Abstract
Cancer research in Africa will have a pivotal role in cancer control planning in this continent. However, environments (such as those in academic or clinical settings) with limited research infrastructure (laboratories, biorespositories, databases) coupled with inadequate funding and other resources have hampered African scientists from carrying out rigorous research. In September 2012, over 100 scientists with expertise in cancer research in Africa met in London to discuss the challenges in performing high-quality research, and to formulate the next steps for building sustainable, comprehensive and multi-disciplinary programmes relevant to Africa. This was the first meeting among five major organizations: the African Organisation for Research and Training in Africa (AORTIC), the Africa Oxford Cancer Foundation (AfrOx), and the National Cancer Institutes (NCI) of Brazil, France and the USA. This article summarizes the discussions and recommendations of this meeting, including the next steps required to create sustainable and impactful research programmes that will enable evidenced-based cancer control approaches and planning at the local, regional and national levels.
Introduction
Africa is facing an unprecedented growth in cancer burden and is inadequately prepared to meet this public health challenge. By 2030, the projected new cancer cases per year are 1.27 million and 0.97 million deaths.1,2 This increasing number of cancer cases takes into account the predicted increase in the African population from 1.02 billion to 1.56 billion.1,2 Given the inadequate surveillance of cancer in the African population and the dearth of high quality cancer registries, projections for cancer incidence and mortality may be underestimates. These projections might be even higher owing to the increasing exposure to established cancer risk factors, such as infections with viruses (including HIV, Epstein–Barr virus [EBV], human herpesvirus 8 [HHV8], hepatitis B and C, human papilloma virus [HPV]),3–5 tobacco, diet, obesity and physical inactivity, and altered reproductive patterns.2 Available data from few cancer registries have also shown that a significant proportion of cancers are diagnosed in children, including HIV-related paediatric malignancies.6–9 The cancer burden in Africa is further exacerbated by the low survival, which is among the worse in the world because of advanced-stage disease at diagnosis and extremely limited human resources and treatment options.2
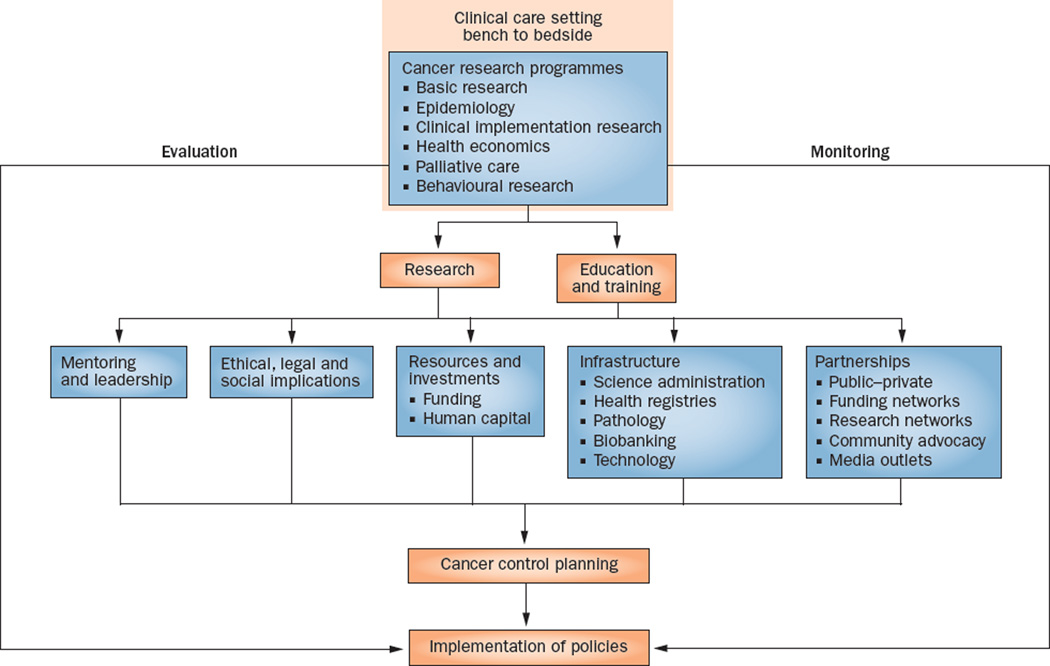
Given the limited preventive and health-care resources in Africa, it is imperative that cancer control policies are evidence-based and target those cancers associated with the highest burden (cancer incidence, morbidity and mortality) in this continent.10 Comprehensive cancer control planning evaluates a variety of ways to enforce the most cost-effective and beneficial ways to reduce cancer incidence, mortality and morbidity, and to improve the quality of life of cancer survivors through the implementation of evidence-based strategies across the cancer continuum (that is, prevention, early detection, diagnosis, treatment, and palliation).11 Research will have a pivotal role in cancer control in Africa because it will address the aetiology of cancers unique to Africa, which will lead to developing locally-appropriate strategies to prevent and treat cancer. Research will also contribute to effective, affordable and evidence-based interventions (practices that have been proven effective through research and outcome evaluations) that can be integrated into existing clinical and public health. Cancer research can become an opportunity for development and poverty alleviation through the creation of sustainable cancer control programmes because cancer is a common cause of loss of social status and bankruptcy in low-and middle-income countries.10,12 Through these programmes, African scientists are trained to conduct, lead and formulate new directions for cancer research, thus establishing agendas that address cancer prevention, improve early detection and provide cost-beneficial treatments that enable populations to avoid the catastrophic health cost of cancer care, avoid loss of social status and financial ruin. In addition, African scientists should serve as mentors for future African cancer researchers. Lastly, the process should not be linear, but rather iterative. For example, once cancer control and prevention initiatives are implemented, cancer research is a necessary part of the evaluation process that determines their efficacy and cost-effectiveness (Figure 1).
Figure 1.
Capacity building framework for cancer research in Africa. A comprehensive cancer research and training programme will need appropriate infrastructure, resources, mentorship and leadership training, funding and research partnerships, which should be accompanied by the highest levels of ethical, legal and socially appropriate standards for research. Evidence obtained from cancer research will be used for the creation of cancer control and prevention initiatives. In addition, cancer research will be important for the monitoring and evaluation of those initiatives for efficacy and effectiveness.
