Abstract
Recent theories have proposed a metastructure that organizes related mental disorders into broad dimensions of psychopathology (i.e., internalizing and externalizing dimensions). Prevalence rates of most mental disorders, when examined independently, are substantially lower in older than in younger adults, which may affect this metastructure. Within a nationally representative sample, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; N = 43,093), we developed a dimensional liability model of common psychiatric disorders to clarify whether aging affects specific disorders or general dimensions of psychopathology. Significant age differences existed across age groups (18-24, 25-34, 35-44, 45-54, 55-64, 65-75 and 75+), such that older adults showed lower prevalence rates of most disorders compared to younger adults. We next investigated patterns of disorder comorbidity for past-year psychiatric disorders and found that a distress-fear-externalizing liability model fit the data well. This model was age-group invariant and indicated that that the observed lower prevalence of mental disorders with advancing age originates from lower average means on externalizing and internalizing liability dimensions. This unifying dimensional liability model of age and mental disorder comorbidity can help inform the role of aging on mental disorder prevalence for research and intervention efforts, and service planning for the impending crisis in geriatric mental health.
Keywords: age differences, age invariance, older adults, elderly, psychiatric disorders, mental disorders, comorbidity, internalizing-externalizing
Introduction
The rapid growth of the geriatric population in the U.S calls for a better understanding of lifespan psychopathology and how prevalence rates of mental disorders progress into late adulthood (Jeste et al. , 1999). Because mental disorders often co-occur (Beekman et al., 1998; Kessler et al., 2005b; Lenze et al., 2000; Schoevers et al., 2003; Manetti et al., 2013; Schuster et al., 2013b), recent theories have proposed a metastructure of psychiatric diagnoses that organizes disorders into broad dimensions of psychopathology (i.e., internalizing and externalizing dimensions) (Eaton, 2015). This dimensional internalizing-externalizing model has been well established in the general population (Blanco et al., 2013; Insel et al., 2010; Kendler et al., 2003; Kessler et al., 2011; Kotov et al., 2011; Krueger et al., 2011; Krueger and Markon, 2006; Krueger et al., 2003; Krueger, 1999; Krueger et al., 1998; Vollebergh et al., 2001) and has been shown to be invariant across numerous nationalities and cultures (Krueger et al., 2003), race/ethnicity (Eaton et al., 2013), gender (Eaton et al., 2012) and sexual orientation (Eaton, 2014), but it has never been examined specifically in geriatric populations.
When examined independently, the prevalence rates of most common psychiatric disorders are substantially lower in older than in younger adults (Donnellan and Lucas, 2008; Gum et al., 2009; Hasin et al., 2005; Hoertel et al., 2013; Jorm, 2000; Kessler et al., 2005a; Manetti et al., 2013; Schuster et al., 2013a; Seitz et al., 2010; Sunderland et al., 2014; Weissman et al., 1985), which may affect the structure of comorbidity. Three previous studies (Buchan et al., 2014; Eaton et al., 2011; Sunderland et al., 2013) have suggested that the structure of comorbidity may hold in individuals as they age. However, their conclusions are mainly based on models of a limited number of psychiatric disorders (i.e., internalizing disorders). In addition, since dimensions underlying psychopathology (i.e., internalizing and externalizing dimensions) are positively correlated (Blanco et al., 2013), it remains unclear whether age differences in prevalence rates of mental disorders are due to a decrease in the prevalence of specific disorders (and thus to a different metastructure of mental disorders in older adults) or to a decrease in the predisposition to one or more broad dimensions of psychopathology, which would be the case if this structure holds across age groups.
Testing these competing hypotheses may help explain variations in psychiatric disorders prevalence across the lifespan and would inform the utility of the dimensional liability model to frame key aspects of psychiatric nosology in older age groups (Andrews et al., 2009; Blanco et al., 2013). If the latent structure of common psychiatric disorders is not invariant between younger and older adults, the liability model of internalizing and externalizing dimensions would not apply to older adults, suggesting that the mechanisms underlying predisposition to psychopathology might vary with age. By contrast, if invariance were found, it would indicate that age group differences in latent psychopathological liabilities account for the observed age group differences in prevalence rates of psychiatric disorders. It might also be possible to develop a dimensional liability model of age and disorder comorbidity to inform the role of aging in mental disorder prevalence for research and intervention efforts (Eaton et al., 2012; Eaton et al., 2011).
This report used a nationally representative sample of 43,093 individuals to examine the age invariance of a liability model of common psychiatric disorders in the US. We a priori divided adult participants into seven age groups, i.e., 18-24, 25-34, 35-44, 45-54, 55-64, 65-75 and >75 years. First, we sought to determine the latent comorbidity structure of common psychiatric disorders in these seven age groups separately. Secondly, we tested whether the structure of psychopathology was similar across the seven age groups (i.e., age group invariant). Finally, if invariance were found, we sought to examine whether the lower predisposition to mental disorders among older adults would concern externalizing or internalizing dimensions or both dimensions.
Material and methods
Participants
This study utilized data from 43,093 individuals who participated in the first wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), conducted in 2001-2002. The design of the NESARC has been detailed elsewhere (Grant et al. , 2009; Grant et al., 2003). The first wave of NESARC was a representative sample of the civilian, non-institutionalized United States population, aged 18 and older. The overall survey response rate was 81%. Young adults, African Americans, and Hispanics were oversampled. Data were weighted at the individual and household levels in order to adjust for oversampling and nonresponse on demographic variables (e.g., age, race/ethnicity, sex, region, and place of residence) to be representative of the U.S. civilian population based on the 2000 census (Grant et al., 2009). The research protocol, including written informed consent procedures, received full human subjects review and approval from the U.S. Census bureau and the Office of Management and Budget.
