Abstract
BACKGROUND
Often psychosocial interventions address only one domain of quality of life (QOL), are offered to early stage cancer patients, do not include the caregiver, and are delivered after cancer treatment has been completed.
METHODS
In this randomized controlled trial, 131 radiation therapy patients with advanced cancer and their caregivers were randomly assigned to either a six-session structured multidisciplinary intervention arm or a standard care arm. Average age of the patients was 58 years, most were male (63%), and tumor types varied: gastrointestinal (37%), brain (22%), head and neck (16%), lung (13%), and other (12%). The six 90-minute sessions addressed the five domains of QOL: cognitive, physical, emotional, social, and spiritual. The in-person intervention was followed by ten brief telephone counseling sessions over the next six months.
RESULTS
Of the 117 study completers, overall QOL (assessed by FACT-G) at week 4 was significantly higher (75.2) in the intervention group (n = 54) compared with the standard arm (n = 63) control group (68.7; p=0.02). The ten brief telephone contacts did not impact QOL as at week 27 the groups had identical QOL (means of 77.6 and 77.7). There was no effect of the intervention on caregiver QOL.
CONCLUSIONS
Participating in a six-session multidisciplinary intervention was effective in maintaining the QOL of patients with advanced cancer who were actively receiving radiation therapy. The QOL and symptom burden of this population is striking, making it important to identify effective QOL strategies to implement in conjunction with cancer care.
Keywords: Quality of Life, Radiation Therapy, Caregivers, Support Groups, Advanced Cancer
INTRODUCTION
Quality of life (QOL) can be defined as a hierarchical multidimensional construct consisting of a primary overall QOL and five sub-domains of cognitive, physical, emotional, social, and spiritual functioning.1, 2 Many cancer patients experience reduction in their QOL during and after cancer treatment.3, 4 This reduction in QOL is understandable as during the intense period of cancer treatment, many will experience pain, fatigue, nausea, sleep disturbance, spiritual uncertainty, distress, mood disturbance, mental status difficulties, or relationship challenges.5-7
Given the symptom burden associated with cancer treatment, it is our premise that QOL interventions should be offered during cancer treatment.1 Unfortunately many previous interventions have focused primarily on psychosocial issues (distress, education, coping skills, or communication),8 rather than seeking to most effectively improve patients’ overall QOL by targeting all five QOL domains. Others who have adopted this approach—e.g., an intervention designed to improve QOL of women surgically treated for breast cancer—have included strategies for improvement of health behaviors, stress reduction, problem solving, support, assertiveness, increasing physical activity, coping with treatment side effects, and adherence to medical treatment.9 We previously found in a study of 103 radiation therapy patients with advanced cancer, participation in an eight-session structured multidisciplinary QOL intervention maintained QOL during cancer treatment,2 and their caregivers recommended that caregivers be included in the QOL intervention.10
Therefore, this project's primary aim was to replicate our previous finding that a multidisciplinary intervention can maintain QOL of advanced cancer patients actively receiving radiation therapy, providing further empirical support for the delivery of QOL interventions during active cancer treatment. The secondary aims were to positively impact caregiver QOL by including them in the intervention and to improve long-term patient QOL by providing ongoing support through regular telephone contact during the 6-month follow-up period.
METHODS
Design
A randomized, two-group, controlled clinical trial was conducted to compare the efficacy of a six-session structured multidisciplinary intervention including caregivers and ten brief telephone counseling sessions to standard care in maintaining overall QOL of patients with advanced cancer undergoing radiation therapy. The primary endpoint was the patients’ FACT-G score at week 4. The study was reviewed and approved by the Institutional Review Board.
Participants were recruited from adult advanced cancer patients at the cancer center who were scheduled to undergo radiation therapy. Eligibility criteria included at least 18 years of age, initial diagnosis of cancer within the previous 12 months, intermediate to poor prognosis (0%-50% expected 5-year survival judged by the primary radiation oncologist enrolling the participant), Eastern Cooperative Oncology Group (ECOG) performance status of 0, 1, or 2, scheduled for at least one week of radiation therapy, and a caregiver also willing to participate. Exclusion criteria included Mini-Mental State Examination (MMSE) score <20, expected survival <6 months, active substance abuse (alcohol or drug), participation in other psychosocial trials, active untreated thought disorder (e.g., bipolar disorder or schizophrenia), suicide risk, or in need of psychiatric hospitalization. Participants receiving psychotropic medications or counseling were not excluded.