The challenges of addressing these issues are formidable, multiple and complex. The overall shortage of healthcare workers and facilities in Africa, which is even more acute in the field of cancer,13 results in limited availability of treatment and research. Despite the endorsement by African governments of a recommendation that each nation spend 1% of its gross domestic product on research and development, a report released by the African Union in 2010 indicated that only three countries were able to top this threshold, and interviews with scientists and government officials across the continent have suggested high inadequacy of research funding.14 Lack of infrastructure, funding, personnel and other resources to support cancer research, unsupportive working environments for research, scarce research collaborations, and lack of adequate research training programmes are challenges that must be overcome to improve cancer research productivity in Africa. It is also important to prioritize research interventions to those that are likely to have the highest public health impact for the population.10 One recommendation is to carry out an economic analysis to prioritize research initiatives that give the best value for money, for example, to allocate money to those projects likely to result in the highest increase in overall survival or disability-adjusted survival per dollar spent. In oncology, a recent modelling study for the WHO assessed the cost-effectiveness of a range of interventions for breast, cervical and colon cancer in sub-Saharan Africa where 85% of the African population resides.15–17 The results of this study suggested that there are both treatment and prevention options for these cancers that would be highly cost-effective in this region. However, the utility of cost-effectiveness analyses for decision making depends on the quality of data on which they are based, and more studies using different models are needed.17
To evaluate current status and future opportunities in cancer research in Africa, a workshop of international and African experts with decades of experience conducting research, developing capacity and implementing cancer control policies in Africa was convened by the African Organisation for Research and Training in Africa (AORTIC), the Africa Oxford Cancer Foundation (AFROX), and the National Cancer Institutes (NCI) of USA, France and Brazil, in September 2012 in London, UK. This article synthesizes the conference proceedings and actionable items to build sustainable cancer research capacity and reduce the burden of cancer in Africa.
Building research capacity
Infrastructure
The ability of African scientists to carry out rigorous cancer research depends on the availability of infrastructure at both the institutional and national levels. The availability of research infrastructure—although highly variable across the continent—remains inadequate in almost all countries. The limitations surrounding the infrastructure in laboratories and in clinical, pathological and computational research are well known, but a lack of research administration is often overlooked.18–21 Research administration provides the necessary oversight and coordination of activities within an institute and sets the tone for fiscal responsibility ensuring the appropriate use of research funds. There have been several recent initiatives to address the lack of research administration. These initiatives include competitive funding from the US National Institute of Child Health and Human Development (NICHD), at the National Institutes of Health (NIH), that allows African institutions to create research administrative infrastructure to address key areas in grant management, such as fiscal accountability, data management, research oversight, and submission of grant applications.22,23 Local institutional ownership of such structures is ensured through their commitment to sustain and integrate these activities into their overall strategic plan for research support.22 Moreover, funded institutions are encouraged to work and strengthen the capacity for research administration at other institutes that lack this component.22 The developments made in this area led to the formation of the Association of Research Administrators in Africa in 2009, which aims to establish a hub of excellence for research administrators and fill the gaps of research administration in Africa.24
Despite this increased appreciation for administrative infrastructure, situational analyses to ensure that strategies to address these needs are evidence-based and appropriate to local research needs and already existing infrastructure are still needed. Furthermore, better coordination among the stakeholders involved in various components for research capacity building should be implemented to avoid duplication of efforts.
Health data for cancer research
African scientists should be able to access local, regional and national health information systems data (such as birth and death registration, census, cancer surveillance) to guide effective execution of cancer research. In many regions poor in resources, gaps in the quality and timely availability of vital statistics have greatly hampered the ability to quantify the burden of cancer and direct research priorities.25 Cancer registries are an essential component of those cancer control programmes that aim to achieve the most efficient use of limited resources to gather information on the impact of cancer.1,26–30 Population-based cancer registries provide data on incidence, mortality, stage distribution, treatment patterns, and survival. These data also give information about the cause of cancer as well as about the prevalence of some exposures relative to cancer incidence in the population.31 The costs for registries that cover only a limited proportion of a national population, are relatively little, but the technical and structural barriers to overcome in low-income countries are major. In Africa, in particular, there are few high-quality cancer registries and, although only five registries—which covered just 1% of the African population—were of high enough quality to be published in Cancer Incidence in Five Continents, many more registries are now available.32 In addition, it has been argued that although hospital-based cancer registries cannot provide reliable information about population-based cancer incidence, they can guide governments and public policy interventions.33
Nevertheless, although no firm recommendations can be given on the optimal coverage of a population,34 the number of registries providing coverage for populations in Africa is far below what is needed, and the quality of many, in terms of completeness and validity of data, needs improvement.35 The International Network for Cancer Treatment and Research (INCTR) cancer registry programme is coordinating an African Cancer Registry Network (AFCRN) and works with partners to improve the performance of existing registries and to assist in the establishment of new ones. AFCRN is acting as a consortium that is building several ‘regional hubs’ for the registries in sub-Saharan Africa as part of the International Agency for Research on Cancer (IARC) Global Initiative for Cancer Registration. The hubs serve as centres of expertise that support cancer registration activities by providing training and technical support (including use of registration software, staging of cancers from clinical records, basic data analysis), acting as a focus for collaborative research, and provision of opportunities for networking of members.36
Research funding
Access to cancer research funding continues to be a concern for institutions in Africa. Most African scientists obtain funding support through research collaborations with partners from Europe or North America, where the funding environment is substantially better than in Africa.37 However, this may diminish the ability of African scientists to lead and perform sustainable research relevant to Africa and to build South–South collaborative networks within the continent. Funding agencies have started initiatives with the goal of producing research, education and training opportunities that focus on the needs of African scientists and encourage intracontinental collaborations. Examples include the Medical Education Partnership Initiative (MEPI)38 and the Human Heredity and Health in Africa (H3Africa)39 initiative, which supports the development of networks of African investigators to promote medical education and genomics research in Africa. In these models, African researchers and their institutions serve as the principal investigator and funding recipient. MEPI expects partner institutions in Africa to gradually assume leadership within the 5-year span of the grant.38,39
