Abstract
Context
Posttraumatic stress disorder (PTSD) is a prevalent condition associated with intimate relationship problems, and intimate relationship factors have been shown to affect individual PTSD treatment outcomes.
Objective
To compare cognitive-behavioral conjoint therapy for PTSD (a manualized couple therapy delivered to patients with PTSD and their significant others to simultaneously treat PTSD symptoms and enhance relationship satisfaction) with a wait-list condition.
Design, Setting, and Participants
Randomized controlled trial of heterosexual and same-sex couples (n=40 couples; n=80 individuals) in which one partner met criteria for PTSD according to the Clinician-Administered PTSD Scale, conducted from 2008 to 2012 in a Department of Veterans Affairs outpatient hospital setting in Boston, Massachusetts, and a university-based research center in Toronto, Ontario, Canada. Symptoms of PTSD, comorbid conditions, and relationship satisfaction were collected by blinded assessors at baseline, at mid treatment (median, 8.00 weeks [range, 1.71–20.43 weeks] after baseline), and at posttreatment (median, 15.86 weeks [range, 7.14–38.57 weeks] after baseline). An uncontrolled 3-month follow-up (median, 38.21 weeks [range, 28.43–50.57 weeks] after baseline) was also completed.
Intervention
Couples were randomly assigned to take part in the 15-session cognitive-behavioral conjoint therapy for PTSD protocol immediately (n=20) or were placed on a wait list for the therapy (n=20).
Main Outcome Measures
Clinician-rated PTSD symptom severity was the primary outcome and was assessed with the Clinician-Administered PTSD Scale. Intimate relationship satisfaction, assessed with the Dyadic Adjustment Scale, patient- and partner-rated PTSD symptoms, and comorbid symptoms were secondary outcomes.
Results
PTSD symptom severity (score range, 0–136) was significantly more improved in the couple therapy condition than in the wait-list condition (mean change difference, −23.21; 95% CI, −37.87 to −8.55). Similarly, patients’ intimate relationship satisfaction (score range, 0–151) was significantly more improved in couple therapy than in the wait-list condition (mean change difference, 9.43; 95% CI, 0.04–18.83). The time×condition interaction effect in the multilevel model predicting PTSD symptoms (t37.5=−3.09; P =.004) and patient-reported relationship satisfaction (t68.5=2.00; P=.049) revealed superiority of the couple therapy compared with the wait list. Treatment effects were maintained at 3-month follow-up.
Conclusion
Among couples in which one partner was diagnosed as having PTSD, a disorder-specific couple therapy, compared with a wait list for the therapy, resulted in decreased PTSD symptom severity and patient comorbid symptom severity and increased patient relationship satisfaction.
Trial Registration
clinicaltrials.gov Identifier: NCT00669981
There are well-documented associations between post-traumatic stress disorder (PTSD) and intimate relationship problems, including relationship distress and aggression,1 and studies demonstrate that the presence of PTSD symptoms in one partner is associated with caregiver burden and psychological distress in the other partner.2 Although currently available individual psychotherapies for PTSD produce overall improvements in psychosocial functioning, these improvements are not specifically found in intimate relationship functioning.3 Moreover, it has been shown that even when patients receive state-of-the-art individual psychotherapy for the disorder, negative interpersonal relations predict worse treatment outcomes.4,5
Conjoint therapy is a form of psychotherapy involving 2 patients, usually intimate partners. Participants in the current investigation were all intimate couples; therefore, we refer to the intervention reported on in this article as a type of couple therapy. Uncontrolled trials of couple therapy for PTSD have shown improvements in overall PTSD symptoms and relationship satisfaction6–8 and avoidance symptoms,9 but these studies have not used appropriate methodological controls and included small samples that were not diverse with respect to type of trauma, race or ethnicity of the traumatized partner, or sexual orientation of the couple. Therefore, the goal of the present study was to conduct a randomized controlled trial of cognitive-behavioral conjoint therapy (CBCT) for PTSD,10 a 15-session therapy designed to treat PTSD and its comorbid symptoms and enhance intimate relationships, in intimate couples in which one partner was diagnosed as having PTSD. Given the absence of conclusive findings that a couple therapy can simultaneously improve PTSD symptoms and relationship satisfaction, we followed recommendations for the development and testing of psychotherapies and used a wait-list control condition as an initial test of the efficacy and safety of CBCT. Waiting lists control for important threats to internal validity, including history and maturation, effects of instrumentation, effects of repeated testing, and statistical regression.11
METHODS
Participants
Forty intimate couples in which one partner met criteria for PTSD were enrolled across the 2 sites in Boston, Massachusetts (Department of Veterans Affairs outpatient hospital setting), and Toronto, Ontario, Canada (university-based research center) during the study, which was conducted from 2008 to 2012. Each partner’s PTSD diagnostic status was assessed by clinician-administered semistructured interview (described below). Both partners had to be between 18 and 70 years old. Exclusion criteria for both partners included substance dependence (abuse allowed) not in remission for at least 3 months, current uncontrolled bipolar or psychotic disorder, imminent suicidality or homicidality, severe cognitive impairment, or severe intimate partner aggression in the past year. Participants were asked to refrain from receiving any other couple therapy or evidence-based individual therapy for PTSD during the study and, if taking psychotropic medications, to maintain a stabilized regimen for at least 2 months prior to study entry.
Measures
Diagnosis of PTSD and symptom severity were established with the Clinician-Administered PTSD Scale (CAPS),12 a semistructured clinician interview consistent with the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) (DSM-IV-TR).13 Posttraumatic stress disorder diagnostic status was based on meeting the DSM-IV-TR symptom cluster criteria (to be counted as a symptom, minimum frequency=1 and intensity=2) and a total CAPS severity score of 45 or higher.14 Total CAPS symptom severity was the primary outcome. The range of scores on the CAPS is 0 to 136, with higher scores indicating greater PTSD symptom severity. A clinically significant change on the CAPS (ie, 10 points) has been previously established.15
The Structured Clinical Interview for DSM-IV–Patient Version (SCID-P)16 was used to determine exclusion criteria and to describe mental health diagnoses at study entry. All CAPS and SCID-P assessments were audio-recorded, and a random sample of 10% of each sites’ administrations was evaluated by an independent doctoral-level clinical psychologist for reliability. The intraclass correlation17 between the assessors’ and independent assessment reliability monitor’s CAPS ratings was excellent (0.99 for total score), and reliability for current and lifetime SCID-P diagnoses was excellent (κ =0.71–1.00) across all disorders except mood disorders, which was at the moderate level (κ =0.60).
