Abstract
Thyroid disorders are common in chronic kidney disease.
The aim:
The purpose of this study was to compare thyroid gland disorders among healthy participants and renal transplant patients and to assess the duration of dialysis on thyroid disorders before transplantation.
Material and methods:
Prospective study during 12 months period included 80 participants divided into two groups. Study group of 40 patients with transplanted kidney was divided in two subgroups, according to the time spent on dialysis (i.e. under and over 72 months). The control group included 40 healthy participants. The exclusion criteria was represented by the previous thyroid disorders and systemic illnesses and treatment with drugs that interfere with thyroid function (amiodarone, propranolol, lithium). The blood samples were taken for standard laboratory analysis, total thyroid hormone levels. Serum level of free thyroxine (T4) and free triiodothyronine (T3) were assayed by RIA using commercially available kits. Subclinical hypothyroidism is defined by the finding of elevated thyroid-stimulating hormone (TSH) > 4.4 mmol/L and normal values of T3 and T4.
Results:
The relative distribution of the functional thyroid disorders is statistically significantly higher in the experimental group: the low T3 syndrome in 12.5% (n = 5) patients (p = 0.017); low T4 syndrome in 7.5% (n = 3) patients (p = 0.072) and subclinical hypothyroidism in 17.5% (n = 7) patients (p = 0.021). There is statistically significant difference in the relative representation (percentage) between respondents to 72 months and respondents over 72 months duration of hemodialysis, namely: low T3 syndrome, which is a higher percentage was recorded in patients up to 72 months duration of dialysis (19.23%), then subclinical hypothyroidism where a greater percentage recorded in subjects over 72 months duration of dialysis (35.71%) before transplantation.
Conclusion:
Considering that we are found in kidney transplant patients a significant link of subclinical hypothyroidism with decreased level of T3 and higher incidence of low T3 syndrome, which are associated with increased cardiovascular mortality and morbidity, and act as markers of survival patients after transplantation, it is necessary to conduct a periodically measuring levels of T3, T4 and TSH in these patients in order to assess the relationship between thyroid dysfunction and mortality risk in this population.
Keywords: thyroid disorders, renal transplant, cardiovascular risk
1. INTRODUCTION
Chronic kidney disease (CKD) are accompanied by numerous metabolic and hormonal disorders which include thyroid function (1).
Subclinical hypothyroidism is defined biochemically as a normal serum free thyroxine (T4) concentration in the presence of an elevated serum thyroid-stimulating hormone (TSH) concentration. Some patients with subclinical hypothyroidism may have vague, non-specific symptoms suggestive of hypothyroidism, but attempts to identify patients clinically have not been successful (1,2). Thus, this disorder can only be diagnosed on the basis of laboratory test results. A substantial proportion of patients with subclinical hypothyroidism eventually develop overt hypothyroidism.
Subclinical hypothyroidism may be associated with an increased risk of cardiovascular disease (CVD), e.g. chronic heart disease (CHD), heart failure. It was also observed also that thyroid dysfunction has a significant impact on renal function or disruptive glomerular and tubular function and mineral metabolism. Hypothyroidism was accompanied by a decrease in glomerular filtration rate, hyponatremia and impaired ability excretion of water (3). Some authors have demonstrated that thyroid dysfunction accelerates and exacerbates pre-existing CKD (4). Level of serum thyroid stimulating hormone (TSH) is usually normal or elevated in CKD, but has reduced response to its releasing hormone (TRH) (3,4,5). In CKD are also disturbed circadian rhythm of TSH and TSH glycosylation (6).
Recent studies have shown the prevalence of subclinical hypothyroidism in 7% of patients with an estimated GFR ≥ 90 mL/min/1.73m2, which increases to 17,9% in patients with GFR <60 mL/min/1.73m2. The prevalence of subclinical hypothyroidism in relation to the general population is 9.6% (7,8), higher in women and it is linked to an increased frequency of high titer of anti-thyroid antibodies (9).
