Abstract
Background
Low adherence to pharmacological treatments is one of the factors associated with poor blood pressure control. Questionnaires are an indirect measurement method that is both economic and easy to use. However, questionnaires should meet specific criteria, to minimize error and ensure reproducibility of results. Numerous studies have been conducted to design questionnaires that quantify adherence to pharmacological antihypertensive treatments. Nevertheless, it is unknown whether questionnaires fulfil the minimum requirements of validity and reliability. The aim of this study was to compile validated questionnaires measuring adherence to pharmacological antihypertensive treatments that had at least one measure of validity and one measure of reliability.
Methods
A literature search was undertaken in PubMed, the Excerpta Medica Database (EMBASE), and the Latin American and Caribbean Health Sciences Literature database (Literatura Latino-Americana e do Caribe em Ciências da Saúde [LILACS]). References from included articles were hand-searched. The included papers were all that were published in English, French, Portuguese, and Spanish from the beginning of the database’s indexing until July 8, 2013, where a validation of a questionnaire (at least one demonstration of the validity and at least one of reliability) was performed to measure adherence to antihypertensive pharmacological treatments.
Results
A total of 234 potential papers were identified in the electronic database search; of these, 12 met the eligibility criteria. Within these 12 papers, six questionnaires were validated: the Morisky–Green–Levine; Brief Medication Questionnaire; Hill-Bone Compliance to High Blood Pressure Therapy Scale; Morisky Medication Adherence Scale; Treatment Adherence Questionnaire for Patients with Hypertension (TAQPH); and Martín–Bayarre–Grau. Questionnaire length ranged from four to 28 items. Internal consistency, assessed by Cronbach’s α, varied from 0.43 to 0.889. Additional statistical techniques utilized to assess the psychometric properties of the questionnaires varied greatly across studies.
Conclusion
At this stage, none of the six questionnaires included could be considered a gold standard. However, this revision will assist health professionals in the selection of the most appropriate tool for their individual circumstances.
Keywords: validation, hypertension, medication, compliance, scale, validity, reliability
Introduction
Hypertension is a major public health concern worldwide. It is one of the leading risk factors for cardiovascular disease and is associated with a decrease in a patient’s quality of life and an increase in the probability of health complications.1 An estimated 14% of all deaths worldwide are attributable to high blood pressure (systolic blood pressure >140 mmHg; diastolic blood pressure >90 mmHg).2 In Spain, 54% of cardiovascular-related deaths in people older than 50 years are due to hypertension.3
It is widely accepted that there are relationships between poor blood pressure control and a patient’s lack of adherence to antihypertensive treatment, as well as lack of effectiveness to antihypertensive treatments.4–8 Research has been conducted in an attempt to reduce nonadherence.6,8,9 In spite of this, a study showed the mean prevalence of nonadherence to antihypertensive treatments to be 30%.10
Several terms are found in biomedical literature to explain the degree to which patients follow prescribed medication directions, including the terms “adherence” and “compliance”. Haynes et al defined “compliance” in 1979 as the extent to which a person’s behavior (in terms of taking medications, following diets or executing lifestyle changes) coincides with medical care or health advice; thus, noncompliance is the extent to which these instructions are not accomplished.11 The World Health Organization (WHO) combined the definitions developed by Haynes et al with one by Rand12 to obtain their definition of adherence to long-term treatment as
the extent to which a person’s behavior (in terms of taking medications, following diets or executing lifestyle changes) corresponds to the recommendations agreed by a health care provider.13
Later, Osterberg and Blaschke stated the term “adherence”
… is preferred by many health care providers, because compliance suggests that the patient is passively following the doctor’s orders and that the treatment plan is not based on a therapeutic alliance or contract established between the patient and the physician.14
Regardless of the definition used, health discipline, or health problem, measuring adherence has been complicated. Both direct (biological measures) and indirect (pill counts, patient-kept diaries of medication-taking, and questionnaires) methods have been used.14,15 Biological measures are considered a gold standard due to their objectivity, but their high cost is prohibitive. On the other hand, pill counts are simple, but they do not guarantee patient collaboration, and as such, results of pill counts may be inaccurate. Questionnaires are an alternative. Even though questionnaires have the disadvantage of overestimating patient adherence or nonadherence,14 their advantage is they are easy to use and are relatively inexpensive.16 Moreover, questionnaires are the most common method used in clinical settings because they have the ability to provide information about a patient’s reasons for not adhering to prescribed treatments.14 A number of scales of adherence to antihypertensive medication have been developed, but a questionnaire considered to be a gold standard does not exist. The most widely used17–20 questionnaire is that designed by Morisky–Green–Levine (MGL)21 in 1986. This is a unidimensional questionnaire containing four items.
In order to be a useful tool, a questionnaire must be valid and reliable.22 Scale validity refers to
the degree of confidence we can have that the measurement corresponds to the reality of the phenomenon that is being measured,23
that is,
the degree to which an instrument measures what it is supposed to measure.24
Whereas reliability is
the extent to which a measure yields the same number or score each time it is administered when the construct being measured has not changed.25
A number of questionnaires used in daily clinical practice do not reach the minimum standards for validity and reliability.26 Given this, it is necessary to compile an exhaustive list of the available validated tools measuring adherence to pharmacological antihypertensive treatment.
