, more recently, other subpopulations have been explored based on the expression of CD27 and CD28 costimulatory molecules (46).
Previous studies in mice have shown that, following HSV-1 infection, CD8+ T cells persist in the cornea and trigeminal ganglia (TG) for prolonged periods of time after corneal herpes lesions are cleared (5, 47–53). The phenotype and function of these persistent CD8+ T cells have not been fully elucidated. In this report, we investigated the association between the severity of herpes disease and the quantity, quality, and diversity of HSV-specific memory CD8+ T cell subpopulations from blood (in humans) and cornea (in “humanized” HLA-A*02:01 Tg mice). We found that (i) circulating and tissue-resident HSV-1 gB epitope-specific memory CD8+ T cells differ in individuals with mild (ASYMP) versus severe (SYMP) ocular HSV-1 diseases and (ii) a specific phenotype and function of HSV-1 gB epitope-specific, tissue-resident, memory CD8+ T cells are associated with ocular herpes disease in “humanized” HLA-A*02:01 Tg mice. Whether the phenotype and function of CD8+ T cells found in HLA-A*02:01 Tg mice can be extrapolated to human corneal tissue resident memory, as has been reported for the genital herpes system (54, 55), remains to be determined. We are planning to obtain human cornea samples from ASYMP versus SYMP cohorts with mild and severe disease in order to characterize cornea-resident CD8+ T cells. These studies would define the phenotypic and functional characteristics of cornea-resident HSV-specific CD8+ T cells, information that will help guide our ongoing herpes vaccine development.
It has been established that HSV-specific CD8+ T cells elicited during a primary infection persist for years after clearance of the virus (3, 5, 13). These memory CD8+ T cells likely mediate recall responses that result in halting attempts at virus reactivation from latency and in accelerating viral clearance. We report that circulating CD8+ T cells from HSV-1-seropositive ASYMP individuals had a greater frequency of polyfunctional HSV-specific CD8+ TEM cells than those from SYMP patients. The functional characterization of HSV-specific CD8+ T cells in humans has so far been largely restricted to studies of IFN-γ production. The T cell receptor (TC)R-triggered release of the effector molecules perforin and GzmB, however, is thought to be a central pathway for the destruction of virus-infected target cells by effector CD8+ T cells (43, 56). We found that HSV-1 gB-epitope-specific CD8+ T cells in ASYMP individuals produced elevated levels of IFN-γ and CD107a/b, whereas SYMP individuals have HSV-1 gB-specific CD8+ T cells that produced low levels of IFN-γ and CD107a/b. Moreover, production of lytic granules such as perforin and GzmB point to HSV-specific effector memory CD8+ T (TEM) cells in ASYMP individuals. Our results confirm our previous report which showed that up to 95.5% of ASYMP individuals had CD8+ T cells that were able to produce 3 to 5 functions concurrently, compared to only 32% of SYMP individuals (13). These polyfunctional CD8+ T cells from ASYMP individuals may provide active and fast immune surveillance to protect against recurrent herpetic disease.
In the present study, we found high expression of T-bet and Eomes by HSV-specific CD8+ T cells from ASYMP individuals compared to SYMP patients. There was also a significant increase in the frequency of T-bethigh Eomeshigh CD8+ T cells from ASYMP individuals compared to SYMP individuals (P < 0.01). This is consistent with differentiated CD8+ T cells in ASYMP individuals. To our knowledge, this is the first study to show differential expression of transcription factors in HSV-specific human memory CD8+ T cells among HLA-A*02:01-positive, HSV-1-seropositive SYMP and ASYMP individuals. T-bet expression is also required for the early production of IFN-γ and GzmB by antigen-specific CD8+ T cells (57, 58). Similar to the case for T-bet and Eomes, levels of the transcriptional regulators ID1 (inhibitor of differentiation 1), ID3, Blimp-1 (prdm1), Bcl-2, and TCF, which play critical roles in the effector-to-memory CD8+ T cell transition (39, 59), were also high in HSV-specific CD8+ T cells from ASYMP individuals compared to HSV-specific CD8+ T cells from SYMP patients (data not shown). It is likely that the concerted action of T-bet, Eomes, and other transcription factors results in the development in ASYMP individuals of fully differentiated CD8+ TEM cells that migrate to inflamed tissues (i.e., eyes and sensory ganglia) following antigen recognition and secrete IFN-γ and CD107a/b, and/or release cytotoxic granules such as GzmB and perforin (26, 60).
In general, after clearance of primary infections, the vast majority (often as much as 90 to 95%) of effector CD8+ T cells die, leaving behind only 5 to 10% of CD8+ T cells destined to differentiate into a heterogeneous pool of memory CD8+ T cells that can survive long-term in the absence of antigens (over 2 years in mice and over 50 years in humans) (39, 58, 61–63). The CD8+ TCM versus CD8+ TEM cell lineage decision is influenced by many exogenous and endogenous factors, including the nature and strength of TCR signaling, cytokines (e.g., IL-2 and IL-15), and transcription factors (as we recently reviewed in reference 26). In the case of HSV-1, once primary infection has cleared, it is likely that certain human ASYMP epitopes (such as gB342–350 and gB561–569) may have the intrinsic ability to generate CD8+ TEM cell subpopulations, which might have received signals during the primary response not to contract but instead to be maintained at high frequencies in peripheral tissues, as has been reported in other systems (64–68). Thus, most ASYMP CD8+ TEM cells (similar to TRM cells) may reside mainly in peripheral tissues, such as the cornea and TG, where they provide an efficient and quick response following HSV-1 infection/reactivation (39, 69–71)—a plausible explanation of decreased frequencies of recurrent disease in ASYMP individuals. In contrast, CD8+ TCM cells specific to HSV-1 SYMP epitopes (such as gB17–25 and gB183–191) might have received different signals that lead to increased expression of CD62L and CCR7 lymph node-directing molecules, making CD8+ TCM cells destined to home to lymphoid organs instead of residing in peripheral tissues. Since SYMP CD8+ TCM cells do not reside in peripheral tissues, they are unable to provide efficient immunosurveillance for HSV-1 infection/reactivation—a plausible explanation of increased frequencies of recurrent herpetic disease in SYMP individuals.