Subclinical primary hypothyroidism in a number of studies was associated with cardiovascular risk (10, 11, 12, 13). Slight changes in the level of TSH can accelerate the development of atherosclerosis in the general population (14). Various authors were reported that subclinical hypothyroidism can induce deterioration of systolic and diastolic heart function, beside traditional risk factors for cardiovascular disease, including blood pressure, lipid profile and endothelial dysfunction (15, 16, 17, 18). Subclinical hypothyroidism was identified as a strong predictor of all-cause mortality in patients with chronic renal failure and risk factor for nephropathy and cardiovascular events in patients with type 2 diabetes (19).
It had been observed also that thyroid dysfunction had a significant impact on renal function and disruption of glomerular and tubular function either metabolism of electrolytes and water. Hypothyroidism was accompanied by a decrease in glomerular filtration rate, hyponatremia and impaired ability excretion of water (20). Some authors have demonstrated that thyroid dysfunction accelerated and exacerbated pre-existing CHD (21).
According to previous researches, the most common thyroid imbalance in renal transplant patients is a low T3 syndrome with FT3 levels generally within the normal limits (22). This reduction is associated with reduced peripheral conversion of T4 to T3, systemic acidosis, the length of dialysis and markers of endothelial dysfunction and inflammation (23, 24, 25). Total and free T3 are acting as markers of survival after renal transplantation (26). Finally, there are reports which concluded that low serum T3 levels before renal transplantation are associated with decreased graft survival (27).
Targher and associates (28) have shown that patients with chronic renal failure with GFR <60 mL/min/1.73 m2 who not require dialysis treatment had subclinical hypothyroidism in 10.7% of cases, while 23.3% of cases had elevated anti-thyroid antibodies. In the analysis of subgroups stratified according to TSH and thyroid antibody titers it was observed greater decline in GFR in relation to the increase in TSH, as well as the increase in titer of anti-thyroid antibodies.
TSH levels according to several study results in patients with CKD are not uniform.
2. RESEARCH GOALS
The aim of this study was to compare types and incidence of thyroid biochemical disorders among healthy participants and renal transplant patients and to assess if it is associated with the duration of dialysis before transplantation.
3. MATERIALS AND METHODS
A prospective single center study in 12 months period included 40 stabile a sample of 80 patients divided into two groups, test and control. In the study group is 40 stable patients with transplanted kidney of which 26 respondents forms a subgroup with duration of hemodialysis to 72 months and 14 patients forms a subgroup with duration of dialysis over 72 months before transplantation. In the control group are 40 patients with normal renal function.
Exclusion criteria were previous thyroid disorders, systemic illnesses, critically ill patients, acute inflammatory diseases.
The values of T3, T4, TSH were measured on the device Abbott Architect i2000. Reference values for TSH are 0.35 to 4.94 mIU/mL. Reference values for T4 are from 63.06 to 150.58 nmol/L, and for T3 are from 0.44 to 0.89 nmol/L. FT4 and FT3 were determined by radioimmunoassay RIA using commercial kits available. The reference values are: FT3 from 2.5 to 5.8 nmol/L, FT4 from 11.5 to 23 pmol/L. Subclinical hypothyroidism is defined by the finding of elevated TSH> 4.4 mmol/L and normal values of T3 and T4 (29). Clinical hypothyroidism is defined by the finding of TSH >10 mmol/L and a decreased level of T3 and T4 (29). Low T3 syndrome is defined by finding T3 <0.89 nmol/L, a low T4 syndrome by finding T4 <63.06 nmol/L and high T4 syndrome by findings T4 >150 nmol/L (30).
Statistical analysis
Data are expressed as means ± standard deviations. Statistical differences in the variables were tested using parametric and non parametric tests where appropriate. The relationship between tested variables was assessed using Spearman correlation coefficients. P values less than 0.05 were considered statistically significant. Data processing software package was used SPSS for Windows.
4. RESULTS
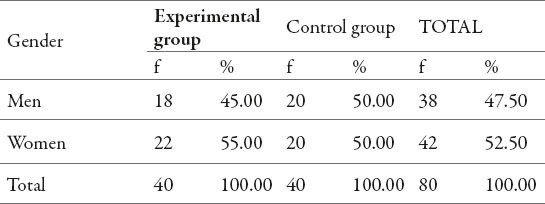
Results presented in Table 1 show that the average age of the experimental group was 53.28 years with an average deviation of 11.76 years, while the average age of the control group was 49.43 years with an average deviation of 7.80 years. Based on the calculated value of p >0.05, we conclude that there is no statistically significant difference in mean age between the experimental and control groups (Table 1).
