Abstract
Objective
Innovations in health information technology (HIT) provide opportunities to reduce health care spending, improve quality of care, and improve health outcomes for older adults. However, concerns relating to older adults’ limited access and use of HIT, including use of the Internet for health information, fuel the digital health divide debate. This study evaluated the potential digital health divide in relation to characteristic and belief differences between older adult users and nonusers of online health information sources.
Methods
A cross-sectional survey design was conducted using a random sample of older adults. A total of 225 older adults (age range = 50–92 years, M = 68.9 years, SD = 10.4) participated in the study.
Results
Seventy-six percent of all respondents had Internet access. Users and nonusers of online health information differed significantly on age (M = 66.29 vs. M = 71.13), education, and previous experience with the health care system. Users and nonusers of online health information also differed significantly on Internet and technology access, however, a large percentage of nonusers had Internet access (56.3%), desktop computers (55.9%), and laptop computers or netbooks (43.2%). Users of online health information had higher mean scores on the Computer Self-Efficacy Measure than nonusers, t(159) = −7.29, p < .0001.
Conclusion
This study found significant differences between older adult users and nonusers of online health information. Findings suggest strategies for reducing this divide and implications for health education programs to promote HIT use among older adults.
Keywords: consumer health information, e-health, health information technology, older adults, self-efficacy
Recent U.S. health care reform changes in the Patient Protection and Affordable Care Act mandate increased use of health information technology (HIT; Buntin, Jain, & Blumenthal, 2010; Hersh, 2009). Currently, meaningful use guidelines (i.e., using electronic health records to improve the quality and efficiency of care and to reduce health disparities) are requiring eligible health care providers to offer increased patient access to their online health information and provide secure messaging to communicate relevant health information; other meaningful use requirements are forthcoming (Centers for Disease Control and Prevention, 2014). These policy changes have, in part, fueled rapid growth in the e-Health technology market (i.e., delivery of health information and health resources through the Internet; World Health Organization, 2012) which are exemplified by a rapid growth in HIT tools and devices which offer an array of technology for both the prevention and self-management of chronic diseases (Bates & Bitton, 2010; Or & Karsh, 2009).
The availability of HIT provides increasing opportunities to engage and empower individuals to participate in their health care (Hall, Stellefson, & Bernhardt, 2012; Martin, 2012). Growth in the HIT market is supported by many health care providers who perceive HIT and e-Health as tools that can improve patient–provider communication, especially in the areas of patient care and education, compliance with treatment regimens, and patient access to relevant services and health information. While many market sectors perceive the increased reliance on HIT as promising, other sectors are concerned that widespread use will exacerbate the digital divide currently existing between HIT users and nonusers (Kieschnick & Raymond, 2011).
Digital Divide and Older Adults
The “digital divide” is defined as a gap between those who have access to information and communication technologies and those who do not (Bernhardt, 2000). The gap between those who access and use health information technology and those who do not is referred to as the digital health divide. This divide is characterized by concerns related to lower levels of HIT use by members of vulnerable populations. Among the most vulnerable populations are older adults because their access to health care services and technology are often compromised by access issues, and exacerbated by numerous health concerns and medical conditions. Unlike younger adult cohorts, technology use by many older adults is limited by the increased prevalence of chronic diseases, lack of experience using technology, lack of access to technology, and other limiting factors (Anderson, 2010; Czaja et al., 2013; Jimison et al., 2008).
The National Telecommunications and Information Administration (NTIA) report on broadband and Internet access estimates the 2010 nationwide adoption rate for broadband use was 68.2%, with nearly 72% of Americans using the Internet (NTIA, 2011). According to the report, most people access the Internet from home followed by work, school, public libraries, and last, someone else’s residence (NTIA, 2011). While in 2010 adults between the ages of 18 and 24 years led in broadband use, older adults showed the largest growth rate from the previous year; however, overall, in adults 55 years and older, rates of broadband use at home equaled 50.1% compared with 80.5% among younger adults (NTIA, 2011).