Measures
Definition of age groups
To provide a finer-grained examination of the effects of age on the structure of psychiatric disorders that has been possible in previous national studies, we divided participants into seven age groups, i.e., 18-24, 25-34, 35-44, 45-54, 55-64, 65-75 and >75 years. The two later age groups offer the opportunity to detect a change of the metastructure of common psychiatric disorders that could occur later in life and would thus have been blurred by merging all participants older than 65 years of age (Reynolds et al., 2006). The five other age groups comprised participants 18 to 64 years of age. In the NESARC, participants aged 18-24 years (N=5199), 25-34 years (N=7759), 35-44 years (N=9090), 45-54 years (N=7625), 55-64 years (N=5215), 65-75 years (N=4685) and >75 years (N=3520) included, respectively, 13.0% (SE=0.3), 18.5% (SE=0.3), 21.2% (SE=0.3), 18.8% (SE=0.3), 12.3% (SE=0.2), 9.6% (SE=0.2) and 6.6% (SE=0.2) of the sample.
Assessments of DSM-IV mental disorders
Mental disorders were assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule, DSM-IV version (AUDADIS-IV), a structured diagnostic instrument administered by trained lay interviewers (Grant et al., 2009). Axis I diagnoses included nicotine dependence, alcohol dependence, dependence on drugs (i.e., cannabis, amphetamine, hallucinogen, cocaine, heroin, opioid and inhalant), major depressive episode, dysthymic disorder and anxiety disorders (panic disorder with and without agoraphobia, social anxiety disorder, specific phobia, and generalized anxiety disorder). For all Axis I disorders, diagnoses were made in the past 12 months. Antisocial personality disorder was assessed on a lifetime basis (Grant et al., 2009). The test-retest reliability and validity of AUDADIS-IV measures of past year DSM-IV psychiatric disorders and lifetime antisocial personality disorder range from good to excellent for substance use disorders and fair to good for other disorders (Canino et al., 1999; Chatterji et al., 1997; Grant et al., 2003; Grant et al., 1995; Hasin et al., 1997). Further, the AUDADIS-IV includes assessment of clinically significant distress and impairment after the syndrome is fully characterized (Hasin et al., 2005).
Statistical Analyses
Weighted percentages and their corresponding standard errors were calculated to provide descriptive information about the prevalence of past year psychiatric disorders and lifetime antisocial personality disorder across the 7 age groups. We performed a set of bivariate logistic regressions to yield odds ratios (ORs) and 95% confidence intervals (CIs) characterizing the association between disorders and the 7 age groups (Le Strat and Hoertel, 2011). Odds ratios used younger age group (participants aged 18 to 24 years) as the reference comparison group.
Next, we used confirmatory factor analysis (CFA) to identify the latent structure underlying individual mental disorders assessed at Wave 1. We built upon the CFA model fit in prior work (Insel et al., 2010; Kendler et al., 2003; Kessler et al., 2011; Kotov et al., 2011; Krueger et al., 2011; Krueger and Markon, 2006; Krueger et al., 2003; Krueger, 1999; Krueger et al., 1998; Vollebergh et al., 2001), including on these data (Eaton et al., 2012; Blanco et al., 2013; Magidson et al., 2014), which generated two broad dimensions of psychopathology: (1) an internalizing dimension defined by two latent factors, i.e., distress (measured by major depression, dysthymia and generalized anxiety disorder) and fear (measured by panic disorder with and without agoraphobia, social anxiety disorder and specific phobia) and (2) an externalizing dimension measured by nicotine dependence, alcohol dependence, drug dependence and antisocial personality disorder (Figure 1). We examined measures of goodness-of-fit, including the comparative fit index (CFI), the Tucker–Lewis index (TLI), and the root mean squared error of approximation (RMSEA). CFI and TLI values greater than 0.95 and values of RMSEA less than 0.06 are commonly used to indicate good model fit and were used as cut-offs (Hu and Bentler, 1999).
Figure 1. Age groups invariant (constrained) model of the latent structure of psychiatric disorders.
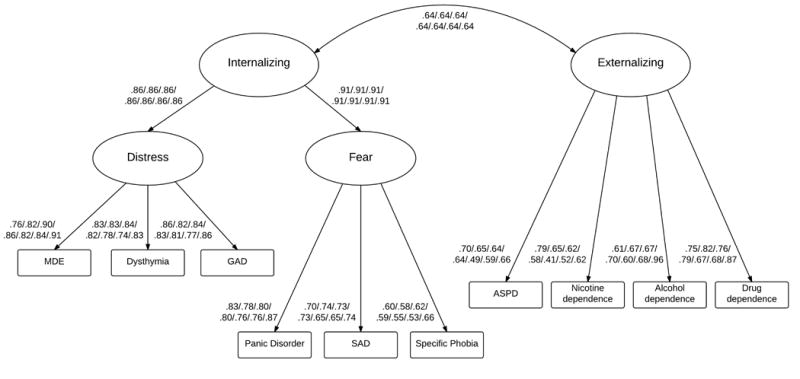
Ellipses are used to denote latent constructs; rectangles are used to denote the observed variables measuring these constructs.
All factor loadings and covariance measures are standardized and significant (two-sided p < .005).
Values separated by slashes are respectively for participants 18-24, 25-34, 35-44, 45-54, 55-64, 65-75 and >75 years of age. Values differ slightly across age groups due to standardization.
All disorders were assessed on a 12-month basis except for antisocial personality disorder which was assessed on a lifetime basis.
MDE: major depressive episode, GAD: generalized anxiety disorder, SAD: social anxiety disorder, ASPD: antisocial personality disorder.
Finally, we used a multiple-group structural equation model and examined whether the measurement parameters were invariant across age groups. Tests of invariance for indicators such as categorical diagnoses require methods appropriate for modeling categorical variables (Millsap and Meredith, 2007). In this approach, factor loadings and thresholds are constrained to equality or freed, in tandem, across the seven age groups. In our first model (the “unconstrained model”), loadings and thresholds were free across groups, factor means were set to zero in all groups, and scaling factors were fixed to one in all groups. In the second model (the “constrained model”), loadings and thresholds were constrained to equality across age groups, factor means were set to zero in the youngest age group and were free in all older age groups, and scaling factors were fixed to one in the youngest age group and were free in all older age groups.