IARC started collaborative research in Africa in the late 1960s with some of the earliest work on Burkitt lymphoma and liver cancer. Its current active research projects in Africa focus on some of the most frequent types of cancer in the continent (such as cervical, lung, breast, Kaposi sarcoma, and cancer of the oesophagus) with the aims of understanding their aetiology and establishing effective and applicable approaches to prevention. IARC establishes Collaborative Research Agreements to support research projects and thus engendering training for African scientists through the conduct of these joint projects with IARC scientists and other international partners. Other examples include the AORTIC’s Beginning Investigator Grant for Catalytic Research Programme, an early career grant programme that has provided young African scientists with the opportunity to build their research programmes; and the Union for International Cancer Control (UICC) International Cancer Technology transfer (ICRETT) fellowship, which supports professional development for health workers and other stakeholders and facilitates the international transfer of research and clinical skills. In francophone African countries, long-term funding may be secured through research infrastructures that have been established in Africa in collaboration with international institutes and are co-owned with local governments, such as those developed by France’s Institute for Development Research (IRD) or the Institut Pasteur. Longer term funding programmes that support independent and innovative investigator-initiated research for both early-career scientists and senior scientists will be of great importance for the sustainability of research in Africa. The development of international co-ownership of research infrastructures, modelled in francophone Africa, and the partnership between the NIH and Wellcome Trust to support H3Africa serve as great examples for other funding institutes to emulate.39,40
Training programmes
Investments in cancer research personnel through training should be aligned with research activities at both institutional and national levels. Regional training networks create new opportunities for efficient sharing of information and best practices. There are several examples of these training approaches. One is Operation Stop Cervical Cancer in Nigeria (OSCCN), an initiative of MD Anderson Cancer Center, Rice University Department of Bioengineering, The British Columbia Cancer Agency and the University of Ibadan funded by the ExxonMobil Foundation. The OSCCN established six Centres of Excellence for management of cervical cancer in Nigeria and trained over 100 specialists drawn from pathology, gynaecology and nursing specialities.41,42
The field of HIV-associated malignancies (HIVAM) comprises a large and growing number of cancer cases in sub-Saharan Africa, due to the high prevalence of HIV and other infectious agents in many parts of the continent;43 the NIH has supported training grants in HIVAM that partner US and sub-Saharan African institutions. In one model, the nearly decade-old collaboration between the Uganda Cancer Institute (UCI) and the Fred Hutchinson Cancer Research Centre (FHCRC) has three goals: conducting collaborative research on cancer and infectious diseases that may lead to reduced mortality attributable to cancer in both resource-rich and resource-poor settings, building human and physical capacity for cancer research and care in Uganda, and developing new models of cancer care delivery in resource-limited settings.13,44 The collaboration between this Ugandan and US cancer centre also includes the formal stakeholders of the Ugandan Ministry of Health and the two academic partners, Makerere University and the University of Washington. This collaboration has focused on training three types of research team members: research leaders, research managers, and research implementers. Research leaders are enrolled in a 3-year PhD programme featuring didactic coursework at the University of Washington and Makerere University and in a dissertation project conducted by the trainee in Kampala. A fundamental feature of this training is the recognition that, since few researchers in sub-Saharan Africa have the luxury of working exclusively in research, most African researchers must also engage in clinical care and public service. Thus, the research leaders in this programme also engage in coursework in leadership, policy and management, and participate in clinical rotations at both the FHCRC and UCI. Research managers enrol in a Masters of Public Health programme to assure proficiency in the skills of translational research, and also participate in intensive internships in human subjects’ protection, data management, fiscal accountability and grants management, and the responsible conduct of international research. Finally, research implementers are trained through short-term workshops offered regularly in Kampala and taught jointly by faculty from the USA and Uganda. This collaboration also recognized the need for physical infrastructure for excellent patient care and research, and will complete the construction of a state-of-the-art Cancer Centre in Kampala by mid-2014 that will provide care to more than 30,000 outpatients annually, house research staff, and feature four laboratories (pathology, immunology, molecular diagnostics and clinical chemistry/haematology) for both patient care and research.45,46 The multiple research teams built as described above are now carrying out studies including randomized clinical trials, translational studies of cancer biology, epidemiological investigations of cancer aetiology, incidence, and survival in sub-Saharan Africa.4,45–49 A key principle of the collaboration is to transfer as much technology as possible from the US to Uganda to conduct the laboratory investigations associated with patient-oriented research. Currently, more than 50,000 assays are conducted at the Molecular Diagnostics lab in Kampala annually, with new assays being developed with the goal of supporting increasingly complex research as well as serving to benefit patient care.45,46
Yet another example is the University of Ibadan and the University of Chicago international partnership for Interdisciplinary Research Training in Chronic Non-Communicable Diseases and Disorders Across the Lifespan. This partnership builds upon existing trans-national research infrastructure, which began in 1998, and has led to new insights in understanding of the genetic basis of breast cancer across the African diaspora.50,51 The University of Ibadan invested in advanced planning to foster the partnership and has supported over 50 junior academic staff in gaining expertise in clinical research. The University of Ibadan has also prioritized and developed a strategic plan for building high-quality postgraduate training programmes through international partnerships, which has resulted in a nearly 30% growth in the academic professorial cadre. Both, the University of Ibadan and the University of Chicago have benefited from this two-way partnership and have identified additional opportunities for future collaborative research training. In turn, the University of Chicago has benefited by having access to an exceedingly rich experience in country global health for their students and faculty at the University of Ibadan. In addition, the University of Chicago has been able to develop new interdisciplinary areas of scholarship that address health challenges shared by African Americans within the catchment area of the medical centre in Chicago and Africans in Southwest Nigeria. Thus, both the University of Chicago and the University of Ibadan have benefited from this two-way partnership and have identified additional opportunities for future collaborative research. Training will have an interdisciplinary research approach, or a ‘lateral shift’, whereby trainees receive instruction in other disciplines including behavioural research, cancer biology, clinical pharmacology and pharmacogenetics, economics, health services research, genetics, immunology and molecular pathology. This ‘lateral shift’ expands trainees’ knowledge and increases their ability to develop relevant hypotheses, plan appropriate study designs, operationalize research findings, form multi-disciplinary collaborations, and potentiate considerable shifts in thinking and approaches to prevent and cure diseases that affect populations in this region and continent.
A number of funding organizations, such as NCIs of Brazil, France and USA, UICC, AfrOx, and IARC offer a large range of short-term and long-term training activities (science training exchange, training courses in cancer prevention and molecular biology, grantsmanship and publication writing) that fill the gap of research knowledge and leadership among African cancer researchers. Future endeavours should continue to offer opportunities to support leadership programmes within training and career-building programmes.