Table 1.
Number of subjects by gender and belonging to the groups
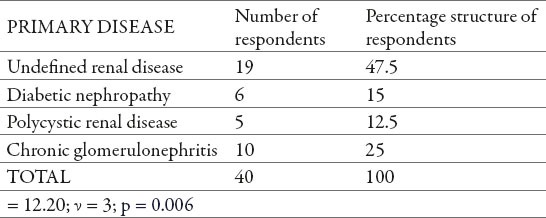
Undefined renal disease was the most common underlying cause of CKD (47%), followed by chronic glomerulonephritis (25%). Diabetic nephropathy and polycystic renal disease were presented in 15% and 13% of patients respectively (Table 2).
Table 2.
Number and percentage structure of the subjects according to the primary disease
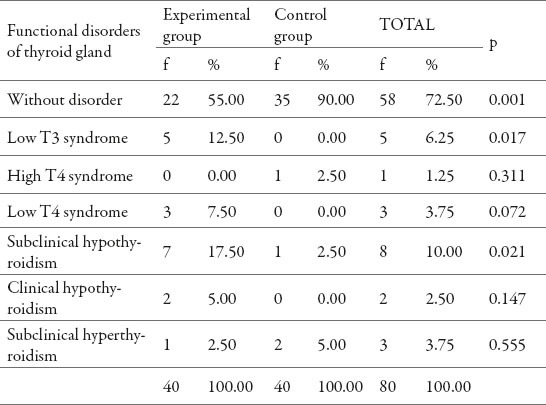
It was found that the relative distribution of the thyroid functional disorders were statistically significantly higher in the experimental group. Thus it was confirmed the low T3 syndrome in 12.5% (n = 5) subjects (p = 0.017); low T4 syndrome in 7.5% (n = 3) patients (p = 0.072) and subclinical hypothyroidism in 17.5% (n = 7) of subjects (p = 0.021), (Table 3).
Table 3.
Absolute and relative frequency of functional disorders of thyroid gland
The research included 40 patients, of which 26 respondents forms a group with duration of hemodialysis to 72 months and 14 patients forms a group with duration of dialysis over 72 months. The remainder of this paper examines the dysfunction of the thyroid gland in the above groups of respondents. The results that were obtained during the study are shown in the Table 4.
Table 4.
Absolute and relative frequency of functional disorders of thyroid gland
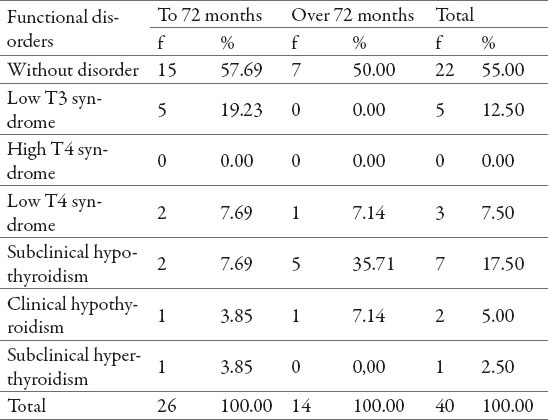
It was found a statistically significant difference in the relative representation (percentage) between patients up to 72 months and patients over 72 months duration of hemodialysis. Low T3 syndrome was found in patients up to 72 months dialysis duration in 19.23% cases. Subclinical hypothyroidism was found in higher percentage in patients who were over 72 months dialysis duration (35.71%), (Figure 1).
Figure 1.
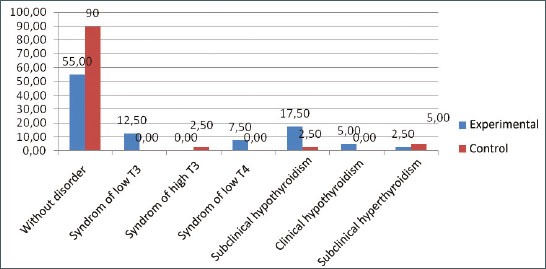
Structure of subjects by thyroid function disorders according to duration of hemodialysis
5. DISCUSSION
The concept of subclinical hypothyroidism was given the importance in the last few decades, with improved methods to detect slight changes in thyroid function tests. TSH levels according to several study results in renal transplant patients are not uniform. In some studies were not found significant differences in mean TSH levels among transplanted and healthy subjects (31).
