Abstract
Background
Acute short-term hypothyroidism induced by thyroid hormone withdrawal (THW) for follow-up surveillance or therapeutic radioiodine causes patients with differentiated thyroid cancer to suffer from a myriad of deleterious symptoms.
Objectives
To know how patient recognition of hypothyroid symptoms compares to physician perception of patient symptoms.
Methods
The survey was performed in 10 referral hospitals throughout Korea from December 2010 to May 2011 and targeted patients with total thyroidectomy and remnant ablation. The survey consisted of questions regarding the effect of THW on patient symptoms, the duration of symptoms, impact on social life, and patient complaints. The physicians treating thyroid cancer patients also responded to the survey and provided their perceptions of patient symptoms and treatment decisions.
Results
About 70% of the patients responded that they experienced a negative physical or psychological impact on their life and work due to hypothyroid symptoms. However, 76% of doctors thought hypothyroidism could negatively impact a patient's daily life but would be endurable. Two thirds of physicians do not routinely recommend recombinant human TSH (rhTSH) to their patients. Multivariate analysis showed patients with female sex, stronger educational background, emotionally negative experiences of hypothyroidism, and younger age were more willing to pay for therapy that could prevent hypothyroidism symptoms.
Conclusions
There was a substantial gap in the perception of hypothyroid symptoms during THW between physicians and patients. Physicians who are aware of the seriousness of hypothyroidism in their patients were more likely to recommend the use of rhTSH for their patients.
Key Words: Thyroid cancer, Hypothyroidism, Symptoms, Physicians, Patients
Introduction
For the last 10 years, cases of thyroid cancer have drastically increased, becoming the number one cancer in annual incidence among Korean women in 2008 [1]. In the management of differentiated thyroid cancer (DTC), thyroid hormone withdrawal (THW) has been an essential part of the diagnostic process and treatment to elevate TSH levels using radioactive iodine. However, acute short-term hypothyroidism induced by THW is the most distressing time during follow-up for DTC patients and can result in a myriad of deleterious symptoms and impaired quality of life (QoL) [2,3].
According to the recent clinical practice guidelines, recombinant human TSH (rhTSH) can be used as an alternative to THW for remnant ablation or for surveillance of cancer recurrence during the follow-up period in DTC patients [4,5]. However, in many Asian countries including Korea, using rhTSH in those situations is restricted mainly due to its high costs and reimbursement issues [6]. Given the restrictions surrounding the use of rhTSH, if physicians had a better awareness of potential patient discomfort induced by THW, they might be more inclined to prescribe this medication. However, there have been no studies evaluating patient or physician awareness of acute hypothyroid symptoms during THW in an Asian country. In particular, physician perception of patient symptoms could affect the decision to treat and the disease outcome. Evaluation of the differences between physician and patient perceptions of symptoms induced by the disease itself or during treatment is a very important step in the management of symptoms [7].
The aim of this study was to evaluate the effect of THW for radioiodine therapy or follow-up testing on patient QoL and to determine if there is any difference in the perception of acute hypothyroid symptoms between patients and their doctors.
Patients and Methods
Study Subjects
This survey was prospectively performed in 10 tertiary referral hospitals throughout Korea from December 2010 to May 2011. All enrolled patients underwent total thyroidectomy with or without lymph node dissection and remnant ablation as needed. The patients who had undergone a diagnostic whole body scan (WBS) or radioiodine therapy with THW within the previous 6 months were enrolled in this survey so as to maximize patient ability to recall their symptoms during THW. A total of 700 patients responded to the survey questionnaire in an outpatient setting. The survey questions are provided in the online supplementary questionnaires (for online suppl. material, see www.karger.com/doi/10.1159/000371512).
During the same period, a doctor questionnaire (DQ) was sent via e-mail to 35 physicians treating DTC patients from 20 tertiary hospitals, and they were asked to complete the questionnaire. A total of 35 physicians, composed of 31 endocrinologists, 2 nuclear physicians, and 2 endocrinologist-nuclear physicians, completed the questionnaire.
This study was approved by the institutional review board of each participating hospital. Written informed consent was obtained from all patients.