The PTSD Checklist (PCL)18 provided an additional measure of PTSD symptom severity. The PCL is a 17-item self-report measure of PTSD symptoms corresponding with those included in the DSM-IV-TR. The score range for the PCL is 17 to 85, with higher scores indicating greater PTSD symptom severity. Partners’ ratings of their perception of the patients’ symptoms were also obtained using the PCL. Patients completed the Beck Depression Inventory II (BDI; score range, 0–63),19 the trait (score range, 10–40) and anger expression (score range, 0–72) subscales of the State-Trait Anger Expression Inventory,20 and the state subscale of the State-Trait Anxiety Inventory (score range, 20–80).21 Higher scores on all measures indicate greater symptom severity. Clinically significant changes on the PCL (ie, 5 points) and the BDI (ie, 5 points) have been previously established.6,11
The Dyadic Adjustment Scale (DAS)22 is a 32-item self-report inventory (score range, 0–151) that was used to measure intimate relationship satisfaction according to each partner. A total score of 98 or higher was the criterion for relationship satisfaction. A clinically significant change on the DAS (ie, 10 points) has been previously established.23 The Conflict Tactics Scale–Revised24 was used to establish exclusion criteria related to severe aggression. Endorsement of any severe physically or sexually aggressive behavior as defined by the Conflict Tactics Scale–Revised in the past year (eg, punching, threatening with knife or gun) excluded couples from the study.
Procedures
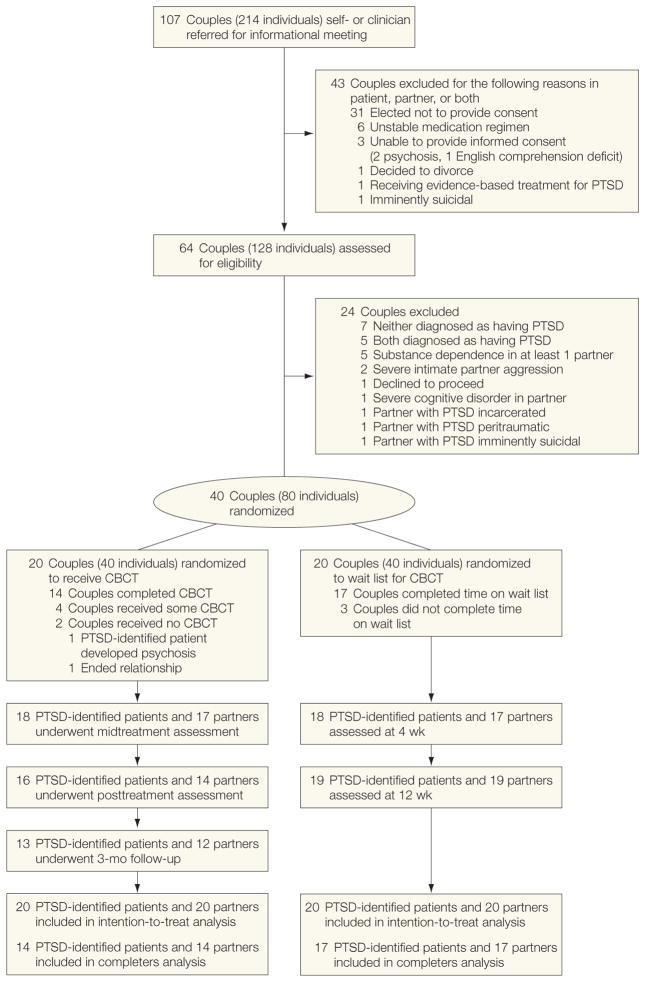
Institutional review boards at each study site approved the protocol. Participants were recruited via clinician referral, media advertisement, and self-referral from community postings (Figure). Potentially eligible couples were invited to an in-person meeting, during which they were given an overview of the study and reviewed the informed consent form. For those interested in participation, each member of the couple subsequently provided written informed consent and was assessed for the inclusion/exclusion criteria. To characterize the sample, participants self-identified race and ethnicity by selecting 1 of the following categories: white (non-Hispanic), black, Hispanic, Asian or Pacific Islander, Native American, or other (specify).
Figure.
Participant Flow
CBCT indicates cognitive-behavioral conjoint therapy; PTSD, posttraumatic stress disorder.
Eligible couples were randomly assigned using a simple type of randomization to CBCT or the wait-list condition requiring them to wait for 3 months before receiving the treatment. The study biostatistician generated and implemented the randomization. Allocation results were concealed with separate sealed privacy envelopes that were opened when a couple was deemed eligible to participate. Participants were assessed on the following occasions: baseline, mid treatment (or after 4 weeks of waiting; median, 8.00 weeks [range, 1.71–20.43 weeks] after baseline), and posttreatment (or after 12 weeks of waiting; median, 15.86 weeks [range, 7.14–38.57 weeks] after baseline). Participants who received CBCT were also assessed 3 months after completing treatment (ie, uncontrolled follow-up assessment; median, 38.21 weeks [range, 28.43–50.57 weeks] after baseline). Master’s- or doctoral-level clinicians conducted independent assessments of PTSD symptoms, blinded to condition assignment. Consistent with intention-to-treat principles, irrespective of treatment dropout, participants were asked to continue with assessments.
Treatment and Treatment Fidelity Monitoring
Cognitive-behavioral conjoint therapy is a manualized intervention for PTSD delivered in a couple therapy format that is designed to simultaneously reduce PTSD and its comorbid symptoms and enhance relationship satisfaction.10 The therapy consists of 15 sessions organized into 3 phases that build on one another and includes both in- and out-of-session exercises to increase skill acquisition and use. Therapy sessions were conducted on a twice-weekly basis for phases 1 and 2 whenever possible and weekly during phase 3.
Phase 1 of CBCT focuses on establishing the rationale for the therapy and establishing safety within the relationship. In session 1, couples are provided psychoeducation about the reciprocal influences of PTSD symptoms and relationship functioning, the rationale for the cognitive and behavioral treatment targets, and an overview of the course of therapy. Specific goals for improvements in PTSD and couple functioning are also set. At the end of the first session, the couple is instructed to catch each other doing nice things to promote positivity in their relationship and decrease selective attention to negativity. Each partner is also asked to complete the Trauma Impact Questions, a set of questions designed to elicit each partner’s thoughts about how PTSD has affected their relationship and the perceived cause(s) of the traumatic event(s), as well as each partner’s thoughts about oneself, his or her partner, and the world in general in the areas of trust, control, emotional closeness, and physical intimacy. In session 2, these responses are then shared aloud. The couple also is educated about how PTSD can contribute to a range of aggressive or withdrawing behaviors because of dysregulation in the fight-flight-freeze system. They learn strategies to facilitate a shared sense of safety, such as recognizing early warning signs of anger, slowed breathing, and time-out conflict management strategies, and they practice these skills in and out of session.