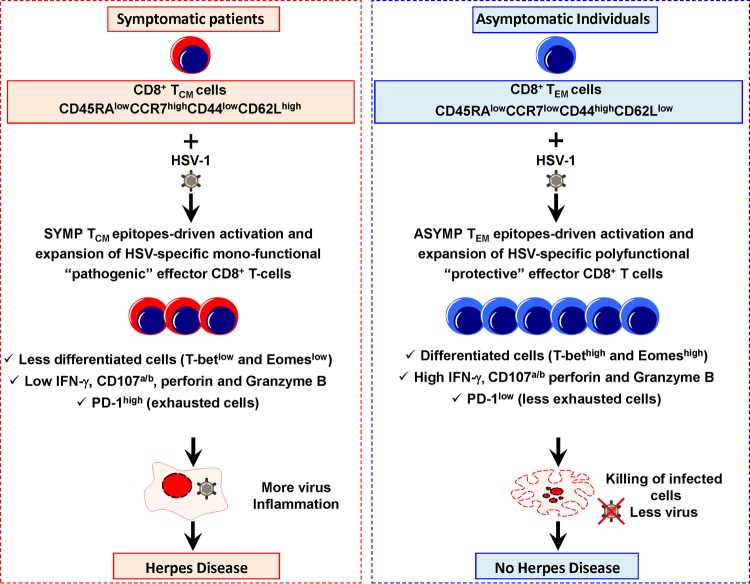
Based on our present findings, we propose a mechanism built on a novel “symptomatic/asymptomatic concept,” in which the immunopathology associated with corneal lesions is not a direct consequence of damage caused by the virus or by autoreactive or bystander T cells but rather results from the balance between “nonprotective” TCM cell responses specific to SYMP HSV-1 epitopes and protective TEM cell responses specific to ASYMP HSV-1 epitopes, as illustrated in Fig. 7. Clearly, the polyfunctionality of HSV-specific ASYMP CD8+ TEM cells is likely to be one of the important factors that accounts for the immunological control of herpes infection and disease. In contrast, monofunctional HSV-specific SYMP CD8+ TCM cells may be involved in the appearance and/or exacerbation of immunopathological recurrent corneal disease. However, this does not exclude that other host or viral factors, acting either alone or in concert with cellular immune responses, can also play a role in determining the course of herpes infection and disease. Regardless of the mechanism, if ASYMP individuals develop protective CD8+ TEM cells that recognize specific ASYMP epitopes while SYMP patients develop significantly larger frequencies of CD8+ TCM cells that recognize nonoverlapping SYMP epitopes, it would be logical to exclude such SYMP epitopes from future herpes vaccines on the grounds that they may exacerbate rather than protect against recurrent herpetic disease.
FIG 7.
A proposed model of HSV-specific CD8+ T cell-mediated mechanisms that operate in SYMP and ASYMP individuals. In ASYMP individuals, the CD8+ T cells (purple, right panel) develop more toward “protective” CD45RAlow CCR7low CD44high CD62Llow CD8+ TEM cells. After stimulation with HSV-1 ASYMP epitopes, differentiated CD8+ TEM cells from ASYMP individuals (T-bethigh and Eomeshigh) proliferate efficiently, produce high levels of IFN-γ and CD107a/b, express high levels of perforin and GzmB, and appear to be less exhausted (PD-1low), resulting in multifunctional CD8+ T cells that efficiently kill HSV-1-infected cells and decrease herpetic disease. In contrast, in HSV-seropositive SYMP patients, CD8+ T cells (orange, left panel) appear to develop more toward “less-protective” and maybe “pathogenic” CD45RAlow CCR7high CD44low CD62Lhigh CD8+ TCM cells. After stimulation with HSV-1 SYMP epitopes, CD8+ TCM cells from SYMP patients appear as less-differentiated cells (T-betlow and Eomeslow), produce low levels of IFN-γ and CD107a/b, express low levels of perforin and GzmB, and appear to be PD-1high exhausted cells. These cells are unable to resolve herpes infection and disease.
Lastly, we found a higher expression of PD-1 coinhibitory receptor on HSV-specific CD8+ T cells from SYMP patients than on HSV-specific CD8+ T cells from ASYMP individuals. This suggests that functional exhaustion of CD8+ T cells may contribute to symptomatic herpes disease. We do not exclude that infection with a highly pathological strain of HSV-1 in SYMP individuals leads, by a yet-to-be-determined mechanism, to functionally compromised HSV-specific CD8+ T cells. Differences in the immunological and pathological properties of HSV-2 strains from the United States and South Africa have been recently reported (72). Although continuous production of antigens does not occur during latent HSV-1 infections, antigenic stimulation during sporadic reactivations of HSV-1 from latency may lead to T cell exhaustion. We are currently testing whether blockade of negative T cell costimulatory molecules, including PD-1, using specific MAb therapy in combination with vaccination will restore the function of exhausted HSV-specific CD8+ T cells in latently infected HLA-A*02:01 Tg mice. This might enhance epitope-specific TEM cell responses in otherwise SYMP mice and protect against herpetic disease.