Procedures
The study coordinator approached all patients meeting study eligibility criteria. Written informed consent was obtained from each participant (patients and caregivers) prior to study participation. A psychologist or psychiatrist screened potential participants for disqualifying psychiatric disorders and active suicidality. Participants were randomly assigned to either the structured intervention arm or the standard medical care arm. For intervention group participants, a physiatrist provided medical clearance and guidance for the physical therapy component. Stratification for type of primary malignant disease, ECOG performance status, age, and treatment planned was undertaken.
Participants provided demographic data at baseline (Table 1) and completed study questionnaires before starting the intervention. Because there was rolling entry onto the intervention group, participants attended the six sessions in no particular order. The intervention was delivered on Tuesdays, Wednesdays, and Thursdays; caregivers attended only the Tuesday and Thursday sessions. The number of patients in the intervention at any time ranged from one to four with up to an additional four caregivers. At baseline, week 4, and week 27, all participants received a study packet questionnaire. A study psychologist (master's or doctoral level) completed the majority of the structured brief telephone contacts. A physical therapist made the week 8 and week 18 calls. Intervention participants were included in the analysis for the primary endpoint if they completed at least four of the six sessions (two-thirds of the intervention) and completed both baseline and week 4 questionnaires.
Table 1.
Baseline Participant and Caregiver Characteristics
| Characteristics | Intervention Group (n=65) | Control Group (n=66) |
|---|---|---|
| Participants | ||
| Age, years: Mean (sd) | 58.7 (10.6) | 59.9 (10.9) |
| Sex | ||
| Female | 24 (37%) | 21 (32%) |
| Male | 41 (63%) | 45 (68%) |
| Race | ||
| Caucasian | 63 (97%) | 64 (97%) |
| Currently Employed | ||
| Yes | 37 (57%) | 40 (61%) |
| Marital Status | ||
| Divorced | 0 | 6 (9%) |
| Married | 59 (91%) | 56 (85%) |
| Single | 1 (2%) | 2 (3%) |
| Widowed | 5 (7%) | 2 (3%) |
| Religiouis Affiliation | ||
| Catholic | 18 (28%) | 28 (42%) |
| Protestant | 39 (60%) | 35 (53%) |
| None | 5 (8%) | 2 (3%) |
| Other | 3 (4%) | 1 (2%) |
| MMSE Score: Mean (sd) | 29.1 (1.3) | 29.2 (1.2) |
| ECOG PS, Fully Active | 33 (52%) | 31 (48%) |
| Beck Depression Inventory: Mean (sd) | 10.3 (7.0) | 9.6 (4.9) |
| Tumor Type | ||
| Brain | 11 (17%) | 18 (27%) |
| Gastrointestinal | 25 (39%) | 24 (36%) |
| Head and Neck | 10 (15%) | 11 (17%) |
| Lung | 10 (15%) | 7 (11%) |
| Other | 9 (14%) | 6 (9%) |
| Current Chemotherapy | 56 (86%) | 57 (86%) |
| Prior Surgery | 60 (92%) | 64 (97%) |
|
Caregivers | ||
| Significant Other | 80% | 78% |
| Currently Employed | 41 (63%) | 40 (61%) |
| Marital Status | ||
| Divorced | 3 (5%) | 4 (6%) |
| Married | 57 (7%) | 58 (88%) |
| Single | 3 (5%) | 3 (4%) |
| Widowed | 2 (3%) | 1 (2%) |
Measures
Screening Measures
ECOG Performance Index is a numeric representation of an individual's ability to do daily work and their need for assistance. The scale ranges from 0 (normal with no complaints) to 5 (dead). The Mini-Mental State Examination (MMSE) is the most widely used screening test for assessing mental status and dementia and includes items relating to orientation, memory, executive functions, and language.11 The Beck Depression Inventory-II (BDI-II) is a 21-item scale to assess current severity of depression symptomatology. The BDI-II closely corresponds to diagnostic criteria for depression;12, 13 a study psychologist or psychiatrist reviewed the BDI-II with patients as part of the enrollment process.
Pre- and Post-Intervention Assessments
Patient
The Functional Assessment of Cancer Therapy-General (FACT-G Version 4)14, 15 is a well-validated 28-item general patient-rated QOL life measure for cancer patients with any tumor type. Each item is scored from 0 to 4, anchored from “not at all” to “very much.” There are four subscales: Functional Well-Being (7 items), Physical Well-Being (7 items), Social/Family Well-Being (7 items), and Emotional Well-Being (6 items). The FACT-G total score is the sum of the subscales, and ranges from 0 to 108. The FACT-G has been used widely in clinical trials, is easy to complete, and has demonstrated sensitivity according to performance status and extent of disease.
