Abstract
Purpose of review
This review focuses on recent studies of osteoarthritis epidemiology, including research on prevalence, incidence, and a broad array of potential risk factors at the person level and joint level.
Recent findings
Studies continue to illustrate the high impact of osteoarthritis worldwide, with increasing incidence. Person-level risk factors with strong evidence regarding osteoarthritis incidence and/or progression include age, sex, socioeconomic status, family history, and obesity. Joint-level risk factors with strong evidence for incident osteoarthritis risk include injury and occupational joint loading; the associations of injury and joint alignment with osteoarthritis progression are compelling. Moderate levels of physical activity have not been linked to increased osteoarthritis risk. Some topics of high recent interest or emerging evidence for association with osteoarthritis include metabolic pathways, vitamins, joint shape, bone density, limb length inequality, muscle strength and mass, and early structural damage.
Summary
Osteoarthritis is a complex, multifactorial disease, and there is still much to learn regarding mechanisms underlying incidence and progression. However, there are several known modifiable and preventable risk factors, including obesity and joint injury; efforts to mitigate these risks can help to lessen the impact of osteoarthritis.
Keywords: epidemiology, incidence, osteoarthritis, prevalence, risk factors
INTRODUCTION
Osteoarthritis is one of the most common chronic health conditions and a leading cause of pain and disability among adults [1–5], impacting many health outcomes [6–10]. This review builds upon previous comprehensive reviews of osteoarthritis epidemiology [11–13] by focusing on new research since 2013. Similarly to other reviews [11,12], potential risk factors are grouped according to person-level and joint-level characteristics. Genetic factors are covered in a separate article in this issue.
OSTEOARTHRITIS PREVALENCE AND INCIDENCE
Although osteoarthritis prevalence and incidence estimates have varied somewhat across studies [11,12], there is agreement that a substantial proportion of adults are affected. Recent cohort and community-based studies [14–20,21▪,22▪▪] have further documented the prevalence of osteoarthritis at different joints, based on radiographic findings and/or patient report. The following are highlights from these studies.
Hip
In one of few prevalence studies of hip osteoarthritis, the age-standardized prevalences of radiographic and symptomatic hip osteoarthritis were 19.6% [95% confidence interval (CI) = 16.7, 23.0%] and 4.2% (95% CI = 2.9, 6.1%), respectively, in the Framingham Study Community Cohort; men had higher prevalence of radiographic but not symptomatic hip osteoarthritis than women [14].
Knee
Among a cohort of adults (age 56–84) in Malmo, Sweden, the prevalences of radiographic and symptomatic knee osteoarthritis were 25.4% (95% CI = 24.1, 26.1) and 15.4% (95% CI = 14.2, 16.7), respectively [23]; the latter is comparable with similarly aged cohorts [11,12].
Foot
A review of midfoot and forefoot osteoarthritis found that most studies focused on radiographic osteoarthritis, with wide variability in prevalence estimates (0.1–61%) based on age, sex, and joint(s) studied [18]. Well controlled population studies are still needed to understand the prevalence and risk factors for foot osteoarthritis.
Multiple joints
Based on a 72% response rate from over 26 000 adults at least 50 years in England who completed mailed surveys [21▪], about half reported having osteoarthritis in at least one of four joint regions (hand, hip, foot, knee), and about 22% reported disabling osteoarthritis. As part of the Global Burden of Disease 2010 study, a systematic review reported that the global age-standardized prevalence of knee osteoarthritis was 3.8%, and hip osteoarthritis was 0.85% [22▪▪]; of almost 300 health conditions studied, osteoarthritis was the 11th highest contributor to disability.
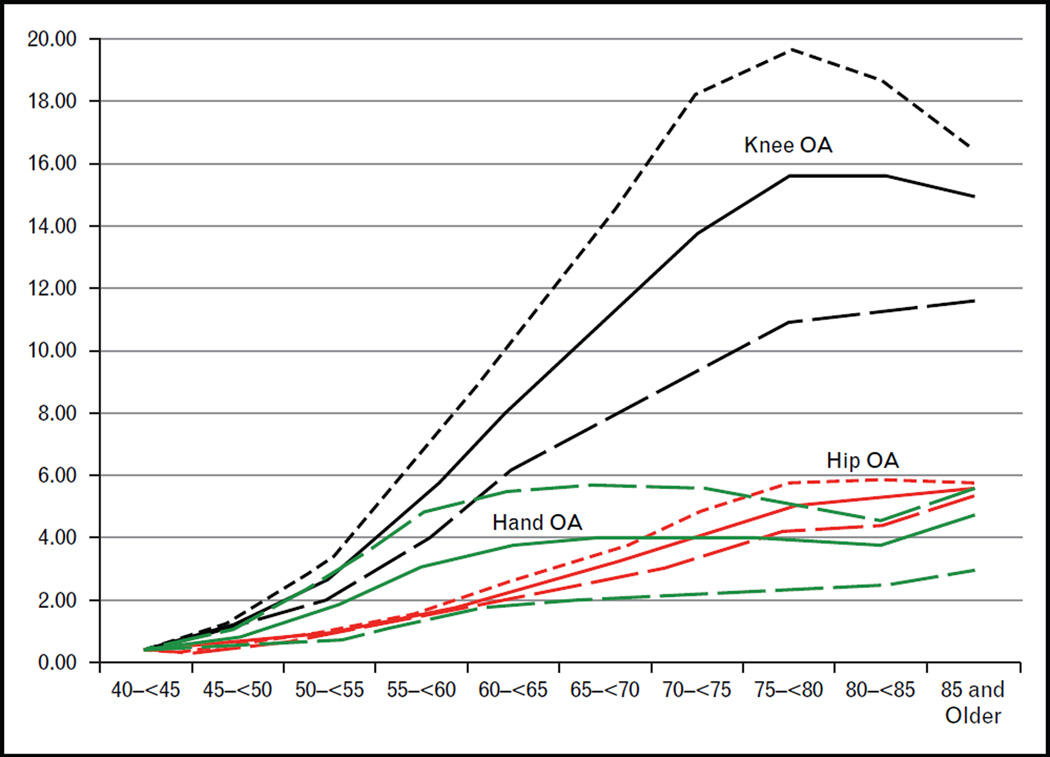
An increasing number of studies [24,25▪▪,26,27] have utilized large health administrative databases to document osteoarthritis incidence. For example, based on 18 years of health records from British Colombia, Canada, the crude incidence rate of osteoarthritis was 14.6 (95% CI = 14.0, 14.8) per 1000 person-years in 2000/2001, rising 2.5–3.3% per year through 2008/2009 [25▪▪]. Primary care health records from over 3 million patients in northeast Spain showed that incidence rates per 1000 personyears (99%CIs) for knee, hip, and hand osteoarthritis were 6.5 (6.4, 6.6), 2.1 (2.0–2.1), and 2.4 (2.4–2.4) (Fig. 1) [26]. Although ascertaining osteoarthritis using administrative health records is challenging (e.g. limitations in coding accuracy, establishing valid case definitions), these studies demonstrate the strong potential of these databases to estimate the population burden and trends in osteoarthritis.