NTIA findings are consistent with other national findings, reporting that 70% of Americans have broadband access at home (Zickuhr, 2013). According to recent Pew Internet and American Life Project data, 53% of adults 65 years and older use the Internet or e-mail, and 70% of those who access the Internet do so daily (Zickuhr & Madden, 2012). However, after age 75 this percentage decreases significantly. Among this group 34% access the Internet and 21% report home broadband use (Zickuhr & Madden, 2012). Furthermore, a survey exploring computer and Internet experience and use among younger (n = 430, aged 18–28 years) and older (n = 251, aged 65–90 years) adults found significant differences between groups, specifically, 80% of older adults reported experience with a computer, but less than 50% reported use of the Internet, compared with 99% and 90% of younger adults, respectively (Olson, O’Brian, Rogers, & Charness, 2011).
Health Information Technology Engagement and Older Adults
Technology and mobile device use among older adults is increasing with mobile phone ownership among adults 65 years and older at 69%, along with other technology use/ownership as follows: desktop computers = 48%, laptop computers = 32%, e-readers = 11%, and tablets = 8%. Among adults aged 76 years and older, technology use/ownership includes cell phones = 56%, desktop computers = 31%, laptops = 20%, e-readers = 5%, and tablets = 3% (Zickuhr & Madden, 2012).
Recent trend reports show an increase in the number of adults who access health information online (Zickuhr & Madden, 2012). Specifically, among U.S. adults aged 18 years and older, approximately 74% use the Internet, and among those who use the Internet, 80% report searching for health information online (Fox, 2011). However, among adults aged 66 to 74 years, the percentage accessing the Internet for health information drops to 63%, and further decreases to 49% for adults aged 75 years and older (Rainie, 2012).
Health information seeking is defined as the search for knowledge or advice to help lessen uncertainty and increase understanding about one’s health status (Cotten & Gupta, 2004). In a sample of 713 primary care patients, Kruse et al. reported Internet use by 78% of the sample. Predictors of Internet use included age, income, socioeconomic status, health status, and lack of chronic conditions; however, age was the strongest predictor of Internet use among patients with chronic diseases (Kruse et al., 2012). In a sample of 385 respondents Cotten and Gupta (2004) found that age, income, education, and health were defining characteristics between online and offline health information seekers.
Another predictive factor of HIT use among older adults is self-efficacy. According to Bandura’s (1994) self-efficacy theory, beliefs demonstrate stability with advancing age and this theoretical framework is measured by assessing individual perceptions of confidence or skill level when performing a particular task or behavior (Bandura, 1997). Lower levels of self-efficacy predict less engagement in a particular behavior (Bandura, 1997; Lorig, 2001). In previous studies, measures of self-efficacy predicted technology use and engagement (Chu, Huber, Mastel-Smith, & Cesario, 2009; Cranney et al., 2002; Czaja et al., 2006).
For instance, Campbell (2004) developed the Computer Self-efficacy Measure (CSEM) to determine individual self-efficacy levels for use of computers, online search tools, online searches for health information, and managing personal health care online. The CSEM was initially tested and implemented in a population of older women (Campbell, 2004). The CSEM instrument was later modified slightly and further validated for content by Chu et al. (2009) for use in an online health information education intervention among older adults in a low socioeconomic community; results of the study found that computer self-efficacy increased significantly from baseline during the 5-week intervention, and remained high 6 weeks after study completion. Approximately 95% of participants reported more confidence for finding and evaluating online health information, planned to use information they found online to manage their chronic illnesses, and would share information with friends and family (Chu et al., 2009).
Digital Health Divide
Despite increasing Internet use among older adults, a digital divide persists between older adult users and nonusers of the Internet and other new media. Furthermore, an important, yet less studied concern, is the digital health divide. The purpose of this study with older adults was to (a) examine differences in technology access and use between users and nonusers of online health information, (b) assess the differences between users and nonusers, and (c) to determine the presence of a digital health divide among users and nonusers of HIT. The following hypotheses were tested:
-
Hypothesis 1
Users will have higher Computer Self-Efficacy Measure than nonusers.
-
Hypothesis 2
Use of the Internet or World Wide Web sites for health information will moderate the relationship between Computer Self-Efficacy Measures and age.
Materials and Method
A telephone survey was administered to 225 English-speaking Florida residents aged 50 years and older by the Bureau of Economic and Business Research at the University of Florida using random digital dialing to contact landline telephone numbers. Approval for this study was granted through the University of Florida’s Institutional Review Board. Trained telephone interviewers collected all data. To account for gender nonresponse bias, using random digital dialing sampling methods, the interview script directed interviewers to initially ask to speak with a male household resident aged 50 years or older. If a male fitting the criteria was not available, the interviewer asked to speak with a female household resident aged 50 years or older (Hu, Pierannunzi, & Balluz, 2011).
