1. Introduction
Emergency Medical Services (EMS) providers care for patients of all ages, including pediatric patients. They see children with a wide variety of critical illnesses including cardiac arrest, respiratory failure, and trauma. Airway management is often one of the initial steps taken in stabilizing a patient with many critical conditions. The purpose of airway management is to achieve adequate tissue oxygenation, ventilation, and limit aspiration of oral and gastric contents. Airway management procedures include suctioning, bag-mask-ventilation (BVM), airway adjuncts (oral and nasal airways), alternative airways (supraglottic devices), and endotracheal intubation (ETI).
Successful airway management requires training, skills and ongoing experience to consistently perform these procedures in an effective, timely, and safe manner. Airway management procedures in children require unique skill sets and equipment due to variations in anatomy based on patient age and size.1 For example, the pediatric glottis is more superior and anterior than the adult glottis. Previous studies have shown that airway management procedures are rarely performed by individual EMS providers.2 In addition, airway management skills rapidly deteriorate after training indicating that frequent training is needed to maintain airway management skills, which is likely challenging given limited resources and competing needs for training on other topics.3 Many EMS agencies continue to support ETI as the gold standard for pediatric airway management while others have abandoned ETI due to safety concerns, highlighting the current controversy among experts in out-of-hospital care. There is evidence to suggest that out-of-hospital pediatric airway management may have increased complications compared to hospital-based airway management; a large controlled trial failed to show benefit of ETI and suggested harm in certain subgroups.4–7
The National Emergency Medical Services Information System (NEMSIS) is the largest registry of EMS responses in the US. In this report, we sought to describe the characteristics of out-of-hospital pediatric airway management in the United States.
2. Methods
2.1 Study Design
The institutional review board of the Oregon Health & Science University reviewed and approved the protocol (IRB00010366). In this descriptive study, we analyzed data from the NEMSIS 2012 Public Release Research Dataset.
2.2 Study Setting
The Office of Emergency Medical Services of the National Highway Traffic Safety Administration (NHTSA) funds the NEMSIS project. The goal of NEMSIS is to standardize the data obtained by EMS providers through their patient care reports and aggregate these data for analysis on a local, state, and national level. The NEMSIS national EMS dataset is maintained by the NEMSIS Technical Assistance Center (TAC) housed at the University of Utah School of Medicine.
The NEMSIS TAC promotes the standardized electronic collection of over 400 data elements by encouraging use of electronic patient care report software that is compliant with the NEMSIS system. The lead EMS office in each state coordinates data collection from local EMS agencies then exports the data to the NEMSIS Technical Assistance Center to be placed in the national repository. Of the 400 data elements, only 83 are submitted to the national database with the remainder being housed in individual, local, and state databases. The NEMSIS program does not define inclusion or exclusion criteria of EMS activations to be included in the database, but takes all data meeting the state inclusion criteria. In addition, states can submit data from any number of participating EMS agencies throughout the state, so the data may not represent all EMS agencies in any given participating state.
For this study we identified patients less than 18 years of age from the NEMSIS 2012 Public Release Research Dataset totaling over 1.1 million pediatric EMS activations. Forty states participated in data submission to the 2012 NEMSIS dataset. Among the 40 participating states, 21 reported capture of more than 95% of all 911 ground EMS activations. The remaining states report inclusion of more than 75% of 9-1-1 ground EMS activations. It is estimated that approximately 50% of helicopter based transports in the US states submitting to NEMSIS are captured.
2.3 Selection of Participants
This study included all EMS activations for patients less than 18 years of age, including activations where care was provided but the patient was not transported. We excluded EMS activations where EMS responded but there was no patient care. We then identified patients receiving NEMSIS-defined airway interventions or ventilatory support, including endotracheal intubation (ETI), alternate airway insertion, cricothyroidotomy, bag-valve-mask ventilation (BVM), continuous positive airway pressure (CPAP), Bi-level positive airway pressure (BiPAP), or other ventilation.