In phase 2, the generalization of avoidance beyond specific trauma memories and reminders to avoidance of emotions and other internal states (ie, experiential avoidance), and its role in maintaining both PTSD and relationship problems, are taught. Enhanced dyadic communication is used as an antidote to PTSD-related emotional numbing and avoidance as well as a means of increasing emotional intimacy. In session 3, the couple uses the communication skill of reflective listening to begin generating a list of people, places, situations, and feelings that they have avoided as a couple as a result of PTSD. Starting in session 4 and continuing through the rest of the therapy, this “avoidance” list becomes their “approach” list, and ideographically programmed, in vivo approach assignments from the list are completed after each session in a graduated manner. Special attention is paid to the selection of in vivo approach activities that will address behavioral and experiential avoidance and concurrently double as shared rewarding activities for the couple.
Communication skills presented and practiced in each session build on each other over the next several sessions to help the couple identify and share their feelings and notice the way that their thoughts influence their feelings and behaviors. In session 6, the couple learns a dyadic cognitive intervention process that has the goal of collaboratively increasing flexibility in each partner’s thinking and evaluating cognitions that maintain both PTSD and relationship problems. Each partner nominates thoughts that are subjected to this process to improve relationship satisfaction and PTSD symptoms. In session 7, the couple is taught problem-solving/decision-making skills to facilitate behavioral action based on more accurate perceptions of problems and decisions to be made.
The final phase of therapy capitalizes on the couple’s improved communication skills and their developing propensity to approach rather than avoid by examining beliefs that they may each hold that contribute to PTSD symptoms and relationship problems. Discussions focus directly on the resolution of problematic appraisals of the trauma and then proceed to specific problematic core beliefs that maintain PTSD and relationship difficulties. These domains include trust, control, emotional closeness, and physical intimacy. The therapist guides the couple to investigate how trauma has influenced thoughts in each core area and to challenge any appraisals that influence individual and relationship functioning. Treatment culminates with a discussion of the potential for benefit finding and posttraumatic growth and ends with a review of gains made in therapy and challenges expected in the future.
Four therapists provided CBCT (2 treatment developers; 1 postdoctoral fellow; and 1 doctoral student). All therapists received ongoing group consultation and individual supervision throughout the study period. Therapy sessions were video-recorded for supervision and fidelity assessment. An expert clinician in CBCT who was independent of the study rated a random sample of 10% of the treatment sessions delivered for protocol adherence and therapist competence in delivering the specific, prescribed elements of that session. Adherence to the essential elements of the therapy was good, with 86% of these elements delivered. Competence in providing these treatment elements was very good, with an average rating of 6.52 (6=very good and 7=excellent).
Statistical Analyses
Power analysis was conducted using G*Power 325 and was based on the primary hypothesis that CBCT would result in significantly lower clinician-rated PTSD symptoms compared with a wait list in multilevel modeling. A Hedge g effect size estimate was used in the power analysis because it includes a correction for sample size and is therefore more appropriate to use with small samples.26 The interpretation of g is similar to the interpretation of the Cohen d: 0.80 or greater is considered large, 0.50 to 0.79 is considered medium, and 0.20 to 0.49 is considered small.27 A minimum effect size of g =1.0 was expected based on prior uncontrolled studies of CBCT and the broader psychotherapy research for PTSD.28 An effect size of g =1.0 represents an approximately 25-point improvement in total CAPS scores. Assuming the use of multilevel modeling, a more conservative effect of g =0.80, a conservative estimate of correlation between repeated administrations of the CAPS (ie, r =0.65), a conservative estimate of 20% measurement attrition, and a 2-tailed test with α = .05, the sample of 40 couples (20 per condition) yielded power greater than 90% to find the expected effect.
Analyses were performed according to intention-to-treat principles. Thus, available data at each assessment for the entire sample were used in the multilevel models conducted using SAS software, version 9.2.29 The primary outcome was the least-squares mean difference in clinician-rated PTSD symptoms, derived from these models (see below), from pretreatment to post-treatment compared between the CBCT and wait-list groups. The difference in these pretreatment to posttreatment differences was then tested with a between-group independent samples t test. The secondary outcomes were also evaluated with this method. Multilevel modeling was also conducted on each outcome, with condition, time, and the condition×time interaction included in the model; random intercepts and slopes were estimated for each participant. Site effects were included as fixed effects in the original models for the primary outcomes, but because site was not a significant predictor, it was not retained in the final models.
We estimated clinical significance using change ratios and between-group effect sizes (g). Change ratios were calculated by dividing the change in the CBCT condition from pretreatment to posttreatment by the change in the wait-list condition over this period. Between-group effect sizes were calculated by subtracting the mean change from pretreatment to posttreatment in the wait-list group from the mean change in the CBCT group, dividing by the associated pooled standard deviation, and adjusting for small sample size. To examine maintenance of treatment gains in CBCT from post-treatment to 3-month follow-up, paired samples t tests were conducted. For these analyses, only completers were examined because of measurement attrition at this assessment for those who dropped out of treatment. Finally, clinically significant change criteria and diagnostic status for the primary outcomes (ie, loss of PTSD diagnosis per the CAPS; satisfied with relationship per the DAS) were also evaluated at each assessment.
RESULTS
Table 1 contains the characteristics of the sample within each condition at study entry. Fewer male partners were randomized to CBCT than to the wait list. Three same-sex female couples were randomized to CBCT, which accounted for this baseline difference in partner sex. There were several differences between sites. Compared with the Toronto site, the Boston site enrolled more partners with a lifetime history of substance use disorder (Boston, n=11 [27.5%]; Toronto, n = 6 [15.0%]; P =.02), a lifetime history of other anxiety disorder (Boston, n=10 [58.8%]; Toronto, n=1 [5.0%]; P < .001), and concurrent comorbid anxiety disorders (Boston, n=5 [25.0%]; Toronto, n=0; P =.005).
Table 1.