Based on simulations, Cheung and Rensvold (2002) proposed a CFI difference critical value of .01 be used to test whether the addition of constraints leads to notably worse model fit in factorial invariance studies. More parsimonious models use fewer freely estimated parameters. In model comparisons, we defined the optimal model by means of the best fit (CFI, TLI, and RMSEA), model parsimony (number of free parameters), CFI critical difference of .01 and interpretability of the factors.
Standardized estimates indicate how many standard deviations higher (or lower) the mean of the latent variable underlying the binary outcome are expected to be for each increase in an additional unit of that latent factor while adjusting for all other factors. To avoid including associations that could be significant due to multiple testing or the large sample size, we decided a priori to evaluate statistical significance using a two-sided design with alpha set at 0.005 (Godfrey, 1985).
All analyses were conducted in Mplus Version 7.2 (Muthén and Muthén, 1998) to account for the NESARC's complex design. The default estimator for the analysis was the variance-adjusted weighted least squares (WLSMV), a robust estimator appropriate for dichotomous observed variables such as the ones used in this study (Muthén and Muthén, 1998).
Results
Prevalence rates of past year psychiatric disorders and lifetime antisocial personality disorder across age groups
Compared to the youngest age group, major depressive episode, alcohol dependence and drug dependence were significantly less prevalent in all of the older age groups. Prevalence rates of panic disorder, social anxiety disorder and specific phobia were significantly lower among participants older than 65 of age than among those aged 18-24 years. Antisocial personality disorder, nicotine dependence and generalized anxiety disorder were significantly less prevalent respectively in participants older than 35 years, 45 years and 75 years than in those aged 18-24 years. There was no significant difference in prevalence of dysthymia in older age groups compared to the youngest group (Tables 1 and 2).
Table 1. Prevalence rates of past-year common psychiatric disorders and lifetime antisocial personality disorder across age groups.
| Mental Disorders | 18-24y (N=5199) |
25-34y (N=7759 |
35-44y (N=9090) |
45-54y (N=7625) |
55-64y (N=5215) |
65-75y (N=4685) |
>75y (N=3520) |
|---|---|---|---|---|---|---|---|
| % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | |
| MDE | 10.9 (0.6) | 8.1 (0.4) | 7.1 (0.4) | 8.1 (0.4) | 5.3 (0.3) | 2.9 (0.3) | 3.0 (0.4) |
| Dysthymia | 1.7 (0.2) | 1.7 (0.2) | 2.3 (0.2) | 2.2 (0.2) | 1.6 (0.2) | 1.2 (0.2) | 1.3 (0.3) |
| GAD | 1.8 (0.2) | 2.6 (0.2) | 2.5 (0.2) | 2.6 (0.2) | 1.4 (0.2) | 1.1 (0.2) | 0.9 (0.2) |
| Panic disorder | 2.0 (0.3) | 2.6 (0.2) | 2.6 (0.2) | 2.7 (0.2) | 1.6 (0.2) | 0.9 (0.1) | 0.8 (0.2) |
| SAD | 3.4 (0.3) | 2.6 (0.2) | 3.3 (0.3) | 3.0 (0.3) | 2.6 (0.3) | 1.7 (0.2) | 1.4 (0.2) |
| Specific phobia | 8.1 (0.5) | 7.9 (0.4) | 7.6 (0.4) | 7.9 (0.5) | 6.6 (0.4) | 5.2 (0.4) | 3.5 (0.4) |
| Alcohol dependence | 11.7 (0.6) | 4.9 (0.3) | 3.6 (0.3) | 2.5 (0.2) | 0.9 (0.1) | 0.4 (0.1) | 0.1 (0.1) |
| Drug dependence | 2.9 (0.3) | 0.9 (0.2) | 0.7 (0.1) | 0.4 (0.1) | 0.1 (0.1) | 0.1 (0.1) | 0.1 (0.1) |
| Nicotine dependence | 17.2 (0.7) | 15.3 (0.7) | 14.7 (0.7) | 13.9 (0.6) | 10.6 (0.6) | 5.4 (0.4) | 2.0 (0.3) |
| Antisocial PD | 6.7 (0.4) | 5.4 (0.4) | 3.7 (0.3) | 3.2 (0.3) | 2.4 (0.3) | 0.8 (0.2) | 0.3 (0.1) |
Abbreviations: MDE, major depressive episode; GAD, generalized anxiety disorder; SAD, social anxiety disorder; PD, personality disorder; SE, standard error.
Percentages are weighted to account for sampling biases.
All disorders were assessed on a 12-month basis except for antisocial personality disorder which was assessed on a lifetime basis.
Table 2. Comparing the prevalence rates of past-year common psychiatric disorders and lifetime antisocial personality disorder across age groups.