Caregiver
The Caregiver Quality of Life Index-Cancer Scale is a 35-item, 5-point Likert-type scale16 that assesses the physical, social, financial, psychological, caregiver burden, and family dimensions of QOL. Internal consistency has ranged from 0.87 to 0.90, test-retest reliability from 0.69 to 0.95, and content, discriminant, and group validity in cancer populations has been established.17
Participants
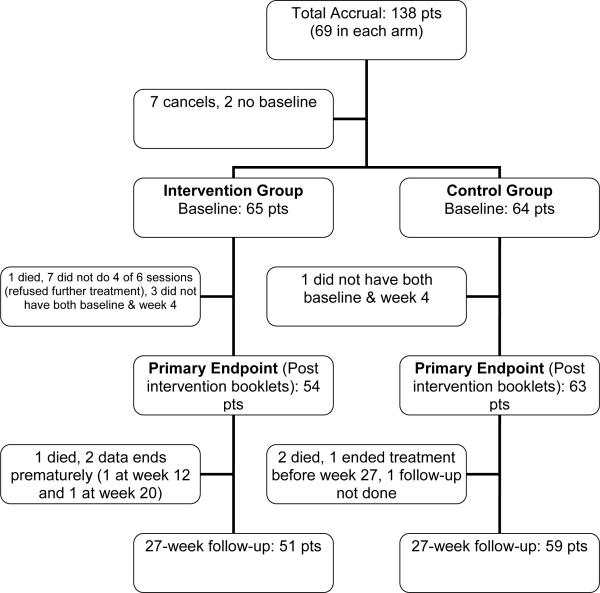
Over a 57-month period, of a possible 946 radiation oncology patients being treated who met criteria, 138 agreed to participate in our study (Figure 1). Information was not obtained from those that declined participation. Randomization was completed using standard Pocock-Simon randomization procedures. Nine participants did not complete randomization. Of the 129 randomized participants, eight were excluded as a result of not attending at least four of the six intervention sessions (1 death; 7 due to illness). One control participant and three intervention participants were excluded for not completing the week 4 assessments. Between week 4 and the 27 week follow-up, three of the intervention and four of the control participants died.
Figure 1.
Patient enrollment and follow-up
Intervention
The structured, multidisciplinary intervention focused on specific strategies to address all five QOL domains (Table 2).2 The content was developed by a multidisciplinary treatment and designed to impact physical, mental, social, emotional, and spiritual QOL.2 The content of the six sessions was derived from our prior eight-session multidisciplinary intervention and from recommendations of these previous study participants.18, 19 The recommendations were that the intervention be modified to include caregivers10 and that substance use (alcohol and tobacco), mood disorders, anxiety disorders and sleep disorders, and sleep hygiene all be addressed.20 The patients also requested that some of the sessions be for patients only, so that they would feel comfortable disclosing their distress without being concerned about burdening their or other caregivers. Caregivers were invited to attend sessions 1, 3, 4, and 6. Each session was designed to stand alone to accommodate ongoing enrollment. Sessions were 90 minutes, starting with 20 minutes of conditioning exercises led by a physical therapist,21 followed by education, cognitive behavioral strategies for coping with cancer,22-24 open discussion and support, concluding with a 15-minute deep breathing or guided imagery relaxation segment. A clinical psychologist or psychiatrist led each session; other study staff members varied from an advanced practice nurse, a certified hospital chaplain, or a licensed independent clinical social worker, depending on the specific session content. Three sessions of the multidisciplinary intervention addressed spiritual QOL, during which a certified hospital chaplain asked two structured open-ended questions related to the day's topic (e.g., life review, meaning and purpose, blessing and burdens) and invited study participants into conversation.25, 26 The chaplain's goal was to provide an invitation to discuss hopes and concerns in an accepting and supportive environment, engage in active listening, and provide appropriate counsel. Discussions of each spiritual topic lasted 20-30 minutes. To address fidelity of treatment, data projector images were used for each session, written materials were standardized and used at each session, participants received a 200-page manual, and all intervention staff received training. To promote long-term adoption of the coping strategies, participants received ten brief structured telephone counseling sessions (Table 3).
Table 2.