Baseline Characteristics by Condition and Partner Status
| Characteristics | PTSD-Identified Patients
|
Partners
|
||||
|---|---|---|---|---|---|---|
| CBCT (n = 20)a | Wait List (n = 20)a | Difference (95% CI)b | CBCT (n = 20)a | Wait List (n = 20)a | Difference (95% CI)b | |
| Age, mean (SD), y | 40.4 (11.3) | 33.8 (10.5) | 6.6 (−13.6 to 0.4) | 40.7 (12.5) | 34.9 (10.0) | 5.9 (−13.1 to 1.4) |
|
| ||||||
| Male | 7 (35.0) | 3 (15.0) | 20.0 | 10 (50.0) | 17 (85.0) | −35.0c |
|
| ||||||
| Nonwhite | 5 (25.0) | 6 (30.0) | −5.0 | 4 (20.0) | 4 (20.0) | 0 |
|
| ||||||
| Relationship | ||||||
| Married | 8 (40.0) | 5 (25.0) | 15.0 | 8 (40.0) | 5 (25.0) | 15.0 |
|
| ||||||
| Length, mean (SD), y | 8.1 (8.7) | 5.4 (5.8) | 2.7 (−7.6 to 2.2) | 8.2 (9.0) | 5.4 (5.8) | −2.8 (−7.7 to 2.0) |
|
| ||||||
| Previously divorced | 5 (25.0) | 5 (25.0) | 0 | 4 (20.0) | 1 (5.0) | 15.0 |
|
| ||||||
| Military veteran | 6 (30.0) | 3 (7.5) | 22.5 | 1 (5.0) | 0 | 5.0 |
|
| ||||||
| Employment (at least part time) | 12 (60.0) | 12 (60.0) | 0 | 13 (65.0) | 13 (65.0) | 0 |
|
| ||||||
| Index trauma | ||||||
| Adult sexual trauma | 4 (20.0) | 4 (20.0) | 0 | |||
|
| ||||||
| Child sexual trauma | 3 (15.0) | 8 (40.0) | −25.0 | |||
|
| ||||||
| Noncombat physical assault | 4 (20.0) | 2 (10.0) | 10.0 | |||
|
| ||||||
| Motor vehicle collision | 1 (5.0) | 2 (10.0) | −5.0 | |||
|
| ||||||
| Witnessing/learning about death/illness | 2 (10.0) | 3 (15.0) | −5.0 | |||
|
| ||||||
| Combat | 2 (10.0) | 0 | 10.0 | |||
|
| ||||||
| Other | 4 (20.0) | 1 (5.0) | 15.0 | |||
|
| ||||||
| Years since trauma, median (range) | 13.0 (1.0–44.0) | 6.5 (0.5–42.0) | 6.5 | |||
|
| ||||||
| Any current comorbid diagnosesd | 11 (55.0) | 14 (70.0) | −15.0 | 3 (15.0) | 7 (35.0) | −20.0 |
|
| ||||||
| Mood disorder | 7 (35.0) | 9 (45.0) | −10.0 | 1 (5.0) | 2 (10.0) | −5.0 |
|
| ||||||
| Other anxiety disorder | 5 (25.0) | 7 (35.0) | −10.0 | 2 (10.0) | 3 (15.0) | −5.0 |
|
| ||||||
| Substance abuse | 0 | 0 | 0 | 0 | 1 (5.0) | −5.0 |
|
| ||||||
| Other | 2 (10.0) | 2 (10.0) | 0 | 0 | 2 (10.0) | −10.0 |
|
| ||||||
| Lifetime comorbid diagnosesd | 19 (95.0) | 20 (100.0) | −5.0 | 15 (75.0) | 13 (65.0) | 10.0 |
|
| ||||||
| Mood disorder | 18 (90.0) | 17 (85.0) | 5.0 | 12 (60.0) | 9 (45.0) | 15.0 |
|
| ||||||
| Other anxiety disordere | 9 (45.0) | 10 (50.0) | −5.0 | 6 (30.0) | 5 (25.0) | 5.0 |
|
| ||||||
| Substance abuse or dependence | 9 (45.0) | 8 (40.0) | 5.0 | 10 (50.0) | 7 (35.0) | 15.0 |
|
| ||||||
| Other | 5 (25.0) | 4 (20.0) | 5.0 | 1 (5.0) | 2 (10.0) | −5.0 |
|
| ||||||
| Stable psychotropic medications | 7 (35.0) | 11 (55.0) | −20.0 | 7 (35.0) | 2 (10.0) | 25.0 |
|
| ||||||
| Concurrent psychotherapy | 8 (40.0) | 7 (35.0) | 5.0 | 7 (35.0) | 5 (25.0) | 10.0 |
|
| ||||||
| Outcome measures, mean (SD) | ||||||
| Clinician-Administered PTSD Scale (total) | 69.5 (12.7) | 74.8 (15.0) | −5.3 (−3.5 to 14.2) | |||
|
| ||||||
| PTSD Checklist (total self- and partner report) | 50.3 (11.0) | 58.5 (11.6) | −8.2 (1.0 to 15.5)c | 44.5 (11.8) | 43.7 (16.0) | 0.7 (−9.8 to 8.3) |
|
| ||||||
| Dyadic Adjustment Scale (total) | 101.3 (22.2) | 98.1 (20.8) | 3.2 (−16.9 to 10.6) | 104.0 (21.0) | 99.5 (19.9) | 4.5 (−17.6 to 8.6) |
|
| ||||||
| Beck Depression Inventory II (total) | 23.0 (11.9) | 22.9 (10.5) | 0.1 (−7.4 to 7.1) | |||
|
| ||||||
| State-Trait Anxiety Inventory state subscale | 48.8 (12.6) | 51.2 (12.0) | −2.4 (−5.6 to 10.3) | |||
|
| ||||||
| State-Trait Anger Expression Inventory | ||||||
| Trait subscale | 23.7 (8.5) | 22.7 (5.7) | 1.0 (−5.6 to .3.7) | |||
|
| ||||||
| Anger expression subscale | 35.2 (13.0) | 37.1 (7.9) | −1.9 (−5.0 to 8.8) | |||
Abbreviations: CBCT, cognitive-behavioral conjoint therapy; PTSD, posttraumatic stress disorder.
Data are expressed as No. (%) unless otherwise indicated.
Percentage difference between CBCT and wait list reported for categorical variables; mean difference and 95% CI reported for continuous variables. Negative values indicate smaller means or percentages in the CBCT condition.
Significantly different at P < .05.
All comorbid diagnoses were determined by the Structured Clinical Interview for DSM-IV–Patient Version.
Includes lifetime PTSD diagnosis in other anxiety disorder diagnosis category for partners.