2.4 Outcomes
The primary outcomes were frequency, success and complication rates of pediatric airway management procedures. In this analysis we defined endotracheal intubation (ETI) as direct laryngoscopy, video laryngoscopy, orotracheal intubation, nasotracheal intubation, or rapid sequence intubation (RSI). The alternative airways recorded by NEMSIS include the LMA, the King LT, the Combitube, and the Esophageal Obturator airway. We included methods of ventilation other than bag-valve-mask as “other ventilation” which includes bag ventilation via endotracheal tube or alternate airway, respirator operation, or ventilator operation. We combined surgical and needle cricothyroidotomy into a single category unless otherwise specified. When patients were ventilated with a bag-valve-mask setup, this was defined as BVM. When patients were ventilated without a mask via a tube, had “respirator operation,” or “ventilator operation”, they were classified as “other ventilation.”
When a procedure appeared more than once for a single patient it was counted only once in the analysis. For example, if a patient had 2 ETIs during their patient care event it would be classified as a single ETI. However, if patients had both BVM and ETI during the same encounter they were classified separately in the analysis. The NEMSIS data also indicated the success of each procedure. In instances where procedures were attempted several times, we considered it a success if any of the attempts were recorded as successful. If two separate intubations took place, and either one or both were successful, this was classified as a successful intubation for that patient care episode. Airway procedural complications included bleeding, bradycardia, esophageal intubation, hypotension, hypoxia, injury, vomiting and other as defined by the paramedic completing the medical record.
Patient level variables included age, gender, race, and ethnicity. Illness specific variables included cardiac arrest, possible injury, provider’s primary impression, and cause of injury.
The population setting of the EMS encounter, “urbanicity”, is classified in NEMSIS according to the United States Department of Agriculture (USDA) and the Office of Management and Budget (OMB) definitions: urban areas that have large (1+million residents) or small (less than 1 million residents) metropolitan areas; suburban areas with micropolitan (urban core of at least 10,000 residents) counties adjacent to large or small metropolitan areas; rural areas that have non-urban core counties adjacent to a large or small metropolitan area; and wilderness that are considered non-core counties adjacent to micropolitan counties.
The NEMSIS program has individual data use agreements with each state that preclude release of any state, agency, or provider specific data in the public use dataset. To analyze by region we stratified the data according to the US census regions (Northeast, South, Midwest, and West).
2.5 Primary Data Analysis
We analyzed the data with descriptive statistics including binomial proportions and exact 95% confidence intervals for those proportions.