Structured Multidisciplinary Intervention Session Outline
| Time | Session 1 Caregivers invited | Session 2 Patients only | Session 3 Cargivers invited | Session 4 Caregivers invited | Session 5 Patients only | Session 6 Caregivers invited |
|---|---|---|---|---|---|---|
| 15 min | Physicial Therapy | Physicial Therapy | Physicial Therapy | Physicial Therapy | Physicial Therapy | Physicial Therapy |
| 30 min | Health Behavior Changes: How to eat healthy and to avoid alcohol and nicotine during cancer treatment | Mood Management: Distress, depression, anxiety disorders, and sleep disorders | Coping with Cancer: The role of thoughts and behaviors Problem solving skills |
Social Needs: Advanced directives Finances Community Resources |
Defining your Quality of Life | Communication strategies with health care providers and your support system |
| 30 min | Radiation and Chemotherapy Education Topics: Self-care and symptom management | Spirituality: Life review | Spirituality: Meaning and purpose | Record Keeping: Symptoms, food intake, pain, and health status Coping Strategies Benefits of physical activity | Spirituality: Grief, loss, hope, and blessings | Maintenance: Distress Mood management Spiritual resources Medical issues Health behaviors Physical activity |
| 15 min | Relaxation training | Relaxation training | Relaxation training | Relaxation training | Relaxation training | Relaxation training |
Table 3.
Brief Telephone Counseling Intervention
| Brief Phone Contact Topic | Mailing of Written Self-Help Material | Indivudally Tailored Questions | |
|---|---|---|---|
| Week 5 | Review of self-care: Journaling relaxation | Relaxation CD | Are you using self-care strategies? |
| Week 6 | Mood management skills | Extending a Hand of Hope (ACS) | How is your distress level? |
| Week 7 | Spiritual needs | Taking time (NIH) | How are you doing from a spiritual perspective? |
| Week 8 | Physial therapy | Complete the Exercise Behavior Measures with the participant | |
| Week 10 | Health behavior changes | How are your health beahviors (e.g., diet, smoking)? | |
| Week 12 | Communication and social support | How is your support system? | |
| Week 14 | Social needs | Have you completed your advance directives? Have you been able to access community resources? Have you addressed your financial planning needs? | |
| Week 16 | Mood assessment | How is your distress level? | |
| Week 18 | Physical therapy | Complete the Exercise Behavior Measures with the participant | |
| Week 20 | Questions for us/open agenda | What would you like to review today? How is your quality of life? | |
| Week 27 all subjects | Thank you for your participation in our research protocol | Study questionnaires | Any feedback for us on your participation in the study? How is your quality of life? |
Standard Care
The control group received standard medical care as recommended by their radiation oncologist including medical appointments and referrals to specialists such as medical oncology, surgery, primary care, neurology, gastroenterology, or pulmonary when needed.
STATISTICAL ANALYSIS
The primary endpoint was the participant's QOL at the end of the intervention, which was approximately week 4 post randomization. The intervention's short-term impact was measured by the QOL change from baseline as reported on the FACT-G at week 4; long-term impact was measured by changes to week 27. All assessments were scored according to the specific scoring algorithms. Scores were converted to a 0-100 point scale, for comparability, with 100 being best QOL. Summary statistics were compiled to compare study arms. Kruskall-Wallis or Chi-Square methodology was employed as appropriate. Supplementary analyses via ANOVA/GEE modeling were used to determine associations between QOL scores and sociodemographic variables. Furthermore, the empirical rule of statistical theory and the work of Cohen in defining small, moderate, and large effect sizes for behavioral endpoints was employed.27 This approach defines 3%, 8%, and 12% shifts in the average QOL scores between study groups as indicative of these clinically important differences. Summary statistics of the effect size distribution per assessment were calculated. All hypothesis testing was done using two-tailed alternatives and a 5% Type I error rate. The study was ensured to have 80% power to detect a clinically significant difference of 0.5 standard deviations (a shift of 8% or more on a 100-point scale) in QOL scores between study arms. Any smaller effect was likely to be unimportant and, for the pragmatic purposes of this intervention, not clinically meaningful. The study was powered to declare such a difference statistically significant as well. Hence, any statistically significant result gleaned from this study will have inherent clinical significance.
RESULTS
Patient Characteristics
Baseline characteristics were balanced across treatment arms (Table 1). On average, patients were in their late fifties (59.3 years old), two-thirds male (65.6%), almost all Caucasian (97%), more than half employed (58.8%), most married (87%), and most reported their religious affiliation as Protestant (56.5%) followed by Catholic (35%). Tumor types were 37% gastrointestinal, 22% brain, 16% head/neck, 13% lung, and 12% other; almost all had surgery (95%); and >85% were also receiving chemotherapy. The majority of caregivers were the significant other (79%) and were employed (62).