The aim of this work was to compile the questionnaires designed to measure adherence to pharmacological antihypertensive treatment that have at least one test of validity and one test of reliability.
Materials and methods
A literature search was undertaken in three electronic databases: US National Library of Medicine (PubMed), Excerpta Medica Database (EMBASE), and the Latin American and Caribbean Health Sciences Literature database (Literatura Latino-Americana e do Caribe em Ciências da Saúde [LILACS]). The search terms were: “patient adherence”, “patient compliance [Medical Subject Headings {MeSH}]”, “compliance”, “predictive validity”, “content validity”, “concurrent validity”, “convergent validity”, “discriminant validity”, “construct validity”, “psychometric properties”, “clinimetric properties”, “test-retest reliability”, “temporal stability”, “interobserver agreement”, “internal homogeneity”, “internal consistency”, “questionnaires [MeSH]”, “reproducibility of results [MeSH]”, “cronbach’s alpha”, and “hypertension [MeSH]”. Keywords were truncated in the LILACS database to avoid the loss of papers that could be of interest. In addition, the search was complemented by reference lists from the included papers.
Inclusion criteria
Articles needed to include the validation of a questionnaire to measure patient adherence to pharmacological antihypertensive treatments, published from the beginning of the database’s indexing until July 8, 2013. The articles had to include at least one validity test (content-, construct-, or criterion-related) and one reliability test (stability, equivalence, or homogeneity) of the questionnaire. Language limits were English, Spanish, French, and Portuguese.
Article selection
Duplications were removed. Two independent authors read the titles and abstracts to select the articles that met the inclusion criteria. If doubts appeared, the whole article was read. If there was disagreement, a third author arbitrated the debate between the two first authors.
Data extraction
Two authors extracted data independently. These data referred to the characteristics of the studied population and to the psychometric properties of the questionnaire being tested.26 Afterwards, extracted data was checked for any disagreement. When there was disagreement, the third author resolved the conflict.
Results
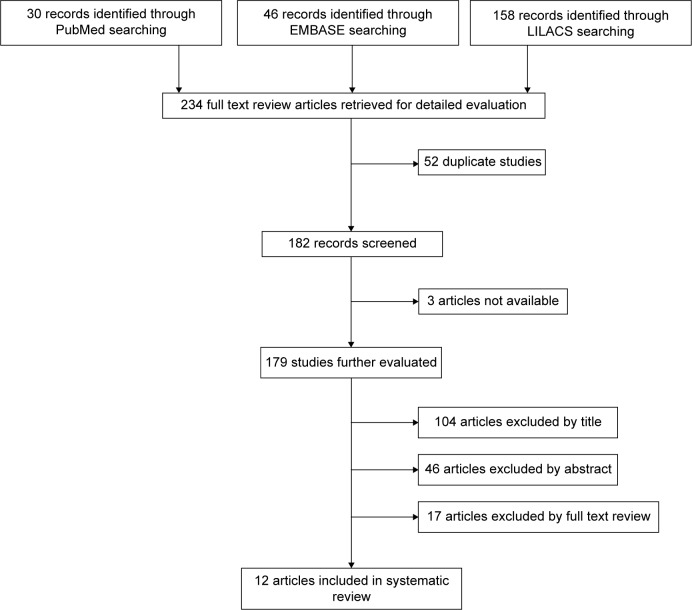
A total 234 articles were retrieved. Three were not available. From the remaining 231, 52 were duplicated. Of these,104 articles were removed by title, 46 by abstract, and finally, 17 were removed after reading the whole article. Ultimately 12 articles were included in the revision (Figure 1).
Figure 1.
Flow of information through the different phases of the systematic review.
Abbreviations: EMBASE, Excerpta Medica Database; LILACS, Literatura Latino Americana e do Caribe em Ciências da Saúde (Latin American and Caribbean Health Sciences Literature).
Articles were removed if they did not meet the inclusion criteria, that is, they did not validate a questionnaire for measuring adherence to antihypertensive treatments or demonstrate the required psychometric properties. For example, some articles did not measure treatment adherence but rather, reported the patients’ understanding about hypertension treatment, while others measured quality of life in hypertensive patients, patient knowledge about the disease, or patient satisfaction with their medication. Furthermore, there were articles that measured adherence in diseases other than hypertension and in other fields, such as nutrition. Articles in which adherence was the subject but measured related factors (aptitudes, beliefs, etc) instead of classifying patients as adherent or nonadherent, were similarly eliminated.
The 12 articles selected included 15 validation processes for six questionnaires that measured adherence to pharmacological antihypertensive treatments (Table 1). The questionnaires were the following:
– Brief Medication Questionnaire (BMQ) (one validation)27
– Hill-Bone Compliance to High Blood Pressure Therapy Scale (HB Comp Scale) (six validations)7,28–30
– Morisky Medication Adherence Scale (MMAS-8) (three validations)31–33
– Treatment Adherence Questionnaire for Patients with Hypertension (TAQPH) (one validation)34
Table 1.