The results of our study showed that the relative distribution of the thyroid functional disorder were statistically significantly higher in the experimental group than in control group. The low T3 syndrome was found in 12.5% patients (p = 0.017), low T4 syndrome in 7.5% patients (p = 0.072) and subclinical hypothyroidism in 17.5% of patients (p = 0.021).
Our study found that low T3 syndrome presented in 19,23% patients who underwent hemodialysis up to 72 months, while subclinical hypothyroidism was presented in higher percentage in patients who were on hemodialysis treatment more than 72 months (35.71%).
Undefined renal disease was the most common underlying cause of CKD (47%), followed by chronic glomerulonephritis (25%). Diabetic nephropathy and polycystic kidney disease was presented in 15% and 13% of patients, respectively.
Function disorders and thyroid gland in CHD are common but unrecognized problem. Song et associates (32) examined the prevalence of decreased T3 levels in patients in different stages of CHD. This retrospective study included 2.284 patients with normal TSH level, and it concluded that in these patients, there is a positive correlation between GFR and the level of T3 which is in accordance with our study.
In study of Conchol et associates (33) were included 3.089 adult renal transplant patients with conclusion that subclinical primary hypothyroidism was relatively common in these patients (18%) and was positively correlated with decline in GFR. Concomitant diseases of the thyroid gland in patients after renal transplantation have been identified as a strong risk factor for cardiovascular disease and a predictor of all-cause mortality, which is a major health and financial problem (34).
6. CONCLUSION
The results of this study showed that functional thyroid gland disorders were more common among renal transplant patients compared with healthy subjects, and reveal their link with time on dialysis. We found a significant link of subclinical hypothyroidism with decreased level of T3 and higher incidence of low T3 syndrome in the transplant renal patients compare to control group. It is necessary to screen thyroid hormone levels in these patients periodically in order to check thyroid gland function and to assess the relationship between thyroid dysfunction and mortality risk.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Adler SM, Wartofsky L. The nonthyroidal illness syndrome. Endocrinology and Metabolism Clinics of North America. 2007:657–672. doi: 10.1016/j.ecl.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Bemben DA, Hamm RM, Morgan L. Thyroid disease in the elderly. Part 2. Predictability of subclinical hypothyroidism. J Fam Pract. 1994;38(6):577–582. [PubMed] [Google Scholar]
- 3.Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. Arch Intern Med. 2000;160(4):526–534. doi: 10.1001/archinte.160.4.526. [DOI] [PubMed] [Google Scholar]
- 4.Kanaya AM, Harris F, Volpato S, Pérez-Stable EJ, Harris T, Bauer DC. Association between thyroid dysfunction and total cholesterol level in an older biracial population: the health, aging and body composition study. Arch Intern Med. 2002;162(7):773–779. doi: 10.1001/archinte.162.7.773. [DOI] [PubMed] [Google Scholar]
- 5.Bell RJ, Rivera-Woll L, Davison SL, Topliss DJ, Donath S, Davis SR. Well-being, health-related quality of life and cardiovascular disease risk profile in women with subclinical thyroid disease–a community-based study. Clin Endocrinol (Oxf) 2007;66(4):548–556. doi: 10.1111/j.1365-2265.2007.02771.x. [DOI] [PubMed] [Google Scholar]