We calculated the number and proportion of airway interventions in EMS patient care events for patients less than 18 years. We described demographics of the population receiving airway intervention including age, gender, race, ethnicity, urbanicity of the incident location, and US census region. We also described several illness specific factors such as cardiac arrest status, injury status, and the most common medical or traumatic primary impression provided by the EMS provider.
We calculated success of ETI, cricothyroidotomy, and alternate airways for patients in various age subgroups, by cardiac arrest status, injury status, urbanicity, and region. After univariate odds ratio calculations we performed multiple logistic regression to control for potential collinearity among the various variables.
Results
3.1 Overall results
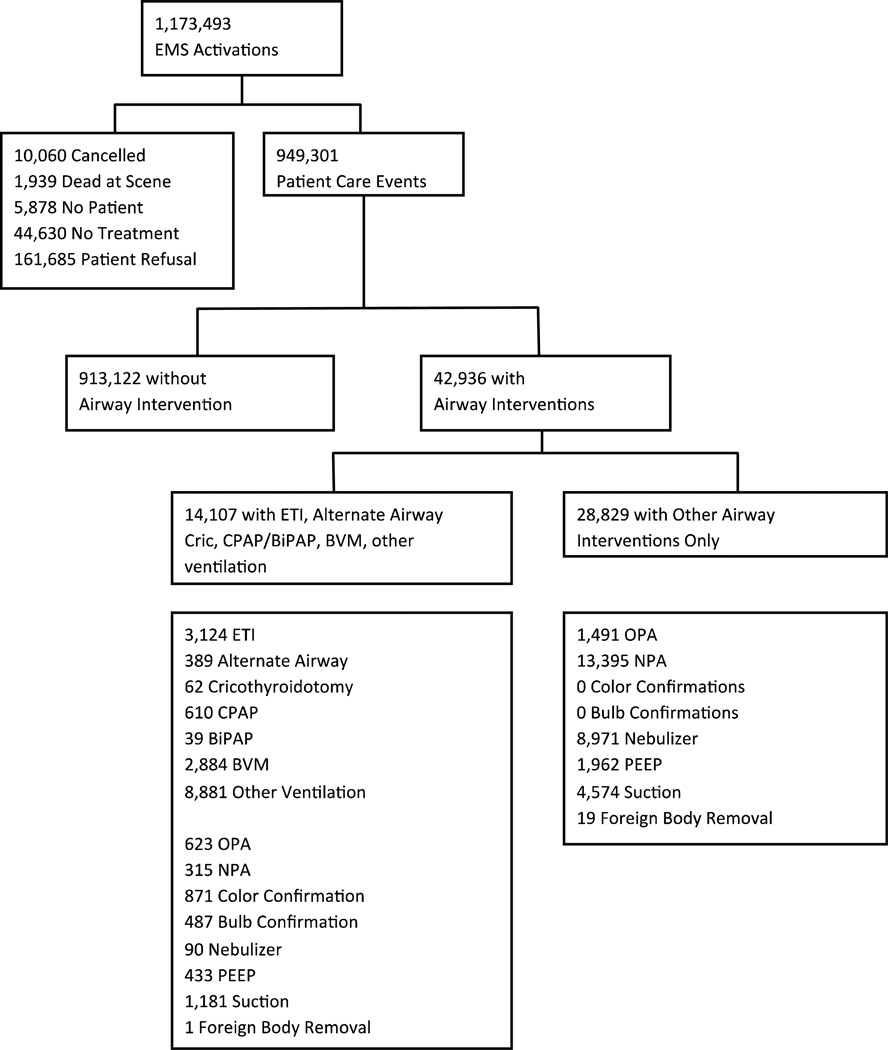
During the 2012 study period there were a total of 1,173,493 pediatric EMS activations resulting in 949,301 patient care episodes (Figure 1 and Table 1). 4.5% of patient care events involved airway management procedures (42,936). The most commonly reported airway events were nasopharyngeal airway insertion, other ventilation, and nebulizer treatment. Invasive airway management or invasive ventilation (ETI, cricothyroidotomy, alternate airway, CPAP/BiPAP, BVM and other ventilation) took place in 1.5% of patient care events (14,107). Of those who had invasive airway management, 29.9% were less than 1 year of age, 58.1% were male, 42.3% were white, and 83.6% were in urban areas (Table 2).
Figure 1.
Airway management procedures performed during NEMSIS events. EMS: Emergency Medical Services. ETI: endotracheal intubation, Cric: crocothyroidotomy, BVM: bag-valve-mask-ventilation. BiPAP: bilevel positive airway pressure, CPAP: continuous positive airway pressure, OPA: oral pharyngeal airway, NPA: nasal pharyngeal airway, PEEP: positive end expiratory pressure.
Table 1.
Prevalence of airway management interventions. Reported rates represent portion of 949,301 total patient care events. BiPAP = bilevel positive airway pressure. CPAP = continuous positive airway pressure. PEEP = positive end expiratory pressure.
| Intervention | N | N per 100,000 patient care events (95% CI) |
|---|---|---|
| Bag-valve-mask ventilation | 2,884 | 304 (293–315) |
| Other ventilation | 8,881 | 935 (916–955) |
| Endotracheal intubation | 3,124 | 329 (318–341) |
| Orotracheal intubation | 2,985 | 314 (303–325) |
| Nasotracheal intubation | 130 | 14 (11–16) |
| Rapid Sequence intubation | 426 | 45 (41–49) |
| Alternate airway | 389 | 41 (37–45) |
| Combitube | 105 | 11 (9.0–13) |
| Esophageal-Obturator | 21 | 2.2 (1.4–3.4) |
| Laryngeal Mask Airway | 167 | 17 (15–20) |
| King LT | 96 | 10 (8–12) |
| Cricothyroidotomy | 62 | 6.5 (5.0–8.4) |
| Needle cricothyroidotomy | 47 | 5.0 (3.6–6.6) |
| Surgical cricothyroidotomy | 15 | 1.6 (0.88–2.6) |
| BiPAP/CPAP | 649 | 68 (63–74) |
| Oropharyngeal airway | 2,114 | 223 (213–232) |
| Nasopharyngeal airway | 13,710 | 1444 (1420–1468) |
| Colorimetric tube confirmation | 871 | 92 (86–98) |
| Bulb tube confirmation | 487 | 51 (47–56) |
| Nebulizer | 9,061 | 954 (935–974) |
| PEEP | 2,935 | 252 (242–263) |
| Suction | 5,755 | 606 (590–622) |
| Foreign Body Removal | 20 | 2.1 (1.3–3.3) |
Table 2.