Characteristics of the articles included
| Author, year of publication | Questionnaire | Mean age (SD) | Sex % female, (n) | Language | Setting | Sample (n) | Items |
|---|---|---|---|---|---|---|---|
| Morisky et al21 1986 | MGL | 54a | 70.00 (–) | English | Hospital (outpatient clinics) |
290 | 4 |
| Ben et al27 2012 | BMQ vs MGL | 66.60 (13.20) | 64.60 (133) | Portuguese Portuguese |
Primary health care unit | 206 | 11 4 |
| Kim et al28 2000 | HB Comp Scale | 41.30 (5.30) 59.20 (13.10) |
0.00 (0) 69.20 (236) |
English | Outpatient clinic | Study 1: 139 Study 2: 341 |
14 |
| Krousel-Wood et al7 2005 | HB Comp Scale (elderly) | 69.00 (–) | 49.00 (121) | English | Elderly community-dwelling | 239 | 14 |
| Lambert et al29 2006 | Xhosa HB Comp Scale Xhosa Adapted HB Comp Scale |
52.00 (7.60) | 51.00 (50) | Xhosa | Community health centers | 79 82 |
14 10 |
| Song et al30 2011 | HBMA-K | 52.54 (5.40) 70.88 (5.40) |
56.80 (88) 70.50 (261) |
Korean | Baltimore- Washington metropolitan area | Study 1: 155 Study 2: 370 |
8 |
| Morisky et al32 2008 | MMAS-8 | 52.50 (12.20) | 59.20 (809) | English | Hospital | 1,367 | 8 |
| Korb-Savoldelli et al31 2012 | MMAS-8 | 55.70 (14.60) | 42.70 (85) | French | Hospital, day care unit | 199 | 8 |
| Saleem et al33 2012 | MMAS-8 | 39.50 (6.93) | 28.20 (31) | Urdu | Hospital | 110 | 8 |
| Ma et al34 2012 | TAQPH | 59.68 (10.69) | 58.30 (162) | Chinese | Hospital | 278 | 28 |
| Martín Alfonso et al35 2008 | MBG | – | – | Spanish | Polyclinic | 114 | 12 |
| Martínez et al36 2011 | MBG | Not indicatedb | 81.00 (115) | Spanish | Health care center | 142 | 12 |
Notes:
Median.
Range 37–90 years.
Abbreviations: BMQ, Brief Medication Questionnaire; HB Comp Scale, Hill-Bone Compliance to High Blood Pressure Therapy Scale; HBMA-K, Hill-Bone Medication Adherence – Korean version scale; MBG, Martín–Bayarre–Grau; MGL, Morisky–Green–Levine; MMAS-8, Morisky Medication Adherence Scale; SD, standard deviation; TAQPH, Treatment Adherence Questionnaire for Patients with Hypertension.
Content validity
Content validity was assessed in four questionnaires: HB Comp Scale,28 TAQPH,34 MMAS-8 (Urdu version), 31 and MBG (validated in Cuba).35 In all four validation studies, the authors used an expert panel. In addition, for item generation, two questionnaires (HB Comp Scale and TAQPH) included a narrative review, and one (TAQPH) performed a focus group.
Construct validity
Construct validity was assessed in eleven of 15 validation processes (Table 2). The Urdu version of the MMAS-833 evaluated both convergent validity, by comparing the results to the MGL,21 and known group validity, comparing the results of the questionnaire to blood pressure control. The remaining construct validity assessments were performed by factor analysis. In the MGL,21 HB Comp Scale,28 Hill-Bone Medication Adherence-Korean version (HBMA-K) scale (a validation of HB Comp Scale),30 and MMAS-8 (English32 and French31 versions) the factor analysis yielded a one-dimensional solution. On the other hand, the TAQPH34 questionnaire yielded six factors, and the Colombian MBG36 yielded five.
Table 2.
