Abstract
Objective
Knee and hip osteoarthritis (OA) are known risk factors for falls, but whether they together additionally contribute to falls risk is unknown. This study utilizes a biracial cohort of men and women to examine the influence of lower limb OA burden on the risk for future falls.
Methods
A longitudinal analysis was performed using data from 2 time points of a large cohort. The outcome of interest was falls at follow up. Covariates included age, sex, race, body mass index, a history of prior falls, symptomatic OA of the hip and/or knee, a history of neurologic or pulmonary diseases, and current use of narcotic medications. Symptomatic OA was defined as patient reported symptoms and radiographic evidence of OA in the same joint. Logistic regression analyses were used to determine associations between covariates and falls at follow-up.
Results
The odds of falling increased with an increasing number of lower limb symptomatic OA joints: those with 1 joint had 53% higher odds, those with 2 joints had 74% higher odds, those with 3–4 OA joints had 85% higher odds. When controlling for covariates, patients who had symptomatic knee or hip OA had an increased likelihood of falling (aOR 1.39 95% CI [1.02, 1.88]; aOR 1.60 95% CI [1.14, 2.24], respectively).
Conclusions
This study reveals the risk for falls increases with additional symptomatic OA lower limb joints and confirms that symptomatic hip and knee OA are important risk factors for falls.
Falls are a leading cause of morbidity and mortality in the elderly population and provide a substantial contribution to the healthcare cost burden [1–4]. In 2005, the CDC estimated that falls were associated with an estimated 24 billion healthcare dollars [1]. Approximately 15–33% of the elderly population experience a fall every year and approximately 10 percent of all emergency department visits are secondary to falls [5–7]. As the population ages, the number of falls continues to grow. According to one study, the number of falls in the United States increased by 50% from 2001 to 2008 [7, 8]. Given this large impact of falls, it is essential to identify risk factors contributing to falls, particularly those that are modifiable. Many risk factors for falls have been considered; including female sex, balance, gait and visual deficits, diabetes and musculoskeletal diseases, including osteoarthritis (OA) [2–4, 9, 10].
OA is the most common form of arthritis, affecting an estimated 26.9 million adults in the U.S. in 2005, and is thought to be a risk factor for falls in the adult population [1, 11–13]. It has been reported that individuals with self-reported OA experience 25% more falls than those without OA, and up to 50% of people with OA experience a fall every year [6, 13]. The Centers for Disease Control and Prevention recently reported that older adults with self-reported physician-diagnosed arthritis had an increased risk for fall-related injuries, and were more than twice as likely to have 2 or more falls than those without arthritis [14]. Although this study helps show that arthritis is an important risk for falls, and should be considered in fall prevention, it has several limitations. The definition of arthritis was based on patient self-report of a healthcare professional diagnosis including “some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia.” Information regarding specific types of arthritis, what joints or how many joints were affected, or whether there was radiographic evidence of arthritis were lacking. Additionally, the results were based on a cross-sectional analysis and could not infer causality, especially when examining a chronic disease such as arthritis.
Also illustrating the need for further research on the association between OA and falls are several studies that have shown OA may not be a risk for falls in certain populations [15]. For example, elderly men with radiographic OA of the knee and/or lumbar spine may not have an increased risk for falls, whereas women likely do [16]. Another group concluded that women with radiographic hip OA actually had a risk reduction by 30–40% for 2 or more falls, while those with self-reported arthritis or musculoskeletal symptoms had an increased risk for recurrent falls [17]. Foley et al. found that falls were associated with musculoskeletal pain and dysfunction but not with radiographic OA [11]. This literature suggests that certain populations with OA may be at more risk for falls than others, but is limited by the demographics of the study populations (each study was based solely on a single race or sex) and a lack of available simultaneous symptomatic and radiographic evidence of OA. Further illustrating the need for more research, OA in multiple joint sites may increase risk beyond a single joint site alone. However, to date, there have been no studies exploring the effects of multi-joint OA on risk for falls.