FIGURE 1.
Age and sex-specific incidence rates (/1000 person-years) of knee osteoarthritis (black), hip osteoarthritis (red), and hand osteoarthritis (green). Solid, all population; short dash line, women; long dash line, men. Reproduced from [26].
PERSON-LEVEL RISK FACTORS
The following are person-level risk factors with some evidence for association with osteoarthritis onset and/or progression.
Demographic characteristics and family history
Many studies have documented that osteoarthritis risk is greater among females and with increasing age [11,12], and some studies have shown an increased risk with lower socioeconomic status [28–30] and African American race [31,32]. Adding to prior data showing a considerable genetic and family history component to osteoarthritis, two new studies showed that having a parent with total knee replacement was associated with greater knee pain prevalence and worsening [33], as well as greater medial joint space narrowing over time [34].
Obesity and metabolic syndrome
Obesity is a key risk factor for knee osteoarthritis, increasing the risk three-fold, and evidence suggests that obesity accelerates progression of knee osteoarthritis [11,12,35]; recent work has enhanced this body of literature [36–38]. In a cohort study [39] of US women, higher baseline serum leptin was associated with greater odds of severe knee joint damage on MRI after 10 years, adjusting for BMI and other factors. Another study [40▪▪] of older adults found that almost half of the association between BMI and knee osteoarthritis was explained by leptin levels. These studies illustrate evidence for a metabolic/inflammatory pathway between obesity and osteoarthritis. A systematic review also found strong evidence for higher serum lipids and moderate evidence for obesity as risk factors for knee bone marrow lesions among individuals with asymptomatic preosteoarthritis and established osteoarthritis [41▪▪]; the finding regarding serum lipids, if confirmed, could represent an important early modifiable risk factor. Interestingly, a case–control study [42] found that statin use was associated with a lower prevalence of generalized osteoarthritis, although results of other studies regarding statin use have been mixed. Another study [43] supported the beneficial effect of weight loss or maintenance to improve osteoarthritis symptoms, finding that among a group of obese individuals, percentage change in weight was significantly associated with changes in medial tibial cartilage volume and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) WOMAC scores.
Both earlier data and recent research have also shown an association of obesity with hand osteoarthritis [11,12,44], suggesting a metabolic or inflammatory role of obesity. A Netherlands-based cohort study [45] found that percentage body fat, fat mass, and waist-to-hip ratio were all associated with hand osteoarthritis; visceral adipose tissue was associated with hand osteoarthritis in men only. The association of obesity with hip osteoarthritis has been weak and inconsistent across studies [11,12].
Nutritional and vitamin factors
The role of dietary factors in osteoarthritis has been a very active area of recent research. Among Osteoarthritis Initiative (OAI) participants, greater baseline milk intake was associated with less joint space narrowing over 4 years among women [46]. Previous studies of vitamin D and osteoarthritis have been conflicting [11,12], and a clinical trial showed no effect of vitamin D supplementation on knee cartilage loss [47]. However, two recent studies [48▪,49] of individuals with osteoarthritis showed an association between vitamin D deficiency and greater progression of symptoms and joint space progression; the latter was accentuated among individuals with high parathyroid hormone. Building on prior studies [11,12] suggesting an association of low vitamin K with osteoarthritis, a study [50] of older adults found that those with low plasma phylloquinone (vitamin K1) were more likely to have articular cartilage and meniscus damage progression on MRI over 3 years than those with sufficient levels. A protective effect of higher circulating vitamin C and E levels with osteoarthritis risk and progression has been suggested, but results have been inconsistent [11,12]. A longitudinal study of the Multicenter Osteoarthritis Study (MOST) cohort found that those in the highest tertile of circulating vitamin C actually had greater incidence of radiographic knee osteoarthritis [adjusted odds ratio (OR) = 2.20, 95% CI 1.12, 4.33] compared with the lowest tertile, with similar findings for vitamin E (adjusted OR = 1.89, 95% CI 1.02, 3.50) [51]. Overall additional research is needed to clarify the role of vitamins and other dietary factors with respect to osteoarthritis risk and outcomes.
Bone density and bone mass
Previous research identified high bone density as a risk factor for incident osteoarthritis [12], although mechanisms and a direct causal relationship remain unclear. Two recent studies [52▪,53▪] found that individuals with extreme high bone mass had greater prevalence of radiographic hip and knee osteoarthritis than control populations. Because high bone mass is likely a lifelong genetic trait, with osteoarthritis being a disease that occurs later in life, this study supports a role of high bone mass in osteoarthritis development. These studies also confirmed previous research showing that high bone mass was more strongly associated with subchondral bone sclerosis than with joint space narrowing, suggesting a hypertrophic osteoarthritis phenotype.