| Mental Disorders | 25-34y Vs. 18-24y |
35-44y Vs. 18-24y |
45-54y Vs. 18-24y |
55-64y Vs. 18-24y |
65-75y Vs. 18-24y |
>75y Vs. 18-24y |
|---|---|---|---|---|---|---|
| OR [95%CI] | OR [95%CI] | OR [95%C] | OR [95%C]] | OR [95%CI] | OR [95%CI] | |
| MDE | 0.71 [0.62-0.82]**** | 0.62 [0.54-0.72]**** | 0.71 [0.61-0.83]**** | 0.46 [0.39-0.54]**** | 0.24 [0.19-0.31]**** | 0.25 [0.19-0.35]**** |
| Dysthymia | 1.00 [0.71-1.40] | 1.30 [0.97-1.74] | 1.27 [0.94-1.71] | 0.92 [0.67-1.28] | 0.65 [0.44-0.97]* | 0.71 [0.42-1.21] |
| GAD | 1.47 [1.13-1.91]** | 1.41 [1.05-1.90]* | 1.50 [1.12-2.02]** | 0.79 [0.56-1.12] | 0.62 [0.43-0.89]* | 0.50 [0.31-0.81]*** |
| Panic disorder | 1.29 [0.93-1.79] | 1.30 [0.95-1.77] | 1.37 [1.01-1.84]* | 0.79 [0.53-1.18] | 0.43 [0.28-0.65]**** | 0.38 [0.21-0.70]**** |
| SAD | 0.76 [0.58-0.99]* | 0.94 [0.74-1.20] | 0.86 [0.68-1.09] | 0.74 [0.56-0.97]* | 0.48 [0.35-0.65]**** | 0.40 [0.28-0.59]**** |
| Specific phobia | 0.97 [0.83-1.14] | 0.93 [0.80-1.08] | 0.98 [0.84-1.14] | 0.80 [0.68-0.95]* | 0.62 [0.51-0.76]**** | 0.42 [0.33-0.52]**** |
| Alcohol dependence | 0.39 [0.33-0.47]**** | 0.28 [0.23-0.33]**** | 0.20 [0.16-0.24]**** | 0.07 [0.05-0.10]**** | 0.03 [0.02-0.05]**** | 0.00 [0.00-0.02]**** |
| Drug dependence | 0.29 [0.18-0.46]**** | 0.23 [0.16-0.34]**** | 0.13 [0.08-0.23]**** | 0.04 [0.01-0.10]**** | 0.04 [0.02-0.09]**** | 0.02 [0.00-0.13]**** |
| Nicotine dependence | 0.87 [0.77-0.98]* | 0.83 [0.73-0.94]** | 0.78 [0.69-0.88]**** | 0.57 [0.49-0.66]**** | 0.28 [0.23-0.33]**** | 0.10 [0.07-0.13]**** |
| Antisocial PD | 0.80 [0.67-0.96]* | 0.54 [0.44-0.65]**** | 0.46 [0.37-0.57]**** | 0.35 [0.27-0.44]**** | 0.11 [0.07-0.18]**** | 0.05 [0.02-0.10]**** |
Abbreviations: MDE, major depressive episode; GAD, generalized anxiety disorder; SAD, social anxiety disorder; PD, personality disorder; OR, odds ratio, CI, confidence interval.
ORs are crude (d.f.=1) and were estimated using logistic regression.
Reference group comprises participants aged 18-24 years.
All disorders were assessed on a 12-month basis except for antisocial personality disorder which was assessed on a lifetime basis.
p<.001;
p<.005;
p<.01;
p<.05.
Values in bold are statistically significant (two-sided p<.005).
Structure of disorders
In CFAs (Table 3), guided by previous studies (Blanco et al., 2013; Magidson et al., 2014; Eaton et al., 2012; Insel et al., 2010; Kendler et al., 2003; Kessler et al., 2011; Kotov et al., 2011; Krueger et al., 2011; Krueger and Markon, 2006; Krueger et al., 2003; Krueger, 1999; Krueger et al., 1998; Vollebergh et al., 2001), we parameterized each diagnosis to load on only one of the dimensions of psychopathology. Internalizing and externalizing dimensions were allowed to correlate each other. The distress-fear-externalizing CFA model met statistical criteria for a good fit in the total sample and within each age group (Table 3).
Table 3. Model fit statistics.
| Model | CFI | TLI | RMSEA | # Free |
|---|---|---|---|---|
| Total Sample (N=43,093) | 0.985 | 0.979 | 0.012 | 23 |
| 18-24y (N=5199) | 0.984 | 0.978 | 0.014 | 23 |
| 25-34y (N= 7759) | 0.985 | 0.979 | 0.012 | 23 |
| 35-44y (N=9090) | 0.983 | 0.976 | 0.014 | 23 |
| 45-54y (N= 7625) | 0.984 | 0.977 | 0.012 | 23 |
| 55-64y (N= 5215) | 0.970 | 0.957 | 0.011 | 23 |
| 65-75y (N=4685) | 0.970 | 0.958 | 0.008 | 23 |
| >75y (N=3520) | 0.981 | 0.973 | 0.013 | 23 |
| Multi-group (7 age groups) | ||||
| Unconstrained model | 0.981 | 0.973 | 0.012 | 161 |
| Constrained model | 0.977 | 0.975 | 0.011 | 95 |
Total sample analyses modeled the seven age groups together. Multiple group analyses modeled the seven age groups simultaneously as seven separate groups.
Unconstrained models allowed each age group to have unique model parameters.
Constrained (invariant) models constrained factor loadings and thresholds to equality across age groups.
CFI: comparative fit index, TLI: Tucker-Lewis index, RMSEA: root mean squared error of approximation.
Free: number of freely estimated parameters.
Age groups invariance of the distress-fear-externalizing psychopathological structure
Because the distress-fear-externalizing model fit well in the seven age groups, we further examined whether the magnitude of measurement parameters were invariant across age groups. We fit the unconstrained and constrained models in the seven age groups simultaneously using a multiple-group CFA (Table 3). The constrained model had a better fit for TLI and RMSEA with greater parsimony than did the unconstrained model and the CFI critical difference of .01 was not exceeded. The constrained model is depicted in Figure 1. In addition to the general structure, factor loadings and thresholds for all diagnoses were not significantly different across the seven age groups. Thus, the structure of the 10 assessed disorders, including the relationships between them and the underlying latent dimension, can be considered age invariant.
