INTRODUCTION
Since Obwegeser's description of the use of LeFort I advancement to improve midface deficiency, the procedure has been adopted by many surgeons.1 In the hierarch of stability, the operation ranks high for maintaining maxillary projection.2,3 Vertical instability is commonly associated with the procedure, especially when the maxilla is advanced and inferiorly displaced. This vertical instability is caused by stretching of the muscles of mastication, as occurs when the mandibular angle and ramus are rotated downward and backward. The vertical relapse occurs short term and is minimal after six months post surgery. When the maxilla is moved superiorly as well as anteriorly, vertical stability is more predictable.
Prior to the availability of bone plates and screws, LeFort I osteotomy was stabilized with wire fixation alone and/or in combination with bone grafts and intermaxillary fixation. Once mini-plates became commercially available, most surgeons quickly adopted them for stabilizing maxillary advancement, primarily because of the elimination of the need for intermaxillary fixation.6
Bioresorbable materials are not new, but polylactate bioresorbable bone plates and screws have been commercially available in the USA for only the past 12 years. Multiple studies have been published reporting the use of these materials in the facial skeleton and their benefits, especially with orthognathic surgery. Several studies demonstrate good stability when they are used to stabilize mandibular osteotomies, but fewer studies are available demonstrating acceptable stability when used for stabilizing maxillary osteotomies.7,8,9,10 No studies have compared stability of maxillary advancement via LeFort I osteotomy over time when stabilized with polylactate bioresorbable and titanium devices.
The purpose of this study was to analyze the stability of LeFort I advancement one year post surgery comparing polylactate (PLLDL 70/30) and titanium devices.
MATERIALS AND METHODS
From the UNC Dentofacial Data Base 57 patients who underwent isolated maxillary advancement with at least one year follow up were identified spanning the years 2000 to 2010. This retrospective study was approved by the Biomedical Institutional Review Board. Patients with craniofacial, traumatic or pathological etiology were excluded from the study as were those who did not have preoperative, immediate postoperative, and at least one year postoperative cephalometric radiographs. Twenty-seven patients underwent isolated maxillary advancement and each was stabilized with 4 bioresorbable plates and screws (Group R). Thirty patients were identified who underwent a similar operation but were stabilized with titanium bone plates and screws (Group M).
The bioresorbable material used was polylactate PLLDL(70/30), 2mm plates and screws that were manufactured either by injection molding or extrusion. They were provided by 2 vendors, Inion CPS (Tampera Finland) and Bionx Ltd. Corp (Con Med Lindvitec, Key Largo, Florida). The titanium hardware was either 2mm Liebinger or 2mm Synthes titanium orthognathic systems. All patients underwent pre- and postsurgical orthodontic care. The operations were conducted at UNC Hospitals under general anesthesia with modified hypotension by three experienced faculty surgeons utilizing similar techniques A traditional or high level LeFort I osteotomy was completed and stabilized with 2mm bone plates and screws placed bilaterally at the piriform aperture and zygomaticomaxillary buttress. In most patients occlusal splints were used with guiding intermaxillary elastics for 6 weeks post surgery.
All cephalograms were obtained in identical format and were traced and digitized by the same technician using the UNC digitized model. The technique, reliability and reproducibility of the method have previously been published.12 The principal outcome variables considered most important clinically were the changes in maxillary forward movement from immediately post surgery to follow up. Analysis of covariance was used to compare the post-surgical change between the two stabilization methods. Stabilization method was the primary explanatory variable, the post-surgical position was included as a covariate as well as the interaction term with the stabilization method. Demograpic characteristics (sex, race) and clinical covariates of interest (use of bone grafts; segmentation of the maxilla) were compared between the two stabilization methods using Fisher's Exact test. Age at surgery and the amount of surgical change were compared using unpaired t-tests. Level of significance was set at 0.05.
Results
A total of 57 patients met the criteria for inclusion, 27 were stabilized using bioresorbable devices (Group R) and 30 were stabilized using titanium devices (Group M). The demographic characteristics for the groups were similar (P> 0.17). Average ages were similar in the two groups (Table 1) and more subjects in each group were female, Group R 74% and Group M 55%. The majority of subjects in each group had single segment maxillary osteotomies, Group R 63% and Group M 63%. Substantially more patients in Group R had bone grafts (88.9%) than in Group M (47%). (Table 1).