Characteristics of patients who received airway management intervention. ETI: endotracheal intubation, BiPAP: Bilevel positive airway pressure.
| Characteristic | All invasive airway or ventillatory support (n=14,107) |
ETI, alternate airway, cricothyroidotomy, BiPAP only (n=3523) |
ETI only (n=2984) |
|||
|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | |
| Age group | ||||||
| 0–1 month | 1,881 | (13.4) | 554 | (15.7) | 534 | (18.0) |
| 1–12 months | 2,317 | (16.5) | 718 | (20.4) | 667 | (22.4) |
| 1–5 years | 2,406 | (17.1) | 453 | (12.9) | 381 | (12.8) |
| 5–11 years | 1,626 | (11.6) | 341 | (9.7) | 289 | (9.7) |
| 11–17 years | 4,086 | (29.0) | 1,087 | (30.9) | 813 | (27.2) |
| unknown | 1,755 | (12.5) | 370 | (10.5) | 300 | (10.1) |
| Sex | ||||||
| Male | 8,172 | (58.1) | 2,178 | (61.8) | 1862 | (62.4) |
| Female | 5,751 | (40.9) | 1,323 | (37.6) | 1101 | (36.9) |
| Unknown | 148 | (1.1) | 22 | (0.62) | 21 | (0.7) |
| Race | ||||||
| American Indian | 161 | (1.1) | 44 | (1.3) | 33 | (1.1) |
| Asian | 203 | (1.4) | 39 | (1.1) | 29 | (0.97) |
| African American | 2,440 | (17.3) | 642 | (18.2) | 547 | (18.3) |
| Pacific Islander | 155 | (1.1) | 5 | (0.14) | 4 | (0.13) |
| White | 5,953 | (42.3) | 1,853 | (52.6) | 1,615 | (54.1) |
| Other | 676 | (4.8) | 181 | (5.1) | 150 | (5.0) |
| Unknown | 4,483 | (31.9) | 759 | (21.5) | 606 | (20.3) |
| Ethnicity | ||||||
| Hispanic | 977 | (6.9) | 213 | (6.1) | 171 | (5.7) |
| Not Hispanic | 7,297 | (51.9) | 2,163 | (61.4) | 1,892 | (63.4) |
| Unknown | 5,797 | (41.2) | 1147 | (32.6) | 921 | (30.9) |
| Cardiac Arrest | ||||||
| Yes | 1,789 | (12.7) | 1,202 | (34.1) | 1,082 | (34.3) |
| No | 8,052 | (57.2) | 1,612 | (45.8) | 1,360 | (45.6) |
| Unknown | 4,230 | (30.1) | 709 | (20.1) | 542 | (18.1) |
| Injury | ||||||
| Yes | 2,822 | (20.1) | 997 | (28.3) | 851 | (28.5) |
| No | 9,799 | (69.6) | 1,925 | (54.6) | 1,607 | (53.9) |
| Unknown | 1,450 | (10.3) | 601 | (17.1) | 526 | (17.6) |
| Population Setting | ||||||
| Rural | 1,179 | (8.6) | 374 | (11.0) | 322 | (11.3) |
| Suburban | 824 | (6.0) | 222 | (6.5) | 191 | (6.7) |
| Urban | 11,493 | (83.6) | 2,725 | (80.3) | 2,297 | (80.3) |
| Wilderness | 257 | (1.9) | 73 | (2.2) | 52 | (1.8) |
| Unknown | 318 | (2.3) | 131 | (3.7) | 122 | (4.1) |
| US census region | ||||||
| Midwest | 2,611 | (18.6) | 930 | (26.4) | 778 | (26.1) |
| Northeast | 4,075 | (29.0) | 672 | (19.1) | 519 | (17.4) |
| South | 4,709 | (33.5) | 1,659 | (47.1) | 1,479 | (49.6) |
| West | 2,646 | (18.8) | 261 | (7.4) | 207 | (6.9) |
3.2 Clinical impression in airway management cases
For the 70% of encounters with invasive airway management where a clinical impression was reported (9,810 of 14,107), the primary impression was respiratory distress in 21.8%, 21.2% traumatic injury, 16.1% cardiac arrest, 14.5% seizure, and 6.6% altered level of consciousness. For the 12% of patients with invasive airway management who had a cause of injury reported (1,707 of 14,107), 25.5% indicated motor vehicle traffic accident, 24.1% falls, 8.7% pedestrian traffic accident, and 7.0% motor vehicle non-traffic accident.