On reaching an eligible respondent interviewers read the informed consent script. Once an eligible respondent verbally consented, they were read each survey question and all response options. The survey was pilot tested and refined to ensure item clarity. Respondents were not asked to provide any identifiable or confidential information.
Data collection occurred during a 6-week period between April and May of 2013. The total number of dialed calls was 4,524 and a total of 957 potential respondents were reached. A total of 159 of the 957 potential respondents were excluded from participation for not meeting the inclusion criteria (i.e., able to speak English and be 50 years or older). Refusals from eligible respondents totaled 573, yielding a final sample of 225 eligible respondents with a response rate of 28.2% eligible respondents.
Measures
Online health information use was measured using the following yes/no question: “During the past 12 months have you sought information regarding a health concern or medical problem from the Internet or World Wide websites?” (Cotten & Gupta, 2004). Respondents affirming use of “Internet or World Wide websites” were asked additional questions relating to their frequency of use (i.e., daily, weekly, monthly, or more than monthly), preferred health information websites, and if during the past 12 months they had used the Internet to keep track of personal health information (Fox, 2011; Lustria, Smith, & Hinnant, 2011).
Technology access was measured by reading respondents a list of technology devices (i.e., a desktop computer, a cell phone, etc.) and asking them to identify any that were available in their homes. Respondents answering “yes” to owning cell phones were asked additional questions concerning their use of cell phones for accessing health information, and whether they used software applications (apps) to track or manage their health. Internet access was measured with the yes/no question: “Do you access the Internet or World Wide Web at home, from work or any other location?” (Fox, 2011; Health Information National Trends Survey, 2013). Older adults’ confidence in using computers, the Internet, searching for health information, and managing personal health care online was assessed via the CSEM (Chu et al., 2009).
Analysis
All analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC). Tests of reliability for internal consistency of the CSEM were performed using a standardized Cronbach’s alpha (α = .91). Univariate analyses were performed to examine the frequency and distribution of study variables; bivariate and multivariate analyses were used to test Hypotheses 1 and 2. Pearson chi-square (χ2) tests were performed to detect differences between independent variables among users and nonusers. A confirmatory factor analysis for latent variables was conducted on the CSEM using Mplus 7.1 (Muthén & Muthén, Los Angeles, CA). Factors and model fit were tested using the goodness-of-fit indices criteria on the comparative fit index (CFI) ≥.95 and root mean square error of approximation (RMSEA) <.05.
Results
Respondent Characteristics
Respondents (N = 225) consisted of adults ranging in age from 50 to 92 years (M = 68.9 years, SD = 10.4); 45.8% were male; 87.6% were White, 6.7% Black, and 6.3% Hispanic. Overall, the majority (78.1%) of respondents had some college education or greater, while approximately 22% had a high school education or less. The majority (64.5%) reported their health status as “good” or “very good” even though most respondents reported living with one or more chronic conditions. Regarding previous experience with the health care system, 67.1% had close friends or family members in the medical field and 44.4% reported taking a health-related course or emergency training (i.e., cardiopulmonary resuscitation) at some time in the past.
Users (n = 105) and nonusers (n = 119) did not differ significantly on self-reported race, gender, health status, or chronic disease. The two groups differed significantly on education, χ2(5, N = 222) = 11.47, p = .04; age, χ2(2, N = 220) = 16.65, p = .0002; and experience with the health care system, with users significantly more likely to report “having taken health-related courses or emergency training,” χ2(1, N = 224) = 4.79, p = .03.
Health Information Technology Access and the Digital Health Divide
Technology access and use among users and nonusers is presented in Table 1. More than three quarters (76%) of respondents reported having access to the Internet. Almost all users (99.1%) reported having Internet access and more than half (56.1%) of nonusers also reported having Internet access χ2(1, N = 224) = 56.43, p < .0001. The majority of all respondents reported home access to cell phones (79%), desktop computers (65.6%), and laptop computers or netbooks (58.6%); fewer respondents had home access to tablet computers (34.8%), electronic book devices (29.6%), iPods or other MP3 players (29.5%), or game consoles (17.9%). Overall, when compared with nonusers, users reported significantly more home access to all types of technology.