While developing an effective herpes vaccine is scientifically feasible, progress has been slow. Surprisingly, during the last 20 years only a single vaccine strategy, which consists of recombinant HSV glycoprotein D (gD) with or without gB, has been tested and retested in clinical trials (73). This strategy, which obviously delivered both SYMP and ASYMP epitopes in one protein, failed to reach its primary endpoint of reducing herpes disease, in spite of its ability to induce strong HSV-specific neutralizing antibodies (73). These failures emphasize the need for novel vaccine strategies that induce cell-mediated immunity (in addition to antibody-mediated immunity) for better protection against herpes (74). The present study supports this so-called “SYMP/ASYMP concept” by showing that immunization with ASYMP gB epitopes that are recognized mainly by CD8+ T cells from “naturally” protected ASYMP individuals also protected HLA-A*02:01 Tg mice against ocular herpes infection and disease. In contrast, immunization with SYMP gB epitopes that are mainly recognized by CD8+ TCM cells from SYMP patients did not protect. This novel approach is being extended in our laboratory to other HSV proteins, including tegument proteins, which are major targets of T cells (1).
In this study, we choose HLA-A*02:01-positive individuals because the HLA-A*02:01 allele is present in over 50% of most populations worldwide, regardless of race and ethnicity (75–78). However, a question of practical importance is the translation of the current preclinical findings in HLA-A*02:01-positive individuals for the development of an epitope-based clinical vaccine for a genetically diverse and heterogeneous human population (11, 12, 21, 34, 79, 80). A universal herpes vaccine should induce protective CD8+ T cell responses in the context of many different HLA alleles. The high degree of HLA polymorphism, which might be a hindrance to epitope-based vaccines, can be dealt with by the inclusion of multiple HLA-restricted epitopes that are recognized in the context of diverse related HLA alleles and by designing peptide-based vaccines with high densities of ASYMP CD8+ T cell epitopes. A combination of nine HLA supertypes has been defined to provide an almost perfect coverage (greater than 99%) of the entire repertoire of HLA molecules (81). We previously demonstrated that immunization with multiple ASYMP epitopes produced polyclonal CD8+ T cell lines (one T cell clone for each epitope) and broader effector and memory CD8+ T cells than a single epitope (11, 82). To further increase efficacy, a multiepitope-based peptide vaccine should include several ASYMP CD8+ T cell epitopes from several different glycoproteins and tegument proteins (1), each chosen to represent the HLA supertypes known to provide recognition in a large proportion of the global population, regardless of race and ethnicity.
In summary, our study provides new insights about the phenotypes and the functions of HSV-specific CD8+ T cell subpopulations that are associated with immunological control of herpes infection and disease in ASYMP individuals. It highlights the importance of CD8+ TEM cells in antiviral defense against ocular HSV-1 infection and disease. Human ASYMP HSV-1 gB epitopes that specifically recalled polyfunctional CD8+ TEM cell responses in HLA-A*02:01-positive, HSV-1-seropositive ASYMP individuals protected “humanized” HLA-A*02:01 Tg mice from ocular herpes infection and disease. In contrast, HLA-A*02:01-restricted SYMP epitopes derived from HSV-1 gB, which tended to recall monofunctional CD8+ TCM cell responses in HLA-A*02:01-positive, HSV-seropositive SYMP patients, were unable to protect HLA-A*02:01 Tg mice from ocular herpes infection and disease. The findings demonstrate quantitative and qualitative features of an effective HSV-specific CD8+ T cell response that should be taken into consideration in designing a T cell-based herpes vaccine.
ACKNOWLEDGMENTS
This work is supported by Public Health Service research grants EY14900, EY019896, EY024618, EY013191, 1R56AI098985, and 1R56AI093133 from the NIH, by the Discovery Center for Eye Research, and by a Research to Prevent Blindness Challenge grant.
We thank Dale Long from the NIH Tetramer Facility (Emory University, Atlanta, GA) for providing the tetramers used in this study. We also thank Barbara Bodenhoefer from UC, Irvine's, Institute for Clinical and Translational Science (ICTS) for helping with blood drawing from HSV-1-seropositive symptomatic and asymptomatic individuals.
We declare that no conflict of interest exists.