Means standing on the internalizing and externalizing dimensions across age groups
Standardized means of the latent internalizing and externalizing factors were fixed to zero in the youngest age group and freely estimated in older age groups. Standardized means of the externalizing dimension were significantly lower in all older age groups compared to the youngest group, ranging from -.39 (SE=0.09) in participants aged 25-34 years to -2.00 (SE=0.23) in those older than age 75. The standardized mean of the internalizing dimension was significantly lower in participants older than 55 years compared to those aged 18-24 years, ranging from -.38 (SE=0.11) in participants aged 55-64 years to -.72 (SE=0.14) in those aged 65-75 years (Table 4). These standardized means can be interpreted as z-scores (e.g., individuals aged 18-24 years were approximately 0.72 standard deviations higher on past-year internalizing liability than those aged 65-75 years). Because of the complete factorial invariance, these results indicate that the observed lower prevalence of mental disorders with advancing age originates from lower average levels of the externalizing dimension in individuals aged 25-54 years and from lower average levels of both externalizing and internalizing dimensions in individuals older than 55 years compared to those aged 18-24 years.
Table 4. Comparing standard mean differences (SMD) in internalizing and externalizing dimensions.
| 25-34y vs. 18-24y |
35-44y vs. 18-24y |
45-54y vs. 18-24y |
55-64y vs. 18-24y |
65-75y vs. 18-24y |
>75y vs. 18-24y |
|
|---|---|---|---|---|---|---|
| SMD (SE) | SMD (SE) | SMD (SE) | SMD (SE) | SMD (SE) | SMD (SE) | |
| Internalizing | -0.05 (0.10) | 0.05 (0.10) | 0.03 (0.10) | -0.38 (0.11)**** | -0.72 (0.14)**** | -0.41 (0.23)**** |
| Externalizing | -0.39 (0.09)**** | -0.62 (0.10)**** | -0.74 (0.14)**** | -1.88 (0.32)**** | -1.93 (0.40)**** | -2.00 (0.23)*** |
Abbreviations: SMD, standard mean difference; SE, standard error.
Reference group comprises participants aged 18-24 years.
p<.001;
p<.005;
p<.01;
p<.05.
Values in bold are statistically significant (two-sided p<.005).
Discussion
In a large nationally representative sample, the underlying structure of 10 common mental disorders was well described by the distress-fear-externalizing structure in older adults. This structure was invariant across seven age groups. A lower predisposition to both internalizing and externalizing dimensions, as measured by lower scores on these latent variables, contributed to explain the observed lower prevalence of mental disorders in older adults.
The present study is the first, to our knowledge, to test age invariance in the internalizing-externalizing liability model of disorder comorbidity using a wide range of categorical DSM-IV disorders as indicators in seven age groups. Our results indicate that this model, well established for the general adult population (Blanco et al., 2013; Eaton et al., 2012; Insel et al., 2010; Kendler et al., 2003; Kessler et al., 2011; Kotov et al., 2011; Krueger et al., 2003; Krueger et al., 1998; Vollebergh et al., 2001), holds for the older population, and suggests that these dimensions of psychopathology remain invariant from early to late adulthood. These results also suggest that psychiatric disorders in older adults are not mere the consequence of aging, but rather reflect the continuity of shared psychological and biological processes underlying these broad psychopathological dimensions that remain active throughout adult life. From the biological perspective, older and younger adults have similar genetic risk profiles for depressive and anxiety disorders (Demirkan et al., 2011). There is also evidence of the general continuity across the lifespan of some adaptive defense mechanisms (e.g., sublimation or suppression) (Lenzenweger et al., 2004; Segal et al., 2007) and cultural representations and practices, which may contribute to the continuity of mechanisms underlying these broad dimensions. These findings suggest that intervention programs (Andrews et al., 2009; Galea et al., 2004) that target the global core processes of internalizing and externalizing dimensions would also apply to the older population. Furthermore, the percentage of persons in the US living in institutional settings increases with age from 1% (65-74 years) to 3% (75-84 years) to 11% (≥85) (American Association for Geriatric Psychiatry, 2008). The invariance of this structure of psychopathology across age groups found in this study underscores the need to anticipate the shortage of health care providers with geriatric expertise, and specifically health care providers with geriatric mental health expertise, that this demographic transition will induce.
While numerous previous studies have consistently demonstrated that psychiatric disorders are less common in the older population (Donnellan and Lucas, 2008; Gum et al., 2009; Hasin et al., 2005; Hoertel et al., 2013; Jorm, 2000; Kessler et al., 2005a; Manetti et al., 2013; Schuster et al., 2013a; Seitz et al., 2010; Sunderland et al., 2014; Weissman et al., 1985), our study demonstrates that the observed lower prevalence of mental disorders in this population originates from its decrease in average psychopathological load, as measured by lower scores on the internalizing and externalizing latent liability dimensions. Several factors may contribute to this decreased load. Neuroticism is strongly related to the latent internalizing dimension (Griffith et al., 2010). Because dimensions of psychopathology are correlated (Slade, 2007), lower levels of neuroticism may contribute to decrease latent propensities in the other dimensions to experience comorbid mental disorders in older adults. According to socioemotional selectivity theory (Blazer and Hybels, 2005), when constraints on time are perceived, as is often the case in old age, emotional regulation becomes a higher priority and emotional goals focused on regulation assume primacy (Charles, 2010). As individuals accumulate experiences during their lives, many may acquire a greater ability to maintain an attitude of serenity through stressful events. Furthermore, lower levels of neuroticism in older adults may be related to changes in the neural substrates of emotion (Williams et al., 2006). Prior research (Mather, 2012; Mather et al., 2004; Williams et al., 2006) suggests that the responsiveness of amygdalae decreases over time for negative but not for positive emotions. As they age, adults may thus start to pay less attention to negative than positive emotional stimuli, and become less likely to remember negative than positive emotional events.