Table 1.
Technology Access and Use Between Users and Nonusers of Online Health Information by Age.
| Technology Access and Use | Users of Online Health Information (n = 105) | Nonuser of Online Health Information (n = 119) | Total (N = 225) | pa |
|---|---|---|---|---|
| Access to Internet (%) | 99.1 | 56.3 | 76.0 | <.0001 |
| 50–64 (years) | 100 | 75.8 | 90.0 | |
| 65–74 (years) | 100 | 56.3 | 80.3 | |
| 75+ (years) | 94.7 | 46.0 | 58.6 | |
| Technology use | ||||
| Desktop computer | 77.1 | 55.9 | 65.6 | .0009 |
| 50–64 (years) | 72.3 | 66.7 | 70.0 | |
| 65–74 (years) | 76.9 | 51.6 | 65.7 | |
| 75+ (years) | 89.5 | 52.0 | 61.4 | |
| Laptop computer or netbook | 76.7 | 43.2 | 58.6 | <.0001 |
| 50–64 (years) | 87.0 | 68.8 | 79.5 | |
| 65–74 (years) | 73.7 | 56.3 | 65.7 | |
| 75+ (years) | 57.9 | 20.0 | 30.0 | |
| Tablet computer (iPad) | 48.1 | 23.5 | 34.8 | .0001 |
| 50–64 (years) | 56.5 | 39.4 | 49.4 | |
| 65–74 (years) | 53.9 | 25.0 | 40.8 | |
| 75+ (years) | 15.8 | 14.0 | 14.3 | |
| Electronic book device | 37.5 | 22.9 | 29.6 | .0174 |
| 50–64 (years) | 39.1 | 30.3 | 35.4 | |
| 65–74 (years) | 41.0 | 31.3 | 36.6 | |
| 75+ (years) | 26.3 | 14.0 | 17.1 | |
| Cell phone or mobile device | 85.6 | 73.1 | 79.0 | .0228 |
| 50–64 (years) | 87.0 | 78.8 | 83.5 | |
| 65–74 (years) | 89.7 | 78.1 | 84.5 | |
| 75+ (years) | 73.7 | 70.0 | 71.4 | |
| iPod or other MP3 player | 44.8 | 16.1 | 29.5 | <.0001 |
| 50–64 (years) | 61.7 | 24.2 | 46.2 | |
| 65–74 (years) | 41.0 | 21.9 | 32.4 | |
| 75+ (years) | 10.5 | 8.0 | 8.6 | |
| Game console (Xbox or Play Station) | 23.8 | 12.7 | 17.9 | .0311 |
| 50–64 (years) | 34.0 | 33.3 | 33.7 | |
| 65–74 (years) | 23.1 | 9.4 | 16.9 | |
| 75+ (years) | 0.0 | 2.0 | 1.4 | |
Pearson chi-square.
Respondents reporting use of the Internet or World Wide Web sites for health information or having access to a cell phone were asked additional questions about technology use for health information. Users reported use of the Internet, daily (4%), weekly (18%), monthly (48%), and more than monthly (30%). Almost half of the users (45.7%) were able to name a preferred health website and a third reported keeping track of personal health information online. The most preferred health website mentioned by respondents was WebMD followed by Mayo Clinic. Among respondents responding “yes” to having a cell phone, 15.3% had used a cell phone in the past 12 months to look up health or medical information and 12.1% reported tracking or managing their health via use of a health app.
Computer Self-Efficacy
A t test was performed to detect CSEM mean score differences between users and nonusers. CSEM scores were found to differ significantly between users and nonusers. Therefore, Hypothesis 1 was supported. Table 2 offers additional information.
Table 2.
Computer Self-Efficacy Differences Between Users and Nonusers of Online Health Information.
| Measure | Users of Online Health Information
|
Nonusers of Online Health Information
|
Cohen’s d | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | CI
|
M | SD | CI
|
||||
| LL | UL | LL | UL | ||||||
| Computer self-efficacya | 17.39 | 2.39 | 16.9b | 17.9b | 13.43 | 5.19 | 12.5b | 14.4b | .98 |
Note. CI = confidence interval; LL = lower limit; UL = upper limit; M = mean; SD = standard deviation.
Higher scores correspond with higher levels of computer self-efficacy.