- 6.Parle JV, Franklyn JA, Cross KW. Prevalence and follow-up of abnormal thyrotrophin (TSH) concentrations in the elderly in the United Kingdom. Clin Endocrinol. (Oxf) 1991;34(1):77–83. doi: 10.1111/j.1365-2265.1991.tb01739.x. [DOI] [PubMed] [Google Scholar]
- 7.Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008;29(1):76–131. doi: 10.1210/er.2006-0043. [DOI] [PubMed] [Google Scholar]
- 8.Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012;379(9821):1142–1154. doi: 10.1016/S0140-6736(11)60276-6. [DOI] [PubMed] [Google Scholar]
- 9.Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, Pessah-Pollack R, Singer PA, Woeber KA. American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22(12):1200–1235. doi: 10.1089/thy.2012.0205. [DOI] [PubMed] [Google Scholar]
- 10.Hak AE, Pols HA, Visser TJ. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med. 2000;132(4):270–278. doi: 10.7326/0003-4819-132-4-200002150-00004. [DOI] [PubMed] [Google Scholar]
- 11.Lindeman RD, Romero LJ, Schade DS. Impact of subclinical hypothyroidism on serum total homocysteine concentrations, the prevalence of coronary heart disease (CHD), and CHD risk factors in the New Mexico Elder Health Survey. Thyroid. 2003;13(6):595–600. doi: 10.1089/105072503322238863. [DOI] [PubMed] [Google Scholar]
- 12.Imaizumi M, Akahoshi M, Ichimaru S, Nakashima E, Hida A, Soda M, Usa T, Ashizawa K, Yokoyama N, Maeda R, Nagataki S, Eguchi K. Risk for ischemic heart disease and all-cause mortality in subclinical hypothyroidism. J Clin Endocrinol Metab. 2004;89(7):3365–3370. doi: 10.1210/jc.2003-031089. [DOI] [PubMed] [Google Scholar]
- 13.Vanderpump MP, Tunbridge WM. Epidemiology and Prevention of Clinical and Subclinical Hypothyroidism. Thyroid. 2002;12(10):839–847. doi: 10.1089/105072502761016458. [DOI] [PubMed] [Google Scholar]
- 14.Bando Y, Ushiogi Y, Okafuji K, Toya D, Tanaka N, Miura S. Non-autoimmune primary hypothyroidism in diabetic and non-diabetic chronic renal dysfunction. Exp Clin Endocrinol Diabetes. 2002;110(8):408–415. doi: 10.1055/s-2002-36427. [DOI] [PubMed] [Google Scholar]
- 15.Razvi S, Weaver JU, Vanderpump MP, Pearce SH. The incidence of ischemic heart disease and mortality in people with subclinical hypothyroidism: reanalysis of the Whickham Survey cohort. J Clin Endocrinol Metab. 2010;95(4):1734–1740. doi: 10.1210/jc.2009-1749. [DOI] [PubMed] [Google Scholar]
- 16.Rodondi N, Newman AB, Vittinghoff E, de Rekeneire N, Satterfield S, Harris TB, Bauer DC. Subclinical hypothyroidism and the risk of heart failure, other cardiovascular events, and death. Arch Intern Med. 2005;165(21):2460–2466. doi: 10.1001/archinte.165.21.2460. [DOI] [PubMed] [Google Scholar]
- 17.Cappola AR, Fried LP, Arnold AM, Danese MD, Kuller LH, Burke GL, Tracy RP, Ladenson PW. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA. 2006;295(9):1033–1041. doi: 10.1001/jama.295.9.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyland KA, Arnold AM, Lee JS, Cappola AR. Persistent subclinical hypothyroidism and cardiovascular risk in the elderly: the cardiovascular health study. J Clin Endocrinol Metab. 2013;16(324):533–540. doi: 10.1210/jc.2012-2180. 98(2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, Asvold BO, Iervasi G, Imaizumi M, Collet TH, Bremner A, Maisonneuve P, Sgarbi JA, Khaw KT, Vanderpump MP, Newman AB, Cornuz J, Franklyn JA, Westendorp RG, Vittinghoff E, Gussekloo J Thyroid Studies Collaboration. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304(12):1365–1374. doi: 10.1001/jama.2010.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gencer B, Collet TH, Virgini V, Bauer DC, Gussekloo J, Cappola AR, Nanchen D, den Elzen WP, Balmer P, Luben RN, Iacoviello M, Triggiani V, Cornuz J, Newman AB, Khaw KT, Jukema JW, Westendorp RG, Vittinghoff E, Aujesky D, Rodondi N Thyroid Studies Collaboration. Subclinical thyroid dysfunction and the risk of heart failure events: an individual participant data analysis from 6 prospective cohorts. Circulation. 2012;126(9):1040–1049. doi: 10.1161/CIRCULATIONAHA.112.096024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008;29(1):76–131. doi: 10.1210/er.2006-0043. [DOI] [PubMed] [Google Scholar]