Statistical Analysis
All data are expressed as number and proportion. A χ2 test or Fisher's exact test was used to compare differences between physical and mental disturbances in men and women. A multivariate logistic regression analysis was used to identify clinical or social factors for the decision as to pay the extra financial costs for avoiding hypothyroidism. p < 0.05 was considered statistically significant. SPSS 13.0 for Windows (SPSS Inc., Chicago, Ill., USA) software was used for data analysis.
Results
Among the 700 eligible patients who participated in the present survey, 532 patients (76.0%) responded to all of the questions and were included in the analysis. The baseline demographics of the study population are presented in the online supplementary table.
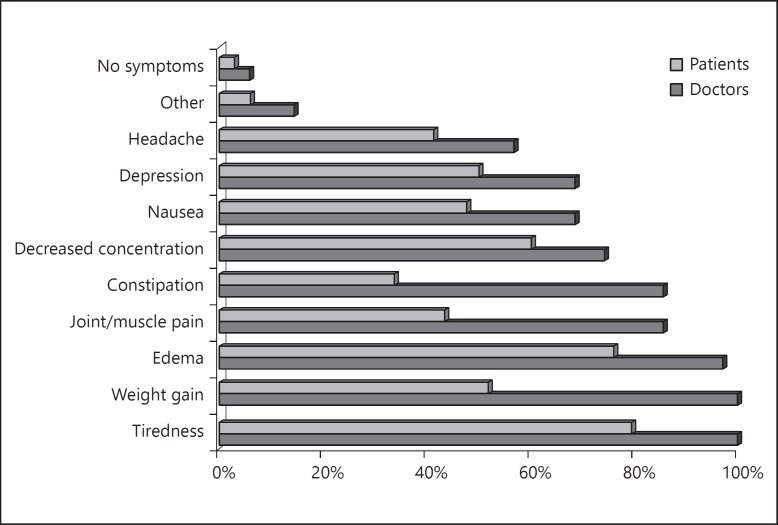
The most frequent patient symptom was fatigue, followed by edema, difficulty in concentration, weight gain, depression, and nausea (in that order; Q6; fig. 1). However, symptoms reported to physicians were fatigue and weight gain, followed by edema, joint/muscle pain, and constipation (DQ2; fig. 1).
Fig. 1.
Symptoms experienced by patients during thyroid hormone discontinuation (Q6, multiple choices selected, gray bar) and doctors' report of patient complaints during thyroid hormone discontinuation (DQ2, multiple choices selected, black bar).
148 patients out of 253 (58.5%) experienced these symptoms for more than 3 weeks, even after resuming thyroid hormone replacement (Q7; table 1). Female patients showed a more delayed recovery than males. Around 70% of patients indicated that the hypothyroid symptoms had a negative impact on daily life, both physically and emotionally, during the discontinuation of thyroid hormone (table 2; Q8, Q9, and Q10). On the other hand, nearly all physicians expected their patients to experience physical (100.0%) and emotional (97.1%) disturbances (table 2; DQ4 and DQ5). No gender differences were observed in terms of experiencing physical discomfort (table 2), but more female patients suffered from emotional or psychological disturbance due to THW than did male patients.
Table 1.
Duration of hypothyroid symptoms during THW and resumption of thyroid hormone (Q7)
| Respondents (n = 253)a | Duration of hypothyroid symptoms |
p | ||
|---|---|---|---|---|
| <2 weeks | 2–4 weeks | >4 weeks | ||
| Patients, n (%) | 105 (41.5) | 80 (31.6) | 68 (26.9) | |
| Age, years | 45.8±11.4 | 48.6±11.1 | 49.2±10.1 | 0.086 |
| Gender (female/total patients), n (%) | 69/105 (65.7) | 65/80 (81.2) | 63/68 (92.6) | 0.000 |
These patients described the exact duration of hypothyroid symptoms in the questionnaire (4.5 ± 5.6 weeks, range: 1–30).
Table 2.