95% CI more self-reliant.
p < .05, one-tailed.
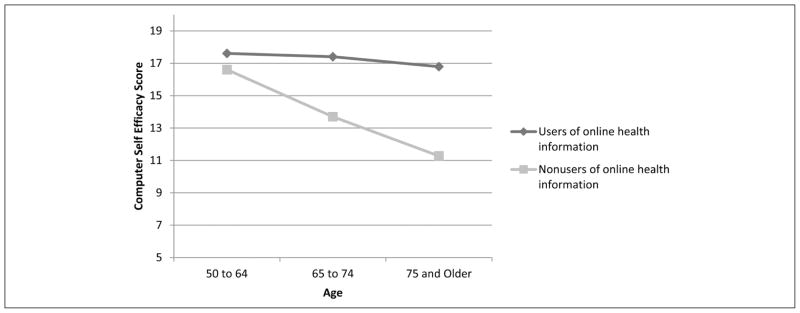
Using the CSEM scores, an ANOVA was used to evaluate the effects of age (50–64 years, 65–74 years, and 75+ years) and use of the Internet or World Wide Web sites for users and nonusers. Significant effects included age, F(2, 213) = 10.68, p ≤ .0001, ω2 = .064; World Wide Web sites, F(1, 213) = 40.00, p ≤ .0001, ω2 = .128; and Age × World Wide Web sites, F(2, 213) = 5.98, p = .003, ω2 = .032; mean square error (MSE) for each of the effects is 3.77. CSEM scores were found to be lower between nonusers and users across all age groups: users 50 to 64 years (M = 17.61) versus nonusers 50 to 64 years (M = 16.61); users 65 to 74 years (M = 17.44) versus nonusers 65 to 74 years (M = 13.7); and users ages 75+ (M = 16.79) versus nonusers ages 75+ (M = 11.28). Post hoc comparison tests on age and World Wide Web sites (Q Table, Tukey–Kramer) indicated statistically significant differences between the 65-to-74 nonuser and user age groups, p < .05, and between the 75+ nonuser and user age groups, p < .05 (see Figure 1). Therefore, Hypothesis 2 was not supported.
Figure 1.
CSEM scores by age group betweeen users and nonusers of online health information.
Discussion
A number of initiatives are currently underway to address digital divide concerns among older adults. For example, recent health care reform and health care IT adoption incentive programs show promise in reducing technology and health care access barriers among seniors. Programs and initiatives such as Healthy People 2020, the American Reinvestment and Recovery Act, “meaningful use” guidelines and regulations for electronic health record investment reimbursements, and accountable care organizations all promote the development of electronic methods to better engage patients in their health care (Kieschnick & Raymond, 2011; Monsen et al., 2012; Shrewsbury, 2002).
Several studies have focused on the existence of a “digital divide” between older and younger adults, as well as the characteristic differences between these groups and their use of online health information (Cotten & Gupta, 2004; Kieschnick & Raymond, 2011; Kruse et al., 2012; Olson et al., 2011; Ybarra & Suman, 2005; Zickuhr & Madden, 2012). The literature also offers information on adults’ online searches for medical topics and barriers to technology use (Couper et al., 2010; Fox & Duggan, 2013; Gatto & Tak, 2008; Jimison et al., 2008; Schwartz et al., 2006). However, to date, the literature lacks research confirming and quantifying the existence of a possible digital health divide among older adults or investigating CSEMs among older adult users and nonusers. The current study examined differences between older adult users and nonusers of online health information and their perceptions of computer self-efficacy, which updates information on older adult HIT engagement in the following age groups: 50 to 64, 65 to 74, and 75+ years. This research also contributes to the body of literature regarding the trends of technology access and use among older adults.
As expected, comparisons of these findings to 2012 national data confirm that older adults now have greater access to both technology and the Internet than in previous years, particularly respondents aged 65 years or older (Zickuhr & Madden, 2012). Additionally, in the present study, a higher percentage of respondents reported using the Internet for managing online personal health information (Lustria et al., 2011). Overall, study findings imply that, among older adults, population-level digital divide initiatives may have been successful in increasing access to technology.