Validity and reliability assessment
| Questionnaire | Construct validity | Criterion validity | Stability (test–retest) | Homogeneity (internal consistency)
|
|
|---|---|---|---|---|---|
| Item–total correlations | Cronbach’s α | ||||
| MGL21 | PCFA: one factor | Comparative test: BP control. Concurrent validity: r=0.43 (6 months) Predictive validity: r=0.58 (42 months) – Student’s t-test=6.43, P<0.01 – Medication intake vs BP control: R2=0.33, P<0.01 S =81.00% SP =44.00% PPV =75.00% NPV =52.00% |
– | 0.479–0.561 | 0.61 |
| BMQ27 | – | – | BMQ: r=0.83, P<0.001 Screen 1: r=0.84, P=0.010 Screen 2: r=0.86, P=0.004 Screen 3: r=0.94, P=0.120 |
– | BMQ: 0.67 (95% CI; 0.60–0.73) Screen 1: 0.67 (95% CI; 0.60–0.73) Screen 2: 0.84 (95% CI; 0.80–0.87) Screen 3: 0.76 (95% CI; 0.70–0.81) |
| MGL27 | – | – | MGL: r=0.70, P=0.020 | – | 0.73 (95% CI; 0.67–0.79) |
| HB Comp Scale28 | |||||
| Study 1 | Factor analysis variance (%): 27.00, one factor | Comparative test: BP control. Predictive validity: r=0.21, P=0.030 |
– | Range: −0.02 to 0.60 Mean: 0.34 (SD 0.17) |
0.74 |
| Study 2 | Factor analysis variance (%): 35.00, one factor | Comparative test: BP control. Predictive validity: r=0.16, P<0.001 |
– | Range: 0.01–0.64 Mean: 0.46 (SD 0.16) |
0.84 |
| HB Comp Scale7 (elderly) | Factor analysis two factors | – | Not availablea | Range: 0.13–0.59b | Full questionnaire: 0.43 – Medication compliance subscale: 0.68 – Salt intake subscale: 0.49 |
| Xhosa HB Comp Scale29 | – | Comparative test: BP control. Predictive validity: questionnaire vs – Mean SBP: ρ=0.17, P=0.140 – Mean DBP: ρ=0.18, P=0.130 |
– | Range: 0.10–0.64 Mean: 0.38 (SD: 0.18) Subscale I (salt intake): 0.27 Subscale II (appointment-keeping): no resultc Subscale III (medication compliance): 0.46 |
Full questionnaire: 0.77 Subscale I (salt intake): 0.41 Subscale II (appointment-keeping): no resultc Subscale III (medication compliance): 0.76 |
| Xhosa Adapted | – | Comparative test: BP control. | – | Range: 0.31–0.64 | 0.79 |
| HB Comp Scale29 | Predictive validity: questionnaire vs – Mean SBP: ρ=0.19, P=0.080 – Mean DBP: ρ=0.21, P=0.050 |
Mean: 0.45 (SD 0.11) | |||
| HBMA-K30 | Factor analysis variance (%): 35.40, one factor | Comparative test: questionnaire vs – HBP knowledge with 26 item test – Beliefs about HBP – BP control Concurrent validity, comparative test: questionnaire vs – HBP knowledge (r=−0.13, P<0.01) – HBP belief (r=−0.18) – BP outcomes (SBP: r=0.18, P<0.01; and DBP: r=0.24, P<0.01) |
– | Range: 0.37–0.63 | 0.80 |
| MMAS-832 (English) | Factor analysis CFA: one factor | Comparative test: −Concurrent validity: questionnaire vs MGL r=0.64, P<0.05 S =93.00% SP =53.00% Predictive validity: questionnaire vs – BP control (χ2=6.6, P<0.05) – knowledge,37 attitude,38 social support,39 stress coping,40 medication complexity, and patient satisfaction with clinic visits41,42 (P<0.05 for all, except for attitude) |
– | Range: 0.3038–0.5896 | 0.83 |
| MMAS-831 (French) | Factor analysis PCFA variance (%): 27.50, one factor CFA: one factor | – | ICC =0.68 (95% CI; 0.63–0.72) | Range: −0.05 to 0.43 | 0.54 (95% CI; 0.44–0.63) |
| MMAS-833 (Urdu) | Convergent validity, comparative test: questionnaire vs MGL ρ=0.765, P<0.001 Known group validity vs BP control χ2=19.996, P<0.001 | S =46.20% SP =60.00% PPV =45.00% NPV =61.10% |
ICC meaningful (P<0.001) | Range: 0.30–0.48 | 0.701 |
| TAQPH34 | EFA variance (%): 62.50, six factors CFA: six factors | Concurrent validity, comparative test: questionnaire vs MMAS-8; GSES43 MMAS-8→ r=0.76, P<0.01 GSES→ r=0.69, P<0.01 |
ICC =0.82 | Range: 0.31–0.66 | Full questionnaire: 0.86; dimension I: 0.94; dimension II: 0.88; dimension III: 0.92; dimension IV: 0.76; dimension V: 0.83; dimension VI: 0.72 |
| MBG35 | PCFA variance (%): 68.70, three factors | − | – | Range: 0.28–0.70 | 0.889 |
| MBG36 | PCFA variance (%): 63.40, five factors | − | – | – | 0.694 |
Notes:
Longitudinal data to assess test–retest reliability were not available.
The appointment-keeping subscale of the scale consists of only two items and was not included in this analysis.
The appointment-keeping subscale did not provide an interpretable result, probably as a result of the South African public health system, in which reappointments are standard procedure.
Abbreviations: BMQ, Brief Medication Questionnaire; BP, blood pressure; CFA, confirmatory factorial analysis; CI, confidence interval; DBP, diastolic blood pressure; EFA, exploratory factorial analysis; GSES, General Self-Efficacy Scale; HB Comp Scale, Hill-Bone Compliance to High Blood Pressure Therapy Scale; HBMA-K, Hill-Bone Medication Adherence – Korean version (scale); HBP, high blood pressure; ICC, intraclass correlation coefficient; MBG, Martín–Bayarre– Grau (scale); MGL, Morisky–Green–Levine (scale); MMAS-8, Morisky Medication Adherence Scale; NPV, negative predictive value; PCFA, principal components factorial analysis; PPV, positive predictive value; S, sensitivity; SBP, systolic blood pressure; SD, standard deviation; SP, specificity; TAQPH, Treatment Adherence Questionnaire for Patients with Hypertension.