Cancer research partnerships
The formation of partnerships and networks is one of the most important ways of building sustainable cancer research programmes while fostering improvements in multidisciplinary cancer care in Africa. Aware of the fact that limitations in cancer care infrastructure are often a barrier to good quality research, several of these partnerships have proven to be successful at developing, adapting, and maintaining research collaborations to address important questions and create the needed infrastructure for clinical care and research purposes. One example is the unique public–private partnership, which led to the formation of the Dakar Cancer Consortium (DCC) that has evolved to address prostate and other urological cancers in Senegal. This collaborative group began in 2001 with the interaction of investigators who were united by a common interest in prostate cancer in the African diaspora. The collaboration was preceded by an assessment of the needs regarding clinical and laboratory resources, qualified researchers, and administrative infrastructure. Whereas these resources are often available at a single US institution, no single institution in Dakar could meet all of these needs. However, the required resources were identified or could be developed across multiple institutions in Dakar and illustrate how research can be appropriate to local health challenges, and be conducted within existing research and clinical infrastructure. Thus, patient and clinical resources were found at the private Hôpital General de Grand Yoff and the public Hôpital Aristide le Dantec; state of the art laboratory resources were identified in private clinical laboratories including the Centre de Diagnostic et de Recherche en Medicine Moleculaire (CDRMM) and Bio24; and qualified researchers in a variety of disciplines were identified at each of these institutions as well as the Université Cheikh Anta Diop and the Institut Pasteur. Thus, the required research resources were available and could be enhanced through a partnership of public and private institutions.52 It also became clear that a neutral body could help in facilitating the multi-institutional interactions and submission of grant applications. Thus, the Institut de Recherche et de Formation en Urologie et en Santé Familiale (IFRU-SF) was founded in Dakar in 2004.53 The IFRU-SF serves as a focal point for the interaction of multiple institutions and investigators involved in collaborative clinical and research activities in Senegal. The IFRU-SF and the DCC also serve as leaders in larger collaborative activities for prostate cancer research across the African diaspora, including the multinational Men of African Descent and Carcinoma of the Prostate (MADCaP) consortium.54
With initial seed funding from the Institute National du Cancer (INCa), MADCaP has inspired a move towards setting up an HPV-Cervical Cancer Network in some African countries to address cervical cancer in sub-Saharan African women.55 Such research has important implications in establishing the pattern, prevalence, and carcinogenicity of different high-risk HPV infection in African women and the interaction with HIV.56 It also has the potential to contribute to policy and implementation of HPV screening and vaccination. However, it will constitute a much needed forum to discuss current or planned HPV/cervical cancer research protocols, study design, patient recruitment, data collection, analysis of outcomes and recommendations.
IARC, the Medical Research Council UK and the Gambian Government established the Gambia Hepatitis Intervention Study (GHIS) in the mid-1980s to conduct a randomized trial of the HBV vaccine among 120,000 newborns in relation to liver cancer prevention.57 The IARC-led GHIS resulted in advances in cancer control through introduction of the HBV vaccine nationally and with high coverage. As a result, chronic HBV infection rates in young Gambian children are now less than 1% compared with 15–20% when the research project—which provided much of the vaccine delivery infrastructure and expertise—was started.58 The GHIS has been seminal in establishing the efficacy of the vaccine in preventing chronic HBV carriage. The long-term follow-up (40 years) is ongoing and needed the establishment of the Gambian National Cancer Registry, which is one of the few national population-based registries in Africa to provide data from rural communities. The GHIS has also served as a stimulus to a wide range of associated cancer research studies59–61 and developments of the expanded programme of immunization in the country.57
The Nigerian Breast Cancer Study (NBCS) is an ongoing genetic epidemiology study of invasive breast cancer conducted in Ibadan since January 1998 and has expanded as the African Breast Cancer Study to Uganda and Cameroon.52 A multidisciplinary team of African breast surgeons, radiation oncologists, pathologists, laboratory scientists, and field epidemiologists at the University of Ibadan and Ibadan Cancer Registry have collaboratively published extensively on breast cancer genetics.62–64 This study continues to provide new opportunities for collaborative and practical research training. Collaborative work between pathologists and technicians from the University of Chicago and Ibadan has led to the establishment of the Breast Cancer Laboratory at the Institute of Medical Research and Training at the University of Ibadan in 2004. This initiative has helped the development of local expertise to operate the laboratory, and the University of Chicago continues to provide Quality Assurance support with web-based conferences held periodically to discuss technical aspects of pathology/cytology and to resolve discrepant cases.65 The NBCS has also allowed the University of Ibadan to develop the Breast Imaging Centre of Excellence, where lead investigators from this University are trained in sound-mammography and ultrasound-guided breast-core biopsies. In turn, the University of Ibadan has developed a training programme for breast imaging in West Africa, and this investment has led to the creation of one of the largest databases of mammogram and ultrasound imaging in sub-Saharan Africa.59,61–64 In addition, the NBCS team developed infrastructure to support multi-institutional clinical research and completed the enrolment in a multicentric phase II study that evaluated the efficacy, safety, and genomic markers of response to capecitabine as neoadjuvant therapy in women with newly diagnosed, locally advanced breast cancer.60 The study was developed and implemented in collaboration with the University of Ibadan and the Obafemi Awolowo University Teaching Hospital. Conducting this study provided a first-hand opportunity to assess the enormous difficulties faced by investigators in Nigeria and other African countries in conducting clinical research. There remains great need to continue to build and strengthen ethics review boards, train clinicians and staff to conduct research, monitor compliance with study protocol, prepare for a site audit, and create a robust clinical trial infrastructure.
Community engagement
Although it is certainly important for scientists to engage each other, it is equally important that scientists engage the communities who will participate in their research and benefit from it.66 The Epidemiology of Burkitt lymphoma in East-African Children and Minors (EMBLEM) consortia—a partnership among investigators from the US NCI, Uganda, Kenya and Tanzania—uses a mixture of research collaboration and community engagement to improve the management of Burkitt lymphoma in Africa.67–73 Whereas significant progress has been made in the treatment of childhood cancers in the developed world, children with cancer living in Africa have a lesser chance of being cured due to a lack of healthcare resources.74 Burkitt lymphoma is one of the most common forms of paediatric cancer, and is easily treatable if diagnosed early; however, the incidence of Burkitt lymphoma has increased in endemic areas in Africa where infections by HIV and malaria are also high.71
Given the historical challenges of the previous research collaboration for Burkitt lymphoma between the US NCI and Ugandan Cancer Institute, EMBLEM has embedded their research activities within the African government healthcare services. In this process, innovative health communication messages have been developed and community research assistants have been trained as local knowledge point sources to strengthen referral of Burkitt lymphoma cases to regional healthcare centres with capacity to diagnose and treat Burkitt lymphoma, such as the St Mary’s Hospital, in Lacor, northern Uganda. A relevant mix of advanced research technologies, including proteomics and genomics, has been implemented. This infrastructure is nested within local community health system and provides improvements in community engagement, diagnostic pathology, and consistent use of protocol-based treatment. The result is an immediate broad-based impact on local patient care and a positive impact on community health workers who are involved in case spotting, referral, diagnosis and treatment. In addition, the EMBLEM centres are regionally linked resulting in easier transfer of best practices and clinical information. One of EMBLEM’s long-term objectives is to advocate for support for cancer research, something that has been successfully implemented at the EMBLEM sites in Kenya and Tanzania. In Kenya, discussions that led to the formulation of the National Cancer Control Plan indicated an intention to implement and strengthen the components of the paediatric cancer control plan at EMBLEM sites.