Despite the overall growth of access, significant differences remain between users and nonusers. Specifically, users in this study were younger and more educated, which is consistent with previous data (Cotten & Gupta, 2004; Fox & Duggan, 2013). However, more than 50% of “nonuser” respondents reported access to desktop computers and the Internet. Interestingly, even though these respondents had access to technology and the Internet they did not report using it to obtain information related to any health or medical concerns. Access to the Internet and technology still remained higher in the “user” group. Therefore, to prevent widening of the digital health divide, interventions (i.e., adaptive devices, technology assistance, or physician-advised health websites and applications) and educational programs are recommended to encourage HIT engagement by older adults with online access, particularly adults older than 65 years with lower levels of education (Chu et al., 2009). More research is needed to confirm the presence of the digital health divide, as well as to identify contributing factors.
To our knowledge this is the first study to use the CSEM in relation to online health information use among older adults. Among this random sample of older adults, self-efficacy mean scores were higher among users of online health information. This finding is not surprising since one’s perceived self-efficacy is directly associated with their level of confidence when performing a task or behavior. Therefore, higher levels of computer self-efficacy would be expected to predict greater use of computer technology (Bandura, 1997; Lorig, 2001).
In this sample, mean computer self-efficacy scores were higher than nonuser scores across all age groups. However, the gap in self-efficacy mean scores between the 50- to 64-year-old user and nonuser groups was less extreme and with increasing age the gap widened significantly. These findings are particularly important in light of more recent findings presented in the Pew Internet and American Life Project. The report describes that Internet use between adults aged 70 to 74 years and adults aged 75 to 79 years to 80+ declined significantly (Smith, 2014), with the majority of older adults reporting the need for assistance or support when learning to use new technology. Although, older adults reported that once they became engaged online they remained engaged and felt that access to online information was beneficial (Smith, 2014).
Therefore, findings from this study expand the work conducted by Chu et al. (2009) and promote the use of educational programs designed to encourage older adults use of HIT (i.e., online health information searches and to manage personal health care via the Internet), while fostering activities to increase their computer self-efficacy. Programs offering these components will likely improve the health outcomes of attendees. Findings suggest that courses or applications designed to increase computer self-efficacy in older adults may serve to promote sustained computer self-efficacy and use of the Internet for seeking health information. Program evaluation will be critical to determine the sustainability of older adult computer use and HIT engagement over time. Additionally, the association between one’s perceived self-efficacy and willingness to engage in specific behaviors confirms the need for health care providers to use validated instruments such as the CSEM to assess an older adult’s perceived level of self-efficacy in relation to any newly recommended online health education program or health information site.
Limitations
This study used a random digit dialing sample to collect respondent data; however, findings are generalizable only to similar populations of adults aged 50 years and older, residing in the state of Florida. The study sample was limited to respondents with landline telephones. This limits applicability of findings to only adults in households with landlines and excludes respondents owning a cell phone. Data were self-reported and measures may be limited by response bias and respondent interpretation of questions. Furthermore, respondents may have responded to questions in a socially desirable manner by providing responses assumed to be favorable to the interviewer. The results of this study are limited to the time in which the survey was administered and provide information from respondents at this one point in time.
Conclusion
HIT initiatives designed to help slow rising health care costs and to improve the quality of health care will continue to enter the marketplace. However, among older adult populations these programs and initiatives must be monitored closely to prevent the unintentional widening of the digital health divide. Results of this study provide insight into the differences between older adult users and nonusers and the presence of a digital health divide. As HIT continues to rapidly diffuse and becomes standard in medical practices used throughout the country, it is increasingly important to replicate and expand this line of research to better understand and address the digital divides that may otherwise prevent older adults from fully benefiting from these technologies.