Smoking
A review summarized studies on the association of smoking with osteoarthritis [54], updating a meta-analysis that found an inverse association, except in cohort studies [55]. Overall this review concluded that research to date (including one recent study [56]) suggests smoking confers moderate protection for knee and hip osteoarthritis. However, smokers have a somewhat increased risk for painful osteoarthritis [55].
Other person-level risk factors
Two recent studies [57,58] examined the association of low birth weight with osteoarthritis. In an Australian cohort, both low birth weight and pre-term birth were associated with increased adjusted risk of future hip arthroplasty (but not knee arthroplasty) [57]. In the Hertfordshire Cohort Study, individuals with lower birth weight were more likely to have hip osteophytes. Although the mechanisms of the low birth weight and osteoarthritis association are not understood, this high-risk group should be monitored for other osteoarthritis risk factors and early symptoms. Prior studies [59–62] have examined the association of index-to-ring finger length ratio, an indicator for prenatal testosterone exposure, with osteoarthritis, showing mixed results for knee osteoarthritis and no association for hip osteoarthritis. A Melbourne-based cohort study [63] recently showed that lower index-to-ring finger ratio was associated with knee but not hip replacement (proxies for severe osteoarthritis).
JOINT-LEVEL RISK FACTORS
The following are joint-level risk factors with some evidence for association with osteoarthritis onset and/or progression.
Bone/joint shape
There has been increasing interest in the role of joint shape in osteoarthritis risk, with prior research showing an association of proximal femur shape with incident hip osteoarthritis [12]. Two recent studies [64,65▪] used active shape modeling to examine the association of proximal femur shape with osteoarthritis. In the Johnston County osteoarthritis Project, proximal femur shape differed between hips with incident osteoarthritis and control hips, but only among men [64]. Among OAI participants, ipsilateral proximal femur shape differed between prevalent case and control knees for both medial and lateral osteoarthritis [65▪]. In the MOST study [66▪], knees with lateral compartment osteoarthritis were associated with reduced femoral offset and increased hip height center, more valgus neck-shaft angle, and increased abductor angle compared with knees without osteoarthritis; women also had reduced femoral offset and more valgus neck-shaft angle than men, potentially clarifying sex differences in prevalence of lateral tibiofemoral osteoarthritis. Findings from another study [67] supported femoroacetabular impingement and acetabular dysplasia in the development of radiographic hip osteoarthritis and total hip arthroplasty, specifically among women.
Injury
Traumatic joint injury is a major risk factor for osteoarthritis, particularly at the knee (i.e. meniscal damage, anterior cruciate ligament rupture, or direct articular cartilage injury) [68–73] and ankle [74–76]. A recent systematic review of 20 studies supported the injury-osteoarthritis link by demonstrating that patients with anterior cruciate ligament (ACL) deficient and reconstructed knees had altered synovial fluid biomarker levels indicative of osteoarthritis, compared with controls [77▪]. Notably, injury may rapidly accelerate joint disease, as shown by an analysis of OAI data [78];among participants without baseline knee osteoarthritis, prior knee injury was associated with accelerated progression to end-stage radiographic knee osteoarthritis in 48 months (OR 9.22, 95% CI 4.50, 18.90).
Surgical reconstruction as a strategy to protect against knee osteoarthritis is questionable. In the National Swedish Patient Register [79], the hazard of knee osteoarthritis over an average of 9 years was higher among patients with reconstructed cruciate ligament injury than those treated nonoperatively (hazard ratio 1.42, 95% CI 1.27–1.58). In a study of administrative databases in Ontario, Canada [74], the cumulative incidence of knee arthroplasty over 15 years was seven times greater among patients with cruciate ligament reconstruction (1.4%) than matched control participants (0.2%, P < 0.001).
Muscle strength and mass
Associations between muscle strength and osteoarthritis have varied, based on specific muscles and joints examined [11,12], with recent reviews concluding that muscle weakness may confer risk for knee osteoarthritis onset and progression [80,81▪]. Among OAI participants with early radiographic knee osteoarthritis in one limb, there were no differences in muscle strength or cross-sectional area between the affected and unaffected limbs [82]. In the full OAI cohort, isometric knee extensor and flexor strength were significantly lower for symptomatic vs. asymptomatic knees, but these strength measures did not differ by radiographic severity [83]. A third OAI study [84] found that among women, frequently painful knees had greater intramuscular fat areas than contralateral pain-free knees. Whereas the specific role of muscle strength and mass in osteoarthritis structural development and progression is still somewhat unclear, muscle strength appears to play a role in knee symptoms.
Joint loads and alignment
A large body of literature addresses the role of static and dynamic alignment in knee osteoarthritis [11,12,85–87]. Although knee alignment is a clear predictor of knee osteoarthritis progression [88], findings are inconsistent for knee osteoarthritis incidence [89]. A recent study [86] of overweight women without knee osteoarthritis found an association of varus alignment with incident radiographic but not symptomatic knee osteoarthritis. A meta-analysis reported greater odds of structural knee osteoarthritis progression with increasing knee adduction moment [87]. Hallux valgus (malalignment and medial enlargement of the first metatarsophalangeal joint) has been linked with osteoarthritis in the first metatarsophalangeal joint [90], as well as knee and hip osteoarthritis [91].
Occupation and physical activity
A number of previous studies [11,12] have shown that occupational tasks involving abnormal or excessive lower extremity joint loading are associated with risk for hip and knee osteoarthritis. Moderate levels of physical activity have not been associated with osteoarthritis risk [11,12], and a new study [92▪] from the Johnston County Osteoarthritis Project reported that individuals who met physical activity recommendations were not more likely to have either radiographic or symptomatic osteoarthritis than those who were less active.