FACT-G Results
Total FACT-G scores were significantly different between study arms at week 4, with the intervention patients having higher average overall QOL (mean 74.2 vs 68.7, p=0.02, Tables 4-5). Change from baseline analysis indicated the intervention arm maintained overall QOL (mean change −1.4, SD 24.25), while the control arm experienced reduction (mean change −6.2, SD 19.93) in overall QOL (p=0.01). In an intent-to-treat analysis, assuming that non-evaluable patients were failures (defined by having a clinically meaningful QOL decrease [8%] at week 4), no statistically significant difference was found between treatment arms (p=0.54, Table 6). Assuming that these patients were successes, i.e., maintained or improved QOL, the intervention arm had fewer failures than the standard care arm (14 vs 26, p=0.02).
Table 4.
Overall Quality of Life Measured by the FACT-G Summated Score
| Intervention | Control | Kruskal-Wallis P-value | ||
|---|---|---|---|---|
| Baseline | Mean (SD) | 75.2 (13.8) (n=65) | 74.8 (11.4) (n=64) | 0.59 |
| Week 4 | Mean (SD) | 74.2 (12.6) (n=54) | 68.7 (13.1) (n=63) | 0.02 |
| Week 27 | Mean (SD) | 77.6 (12.1) (n=51) | 77.7 (11.8) (n=59) | 0.88 |
Table 5.
FACT-G Subscales Means (SD)
| Baseline | Week 4 | Week 27 | |
|---|---|---|---|
| Physical | |||
| Intervention | 71.9 (20.9) | 67.7 (20.7) | 76.4 (17.8) |
| Control | 70.8 (17.1) | 57.7 (21.7)* | 76.7 (16.6) |
| Social | |||
| Intervention | 85.9 (11.8) | 85.6 (12.4) | 84.6 (14.4) |
| Control | 84.4 (12.7) | 83.7 (13.3) | 82.5 (15.0) |
| Emotional | |||
| Intervention | 79.2 (17.5) | 79.8 (15.5) | 80.0 (12.6) |
| Control | 81.4 (13.6) | 78.4 (17.5) | 81.2 (14.1) |
| Functional | |||
| Intervention | 64.5 (20.3) | 64.5 (17.8) | 69.9 (19.4) |
| Control | 63.6 (22.2) | 57.1 (21.3) | 71.4 (17.5) |
difference between intervention and control p<0.01
Table 6.
Intent-to-Treat FACT-G Failure at Week 4
| Intervention Group (N=65) | Control Group (N=66) | Total (N=131) | p value | |
|---|---|---|---|---|
| All missing are success | <0.05 | |||
| Fail | 14 (21.5%) | 26 (39.4%) | 40 (30.5%) | |
| Success | 51 (78.5%) | 40 (60.6%) | 91 (69.5%) | |
| 25% of missing are as signed as failure | 0.11 | |||
| Fail | 17 (26.2%) | 26 (39.4%) | 43 (32.8%) | |
| Success | 48 (73.8%) | 40 (60.6%) | 88 (67.2%) | |
| 50% of missing are as signed as failure | 0.30 | |||
| Fail | 20 (30.8%) | 26 (39.4%) | 46 (35.1%) | |
| Success | 45 (69.2%) | 40 (60.6%) | 85 (64.9%) | |
| 75% of missing are as signed as failure | 0.64 | |||
| Fail | 23 (35.4%) | 26 (39.4%) | 49 (37.4%) | |
| Success | 42 (64.6%) | 40 (60.6%) | 82 (62.6%) | |
| all missing are failure | 0.42 | |||
| Fail | 25 (38.5%) | 30 (45.5%) | 55 (42.0%) | |
| Success | 40 (61.5%) | 36 (54.5%) | 76 (58.0%) |
The Physical Well-Being subscale of the FACT-G was also statistically significantly different between study arms at week 4 (p<0.01). Change from baseline indicates that the intervention arm experienced non-clinically meaningful reduction (4.2 points) in Physical Well-Being while the standard arm declined 13.1 points (p<0.01). The Functional Well-Being subscale change from baseline at week 4 was also statistically significant, with patients in the intervention arm maintaining QOL while those in the standard care arm decreased (mean −0.3 vs −7.1, p=0.02). There were no statistically significant or clinically meaningful differences in total or change scores, either between or within the study arms, at week 27 (Tables 4-6).
Caregiver QOL Results
Caregiver QOL (measured by Caregiver Quality of Life Index-Cancer Scale) was maintained at a low level over time, both in the intervention and standard care arms, with the average QOL scores remaining in the fifties on the 0-100 point scale throughout the study (Table 7).