Table 1.
Descriptive Statistics for Demographic and Clinical Characteristics of the Two Fixation Method Groups
| Group R (n = 27) | Group M (n = 30) | p-Value | ||
|---|---|---|---|---|
| Age | 19.7±5.5 | 20.8±6.4 | 0.50 | |
| Gender | Female | 20 (74.0%) | 16 (53.3%) | 0.17 |
| Male | 7 (26.0%) | 14 (46.7%) | ||
| Race | Asian | 2 (7.7%) | 0 (0.0%) | 0.67 |
| African-American | 2 (7.7%) | 2 (6.7%) | ||
| Caucasian | 19 (69.2%) | 22 (73.3%) | ||
| Native American | 2 (7.7%) | 2 (6.7%) | ||
| Other | 2 (7.7%) | 4 (13.3%) | ||
| Lefort I | Single | 17 (63.0%) | 19 (63.3%) | 1.00 |
| Segmented | 10 (37.0%) | 11 (36.7%) | ||
| Bone Graft | Yes | 24 (88.9%) | 14 (46.7%) | 0.001 |
| No | 3 (11.1%) | 16 (53.3%) |
Surgical Movement
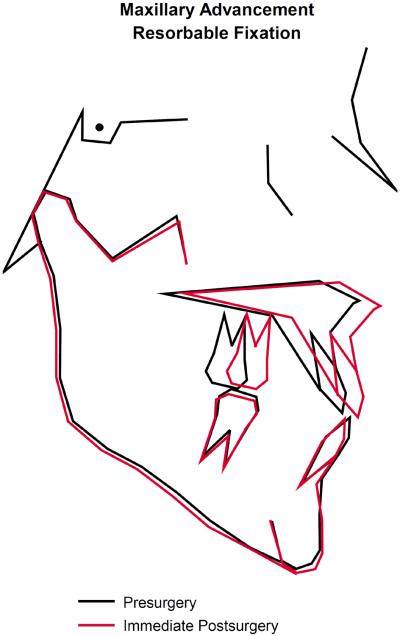
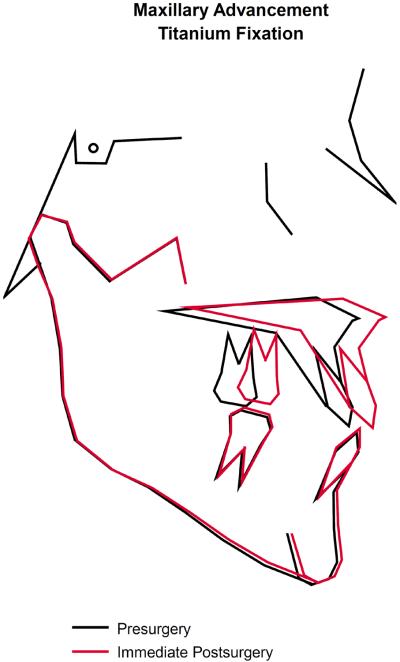
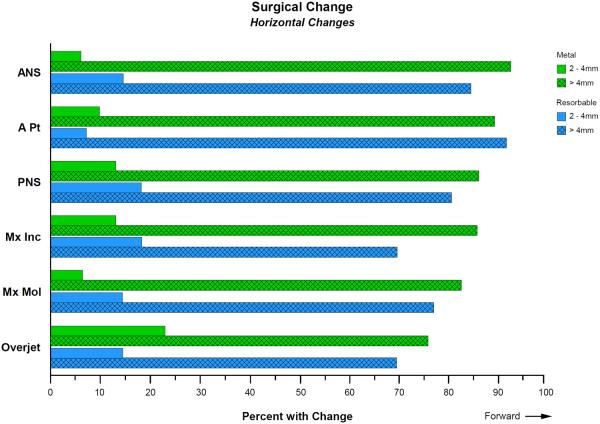
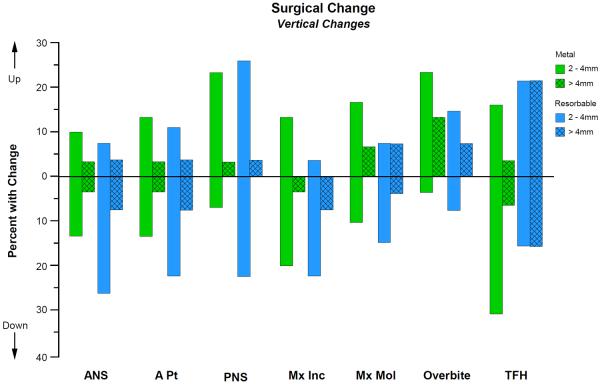
In general, the mean amount of skeletal and dental advancement was significantly different in the two groups with the average horizontal movement less.in Group R than in Group M. At point A subjects in Group R were advanced a mean of 5.6mm (SD±1.3mm) and Group M a mean of 7.1mm (SD±2.3mm). At PNS the forward movement for Group M was a mean of 6.9mm (SD±2.6mm) and a mean 5.5mm (SD±1.8mm) for Group R. (Table 2). The mean vertical skeletal movement between the groups was subtly but not statistically significantly different, The maxilla moved down, increasing face height a mean of 0.8mm (SD±4.6mm) in Group R and up, decreasing face height 0.7mm (SD±3.2mm) in Group M. The vertical dental movements were slightly different with Group R demonstrating inferior movement in both the incisors and molars while the Group M dental movements were inferiorly for the incisors and superiorly for the molars. The differences in movement between the groups were minimal and not statistically significant (Table 2 and Figures 1A and 1B).