3.3 Endotracheal Intubation
ETI occurred in 3,124 of 949,301 (Table 1) patient care events (329 per 100,000; 95%CI 318–341). Overall ETI success was 81.1% (95%CI 79.7–82.6). ETI success was not reported in 431 cases (13.8%). ETI success was lowest for patients in cardiac arrest and for those aged 1–12 months, and was higher for patients aged 0–1months (Table 3). Of note, 35% of all cardiac arrests in the cohort occurred in patients less than 1 year of age. RSI demonstrated higher success rates though only 23% of RSI was in children less than 1 year of age, 28% in patients 1–11 years, and 49% in children over 11. The success rate for RSI was 88.2% for children less than 1 year of age, compared to 71% for non-RSI ETI, though only 34 total RSIs were performed in children less than 1. ETI success was higher in the Midwest and West, and was lowest in the South (Table 3). ETI success was highest in urban areas and lowest in rural areas (Table 3). Multiple logistic regression demonstrated that region, rural status, age, and RSI were significantly associated with ETI success with very similar odds ratios to univariate analysis, though cardiac arrest status was no longer significantly associated with success (OR 0.88 95%CI 0.576–1.342). We found that overall ETI success on the first attempt was 68.9%, with an additional 9.8% successful after a second attempt and 2.9% after a third attempt. Number of attempts was not reported in 9.7% of cases. Capnography was used during 36.8% of intubations. Colorimetric end-tidal CO2 devices were documented as being used in 14.6% of intubations, quantitative capnography in 22.2%, and esophageal bulbs were used in 3.9%. We found that ETI success among calls where a rotary wing EMS service responded was 89.9% (out of 652 total EMS care events where rotary wing response present). However level of service was not documented in 32.1% of cases where ETI was performed.
Table 3.
Airway intervention success including orotracheal, nasotracheal, and rapid sequence intubation. Unadjusted odds ratios are presented for selected comparisons only.
| Procedure | Successful/subgroup total (n=2852) |
% successful; 95% CI | Univariate odds ratio (95%CI) |
|---|---|---|---|
| Endotracheal Intubation | 2,314/2,852 | 81.1; 79.7–82.6 | N/A |
| Clinical Condition | |||
| Non-arrest medical | 1,074/1,278 | 84.0; 80.9–86.0 | Referent |
| Cardiac arrests | 695/920 | 75.5; 72.6–78.3 | 0.59 (0.48–0.73) |
| Non-arrest injury | 545/654 | 83.3; 80.3–86.1 | 0.95 (0.74–1.23) |
| Age | |||
| Age 0–1 month | 415/481 | 86.3; 82.9–89.2 | 1.22 (0.89–1.67) |
| Age 1–12 months | 431/598 | 72.1; 68.3–75.6 | 0.50 (0.39–0.64) |
| Age 1–5 years | 306/370 | 82.7; 78.5–86.4 | 1.13 (0.85–1.50) |
| Age 5–11 years | 251/297 | 84.5; 80.0–88.4 | 0.92 (0.67–1.28) |
| Age 11–17 years | 700/835 | 83.8; 81.2–86.3 | Referent |
| Rapid Sequence Intubation | 379/408 | 92.9; 90.0–95.2 | N/A |
| Population Setting | |||
| Urban | 1,776/2,171 | 81.8; 80.1–83.4 | Referent |
| Rural | 222/299 | 74.3; 68.9–79.1 | 0.64 (0.48–0.85) |
| Suburban | 153/194 | 78.9; 0.72–0.84 | 0.83 (0.59–1.51) |
| Wilderness | 41/52 | 78.9; 65.3–88.9 | 0.83 (0.42–1.63) |
| US census region | |||
| South | 1,124/1,426 | 78.2 (76.6–80.9) | Referent |
| Midwest | 576/675 | 85.3 (82.4–87.9) | 1.61 (1.26–2.08) |
| Northeast | 407/507 | 80.3 (76.5–83.7) | 1.20 (0.93–1.55) |
| West | 205/242 | 84.7 (79.6–89.0) | 1.38 (0.95–2.01) |
| Alternate airways | |||
| Combitube | 73/84 | 86.9; 77.8–94.12 | |
| Esophageal Obturator | 12/21 | 57.1; 34.0–78.2 | |
| Airway | |||
| Laryngeal Mask Airway | 89/145 | 61.4; 52.9–69.3 | |
| King | 80/90 | 88.9; 80.5–94.5 | |
| Cricothyroidotomy (needle and open) | 27/30 | 90; 73.5–97.9 | |
Totals are different than reported in table 1 due to missing data for procedural success. Records not included in analysis if success was not reported. Odds ratios not reported for alternate airways due to low numbers and overlapping missing data for procedural success.