Healthier lifestyles (including the absence of alcohol, nicotine and illicit drug consumption) and better protection from some social risks in older adults (Blazer and Hybels, 2005), cohort effects on sociodemographic and environmental characteristics (e.g., differential rate in exposure to stressful life events or use of drugs) (Keyes et al., 2011; Simon et al., 1995), premature mortality among individuals with mental disorders and period effects (Beekman et al., 1999; Bruce and Leaf, 1989; Hoertel et al., 2014; Kessler et al., 2010; Lemogne et al., 2013; Tsuang and Simpson, 1985) may also contribute to explain lower propensity to psychopathology among older adults. These findings suggest that prevention efforts that focus on age-related core psychological processes (such as neuroticism levels) are likely to be effective in multiple disorders. A better understanding of the causes of the lower predisposition to psychopathology in the elderly (e.g., shift in responsiveness to positive and negative emotional stimuli) may also lead to improving the prevention of mental disorders in younger adults. Since older adults tend to report lower rates of some stressful life events than younger adults (Blazer and Hybels, 2005), the interaction between dimensions of psychopathology and environmental stressors could be a particularly fruitful focus for future research on aging and mental disorders.
This study has several limitations. First of all, although diagnoses were obtained with a structured diagnostic instrument, they could have been subject to recall biases, particularly in older adults with cognitive impairment (Zahodne and Tremont, 2013). However, all disorders (except for antisocial personality disorder) were assessed on a 12-month time frame, limiting those biases. In addition, the prevalence rates found in this study are consistent with those of prior studies (Donnellan and Lucas, 2008; Gum et al., 2009; Hasin et al., 2005; Hoertel et al., 2013; Jorm, 2000; Kessler et al. 2005a; Manetti et al., 2013; Schuster et al. 2013a; Seitz et al., 2010; Sunderland et al., 2014; Weissman et al., 1985), including studies conducted among institutionalized individuals. Secondly, the lifetime assessment of antisocial personality disorder may have favored the invariance across age groups. However, measurement parameters, including correlations between latent factors, were invariant across age groups. Finally, diagnostic information was collected by extensively trained lay interviewers rather than clinicians. However, a fully structured instrument was used, which resulted in generally good diagnostic reliability levels for all diagnoses (Canino et al., 1999; Chatterji et al., 1997; Grant et al., 2003; Grant et al., 1995; Hasin et al., 1997).
Despite these limitations, we found that a internalizing-externalizing dimension liability model of mental disorder comorbidity is age invariant, indicating that the lower prevalence of categorical mental disorders in older adults originates from lower average means on these two latent liability dimensions. This age-invariant dimensional liability model of mental disorder comorbidity may help improve integrative understanding of the interplay of aging with psychopathology and the development of new and developmentally matched treatments of mental disorders in older adults.
Highlights.
Prevalence rates of most mental disorders are lower in older than in younger adults.
We examined whether aging affects specific disorders or dimensions of psychopathology.
A distress-fear-externalizing liability model of mental disorders fit the data well.
This model was invariant across seven age groups.
Aging affected dimensions of psychopathology and not specific disorders.
This model can help inform the role of aging for research and intervention efforts.
Acknowledgments
This study was supported by NIH grants DA019606, MH076051 and MH082773 (Drs. Blanco and Wall) and the New York State Psychiatric Institute (Drs. Blanco, Hoertel, Olfson and Wall) and a fellowship grant from Public Health Expertise (Dr. Hoertel).
Role of the Funding Source: The Funding Sources had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Funding/support: supported by NIH grants DA019606, MH076051 and MH082773 (Drs. Blanco and Wall) and the New York State Psychiatric Institute (Drs. Blanco, Hoertel, Olfson and Wall) and a fellowship grant from Public Health Expertise (Dr. Hoertel).
Footnotes
Conflicts of interest: none
Contributors: NH, KM, MW, FL and CB designed the study. NH and KM undertook statistical analyses. NH, KM and CB wrote the first draft of the manuscript. MO, MW, JMRF, CL and FL reviewed the draft. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andrews G, Goldberg DP, Krueger RF, Carpenter WT, Jr, Hyman SE, Sachdev P, et al. Exploring the feasibility of a meta-structure for DSM-V and ICD-11: could it improve utility and validity? Psychol Med. 2009;39:1993–2000. doi: 10.1017/S0033291709990250. [DOI] [PubMed] [Google Scholar]
- American Association for Geriatric Psychiatry. IOM Study on Mental Health Workforce of Older Adults Fact Sheet. 2008 http://www.aagponline.org/index.php?rc=gendocs&ref=FactSheetIOMStudyonMentalHealthWorkforceofOlderAdults&category=Advocacy.