Individuals randomized to CBCT did not differ from individuals randomized to the wait list at baseline on the outcome variables, except that patients in CBCT had lower self-rated PTSD symptom severity relative to those on the wait list. There was no statistical difference in dropout rate by condition (CBCT, n = 6 [30%]; wait-list, n=3 [15%]; P =.26). There was 1 serious adverse event of severe intimate aggression in the CBCT group. The couple did not disclose their history of severe physical aggression at intake, which would have precluded their inclusion in the study. The study team discontinued CBCT because one of the partners in this couple did not agree to identify intimate aggression as a necessary treatment target in therapy. No events were deemed study-related.
Table 2 shows least-squares mean scores on primary and secondary outcome measures by condition, mean change scores from pretreatment to posttreatment, and within-group effect sizes for each group. Change ratios, mean change differences, and between-group effect sizes are shown in Table 3. Change ratios revealed that PTSD symptom severity as measured by the CAPS decreased almost 3 times more in CBCT from pretreatment to posttreatment compared with the wait list (CBCT: mean change, −35.42 [95% CI, −47.84 to −23.00]; wait list: mean change, −12.20 [95% CI, −21.51 to −2.89]; mean change difference, −23.21 [95% CI, −37.87 to −8.55]) and patient-reported relationship satisfaction, as measured by the DAS, increased more than 4 times more in CBCT compared with the wait list (CBCT: mean change, 12.22 [95% CI, 5.72–18.72]; wait list: mean change, 2.79 [95% CI, −3.95 to 9.53]; mean change difference, 9.43 [95% CI, 0.04–18.83]). In support of these results, multilevel modeling of the outcomes revealed the predicted time×condition interaction for the primary outcome of clinician-rated PTSD symptom severity (t37.5=−3.09; P =.004) and for patient-reported relationship satisfaction (t68.5=2.00; P =.049). The CBCT condition had a greater decline in PTSD symptoms and greater improvement in patient-reported relationship satisfaction over time compared with the wait list.
Table 2.
Scores, Change Scores Within Condition, and Within-Condition Effect Sizes of Primary and Secondary Outcomes by Condition
| Outcome Measures | Score, Mean (95% CI)a
|
Change Score, Mean (95% CI)b | Effect Size, Hedge g, Pretreatment to Posttreatment (95% CI)c | ||
|---|---|---|---|---|---|
| Pretreatment | Mid Treatment or 4-Week Wait | Posttreatment or 12-Week Wait | |||
| Clinician-Administered PTSD Scaled | |||||
| CBCT | 68.87 (62.12–75.61) | 51.16 (43.59–58.72) | 33.45 (22.03–44.87) | −35.42 (−47.84 to −23.00) | 1.82 (1.00 to 2.62) |
|
| |||||
| Wait list | 73.03 (66.29–79.76) | 66.92 (59.50–74.35) | 60.82 (49.87–71.78) | −12.20 (−21.51 to −2.89) | 0.57 (0.12 to 1.00) |
|
| |||||
| Dyadic Adjustment Scalee | |||||
| Patient | |||||
| CBCT | 100.64 (91.92–109.37) | 106.76 (98.39–115.12) | 112.87 (103.53–122.20) | 12.22 (5.72 to 18.72) | 0.64 (0.06 to 1.21) |
|
| |||||
| Wait list | 97.63 (88.92–106.34) | 99.02 (90.78–107.27) | 100.42 (91.62–109.21) | 2.79 (−3.95 to 9.53) | 0.13 (−0.17 to 0.44) |
|
| |||||
| Partner | |||||
| CBCT | 104.28 (95.51–113.06) | 105.90 (97.29–114.51) | 107.52 (98.29–116.75) | 3.23 (−2.35 to 8.81) | 0.15 (−0.08 to 0.37) |
|
| |||||
| Wait list | 99.59 (90.83–108.36) | 101.07 (92.52–109.62) | 102.55 (93.59–111.50) | 2.95 (−2.50 to 8.40) | 0.15 (−0.11 to 0.40) |
|
| |||||
| PTSD Checklistf | |||||
| Patient report | |||||
| CBCT | 49.92 (45.12–54.71) | 40.15 (34.98–45.32) | 30.38 (22.81–37.96) | −19.53 (−27.30 to −11.77) | 1.61 (0.83 to 2.37) |
|
| |||||
| Wait list | 57.89 (53.10–62.67) | 52.34 (47.28–57.41) | 46.80 (39.61–53.99) | −11.09 (−18.34 to −3.85) | 0.71 (0.21 to 1.20) |
|
| |||||
| Partner report | |||||
| CBCT | 44.35 (38.33–50.38) | 38.29 (32.86–43.71) | 32.22 (25.53–38.92) | −12.13 (−20.24 to −4.03) | 1.02 (0.35 to 1.66) |
|
| |||||
| Wait list | 43.99 (37.97–50.00) | 40.87 (35.58–46.16) | 37.75 (31.63–43.88) | −6.23 (−12.36 to −0.10) | 0.38 (0.00 to 0.74) |
|
| |||||
| Beck Depression Inventory IIg | |||||
| CBCT | 24.36 (19.59–29.12) | 18.26 (13.60–22.91) | 12.16 (6.35–17.96) | −12.20 (−19.10 to −5.31) | 1.16 (0.40 to 1.89) |
|
| |||||
| Wait list | 22.60 (17.88–27.32) | 21.46 (16.87–26.05) | 20.32 (14.79–25.85) | −2.29 (−6.37 to 1.79) | 0.17 (−0.13 to 0.47) |
|
| |||||
| State-Trait Anxiety Inventory state subscaleh | |||||
| CBCT | 49.25 (43.67–54.82) | 43.95 (38.70–49.19) | 38.65 (31.97–45.32) | −10.60 (−19.04 to −2.16) | 0.84 (0.17 to 1.49) |
|
| |||||
| Wait list | 50.90 (45.47–56.33) | 51.32 (46.25–56.38) | 51.73 (45.47–57.99) | 0.84 (−4.40 to 6.08) | −0.06 (−0.41 to 0.29) |
|
| |||||
| State-Trait Anger Expression Inventoryi | |||||
| Trait subscale | |||||
| CBCT | 23.65 (20.80–26.51) | 21.48 (18.75–24.22) | 19.32 (15.93–22.70) | −4.33 (−8.04 to −0.63) | 0.59 (0.04 to 1.12) |
|
| |||||
| Wait list | 22.99 (20.21–25.77) | 22.76 (20.13–25.40) | 22.53 (19.42–25.65) | −0.46 (−3.12 to 2.20) | 0.07 (−0.31 to 0.45) |
|
| |||||
| Anger expression subscale | |||||
| CBCT | 36.18 (31.72–40.63) | 32.16 (28.01–36.32) | 28.15 (23.51–32.79) | −8.02 (−12.63 to −3.42) | 0.68 (0.25 to 1.09) |
|
| |||||
| Wait list | 36.55 (32.21–40.90) | 35.97 (31.94–40.01) | 35.39 (20.99–39.79) | −1.16 (−4.55 to 2.23) | 0.13 (−0.23 to 0.50) |
Abbreviations: CBCT, cognitive-behavioral conjoint therapy; PTSD, posttraumatic stress disorder.
