Abstract
Background:
Visceral leishmaniasis (VL) as one of the most important human parasitic disease is endemic in some parts of Iran. Several cases of VL have been reported recently in the Ilam Province. The current study aimed to assess the present status of human VL in the region.
Methods:
A random cluster sampling method was used to collect 456 serums samples from the children up to 12 years of age and 10% of adults living in urban and rural areas of the province. All the collected serum samples were tested by direct agglutination test (DAT) to detect anti- Leishmania infantum antibodies.
Results:
Of the examined 456 serum samples with direct agglutination test (DAT), only 21 (0.43%) sera showed anti- Leishmania antibodies at titers 1:400 and higher. Distribution of anti- Leishmania antibodies titers were: 1:400(n=4), 1:800(n=11), 1:1600(n=3), 1:3200(n=1), and 1:6400(n=1). Individuals with titers ≥1:3200 showed clinical signs and symptoms such as fever and splenomegaly. The highest and lowest seropositivity were observed in the age groups of 5–9 and >15 years old, respectively. There were no significant difference between the rate of seropositivity in males and females.
Conclusion:
VL with a low prevalence circulates in some parts of Ilam province, particularly in the southern parts. Complementary studies should be needed to find animal reservoir hosts and vectors. Furthermore, health systems and physicians should pay particular attention to the disease.
Keywords: Visceral leishmaniasis, Human, Seroprevalence, Iran
Introduction
Leishmaniasis, a parasitic disease of the reticuloendothelial system, is extremely significant in health systems. The flagellate protozoan responsible for the disease belongs to the order Kinetoplastidae, family Trypanosomatidae, and genus Leishmania. Leishmaniasis is endemic in Iran and is reported from 80 countries across the world. The disease is caused by more than 20 species of Leishmania and transmitted by nearly 30 species of sand flies species (Phlebotomus) (1). The disease presents four clinical syndromes, namely cutaneous leishmaniasis, mucocutaneous leishmaniasis (Espondia), visceral leishmaniasis (VL or kala-azar), and post kala-azar dermal leishmaniasis (PKDL) (2–4).
VL is a fatal systemic disease, which is caused by a L. donovani complex. There are two types of VL, which differ in their transmission characteristics: zoonotic visceral leishmaniasis (ZVL) is transmitted from animal to vector to human and anthroponotic visceral leishmaniasis (AVL) is transmitted from human to vector to human (3, 5).
Annually, 500,000 new cases and 50,000 deaths are reported from the disease worldwide (6). VL mainly occurs in six countries: India, Nepal, Bangladesh, Sudan, Ethiopia, and Brazil (7). A severe epidemic occurred in southern Sudan, with 100,000 deaths in a population of 280,000 people, from 1984 to 1994 (4, 8).
Kala-azar or VL, a Mediterranean disease widespread in Iran, is caused by L. infantum (9), the vector is Phlebotomous, and domestic dogs and wild canines are the major animal reservoirs host of VL in Iran (3, 10, 11). Rodents infected with L. infantum have also been reported in Meshkinshahr district, Iran (12).
In addition, VL is endemic in some parts of Iran such as Ardebil, Fars, and East Azerbaijan, Bushehr, Kerman, Qum and North Khorasan and is sporadic in some other areas. Most infections are seen in children, with fever, enlarged spleen and liver, and blood loss in all cells and can be fatal because of internal bleeding or secondary infections (3).
Based on the above findings about the prevalence of L. infantum and reports of cases of VL, two 17 year–old-boys with splenomegaly and seropositivity, in the Ilam Province six months ago, and lack of studies on the disease we decided to determine the prevalence of VL in this region for the first time.
Materials and Methods
Geographical area
Ilam Province is situated in the cold mountainous region of Iran at a height of 1,319 meters (4,330 ft) above sea level. It is located in the west of Iran at latitude of 33° 38′ north and longitude of 46° 26′ east. Although this province is surrounded by mountains, its climate is also affected by deserts from the west and the south. This region presents a highly variable annual weather profile. Heavy showers or snow in the winter and dusty, brutally hot, dry weather in the summer are common for this region. The climate is classed under the Köppen climate classification as a Mediterranean climate (Csa) but the seasonal variation in temperature is much greater than usual for this type of climate. This province has 7 counties (Fig. 1) and most of people have rural life. The local population is employed in agriculture and animal husbandry and dog plays a major role in protecting animals. According to the Census, statistical center of Iran, Ilam Province’s population in 2006 was equal to 545,787.