The differences between patient response and physician perception about physical discomfort (Q8/DQ4) and emotional and psychological impacts (Q9/DQ5) induced by THW
| Questions | Response | Patients (n = 532) | Doctors (n = 35) | p |
|---|---|---|---|---|
| Physical discomfort (Q8/DQ4) | no | 150 (28.2) | 0 (0) | 0.001 |
| somewhat | 286 (53.8) | 24 (68.6) | ||
| strong | 96 (18.0) | 11 (31.4) | ||
| Emotional and psychological | no | 171 (32.1) | 1 (2.9) | 0.001 |
| impacts (Q9/DQ5) | somewhat | 285 (53.6) | 26 (74.3) | |
| strong | 76 (14.3) | 8 (22.9) | ||
| Male (n = 113) | Female (n = 419) | |||
| Physical discomfort (Q8) | 73 (64.6) | 309 (73.8) | 0.055 | |
| Emotional and psychological impacts (Q9) | 65 (57.5) | 296 (70.6) | 0.008 | |
Values represent n (%). The differences according to the sex were shown in this table.
Table 3 shows how adequately doctors explained upcoming hypothyroid symptoms and the prevention and alleviation of symptoms to their patients.
Table 3.
Doctor explanations to patients about upcoming hypothyroid symptoms and the prevention and alleviation of symptoms
| Response |
p | ||||
|---|---|---|---|---|---|
| No | Yes, but somewhat | Yes, fully | |||
| Questions to patients (n = 530) | |||||
| Q11 | An explanation about the symptoms by the medical staff before the discontinuation of hormone | 26 (4.9%) | 175 (33.0%) | 329 (62.1%) | 0.081a |
| Q12 | A full explanation about how to prevent and alleviate the symptoms by the medical staff before discontinuation | 95 (17.9%) | 175 (33.0%) | 260 (49.1%) | 0.404b |
| Q13 | Separate treatment to control the symptoms (e.g. over-the-counter drugs or visit to an herbal doctor) | 491 (92.6%) | 39 (7.4%) | ||
| Questions to physicians (n = 35) | |||||
| DQ7 | Actually complaining their symptoms to physicians | 1 (2.9%) | 23 (65.7%) | 11 (31.4%) | |
| DQ8 | Explaining to patients the symptoms which may occur and how to manage them | 4 (11.4%) | 15 (42.9%) | 16 (45.7%) | |
Values represent n (%).
The difference between Q11 and DQ8 was compared using a χ2 test.
The difference between Q12 and DQ8 was compared using a χ2 test.
Doctors believe that their patients' experience of hypothyroid symptoms could negatively impact patients' daily life but that these symptoms are endurable, and two thirds of the doctors would not routinely recommend rhTSH (table 4). Patients prefer to have an alternative to THW to avoid suffering from hypothyroidism (table 5). The more severe the patient symptoms were, whether physical or emotional, the more patients preferred rhTSH as an alternative method to THW (Q7, Q8, and Q14; p = 0.002 and p = 0.000, respectively)
Table 4.
Doctor response to question DQ9 and DQ10
| Questions and answers | n (%) | |
|---|---|---|
| DQ9 | What do you believe about the patient experience of hypothyroidism? | |
| (1) | Most of patients will not experience hypothyroidism | 0 |
| (2) | It will be a little tough but tolerable | 20 (57.1) |
| (3) | It will be a difficult and painful experience | 15 (42.9) |
| (4) | I don't know | 0 |
| DQ10 | Do you think Thyrogen treatment, which may replace the discontinuation of thyroid hormone, can be helpful to patients? | |
| (1) | I think it is helpful and actively recommend it | 1 (2.9) |
| (2) | It is helpful, but I recommend it only to some patients under specific conditions | 22 (62.9) |
| (3) | I give patients two options (discontinuation of hormone or Thyrogen) and let him/her make a decision | 12 (34.3) |
| (4) | I think it is enough to discontinue thyroid hormone | 0 |
Table 5.
Patient response (respondents n = 532) to an alternative way to discontinuing thyroid hormone without suffering hypothyroidism (Q14)
| Response |
|||
|---|---|---|---|
| consider it regardless of expense | consider it if it costs a maximum of USD 1,000 | not consider it at all | |
| Patients, n (%) | 180 (33.8) | 194 (36.5) | 158 (29.7) |
Multivariate logistic regression analysis showed that female sex, stronger educational background, emotionally negative experiences of hypothyroidism, and younger age were significant variables associated with the decision to incur extra financial costs for avoiding hypothyroid symptoms if a method was available (table 6).