TABLE 2.
MEAN AND STANDARD DEVIATION FOR EACH OF THE SURGICAL MOVEMENTS SEPARATELY BY FIXATION METHOD GROUP
| Movement | Measure | Group R Mean ± S.D. | Group M Mean ± S.D. | p-Value |
|---|---|---|---|---|
| X (Horizontal) | ANS | 5.81 ± 1.59 | 7.15 ± 2.34 | 0.02 |
| A Point | 5.61 ± 1.30 | 7.07 ± 2.30 | 0.005 | |
| PNS | 5.46 ± 1.75 | 6.85 ± 2.59 | 0.02 | |
| Max Inc | 4.76 ± 1.84 | 6.50 ± 2.43 | 0.004 | |
| Max Mol | 5.63 ± 2.32 | 6.40 ± 3.27 | 0.31 | |
| Overjet | 5.60 ± 3.29 | 6.03 ± 2.41 | 0.57 | |
| Y (Vertical) | ANS | 0.95 ± 2.74 | −0.08 ± 2.14 | 0.12 |
| A Point | 0.84 ± 2.53 | −0.13 ± 2.01 | 0.11 | |
| PNS | −0.34 ± 2.37 | −1.01 ± 1.79 | 0.23 | |
| Max Inc | 1.21 ± 2.36 | 0.27 ± 2.05 | 0.11 | |
| Max Mol | 0.18 ± 2.39 | −0.64 ± 2.26 | 0.19 | |
| Overbite | 0.63 ± 2.33 | 1.32 ± 2.87 | 0.32 | |
| Tot Face Ht | 0.59 ± 4.59 | −0.67 ± 3.16 | 0.23 |
Figure 1A.
Figure 1B.
When examining Figure 1A, there is a striking similarity in the horizontal changes that occurred at surgery in both groups. All measures had very closely matched percentages of patients experiencing the same amounts of advancement. The percentages of patients experiencing vertical changes in both groups are also similar but the percentage of patients experiencing inferior movement of most skeletal and dental landmarks in Group R exceeds that of Group M (Figure 1B). In both groups PNS moved superiorly in almost identical percentages of patients but there was a greater percentage of patients who experienced inferior movement in group R. Also, the percentage of patients in Group R who experienced an increase in total face height exceeded Group M but a similar percentage in both groups experienced reduction of total face height.