Fig. 1:
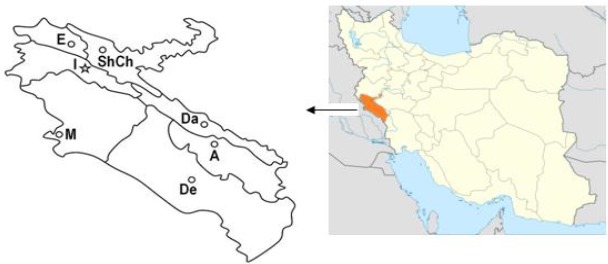
Situation and counties of Ilam Province in west of Iran. A (Abdanan), De (Dehloran), M (Mehran), Dareshahr, ShCh (Shirvanchardavol), I (Ilam), E (Eivan). Mehran, Abdanan, Dareshahr and Dehloran, areas are known as positive area for visceral leishmaniasis in this present study
Sampling methods and target groups
This descriptive cross-sectional study was carried out in the Mehran, Dehloran, Abdanan, and Dareshahr counties (Fig. 1), and multi stage clustering random method was used for sampling. From collected samples, 261 people had urban and 195 people had rural life. Subjects were primarily children aged 12 or under, while 10 percent were adult residents. The number of samples obtained was at a prevalence of 5%, confidence interval of 95% and coefficient error of 2%.
Using a sterile syringe, 2 ml of venous blood of each individual was collected and were transferred to the laboratory at the Ilam University of Medical Sciences, centrifuged for 5 minutes at 5000 rpm and serum was separated. After separation, the serum samples were kept in the freezer at −20 °C until testing. DAT was performed at the School of Public Health at Tehran University of Medical Sciences.
Sera were diluted 1:10 to 1:3200 into a dilution fluid (0.9% saline and 0.78% 2-mercaptoethanol) and poured in the V form 96 well plates containing the Iranian strain of VL antigens (L. infantum MCAN/IR/07/Moheb-gh). The results were read after 18 to 24 h of incubation in a wet chamber, at room temperature. Cut off point of 1:3200 or higher were considered positive.
Data were analyzed using SPSS software and significance test was examined using the chi-square test at P<.05.
Results
The names of districts and the number of samples that tested positive for antibodies against L. infantum are presented in Fig. 2, while the age and gender distribution of samples are listed in Table 1. Frequency of anti-Leishmania antibodies titers with DAT according to the age groups can be seen in Table 2. Of the 456 blood samples of subjects who were studied using the DAT test, 43 percent were positive for the anti-Leishmania antibodies. Thus, five subjects presented a titre of 1:400, 11 had a titer of 1:800, three patients had a titer of 1:1600, one had a titer of 1:3200 and one had a titer of 1:6400. People with titers of 1:3200 and 1:6400 had fever and splenomegaly. There was no significant difference between age group and the rate of seropositivity. Except one person from villages of Abdanan City, all of seropositive samples had urban life. The highest and lowest seroprevalence was observed in the age groups of 5–9 and >15 years old, respectively; however, gender did not influence the rate of seropositivity.
Fig. 2:
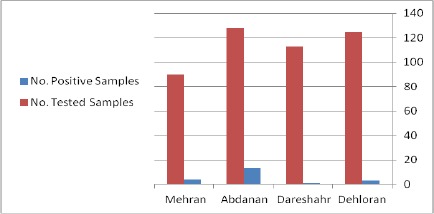
Study districts for detection of seroprevalence of human VL infection in Ilam province using DAT test at titer of 1/400 to 1/6400
Table 1:
Distribution of studied population for seroprevalence of human Leishmania infantum infection by gender and age groups in Ilam Province in 2013
| Age | Male | Female | Total | |||
|---|---|---|---|---|---|---|
| Groups (yr) | No. of Sera | Percent | No. of Sera | % | No. of Sera | % |
| 0–4 | 40 | 58.3 | 32 | 41.7 | 72 | 15.7 |
| 6–9 | 124 | 57.6 | 91 | 42.4 | 215 | 47.14 |
| 10–15 | 61 | 57 | 46 | 43 | 107 | 23.46 |
| >15 | 33 | 53.2 | 29 | 46.8 | 62 | 13.6 |
| Total | 258 | 56.57 | 198 | 43.42 | 456 | 100 |
Table 2:
Seroprevalence of human Leishmania infantum infection by direct agglutination test with anti-L. infantum antibodies by age groups in Ilam Province in 2012
| Age groups(yr) | No. of Sera | Antibody Titers | Total | ||||
|---|---|---|---|---|---|---|---|
| 1:400 | 1:800 | 1:1600 | 1:3200 | 1:6400 | |||
| 0–4 | 72 | 1 | 1 | 0 | 0 | 0 | 2 |
| 6–9 | 215 | 4 | 6 | 4 | 1 | 0 | 15 |
| 10–15 | 107 | 1 | 1 | 1 | 0 | 0 | 3 |
| >15 | 62 | 0 | 0 | 0 | 0 | 1 | 1 |
| Total | 456 | 5 | 11 | 3 | 1 | 1 | 21 |
Discussion
The present epidemiological study on kalaazar carried out in Ilam Province for the first time and obtained significant results. The results of this study revealed that VL could be circulated in Ilam, particularly in the south of the region.