Total variance ranged from 68.7%, in the MBG validated in Cuba,35 to 27%, in the HB Comp Scale validated in young African American males.28
Criterion validity
Four validations (MGL,21 HBMA-K,30 MMAS-832 (English), and TAQPH34) assessed concurrent validity, and six evaluated predictive validity (MGL,21 Xhosa HB Comp Scale,29 HB Comp Scale28 [two validations], and the MMAS-832 [English]). The comparison tests are detailed in Table 2.
Reliability
Cronbach’s α was used to estimate internal consistency as a reliability measure in every validation. The MBG validated in Cuba35 obtained the highest coefficient (α=0.889), while the lowest (α=0.43) was obtained in the HB Comp Scale7 validated in an elderly population, published by Krousel-Wood et al. Item-total scale correlation was also used in all but three validations (Table 2).
The MMAS scale in Urdu33 and French,31 the TAQPH,34 and the BMQ27 evaluated temporal stability with the test–retest method. In each of these validations, temporal stability was demonstrated with a moderate to high correlation, except for the TAQPH34 questionnaire, which had an intraclass correlation coefficient of 0.82.
Discussion
This review provides health professionals with a report summarizing the evidence across different questionnaires according to the psychometric properties evaluated. The review did not intend to determine or indicate an optimum questionnaire but rather, to compile validated scales that measure antihypertensive treatment adherence. Consequently, health professionals can choose the most appropriate questionnaire, depending on their circumstances. To our knowledge there is no similar published study.
A large number of authors have designed questionnaires in order to measure adherence to antihypertensive treatments. Nevertheless, no questionnaire could be considered a gold standard. Any tool to be used as a measure must demonstrate validity and reliability, including questionnaires.22 Furthermore, validity and reliability must be measured in each sample or have been conducted in a comparable sample since it is not possible to extrapolate results among different populations. Differences in validity and reliability results obtained across versions of the MMAS-831–33 can be seen as an example.
A sensitive search strategy was designed to ensure the collection of all papers validating questionnaires to measure adherence to pharmacological antihypertensive treatment. Inclusion criteria in this review required that articles have at least one validity test and one of reliability. Taking into account these criteria, such well-known questionnaires as the BMQ (English version),44 the Haynes–Sackett11 and Batalla questionnaires,45 etc were not included.
The validity of a questionnaire (the confirmation that it measures what it is supposed to measure) is evaluated in several ways, as: content validity, construct validity, and criterion validity.
The methods most commonly used to assess content validity are expert opinion and systematic review. However, researchers often choose only one of these options. From the 15 validations found, only four studied content validity, and even these did not explain in detail the process followed to assess it. It is suspected that in the remaining questionnaires, authors assumed, without testing, content validity was present. In the four validations that assessed content validity, the technique utilized was an expert panel. None of the authors based content validity on a systematic review. This method could be of great interest, but it can increase costs and research time.
The most common technique to assess construct validity was factor analysis. A one-dimensional solution emerged in the majority of the scales, but the factor explained only a small percentage of the total response variability. As an example, the HB Comp Scale28 and the HBMA-K30 explained up to 35% of the total variance. Consequently questionnaires should consider including further dimensions and items to explain more of the total response variance. This could be observed in the TAQPH,34 which had 28 items and six factors, and was able to explain 62.5% of the variance. The total explained variance is considered an indicator of how factors extracted from a questionnaire actually correspond to patient answers. When little variance is explained, the scale shows a deficiency that indicates lack of variables or a poor initial theoretical construct. However, it is also important that a questionnaire does not have too many items, to minimize patient resistance to being interviewed and interview duration. As such, the number of items needs to be balanced between explaining variance and user acceptance.
Construct validity assessment by convergent validity was completed in two questionnaires. The correlation between the Urdu version of the MMAS-833 and the same language version of the MGL21 was checked. A high correlation was found between the scales (ρ=0.765, P<0.001), which in theory confirmed that both questionnaires measured the same construct. However such a correlation is not surprising as the MMAS-8 was based on the MGL four-item questionnaire, onto which more questions were added.32
Criterion validity is traditionally defined as
the correlation of a scale with some other measure of the trait or disorder under study, ideally a gold standard which has been used and accepted in the field.46
Criterion validity consists of two types: concurrent and predictive. In concurrent validity, both the new scale and a criterion measure are applied simultaneously and subsequently correlated. On the other hand, when using predictive validity, the criterion measure will not be available until sometime in the future. This implies that testing predictive validity may extend the time of study.
With the exception of six validations, the remainder tested criterion validity. The validation of HBMA-K30 obtained a low correlation to systolic blood pressure control (r=0.18; P<0.01) and diastolic blood pressure (r=0.24; P<0.01). This low correlation could be due to the fact that medication adherence is not perfectly correlated to blood pressure control. That is, it is possible for a patient to have high medication adherence and to not have controlled blood pressure due to another factor, such as lack of effectiveness of the treatment. Nevertheless, it is assumed that there is a direct relationship between adherence and blood pressure control.47 On the other hand, the MMAS-8,32 compared with the MGL21 to assess concurrent validity, obtained a moderate to high correlation (r=0.64; P>0.05). It is necessary to keep in mind that the development of the MMAS-8 was based on the MGL, as stated previously.