REFERENCES
- 1.Srivastava R, Khan AA, Spencer D, Vahed H, Thai NTU, Lopes PP, Wang C, Pham TT, M SV, J H, Nesburn AB, Wechsler SL, BenMohamed L. 23January2015. HLA-A02:01-restricted epitopes identified from the herpes simplex virus tegument protein VP11/12 preferentially recall polyfunctional effector memory CD8+ T cells from seropositive asymptomatic individuals and protect “humanized” HLA-A*02:01 transgenic mice against ocular herpes. J Immunol doi: 10.4049/jimmunol.1402606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuo T, Wang C, Badakhshan T, Chilukuri S, BenMohamed L. 2014. The challenges and opportunities for the development of a T-cell epitope-based herpes simplex vaccine. Vaccine 32:6733–6745. doi: 10.1016/j.vaccine.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samandary S, Kridane-Miledi H, Sandoval JS, Choudhury Z, Langa-Vives F, Spencer D, Chentoufi AA, Lemonnier FA, BenMohamed L. 2014. Associations of HLA-A, HLA-B and HLA-C allele frequency with prevalence of herpes simplex virus infections and diseases across global populations: implication for the development of a universal CD8+ T-cell epitope-based vaccine. Hum Immunol 75:715–729. doi: 10.1016/j.humimm.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang X, Dervillez X, Chentoufi AA, Badakhshan T, Bettahi I, BenMohamed L. 2012. Targeting the genital tract mucosa with a lipopeptide/recombinant adenovirus prime/boost vaccine induces potent and long-lasting CD8+ T cell immunity against herpes: importance of MyD88. J Immunol 189:4496–4509. doi: 10.4049/jimmunol.1201121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chentoufi AA, Dasgupta G, Christensen ND, Hu J, Choudhury ZS, Azeem A, Jester JV, Nesburn AB, Wechsler SL, BenMohamed L. 2010. A novel HLA (HLA-A*0201) transgenic rabbit model for preclinical evaluation of human CD8+ T cell epitope-based vaccines against ocular herpes. J Immunol 184:2561–2571. doi: 10.4049/jimmunol.0902322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chentoufi AA, Zhang X, Lamberth K, Dasgupta G, Bettahi I, Nguyen A, Wu M, Zhu X, Mohebbi A, Buus S, Wechsler SL, Nesburn AB, BenMohamed L. 2008. HLA-A*0201-restricted CD8+ cytotoxic T lymphocyte epitopes identified from herpes simplex virus glycoprotein D. J Immunol 180:426–437. doi: 10.4049/jimmunol.180.1.426. [DOI] [PubMed] [Google Scholar]
- 7.Langenberg AG, Corey L, Ashley RL, Leong WP, Straus SE. 1999. A prospective study of new infections with herpes simplex virus type 1 and type 2. Chiron HSV Vaccine Study Group. N Engl J Med 341:1432–1438. [DOI] [PubMed] [Google Scholar]
- 8.Dasgupta G, BenMohamed L. 2011. Of mice and not humans: how reliable are animal models for evaluation of herpes CD8(+)-T cell-epitopes-based immunotherapeutic vaccine candidates? Vaccine 29:5824–5836. doi: 10.1016/j.vaccine.2011.06.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chentoufi AA, Binder NR, Berka N, Durand G, Nguyen A, Bettahi I, Maillere B, BenMohamed L. 2008. Asymptomatic human CD4+ cytotoxic T-cell epitopes identified from herpes simplex virus glycoprotein B. J Virol 82:11792–11802. doi: 10.1128/JVI.00692-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.BenMohamed L, Bertrand G, McNamara CD, Gras-Masse H, Hammer J, Wechsler SL, Nesburn AB. 2003. Identification of novel immunodominant CD4+ Th1-type T-cell peptide epitopes from herpes simplex virus glycoprotein D that confer protective immunity. J Virol 77:9463–9473. doi: 10.1128/JVI.77.17.9463-9473.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang X, Issagholian A, Berg EA, Fishman JB, Nesburn AB, BenMohamed L. 2005. Th-cytotoxic T-lymphocyte chimeric epitopes extended by Nepsilon-palmitoyl lysines induce herpes simplex virus type 1-specific effector CD8+ Tc1 responses and protect against ocular infection. J Virol 79:15289–15301. doi: 10.1128/JVI.79.24.15289-15301.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nesburn AB, Bettahi I, Zhang X, Zhu X, Chamberlain W, Afifi RE, Wechsler SL, BenMohamed L. 2006. Topical/mucosal delivery of sub-unit vaccines that stimulate the ocular mucosal immune system. Ocul Surf 4:178–187. doi: 10.1016/S1542-0124(12)70164-7. [DOI] [PubMed] [Google Scholar]
- 13.Dervillez X, Qureshi H, Chentoufi AA, Khan AA, Kritzer E, Yu DC, Diaz OR, Gottimukkala C, Kalantari M, Villacres MC, Scarfone VM, McKinney DM, Sidney J, Sette A, Nesburn AB, Wechsler SL, BenMohamed L. 2013. Asymptomatic HLA-A*02:01-restricted epitopes from herpes simplex virus glycoprotein B preferentially recall polyfunctional CD8+ T cells from seropositive asymptomatic individuals and protect HLA transgenic mice against ocular herpes. J Immunol 191:5124–5138. doi: 10.4049/jimmunol.1301415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banerjee K, Biswas PS, Rouse BT. 2005. Elucidating the protective and pathologic T cell species in the virus-induced corneal immunoinflammatory condition herpetic stromal keratitis. J Leukoc Biol 77:24–32. doi: 10.1189/jlb.0904486. [DOI] [PubMed] [Google Scholar]