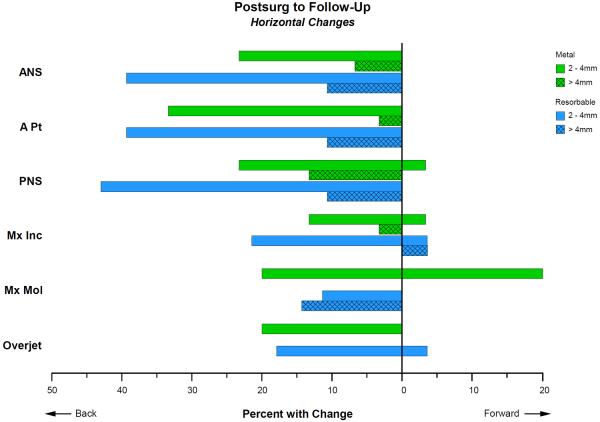
Postsurgical Movement
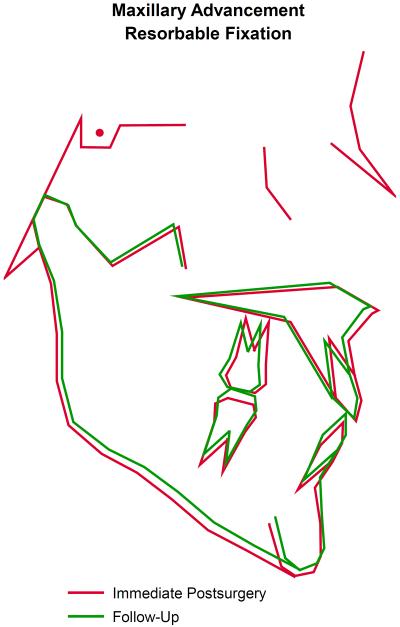
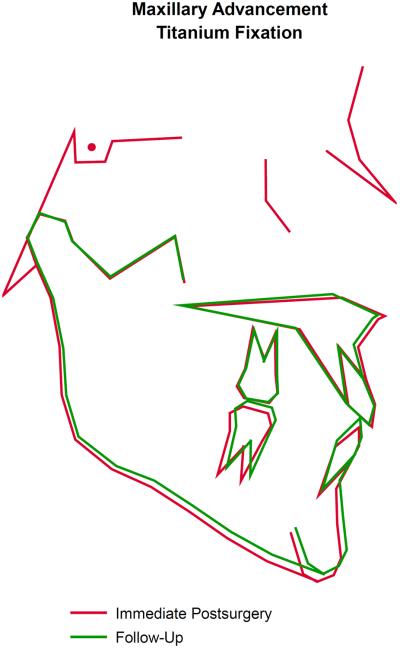
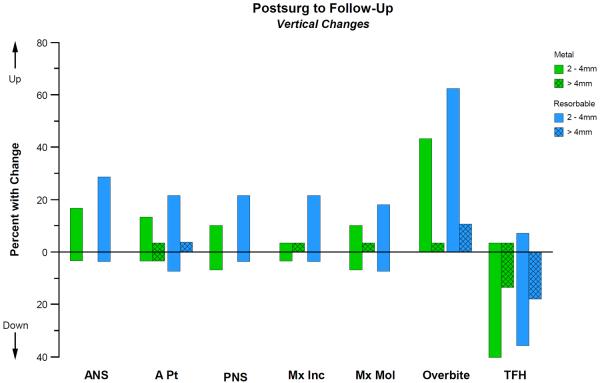
From immediate post surgery to 1 year post surgery, the direction of movement was similar in the two groups. The average magnitude of movement differed (Table 3 and Figures 2A and 2B) but were not statistically significantly different (P>0.16). In both groups, the maxilla moved posteriorly and superiorly with Group R exceeding the measures of Group M. The frequency distribution graphs demonstrated a greater percentage of patients experiencing changes in Group R in most measures, with the exception of the maxillary molar in Group M (graphs 3 and 4). The maxillary molar was as likely to move posteriorly as it was to move anteriorly in Group M but only posterior movement was noted in Group R. The maxillary incisors of Group R were also noted to move further forward compared to Group M in a greater number of patients. The total face height was reduced in both groups. Similar vertical changes (primarily superior movement) were noted to occur in both groups with the frequency of occurrence favoring Group R.
TABLE 3.