The purpose of this analysis, therefore, was to explore risk factors associated with falls in persons with and without lower extremity OA. This was accomplished using a large cohort and longitudinal analysis of African American and Caucasian men and women, with a focus on symptomatic knee and/or hip OA and the cumulative effects of lower extremity multi-joint OA. The results of this study will help determine which people are at a higher risk for falls and lead to a better understanding of the relationship between lower extremity OA and the risk for falls.
PARTICIPANTS AND METHODS
This longitudinal study used data from the Johnston County OA Project, a community-based prospective cohort study of non-institutionalized African American and Caucasian men and women, aged 45 years and older, living in rural North Carolina, both with and without OA, as previously described [18]. All participants provided written informed consent and completed 2 home interviews and one clinic visit during the baseline data collection (between 1999–2003, including the first follow-up [T1] of the parent cohort and a cohort enrichment group [T1*]) and follow-up time point (between 2006–2010 [T2], Figure); mean follow-up time was 5.96 ± 0.88 years (range 3–10 years). Demographics, other than the expected increase in age, were similar between the baseline cohort and the population with data at follow-up. The clinic visits included a physical examination, including radiographs (hands, knees, hips, and lumbar spine) administered by trained study personnel. Baseline data were obtained from interviewer-administered questionnaires. The analysis, which followed STROBE guidelines [19] included demographic, clinical, and radiographic data for each participant at the initial evaluation and the outcome of falls determined at the follow-up visit. The Johnston County OA Project has been continuously approved by the Institutional Review Boards of the University of North Carolina at Chapel Hill and of the Centers for Disease Control and Prevention in Atlanta, GA.
Figure.
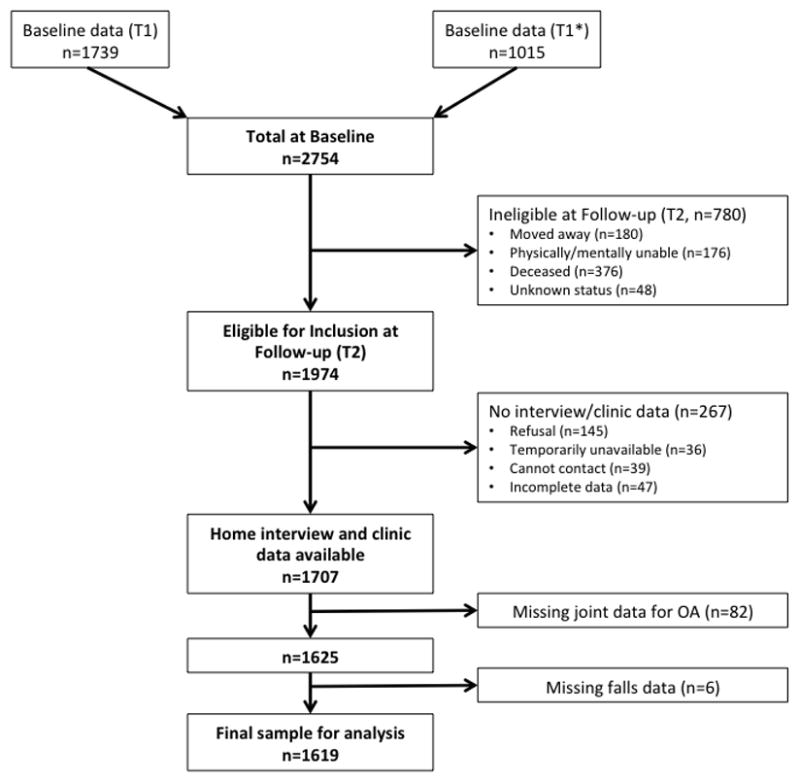
Sample size definition
Definition of Falls
A participant was considered to have a fall if he or she answered “yes” to the question “In the last 12 months, have you had any falls of any type?” If the participant answered yes, the question was followed by “how many?” in order to determine the number of falls the participant experienced in the last 12 months. The primary outcome was one or more falls, although a sensitivity analysis was additionally performed with the outcome defined as two more falls.
Symptomatic OA Definition
Symptomatic OA was assessed separately for right and left sides at each joint site (knee and/or hip) and defined for analysis as the presence of symptoms, including pain, aching, or stiffness on most days, and radiographic evidence of OA (defined below) in the same joint. A sensitivity analysis was performed categorizing symptomatic OA by joint-specific severity: no symptomatic OA, mild symptoms and Kellgren Lawrence (KL) grade ≥ 2, or moderate/severe symptoms and KL grade ≥ 2 at the knee and hip.