Table 7.
Caregiver Quality of Life Index-Cancer Scale
| Intervention Caregivers | Control Caregivers | |
|---|---|---|
| Baseline | 55.5 (±20.7) n=65 | 54.0 (±19.5) n=65 |
| Week 4 | 58.0 (±20.7) n=54 | 57.7 (±19.6) n=62 |
| Week 27 | 58.5 (±20.3) n=52 | 59.1 (±20.5) n=58 |
Additional Measures
There were no between group differences on other study measures, which included the Profile of Mood States,28 Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being,29 Pittsburgh Sleep Quality Index,30 and Exercise Behaviors.31
ANOVA/GEE Modeling Results
Week 4 change from baseline was modeled using ANOVA/GEE procedures to determine whether there was a relationship between baseline characteristics and study results. Arm, tumor type, and performance status were all significant contributors to the change from baseline, but the model itself was not a good fit, having only 27% of the variability in the change scores explained by the model. Independent factors of cancer treatment regimen and age group were not statistically significant.
DISCUSSION
Quality of life is important during active cancer treatment and through survivorship. In this randomized controlled trial of a multidisciplinary structured intervention targeting all five QOL domains, participants diagnosed with advanced cancer were able to maintain their QOL while receiving radiation therapy. In contrast, those in the standard care arm demonstrated a reduction in their QOL. Given the significant symptom burden and side effects associated with receiving radiation therapy combined with surgery and chemotherapy side effects, this is an important clinically meaningful and statistically significant outcome. This study involved a cancer population receiving limited psychosocial empirical attention; the majority of published psychosocial interventions are delivered after active cancer care completion, recruit early stage cancer patients, or have mostly female participants.
The finding that intervention participants were able to maintain overall QOL during radiation therapy appears to be due in large part to the domain of physical QOL. Several of the interventional strategies may account for this significant difference in physical QOL. Perhaps foremost in impacting physical QOL was the physical therapy assessment and intervention. Participants met with a physiatrist, and each session started with 15 minutes of physical activity instructed by a physical therapist. A majority of patients with cancer, even those situated in rural areas, have access to physiatric and physical therapy services that are, at least partially, covered by third party payers.32, 33 The exercises included in the trial were deigned to be simple and well within the purview of community-based therapists to ensure generalizability. Physician attention to a behavior has been shown to promote positive behavior change, and the advice from the study psychiatrist may have enhanced motivation for physical activity.34 In addition, the nurse educator provided information about cancer treatment side effects and strategies for symptom management that may have specifically impacted physical well-being. The participants were also taught the importance of record keeping and communication strategies with caregivers and health care providers to minimize pain and discomfort. The in-session relaxation training might also have helped participants manage symptoms (e.g., pain and nausea) and reduce stress levels. Maintaining physical activity levels during cancer treatment has been shown to reduce treatment-related fatigue; therefore, this dimension of the multidisciplinary intervention might have been the key component to maintaining overall QOL during radiation therapy.
The intention of the brief telephone contacts was to improve QOL once active cancer treatment was completed and to provide ongoing support to patients and caregivers. Telemedicine is an exciting new strategy for improving cancer care.35 Investigators discovered that providing telecare management can reduce pain and depression in cancer patients.36 Although it is disappointing that QOL did not improve over the follow-up period, participants did maintain their QOL level throughout the study. In seeking sources of potential symptom burden, many participants continued to receive chemotherapy or undergo further surgery during study follow-up. Additionally, the side effects of radiation therapy, surgery, and chemotherapy can have an extended negative impact on QOL. Perhaps the inability to improve QOL during a time of continued cancer-related symptom burden and side effects is understandable in a population of cancer patients still receiving cancer care with numerous ongoing health issues. If confirmed by other investigators, it is plausible that multidisciplinary interventions can be designed and delivered to improve the QOL of those diagnosed with early stage cancer, and that multidisciplinary interventions can be tailored to maintain the QOL of those diagnosed with advanced stage cancer.
As previous research has shown that caregivers can experience significant burden, it is disappointing that the intervention did not impact the caregivers’ QOL.10 In this intervention, the strategies employed to impact caregiver QOL were to improve patient QOL and to involve the caregiver in the intervention. At the study's end, many caregivers expressed desire for two major changes. The first was that the caregivers felt their needs could have been better addressed in a separate caregivers only group. Many stated they did not want to express how challenging it is to be a cancer caregiver around their loved ones, or even in the presence of other cancer patients, but believed discussing their burden with other caregivers would have been beneficial to them. Second, they inquired whether they could be taught (similar to our patient-focused interventions) specific strategies for improving their own QOL. Perhaps incorporating these two strategies would prove beneficial to the cancer caregivers’ QOL.