MEAN AND STANDARD DEVIATION FOR EACH OF THE POST SURGERY TO FOLLOW-UP (1 YEAR) MOVEMENTS SEPARATELY BY FIXATION METHOD GROUP
| Movement | Measure | Group R Mean ± S.D. | Group M Mean ± S.D. | p-Value |
|---|---|---|---|---|
| X (Horizontal) | ANS | −2.31 ± 2.02 | −1.67 ± 1.90 | 0.79 |
| A Point | −2.06 ± 1.91 | −1.34 ± 1.34 | 0.33 | |
| PNS | −2.03 ± 1.62 | −1.84 ± 2.61 | 0.94 | |
| Max Inc | −0.65 ± 1.91 | −0.62 ± 1.60 | 0.16 | |
| Max Mol | −1.55 ± 1.77 | 0.00 ± 2.03 | 0.22 | |
| Overjet | −0.70 ± 1.43 | −0.67 ± 1.39 | 0.18 | |
| Y (Vertical) | ANS | −0.78 ± 2.02 | −0.51 ± 1.41 | 0.94 |
| A Point | −0.75 ± 1.91 | −0.56 ± 1.85 | 0.35 | |
| PNS | −0.68 ± 1.62 | −0.46 ± 1.36 | 0.90 | |
| Max Inc | −0.76 ± 1.27 | −0.36 ± 1.43 | 0.98 | |
| Max Mol | −0.22 ± 1.76 | −0.14 ± 1.73 | 0.47 | |
| Overbite | 2.25 ± 1.60 | 2.06 ± 1.25 | 0.58 | |
| Tot Face Ht | −1.99 ± 2.43 | −2.21 ± 2.27 | 0.56 |
Figure 2A.
Figure 2B.
Overbite and overjet comparisons between the groups demonstrated similarity. The average differences were small and were not statistically significant..
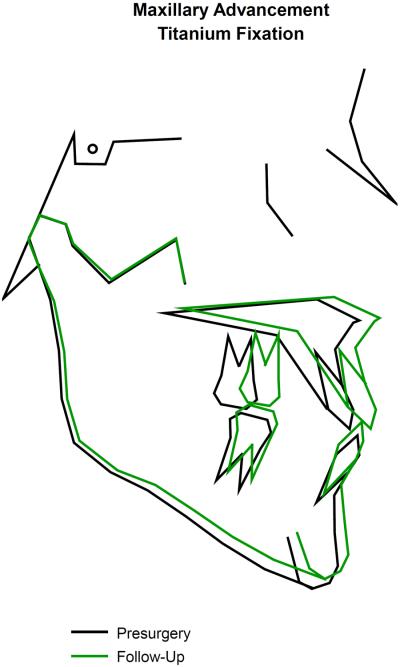
Presurgery to 1-Year Follow-up
From presurgery to 1-year postsurgery, the results are similar, but the average maxillary anterior movement in Group M exceeded Group R. Vertically, there was more superior movement in Group M and inferior movement in Group R. This was reflected in all skeletal and dental landmarks, as well as the total face height. T (Table 4, Figures 3A and 3B).
TABLE 4.
MEAN AND STANDARD DEVIATION FOR EACH OF THE PRE SURGERY TO FOLLOW-UP (1 YEAR) MOVEMENTS SEPARATELY BY FIXATION METHOD GROUP
| Movement | Measure | Group R Mean ± S.D. | Group M Mean ± S.D. |
|---|---|---|---|
| X (Horizontal) | ANS | 3.50 ± 1.72 | 5.48 ± 2.91 |
| A Point | 3.55 ± 2.10 | 5.73 ± 2.75 | |
| PNS | 3.42 ± 1.62 | 5.01 ± 2.83 | |
| Max Inc | 4.10 ± 2.46 | 5.88 ± 2.99 | |
| Max Mol | 4.07 ± 2.83 | 6.40 ± 3.19 | |
| Overjet | 4.90 ± 2.85 | 5.36 ± 2.74 | |
| Y (Vertical) | ANS | 0.17 ± 2.13 | −0.60 ± 1.93 |
| A Point | 0.09 ± 1.99 | −0.69 ± 2.42 | |
| PNS | −1.02 ± 1.94 | −1.47 ± 2.01 | |
| Max Inc | 0.46 ± 2.14 | −0.10 ± 2.24 | |
| Max Mol | −0.04 ± 2.05 | −0.78 ± 2.67 | |
| Overbite | 2.88 ± 1.83 | 3.38 ± 2.64 | |
| Tot Face Ht | −1.39 ± 3.50 | −2.88 ± 3.03 |
Figure 3.