Means are least-squares means estimated from multilevel models.
Pretreatment to posttreatment change calculated using least-squares means estimated from multilevel models. Confidence intervals calculated using standard errors from actual data.
Effect sizes of g ≥ 0.80 are considered large; g =0.50 to 0.79 are considered moderate; and g =0.20 to 0.49 are considered small.27 Negative values indicate worsening.
The Clinician-Administered PTSD Scale was the primary outcome measure. Maximum possible score, 136.
Maximum possible score, 151.
Maximum possible score, 85.
Maximum possible score, 63.
Maximum possible score, 80.
Maximum possible score for trait subscale, 40; for anger expression subscale, 72.
Table 3.
Change Difference Scores and Between-Group Effect Sizes of Primary and Secondary Outcomes at Posttreatment or 12-Week Wait for CBCT vs Wait List
| Outcome Measures | Differences-in-Differences Change Ratio (95% CI)a | Change Difference, Mean (95% CI)b | Effect Size, Hedge g, Pretreatment to Posttreatment, Between Groups (95% CI)c | ||
|---|---|---|---|---|---|
| Clinician-Administered PTSD Scaled | 2.90 (1.45–11.34) | −23.21 (−37.87 to −8.55) | 1.13 (0.40 to 1.85) | ||
|
| |||||
| Dyadic Adjustment Scalee | |||||
| Patient | 4.38f | 9.43 (0.04 to 18.83) | 0.47 (−0.27 to 1.20) | ||
|
| |||||
| Partner | 1.10f | 0.28 (−7.37 to 7.93) | 0.01 (−0.68 to 0.70) | ||
|
| |||||
| PTSD Checklistg | |||||
| Patient report | 1.76 (0.89–4.99) | −8.44 (−18.71 to 1.83) | 0.60 (−0.10 to 1.29) | ||
|
| |||||
| Partner report | 1.95 (0.59–43.49) | −5.90 (−15.45 to 3.65) | 0.41 (−0.30 to 1.10) | ||
|
| |||||
| Beck Depression Inventory IIh | 5.36f | −9.91 (−17.22 to −2.60) | 0.83 (0.10 to 1.54) | ||
|
| |||||
| State-Trait Anxiety Inventory state subscalei | 12.69f | −11.43 (−20.55 to −2.31) | 0.85 (0.13 to 1.57) | ||
|
| |||||
| State-Trait Anger Expression Inventoryj | |||||
| Trait subscale | 9.49f | −3.88 (−8.12 to 0.36) | 0.56 (−0.17 to 1.28) | ||
|
| |||||
| Anger expression subscale | 6.91f | −6.86 (−12.22 to −1.50) | 0.67 (−0.06 to 1.38) | ||
Abbreviations: CBCT, cognitive-behavioral conjoint therapy; PTSD, posttraumatic stress disorder.
Differences-in-differences change ratio is equal to change from pretreatment to posttreatment in CBCT condition divided by change from pretreatment to posttreatment in wait-list condition. The change ratio was calculated using least-squares means estimated from multilevel models.
Change difference represents the difference in the mean change from pretreatment to posttreatment between CBCT and wait-list conditions. Change difference calculated using least-squares means estimated from multilevel models. Confidence intervals calculated using standard errors from actual data.
Effect sizes of g≥0.80 are considered large; g =0.50 to 0.79 are considered medium; and g =0.20 to 0.49 are considered small.27 Positive values indicate improvements in CBCT relative to wait list.
The Clinician-Administered PTSD Scale was the primary outcome measure. Maximum possible score, 136.
Maximum possible score, 151.
It was impossible to calculate a CI for the change ratio when the CI for the wait-list group included 0.
Maximum possible score, 85.
Maximum possible score, 63.
Maximum possible score, 80.
Maximum possible score for trait subscale, 40; for anger expression subscale, 72.
The secondary outcomes of depression, general anxiety, and anger expression symptoms improved more in CBCT relative to the wait list (Table 3), and there were significant time×condition interactions for these outcomes in the multilevel models: depression (t40.7=−2.87; P =.007), general anxiety (t44 = −2.62; P = .01), and anger expression (t70 .9 = −2.62; P = .01). Paired-sample t tests comparing outcome measures immediately after treatment with 3-month follow-up in those who received CBCT demonstrated that treatment gains were maintained at follow-up (CAPS mean change, −5.00 [95% CI, −14.36 to 4.36]; patient-reported DAS mean change, 2.64 [95% CI, −6.38 to 11.65]).
Table 4 contains data regarding clinical status for PTSD and relationship satisfaction. At the end of treatment, 81% of those in CBCT had a clinically significant improvement in their PTSD symptoms and 81% no longer met criteria for PTSD, which was defined as not meeting DSM-IV-TR symptom criteria and a total score lower than 45 on the CAPS. Sixty-two percent of the CBCT patients reported a clinically significant improvement in their relationship satisfaction on the DAS and 100% were classified as satisfied in their relationship according to a DAS score of 98 or higher at the end of treatment.
Table 4.
PTSD Response, Loss of Clinical PTSD Diagnosis, and Relationship Satisfaction Response by Study Conditiona
| Outcome Measures | No. (%)of Participants
|
||||
|---|---|---|---|---|---|
| Baseline
|
Posttreatment or 12-Week Wait
|
3-Month Follow-up
|
|||
| CBCT | Wait List | CBCT | Wait List | CBCT | |
| PTSD | (n = 20) | (n = 20) | (n = 16) | (n = 19) | (n = 14) |
|
| |||||
| Clinically significant response | 13 (81) | 12 (63) | 10 (71) | ||
|
| |||||
| Loss of diagnosis | 13 (81) | 4 (21) | 10 (71) | ||
|
| |||||
| Relationship satisfaction: patient | (n = 20) | (n = 20) | (n = 13) | (n = 19) | (n = 12) |
|
| |||||
| Clinically significant response | 8 (62) | 5 (26) | 5 (42) | ||
|
| |||||
| Satisfied status | 14 (70) | 12 (60) | 13 (100) | 13 (68) | 10 (83) |
|
| |||||
| Relationship satisfaction: partner | (n = 20) | (n = 20) | (n = 14) | (n = 19) | (n = 12) |
|
| |||||
| Clinically significant response | 5 (36) | 6 (32) | 5 (42) | ||
|
| |||||
| Satisfied status | 13 (65) | 12 (60) | 11 (79) | 10 (53) | 9 (75) |
Abbreviations: CBCT, cognitive-behavioral conjoint therapy; PTSD, posttraumatic stress disorder.