Radiographic OA Definition
Radiographs of the knees and hips were obtained on a single clinic visit and obtained using standard protocols. For knees, fixed flexion and weight-bearing posteroanterior radiographs, using the Synaflexer™device (CCBR-Synarc, San Francisco, CA), were read for KL grade [20]. Anteroposterior supine pelvis films were used to determine KL grade for hips. All films were read by a single experienced musculoskeletal radiologist (JBR) shown to have high intra- and inter-rater reliability (κ=0.89 and 0.86, respectively) [21]. Radiographic OA (rOA) was defined as KL grade ≥ 2 in any knee or hip joint. Replaced knees were considered as having OA if the participant reported OA as the reason for the replacement, or if rOA was present in the contralateral non-replaced knee. Replaced hips were categorized as OA only if the participant reported OA as the reason for the joint replacement, as hips more often than knees may undergo replacement for non-OA etiologies such as fracture or osteonecrosis. A sensitivity analysis was performed excluding those with joint replacement who may have improved pain and function after the procedure.
Covariates
Other covariates included age, gender, body mass index (BMI, kg/m2), a history of prior falls, current use of alcohol, tobacco, narcotic medications, bisphosphonate medications, sleep aids, or vitamin D supplement use, a history of lung problems (defined as patient report of chronic bronchitis, emphysema or other chronic respiratory conditions), neurologic disease (defined as patient report of multiple sclerosis, stroke, epileptic seizures or convulsions, paralysis of any kind, or Alzheimer’s disease), depressive symptoms (using the Center for Epidemiologic Studies Depression scale (CES-D), patient reported diabetes, blindness, cancer and low back symptoms.
Statistical Analysis
Descriptive statistics were calculated for the whole sample and separately for people reporting, and not reporting, a fall at the follow-up time point. Measures of central location and dispersion were computed for continuous data. Frequency distributions were determined for categorical variables. Missing data were assumed to be missing at random.
Logistic regression was used to determine the risk for future falls resulting from symptomatic knee and/or hip OA. Unadjusted odds ratios and adjusted odds ratios were determined controlling for baseline risk factors, including age, BMI, gender, race, and prior falls. Age and BMI were used in these models as continuous variables while gender and race were categorical variables. Models for each of our two exposures of most interest, symptomatic hip and/or knee OA, and multiple lower extremity joint OA, were explored. All potential covariates (listed above) were included initially, then dropped from the model if the p-values were >0.1. Covariates that were dropped from the models included: current smoking and alcohol use, the use of sleep and bisphosphonate medications, vitamin D supplement use, a history of diabetes, blindness, cancer, and low back symptoms.
Interactions between symptomatic knee and hip OA and each of the remaining covariates were tested together. In models with significant interactions (p-values <0.1), appropriate sub-groups were examined, and point estimates and 95% confidence intervals were calculated separately for each sub-group. All statistical computations were performed using SAS Version 9.3 software (SAS Institute, Cary, NC).
RESULTS
There were 1,707 people who participated in the follow up visit. Of these, 82 participants did not have the necessary data to evaluate for symptomatic OA at baseline, and an additional 6 participants did not have data regarding a history of falls at both time points. This resulted in a total of 1,619 participants included in this study (Figure 1). Table 1 shows the baseline characteristics of the cohort overall and by fall status at follow-up. At baseline, the mean age was 62 and the mean BMI was 31. Of these participants, approximately 1/3 were African American and 1/3 were men. Approximately 1/5 of participants reported at least 1 fall within 12 months of the baseline time point, and over 1/4 of participants reported the primary outcome of at least 1 fall during the 12 months prior to the follow up visit. More people fulfilled criteria for symptomatic knee OA than symptomatic hip OA. Self-reported comorbidities were frequently seen, while a small minority of participants reported taking narcotic or bisphosphonate medications (Table 1).
Table 1.