3.4 Supraglottic Airways
Supraglottic airway insertion occurred in 389 of 949,301 patient care events (41 per 100,000; 95%CI 37–45). The King airway and Combitube were the most commonly used devices. Success rates were highly variable with esophageal obturator airways having a 57.1% success rate and the King airway 88.9% success rate. Success was not reported in 49 cases (13.0%). Most supraglottic devices were placed in older children with 53% in children 12 years and older. Only 12.8% were placed in children less than 1 year of age.
3.5 Complications
Table 4 displays rates of complications from airway management procedures. The predominant complications were immediately recognized esophageal intubation, bleeding and vomiting. Overall the number of reported complications was very low.
Table 4.
Complications of airway management procedures
| Complication | N (out of 3,936) | (N per 1,000 interventions, 95% CI) |
|---|---|---|
| Bleeding | 35 | (8.9, 6.2–12.3) |
| Bradycardia | 1 | (0.3, 0.0–1.4) |
| Esophageal intubation – Immediately detected | 36 | (9.1, 6.4–12.6) |
| Hypotension | 3 | (0.8, 0.2–2.2) |
| Hypoxia | 6 | (1.5, 0.6–3.3) |
| Injury | 10 | (2.5, 1.2–4.7) |
| Vomiting | 35 | (8.9, 6.2–12.3) |
| Other | 107 | (27.2, 22.3–32.8) |
Discussion
This is the largest study of out-of-hospital pediatric airway management. Airway interventions occurred in 4.5% of pediatric EMS encounters (42,936 of 949,301). ETI and BVM were the most common invasive airway interventions. Pediatric ETI is performed at a slightly lower rate than in adults per patient encounter based on comparison to the 2012 NEMSIS dataset where the rate was 426 of every 100,000 patient care encounters.8 However, the overall frequency of pediatric ETI is much lower than adults since only 7–13% of EMS transports are for children.9–11
Our study shows out-of-hospital ETI, the most commonly used advanced technique, has significantly lower success rates compared to in the hospital and alarmingly low rates of C02-based confirmation of placement. Despite the findings of the Gauche-Hill study 15 years ago that showed no benefit and trend towards harm with pediatric ETI, it continues to be the most commonly practiced advanced airway management technique. It is unclear why the current practice is not consistent with the best available evidence. One possibility is that BVM is challenging to perform and resource intensive in the out-of-hospital environment making EMS providers reluctant to use it. Another is that pediatric intubation is ingrained in EMS culture and providers face cultural stigma when patients are not intubated who could have been. Further studies should more clearly identify the decision making of EMS medical directors and paramedics in pediatric airway management. Supraglottic airways are a promising alternative to ETI, have high success rates in adults, and also warrant further study.19
In this study, supraglottic airways were used nearly 10 times less frequently than ETI. This is also more than 3 times less frequent than supraglottic airway use in the all-age 2012 NEMSIS study.8 In addition, frequency of use was lowest in patients aged less than 1 year who also have the lowest ETI success rates. The low rate of use may be due to lack of availability of supraglottic airways in the full range of pediatric sizes. The LMA is the only device in this study that is suitable for all ages. The King LT is not available for children less than 12 kg. Agencies may also find the cost of stocking supraglottic devices for all ages prohibitive.