In addition to verifying the validity of a questionnaire, it is necessary to check the results are reproducible. That is, it is necessary to assess its reliability. From a technical point of view, it could be said that reliability is
a ratio of the variability between individuals to the total variability in the scores; in other words, the reliability is a measure of the proportion of the variability in scores which was due to true differences between individuals.46
One of the methods used to measure reliability is internal consistency. Internal consistency describes reliability estimations based on the average correlation among items in a test.46 A Cronbach’s α value is considered acceptable when above 0.70.48 Only two validations obtained Cronbach’s α values well below 0.70 (the HB Comp Scale [elderly]7 [0.43] and MMAS-8 [French]31 [0.54]), indicating the items were not highly related. In the remaining questionnaires, Cronbach’s α varied from 0.61 (in the MGL)21 to 0.889 (in the MGB).35 However, it should be noted that Cronbach’s α is sensitive to the number of items and the sample’s variance.
Cronbach’s α is assessed from a single administration of the test, not taking into account variations in time or between administrators, and as such, it can provide an optimistic interpretation of the reliability of a questionnaire. For this reason, it is advisable that internal consistency is accompanied by a stability measure (test–retest) or by interobserver equivalence.46 In the present study, six validations provided stability data and none checked interobserver verifications.
As previously stated, the intent of this article was to gather all questionnaires measuring patient adherence to antihypertensive treatments that contain at least one validity measure and one reliability measure. Furthermore the authors do not consider any of the questionnaires to have sufficient reliability or validity to be highly recommended. Nevertheless, if one had to choose a questionnaire, the authors offer these considerations.
For research, the TAQPH may be advisable. The TAQPH contains the greatest number of items, potentially providing more information to the research investigation, explains a high percentage of variance, and has sound indicators for both stability and criterion validity. The MBG also contains a large number of items but cannot be endorsed as it lacks criterion validity, stability, and item-total correlations.
In clinical practice it is necessary that a questionnaire is acceptable to both health care professionals and patients (containing the fewest possible items), is quick and easy to use, and shows good sensitivity, specificity, positive predictive value, and negative predictive value. The MGL, BMQ, HB Comp Scale, and MMAS-8 have similar indicators of reliability and validity; however, only the MMAS-8 and MGL show the probability of a clinician deciding that a non-adherent patient is not controlled (positive predictive value) or that an adherent patient is controlled (negative predictive value). As such, in clinical practice, both the MMAS-8 and MGL may be recommended. However as previously noted, the MMAS-8 was developed by Morisky et al in 200832 based on the MGL and as such, has an improved capacity to collect information (by having four additional items), sensitivity, specificity, positive predictive value, and negative predictive value, while maintaining acceptable validity and reliability. Consequently in clinical practice, the MMAS-8 may be an appealing option.
Limitations
This study could be influenced by publication bias as a consequence of the general tendency to publish only positive results. Language bias could also have appeared. In spite of including studies published in four languages, it is possible that some studies were not included because of being published in other languages. Moreover, despite the strict methodology followed by reviewers, it is possible that selection bias appeared as a consequence of the lack of availability of some articles.
Conclusion
This review provides information of great relevance to daily clinical practice. In spite of the number of studies performed to measure adherence, not all of the questionnaires used in the studies reach the requirements to be considered valid and reliable tools. Six questionnaires were identified to measure adherence to pharmacological antihypertensive treatment that had at least one validity test and one test of reliability. While some of these questionnaires had evidence to demonstrate acceptable validity, they failed in reliability and vice versa. Therefore although none of the questionnaires can be considered as a gold standard, this revision will assist health professionals in the selection of the most appropriate tool, depending on their circumstances. In the future, the design and validation of a questionnaire to measure adherence to antihypertensive treatments reaching the following requirements is fundamental: a) to be succinct enough to avoid patient and/or administrator fatigue (acceptability) but comprehensive enough to explain variance; b) include explicit content validity, have construct validity in accordance with a logical and reasoned theoretical structure that justifies items and subscales, and/or demonstrate criterion validity and; c) be a tool that provides reproducible results (reliable).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Côté I, Moisan J, Chabot I, Grégoire JP. Health-related quality of life in hypertension: impact of a pharmacy intervention programme. J Clin Pharm Ther. 2005;30(4):355–362. doi: 10.1111/j.1365-2710.2005.00663.x. [DOI] [PubMed] [Google Scholar]