Acknowledgments
Funding
The authors declared the following financial support for the research, authorship, and/or publication of this article: Author Amanda K. Hall’s work was supported in part by the National Institutes of Health, National Library of Medicine (NLM) Biomedical and Health Informatics Training Program at the University of Washington (Grant Nr. T15LM007442).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anderson G. Chronic conditions: Making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation; 2010. Retrieved from http://www.rwjf.org/content/dam/farm/reports/reports/2010/rwjf54583. [Google Scholar]
- Bandura A. Self-efficacy. In: Ramachandran VS, editor. Encyclopedia of human behavior. Vol. 4. New York, NY: Academic Press; 1994. pp. 71–81. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: W.H. Freeman; 1997. [Google Scholar]
- Bates DW, Bitton A. The future of health information technology in the patient-centered medical home. Health Affairs. 2010;29:614–621. doi: 10.1377/hlthaff.2010.0007. [DOI] [PubMed] [Google Scholar]
- Bernhardt JM. Health education and the digital divide: Building bridges and filling chasms. Health Education Research. 2000;15:527–531. doi: 10.1093/her/15.5.527. [DOI] [PubMed] [Google Scholar]
- Buntin MB, Jain SH, Blumenthal D. Health information technology: Laying the infrastructure for national health reform. Health Affairs. 2010;29:1214–1219. doi: 10.1377/hlthaff.2010.0503. [DOI] [PubMed] [Google Scholar]
- Campbell R. Older woman and the internet. Journal of Women and Aging. 2004;16:161–174. doi: 10.1300/J074v16n01_11. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. About meaningful use. 2014 May 23; Retrieved from http://www.cdc.gov/ehrmeaningfuluse/
- Chu A, Huber J, Mastel-Smith B, Cesario S. “Partnering with seniors for better health”: Computer use and internet health information retrieval among older adults in a low socioeconomic community. Journal of the Medical Library Association. 2009;97:12–20. doi: 10.3163/1536-5050.97.1.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotten SR, Gupta SS. Characteristics of online and offline health information seekers and factors that discriminate between them. Social Science & Medicine. 2004;59:1795–1806. doi: 10.1016/j.socscimed.2004.02.020. [DOI] [PubMed] [Google Scholar]
- Couper MP, Singer E, Levin CA, Fowler FJ, Jr, Fagerlin A, Zikmund-Fisher BJ. Use of the internet and ratings of information sources for medical decisions: Results from the DECISIONS survey. Medical Decision Making. 2010;30(5 Suppl):106S–114S. doi: 10.1177/0272989X10377661. [DOI] [PubMed] [Google Scholar]
- Cranney A, O’Connor AM, Jacobsen MJ, Tugwell P, Adachi JD, Ooi DS, Wells GA. Development and pilot testing of a decision aid for postmenopausal women with osteoporosis. Patient Education and Counseling. 2002;47:245–255. doi: 10.1016/s0738-3991(01)00218-x. [DOI] [PubMed] [Google Scholar]
- Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, Sharit J. Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE) Psychology and Aging. 2006;21:333–352. doi: 10.1037/08827974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czaja SJ, Sharit J, Lee CC, Nair SN, Hernández MA, Arana N, Fu SH. Factors influencing use of an e-health website in a community sample of older adults. Journal of the American Medical Informatics Association. 2013;20:277–284. doi: 10.1136/amiajnl-2012-000876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S. The social life of health information. Pew Internet and American Life Project; 2011. May 12, Retrieved from http://pewinternet.org/~/media//Files/Reports/2011/PIP_Social_Life_of_Health_Info.pdf. [Google Scholar]
- Fox S, Duggan M. Health online. Pew Internet and American Life Project; 2013. Jan 15, Retrieved from http://www.pewinternet.org/~/media//Files/Reports/PIP_HealthOnline.pdf. [Google Scholar]
- Gatto SL, Tak SH. Computer, Internet, and e-mail use among older adults: Benefits and barriers. Educational Gerontology. 2008;34:800–811. [Google Scholar]
- Hall AK, Stellefson M, Bernhardt JM. Healthy aging 2.0: The potential of new media and technology. Preventing Chronic Disease. 2012;9:E67. Retrieved from http://dx.doi.org/10.5888/pcd9.110241. [PMC free article] [PubMed] [Google Scholar]
- Health Information National Trends Survey. What does HINTS tell us about . . . Internet use. 2009 Retrieved from http://hints.cancer.gov/topic.aspx?section=Internet+Use.