Leg length inequality
Although there were no new studies published on the association between leg length inequality (LLI) and osteoarthritis in 2014, prior studies from the Johnston County Osteoarthritis Project [93–95] and MOST [96] suggest an important relationship between LLI and prevalent radiographic knee osteoarthritis, particularly in the shorter limb. The link of LLI with osteoarthritis should be further examined, particularly because prior follow-up times were likely too short to evaluate disease development and progression.
Other joint-level risk factors
Several new studies [97▪,98,99,100▪▪,101▪▪] have focused on the predictive value of other patient-reported and/or knee structural characteristics on osteoarthritis risk and outcomes. Greater infrapatellar fat pad maximal area was significantly and beneficially associated with change in knee pain, tibial cartilage volume, and risk of medial cartilage defects among women over about 2.5 years [97▪]. Among women in the Rotterdam study [98], knee crepitus was associated with MRI features of osteoarthritis in the patellofemoral but not tibiofemoral compartment. Among OAI participants without radiographic osteoarthritis evidence, MRI lesions were associated with prevalent and incident persistent knee symptoms and incident cartilage damage [100▪▪]. Another study [101▪▪] reported that minor baseline radiographic changes significantly improved prediction of knee osteoarthritis risk, beyond an initial model including age, sex, and BMI; other questionnaires, genetic and biomarker data only modestly improved prediction.
CONCLUSION
Recent research has continued to highlight the complex nature of osteoarthritis, with confirmed or likely risk factors including demographic characteristics, obesity and dietary factors, joint loading and injury, and joint shape and alignment. Some studies [45,46,49,64,66▪,97▪,102] have highlighted interactions among these risk factors (mostly surrounding sex differences in other osteoarthritis risk factors); given the multifactorial nature of osteoarthritis, future research should carefully consider these interrelationships. Also important is the existence of multiple known modifiable or preventable risk factors for osteoarthritis incidence and/or progression (e.g. obesity, joint injury); efforts are needed to help individuals mitigate these risks, in tandem with continued research that further elucidates the mechanisms underlying osteoarthritis development.
KEY POINTS.
Traditional epidemiologic studies and mining of large health administrative databases show a large and increasing impact of osteoarthritis.
Risk factors with strong evidence for osteoarthritis onset and/or progression include age, sex, socioeconomic status, obesity, family history, joint injury, joint alignment, and occupational joint loading.
Risk factors with emerging interest or evidence for osteoarthritis onset and/or progression include metabolic pathways (e.g. serum leptin), vitamins, joint shape, bone density, limb length inequality, muscle strength and mass, and early structural damage.
Osteoarthritis is complex and multifactorial; future epidemiologic studies should give careful consideration to interrelationships among potential risk factors.
Acknowledgements
None.
Financial support and sponsorship
Drs. Allen and Golightly receive grant funding from the Department of Veterans Affairs, Health Services Research and Development and Rehabilitation Research and Development (Allen); Patient Centered Outcomes Research Institute (Allen, Golightly); National Institute of Musculoskeletal and Skin Diseases (Allen, Golightly); National Center for Advancing Translational Sciences/National Institutes of Health KL2TR001109/ UL1TR001111 (Golightly).
Footnotes
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
- 1.Song J, Chang RW, Dunlop D. Population impact of arthritis on disability in older adults. Arthritis Rheum. 2006;55:248–255. doi: 10.1002/art.21842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation: United States, 2007–2009. MMWR Morb Mortal Wkly Rep. 2010;59:1261–1265. [PubMed] [Google Scholar]
- 4.McDonough CM, Jette AM. The contribution of osteoarthritis to functional limitations and disability. Clin Geriatr Med Aug. 2010;26:387–399. doi: 10.1016/j.cger.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28:5–15. doi: 10.1016/j.berh.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 6.McCurry SM, Von Korff M, Vitiello MV, et al. Frequency of comorbid insomnia, pain, and depression in older adults with osteoarthritis: predictors of enrollment in a randomized treatment trial. J Psychosom Research. 2011;71:296–299. doi: 10.1016/j.jpsychores.2011.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation: United States, 2010–2012. MMWR Morb Mortal Wkly Rep. 2013;62:869–873. [PMC free article] [PubMed] [Google Scholar]
- 8.Theis KA, Murphy L, Hootman JM, et al. Prevalence and correlates of arthritis-attributable work limitation in the US population among persons ages 18–64: 2002 National Health Interview Survey data. Arthritis Rheum. 2007;57:355–363. doi: 10.1002/art.22622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furner SE, Hootman JM, Helmick CG, et al. Health-related quality of life of US adults with arthritis: analysis of data from the behavioral risk factor surveillance system, 2003, 2005, and 2007. Arthritis Care Res. 2011;63:788–799. doi: 10.1002/acr.20430. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Arthritis as a potential barrier to physical activity among adults with obesity. MMWR Morb Mortal Wkly Rep. 2011;60:614–618. [PubMed] [Google Scholar]
- 11.Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28:5–15. doi: 10.1016/j.berh.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Neogi T, Zhang Y. Epidemiology of osteoarthritis. Rheum Dis Clin North Am. 2013;39:1–19. doi: 10.1016/j.rdc.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silverwood V, Blagojevic-Bucknall M, Jinks C, et al. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2014 doi: 10.1016/j.joca.2014.11.019. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Kim C, Linsenmeyer KD, Vlad SC, et al. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis Rheumatol. 2014;66:3013–3017. doi: 10.1002/art.38795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwok WY, Kloppenburg M, Marshall M, et al. The prevalence of erosive osteoarthritis in carpometacarpal joints and its clinical burden in symptomatic community-dwelling adults. Osteoarthritis Cartilage. 2014;22:756–763. doi: 10.1016/j.joca.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tian W, Lv Y, Liu Y, et al. The high prevalence of symptomatic degenerative lumbar osteoarthritis in Chinese adults: a population-based study. Spine. 2014;39:1301–1310. doi: 10.1097/BRS.0000000000000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kobayashi T, Takagishi K, Shitara H, et al. Prevalence of and risk factors for shoulder osteoarthritis in Japanese middle-aged and elderly populations. J Shoulder Elbow Surg. 2014;23:613–619. doi: 10.1016/j.jse.2013.11.031. [DOI] [PubMed] [Google Scholar]
- 18.Kalichman L, Hernandez-Molina G. Midfoot and forefoot osteoarthritis. Foot. 2014;24:128–134. doi: 10.1016/j.foot.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Zhang JF, Song LH, Wei JN, et al. Prevalence of and risk factors for the occurrence of symptomatic osteoarthritis in rural regions of Shanxi Province, China. Int J Rheum Dis. 2014 doi: 10.1111/1756-185X.12470. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Tehrani-Banihashemi A, Davatchi F, Jamshidi AR, et al. Prevalence of osteoarthritis in rural areas of Iran: a WHO-ILAR COPCORD study. Int J Rheum Dis. 2014;17:384–388. doi: 10.1111/1756-185X.12312. [DOI] [PubMed] [Google Scholar]
- 21. Thomas E, Peat G, Croft P. Defining and mapping the person with osteoarthritis for population studies and public health. Rheumatology (Oxford) 2014;53:338–345. doi: 10.1093/rheumatology/ket346. This large mail-based survey in England illustrated the population burden of osteoarthritis, showing that about 22% of respondents reported disabling osteoarthritis.