One framework for empowering patients in research is the Community-Engaged Research (CEnR). With the CEnR, the patient community is engaged in all phases of research, beginning from the development of research objective to study design, to participants’ recruitment and retention, instrument design, and data collection, analysis, interpretation and dissemination.75 The role of the researcher is very important in CEnR as it calls for a researcher–patient collaboration. Researchers can empower patients through partnerships in all phases of research, thus promoting co-learning that facilitates reciprocal transfer of knowledge, skills, and capacity. To that extent balance between research and action, active dissemination of knowledge gained from research to all partners in a language that is understandable and respectful, and long-term commitment to the partnership with patients are needed.75 AORTIC is one of the organizations at the forefront of training research advocates in Africa. In line with AORTIC’s goal of advancing effective cancer control policies and programme implementation in Africa, AORTIC partnered up with the University of Florida and the Prostate Net to implement the first biennial International Workshop on Cancer Advocacy for African Countries (CAAC) during the AORTIC’s 8th International Cancer Conference in Cairo, Egypt in November, 2011. The CAAC workshop trained over 70 African advocates from 12 African countries and led to the founding of the African Cancer Advocates Consortium (ACAC) with a commitment to “make cancer a top priority in Africa”.76,77
Conduct of responsible research
Developing countries have shown a growing interest in joining multi-national oncology clinical trials. Although the proportion of participants recruited into clinical trials from low-income countries has increased from 8.9% in 2003 to 17.5% in 2007, most of these patients were from low-and middle-income countries excluding sub-Saharan African countries.78,79 Nevertheless, there have been concerns about exploitation and vulnerability of African patients where income is low and regulations are lax.79 These ethical concerns need to be addressed if high quality research infrastructure is to be built in Africa. To that end, major investment in several programmes has been made to develop systematic ethics review process and to enhance responsible conduct of research in African nations. Examples of such investments include the French National Agency for Research on AIDS and Viral Hepatitis (ANRS), who fund around 50 projects per annum covering clinical trials and epidemiology, and the US NIH, which funds several research ethics training programmes throughout Africa.39,80,81
ANRS took a three-stage approach: first, establishment of North–South partnerships between collaborating ANRS Sites; second, development of the ANRS Ethics Charter; and third, the building of quality indicators to evaluate compliance to the Charter. After numerous consultations between North and South researchers, representatives of civil societies and members of ethical committees, an ethics charter was published in 2002 which addressed biomedical research, basic science, public health research, social sciences and prevention studies related to AIDS and viral hepatitis.82 This charter is eminently translatable for cancer research as it was based on a philosophy of dynamism and continuous improvement so that it might respond to changing societal values as well as some of the eternal verities.
Nigeria provides another case study of development of research ethics regulatory infrastructure in an African country largely funded through the United States’ National Institutes of Health’s Fogarty International Centre81 as part of a programme for development of research ethics throughout the world.83 As one of the funded programmes, the West African Bioethics (WAB) Training Programme84 has sponsored 32 trainees in Nigerian Masters in Bioethics to date; medium duration diploma training has been given to 33 trainees, and short duration onsite and online trainings in collaboration with Collaborative Institutional Training Initiative (CITI) and the Training and Resources in Research Ethics Evaluation (TRREE) programmes has been offered to over 5,000 participants. In addition, WAB provides technical assistance to the Nigerian National Health Research Ethics Committee in policy and guidelines development as well as central ethics review; it also gives advise to the government on matters relating to research ethics.85 This is representative of the considerable investment that has been made over the past decades in research ethics capacity development in Africa by organizations including the US NIH and the European and Developing Countries Clinical Trials Partnership (EDCTP).83,86
Conclusions
Despite the many and often repeated barriers associated with conducting basic, clinical and translational research studies, we have cited here many excellent examples of successful programmes that have enhanced the development of research capacity and contributed to relevant research data for Africa. The most successful models have been driven initially by collaboration between scientists, in and out of Africa, motivated by science relevant to Africa’s needs, but these soon extended to institutional platforms. Nevertheless, there are still gaps and needs in research capacity building that need addressing (Box 1). How to address these issues will continue to evolve but, so far a coordinated effort among stakeholders to move forward to a more concerted stage of planning for cancer research in Africa is taking shape.
Box 1 | Meeting recommendations.
-
▪
Encourage investigators to address public health issues through research
-
▪
Support multiple disciplines for cancer research, including implementation science, epidemiology, clinical research, health economics, palliative care and behavioural research
-
▪
Align research funding and administrative programmes to set the tone of fiscal responsibility within African institutions. Research administrative offices will also assist African scientists with issues related to grants administration and research oversight
-
▪
Continue to improve the quality of health information and databases that could be used for all aspects of cancer research
-
▪
Perform situational analyses to address infrastructural needs for Africa at both the institutional and national level. Situation analyses will help identify specific needs for various components of research infrastructure and would inform future strategic planning for capacity building
-
▪
Promote better coordination within institutions among the countries (governments, academic institutions, public–private partnerships, international agencies) to minimize duplication of efforts
-
▪
Expand the small grants programmes for early career scientists and create longer term grant funding for all scientists. This funding should support independent and innovative investigator-initiated research in Africa and should also include a training component
-
▪
Reinforce the research collaborations models that already exist and work well. Continue to support research collaborations by creating of research consortia that would strengthen South–South research networks
-
▪
Support the creation of a registry of current research activities in Africa
-
▪
Create education and training opportunities that promote innovation. Training opportunities should also include the development of skills sets such as grant and publication writing
-
▪
Continue to create and support opportunities for leadership training (such as ACLI) and mentoring, building mentor–mentee relationships and leading to sustainable cancer research programmes
-
▪
Engage the community and policy makers. Advocates will be an important asset in working within the communities and government systems to make cancer control and prevention a health priority
-
▪
Development of the capacity to support ethical, legal and social implications (ELSI) for cancer research: ELSI will be extremely important in developing culturally appropriate means of engaging with communities, especially research participants. ELSI will also be important for assessing methods for ethical review of research protocols and other aspects of research in Africa
Key points.
-
▪
Research has a pivotal role in cancer control planning as it will lead to the development of evidence-based strategies for cancer prevention and control relevant to Africa
-
▪
Cancer research programmes should be multi-disciplinary and contain a research–career component for the development of African scientists as research leaders and mentors, which will lead to sustainable research programmes
-
▪
International funding agencies and pharmaceutical companies should support the creation of long-term funding to foster rigorous and innovative investigator-initiated research
-
▪
The formation of North–South and South–South partnerships and networks is essential for the creation of the infrastructure and environment needed to promote research
-
▪
African scientists should engage country communities and policy-makers to promote community and country ownership of research programmes
-
▪
Cancer research should be accompanied by the highest levels of ethical, legal and socially appropriate standards to ensure the protection of patients
Review criteria.