- 15.Stuart PM, Summers B, Morris JE, Morrison LA, Leib DA. 2004. CD8(+) T cells control corneal disease following ocular infection with herpes simplex virus type 1. J Gen Virol 85:2055–2063. doi: 10.1099/vir.0.80049-0. [DOI] [PubMed] [Google Scholar]
- 16.Banerjee K, Deshpande S, Zheng M, Kumaraguru U, Schoenberger SP, Rouse BT. 2002. Herpetic stromal keratitis in the absence of viral antigen recognition. Cell Immunol 219:108–118. doi: 10.1016/S0008-8749(02)00601-9. [DOI] [PubMed] [Google Scholar]
- 17.Bouley DM, Kanangat S, Wire W, Rouse BT. 1995. Characterization of herpes simplex virus type-1 infection and herpetic stromal keratitis development in IFN-gamma knockout mice. J Immunol 155:3964–3971. [PubMed] [Google Scholar]
- 18.Babu JS, Thomas J, Kanangat S, Morrison LA, Knipe DM, Rouse BT. 1996. Viral replication is required for induction of ocular immunopathology by herpes simplex virus. J Virol 70:101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zarling JM, Moran PA, Brewer L, Ashley R, Corey L. 1988. Herpes simplex virus (HSV)-specific proliferative and cytotoxic T-cell responses in humans immunized with an HSV type 2 glycoprotein subunit vaccine. J Virol 62:4481–4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stanberry LR, Spruance SL, Cunningham AL, Bernstein DI, Mindel A, Sacks S, Tyring S, Aoki FY, Slaoui M, Denis M, Vandepapeliere P, Dubin G. 2002. Glycoprotein-D-adjuvant vaccine to prevent genital herpes. N Engl J Med 347:1652–1661. doi: 10.1056/NEJMoa011915. [DOI] [PubMed] [Google Scholar]
- 21.Zhu X, Ramos TV, Gras-Masse H, Kaplan BE, BenMohamed L. 2004. Lipopeptide epitopes extended by an Nε-palmitoyl lysine moiety increases uptake and maturation of dendritic cell through a Toll-like receptor 2 pathway and triggers a Th1-dependent protective immunity. Eur J Immunol 34:1142–1149. doi: 10.1002/eji.200425166. [DOI] [PubMed] [Google Scholar]
- 22.Blaney JE Jr, Nobusawa E, Brehm MA, Bonneau RH, Mylin LM, Fu TM, Kawaoka Y, Tevethia SS. 1998. Immunization with a single major histocompatibility complex class I-restricted cytotoxic T-lymphocyte recognition epitope of herpes simplex virus type 2 confers protective immunity. J Virol 72:9567–9574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.St Leger AJ, Peters B, Sidney J, Sette A, Hendricks RL. 2011. Defining the herpes simplex virus-specific CD8+ T cell repertoire in C57BL/6 mice. J Immunol 186:3927–3933. doi: 10.4049/jimmunol.1003735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suvas S, Azkur AK, Rouse BT. 2006. Qa-1b and CD94-NKG2a interaction regulate cytolytic activity of herpes simplex virus-specific memory CD8+ T cells in the latently infected trigeminal ganglia. J Immunol 176:1703–1711. doi: 10.4049/jimmunol.176.3.1703. [DOI] [PubMed] [Google Scholar]
- 25.Chentoufi AA, BenMohamed L, Van De Perre P, Ashkar AA. 2012. Immunity to ocular and genital herpes simplex viruses infections. Clin Dev Immunol 2012:732546. doi: 10.1155/2012/732546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan AA, Srivastava R, Lopes PP, Wang C, Pham TT, Cochrane J, Thai NT, Gutierrez L, BenMohamed L. 2014. Asymptomatic memory CD8 T cells: from development and regulation to consideration for human vaccines and immunotherapeutics. Hum Vaccin Immunother 10:945–963. doi: 10.4161/hv.27762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Romero P, Zippelius A, Kurth I, Pittet MJ, Touvrey C, Iancu EM, Corthesy P, Devevre E, Speiser DE, Rufer N. 2007. Four functionally distinct populations of human effector-memory CD8+ T lymphocytes. J Immunol 178:4112–4119. doi: 10.4049/jimmunol.178.7.4112. [DOI] [PubMed] [Google Scholar]
- 28.Gebhardt T, Wakim LM, Eidsmo L, Reading PC, Heath WR, Carbone FR. 2009. Memory T cells in nonlymphoid tissue that provide enhanced local immunity during infection with herpes simplex virus. Nat Immunol 10:524–530. doi: 10.1038/ni.1718. [DOI] [PubMed] [Google Scholar]
- 29.Jiang X, Clark RA, Liu L, Wagers AJ, Fuhlbrigge RC, Kupper TS. 2012. Skin infection generates non-migratory memory CD8+ T(RM) cells providing global skin immunity. Nature 483:227–231. doi: 10.1038/nature10851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shin H, Iwasaki A. 2012. A vaccine strategy that protects against genital herpes by establishing local memory T cells. Nature 491:463–467. doi: 10.1038/nature11522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Osorio Y, Mott KR, Jabbar AM, Moreno A, Foster TP, Kousoulas KG, Ghiasi H. 2007. Epitope mapping of HSV-1 glycoprotein K (gK) reveals a T cell epitope located within the signal domain of gK. Virus Res 128:71–80. doi: 10.1016/j.virusres.2007.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mott KR, Chentoufi AA, Carpenter D, BenMohamed L, Wechsler SL, Ghiasi H. 2009. The role of a glycoprotein K (gK) CD8+ T-cell epitope of herpes simplex virus on virus replication and pathogenicity. Invest Ophthalmol Vis Sci 50:2903–2912. doi: 10.1167/iovs.08-2957. [DOI] [PubMed] [Google Scholar]