- 22. Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1323–1330. doi: 10.1136/annrheumdis-2013-204763. This systematic review calculated the global age-standardized prevalence of knee osteoarthritis and hip osteoarthritis and reported that out of almost 300 health conditions studied, osteoarthritis was the 11th highest contributor to disability.
- 23.Turkiewicz A, Gerhardsson de Verdier M, Engstrom G, et al. Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology (Oxford) 2014 doi: 10.1093/rheumatology/keu409. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Moriatis Wolf J, Turkiewicz A, Atroshi I, Englund M. Prevalence of doctor-diagnosed thumb carpometacarpal joint osteoarthritis: an analysis of Swedish healthcare. Arthritis Care Res. 2014;66:961–965. doi: 10.1002/acr.22250. [DOI] [PubMed] [Google Scholar]
- 25. Rahman MM, Cibere J, Goldsmith CH, et al. Osteoarthritis incidence and trends in administrative health records from British Columbia, Canada. J Rheumatol. 2014;41:1147–1154. doi: 10.3899/jrheum.131011. This study examined 18 years of health records in British Columbia to calculate incidence rates of osteoarthritis over time. This research illustrates the utility of electronic health records to track the burden patterns of osteoarthritis on a large scale.
- 26.Prieto-Alhambra D, Judge A, Javaid MK, et al. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Ann Rheum Dis. 2014;73:1659–1664. doi: 10.1136/annrheumdis-2013-203355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turkiewicz A, Petersson IF, Bjork J, et al. Current and future impact of osteoarthritis on healthcare: a population-based study with projections to year 2032. Osteoarthritis Cartilage. 2014;22:1826–1832. doi: 10.1016/j.joca.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 28.Cleveland RJ, Schwartz TA, Prizer LP, et al. Associations of educational attainment, occupation, and community poverty with hip osteoarthritis. Arthritis Care Res. 2013;65:954–961. doi: 10.1002/acr.21920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cleveland RJ, Schwartz TA, Prizer LP, et al. Associations of educational attainment, occupation and community poverty with hip osteoarthritis. Arthritis Care Res. 2013;65:954–961. doi: 10.1002/acr.21920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Callahan LF, Cleveland RJ, Shreffler J, et al. Associations of educational attainment, occupation and community poverty with knee osteoarthritis in the Johnston County (North Carolina) osteoarthritis project. Arthritis Res Therapy. 2011;13:R169. doi: 10.1186/ar3492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–1994. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 32.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;31:172–180. [PubMed] [Google Scholar]
- 33.Pan F, Ding C, Winzenberg T, et al. The offspring of people with a total knee replacement for severe primary knee osteoarthritis have a higher risk of worsening knee pain over 8 years. Ann Rheum Dis. 2014 doi: 10.1136/annrheumdis-2014-206005. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 34.Khan HI, Aitken D, Chou L, et al. A family history of knee joint replacement increases the progression of knee radiographic osteoarthritis and medial tibial cartilage volume loss over 10 years. Osteoarthritis Cartilage. 2014;23:203–209. doi: 10.1016/j.joca.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 35.Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18:24–33. doi: 10.1016/j.joca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 36.Leung YY, Allen JC, Jr, Noviani M, et al. Association between body mass index and risk of total knee replacement, the Singapore Chinese Health Study. Osteoarthritis Cartilage. 2015;23:41–47. doi: 10.1016/j.joca.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shin D. Association between metabolic syndrome, radiographic knee osteoarthritis, and intensity of knee pain: results of a national survey. J Clin Endocrinol Metab. 2014;99:3177–3183. doi: 10.1210/jc.2014-1043. [DOI] [PubMed] [Google Scholar]
- 38.Visser AW, de Mutsert R, Loef M, et al. The role of fat mass and skeletal muscle mass in knee osteoarthritis is different for men and women: the NEO study. Osteoarthritis Cartilage. 2014;22:197–202. doi: 10.1016/j.joca.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 39.Karvonen-Gutierrez CA, Harlow SD, Jacobson J, et al. The relationship between longitudinal serum leptin measures and measures of magnetic resonance imaging-assessed knee joint damage in a population of mid-life women. Ann Rheum Dis. 2014;73:883–889. doi: 10.1136/annrheumdis-2012-202685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fowler-Brown A, Kim DH, Shi L, et al. The mediating effect of leptin on the relationship between body weight and knee osteoarthritis in older adults. Arthritis Rheumatol. 2015;67:169–175. doi: 10.1002/art.38913. This study of older adults found that almost half of the association between BMI and knee osteoarthritis was explained by serum leptin levels, illustrating the potential important role of metabolic factors in osteoarthritis development.