An extensive literature search was performed using PubMed and/or Google Scholar, with the following search terms: “burden of cancer in Africa”, “cancer control in Africa”, “cancer control and cancer research in Africa”, “burden of paediatric cancer in Africa”, “cancer and infectious agents”, “cost-effectiveness of cancer control in Africa”, “role of cancer registries in cancer control and research”, “community engagement in research in developing countries”. Scientific articles published in the time period from 1992 to 2014 were included in this manuscript. Information on various programmes and activities presented in the manuscript was obtained via personnel communication with the principal investigators of the programmes, who are also authors on the manuscript. Published manuscripts or online information describing these programmes or activities are provided in the reference list.
Acknowledgements
We would like to thank all of the attendees of the “Cancer in Africa: building transnational research collaborations” for their tremendous contribution to the discussions during the meeting.
Footnotes
Competing interests
The authors declare no competing interests.
Author contributions
I.A., D.N.M., M.J.W., C.A., K.B., C.B., C.C., C.P.W. and D.J.K. researched data for article. I.A., D.N.M., M.J.W., C.A., C.C., S.M.M., F.T.O., O.I.O., C.O.O., D.M.P., T.R.R., H.R., J.T., C.P.W. and A.M.Y. made a substantial contribution to discussion of content. I.A., D.N.M., M.J.W., C.A., C.B., C.C., R.L., S.M.M., F.T.O., O.I.O., D.M.P., T.R.R., H.R., L.A.S., J.T., C.P.W. and A.M.Y. wrote the article; and all authors reviewed and edited the manuscript before submission.
References
- 1.Ferlay J, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Sylla BS, Wild CP. A million africans a year dying from cancer by 2030: what can cancer research and control offer to the continent? Int.. J. Cancer. 2012;130:245–250. doi: 10.1002/ijc.26333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gondos A, Brenner H, Wabinga H, Parkin DM. Cancer survival in Kampala, Uganda. Br. J. Cancer. 2005;92:1808–1812. doi: 10.1038/sj.bjc.6602540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coghill AE, et al. Contribution of HIV infection to mortality among cancer patients in Uganda. AIDS. 2013;27:2933–2442. doi: 10.1097/01.aids.0000433236.55937.cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Martel C, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012;13:607–615. doi: 10.1016/S1470-2045(12)70137-7. [DOI] [PubMed] [Google Scholar]
- 6.Mgaya EM, Kitinya JN. Histopathology of malignant tumours of childhood in Tanzania. East Afr. Med. J. 2000;77:435–439. [PubMed] [Google Scholar]
- 7.Msyamboza KP, et al. Burden of cancer in Malawi; common types, incidence and trends: national population-based cancer registry. BMC Res. Notes. 2012;5:149. doi: 10.1186/1756-0500-5-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chintu C, Athale UH, Patil PS. Childhood cancers in Zambia before and after the HIV epidemic. Arch. Dis. Child. 1995;73:100–104. doi: 10.1136/adc.73.2.100. discussion 104–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sinfield RL, et al. Spectrum and presentation of pediatric malignancies in the HIV era: experience from Blantyre, Malawi, 1998–2003. Pediatr. Blood Cancer. 2007;48:515–520. doi: 10.1002/pbc.20917. [DOI] [PubMed] [Google Scholar]
- 10.Lingwood RJ, et al. The challenge of cancer control in Africa. Nat. Rev. Cancer. 2008;8:398–403. doi: 10.1038/nrc2372. [DOI] [PubMed] [Google Scholar]
- 11.WHO. 2nd edn. Geneva: WHO; 2002. National cancer control programmes: policies and managerial guidelines. [Google Scholar]
- 12.Kirigia JM, Wambebe C. Status of national health research systems in ten countries of the WHO African Region. BMC Health Serv. Res. 2006;6:135. doi: 10.1186/1472-6963-6-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kingham TP, et al. Treatment of cancer in sub-Saharan Africa. Lancet Oncol. 2013;14:e158–e167. doi: 10.1016/S1470-2045(12)70472-2. [DOI] [PubMed] [Google Scholar]
- 14.Irikefe V, et al. Science in Africa: the view from the front line. Nature. 2011;474:556–559. doi: 10.1038/474556a. [DOI] [PubMed] [Google Scholar]
- 15.Ginsberg GM, Lauer JA, Zelle S, Baeten S, Baltussen R. Cost effectiveness of strategies to combat breast, cervical, and colorectal cancer in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ. 2012;344:e614. doi: 10.1136/bmj.e614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Regional Committee for Africa, WHO. Health financing: a strategy for the African region. Ethiopia: Addis Ababa; 2006. 56 session. [Google Scholar]
- 17.Goldie SJ. Health economics and cervical cancer prevention: a global perspective. Virus Res. 2002;89:301–309. doi: 10.1016/s0168-1702(02)00199-5. [DOI] [PubMed] [Google Scholar]
- 18.Peprah E, Wonkman A. Biomedical research, a tool to address the health issues that affect African populations. Global Health. 2013;9:50. doi: 10.1186/1744-8603-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yusuf S, Baden T, Prieto-Godino LL. Bridging the gap: establishing the necessary infrastructure and knowledge for teaching and research in neuroscience in Africa. Metab. Brain Dis. doi: 10.1007/s11011-013-9443-x. http://dx.doi:10.1007/s11011-013-9443-x. [DOI] [PubMed] [Google Scholar]
- 20.Adesina A, et al. Improvement of pathology in sub-Saharan Africa. Lancet Oncol. 2013;14:e152–e157. doi: 10.1016/S1470-2045(12)70598-3. [DOI] [PubMed] [Google Scholar]
- 21.John TA. Facilities available for biomedical science research in the public universities in Lagos, Nigeria. Niger. Postgrad. Med. J. 2010;17:6–14. [PubMed] [Google Scholar]
- 22.Eunice Kennedy Shriver National Institute of Child. Health and Human Development, National Institute of Health. Biomedical/Biobehavioral Research Administrator Development Program. 2012 [online], http://www.nichd.nih.gov/about/org/od/ohe/brad/Pages/overview.aspx.
- 23.Office of the Director. National Institutes of Health. NIH Record—BRAD trains in development of research infrastructure. 2012 [online], http://nihrecord.od.nih.gov/newsletters/2012/09_14_2012/story9.htm.