This study had several limitations. Due to the demographics of the cancer patient population at the cancer center, the sample population was primarily Caucasian, Christian, and Midwestern. Therefore, these findings might not apply to more diverse populations. The recruitment rate, while similar to most psychosocial interventions, was low, less than 25% of those eligible. Therefore, identification of QOL enhancement strategies with greater appeal to cancer patients is needed. Finally, cost and availability of a highly skilled multidisciplinary team might make the offering of this intervention possible only at large cancer centers or only through the exploration of telemedicine. Future research could also explore the delivery of a multidisciplinary development QOL intervention delivered by a trained facilitator to evaluated a cost-effective dissemination of the intervention.
In summary, participating in a six-session multidisciplinary intervention was effective in maintaining overall QOL of patients with advanced cancer who were receiving radiation therapy. The results were found in both genders and across a range of tumor types. It is important to enhance the QOL of cancer survivors and their caregivers, therefore, future studies should further explore strategies to impact the long-term QOL of patients with advanced cancer and begin identifying effective strategies for improving the cancer caregivers’ QOL.
Condensed Abstract.
In a randomized controlled trial, participation in a six-session multidisciplinary intervention helped maintain the quality of life of patients diagnosed with advanced cancer who were receiving radiation treatment. Research should further explore strategies for enhancing the quality of life of patients diagnosed with advanced cancer and their caregivers.
Acknowledgments
FUNDING SOURCES
This study was supported by the Linse Bock Foundation and the Sponsorship Board, Saint Mary's Hospital, Mayo Clinic.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
This study was presented at the Annual Meeting of the Academy of Psychosomatic Medicine, November 13, 2010, Marco Island, Florida
REFERENCES
- 1.Clark MM, Bostwick JM, Rummans TA. Group and individual treatment strategies for distress in cancer patients. Mayo Clin Proc. 2003;78(12):1538–1543. doi: 10.4065/78.12.1538. [DOI] [PubMed] [Google Scholar]
- 2.Rummans TA, Clark MM, Sloan JA, et al. Impacting quality of life for patients with advanced cancer with a structured multidisciplinary intervention: a randomized controlled trial. J Clin Oncol. 2006;24(4):635–642. doi: 10.1200/JCO.2006.06.209. [DOI] [PubMed] [Google Scholar]
- 3.Hopwood P, Haviland JS, Sumo G, Mills J, Bliss JM, Yarnold JR. Comparison of patient-reported breast, arm, and shoulder symptoms and body image after radiotherapy for early breast cancer: 5-year follow-up in the randomised Standardisation of Breast Radiotherapy (START) trials. Lancet Oncol. 2010;11(3):231–240. doi: 10.1016/S1470-2045(09)70382-1. [DOI] [PubMed] [Google Scholar]
- 4.Rummans TA, Frost M, Suman VJ, et al. Quality of life and pain in patients with recurrent breast and gynecologic cancer. Psychosomatics. 1998;39(5):437–445. doi: 10.1016/s0033-3182(98)71303-9. [DOI] [PubMed] [Google Scholar]
- 5.Gielissen MF, Verhagen S, Witjes F, Bleijenberg G. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: a randomized controlled trial. J Clin Oncol. 2006;24(30):4882–4887. doi: 10.1200/JCO.2006.06.8270. [DOI] [PubMed] [Google Scholar]
- 6.Kuchler T, Bestmann B, Rappat S, Henne-Bruns D, Wood-Dauphinee S. Impact of psychotherapeutic support for patients with gastrointestinal cancer undergoing surgery: 10-year survival results of a randomized trial. J Clin Oncol. 2007;25(19):2702–2708. doi: 10.1200/JCO.2006.08.2883. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 8.Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Educ Couns. 2003;50(2):179–186. doi: 10.1016/s0738-3991(02)00149-0. [DOI] [PubMed] [Google Scholar]
- 9.Andersen BL, Yang HC, Farrar WB, et al. Psychologic intervention improves survival for breast cancer patients: a randomized clinical trial. Cancer. 2008;113(12):3450–3458. doi: 10.1002/cncr.23969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark MM, Rummans TA, Sloan JA, et al. Quality of life of caregivers of patients with advanced-stage cancer. Am J Hosp Palliat Care. 2006;23(3):185–191. doi: 10.1177/1049909106289074. [DOI] [PubMed] [Google Scholar]