Table 6.
Multivariate logistic regression analysis of influencing clinical parameters associated with willingness to incur additional financial costs to avoid hypothyroidism
| Crude OR | 95% CI | Adjusted OR | 95% CI | |
|---|---|---|---|---|
| Age | 0.96 | 0.95–0.98 | 0.98 | 0.96–0.99 |
| Sex (vs. men) | 1.40 | 0.90–2.17 | 1.90 | 1.11–3.26 |
| Having a job | 1.50 | 1.02–2.22 | 1.60 | 0.99–2.59 |
| Stronger educational background | 2.18 | 1.48–3.20 | 1.74 | 1.13–2.67 |
| Experiences of physical discomfort | 2.10 | 1.41–3.13 | 1.32 | 0.80–2.18 |
| Experiences of emotional discomfort | 2.15 | 1.46–3.17 | 1.71 | 1.05–2.78 |
OR = Odds ratio; CI = confidence interval.
Discussion
Acute short-term hypothyroid symptoms during THW for diagnostic WBS or radioiodine therapy are very debilitating and hamper the QoL of patients with DTC [8,9,10,11]. Moreover, socioeconomic burdens including sick leave from work, as well as physical suffering, are markedly increased in all patients undergoing this procedure for thyroid cancer management [12]. To make things worse, some patients experiencing acute short-term hypothyroid symptoms after THW also experience major psychiatric derangements, such as depression or anxiety, and the severity of the disease is comparable to that of patients with major depression requiring regular treatment [11,13].
As considerable time may be needed for thyroid hormone to fully act on transcription and translation of target proteins due to the long half-life of levothyroxine, many patients complain of hypothyroid symptoms several weeks after the reinitiation of the thyroid hormone. Consistent with our results, one previous study showed that the impact of hypothyroidism on sick leave was much higher after, as compared to before, diagnostic WBS, suggesting acute short-term hypothyroid symptoms may be more severe after the readministration of thyroid hormones [12]. Some patients did not recognize that delayed but still noticeable hypothyroid symptoms such as fatigue, edema, and constipation might be attributable to THW because they did not understand the delayed action of thyroid hormone. Therefore, many patients may frequently mistake that other causes such as radioiodine, not hypothyroidism due to THW, might have contributed to their symptoms. This is one reason why patients with thyroid cancer should be informed of their symptoms during and after preparation by THW. It is also why physicians should provide sufficient information and education to their patients.
rhTSH, a recently developed synthetic human thyrotropin, has become a reliable alternative to THW for initial remnant ablation after total thyroidectomy or surveillance with TSH-stimulated thyroglobulin or diagnostic WBS [4,14]. Even though it has shown good efficacy for surveillance or remnant ablation in many previous studies, its wider use has been limited, especially in Asia, due to relatively high costs and potential lack of recognition of patients' complaints by physicians during THW [6].
Our study showed a substantial gap in the level of perception of the severity of acute hypothyroid symptoms between physicians and patients during THW. Usually, doctors have specific knowledge about hypothyroid symptoms and their effects on the body. However, they might not have sufficient recognition regarding the severity of acute hypothyroidism experienced by their patients (table 4). In contrast to this, a more vague overestimation of patients' symptoms by physicians (table 2) was detected from our data, which, however, did not seem to be connected to proper management. On the other hand, one previous report which evaluated QoL in patients with metastatic breast and prostate cancer showed that treating physicians usually underestimate patient symptoms, while patients occasionally rated their symptoms as moderate to severe [15]. This discordance may have an influence on the treatment decision of physicians and could discourage the frequent use of rhTSH in patients with DTC, even though the physicians understand the ability of rhTSH to avoid hypothyroid symptoms, in addition to its diagnostic and therapeutic efficacy.