Various seroepidemiological studies within Iran and outside have been conducted on humans and dogs, and different results have been obtained. Findings of current study are consistent with those of other studies on human in other parts of Iran. For example, in the study of human visceral leishmaniasis in Kermanshah Province, of the 1622 serum samples that were tested by DAT, six cases (0.33%) were positive (13). In addition, in a seroepidemiological study of visceral leishmaniasis using DAT in Bojnord City, North Khorasan Province, of the 1608 blood samples tested 38 subjects (2.36%) had a titer of 1:800 and only nine patients (0.56%) had a titer of 1:3200 (14). Moreover, in another study in Boyer-Ahmad City, 1628 blood samples from children 10 years were examined with DAT test and 50 cases of anti-visceral leishmaniasis antibodies were reported (15). The results of the above studies are different from the results of our present study and do not follow the same pattern. A possible explanation for these results may be due to different geographical conditions of Ilam, Kermanshah, and Bojnurd.
Several studies have also been conducted outside Iran. In a seroepidemiological study of visceral leishmaniasis in Basra (Iraq), the neighboring province of Ilam, 146 suspected cases were studied; 124 patients (84.9%) tested positive on bone marrow examination, 132 (91.1%) with the DAT test, and 3 (2%) with immunochromatography test. In Iraq, L. infantum is another highly prevalent agent of visceral leishmaniasis, possibly due to the high density of stray dogs and wild carnivores that act as a reservoir of the agent (16). In a study of the prevalence of visceral leishmaniasis in an endemic area in Mallorca (Spain), 100 dogs were studied. The clinical signs of canine Leishmania antibodies were examined and an infection rate of 26% was reported (17). A seroepidemiological study of canine visceral leishmaniasis in Iran identified that 14.2% of dogs in the endemic areas (North West 18.2%, Center 12.3%, South West 4.4%) had anti-L. infantum antibodies (18). According to report by Avizhe about the prevalence of visceral leishmaniasis in dogs in urban and rural areas of Ahvaz using DAT test, 2.6% of urban dogs and 16.3% of rural dogs have been infected with VL (19). Khanmohammadi reported that the incidence of serum visceral leishmaniasis, among 384 dogs that were selected randomly from 30 villages of Sarab, is 9.1% (20). In a study for VL carried out in Spanish cats (233 cats), seropositivity was reported 1.23% (3/233) (17).
On examining the results of the studies conducted on dogs, we noticed that the prevalence of antibodies against canine visceral leishmaniasis is very different in each area. Outbreak of visceral leishmaniasis, in addition to dogs and wild carnivores, is related to other factors such as single-carrier frequency, sand flies lost, the temperature and humidity, pets, protection of individuals against sand fly bites, the type of home, and lifestyle. Poorly built homes are more easily infected by sand flies and are ideal sites for insects’ reproduction. Thus, differences in the prevalence appear naturally in various areas.
Conclusion
Visceral leishmaniasis could potentially be an important health problem in Ilam. However, further research and development on healthcare facilities, medical and diagnostic methods are essential to evaluate the extent of the disease in the region.
Acknowledgments
The authors would like to thanks deputy of research and technology of Ilam University of Medical Sciences for financial support and for their cooperation with this research project. The authors declare that there is no conflict of interests.