All PTSD outcomes are defined based on the Clinician-Administered PTSD Scale, with diagnosis defined as meeting symptom-level criteria per Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) and total severity score ≥45; a clinically significant response represents a decrease from baseline of ≥10 points. Relationship outcomes defined based on the Dyadic Adjustment Scale; satisfied status defined as total score of ≥98; clinically significant response represents an increase from baseline of ≥10 points.
COMMENT
This randomized controlled trial provides evidence for the efficacy of a couple therapy for the treatment of PTSD and comorbid symptoms, as well as enhancements in intimate relationship satisfaction. These improvements occurred in a sample of couples in which the patients varied with regard to sex, type of trauma experienced, and sexual orientation. The treatment effect size estimates found for PTSD and comorbid symptoms were comparable with or better than effects found for individual psychotherapies for PTSD.28 In addition, patients reported enhancements in relationship satisfaction consistent with or better than prior trials of couple therapy with distressed couples and stronger than those found for interventions designed to enhance relationship functioning in non-distressed couples.30 Treatment gains were maintained at 3-month uncontrolled follow-up.
The results of this trial were mostly consistent with prior uncontrolled studies of the therapy, with a few exceptions. We found little evidence of differences between CBCT and a wait list in partner-reported relationship satisfaction, and partners’ ratings of PTSD symptom improvements were not as consistent with the clinicians’ ratings. In contrast, prior research found partner-rated improvements in PTSD symptoms consistent with clinician-rated improvements and stronger effects for partner-rated relationship satisfaction.6 These differences may be related to partners’ relatively high levels of baseline satisfaction. Moreover, there were more female patients and male partners in this study compared with prior studies of veterans and a community sample. Research suggests sex differences in the association between partner health problems and relationship satisfaction31 as well as PTSD treatment outcomes.32 The more rigorous methods of the current randomized trial compared with prior studies, including controls for patient inclusion, treatment assignment, and blinded assessment, may also account for the different findings. Future trials should investigate these and other explanations.
Several limitations should be considered in interpreting and generalizing the current results. Consistent with recommendations regarding the developmental sequence in testing psychotherapies,11 we chose a wait-list comparison because of inconclusive evidence that couple therapy for PTSD could be an effective and safe option for treating PTSD and improving relationships. Although a wait list controls for many important threats to internal validity,11 we cannot rule out the possibility that the differences between the conditions were due to more intense attention in CBCT vs the wait list. The wait list had contact with the study team only to schedule assessments and with the independent assessors only to conduct the outcome measures. Moreover, an uncontrolled follow-up assessment is a limitation but was necessary to provide treatment to the wait-list group as soon as possible. Future studies that compare CBCT with other established individual psychotherapies are needed. In addition, trials that determine if CBCT is more effective than general evidence-based couple therapy or a version of the current treatment without a historical trauma focus would also be helpful in determining whether addressing specific trauma memories is essential. Studies that test the boundaries of CBCT by applying it to nonintimate dyads in controlled trials will also be informative.
The current study’s relatively small sample size limited our ability to detect some statistical or clinically important differences between CBCT and a wait list. For example, the lack of a statistically significant difference in the dropout rate across conditions (ie, the dropout rate for CBCT was twice that of the wait list) likely resulted from the small sample size. The sample size also limits investigation of factors that might moderate dropout or treatment outcome, such as comorbidity, type of trauma, and relationship characteristics. In addition, sample heterogeneity can increase generalizability but may mask important factors unique to a particular population (eg, survivors of a particular type of trauma) who may respond differently to the therapy. Larger trials that can investigate the role of baseline relationship functioning on PTSD, and relationship satisfaction outcomes are needed to facilitate treatment-matching efforts and to determine the boundaries of CBCT’s efficacy. In addition, it will be important to determine in future effectiveness trials if clinicians without specialized training in psychotherapy more generally or couple therapy more specifically can achieve similar results, given that the therapy was delivered under close supervision by the treatment developers in clinical research settings.
There is increasing recognition that intimate relationships play a potent role in recovery from PTSD, its comorbid symptoms, and the psychosocial impairments that accompany it. The current investigation demonstrated that CBCT produced improvements in clinician-rated PTSD symptoms and a range of comorbid symptoms, as well as patient-rated relationship satisfaction. Treatment effects for those who received the therapy were maintained at 3-month follow-up. Cognitive-behavioral conjoint therapy may be used to efficiently address individual and relational dimensions of traumatization and might be indicated for individuals with PTSD who have stable relationships and partners willing to engage in treatment with them.
Acknowledgments
Funding/Support: This study was supported by National Institute of Mental Health grant 5R34MH076813 to Dr Monson.
Footnotes
Role of the Sponsor: The National Institute of Mental Health had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or approval authority over the content of the article.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or any other governmental agency.
Additional Contributions: We thank Helen MacDonald, PhD, VA National Center for PTSD and Boston University School of Medicine, for assistance with conducting assessments; Rebekah Majors, PhD, VA Boston Healthcare System, and Anne Wagner, MA, Ryerson University, for serving as study therapists; Suzanne Pineles, PhD, VA National Center for PTSD and Boston University School of Medicine, for coordinating supervision of study therapists and assessors; Yinong Young-Xu, PhD, VA National Center for PTSD and Dartmouth Medical School, for consultation on statistical analysis; Melinda Morrill, MA, Clark University, and Amy Brown-Bowers, MA, and Valerie Vorstenbosch, MA, Ryerson University, for assistance with conducting assessments and study management; K. Carrie Adair, BA, now at the University of North Carolina; Jennifer Belus, BA, Derek Cozzi, BA, Meredith Landy, MA, Marta Maslej, BA, Philippe Shnaider, BA, and Sonya Wanklyn, MA, Ryerson University; and Emily McGuire, BA, VA National Center for PTSD; for assistance with study management. Drs MacDonald, Pineles, and Young-Xu and Ms Vorstenbosch were paid for their work on the project. We also thank all of the patients for their valuable contributions to the study.