- Beekman AT, Bremmer MA, Deeg DJ, van Balkom AJ, Smit JH, de Beurs E, et al. Anxiety disorders in later life: a report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry. 1998;13:717–26. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307–11. doi: 10.1192/bjp.174.4.307. [DOI] [PubMed] [Google Scholar]
- Blanco C, Krueger RF, Hasin DS, Liu SM, Wang S, Kerridge BT, et al. Mapping common psychiatric disorders: structure and predictive validity in the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2013;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland RC, Newman SC, Orn H. Prevalence of psychiatric disorders in the elderly in Edmonton. Acta Psychiatrica Scandinavica Suppl. 1988;338:57–63. doi: 10.1111/j.1600-0447.1988.tb08548.x. [DOI] [PubMed] [Google Scholar]
- Blazer DG, 2nd, Hybels CF. Origins of depression in later life. Psychol Med. 2005;35:1241–52. doi: 10.1017/S0033291705004411. [DOI] [PubMed] [Google Scholar]
- Bruce ML, Leaf PJ. Psychiatric disorders and 15-month mortality in a community sample of older adults. Am J Public Health. 1989;79:727–30. doi: 10.2105/ajph.79.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchan H, Sunderland M, Carragher N, Batterham P, Slade T. Investigating age-related differences in responses to screening items for internalising disorders in three national surveys. J Affect Disord. 2014:152–154. 229–36. doi: 10.1016/j.jad.2013.09.015. [DOI] [PubMed] [Google Scholar]
- Canino G, Bravo M, Ramírez R, Febo VE, Rubio-Stipec M, Fernández RL, et al. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol Drugs. 1999;60:790–9. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- Charles ST. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol Bull. 2010;136:1068–91. doi: 10.1037/a0021232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule--Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47:171–85. doi: 10.1016/s0376-8716(97)00088-4. [DOI] [PubMed] [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Modeling. 2002;9:233–55. [Google Scholar]
- Demirkan A, Penninx BW, Hek K, Wray NR, Amin N, Aulchenko YS, et al. Genetic risk profiles for depression and anxiety in adult and elderly cohorts. Mol Psychiatry. 2011;16:773–83. doi: 10.1038/mp.2010.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnellan MB, Lucas RE. Age differences in the Big Five across the life span: evidence from two national samples. Psychol Aging. 2008;23:558–66. doi: 10.1037/a0012897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR. Latent variable and network models of comorbidity: toward an empirically derived nosology. Soc Psychiatry Psychiatr Epidemiol. 2015 Jan 20; doi: 10.1007/s00127-015-1012-7. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Eaton NR. Transdiagnostic psychopathology factors and sexual minority mental health: evidence of disparities and associations with minority stressors. Psychol Sex Orientat Gend Divers. 2014;1(3):244–54. doi: 10.1037/sgd0000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Noordhof A, Skodol AE, Markon KE, Grant BF, Hasin DS. Ethnicity and psychiatric comorbidity in a national sample: evidence for latent comorbidity factor invariance and connections with disorder prevalence. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):701–10. doi: 10.1007/s00127-012-0595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: Evidence from a national sample. J Abnorm Psychol. 2012;121:282–8. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Oltmanns TF. Aging and the structure and long-term stability of the internalizing spectrum of personality and psychopathology. Psychol Aging. 2011;26:987–93. doi: 10.1037/a0024406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- Godfrey K. Statistics in practice. Comparing the means of several groups. N Engl J Med. 1985;313:1450–6. doi: 10.1056/NEJM198512053132305. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–66. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Griffith JW, Zinbarg RE, Craske MG, Mineka S, Rose RD, Waters AM, et al. Neuroticism as a common dimension in the internalizing disorders. Psychol Med. 2010;40:1125–36. doi: 10.1017/S0033291709991449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gum AM, King-Kallimanis B, Kohn R. Prevalence of mood, anxiety, and substanceabuse disorders for older Americans in the national comorbidity survey-replication. Am J Geriatr Psychiatry. 2009;17:769–81. doi: 10.1097/JGP.0b013e3181ad4f5a. [DOI] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44:133–41. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hoertel N, Le Strat Y, Gorwood P, Bera-Potelle C, Schuster JP, Manetti A, et al. Why does the lifetime prevalence of major depressive disorder in the elderly appear to be lower than in younger adults? Results from a national representative sample. J Affect Disord. 2013;149:160–5. doi: 10.1016/j.jad.2013.01.017. [DOI] [PubMed] [Google Scholar]
- Hoertel N, Limosin F, Leleu H. Poor longitudinal continuity of care is associated with an increased mortality rate among patients with mental disorders: Results from the French National Health Insurance Reimbursement Database. Eur Psychiatry. 2014;29:358–64. doi: 10.1016/j.eurpsy.2013.12.001. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- Insel TR, Cuthbert BN, Garvey MA, Heinssen RK, Pine DS, Quinn KJ, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Alexopoulos GS, Bartels SJ, Cummings JL, Gallo JJ, Gottlieb GL, et al. Consensus statement on the upcoming crisis in geriatric mental health: research agenda for the next 2 decades. Arch Gen Psychiatry. 1999;56:848–53. doi: 10.1001/archpsyc.56.9.848. [DOI] [PubMed] [Google Scholar]
- Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30:11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–37. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005a;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Birnbaum H, Bromet E, Hwang I, Sampson N, Shahly V. Age differences in major depression: results from the National Comorbidity Survey Replication (NCS-R) Psychol Med. 2010;40:225–37. doi: 10.1017/S0033291709990213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005b;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: a review and synthesis. Alcohol Clin Exp Res. 2011;35:2101–12. doi: 10.1111/j.1530-0277.2011.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68:1003–11. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Kramer M, German PS, Anthony JC, Von Korff M, Skinner EA. Patterns of mental disorders among the elderly residents of eastern Baltimore. J Am Geriatr Soc. 1985;33:236–45. doi: 10.1111/j.1532-5415.1985.tb07110.x. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psychol. 1998;107:216–27. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol. 2003;112:437–47. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Eaton NR, Derringer J, Markon KE, Watson D, Skodol AE. Personality in DSM-5: Helping delineate personality disorder content and framing the metastructure. J Pers Asses. 2011;93:325–31. doi: 10.1080/00223891.2011.577478. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin. 2006;2:111–33. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Strat Y, Hoertel N. Correlation is no causation: gymnasium proliferation and the risk of obesity. Addiction. 2011;106:1871–72. doi: 10.1111/j.1360-0443.2011.03547.x. [DOI] [PubMed] [Google Scholar]