- 24.Association of Research Administrators in Africa. 2009 [online], http://araafrica.org. [Google Scholar]
- 25.Hanna TP, Kangolle AC. Cancer control in developing countries: using health data and health services research to measure and improve access, quality and efficiency. BMC Int. Health Hum. Rights. 2010;10:24. doi: 10.1186/1472-698X-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parkin DM. The global burden of cancer. Semin. Cancer Biol. 1998;8:219–235. doi: 10.1006/scbi.1998.0080. [DOI] [PubMed] [Google Scholar]
- 27.Parkin DM, Muir CS, Whelan SL, Gao Y-T, Ferlay J, Powell J, editors. Cancer Incidence in Five Continents. VI. Lyon: IARC Press; 1992. [Google Scholar]
- 28.Parkin DM. Cancer in developing countries. Cancer Surv. 1994;19–20:519–561. [PubMed] [Google Scholar]
- 29.Parkin DMFJ, Hamdi-Cherif M, Sitas F, Thomas JO, Wabinga H, Whelan SL, editors. Cancer in Africa: Epidemiology and Prevention. ARC Press; Lyon: 2003. [Google Scholar]
- 30.Parkin DM, Vizcaino AP, Skinner ME, Ndhlovu A. Cancer patterns and risk factors in the African population of southwestern Zimbabwe, 1963–1977. Cancer Epidemiol. Biomarkers Prev. 1994;3:537–547. [PubMed] [Google Scholar]
- 31.Parkin DM. The role of cancer registries in cancer control. Int. J. Clin. Oncol. 2008;13:102–111. doi: 10.1007/s10147-008-0762-6. [DOI] [PubMed] [Google Scholar]
- 32.Curado MP, et al. Cancer Incidence in Five Continents. IX. Lyon: IARC Press; 2007. [Google Scholar]
- 33.Jedy-Agba EE, et al. The role of hospital-based cancer registries in low and middle income countries-The Nigerian Case Study. Cancer Epidemiol. 2012;36:430–435. doi: 10.1016/j.canep.2012.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jensen OM, Whelan S. Planning a cancer registry. IARC Sci. Publ. 1991:22–28. [PubMed] [Google Scholar]
- 35.Parkin DM. The evolution of the population-based cancer registry. Nat. Rev. Cancer. 2006;6:603–612. doi: 10.1038/nrc1948. [DOI] [PubMed] [Google Scholar]
- 36.African Cancer Registry Network. 2013 [online], http://www.afcrn.org.
- 37.Lansang MA, Dennis R. Building capacity in health research in the developing world. Bull. World Health Organ. 2004;82:764–770. [PMC free article] [PubMed] [Google Scholar]
- 38.Fogarty International Center. The Medical Education Partnership Initiative. 2011 [online], http://www.fic.nih.gov/programs/Pages/medical-education-africa.aspx.
- 39.H3Africa. Human Health and Heredity in Africa. 2011 [online], http://www.h3africa.org. [Google Scholar]
- 40.National Heart, Lung and Blood Institute, National Institutes of Health. United Health and NHLBI Collaborating Centers of Excellence. 2009 [online], http://www.nhlbi.nih.gov/about/globalhealth/centers/
- 41.Miller D, et al. Knowledge dissemination and evaluation in a cervical cancer screening implementation program in Nigeria. Gynecol. Oncol. 2007;107:S196–S207. doi: 10.1016/j.ygyno.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 42.Roblyer D, Richards-Kortum R, Park SY, Adewole I, Follen M. Objective screening for cervical cancer in developing nations: lessons from Nigeria. Gynecol. Oncol. 2007;107:S94–S97. doi: 10.1016/j.ygyno.2007.07.042. [DOI] [PubMed] [Google Scholar]
- 43.Casper C. The increasing burden of HIV-associated malignancies in resource-limited regions. Annu. Rev. Med. 2011;62:157–170. doi: 10.1146/annurev-med-050409-103711. [DOI] [PubMed] [Google Scholar]
- 44.Silberner J. The Seattle Times. Washington: Seattle; 2012. The Hutch, Uganda gets creative in cancer fight. [Google Scholar]
- 45.Gantt S, et al. Clinical presentation and outcome of epidemic Kaposi sarcoma in Ugandan children. Pediatr. Blood Cancer. 2010;54:670–674. doi: 10.1002/pbc.22369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Johnston C, et al. Impact of HIV infection and Kaposi sarcoma on human herpesvirus-8 mucosal replication and dissemination in Uganda. PLoS ONE. 2009;4:e4222. doi: 10.1371/journal.pone.0004222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bateganya MH, et al. Predictors of survival after a diagnosis of non-Hodgkin lymphoma in a resource-limited setting: a retrospective study on the impact of HIV infection and its treatment. J. Acquir. Immune Defic. Syndr. 2011;56:312–319. doi: 10.1097/QAI.0b013e31820c011a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goldman JD, et al. Measurement of the impact of antiretroviral therapy coverage on incidence of AIDS-defining malignancies in sub-Saharan Africa [abstract] Lancet. 2011;377(Suppl.):969–970. a37. [Google Scholar]
- 49.Phipps W, et al. Gender differences in clinical presentation and outcomes of epidemic Kaposi sarcoma in Uganda. PLoS ONE. 2010;5:e13936. doi: 10.1371/journal.pone.0013936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huo D, et al. Population differences in breast cancer: survey in indigenous African women reveals over-representation of triple-negative breast cancer. J. Clin. Oncol. 2009;27:4515–4521. doi: 10.1200/JCO.2008.19.6873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang J, et al. Recurrent BRCA1 and BRCA2 mutations in breast cancer patients of African ancestry. Breast Cancer Res. Treat. 2012;134:889–894. doi: 10.1007/s10549-012-2136-z. [DOI] [PubMed] [Google Scholar]
- 52.Morhason-Bello IO, et al. Challenges and opportunities in cancer control in Africa: a perspective from the African Organisation for Research and Training in Cancer. Lancet Oncol. 2013;14:e142–e151. doi: 10.1016/S1470-2045(12)70482-5. [DOI] [PubMed] [Google Scholar]
- 53.Institut de formation et de Rescherche. Institut de formation et de Rescherche en Urologie. 2014 [online], http://ifru.org. [Google Scholar]
- 54.Rebbeck TR, et al. Global patterns of prostate cancer incidence, aggressiveness, and mortality in men of african descent. Prostate Cancer. 2013;2013:560857. doi: 10.1155/2013/560857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.African Organization for Research and Training Cancer. HPV Cervical Cancer Network in Francophone Africa. 2013 [online], http://www.aortic2013.org/assets/pdf/AORTIC%202013%20Abstract%20Publication.pdf. [Google Scholar]
- 56.Denny L. Cervical cancer prevention: new opportunities for primary and secondary prevention in the 21st century. Int. J. Gynaecol. Obstet. 2012;119(Suppl. 1):S80–S84. doi: 10.1016/j.ijgo.2012.03.023. [DOI] [PubMed] [Google Scholar]
- 57.Viviani S, et al. 20 years into the Gambia Hepatitis Intervention Study: assessment of initial hypotheses and prospects for evaluation of protective effectiveness against liver cancer. Cancer Epidemiol. Biomarkers Prev. 2008;17:3216–3223. doi: 10.1158/1055-9965.EPI-08-0303. [DOI] [PubMed] [Google Scholar]