References
- 1.Pearson RD, Sousa AQ.Clinical spectrum of Leishmaniasis. Clin Infect Dis. 1996; 22: 1– 13. [DOI] [PubMed] [Google Scholar]
- 2.Arevalo J.Influence of Leishmania ( viannia) species on the response to antimonial treatment in patients with american tegumentary leishmaniasis. J Infect Dis. 2007; 195: 1846– 51. [DOI] [PubMed] [Google Scholar]
- 3.Mohebali M.Visceral leishmaniasis in Iran: Review of the Epidemiological and Clinical Features. Iran J Parasitol. 2013; 8( 3): 348– 58. [PMC free article] [PubMed] [Google Scholar]
- 4.Mohebali M.Epidemiological Status of Visceral Leishmaniasis in Iran: Experiences and Review of Literature. J Clin Exp Pathol. 2012: S3: 003. [Google Scholar]
- 5.François C, Shyam S, Asrat H, Hashim G, Suman R, Rosanna WP, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Microbiology. 2007; 5: 873– 82. [DOI] [PubMed] [Google Scholar]
- 6.Desjeux P.Leishmaniasis: current situation and new perspectives. Comp Immunol Microbiol Infect Dis. 2004; 27( 5): 305– 18. [DOI] [PubMed] [Google Scholar]
- 7.Boelaert M.Visceral leishmaniasis control: a public health perspective. Trans R Soc Trop Med Hyg. 2000; 94: 465– 71. [DOI] [PubMed] [Google Scholar]
- 8.Seaman J, Mercer AJ, Sondorp E.The epidemic of visceral leishmaniasis in western Upper Nile, southern Sudan: course and impact from 1984 to 1994. Int J Epidemiol. 1996; 25: 862– 71. [DOI] [PubMed] [Google Scholar]
- 9.Hajjaran H, Mohebali M, Mamishi S, Vasigheh F, Oshaghi MA, Naddaf SR, et al. Molecular Identification and Polymorphism Determination of Cutaneous and Visceral Leishmaniasis Agents Isolated from Human and Animal Hosts in Iran. Bio Med Res Int. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohebali M, Hajjaran H, Hamzavi Y, Mobedi I, Arshi S, Zarei Z.Epidemiological aspects of canine visceral leishmaniasis in the Islamic Republic of Iran. Vet Parasitol. 2005; 129: 243– 51. [DOI] [PubMed] [Google Scholar]
- 11.Mohebali M, Edrissian Gh, Shirzadi MR, Akhoundi B, Hajjaran H, Zarei Z, et al. An observational study on the current distribution of visceral leishmaniasis in different geographical zones of Iran and implication to health policy. Travel Med Infect Dis. 2011; 9( 2): 67– 74. [DOI] [PubMed] [Google Scholar]
- 12.Mohebali M, Poormohammadi B, Kanani A.Gerbillidae and Cricitidae, other animal hosts of visceral leishmaniasis in Meshkin-shahr district of Iran. East Mediterr Health J. 1998; 4234– 8. [Google Scholar]
- 13.Hamzavi Y, Hamzeh B, Mohebali M, Akhoundi B, Ajhang K, Khademi N, et al. Human Visceral Leishmaniasis in Kermanshah Province, Western Iran, During 2011–2012. Iran J Parasitol. 2012; 7( 4): 49– 56. [PMC free article] [PubMed] [Google Scholar]
- 14.Mohebali M, Edrisian Gh, Keshavarz H, Mohajeri M, Hajaran H, Akhundi B.Seroepidemiological survey of visceral leishmaniasis using Direct agglutination test(DAT) in Bojnord ( north Khorasan). J Epidemiol. 2007; 4( 3): 43– 50. [Google Scholar]
- 15.Sarkari B, Moshfe A, Pedram N, Mohebali M, Akhoundi B.Seroepidemiologic survey of visceral leishmaniasis in Boirahmad city. Journal of Armaghane Danesh. 2006; 12( 2): 69– 77. [Google Scholar]
- 16.Hameed Gani Z, Meaad Kadhum H, Abdul-Mohsin HJ.Seroepidemiological study of Visceral Leishmaniasis in Basrah, Southern Iraq. J Pak Med Assoc. 2010; 60: 464– 9. [PubMed] [Google Scholar]
- 17.Ayllon A, Tesouro MA, Amusategui I, Villaescusa A, Rodriguez-Franco F, Sainza A.Serologic and Molecular Evaluation of Leishmania infantum in Cats from Central Spain. Ann NY Acad Sci. 2008; 1149: 361– 4. [DOI] [PubMed] [Google Scholar]
- 18.Mohebali M, Hajjaran H, Hamzavi Y, Mobedi I, Arshi S, Zarei Z, et al. Epidemiological aspects of canine visceral leishmaniasis in the Islamic Republic of Iran. Vet Parasitol. 2005; 129243– 51. [DOI] [PubMed] [Google Scholar]
- 19.Avizeh R, Mohebali M, Sheikholslami M.Seroepidemiological investigation of visceral leishmaniasis in dogs of Ahvaz district, Iran. Arch Razi Institute. 2007; 62( 1): 31– 7. [Google Scholar]
- 20.Khanmohammadi M, Fallah E, Rahbari S, Sohrabi I, Farshchian M, Hamzavi F.Seroepidemiological survey of canine visceral leishmaniasis in Sarab District, East Azerbaijan Province, Northwest of Iran in 2009. Afr J Microbiol Res. 2010; 4( 19): 2022– 8. [Google Scholar]