Baseline Characteristics of the sample (n=1619)
| Characteristic | n/N (%) or mean (range) | Those with fall at follow up (n=425) | Those without fall at follow up (n=1194) | p-value |
|---|---|---|---|---|
| Caucasian: | 1127/1,619 (69.6) | 319 (75.1) | 808 (67.7) | 0.005 |
| Men: | 529/1,619 (32.7) | 113 (26.6) | 416 (34.8) | 0.002 |
| Mean Age: years (range) | 62 (45–89) | 64 (45–89) | 62 (45–85) | 0.001 |
| Mean BMI (kg/m2): (range) | 30.8 (17.1–65.8) | 31.2 (18.8–54.0) | 30.6 (17.1–65.8) | 0.108 |
| Current Smokers: | 223/1,619 (13.8) | 49 (11.5) | 174 (14.6) | 0.118 |
| Current Alcohol use: | 319/1,619 (19.7) | 71 (16.7) | 248 (20.8) | 0.070 |
| History of Narcotic use1: | 50/1,613 (3.1) | 23 (5.5) | 27 (2.3) | 0.001 |
| History of Sleep Aids: | 607/1,611 (37.7) | 178 (42.1) | 429 (36.1) | 0.030 |
| History of Bisphosphonate use: | 96/1,614 (6.0) | 29 (6.9) | 67 (5.6) | 0.358 |
| History of Vitamin D use: | 373/1,561 (23.9) | 105 (25.9) | 268 (23.2) | 0.280 |
| Reported Lung Problems2: | 311/1,619 (19.2) | 109 (25.7) | 202 (16.9) | <.0001 |
| Reported Diabetes: | 258/1,619 (15.9) | 79 (18.6) | 179 (15.0) | 0.082 |
| Reported Neurologic Problems3: | 122/1,619 (7.5) | 47 (11.1) | 75 (6.3) | 0.002 |
| Reported Blindness: | 67/1,619 (4.1) | 24 (5.7) | 43 (3.6) | 0.069 |
| Reported history of Cancer: | 175/1,618 (10.8) | 45 (10.6) | 130 (10.9) | 0.876 |
| Median CES-D4 : (range) | 6.06 (0–53) | 7.21 (0–53) | 5.66 (0–46) | 0.001 |
| Falls at baseline: | 352/1,616 (21.8) | 146 (34.4) | 206 (17.3) | <.0001 |
| Symptomatic Knee OA: | 321/1590 (20.2) | 111 (26.5) | 210 (17.9) | 0.001 |
| Symptomatic Hip OA: | 196/1518 (12.9) | 78 (19.7) | 118 (10.5) | <.0001 |
| 1 Symptomatic Lower Extremity Joint | 218/1498 (14.5) | 72/392 (18.4) | 146/1106 (13.2) | <.0001 |
| 2 Symptomatic Lower Extremity Joints | 166/1498 (11.1) | 63/392 (16.1) | 103/1106 (9.3) | |
| 3–4 Symptomatic Lower Extremity Joints | 45/1498 (3.0) | 19/392 (4.9) | 26/1106 (2.4) | |
| Falls at follow-up time point: | 425 (26.3) | - | - |
Defined as self-reported narcotic use for > 2 weeks (dichotomous)
Includes patient report of chronic bronchitis, emphysema or other chronic lung trouble (dichotomous)
Includes patient report of multiple sclerosis, stroke, epileptic seizures or convulsions, paralysis of any kind, or Alzheimer’s disease
Center for Epidemiologic Studies Depression scale (continuous [0–60], higher scores=more depressive symptoms)
Compared with those not reporting a fall, individuals reporting a fall at follow up were more likely Caucasian, older, and female; those with a fall also more frequently reported use of narcotic medications, sleep aids, a history of lung or neurologic problems, history of prior falls, and scored higher on the CES-D. Symptomatic knee and hip OA, and multiple joint involvement, were more frequent among those reporting a fall at follow up compared to those without a fall (Table 1).