- Hersh W. A stimulus to define informatics and health information technology. BMC Medical Informatics and Decision Making. 2009;9(1):24. doi: 10.1186/1472-6947-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu SS, Pierannunzi C, Balluz L. The impact of a mixed-mode data collection design on response and non-response bias on a RDD Landline Telephone Survey. Proceedings of the AAPOR 66th Annual Conference; Deerfield, IL: American Association for Public Opinion Research; 2011. pp. 5659–5666. Retrieved from http://www.amstat.org/Sections/Srms/Proceedings/y2011/Files/400166.pdf. [Google Scholar]
- Jimison H, Gorman P, Woods S, Nygren P, Walker M, Norris S, Hersh W. Evidence Reports/Technology Assessment, No. 175. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Nov, Barriers and drivers of health information technology use for the elderly, chronically III, and underserved. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK38653. [PMC free article] [PubMed] [Google Scholar]
- Kieschnick T, Raymond B. Health IT roundtable background paper. Oakland, CA: Kaiser Permanente Institute for Health Policy; 2011. Mar 7, Can health IT promote health equity and patient-centered care? Retrieved from http://www.amia.org/sites/amia.org/files/Roundtable-Background-Paper-2011.pdf. [Google Scholar]
- Kruse RL, Koopman RJ, Wakefield BJ, Wakefield DS, Keplinger LE, Canfield SM, Mehr DR. Internet use by primary care patients. Family Medicine. 2012;44:342–347. [PubMed] [Google Scholar]
- Lorig K. Patient education: A practical approach. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- Lustria ML, Smith SA, Hinnant CC. Exploring digital divides: An examination of eHealth technology use in health information seeking, communication and personal health information management in the USA. Health Informatics Journal. 2011;17:224–243. doi: 10.1177/1460458211414843. [DOI] [PubMed] [Google Scholar]
- Martin T. Assessing mHealth: Opportunities and barriers to patient engagement. Journal of Health Care for the Poor and Underserved. 2012;23:935–941. doi: 10.1353/hpu.2012.0087. [DOI] [PubMed] [Google Scholar]
- Monsen KA, Westra BL, Paitich N, Ekstrom D, Mehle SC, Kaeding M, Ruddarraju UK. Developing a personal health record for community dwelling older adults and clinicians: Technology and content. Journal of Gerontological Nursing. 2012;38(7):21–25. doi: 10.3928/00989134-20120605-03. [DOI] [PubMed] [Google Scholar]
- National Telecommunications and Information Administration. Digital nation; expanding Internet usage. 2011 Feb; Retrieved from http://www.ntia.doc.gov/files/ntia/publications/ntia_internet_use_report_february_2011.pdf.
- Olson KE, O’Brien MA, Rogers WA, Charness N. Diffusion of technology: Frequency of use for younger and older adults. Ageing International. 2011;36:123–145. doi: 10.1007/s12126-010-9077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Or CKL, Karsh BT. A systematic review of patient acceptance of consumer health information technology. Journal of the American Medical Informatics Association. 2009;16:550–560. doi: 10.1197/jamia.M2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rainie L. Senior citizens and digital technology. Pew Internet and American Life Project; 2012. Sep 15, Retrieved from http://www.slideshare.net/PewInternet/senior-citizens-and-digital-technology. [Google Scholar]
- Schwartz KL, Roe T, Northrup J, Meza J, Seifeldin R, Neale AV. Family medicine patients’ use of the Internet for health information: A MetroNet study. Journal of the American Board of Family Medicine. 2006;19:39–45. doi: 10.3122/jabfm.19.1.39. [DOI] [PubMed] [Google Scholar]
- Shrewsbury CM. Information technology issues in an era of greater state responsibilities. Journal of Aging & Social Policy. 2002;14(3–4):195–209. doi: 10.1300/j031v14n03_11. [DOI] [PubMed] [Google Scholar]
- Smith A. Older adult and technology use. Pew Internet and American Life Project; 2014. Apr 3, Retrieved from http://www.pewinternet.org/files/2014/04/PIP_Seniors-and-Tech-Use_040314.pdf. [Google Scholar]
- World Health Organization. e-Health. 2012 Retrieved from http://www.who.int/trade/glossary/story021/en/
- Ybarra ML, Suman M. Help seeking behavior and the internet: A national survey. International Journal of Medical Informatics. 2006;75:29–41. doi: 10.1016/j.ijmedinf.2005.07.029. [DOI] [PubMed] [Google Scholar]
- Zickuhr K. Home broadband 2013. Pew Internet and American Life Project; 2013. Aug 26, Retrieved from http://www.pewinternet.org/Press-Releases/2013/Home-Broadband-2013.aspx. [Google Scholar]
- Zickuhr K, Madden M. Older adults and internet use. Pew Internet and American Life Project; 2012. Jun 6, Retrieved from http://pewinternet.org/~/media//Files/Reports/2012/PIP_Older_adults_and_internet_use.pdf. [Google Scholar]