We found the overall ETI success rate was lower than what is described for adult ETI. Success was lowest in those aged 1–12 months which is not unexpected given the anatomic differences of children in this age group. Unexpectedly, we found ETI success to be higher in patients 0–1 month of age. It is possible that ETI is easier in this age group due to lower tone. We also noted relatively high success rates with RSI, even in infants. However, only 34 RSIs were performed in infants limiting the ability to draw definitive conclusions for that age group. Increased success rates with RSI may be due to improved intubating conditions associated with medication facilitated intubation or more experienced providers performing RSI. ETI had lower success rates in rural areas and in the southern region. Rural providers may have lower call volumes and even less experience with pediatric airway management. Training resources may also be more challenging in rural areas. Finally, we found that only half of intubations use end tidal C02 use for confirmation of endotracheal tube placement.
Children less than 1 year of age and victims of cardiac arrest account for a significant portion of ETIs and have low ETI success rates though in multivariate modeling cardiac arrest status was not associated with ETI success. The most recent recommendations for Pediatric Advanced Life Support (PALS) from the American Heart Association (AHA) de-emphasize intubation in pediatric cardiac arrest management.12 In addition, recently reported data for adults suggests that out-of-hospital cardiac arrest victims may have better outcomes when advanced airway devices are not used.8,13 Given the best available current evidence, bag-mask-ventilation may be the most reasonable choice for airway management in pediatric cardiac arrest.
Out-of-hospital pediatric advanced airway management has lower success compared to in-hospital. Pediatric Emergency Physicians have 97–99% success in ETI in the Emergency Departement.12–14 The difference in success rates between out-of-hospital and hospital ETI may partly be due provider training. A survey of paramedic training programs indicated that the median number of ETI attempts for paramedic students in the operating room was between 6–10 and most of these are likely in adults.17 Lack of experience, fear of morbidity and loss of life, and the emotional trauma of seeing children suffer are likely to increase anxiety in pediatric calls and may contribute to reduced success.18 The positive effect of training and experience is further supported by our finding that rotary wing responses have relatively higher ETI success rates, though still not as high as hospital based providers. Rotary wing providers likely see a subset of patients who are more critically ill and have increased exposure to airway management procedures.
This study has several limitations. First, NEMSIS is a large database but is not a representative sample of US EMS activations since not all agencies in the included 40 states submit data to NEMSIS and existing data is not a weighted probability sample. Next, NEMSIS relies on data entered into an electronic patient care report by EMS providers and is subject to bias. Diagnoses are not based on specific criteria and are based on paramedic impression. It also likely suffers from self-reporting biases leading to overestimation of success and underestimation of complications. NEMSIS also has significant missing data that may introduce additional bias. It is possible that procedure success rates and complications are affected by these biases, inflating our estimates. Although these biases are likely present, comparisons with adult data or among airway interventions are less likely to be directly affected. In addition, there is little reason to suspect that systematic biases would exist in certain age groups or types of devices. Finally, the sheer size of the database makes it useful to gain an understanding of current practice on a national level.
Conclusions
ETI is the most commonly performed advanced airway procedure in children in the US. However, advanced airway procedures have lower success rates in children compared to adults. Advanced airway procedures are infrequently performed by individual providers and are likely relatively rare events in their careers. C02 based confirmation techniques were used with low rates though should be used in every pediatric intubation. Further research is needed to identify the optimal strategy for out-of-hospital airway management in pediatric patients
Acknowledgments
Role of the Funding Source