As shown in Table 2, the odds of falls increased with an increasing number of knee and/or hip joints with symptomatic OA. Compared with participants without symptomatic hip or knee OA, individuals with symptomatic OA in 1 lower limb joint had 53% higher odds for future falls, those with symptomatic OA in 2 joints had 74% higher odds, and those with symptomatic OA in 3–4 joints had 85% higher odds for future falls (Table 2). Caucasians, females, older participants, those who had had a previous fall, a history of lung problems, neurologic problems and those who reported use of narcotic medications also had greater odds for future falls.
Table 2.
Associations (Adjusted Odds Ratios and 95% Confidence Intervals) between Number of Lower Extremity Joints with Symptomatic OA, Covariates, and Future Falls
| Characteristic | Adjusted Odds Ratio (95% CI) |
|---|---|
| No Symptomatic OA* Joints | 1.00 |
| 1 Symptomatic OA Joint | 1.53 (1.10, 2.14) |
| 2 Symptomatic OA Joints | 1.74 (1.19, 2.53) |
| 3–4 Symptomatic OA Joints | 1.85 (0.96, 3.55) |
| Caucasian | 1.39 (1.05, 1.84) |
| Female | 1.36 (1.04, 1.77) |
| Age (per year) | 1.02 (1.01, 1.04) |
| BMI (per kg/m2) | 1.01 (0.99, 1.03) |
| Falls at baseline | 2.37 (1.80, 3.12) |
| Lung Problems | 1.50 (1.12, 2.01) |
| Neurologic Problems | 1.63 (1.07, 2.49) |
| Narcotic Use | 1.88 (0.99, 3.57) |
Symptomatic OA is defined as radiographic evidence of OA and pain, aching, or stiffness in the same joint.
As shown in Table 3, when included in the same model, symptomatic knee OA was associated with 39% higher odds, while symptomatic hip OA was associated with 60% higher odds of future falls, compared with participants without symptomatic lower extremity OA (Table 3). There was no significant interaction between these two variables (p=0.33).
Table 3.
Associations (Adjusted Odds Ratios and 95% Confidence Intervals) between Symptomatic Knee and Hip OA, Covariates, and Future Falls
| Characteristic | Adjusted Odds Ratio (95% CI) |
|---|---|
| Symptomatic Knee OA* | 1.39 (1.02, 1.88) |
| Symptomatic Hip OA* | 1.60 (1.14, 2.24) |
| Caucasian | 1.38 (1.04, 1.83) |
| Female | 1.33 (1.02, 1.74) |
| Age (per year) | 1.03 (1.01, 1.04) |
| BMI (per kg/m2) | 1.01 (0.99, 1.03) |
| Falls at baseline | 2.35 (1.80, 3.08) |
| Lung Problems | 1.50 (1.12, 2.01) |
| Neurologic Problems | 1.61 (1.06, 2.46) |
| Narcotic Use | 1.91 (1.01, 3.63) |
Symptomatic OA is defined as radiographic evidence of OA and pain, aching, or stiffness in the same joint.
The results from sensitivity analyses, 1) with the outcome defined as ≥ 2 falls 2) excluding those with knee (n=39) or hip (n=13) replacement and 3) considering symptom severity for symptomatic OA were similar to the reported results (data not presented).
DISCUSSION
This is the first study to demonstrate that increasing lower extremity joint symptomatic OA burden increases the odds of future falls, independent of known risk factors such as age, gender, race, and prior history of falls. It also confirms that symptomatic knee and hip OA are associated with greater odds of future falls. Therefore, individuals with symptomatic OA are at greater risk of falls, and are a group that may benefit from focused falls prevention programs.
The greater odds of falls associated with an increasing number of symptomatic OA joints in the current study is novel, but consistent with prior work examining the role of widespread pain and multiple musculoskeletal disorders on falls. Women with widespread pain had greater than a 60% increased risk for falls compared to those with less pain [12]. These authors also found that patients with more OA had more widespread pain, which may be one contributing factor that leads to more falls [12]. Another group analyzed the role of chronic musculoskeletal diseases in a large population and found that the risk of falls increased with an increasing number of musculoskeletal diseases (including OA, low back pain, and rheumatoid arthritis) in a given individual [9]. Though their investigation included rheumatic conditions in addition to OA, these results help support the finding that people with more musculoskeletal pathology are at an increased risk for falls. We found that symptomatic hip OA was somewhat more strongly associated with falls compared with knee OA (Table 3), although both were independently associated with the outcome. The model was initially adjusted for low back symptoms to account for any overlap in self-reported “hip” and “low back” symptoms by participants, but the presence of low back symptoms was not associated with falls and was dropped from the model, indicating that the association is primarily with hip disease.