- 41. Lim YZ, Wang Y, Wluka AE, et al. Association of obesity and systemic factors with bone marrow lesions at the knee: a systematic review. Semin Arthritis Rheum. 2014;43:600–612. doi: 10.1016/j.semarthrit.2013.10.006. This systematic review found strong evidence for higher serum lipids as a risk factor for knee bone marrow lesions among individuals with asymptomatic pre-osteoarthritis and established osteoarthritis; if the role of lipids is confirmed, this may be an early modifiable risk factor.
- 42.Valdes AM, Zhang W, Muir K, et al. Use of statins is associated with lower prevalence of generalised osteoarthritis. Ann Rheum Dis. 2014;73:943–945. doi: 10.1136/annrheumdis-2013-204382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teichtahl AJ, Wluka AE, Tanamas SK, et al. Weight change and change in tibial cartilage volume and symptoms in obese adults. Ann Rheum Dis. 2014 doi: 10.1136/annrheumdis-2013-204488. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 44.Magnusson K, Osteras N, Haugen IK, et al. No strong relationship between body mass index and clinical hand osteoarthritis: results from a population-based case-control study. Scandinavian J Rheumatol. 2014;43:409–415. doi: 10.3109/03009742.2014.900700. [DOI] [PubMed] [Google Scholar]
- 45.Visser AW, Ioan-Facsinay A, de Mutsert R, et al. Adiposity and hand osteoarthritis: the Netherlands Epidemiology of Obesity study. Arthritis Res Therapy. 2014;16:R19. doi: 10.1186/ar4447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu B, Driban JB, Duryea J, et al. Milk consumption and progression of medial tibiofemoral knee osteoarthritis: data from the Osteoarthritis Initiative. Arthritis Care Res. 2014;66:802–809. doi: 10.1002/acr.22297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McAlindon T, LaValley M, Schneider E, et al. Effect of vitamin D supplementation on progression of knee pain and cartilage volume loss in patients with symptomatic osteoarthritis: a randomized controlled trial. JAMA. 2013;309:155–162. doi: 10.1001/jama.2012.164487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhang FF, Driban JB, Lo GH, et al. Vitamin D deficiency is associated with progression of knee osteoarthritis. J Nutr. 2014;144:2002–2008. doi: 10.3945/jn.114.193227. This study found that vitamin D deficiency was associated with increased risk of knee osteoarthritis progression, and the risk was even greater among individuals with concomitant high parathyroid hormone.
- 49.Laslett LL, Quinn S, Burgess JR, et al. Moderate vitamin D deficiency is associated with changes in knee and hip pain in older adults: a 5-year longitudinal study. Ann Rheum Dis. 2014;73:697–703. doi: 10.1136/annrheumdis-2012-202831. [DOI] [PubMed] [Google Scholar]
- 50.Shea MK, Kritchevsky SB, Hsu F, et al. The association between vitamin K status and knee osteoarthritis features in older adults: the Health, Aging and Body Composition Study. Osteoarthritis Cartilage. 2014;23:370–378. doi: 10.1016/j.joca.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chaganti RK, Tolstykh I, Javaid MK, et al. High plasma levels of vitamin C and E are associated with incident radiographic knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:190–196. doi: 10.1016/j.joca.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hardcastle SA, Dieppe P, Gregson CL, et al. Prevalence of radiographic hip osteoarthritis is increased in high bone mass. Osteoarthritis Cartilage. 2014;22:1120–1128. doi: 10.1016/j.joca.2014.06.007. This study used a novel approach of examining individuals with extreme high bone mass (likely a genetic trait) and found that this phenotype was associated with greater prevalence of radiographic hip osteoarthritis.
- 53. Hardcastle SA, Dieppe P, Gregson CL, et al. Individuals with high bone mass have an increased prevalence of radiographic knee osteoarthritis. Bone. 2015;71:171–179. doi: 10.1016/j.bone.2014.10.015. This study showed that the extreme high bone mass phenotype is also associated with more prevalent knee osteoarthritis.