- 33.Betts MR, Brenchley JM, Price DA, De Rosa SC, Douek DC, Roederer M, Koup RA. 2003. Sensitive and viable identification of antigen-specific CD8+ T cells by a flow cytometric assay for degranulation. J Immunol Methods 281:65–78. doi: 10.1016/S0022-1759(03)00265-5. [DOI] [PubMed] [Google Scholar]
- 34.BenMohamed L, Krishnan R, Auge C, Primus JF, Diamond DJ. 2002. Intranasal administration of a synthetic lipopeptide without adjuvant induces systemic immune responses. Immunology 106:113–121. doi: 10.1046/j.1365-2567.2002.01396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.BenMohamed L, Krishnan R, Longmate J, Auge C, Low L, Primus J, Diamond DJ. 2000. Induction of CTL response by a minimal epitope vaccine in HLA A*0201/DR1 transgenic mice: dependence on HLA class II restricted T(H) response. Hum Immunol 61:764–779. doi: 10.1016/S0198-8859(00)00139-7. [DOI] [PubMed] [Google Scholar]
- 36.Boucherma R, Kridane-Miledi H, Bouziat R, Rasmussen M, Gatard T, Langa-Vives F, Lemercier B, Lim A, Berard M, Benmohamed L, Buus S, Rooke R, Lemonnier FA. 2013. HLA-A*01:03, HLA-A*24:02, HLA-B*08:01, HLA-B*27:05, HLA-B*35:01, HLA-B*44:02, and HLA-C*07:01 monochain transgenic/H-2 class I null mice: novel versatile preclinical models of human T cell responses. J Immunol 191:583–593. doi: 10.4049/jimmunol.1300483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang X, Chentoufi AA, Dasgupta G, Nesburn AB, Wu M, Zhu X, Carpenter D, Wechsler SL, You S, BenMohamed L. 2009. A genital tract peptide epitope vaccine targeting TLR-2 efficiently induces local and systemic CD8+ T cells and protects against herpes simplex virus type 2 challenge. Mucosal Immunol 2:129–143. doi: 10.1038/mi.2008.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sallusto F, Lenig D, Forster R, Lipp M, Lanzavecchia A. 1999. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401:708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 39.Joshi NS, Kaech SM. 2008. Effector CD8 T cell development: a balancing act between memory cell potential and terminal differentiation. J Immunol 180:1309–1315. doi: 10.4049/jimmunol.180.3.1309. [DOI] [PubMed] [Google Scholar]
- 40.Channappanavar R, Twardy BS, Suvas S. 2012. Blocking of PDL-1 interaction enhances primary and secondary CD8 T cell response to herpes simplex virus-1 infection. PLoS One 7:e39757. doi: 10.1371/journal.pone.0039757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mott KR, Bresee CJ, Allen SJ, BenMohamed L, Wechsler SL, Ghiasi H. 2009. Level of herpes simplex virus type 1 latency correlates with severity of corneal scarring and exhaustion of CD8+ T cells in trigeminal ganglia of latently infected mice. J Virol 83:2246–2254. doi: 10.1128/JVI.02234-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.St Leger AJ, Jeon S, Hendricks RL. 2013. Broadening the repertoire of functional herpes simplex virus type 1-specific CD8+ T cells reduces viral reactivation from latency in sensory ganglia. J Immunol 191:2258–2265. doi: 10.4049/jimmunol.1300585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Knickelbein JE, Khanna KM, Yee MB, Baty CJ, Kinchington PR, Hendricks RL. 2008. Noncytotoxic lytic granule-mediated CD8+ T cell inhibition of HSV-1 reactivation from neuronal latency. Science 322:268–271. doi: 10.1126/science.1164164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iancu EM, Corthesy P, Baumgaertner P, Devevre E, Voelter V, Romero P, Speiser DE, Rufer N. 2009. Clonotype selection and composition of human CD8 T cells specific for persistent herpes viruses varies with differentiation but is stable over time. J Immunol 183:319–331. doi: 10.4049/jimmunol.0803647. [DOI] [PubMed] [Google Scholar]
- 45.Hopken UE, Winter S, Achtman AH, Kruger K, Lipp M. 2010. CCR7 regulates lymphocyte egress and recirculation through body cavities. J Leukoc Biol 87:671–682. doi: 10.1189/jlb.0709505. [DOI] [PubMed] [Google Scholar]
- 46.Hikono H, Kohlmeier JE, Takamura S, Wittmer ST, Roberts AD, Woodland DL. 2007. Activation phenotype, rather than central- or effector-memory phenotype, predicts the recall efficacy of memory CD8+ T cells. J Exp Med 204:1625–1636. doi: 10.1084/jem.20070322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ouwendijk WJ, Geluk A, Smits SL, Getu S, Osterhaus AD, Verjans GM. 2014. Functional characterization of ocular-derived human alphaherpesvirus cross-reactive CD4 T cells. J Immunol 192:3730–3739. doi: 10.4049/jimmunol.1302307. [DOI] [PubMed] [Google Scholar]