Our results showing that symptomatic knee and hip OA increase the risk for falls are consistent with prior work [2, 5, 9, 14, 17]. However, our study is unique as we were able to use symptoms and radiographic evidence together to better phenotype OA, while most prior studies used patient-reported arthritis or OA, and symptoms or radiographic evidence of arthritis as individual risk factors. In clinical practice, symptoms and radiographic evidence are often used together in diagnosing and evaluating patients with OA. Using musculoskeletal symptoms alone as an explanatory variable does not allow determination of whether symptoms are secondary to OA or from other etiologies, such as chronic pain syndromes, generalized muscle weakness, inflammatory arthritis, or other underlying musculoskeletal pathology. This makes it difficult to identify any potential underlying modifiable risk for falls. Radiographic definitions alone are also not sufficient, as it is well documented that radiographic OA and symptoms do not correlate perfectly [22]. We were also able to utilize longitudinal data from this cohort to better assess causality, and to include a large number of potentially relevant covariates.
The mechanism by which OA may increase the risk for falls is not entirely understood, and further work in this area is needed to understand how this risk can be modified. As shown in previous studies, people who report more joint pain have an increased risk of falls independent of radiographic presence and severity of OA [11, 12, 16, 17, 23, 24]. This suggests that the radiographic structural changes in OA are not the only factor affecting fall risk. It has been postulated that pain and musculoskeletal symptoms related to OA lead to decreased use of the affected limbs and joints, muscle weakness, postural imbalance, and poor functional performance, resulting in an increased risk of falls [6, 15]. This explanation would be consistent with our findings, as more joints with symptomatic OA may be associated with more cumulative pain, muscle weakness, and decreased functional status, leading to greater risk of falls.
Given the association between musculoskeletal symptoms and falls, pain control could be a potential approach to fall prevention. However, there is sparse evidence that pain medications and pain control in OA have actually been associated with decreased falls. One subgroup analysis based on an observational study involving people with OA showed that daily analgesic use was protective against falls [12]. It is also important to note that prior research has shown that increased narcotic pain prescriptions for treating OA in the elderly are associated with an increased risk for falls [25]. Our study did show a trend towards an association between narcotic use and falls; however, this was not statistically significant likely due to a small number of individuals reporting the use of narcotic medications. Since there is no strong evidence that pain medications help with fall prevention in OA, and may be associated with an increased risk, other modalities such as physical therapy should be considered. There is strong evidence supporting the use of physical therapy, exercise, and strengthening in treating OA-related pain and dysfunction [26–29]. Although research has shown that exercise can prevent falls in the general elderly population, this has not been explored adequately in individuals with OA [15].
This study has many strengths, including the large sample size, availability of detailed symptomatic and radiographic OA data, and detailed questionnaire data regarding other potential risk factors. It also differs from many prior studies exploring OA and falls because the cohort consisted of community-dwelling African American and white men and women with and without OA. The availability of data at more than one time point offers advantages with regard to consistency in measurement and examination of relationships among variables over time.
Limitations to this work include the definition of falls, which is open to subjective bias based on the participants understanding of the question “Have you had any falls of any type within the last 12 months?” This is a common problem in falls research, as there is not a commonly used definition of a “fall” and in most cases defining a “fall” is subject to the participants’ recollection of a fall, rather than having objective evidence of a fall. The question did not include severity of falls, and any additional falls outside of the 12-month window would not have been captured. Self-reported falls data generally agree with prospective calendar-based recording of falls, although under-reporting can be an issue, and self-reported injuries suffered due to falls may be less reliable [30]. There was a relatively small number of participants who had multi-joint symptomatic OA, in particular 3–4 involved joints. This resulted in wider confidence intervals and a lack of statistically significant results in the association between falls and those with 3–4 symptomatic OA joints. However, there remained a trend toward an association between increased number of OA joints and increased risk for falls. The non-OA covariates were self-reported, and it is possible that individuals with a chronic illness such as OA may be more likely to report comorbid conditions than those without. Additionally, as in any observational study, unmeasured confounders (such as diabetic neuropathy) could be important contributors to the outcome and may have been missed.