Grant support: this work is supported by the National Heart Lung and Blood Institute (NHLBI) grant number 5K12HL108974-03. This publication was also supported by Oregon Clinical and Translational Research Institute (OCTRI), grant number (UL1TR000128) from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. The study sponsors did not have involvement in study design, data collection, analysis and interpretation, writing the manuscript, or decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions: All of the authors have made substantial contributions in 1) the conception and design of the study, acquisition of the data, and/or analysis and interpretation of the data 2) drafting and revising the article for important content and 3) finally approving the submitted version.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- 1.Adewale L. Anatomy and assessment of the pediatric airway. Pediatr Anesth. 2009;19:1–8. doi: 10.1111/j.1460-9592.2009.03012.x. [DOI] [PubMed] [Google Scholar]
- 2.Babl FE, Vinci RJ, Bauchner H, Mottley L. Pediatric pre-hospital advanced life support care in an urban setting. Pediatr Emerg Care. 2001;17:5–9. doi: 10.1097/00006565-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Youngquist ST, Henderson DP, Gausche-Hill M, Goodrich SM, Poore PD, Lewis RJ. Paramedic Self-efficacy and Skill Retention in Pediatric Airway Management. Acad Emerg Med. 2008;15:1295–1303. doi: 10.1111/j.1553-2712.2008.00262.x. [DOI] [PubMed] [Google Scholar]
- 4.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA J Am Med Assoc. 2000;283:783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 5.DiRusso SM, Sullivan T, Risucci D, Nealon P, Slim M. Intubation of pediatric trauma patients in the field: predictor of negative outcome despite risk stratification. J Trauma. 2005;59:84–90. doi: 10.1097/01.ta.0000171462.28379.f3. discussion 90–1. [DOI] [PubMed] [Google Scholar]
- 6.Ehrlich PF, Seidman PS, Atallah O, Haque A, Helmkamp J. Endotracheal intubations in rural pediatric trauma patients. J Pediatr Surg. 2004;39:1376–1380. doi: 10.1016/j.jpedsurg.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Gerritse BM, Draaisma JMT, Schalkwijk A, van Grunsven PM, Scheffer GJ. Should EMS-paramedics perform paediatric tracheal intubation in the field? Resuscitation. 2008;79:225–229. doi: 10.1016/j.resuscitation.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 8.Diggs LA, Yusuf J-E (Wie), De Leo G. An update on out-of-hospital airway management practices in the United States. Resuscitation. 2014;85:885–892. doi: 10.1016/j.resuscitation.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 9.Kannikeswaran N, Mahajan PV, Dunne RB, Compton S, Knazik SR. Epidemiology of Pediatric Transports and Non-Transports in an Urban Emergency Medical Services System. Prehosp Emerg Care. 2007;11:403–407. doi: 10.1080/10903120701536677. [DOI] [PubMed] [Google Scholar]
- 10.Shah MN, Cushman JT, Davis CO, Bazarian JJ, Auinger P, Friedman B. The Epidemiology of Emergency Medical Services Use by Children: An Analysis of the National Hospital Ambulatory Medical Care Survey. Prehosp Emerg Care. 2008;12:269–276. doi: 10.1080/10903120802100167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joyce SM, Brown DE, Nelson EA. Epidemiology of pediatric EMS practice: a multistate analysis. Prehospital Disaster Med. 1996;11:180–187. doi: 10.1017/s1049023x00042928. [DOI] [PubMed] [Google Scholar]
- 12.Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: Pediatric Advanced Life Support 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S876–S908. doi: 10.1161/CIRCULATIONAHA.110.971101. [DOI] [PubMed] [Google Scholar]
- 13.Hasegawa K, Hiraide A, Chang Y, Brown DM. ASsociation of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309:257–266. doi: 10.1001/jama.2012.187612. [DOI] [PubMed] [Google Scholar]
- 14.Long E, Sabato S, Babl FE. Endotracheal intubation in the pediatric emergency department. Paediatr Anaesth. 2014 doi: 10.1111/pan.12490. published online July 15. [DOI] [PubMed] [Google Scholar]
- 15.Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med Off J Soc Acad Emerg Med. 2013;20:71–78. doi: 10.1111/acem.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sagarin MJ, Chiang V, Sakles JC, et al. Rapid sequence intubation for pediatric emergency airway management. Pediatr Emerg Care. 2002;18:417–423. doi: 10.1097/00006565-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Johnston BD, Seitz SR, Wang HE. Limited Opportunities for Paramedic Student Endotracheal Intubation Training in the Operating Room. Acad Emerg Med. 2006;13:1051–1055. doi: 10.1197/j.aem.2006.06.031. [DOI] [PubMed] [Google Scholar]
- 18.Cottrell EK, O’Brien K, Curry M, et al. Understanding Safety in Prehospital Emergency Medical Services for Children. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2014 doi: 10.3109/10903127.2013.869640. published online March 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hubble MW, Wilfong DA, Brown LH, Hertelendy A, Benner RW. A Meta-Analysis of Prehospital Airway Control Techniques Part II: Alternative Airway Devices and Cricothyrotomy Success Rates. Prehosp Emerg Care. 2010;14:515–530. doi: 10.3109/10903127.2010.497903. [DOI] [PubMed] [Google Scholar]