- 54.Felson DT, Zhang Y. Smoking and osteoarthritis: a review of the evidence and its implications. Osteoarthritis Cartilage. 2014;23:331–333. doi: 10.1016/j.joca.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hui M, Doherty M, Zhang W. Does smoking protect against osteoarthritis? Meta-analysis of observational studies. Ann Rheum Dis. 2011;70:1231–1237. doi: 10.1136/ard.2010.142323. [DOI] [PubMed] [Google Scholar]
- 56.Leung YY, Ang LW, Thumboo J, et al. Cigarette smoking and risk of total knee replacement for severe osteoarthritis among Chinese in Singapore: the Singapore Chinese health study. Osteoarthritis Cartilage. 2014;22:764–770. doi: 10.1016/j.joca.2014.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hussain SM, Wang Y, Wluka AE, et al. Association of low birth weight and preterm birth with the incidence of knee and hip arthroplasty for osteoarthritis. Arthritis Care Res. 2014 doi: 10.1002/acr.22475. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 58.Clynes MA, Parsons C, Edwards MH, et al. Further evidence of the developmental origins of osteoarthritis: results from the Hertfordshire Cohort Study. J Dev Orig Health Dis. 2014;5:453–458. doi: 10.1017/S2040174414000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang W, Robertson J, Doherty S, et al. Index to ring finger length ratio and the risk of osteoarthritis. Arthritis Rheum. 2008;58:137–144. doi: 10.1002/art.23237. [DOI] [PubMed] [Google Scholar]
- 60.Sigurjonsdottir K, Bjorgulfsson TM, Aspelund T, et al. Type 3 finger length pattern is associated with total knee replacements due to osteoarthritis but not with hip replacements or hand osteoarthritis in the elderly: the AGES-Reykjavik study. BMC Musculoskelet Disord. 2013;14:112. doi: 10.1186/1471-2474-14-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferraro B, Wilder FV, Leaverton PE. Site specific osteoarthritis and the index to ring finger length ratio. Osteoarthritis Cartilage. 2010;18:354–357. doi: 10.1016/j.joca.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 62.Haugen IK, Niu J, Aliabadi P, et al. The associations between finger length pattern, osteoarthritis, and knee injury: data from the Framingham community cohort. Arthritis Rheum. 2011;63:2284–2288. doi: 10.1002/art.30408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hussain SM, Wang Y, Muller DC, et al. Association between index-to-ring finger length ratio and risk of severe knee and hip osteoarthritis requiring total joint replacement. Rheumatology (Oxford) 2014;53:1200–1207. doi: 10.1093/rheumatology/keu021. [DOI] [PubMed] [Google Scholar]
- 64.Nelson AE, Liu F, Lynch JA, et al. Association of incident symptomatic hip osteoarthritis with differences in hip shape by active shape modeling: the Johnston County Osteoarthritis Project. Arthritis Care Res. 2014;66:74–81. doi: 10.1002/acr.22094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Wise BL, Kritikos L, Lynch JA, et al. Proximal femur shape differs between subjects with lateral and medial knee osteoarthritis and controls: the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2014;22:2067–2073. doi: 10.1016/j.joca.2014.08.013. This study found that ipsilateral proximal femur shape differed between prevalent case and control knees for both medial and lateral osteoarthritis, adding to prior literature showing that hip shape is associated with hip osteoarthritis.
- 66. Boissonneault A, Lynch JA, Wise BL, et al. Association of hip and pelvic geometry with tibiofemoral osteoarthritis: Multicenter Osteoarthritis Study (MOST) Osteoarthritis Cartilage. 2014;22:1129–1135. doi: 10.1016/j.joca.2014.06.010. This study found differences in hip shape between knees with and without lateral knee osteoarthritis. Also found related sex differences in hip shape that may help to explain sex differences in lateral knee osteoarthritis.
- 67.Thomas GE, Palmer AJ, Batra RN, et al. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Osteoarthritis Cartilage. 2014;22:1504–1510. doi: 10.1016/j.joca.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 68.Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18:24–33. doi: 10.1016/j.joca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 69.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 70.Muthuri S, McWilliams D, Doherty M, Zhang W. History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies. Osteoarthritis Cartilage. 2011;19:1286–1293. doi: 10.1016/j.joca.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 71.Roos EM, Ostenberg A, Roos H, et al. Long-term outcome of meniscectomy: sympotms, function, and performance tests in patient with or without radiographic osteoarthritis compared to matched controls. Osteoarthritis Cartilage. 2001;9:316–324. doi: 10.1053/joca.2000.0391. [DOI] [PubMed] [Google Scholar]
- 72.Roemer FW, Jarraya M, Niu J, et al. Increased risk for radiographic osteoarthritis features in young active athletes: a cross-sectional matched case-control study. Osteoarthritis Cartilage. 2014;23:239–243. doi: 10.1016/j.joca.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 73.Eckstein F, Wirth W, Lohmander LS, et al. Five-year followup of knee joint cartilage thickness changes after acute rupture of the anterior cruciate ligament. Arthritis Rheumatol. 2015;67:152–161. doi: 10.1002/art.38881. [DOI] [PubMed] [Google Scholar]
- 74.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34:612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 75.Valderrabano V, Horisberger M. Ankle osteoarthritis: a review of the current state of knowledge. European Musculoskelet Rev. 2011;6:114–118. [Google Scholar]
- 76.Valderrabano V, Horisberger M, Russell I, et al. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467:1800–1806. doi: 10.1007/s11999-008-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Harkey MS, Luc BA, Golightly YM, et al. Osteoarthritis-related biomarkers following anterior cruciate ligament injury and reconstruction: a systematic review. Osteoarthritis Cartilage. 2015;23:1–12. doi: 10.1016/j.joca.2014.09.004. This is a systematic review confirming the link between injury and osteoarthritis, showing that individuals with ACL deficient and reconstructed knees had altered synovial fluid biomarker levels indicative of osteoarthritis, compared with controls.
- 78.Driban JB, Eaton CB, Lo GH, et al. Association of knee injuries with accelerated knee osteoarthritis progression: data from the Osteoarthritis Initiative. Arthritis Care Res. 2014;66:1673–1679. doi: 10.1002/acr.22359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nordenvall R, Bahmanyar S, Adami J, et al. Cruciate ligament reconstruction and risk of knee osteoarthritis: the association between cruciate ligament injury and posttraumatic osteoarthritis. a population based nationwide study in Sweden, 1987–2009. PLoS One. 2014;9:e104681. doi: 10.1371/journal.pone.0104681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bennell KL, Wrigley TV, Hunt MA, et al. Update on the role of muscle in the genesis and management of knee osteoarthritis. Rheum Dis Clin North Am. 2013;39:145–176. doi: 10.1016/j.rdc.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 81. Oiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis Cartilage. 2014;23:171–177. doi: 10.1016/j.joca.2014.10.008. This is a meta-analysis showing an overall increased risk of developing symptomatic knee osteoarthritis among individuals with knee extensor muscle weakness, supporting this as a potential modifiable risk factor.