- 22.Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado Thyroid Disease Prevalence Study. Arch Intern Med. 2000;160(4):526–534. doi: 10.1001/archinte.160.4.526. [DOI] [PubMed] [Google Scholar]
- 23.Iglesias P, Diez JJ. Thyroid dysfunction and kidney disease. Eur J Endocrinol. 2009;160(4):503–515. doi: 10.1530/EJE-08-0837. [DOI] [PubMed] [Google Scholar]
- 24.Helfand M, Crapo LM. Screening for thyroid disease. Ann Intern Med. 1990;112(11):840–849. doi: 10.7326/0003-4819-112-11-840. [DOI] [PubMed] [Google Scholar]
- 25.Enia G, Panuccio V, Cutrupi S, Pizzini P, Tripepi G, Mallamaci F, Zoccali C. Subclinical hypothyroidism is linked to micro-inflammation and predicts death in continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant. 2007;22(2):538–544. doi: 10.1093/ndt/gfl605. [DOI] [PubMed] [Google Scholar]
- 26.Lebkowska U, Malyszko J, Mysliwiec M. Thyroid function and morphology in kidney transplant recipients, hemodialyzed, and peritoneally dialyzed patients. Transplant Proc. 2003;35(8):2945–2948. doi: 10.1016/j.transproceed.2003.10.066. [DOI] [PubMed] [Google Scholar]
- 27.Song HS, Kwak IS, Lee DW, Kang YH, Seong EY, Park JS. The prevalence of low triiodothyronine according to the stage of chronic kidney disease in subjects with a normal thyroid-stimulating hormone. Nephrol Dial Transplant. 2009;24(5):1534–1538. doi: 10.1093/ndt/gfn682. [DOI] [PubMed] [Google Scholar]
- 28.Targher G, Chonchol M, Zoppini G, Salvagno G, Pichiri I, Franchini M, Lippi G. Prevalence of thyroid autoimmunity and subclinical hypothyroidism in persons with chronic kidney disease not requiring chronic dialysis. Clin Chem Lab Med. 2009;47(11):1367–1371. doi: 10.1515/CCLM.2009.304. [DOI] [PubMed] [Google Scholar]
- 29.den Hollander JG, Wulkan RW, Mantel MJ, Berghout A. Correlation between severity of thyroid dysfunction and renal function. Clin Endocrinol (Oxf) 2005;62(4):423–427. doi: 10.1111/j.1365-2265.2005.02236.x. [DOI] [PubMed] [Google Scholar]
- 30.Helfand M, Crapo LM. Screening for thyroid disease. Ann Intern Med. 1990;112(11):840–849. doi: 10.7326/0003-4819-112-11-840. [DOI] [PubMed] [Google Scholar]
- 31.Kaptein EM, Quion-Verde H, Massry SG. Hemodynamic effects of thyroid hormone. Contrib Nephrol. 1984;41:151–159. doi: 10.1159/000429278. [DOI] [PubMed] [Google Scholar]
- 32.Singh PA, Bobby Z, Selvaraj N, Vinayagamoorthi R. An evaluation of thyroid hormone status and oxidative stress in undialyzed chronic renal failure patients. Indian J Physiol Pharmacol. 2006;50(3):279–284. [PubMed] [Google Scholar]
- 33.Song HS, Kwak IS, Lee DW, Kang YH, Seong EY, Park JS. The prevalence of low triiodothyronine according to the stage of chronic kidney disease in subjects with a normal thyroid-stimulating hormone. Nephrol Dial Transplant. 2009;24(5):1534–1538. doi: 10.1093/ndt/gfn682. [DOI] [PubMed] [Google Scholar]
- 34.Chonchol M, Lippi G, Salvagno G, Zoppini G, Muggeo M, Targher G. Prevalence of subclinical hypothyroidism in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2008;3(5):1296–1300. doi: 10.2215/CJN.00800208. [DOI] [PMC free article] [PubMed] [Google Scholar]