Author Contributions: Dr Monson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Monson, Resick, Schnurr.
Acquisition of data: Monson, Fredman, Macdonald.
Analysis and interpretation of data: Monson, Fredman, Macdonald, Pukay-Martin.
Drafting of the manuscript: Monson, Fredman, Macdonald, Pukay-Martin.
Critical revision of the manuscript for important intellectual content: Monson, Fredman, Macdonald, Pukay-Martin, Resick, Schnurr.
Statistical analysis: Monson, Macdonald.
Obtained funding: Monson.
Administrative, technical, or material support: Monson, Resick.
Study supervision: Monson, Fredman.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Monson reports that she receives research funding from the Centers for Disease Control and Prevention, Department of Defense, Canadian Institute of Health Research, and National Institute of Mental Health. Drs Monson and Fredman report that they receive royalties for a published book describing CBCT for PTSD. Dr Resick reports that she receives research funding from the Department of Defense and US Department of Veterans Affairs. Dr Schnurr reports that she receives research funding from US Department of Veterans Affairs. Drs Resick and Schnurr report that they have published books on PTSD and its treatment for which they receive income. No other disclosures were reported.
References
- 1.Taft CT, Watkins LE, Stafford J, Street AE, Monson CM. Posttraumatic stress disorder and intimate relationship problems: a meta-analysis. J Consult Clin Psychol. 2011;79(1):22–33. doi: 10.1037/a0022196. [DOI] [PubMed] [Google Scholar]
- 2.Caska CM, Renshaw KD. Perceived burden in spouses of National Guard/Reserve service members deployed during Operations Enduring and Iraqi Freedom. J Anxiety Disord. 2011;25(3):346–351. doi: 10.1016/j.janxdis.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Schnurr PP, Hayes AF, Lunney CA, McFall M, Uddo M. Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(4):707–713. doi: 10.1037/0022-006X.74.4.707. [DOI] [PubMed] [Google Scholar]
- 4.Price M, Gros DF, Strachan M, Ruggiero KJ, Acierno R. The role of social support in exposure therapy for Operation Iraqi Freedom/Operation Enduring Freedom veterans: a preliminary investigation [published online November 7, 2011] Psychol Trauma. doi: 10.1037/a0026244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tarrier N, Sommerfield C, Pilgrim H. Relatives’ expressed emotion (EE) and PTSD treatment outcome. Psychol Med. 1999;29(4):801–811. doi: 10.1017/s0033291799008569. [DOI] [PubMed] [Google Scholar]
- 6.Monson CM, Schnurr PP, Stevens SP, Guthrie KA. Cognitive-behavioral couple’s treatment for posttraumatic stress disorder: initial findings. J Trauma Stress. 2004;17(4):341–344. doi: 10.1023/B:JOTS.0000038483.69570.5b. [DOI] [PubMed] [Google Scholar]
- 7.Monson CM, Fredman SJ, Adair KC, et al. Cognitive-behavioral conjoint therapy for PTSD: pilot results from a community sample. J Trauma Stress. 2011;24(1):97–101. doi: 10.1002/jts.20604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacIntosh HB, Johnson S. Emotionally focused therapy for couples and childhood sexual abuse survivors. J Marital Fam Ther. 2008;34(3):298–315. doi: 10.1111/j.1752-0606.2008.00074.x. [DOI] [PubMed] [Google Scholar]
- 9.Sautter FJ, Glynn SM, Thompson KE, Franklin L, Han X. A couple-based approach to the reduction of PTSD avoidance symptoms: preliminary findings. J Marital Fam Ther. 2009;35(3):343–349. doi: 10.1111/j.1752-0606.2009.00125.x. [DOI] [PubMed] [Google Scholar]
- 10.Monson CM, Fredman SJ. Cognitive-Behavioral Conjoint Therapy for Posttraumatic Stress Disorder: Harnessing the Healing Power of Relationships. New York, NY: Guilford; 2012. [Google Scholar]
- 11.Schnurr PP. The rocks and hard places in psychotherapy outcome research. J Trauma Stress. 2007;20(5):779–792. doi: 10.1002/jts.20292. [DOI] [PubMed] [Google Scholar]
- 12.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 13.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text rev. [Google Scholar]
- 14.Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first 10 years of research. Depress Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- 15.Monson CM, Gradus JL, Young-Xu Y, Schnurr PP, Price JL, Schumm JA. Change in posttraumatic stress disorder symptoms: do clinicians and patients agree? Psychol Assess. 2008;20(2):131–138. doi: 10.1037/1040-3590.20.2.131. [DOI] [PubMed] [Google Scholar]
- 16.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research Dept, New York State Psychiatric Institute; 2002. [Google Scholar]
- 17.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 18.Weathers FW, Litz BT, Herman JA, Huska JA, Keane TM. The PTSD Checklist: reliability, validity and diagnostic utility. Proceedings of the 9th Annual Conference of the International Society for Traumatic Stress Studies (ISTSS); San Antonio, TX: ISTSS; 1993. [Google Scholar]
- 19.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory II. San Antonio, TX: Psychological Corp; 1996. [Google Scholar]
- 20.Spielberger CD. State-Trait Anger Expression Inventory. Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- 21.Spielberger CD. Manual for the State-Trait Anxiety Inventory (Form Y) (Self-Evaluation Questionnaire) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 22.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38(1):15–28. [Google Scholar]
- 23.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 24.Straus MA, Hamby SL, McCoy SB, Sugarman DB. The revised Conflict Tactics Scales (CTS2): development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 25.Faul F, Erdfelder E, Lang AG, Buchner AG. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 26.Hedges LV, Olkin I. Statistical Methods for Meta-analysis. London, England: Academic Press; 1985. [Google Scholar]
- 27.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 28.Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162(2):214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- 29.SAS Institute Inc. SAS/STAT User’s Guide, Version 9.2. Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- 30.Shadish WR, Baldwin SA. Meta-analysis of MFT interventions. J Marital Fam Ther. 2003;29(4):547–570. doi: 10.1111/j.1752-0606.2003.tb01694.x. [DOI] [PubMed] [Google Scholar]
- 31.Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychol Bull. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 32.Cason D, Grubaugh A, Resick P. Gender and PTSD treatment: efficacy and effectiveness. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York, NY: Guilford; 2002. pp. 305–333. [Google Scholar]