- 48.van Velzen M, Jing L, Osterhaus AD, Sette A, Koelle DM, Verjans GM. 2013. Local CD4 and CD8 T-cell reactivity to HSV-1 antigens documents broad viral protein expression and immune competence in latently infected human trigeminal ganglia. PLoS Pathog 9:e1003547. doi: 10.1371/journal.ppat.1003547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Velzen M, Missotten T, van Loenen FB, Meesters RJ, Luider TM, Baarsma GS, Osterhaus AD, Verjans GM. 2013. Acyclovir-resistant herpes simplex virus type 1 in intra-ocular fluid samples of herpetic uveitis patients. J Clin Virol 57:215–221. doi: 10.1016/j.jcv.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 50.Allen SJ, Hamrah P, Gate D, Mott KR, Mantopoulos D, Zheng L, Town T, Jones C, von Andrian UH, Freeman GJ, Sharpe AH, BenMohamed L, Ahmed R, Wechsler SL, Ghiasi H. 2011. The role of LAT in increased CD8+ T cell exhaustion in trigeminal ganglia of mice latently infected with herpes simplex virus 1. J Virol 85:4184–4197. doi: 10.1128/JVI.02290-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arbusow V, Derfuss T, Held K, Himmelein S, Strupp M, Gurkov R, Brandt T, Theil D. 2010. Latency of herpes simplex virus type-1 in human geniculate and vestibular ganglia is associated with infiltration of CD8+ T cells. J Med Virol 82:1917–1920. doi: 10.1002/jmv.21904. [DOI] [PubMed] [Google Scholar]
- 52.Chentoufi AA, BenMohamed L. 2010. Future viral vectors for the delivery of asymptomatic herpes epitope-based immunotherapeutic vaccines. Future Virol 5:525–528. doi: 10.2217/fvl.10.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Held K, Eiglmeier I, Himmelein S, Sinicina I, Brandt T, Theil D, Dornmair K, Derfuss T. 2012. Clonal expansions of CD8(+) T cells in latently HSV-1-infected human trigeminal ganglia. J Neurovirol 18:62–68. doi: 10.1007/s13365-011-0067-9. [DOI] [PubMed] [Google Scholar]
- 54.Zhu J, Hladik F, Woodward A, Klock A, Peng T, Johnston C, Remington M, Magaret A, Koelle DM, Wald A, Corey L. 2009. Persistence of HIV-1 receptor-positive cells after HSV-2 reactivation is a potential mechanism for increased HIV-1 acquisition. Nat Med 15:886–892. doi: 10.1038/nm.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhu J, Koelle DM, Cao J, Vazquez J, Huang ML, Hladik F, Wald A, Corey L. 2007. Virus-specific CD8+ T cells accumulate near sensory nerve endings in genital skin during subclinical HSV-2 reactivation. J Exp Med 204:595–603. doi: 10.1084/jem.20061792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Divito SJ, Hendricks RL. 2008. Activated inflammatory infiltrate in HSV-1-infected corneas without herpes stromal keratitis. Invest Ophthalmol Vis Sci 49:1488–1495. doi: 10.1167/iovs.07-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cruz-Guilloty F, Pipkin ME, Djuretic IM, Levanon D, Lotem J, Lichtenheld MG, Groner Y, Rao A. 2009. Runx3 and T-box proteins cooperate to establish the transcriptional program of effector CTLs. J Exp Med 206:51–59. doi: 10.1084/jem.20081242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Joshi NS, Cui W, Dominguez CX, Chen JH, Hand TW, Kaech SM. 2011. Increased numbers of preexisting memory CD8 T cells and decreased T-bet expression can restrain terminal differentiation of secondary effector and memory CD8 T cells. J Immunol 187:4068–4076. doi: 10.4049/jimmunol.1002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cannarile MA, Lind NA, Rivera R, Sheridan AD, Camfield KA, Wu BB, Cheung KP, Ding Z, Goldrath AW. 2006. Transcriptional regulator Id2 mediates CD8+ T cell immunity. Nat Immunol 7:1317–1325. doi: 10.1038/ni1403. [DOI] [PubMed] [Google Scholar]
- 60.Hufner K, Horn A, Derfuss T, Glon C, Sinicina I, Arbusow V, Strupp M, Brandt T, Theil D. 2009. Fewer latent herpes simplex virus type 1 and cytotoxic T cells occur in the ophthalmic division than in the maxillary and mandibular divisions of the human trigeminal ganglion and nerve. J Virol 83:3696–3703. doi: 10.1128/JVI.02464-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jung YW, Rutishauser RL, Joshi NS, Haberman AM, Kaech SM. 2010. Differential localization of effector and memory CD8 T cell subsets in lymphoid organs during acute viral infection. J Immunol 185:5315–5325. doi: 10.4049/jimmunol.1001948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chandele A, Joshi NS, Zhu J, Paul WE, Leonard WJ, Kaech SM. 2008. Formation of IL-7Ralphahigh and IL-7Ralphalow CD8 T cells during infection is regulated by the opposing functions of GABPalpha and Gfi-1. J Immunol 180:5309–5319. doi: 10.4049/jimmunol.180.8.5309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joshi NS, Cui W, Chandele A, Lee HK, Urso DR, Hagman J, Gapin L, Kaech SM. 2007. Inflammation directs memory precursor and short-lived effector CD8(+) T cell fates via the graded expression of T-bet transcription factor. Immunity 27:281–295. doi: 10.1016/j.immuni.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mackay LK, Rahimpour A, Ma JZ, Collins N, Stock AT, Hafon ML, Vega-Ramos J, Lauzurica P, Mueller SN, Stefanovic T, Tscharke DC, Heath WR, Inouye M, Carbone FR, Gebhardt T. 2013. The developmental pathway for CD103(+)CD8+ tissue-resident memory T cells of skin. Nat Immunol 14:1294–1301. doi: 10.1038/ni.2744. [DOI] [PubMed] [Google Scholar]