- Lemogne C, Nabi H, Melchior M, Goldberg M, Limosin F, Consoli SM, et al. Mortality associated with depression as compared with other severe mental disorders: a 20-year follow-up study of the GAZEL cohort. J Psychiatr Res. 2013;47:851–7. doi: 10.1016/j.jpsychires.2013.03.015. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Shear MK, Schulberg HC, Dew MA, Begley AE, et al. Comorbid anxiety disorders in depressed elderly patients. Am J Psychiatry. 2000;157:722–8. doi: 10.1176/appi.ajp.157.5.722. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Johnson MD, Willett JB. Individual growth curve analysis illuminates stability and change in personality disorder features: the longitudinal study of personality disorders. Arch Gen Psychiatry. 2004;61:1015–24. doi: 10.1001/archpsyc.61.10.1015. [DOI] [PubMed] [Google Scholar]
- Magidson JF, Blashill AJ, Wall MM, Balan IC, Wang S, Lejuez CW, et al. Relationship between psychiatric disorders and sexually transmitted diseases in a nationally representative sample. J Psychosom Res. 2014;76:322–8. doi: 10.1016/j.jpsychores.2013.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manetti A, Hoertel N, Le Strat Y, Schuster JP, Lemogne C, Limosin F. Comorbidity of Late-Life Depression in the United States: A Population-based Study. Am J Geriatr Psychiatry. 2013;22:1292–306. doi: 10.1016/j.jagp.2013.05.001. [DOI] [PubMed] [Google Scholar]
- Mather M. The emotion paradox in the aging brain. Ann N Y Acad Sci. 2012;1251:33–49. doi: 10.1111/j.1749-6632.2012.06471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mather M, Canli T, English T, Whitfield S, Wais P, Ochsner K, et al. Amygdala responses to emotionally valenced stimuli in older and younger adults. Psychol Sci. 2004;15:259–63. doi: 10.1111/j.0956-7976.2004.00662.x. [DOI] [PubMed] [Google Scholar]
- Millsap RE, Meredith W. Factorial invariance: Historical perspectives and new problems. In: Cudeck R, MacCallum RC, editors. Factor analysis at 100: Historical developments and future directions. Mahwah, NJ: Erlbaum; 2007. pp. 131–152. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Los Angeles: 1998. [Google Scholar]
- Orimo H, Ito H, Suzuki T, Araki A, Hosoi T, Sawabe M. Reviewing the definition of “elderly”. Geriatr Gerontol Int. 2006;6:149–58. [Google Scholar]
- Regier DA, Boyd JH, Burke JD, Jr, Rae DS, Myers JK, Kramer M, et al. One-month prevalence of mental disorders in the United States. Based on five Epidemiologic Catchment Area sites Arch Gen Psychiatry. 1988;45:977–86. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, 3rd, Dew MA, Pollock BG, Mulsant BH, Frank E, Miller MD, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354:1130–8. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- Schoevers RA, Beekman AT, Deeg DJ, Jonker C, van Tilburg W. Comorbidity and risk patterns of depression, generalised anxiety disorder and mixed anxiety-depression in later life: results from the AMSTEL study. Int J Geriatr Psychiatry. 2003;18:994–1001. doi: 10.1002/gps.1001. [DOI] [PubMed] [Google Scholar]
- Schuster JP, Hoertel N, Le Strat Y, Manetti A, Limosin F. Personality disorders in older adults: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. American Journal of Geriatric Psychiatry. 2013a;21:757–68. doi: 10.1016/j.jagp.2013.01.055. [DOI] [PubMed] [Google Scholar]
- Schuster JP, Manetti A, Aeschimann M, Limosin F. [Epidemiology of psychiatric disorders in elderly and their impact on somatic health] Geriatr Psychol Neuropsychiatr Vieil. 2013b;11:181–5. doi: 10.1684/pnv.2013.0405. [DOI] [PubMed] [Google Scholar]
- Segal DL, Coolidge FL, Mizuno H. Defense mechanism differences between younger and older adults: A cross-sectional investigation. Aging Ment Health. 2007;11:415–22. doi: 10.1080/13607860600963588. [DOI] [PubMed] [Google Scholar]
- Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. International Psychogeriatrics. 2010;22:1025–39. doi: 10.1017/S1041610210000608. [DOI] [PubMed] [Google Scholar]
- Simon GE, VonKorff M, Ustun TB, Gater R, Gureje O, Sartorius N. Is the lifetime risk of depression actually increasing? J Clin Epidemiol. 1995;48:1109–18. doi: 10.1016/0895-4356(95)00010-2. [DOI] [PubMed] [Google Scholar]
- Slade T. The descriptive epidemiology of internalizing and externalizing psychiatric dimensions. Soc Psychiatry Psychiatr Epidemiol. 2007;42:554–60. doi: 10.1007/s00127-007-0200-5. [DOI] [PubMed] [Google Scholar]
- Sunderland M, Anderson TM, Sachdev PS, Titov N, Andrews G. Lifetime and current prevalence of common DSM-IV mental disorders, their demographic correlates, and association with service utilisation and disability in older Australian adults. Aust N Z J Psychiatry. 2014 doi: 10.1177/0004867414538674. pii: 0004867414538674 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Sunderland M, Slade T, Carragher N, Batterham P, Buchan H. Age-related differences in internalizing psychopathology amongst the Australian general population. J Abnorm Psychol. 2013;122:1010–20. doi: 10.1037/a0034562. [DOI] [PubMed] [Google Scholar]
- Tsuang MT, Simpson JC. Mortality studies in psychiatry. Should they stop or proceed? Arch Gen Psychiatry. 1985;42:98–103. doi: 10.1001/archpsyc.1985.01790240100012. [DOI] [PubMed] [Google Scholar]
- Vollebergh WA, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Myers JK, Tischler GL, Holzer CE, 3rd, Leaf PJ, Orvaschel H, et al. Psychiatric disorders (DSM-III) and cognitive impairment among the elderly in a U.S. urban community. Acta Psychiatr Scand. 1985;71:366–79. doi: 10.1111/j.1600-0447.1985.tb02536.x. [DOI] [PubMed] [Google Scholar]
- Williams LM, Brown KJ, Palmer D, Liddell BJ, Kemp AH, Olivieri G, et al. The mellow years?: neural basis of improving emotional stability over age. J Neurosci. 2006;26:6422–30. doi: 10.1523/JNEUROSCI.0022-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne LB, Tremont G. Unique effects of apathy and depression signs on cognition and function in amnestic mild cognitive impairment. Int J Geriatr Psychiatry. 2013;28:50–6. doi: 10.1002/gps.3789. [DOI] [PubMed] [Google Scholar]