- 2.Hux JE, Ivis F, Flintoft V, Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25(3):512–516. doi: 10.2337/diacare.25.3.512. [DOI] [PubMed] [Google Scholar]
- 3.Gascón Cánovas JJ, Saturno Hernández PJ, Llor Esteban B. Grupo de Investigación del Proyecto EMCA sobre Evaluación y Mejora de la Adhesión Terapéutica en la Hipertensión. [Evaluation and improvement of therapy adherence of hypertensive patients] Aten Primaria. 2001;28(9):615–619. doi: 10.1016/S0212-6567(01)70463-5. Spanish. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berry SD, Quach L, Procter-Gray E, et al. Poor adherence to medications may be associated with falls. J Gerontol A Biol Sci Med Sci. 2010;65(5):553–558. doi: 10.1093/gerona/glq027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Espinosa Garcia J, Martell Claros N, Llerena Ruiz A, Fernández Bergés Gurrea D. Pharmacological compliance in the treatment of arterial hypertension. A review of studies published between 1975 and 2011. Semergen. 2012;38(5):292–300. doi: 10.1016/j.semerg.2012.01.001. Spanish. [DOI] [PubMed] [Google Scholar]
- 6.Fikri-Benbrahim N, Faus MJ, Martínez-Martínez F, Sabater-Hernández D. Impact of a community pharmacists’ hypertension-care service on medication adherence. The AFenPA study. Res Social Adm Pharm. 2013;9(6):797–805. doi: 10.1016/j.sapharm.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Krousel-Wood M, Muntner P, Jannu A, Desalvo K, Re RN. Reliability of a medication adherence measure in an outpatient setting. Am J Med Sci. 2005;330(3):128–133. doi: 10.1097/00000441-200509000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database Syst Rev. 2004;(2):CD004804. doi: 10.1002/14651858.CD004804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jing S, Naliboff A, Kaufman MB, Choy M. Descriptive analysis of mail interventions with physicians and patients to improve adherence with antihypertensive and antidiabetic medications in a mixed-model managed care organization of commercial and Medicare members. J Manag Care Pharm. 2011;17(5):355–366. doi: 10.18553/jmcp.2011.17.5.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract. 2008;62(1):76–87. doi: 10.1111/j.1742-1241.2007.01630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haynes RB, Taylor DL, Sackett D. Compliance in Health Care. Baltimore, MD: John Hopkins University Press; 1979. [Google Scholar]
- 12.Rand CS. Measuring adherence with therapy for chronic diseases: implications for the treatment of heterozygous familial hypercholesterolemia. Am J Cardiol. 1993;72(10):68D–74D. doi: 10.1016/0002-9149(93)90014-4. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . Adherencia a los Tratamientos a Largo Plazo. [Adherence to long-term therapies] Geneva: World Health Organization; 2004. [Accessed, July 2, 2013]. Available from: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=18722&Itemid=>. Spanish. [Google Scholar]
- 14.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 15.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26(5):331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 16.Gozum S, Hacihasanoglu R. Reliability and validity of the Turkish adaptation of medication adherence self-efficacy scale in hypertensive patients. Eur J Cardiovasc Nurs. 2009;8(2):129–136. doi: 10.1016/j.ejcnurse.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Gutiérrez-Angulo ML, Lopetegi-Uranga P, Sánchez-Martin I, Garaigordobil-Landazabal M. Therapeutic compliance in patients with arterial hypertension and type 2 diabetes mellitus. Rev Calid Asist. 2012;27(2):72–77. doi: 10.1016/j.cali.2011.09.008. Spanish. [DOI] [PubMed] [Google Scholar]
- 18.Amado Guirado E, Pujol Ribera E, Pacheco Huergo V, Borras JM, ADIEHTA Group Knowledge and adherence to antihypertensive therapy in primary care: results of a randomized trial. Gac Sanit. 2011;25(1):62–67. doi: 10.1016/j.gaceta.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 19.Gascón JJ, Sánchez-Ortuño M, Llor B, Skidmore D, Saturno PJ, Treatment Compliance in Hypertension Study Group Why hypertensive patients do not comply with the treatment: results from a qualitative study. Fam Pract. 2004;21(2):125–130. doi: 10.1093/fampra/cmh202. [DOI] [PubMed] [Google Scholar]
- 20.Morales Suárez-Varela MT, GEMECOR Study on the use of a smart pillbox to improve treatment compliance. Aten Primaria. 2009;41(4):185–191. doi: 10.1016/j.aprim.2008.07.003. Spanish. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Lamprea JAM, Gómez Restrepo C. Validez en la evaluación de escalas [Validity in scale-testing] Rev Colomb Psiquiat. 2007;36(2):340–348. [Google Scholar]
- 23.Sánchez Pedraza R, Gómez Restrepo CI. Conceptos básicos sobre validación de escalas. [Basic concepts on validation] Rev Colomb Psiquiat. 1998;27(2):121–130. Spanish. [Google Scholar]
- 24.Polit DF, Beck CT. Nursing Research Principles and Methods. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1995. Assessing Data Quality; pp. 413–448. [Google Scholar]