- 65.Gebhardt T, Whitney PG, Zaid A, Mackay LK, Brooks AG, Heath WR, Carbone FR, Mueller SN. 2011. Different patterns of peripheral migration by memory CD4+ and CD8+ T cells. Nature 477:216–219. doi: 10.1038/nature10339. [DOI] [PubMed] [Google Scholar]
- 66.Belz GT, Wilson NS, Smith CM, Mount AM, Carbone FR, Heath WR. 2006. Bone marrow-derived cells expand memory CD8+ T cells in response to viral infections of the lung and skin. Eur J Immunol 36:327–335. doi: 10.1002/eji.200535432. [DOI] [PubMed] [Google Scholar]
- 67.Marzo AL, Yagita H, Lefrancois L. 2007. Cutting edge: migration to nonlymphoid tissues results in functional conversion of central to effector memory CD8 T cells. J Immunol 179:36–40. doi: 10.4049/jimmunol.179.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hogan RJ, Cauley LS, Ely KH, Cookenham T, Roberts AD, Brennan JW, Monard S, Woodland DL. 2002. Long-term maintenance of virus-specific effector memory CD8+ T cells in the lung airways depends on proliferation. J Immunol 169:4976–4981. doi: 10.4049/jimmunol.169.9.4976. [DOI] [PubMed] [Google Scholar]
- 69.Wherry EJ, Teichgraber V, Becker TC, Masopust D, Kaech SM, Antia R, von Andrian UH, Ahmed R. 2003. Lineage relationship and protective immunity of memory CD8 T cell subsets. Nat Immunol 4:225–234. doi: 10.1038/ni889. [DOI] [PubMed] [Google Scholar]
- 70.Plunkett FJ, Franzese O, Belaramani LL, Fletcher JM, Gilmour KC, Sharifi R, Khan N, Hislop AD, Cara A, Salmon M, Gaspar HB, Rustin MH, Webster D, Akbar AN. 2005. The impact of telomere erosion on memory CD8+ T cells in patients with X-linked lymphoproliferative syndrome. Mech Ageing Dev 126:855–865. doi: 10.1016/j.mad.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 71.Akbar AN, Fletcher JM. 2005. Memory T cell homeostasis and senescence during aging. Curr Opin Immunol 17:480–485. doi: 10.1016/j.coi.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 72.Dudek TE, Torres-Lopez E, Crumpacker C, Knipe DM. 2011. Evidence for differences in immunologic and pathogenesis properties of herpes simplex virus 2 strains from the United States and South Africa. J Infect Dis 203:1434–1441. doi: 10.1093/infdis/jir047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Belshe PB, Leone PA, Bernstein DI, Wald A, Levin MJ, Stapleton JT, Gorfinkel I, Morrow RLA, Ewell MG, Stokes-Riner A, Dubin G, Heineman TC, Schulte JM, Deal CD. 2012. Efficacy results of a trial of a herpes simplex vaccine. N Engl J Med 366:34–43. doi: 10.1056/NEJMoa1103151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Knipe DM, Corey L, Cohen JI, Deal CD. 2014. Summary and recommendations from a National Institute of Allergy and Infectious Diseases (NIAID) workshop on “Next Generation Herpes Simplex Virus Vaccines.” Vaccine 32:1561–1562. doi: 10.1016/j.vaccine.2014.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.El-Awar N, Lee JH, Tarsitani C, Terasaki PI. 2007. HLA class I epitopes: recognition of binding sites by mAbs or eluted alloantibody confirmed with single recombinant antigens. Hum Immunol 68:170–180. doi: 10.1016/j.humimm.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 76.Pekiner FN, Aytugar E, Demirel GY, Borahan MO. 2013. HLA-A, B (class I) and HLA-DR, DQ (class II) antigens in Turkish patients with recurrent aphthous ulceration and Behcet's disease. Med Princ Pract 22:464–468. doi: 10.1159/000348366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Castelli EC, Gil DS, Veiga LC, de Camargo JL. 2005. Typing class I HLA-A gene using a nested PCR-RFLP procedure. Braz J Med Biol Res 38:837–842. doi: 10.1590/S0100-879X2005000600004. [DOI] [PubMed] [Google Scholar]
- 78.Sidney J, Southwood S, Mann DL, Fernandez-Vina MA, Newman MJ, Sette A. 2001. Majority of peptides binding HLA-A*0201 with high affinity crossreact with other A2-supertype molecules. Hum Immunol 62:1200–1216. doi: 10.1016/S0198-8859(01)00319-6. [DOI] [PubMed] [Google Scholar]
- 79.BenMohamed L, Belkaid Y, Loing E, Brahimi K, Gras-Masse H, Druilhe P. 2002. Systemic immune responses induced by mucosal administration of lipopeptides without adjuvant. Eur J Immunol 32:2274–2281. doi:. [DOI] [PubMed] [Google Scholar]
- 80.BenMohamed L, Wechsler SL, Nesburn AB. 2002. Lipopeptide vaccines—yesterday, today, and tomorrow. Lancet Infect Dis 2:425–431. doi: 10.1016/S1473-3099(02)00318-3. [DOI] [PubMed] [Google Scholar]
- 81.Sette A, Newman M, Livingston B, McKinney D, Sidney J, Ishioka G, Tangri S, Alexander J, Fikes J, Chesnut R. 2002. Optimizing vaccine design for cellular processing, MHC binding and TCR recognition. Tissue Antigens 59:443–451. doi: 10.1034/j.1399-0039.2002.590601.x. [DOI] [PubMed] [Google Scholar]
- 82.Bettahi I, Nesburn AB, Yoon S, Zhang X, Mohebbi A, Sue V, Vanderberg A, Wechsler SL, BenMohamed L. 2007. Protective immunity against ocular herpes infection and disease induced by highly immunogenic self-adjuvanting glycoprotein D lipopeptide vaccines. Invest Ophthalmol Vis Sci 48:4643–4653. doi: 10.1167/iovs.07-0356. [DOI] [PubMed] [Google Scholar]