Conclusions
Individuals with multi-joint lower extremity symptomatic OA, and those with symptomatic hip or knee OA, are at an increased risk for falls independent of known risk factors. This is the first study examining the direct relationship between multi-joint lower extremity OA and the risk for falls. These results suggest that when designing future interventions aimed at enhancing fall prevention, investigators should not ignore the impact of lower limb OA, particularly hip OA and multi-joint lower extremity OA.
Significance and Innovations.
Falls are a leading cause of morbidity and mortality in the adult population.
Osteoarthritis (OA) is thought to be a risk factor for falls; however, many previous studies have had conflicting results and have been limited due to study design.
To date, no studies have explored the role and cumulative effects of multi-joint lower extremity OA on the risk of falls.
Our study helps to clarify the increased risk of falls associated with knee and hip OA as well as multi-joint lower limb OA.
Acknowledgments
Support was provided in part by NCATS/NIH KL2TR000084 and Arthritis Foundation Postdoctoral Fellowship Award (Golightly), NIAMS K23 AR061406 (Nelson), CDC/Association of Schools of Public Health S043 and S3486 and NIAMS 5-P60-AR30701 (Jordan, Renner).
We would like to thank the staff and participants of the Johnston County Osteoarthritis Project, without whom this work would not have been possible. In addition, we would like to acknowledge the following for their support: NCATS/NIH KL2TR000084 and Arthritis Foundation Postdoctoral Fellowship Award (Golightly), NIAMS K23 AR061406 (Nelson), CDC/Association of Schools of Public Health S043 and S3486 and NIAMS 5-P60-AR30701 (Jordan, Renner).
Footnotes
The authors have no conflicts of interest relevant to this work.
References
- 1.Center for Disease C, Prevention. Cost of Fall Injury in Older Persons in the United States, 2005. 2011 [cited 2013 12/27]; Available from: http://www.cdc.gov/homeandrecreationalsafety/falls/data/cost-estimates.html.
- 2.Cruz D, Ribeiro L, Vieira M, Teixeia M, Bastos R, Leite I. Prevalence of falls and associated factors in elderly individuals. Revista de Saude Publica. 2012;46(1):138. doi: 10.1590/s0034-89102011005000087. [DOI] [PubMed] [Google Scholar]
- 3.Cummings-Vaughn L, Gammack J. Falls, Osteoporosis and Hip Fractures. Med Clin N Am. 2011;95:495. doi: 10.1016/j.mcna.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Rubenstein L. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(s2):37. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 5.Arden NK, Crozier S, Smith H, Anderson F, Edwards C, Raphael H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis & Rheumatism. 2006;55(4):610. doi: 10.1002/art.22088. [DOI] [PubMed] [Google Scholar]
- 6.Hoops M, Rosenblatt N, Hurt C, Crenshaw J, Grabiner M. Does lower extremity osteoarthritis exacerbate risk factors for falls in older adults? Women’s Health. 2012;8:685. doi: 10.2217/whe.12.53. [DOI] [PubMed] [Google Scholar]
- 7.Tinetti ME. Preventing falls in elderly persons. The New Englan Journal of Medicine. 2003;348(1):42. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 8.Hartholt KA, Stevens JA, Polinder S, van der Cammen TJ, Patka P. Increase in fall-related hospitalizations in the United States, 2001–2008. Trauma. 2011;71(1):255. doi: 10.1097/TA.0b013e31821c36e7. [DOI] [PubMed] [Google Scholar]
- 9.Lee W, Kong K, Park H. Effect of preexisting musculoskeletal diseases on the 1-year incidence of fall-related injuries. Journal of Preventive Medicine & Public Health. 2012;45:283. doi: 10.3961/jpmph.2012.45.5.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tilling L, Darawil K, Britton M. Falls as a complication of diabetes mellitus in older people. Journal of Diabetes and its Complications. 2006;20:158. doi: 10.1016/j.jdiacomp.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Foley S, Lord S, Srikanth V, Cooley H, Jones G. Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian Older Adult Cohort study. Osteoarthritis and Cartilage. 2006;14:533. doi: 10.1016/j.joca.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Leveille S, Bean J, Bandeen-Roche K, Jones R, Hochberg M, Guralnik J. Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc. 2002;50:671. doi: 10.1046/j.1532-5415.2002.50161.x. [DOI] [PubMed] [Google Scholar]