There is striking similarity in the percentage of patients experiencing horizontal movements in the same direction and magnitude in both groups
The pre-operative to one-year follow-up composite tracings are presented in Figures 4A and 4B. In both groups, the maxilla was advanced and maintained positive overjet and overbite. There was superior rotation of the mandible in both groups from the immediate postsurgery compared to the one year postsurgical position.
Figure 4.
The percentage of patients experiencing vertical changes in both groups are similar but the percentage of patients experiencing inferior movement in Group R exceeds Group M.
Clinical Changes
At one-year follow-up, all patients experienced improvement in facial esthetics and in overjet. No patient in either group required additional surgery. Six patients were in an edge to edge incisal position at one year. Three were in Group R and three in Group M.
There was no association noted between the amount of relapse and the amount of advancement, or the use of bone grafts or LeFort I segmental surgery.
DISCUSSION
Bioresorbable devices offer many potential benefits compared to metal devices, since they are eventually eliminated from the body over time without the need for additional surgery. A great deal of patient appeal is associated with their use12, but potential advantages, such as delivering bone healing proteins, have not been developed and made available. Although recent publications indicate that titantium is not as innocuous as once believed, to date its long-term presence in the human body has not been linked to any known medical condition..14,15 The incidence of the need to remove these metals in an orthognathic surgery population has been reported to be 10 percent.16 Bioresorbable materials gradually lose strength and integrity and are eventually eliminated from the body as water and carbon dioxide. It has previously been reported that when used in the midface there is about a 4 percent chance of a patient developingan inflammatory reaction significant enough to require removal.13
The use of bioresorbables to stabilize facial osteotomies has been studied by many, including our group. Previously, we reported on stabilizing mandibular advancement with sagittal osteotomy and found no differences in stability when compared to titanium.9 This study is the first to report on the stability of isolated maxillary advancement in similar cohorts, comparing postsurgical changes between one group stabilized with titanium and another group stabilized with polylactate bioresorbables.
In both groups, the patterns of relapse from immediate postsurgery to one year were similar (posterior movement). The magnitude of postsurgical movement in Group R exceeded Group M but was of no clinical or statitistical significance. More mobility of the maxilla in Group R patients was noted during the first several months following surgery since the material is not as rigid as titanium but changes were not clinically important and all patients experienced union. This lack of rigidity actually may be advantageous to the completion of postsurgical orthodontic treatment since elastic traction can effect skeletal as well as dental movements. The net overjet remaining in both groups at one year suggest that the surgical movement remaining was adequate in both groups to allow for satisfactory completion of orthodontic care.
The greater anterior movement of MXM in Group R at one year, but less movement of incisors could be explained by postsurgical orthodontic treatment differing between the groups.
In all patients, the esthetic outcome was positive. The fact that three patients in each group had end on incisal relationships at one year postsurgery indicates that 12% of the patients treated in this study completed care without positive overjet. Eighty-eight percent of the patients finished with positive overjet, suggesting a relatively high rate of success with LeFort I advancement in both groups.
The reduction of face height in both groups at one year reflects the removal of the occlusal splint more so than skeletal or dental movements appear decreased during the post-surgical period.
Figure 5A.
Figure 5B.
Figure 6.
Frequency distributions for horizontal changes noted from immediate post surgery to one year. Notice that more patients in group R experienced more movement of each measure with the exception of the maxillary molar.
Figure 7.
Frequency distribution for vertical changes noted from immediate post surgery to one year. The direction of movement for each measure in both groups was similar but more patients in group R experienced a change.