Around 7% of patients took over-the-counter medication, visited other doctors, or engaged in physical therapy in order to control their various hypothyroidism symptoms, although this supplemental treatment was not reported to the physician (table 3). While most patients received sufficient information from their physicians about hypothyroid symptoms caused by THW, some did not actively consult their physicians about dealing with their symptoms. It is possible that patients regarded their symptoms induced by THW as an unavoidable, ‘must-experience’ process to overcome during treatment or diagnosis, without considering alternative treatment methods, such as rhTSH. We could not posit detailed reasons for such responses from our survey alone. However, this patient belief reflects a greater gap between physicians and patients regarding management of acute hypothyroid symptoms. A more detailed understanding of the relationship based on mutual understanding between physicians and patients is necessary to effectively address patient symptoms.
Younger patients and those with a higher education had a tendency to seek alternatives for alleviating their hypothyroidism. This may be due to a better understanding of acute hypothyroid symptoms and alternative treatments, such as rhTSH injection. More stratified, systematic, and educational approaches for vulnerable patients would be needed to lessen their acute hypothyroid symptoms.
To our knowledge, this is the first report that demonstrates the considerable gap between patients and physicians in recognition of acute hypothyroid symptoms during preparation for diagnostic or therapeutic process with THW. Many physicians in Korea, even if they sufficiently understood the hypothyroid symptoms of their patients, rarely suggested or provided to their patients the proper ways to relieve their symptoms, i.e. all perceptions of morbidity related to severe hypothyroidism did not lead to use of rhTSH. Some physicians might feel pressure to not use a high-cost alternative way compared to inexpensive conventional THW. Others might feel a relief that acute hypothyroid symptoms caused by THW could be endurable to their patients in the middle of thyroid cancer therapy. Passive use of alternative ways could be overcome by active communication between the treating physicians and patients, and by providing both with more accurate information about THW and its therapeutic alternatives.
The present study has some limitations. First, there might be a selection bias due to the fact that only 532 actively responding patients (76.0%) out of 700 respondents were evaluated and data of the remaining 24.0% were dropped from our analysis, due to incompleteness. This could bias the results toward those patients with more aggravated symptoms. Second, previously validated questionnaires for survey of health-related QoL such as the health survey short-form (SF-36) were not used in this study, which may limit the generalizability of patient symptoms and complaints to those with thyroid cancer. The patients should have been asked to grade each symptom, at least, with a visual analogue scale. Third, we could not differentiate discomfort caused by iodine restriction from discomfort caused by acute hypothyroidism during THW. Generally, a low iodine diet might have caused additional discomfort in enduring the hypothyroid symptoms. Lastly, the majority of physicians who participated in the survey were endocrinologists and hence the results of the survey may not reflect the perception of physicians from other specialties (i.e. nuclear physicians, endocrine surgeons) on THW.
In conclusion, many patients with DTC suffer from acute short-term hypothyroid symptoms induced by THW. Treating physicians should more actively consider an alternative way to decrease these symptoms in vulnerable patients, such as using rhTSH.
Disclosure Statement
Dong-Jun Lim received a lecture fee from Genzyme Corporation; otherwise, no competing financial interests exist.
