In 2011, we reported that the incidence of childhood narcolepsy increased several fold in China following the H1N1winter flu pandemic (pH1N1) 1. In parallel with this report, increased incidence was also reported in several countries in Northern Europe, with many children developing the disease following administration of Pandemrix, an adjuvanted pH1N1 vaccine. Studies in Sweden, Finland, and Norway have shown a 4-13 fold increased risk of developing childhood narcolepsy following Pandemrix (only 1 of 16,000 vaccinated children developed narcolepsy, however) 2,3,4. These results bolster the claim that narcolepsy, an autoimmune disease caused by hypocretin cell loss, could be triggered by H1N1 vaccination or infection.
Further evidence of causality may come from studying narcolepsy incidence following the pandemic, as H1N1 infections decreased in subsequent seasons. In Figure 1, we report on the evolution of new onset cases at Beijing University. For better comparison, we only present data on cases diagnosed within one year of onset, so that data is comparable to prior years. Data from 2012 is also included, although curtailed until September, so that a few cases with onset in the first three months of 2012 will still be identified (denoted with a star and not used in any statistical analysis). As can be seen, a return to baseline is evident, suggesting that indeed the 2009-2010 winter was a unique event.
Figure 1.
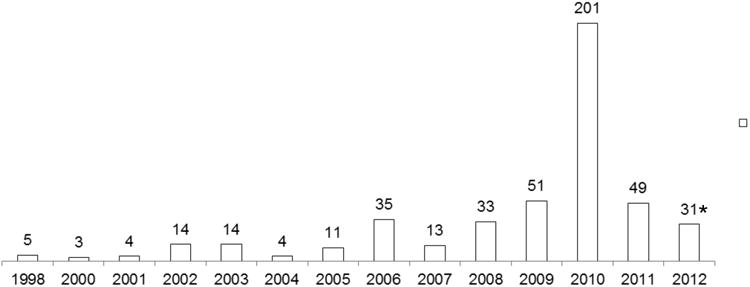
Yearly counts of new narcolepsy onset occurrences (diagnosed within 1 year) in 468 patients with narcolepsy/hypocretin deficiency diagnosed at the People's Hospital, Beijing University, China. *=data curtailed after September 1st, 2013.
We next examined whether patients identified following the pH1N1 pandemic season differed clinically. As before, to avoid issues pertaining to evaluation time since onset, we only compared subjects diagnosed within a year of onset. In 1998-2009, 2010 and 2011 respectively, 187, 201 and 41 subjects were identified (mean ±SEM delay to diagnosis: 4.7±0.3; 4.4± 0.2 and 4.6±0.4 months). Sex, body mass index, age at diagnosis as well as occurrence and age of onset of each narcolepsy symptom, namely sleepiness, cataplexy, sleep paralysis, hypnagogic hallucination and disturbed nocturnal sleep and sleep recording findings (Multiple Sleep Latency Tests, Apnea Hyponea Index) were next compared across the three groups. Remarkably few differences were found. First, although mean age of onset in subjects diagnosed in 2010 was younger than those diagnosed before and after 2010, differences were not statistically significant (8.7 ±0.4 y in 2010 versus 10.0±0.7y before and 10.1±1.7 y in 2011, p=0.2). Second, SOREMPs during the multiple latency tests were more numerous in cases diagnosed in 2010 versus others, whether or not controlled with age (4.65 ±0.05 in 2010 versus 4.32±0.05 before and 4.00±0.18 y in 2011, p<0.001), suggesting increased severity. All other parameters were similar across groups. We conclude that pH1N1 infections during the 2009-2010 season have played a role in triggering narcolepsy in children, but that the phenotypes of these cases is not distinguishable from prior cases.
Acknowledgments
This work was supported by research grants from NSFC (81070069), The Sino-German Center for Research Promotion (GZ538) and Beijing Municipal Science &Technology Commission (D1011000050010029) to F. Han and NIH-NS23724 grant to E. Mignot. We thank parents and most importantly the children for their participation.
Footnotes
Potential conflict if interest: Nothing to report
References
- 1.Han F, Lin L, Warby SC, et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Annals of neurology. 2011 Sep;70(3):410–7. doi: 10.1002/ana.22587. [DOI] [PubMed] [Google Scholar]
- 2.Partinen M, Saarenpaa-Heikkila O, Ilveskoski I, et al. Increased Incidence and Clinical Picture of Childhood Narcolepsy following the 2009 H1N1 Pandemic Vaccination Campaign in Finland. PLoS One. 2012;7(3):e33723. doi: 10.1371/journal.pone.0033723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nohynek H, Jokinen J, Partinen M, et al. AS03 Adjuvanted AH1N1 Vaccine Associated with an Abrupt Increase in the Incidence of Childhood Narcolepsy in Finland. PLoS One. 2012;7(3):e33536. doi: 10.1371/journal.pone.0033536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Centre for Disease Prevention and Control (ECDC) Vaccine Adverse Event Surveillance & Communication (VAESCO) network report. Stockholm: Sep, 2012. Narcolepsy in association with pandemic influenza vaccination – a multi-country European epidemiological investigation. http://www.ecdc.europa.eu/en/publications/Publications/Forms/ECDC_DispForm.aspx?ID=959. [Google Scholar]