- 25.Frost MH, Reeve BB, Liepa AM, Stauffer JW, Hays RD, Mayo/FDA Patient-Reported Outcomes Consensus Meeting Group What is sufficient evidence for the reliability and validity of patient-reported outcome measures? Value Health. 2007;10(Suppl 2):S94–S105. doi: 10.1111/j.1524-4733.2007.00272.x. [DOI] [PubMed] [Google Scholar]
- 26.Nunnally JC, Bernstein IH. Teoría Psicométrica [Psychometric theory] 3rd ed. Mexico DF: McGraw-Hill Inc; 1995. Spanish. [Google Scholar]
- 27.Ben AJ, Neumann CR, Mengue SS. The Brief Medication Questionnaire and Morisky-Green test to evaluate medication adherence. Rev Saude Publica. 2012;46(2):279–289. doi: 10.1590/s0034-89102012005000013. [DOI] [PubMed] [Google Scholar]
- 28.Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs. 2000;15(3):90–96. doi: 10.1111/j.1751-7117.2000.tb00211.x. [DOI] [PubMed] [Google Scholar]
- 29.Lambert EV, Steyn K, Stender S, Everage N, Fourie JM, Hill M. Cross-cultural validation of the hill-bone compliance to high blood pressure therapy scale in a South African, primary healthcare setting. Ethn Dis. 2006;16(1):286–291. [PubMed] [Google Scholar]
- 30.Song Y, Han HR, Song HJ, Nam S, Nguyen T, Kim MT. Psychometric evaluation of hill-bone medication adherence subscale. Asian Nurs Res (Korean Soc Nurs Sci) 2011;5(3):183–188. doi: 10.1016/j.anr.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 31.Korb-Savoldelli V, Gillaizeau F, Pouchot J, et al. Validation of a French version of the 8-item Morisky medication adherence scale in hypertensive adults. J Clin Hypertens (Greenwich) 2012;14(7):429–434. doi: 10.1111/j.1751-7176.2012.00634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 33.Saleem F, Hassali MA, Shafie AA, et al. Translation and validation study of Morisky Medication Adherence Scale (MMAS): the Urdu version for facilitating person-centered healthcare in Pakistan. Int J Pers Cent Med. 2012;2(3):384–390. [Google Scholar]
- 34.Ma C, Chen S, You L, Luo Z, Xing C. Development and psychometric evaluation of the Treatment Adherence Questionnaire for Patients with Hypertension. J Adv Nurs. 2012;68(6):1402–1413. doi: 10.1111/j.1365-2648.2011.05835.x. [DOI] [PubMed] [Google Scholar]
- 35.Martin Alfonso L, Bayarre Vea HD, Grau Ábalo JA. Validation of MBG Questionnaire (Martin-Bayarre-Grau) for the evaluation of therapy adherence in blood hypertension patients. Rev Cuba Salud Publica. 2008;34(1) Spanish. [Google Scholar]
- 36.Martínez JW, Villa Perea JA, Jaramillo J, Quintero Betancur AM, Calderón V. Validación del cuestionario de adherencia al tratamiento anti hipertensivo Martín Bayarré Grau. [Validation of a scale of adherence treatment antihypertensive: Martin Bayarre Grau Test] Rev Med Risaralda. 2011;17(2):101–105. Spanish. [Google Scholar]
- 37.Norman SA, Marconi KM, Schezel GW, Schechter CF, Stolley PD. Beliefs, social normative influences, and compliance with antihypertensive medication. Am J Prev Med. 1985;1(3):10–17. [PubMed] [Google Scholar]
- 38.Stamler R, Stamler J, Civinelli J, et al. Adherence and blood-pressure response to hypertension treatment. Lancet. 1975;2(7947):1227–1130. doi: 10.1016/s0140-6736(75)92070-x. [DOI] [PubMed] [Google Scholar]
- 39.Schoenberg NE. The relationship between perceptions of social support and adherence to dietary recommendations among African-American elders with hypertension. Int J Aging Hum Dev. 1998;47(4):279–297. doi: 10.2190/0L2Y-FXVE-KJYH-318A. [DOI] [PubMed] [Google Scholar]
- 40.Svensson S, Kjellgren KI. Adverse events and patients’ perceptions of antihypertensive drug effectiveness. J Hum Hypertens. 2003;17(10):671–675. doi: 10.1038/sj.jhh.1001596. [DOI] [PubMed] [Google Scholar]
- 41.Bittar N. Maintaining long-term control of blood pressure: the role of improved compliance. Clin Cardiol. 1995;18(6 Suppl 3):III 12–III 16. doi: 10.1002/clc.4960181504. [DOI] [PubMed] [Google Scholar]
- 42.Klein LE. Compliance and blood pressure control. Hypertension. 1988;11(3 Pt 2):II 61–II 64. doi: 10.1161/01.hyp.11.3_pt_2.ii61. [DOI] [PubMed] [Google Scholar]
- 43.Scholz U, Gutiérrez Doña B, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Psychol Assess. 2002;18(3):242–251. [Google Scholar]
- 44.Svarstad BL, Chewning BA, Sleath BL, Claesson C. The Brief Medication Questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ Couns. 1999;37(2):113–124. doi: 10.1016/s0738-3991(98)00107-4. [DOI] [PubMed] [Google Scholar]
- 45.Batalla Martínez C, Blanquer Laguarta A, Ciurana Misol R, et al. Cumplimiento de la prescripción farmacológica en pacientes hipertensos. [Compliance with drug prescriptions in hypertensive patients] Aten Primaria. 1984;1(2):185–191. Spanish. [Google Scholar]
- 46.Streiner D, Norman G. Health Measurement Scales. A Practical Guide to Their Development and Use. 2nd ed. New York, NY: Oxford University Press; 1991. [Google Scholar]
- 47.Quintana Setién C, Fernández-Britto Rodríguez JE. Adherencia terapéutica farmacológica antihipertensiva en adultos de atención primaria y factores relacionados con su incumplimiento. [Antihypertensive drug therapy compliance by adults in the primary health care and factors related to non-compliance] Rev Cubana Invest Bioméd. 2009;28(2) Spanish. [Google Scholar]
- 48.Bland JM, Altman DG. Cronbach’s alpha. BMJ. 1997;314(7080):572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]