- 58.Peto TJ, et al. Efficacy and effectiveness of infant vaccination against chronic hepatitis B in the Gambia Hepatitis Intervention Study (1986–1990) and in the nationwide immunisation program. BMC Infect. Dis. 2014;14:7. doi: 10.1186/1471-2334-14-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fackenthal JD, et al. High prevalence of BRCA1 and BRCA2 mutations in unselected Nigerian breast cancer patients. Int. J. Cancer. 2012;131:1114–1123. doi: 10.1002/ijc.27326. [DOI] [PubMed] [Google Scholar]
- 60.Arowolo OA, et al. Neo-adjuvant capecitabine chemotherapy in women with newly diagnosed locally advanced breast cancer in a resource-poor setting (Nigeria): efficacy and safety in a phase II feasibility study. Breast J. 2013;19:470–477. doi: 10.1111/tbj.12149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zheng Y, et al. Fine mapping of breast cancer genome-wide association studies loci in women of African ancestry identifies novel susceptibility markers. Carcinogenesis. 2013;34:1520–1528. doi: 10.1093/carcin/bgt090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adebamowo CA, et al. Obesity and height in urban Nigerian women with breast cancer. Ann. Epidemiol. 2003;13:455–461. doi: 10.1016/s1047-2797(02)00426-x. [DOI] [PubMed] [Google Scholar]
- 63.Ogundiran TO, et al. Case-control study of body size and breast cancer risk in Nigerian women. Am. J. Epidemiol. 2010;172:682–690. doi: 10.1093/aje/kwq180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fackenthal JD, et al. Complete allelic analysis of BRCA1 and BRCA2 variants in young Nigerian breast cancer patients. J. Med. Genet. 2005;42:276–281. doi: 10.1136/jmg.2004.020446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Oluwasola AO, et al. Use of web-based training for quality improvement between a field immunohistochemistry laboratory in Nigeria and its United States-based partner institution. Ann. Diagn. Pathol. 2013;17:526–530. doi: 10.1016/j.anndiagpath.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 66.Tindana PO, et al. Grand challenges in global health: community engagement in research in developing countries. PLoS Med. 2007;4:e273. doi: 10.1371/journal.pmed.0040273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ogwang MD, Bhatia K, Biggar RJ, Mbulaiteye SM. Incidence and geographic distribution of endemic Burkitt lymphoma in northern Uganda revisited. Int. J. Cancer. 2008;123:2658–2663. doi: 10.1002/ijc.23800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ogwang MD, Zhao W, Ayers LW, Mbulaiteye SM. Accuracy of Burkitt lymphoma diagnosis in constrained pathology settings: importance to epidemiology. Arch. Pathol. Lab. Med. 2011;135:445–450. doi: 10.1043/2009-0443-EP.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schmitz R, et al. Burkitt lymphoma pathogenesis and therapeutic targets from structural and functional genomics. Nature. 2012;490:116–120. doi: 10.1038/nature11378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Baik S, et al. A case-control study of Burkitt lymphoma in East Africa: are local health facilities an appropriate source of representative controls? Infect. Agent Cancer. 2012;7:5. doi: 10.1186/1750-9378-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mbulaiteye SM, et al. African Burkitt’s lymphoma: could collaboration with HIV-1 and malaria programmes reduce the high mortality rate? Lancet. 2010;375:1661–1663. doi: 10.1016/S0140-6736(10)60134-1. [DOI] [PubMed] [Google Scholar]
- 72.Aka P, et al. Incidence and trends in Burkitt lymphoma in northern Tanzania from 2000 to 2009. Pediatr. Blood Cancer. 2012;59:1234–1238. doi: 10.1002/pbc.24194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.National Cancer Institute. The Epidemiology or Burkitt Lymphoma in East African Children and Minors (EMBLEM) 2010 [online], http://emblem.cancer.gov/
- 74.Harif M, Traore F, Hessissen L, Moreira C, Atteby JJ. Challenges for paediatric oncology in Africa. Lancet Oncol. 2013;14:279–281. doi: 10.1016/S1470-2045(12)70569-7. [DOI] [PubMed] [Google Scholar]
- 75.Michener L, et al. Aligning the goals of community-engaged research: why and how academic health centers can successfully engage with communities to improve health. Acad. Med. 2012;87:285–291. doi: 10.1097/ACM.0b013e3182441680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Odedina FT, et al. The African cancer advocacy consortium: shaping the path for advocacy in Africa. Infect. Agent Cancer. 2013;8(Suppl. 1):S8. doi: 10.1186/1750-9378-8-S1-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Segal R, Odedina FT, Pressey S. Proceedings of the international workshop on cancer advocacy for african countries. Infect. Agent Cancer. 2013;8(Suppl. 1):8. doi: 10.1186/1750-9378-8-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mano MS, Rosa DD, Dal Lago L. Multinational clinical trials in oncology and post-trial benefits for host countries: where do we stand? Eur. J. Cancer. 2006;42:2675–2677. doi: 10.1016/j.ejca.2006.02.028. [DOI] [PubMed] [Google Scholar]
- 79.Arai RJ, Mano MS, de Castro G, Jr, Diz Mdel P, Hoff PM. Building research capacity and clinical trials in developing countries. Lancet Oncol. 2010;11:712–713. doi: 10.1016/S1470-2045(10)70168-6. [DOI] [PubMed] [Google Scholar]
- 80.Hanna M, et al. Development of a checklist of quality indicators for clinical trials in resource-limited countries: the French National Agency for Research on AIDS and Viral Hepatitis (ANRS) experience. Clin. Trials. 2013;10:300–318. doi: 10.1177/1740774512470765. [DOI] [PubMed] [Google Scholar]
- 81.Fogarty International Center. International Research Ethics Education and Curriculum Development Award. 2012 [online], http://www.fic.nih.gov/programs/pages/bioethics.aspx.
- 82.Agence Nationale de recherches sur le sida et les hepatites virale. Ethic Charter for Research in Developing Countries. Paris, France: 2008. pp. 1–12. [Google Scholar]
- 83.Glass R. International research ethics education. J. Empir. Res. Hum. Res. Ethics. 2013;8:1–2. doi: 10.1525/jer.2013.8.5.1. [DOI] [PubMed] [Google Scholar]
- 84.Adebamowo CA, Mafe MA, Yakubu AA, Adekeye JM, Jiya JJ. Developing ethical oversight of research in developing countries: case study in Nigeria. Harvard Health Policy Review. 2007;8:96–106. [Google Scholar]
- 85.Yakubu A, Adebamowo CA. Implementing National System of Health Research Ethics Regulations: The Nigerian Experience. BEOnline. 2012;1:4–15. [PMC free article] [PubMed] [Google Scholar]
- 86.Olliaro P, Smith PG. The European and developing countries clinical trials partnership. J. HIV Ther. 2004;9:53–56. [PubMed] [Google Scholar]