References
- 1.Statistics of National Cancer Registry in 2008. Seoul: National Cancer Center; 2010. [Google Scholar]
- 2.Meier CA, Braverman LE, Ebner SA, Veronikis I, Daniels GH, Ross DS, Deraska DJ, Davies TF, Valentine M, DeGroot LJ, et al. Diagnostic use of recombinant human thyrotropin in patients with thyroid carcinoma (phase I/II study) J Clin Endocrinol Metab. 1994;78:188–196. doi: 10.1210/jcem.78.1.8288703. [DOI] [PubMed] [Google Scholar]
- 3.Dagan T, Bedrin L, Horowitz Z, Chaushu G, Wolf M, Kronenberg J, Talmi YP. Quality of life of well-differentiated thyroid carcinoma patients. J Laryngol Otol. 2004;118:537–542. doi: 10.1258/0022215041615137. [DOI] [PubMed] [Google Scholar]
- 4.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–1214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 5.Pacini F, Castagna MG, Brilli L, Pentheroudakis G. ESMO Guidelines Working Group: Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(suppl 7):vii110–vii119. doi: 10.1093/annonc/mds230. [DOI] [PubMed] [Google Scholar]
- 6.Sundram F, Robinson BG, Kung A, Lim-Abrahan MA, Bay NQ, Chuan LK, Chung JH, Huang SM, Hsu LC, Kamaruddin N, Cheah WK, Kim WB, Koong SS, Lin HD, Mangklabruks A, Paz-Pacheco E, Rauff A, Ladenson PW. Well-differentiated epithelial thyroid cancer management in the Asia Pacific region: a report and clinical practice guideline. Thyroid. 2006;16:461–469. doi: 10.1089/thy.2006.16.461. [DOI] [PubMed] [Google Scholar]
- 7.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 8.Luster M, Felbinger R, Dietlein M, Reiners C. Thyroid hormone withdrawal in patients with differentiated thyroid carcinoma: a one hundred thirty-patient pilot survey on consequences of hypothyroidism and a pharmacoeconomic comparison to recombinant thyrotropin administration. Thyroid. 2005;15:1147–1155. doi: 10.1089/thy.2005.15.1147. [DOI] [PubMed] [Google Scholar]
- 9.Chow SM, Au KH, Choy TS, Lee SH, Yeung NY, Leung A, Leung HL, Shek CC, Law SC. Health-related quality-of-life study in patients with carcinoma of the thyroid after thyroxine withdrawal for whole body scanning. Laryngoscope. 2006;116:2060–2066. doi: 10.1097/01.mlg.0000240287.57704.01. [DOI] [PubMed] [Google Scholar]
- 10.Davids T, Witterick IJ, Eski S, Walfish PG, Freeman JL. Three-week thyroxine withdrawal: a thyroid-specific quality of life study. Laryngoscope. 2006;116:250–253. doi: 10.1097/01.mlg.0000192172.61889.43. [DOI] [PubMed] [Google Scholar]
- 11.Schroeder PR, Haugen BR, Pacini F, Reiners C, Schlumberger M, Sherman SI, Cooper DS, Schuff KG, Braverman LE, Skarulis MC, Davies TF, Mazzaferri EL, Daniels GH, Ross DS, Luster M, Samuels MH, Weintraub BD, Ridgway EC, Ladenson PW. A comparison of short-term changes in health-related quality of life in thyroid carcinoma patients undergoing diagnostic evaluation with recombinant human thyrotropin compared with thyroid hormone withdrawal. J Clin Endocrinol Metab. 2006;91:878–884. doi: 10.1210/jc.2005-2064. [DOI] [PubMed] [Google Scholar]
- 12.Borget I, Corone C, Nocaudie M, Allyn M, Iacobelli S, Schlumberger M, De Pouvourville G. Sick leave for follow-up control in thyroid cancer patients: comparison between stimulation with thyrogen and thyroid hormone withdrawal. Eur J Endocrinol. 2007;156:531–538. doi: 10.1530/EJE-06-0724. [DOI] [PubMed] [Google Scholar]
- 13.Tagay S, Herpertz S, Langkafel M, Erim Y, Bockisch A, Senf W, Gorges R. Health-related quality of life, depression and anxiety in thyroid cancer patients. Qual Life Res. 2006;15:695–703. doi: 10.1007/s11136-005-3689-7. [DOI] [PubMed] [Google Scholar]
- 14.Ladenson PW, Braverman LE, Mazzaferri EL, Brucker-Davis F, Cooper DS, Garber JR, Wondisford FE, Davies TF, DeGroot LJ, Daniels GH, Ross DS, Weintraub BD. Comparison of administration of recombinant human thyrotropin with withdrawal of thyroid hormone for radioactive iodine scanning in patients with thyroid carcinoma. N Engl J Med. 1997;337:888–896. doi: 10.1056/NEJM199709253371304. [DOI] [PubMed] [Google Scholar]
- 15.Wilson KA, Dowling AJ, Abdolell M, Tannock IF. Perception of quality of life by patients, partners and treating physicians. Qual Life Res. 2000;9:1041–1052. doi: 10.1023/a:1016647407161. [DOI] [PubMed] [Google Scholar]