- 82.Ruhdorfer AS, Dannhauer T, Wirth W, et al. Thigh muscle cross-sectional areas and strength in knees with early vs knees without radiographic knee osteoarthritis: a between-knee, within-person comparison. Osteoarthritis Cartilage. 2014;22:1634–1638. doi: 10.1016/j.joca.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ruhdorfer A, Wirth W, Hitzl W, et al. Association of thigh muscle strength with knee symptoms and radiographic disease stage of osteoarthritis: data from the Osteoarthritis Initiative. Arthritis Care Res. 2014;66:1344–1353. doi: 10.1002/acr.22317. [DOI] [PubMed] [Google Scholar]
- 84.Dannhauer T, Ruhdorfer A, Wirth W, Eckstein F. Quantitative relationship of thigh adipose tissue with pain, radiographic status, and progression of knee osteoarthritis: longitudinal findings from the Osteoarthritis Initiative. Invest Radiol. 2014 doi: 10.1097/RLI.0000000000000113. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 85.Hall M, Wrigley TV, Metcalf BR, et al. Do moments and strength predict cartilage changes following partial meniscectomy? Med Sci Sports Exerc. 2014 doi: 10.1249/MSS.0000000000000575. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 86.Runhaar J, van Middelkoop M, Reijman M, et al. Malalignment: a possible target for prevention of incident knee osteoarthritis in overweight and obese women. Rheumatology (Oxford) 2014;53:1618–1624. doi: 10.1093/rheumatology/keu141. [DOI] [PubMed] [Google Scholar]
- 87.Henriksen M, Creaby MW, Lund H, et al. Is there a causal link between knee loading and knee osteoarthritis progression? A systematic review and meta-analysis of cohort studies and randomised trials. BMJ Open. 2014;4:e005368. doi: 10.1136/bmjopen-2014-005368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sharma L, Song J, Dunlop D, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69:1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tanamas S, Hanna FS, Cicuttini FM, et al. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61:459–467. doi: 10.1002/art.24336. [DOI] [PubMed] [Google Scholar]
- 90.Menz HB, Roddy E, Marshall M, et al. Demographic and clinical factors associated with radiographic severity of first metatarsophalangeal joint osteoarthritis: cross-sectional findings from the Clinical Assessment Study of the Foot. Osteoarthritis Cartilage. 2015;23:77–82. doi: 10.1016/j.joca.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Golightly YM, Hannan MT, Dufour AB, et al. Factors associated with hallux valgus in a community-based cross-sectional study of adults with and without osteoarthritis. Arthritis Care Res. 2014 doi: 10.1002/acr.22517. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Barbour KE, Hootman JM, Helmick CG, et al. Meeting physical activity guidelines and the risk of incident knee osteoarthritis: a population-based prospective cohort study. Arthritis Care Res. 2014;66:139–146. doi: 10.1002/acr.22120. This study confirmed that meeting physical activity recommendations was not associated with radiographic or symptomatic osteoarthritis, compared with less activity.
- 93.Golightly YM, Allen KD, Helmick CG, et al. Symptoms of the knee and hip in individuals with and without limb length inequality. Osteoarthritis Cartilage. 2009;17:596–600. doi: 10.1016/j.joca.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Golightly YM, Allen KD, Helmick CG, et al. Hazard of incident and progressive knee and hip radiographic osteoarthritis and chronic joint symptoms in individuals with and without limb length inequality. J Rheumatol. 2010;37:2133–2140. doi: 10.3899/jrheum.091410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Golightly YM, Allen KD, Renner JB, et al. Relationship of limb length inequality with radiographic knee and hip osteoarthritis. Osteoarthritis Cartilage. 2007;15:824–829. doi: 10.1016/j.joca.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Harvey WF, Yang M, Cooke TD, et al. Association of leg-length inequality with knee osteoarthritis: a cohort study. Ann Intern Med. 2010;152:287–295. doi: 10.1059/0003-4819-152-5-201003020-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Pan F, Han W, Wang X, et al. A longitudinal study of the association between infrapatellar fat pad maximal area and changes in knee symptoms and structure in older adults. Ann Rheum Dis. 2014 doi: 10.1136/annrheumdis-2013-205108. [Epub ahead of print] This study examined a novel area of infrapatellar fat pad maximal area, finding that greater area was beneficially associated with change in knee pain, tibial cartilage volume, and risk of medial cartilage defects among women.
- 98.Schiphof D, van Middelkoop M, de Klerk BM, et al. Crepitus is a first indication of patellofemoral osteoarthritis (and not of tibiofemoral osteoarthritis) Osteoarthritis Cartilage. 2014;22:631–638. doi: 10.1016/j.joca.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 99.Stefanik JJ, Neogi T, Niu J, et al. The diagnostic performance of anterior knee pain and activity-related pain in identifying knees with structural damage in the patellofemoral joint: the Multicenter Osteoarthritis Study. J Rheumatol. 2014;41:1695–1702. doi: 10.3899/jrheum.131555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Sharma L, Chmiel JS, Almagor O, et al. Significance of preradiographic magnetic resonance imaging lesions in persons at increased risk of knee osteoarthritis. Arthritis Rheumatol. 2014;66:1811–1819. doi: 10.1002/art.38611. This study found that among individuals without radiographic osteoarthritis evidence, lesions found on MRI were associated with prevalent and incident persistent knee symptoms and incident cartilage damage.
- 101. Kerkhof HJ, Bierma-Zeinstra SM, Arden NK, et al. Prediction model for knee osteoarthritis incidence, including clinical, genetic and biochemical risk factors. Ann Rheum Dis. 2014;73:2116–2121. doi: 10.1136/annrheumdis-2013-203620. This study sought to develop a predictive model of osteoarthritis risk based on a broad array of variables. Found that beyond a model including age sex, and BMI minor baseline radiographic changes significantly improved prediction, but other questionnaire, biomarker, and genetic data did not meaningfully improve the model this highlights the potential clinical importance of minor radiographic findings.
- 102.Sharma L, Dunlop D, Cahue S, et al. Quadriceps strength and osteoarthritis progression in malaligned and lax knees. Ann Intern Med. 2003;138:613–619. doi: 10.7326/0003-4819-138-8-200304150-00006. [DOI] [PubMed] [Google Scholar]