References
- 1.Obwegeser HL. Surgical correction of small or retrodisplaced maxillae: the “dish-face” deformity. Plast Reconstr Surg. 1969 Apr;43(4):351–65. doi: 10.1097/00006534-196904000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996;11(3):191–204. [PubMed] [Google Scholar]
- 3.Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predicatability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007 Apr 30;3:21. doi: 10.1186/1746-160X-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Proffit WR, Phillips C, Prewitt JW, Turvey TA. Stability after surgical-orthodotnic correction of skeletal Class III malocclusion. 2:maxillary advancement. Int J Adult Orthodon Orthognath Surg. 1991;6(2):71–80. [PubMed] [Google Scholar]
- 5.Egbert M, Hepworth B, Myall R, West R. Stability of LeFort I osteotomy with maxillary advancement; a comparison of combined wire fixation and rigid fixation. J Oral Maxillofac Surg. 1995 Mar;53(3):243–8. doi: 10.1016/0278-2391(95)90217-1. [DOI] [PubMed] [Google Scholar]
- 6.Waite PD, Tejeera TJ, Anucul B. The stability of maxillary advancement using LeFort I osteotomy with and without genial bone grafting. Int J Oral Maxilloafac Surg. 1996 Aug;25(4):264–267. doi: 10.1016/s0901-5027(06)80052-4. [DOI] [PubMed] [Google Scholar]
- 7.Dhol W, Reyneke JP, Thompson B, Sandor G. Comparison of titanium and resorbable co-polymer fixation after LeFort I impaction. Am. J. Orthod. Dentofacial Orthoped. 2008;134:67–73. doi: 10.1016/j.ajodo.2006.04.049. [DOI] [PubMed] [Google Scholar]
- 8.Cheung LK, Yip HIS, Chow RLK. Stability and morbidity of LeFort I osteotomy with bioresorbable fixation: a randomized controlled trial. Int J Oral Maxillofac Surg. 2008:232–241. doi: 10.1016/j.ijom.2007.09.169. [DOI] [PubMed] [Google Scholar]
- 9.Turvey TA, Bell RB, Phillips C, Proffit WR. Self-reinforced biodegradable screw fixation compared to titanium screw fixation in mandibular advancement. J. Oral and Maxillofac Surg. 2006;64:40–46. doi: 10.1016/j.joms.2005.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landis CA, Ballon A. Skeletal stability in bimaxillary orthognathic surgery: PLLPL resorbable vs. titanium osteofixation. Plast Reconstr Surg. 2006;118:703–710. doi: 10.1097/01.prs.0000232985.05153.bf. [DOI] [PubMed] [Google Scholar]
- 11.Haers PE, Sailer HF. Biodegradable self reinforced poly-L/DL-lactide screws and plates in bimaxillary orthognathic surgery: short term skeletal stability and material related failure. J Craniomaxillofac Surg. 1998;26:363–370. doi: 10.1016/s1010-5182(98)80069-3. [DOI] [PubMed] [Google Scholar]
- 12.Forrsell K, Turvey TA, Phillips C, Proffit WR. Superior repositioning of the maxilla and mandibular advancement: Rigid fixation makes a difference. J. Ortho Dentofac Orthoped. 1992;102:342–350. doi: 10.1016/0889-5406(92)70050-K. [DOI] [PubMed] [Google Scholar]
- 13.Turvey TA, Proffit WR, Phillips C. Biodegradable fixation for craniomaxillofacial surgery: A 10 year experience involving 761 operations and 745 patients. Int J Oral Maxillfac Surg. 2011;40:244–249. doi: 10.1016/j.ijom.2010.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Acero J, Calderon J, Sahmeson JI, Verdauger JJ, Concego C, Samocaro ML. The behavior of titanium as a biomaterial; microscopy study of plate and surrounding tissues in facial osteosynthesis. J. Craniofaxillofac Surg. 1999;27:117–123. doi: 10.1016/s1010-5182(99)80025-0. [DOI] [PubMed] [Google Scholar]
- 15.Schliephake H, Lehmann H, Kunz U, Schmelzelsen H. Ultrastructural findings in soft tissues adjacent to titanium plates used in jaw fracture treatment. Int J. Oral and Maxillofac Surg. 1993:22–25. doi: 10.1016/s0901-5027(05)80350-9. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt BJ, Perrot DH, Mahan D, Kearns G. The removal of plates and screws after LeFort I osteotomy. J. Oral Maxillfac Surg. 1998;56:184–190. doi: 10.1016/s0278-2391(98)90865-5. [DOI] [PubMed] [Google Scholar]