- 13.Preito-Alhambra D, Nogues X, Javaid MK, Wyman A, Arden NK, Azagra R, et al. An increased rate of falling leads to a rise in fracture risk in postmenopausal women with self-reported osteoarthritis: a prospective multinational cohort study (GLOW) Annals of Rheumatic Diseases. 2013;72(6):911. doi: 10.1136/annrheumdis-2012-201451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barbour KE, Stevens JA, Helmick CG, Luo YH, Murphy LB, Hootman JM, et al. Falls and fall injuries among adults with arthritis--United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(17):379–83. [PMC free article] [PubMed] [Google Scholar]
- 15.Ng CT, Tan MP. Osteoarthritis and falls in the older person. Age Ageing. 2013;0:1. doi: 10.1093/ageing/aft070. [DOI] [PubMed] [Google Scholar]
- 16.Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Nakamura K, et al. Prevalence of falls and the association with knee osteoarthritis and lumbar spondylosis as well as knee and lower back pain in Japanese men and women. Arthritis Care Res (Hoboken) 2011;63:1425. doi: 10.1002/acr.20562. [DOI] [PubMed] [Google Scholar]
- 17.Arden N, Nevitt M, Lane N, Gore L, Hochberg M, Scott J, et al. Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Arthritis Rheum. 1999;42(7):1378. doi: 10.1002/1529-0131(199907)42:7<1378::AID-ANR11>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 18.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in african americans and caucasians: The Johnston County Osteoarthritis Project. Journal of Rheumatology Journal of Rheumatology. 2007;34:172. [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 20.Kellgren JH, Lawrence JS. Atlas of standard radiographs: The epidemiology of chronic rheumatism. 2. 1963. [Google Scholar]
- 21.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care and Research. 1995;8:242. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 22.Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27(6):1513–7. [PubMed] [Google Scholar]
- 23.Leveille SG, Jones RN, Keily DK, Hausdorff JM, Shmerling RH, Guralnik JM, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. Journal of American Medical Association. 2009;302:2214. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muraki S, Akune T, Ishimoto Y, Nagata K, Yoshida M, Tanaka S, et al. Risk factors for falls in a longitudinal population-based cohort study of Japanese men and women: The ROAD Study. Bone. 2013;52:516. doi: 10.1016/j.bone.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 25.Rolita L, Spegman A, Tang X, Arden NK. Greater number of narcotic analgesic prescriptions for osteoarthritis is associated with falls and fractures in elderly adults. J Am Geriatr Soc. 2013;61:335. doi: 10.1111/jgs.12148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis AM, MacKay C. Osteoarthritis year in review: outcome of rehabilitation. Osteoarthritis and Cartilage. 2013;21:1414. doi: 10.1016/j.joca.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 27.Stemberger R, Kerschan-Schindl K. Osteoarthritis: physical medicine and rehabilitation - nonpharmacological management. Wiener Medizinische Wochenschrift. 2013;163:228. doi: 10.1007/s10354-013-0181-9. [DOI] [PubMed] [Google Scholar]
- 28.Uthman OA, van der Windt DA, Jordan JL, Dziedzic KS, Healey EL, Peat GM, et al. Exercise for lower limb osteoarthritis: systemic review incorporating trial sequential analysis and network meta-analysis. British medical journal. 2013;347:1. doi: 10.1136/bmj.f5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bennell KL, Hinman RS. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport. 2011;14(1):4–9. doi: 10.1016/j.jsams.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 30.Mackenzie L, Byles J, D’Este C. Validation of self-reported fall events in intervention studies. Clin Rehabil. 2006;20(4):331–9. doi: 10.1191/0269215506cr947oa. [DOI] [PubMed] [Google Scholar]