- 11.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 13.Steer RA, Ball R, Ranieri WF, Beck AT. Further evidence for the construct validity of the Beck depression Inventory-II with psychiatric outpatients. Psychol Rep. 1997;80(2):443–446. doi: 10.2466/pr0.1997.80.2.443. [DOI] [PubMed] [Google Scholar]
- 14.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 15.Janda M, Gebski V, Brand A, et al. Quality of life after total laparoscopic hysterectomy versus total abdominal hysterectomy for stage I endometrial cancer (LACE): a randomised trial. Lancet Oncol. 2010;11(8):772–780. doi: 10.1016/S1470-2045(10)70145-5. [DOI] [PubMed] [Google Scholar]
- 16.Weitzner MA, Jacobsen PB, Wagner H, Jr., Friedland J, Cox C. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res. 1999;8(1-2):55–63. doi: 10.1023/a:1026407010614. [DOI] [PubMed] [Google Scholar]
- 17.Edwards B, Ung L. Quality of life instruments for caregivers of patients with cancer: a review of their psychometric properties. Cancer Nurs. 2002;25(5):342–349. doi: 10.1097/00002820-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Brown P, Clark MM, Atherton P, et al. Will improvement in quality of life (QOL) impact fatigue in patients receiving radiation therapy for advanced cancer? Am J Clin Oncol. 2006;29(1):52–58. doi: 10.1097/01.coc.0000190459.14841.55. [DOI] [PubMed] [Google Scholar]
- 19.Lapid MI, Rummans TA, Brown PD, et al. Improving the quality of life of geriatric cancer patients with a structured multidisciplinary intervention: a randomized controlled trial. Palliat Support Care. 2007;5(2):107–114. doi: 10.1017/s1478951507070174. [DOI] [PubMed] [Google Scholar]
- 20.Rausch SM, Millay S, Scott C, et al. Health behaviors among cancer survivors receiving screening mammography. Am J Clin Oncol. 2012;35(1):22–31. doi: 10.1097/COC.0b013e318200598e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cheville AL, Girardi J, Clark MM, et al. Therapeutic exercise during outpatient radiation therapy for advanced cancer: Feasibility and impact on physical well-being. Am J Phys Med Rehabil. 2010;89(8):611–619. doi: 10.1097/PHM.0b013e3181d3e782. [DOI] [PubMed] [Google Scholar]
- 22.Clark MM, Novotny PJ, Patten CA, et al. Motivational readiness for physical activity and quality of life in long-term lung cancer survivors. Lung Cancer. 2008;61(1):117–122. doi: 10.1016/j.lungcan.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Locke DE, Cerhan JH, Wu W, et al. Cognitive rehabilitation and problem-solving to improve quality of life of patients with primary brain tumors: a pilot study. J Support Oncol. 2008;6(8):383–391. [PubMed] [Google Scholar]
- 24.Petersen LR, Clark MM, Novotny P, et al. Relationship of optimism-pessimism and health-related quality of life in breast cancer survivors. J Psychosoc Oncol. 2008;26(4):15–32. doi: 10.1080/07347330802359578. [DOI] [PubMed] [Google Scholar]
- 25.Johnson ME, Piderman KM, Sloan JA, et al. Measuring spiritual quality of life in patients with cancer. J Support Oncol. 2007;5(9):437–442. [PubMed] [Google Scholar]
- 26.Piderman KM, Lapid MI, Stevens SR, et al. Spiritual well-being and spiritual practices in elderly depressed psychiatric inpatients. J Pastoral Care Counsel. 2011;65(1-2):3, 1–11. [PubMed] [Google Scholar]
- 27.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 28.McNair D, Lorr M, Droppelman L. Profile of Mood States: Manual. Educational and Testing Service; San Diego, CA: 1971. [Google Scholar]
- 29.Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D. A case for including spirituality in quality of life measurement in oncology. Psychooncology. 1999;8(5):417–428. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 30.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 31.Lorig K, Stewart A, Riter P, Gonzalez V, Laurent D, Lynch J. Outcome Measures for Health Education and Other Health Care Interventions. Sage Publications; Thousand Oaks, CA: 1996. [Google Scholar]
- 32.Alfano CM, Ganz PA, Rowland JH, Hahn EE. Cancer survivorship and cancer rehabilitation: revitalizing the link. J Clin Oncol. 30(9):904–906. doi: 10.1200/JCO.2011.37.1674. [DOI] [PubMed] [Google Scholar]
- 33.Alfano CM, Ganz PA, Rowland JH, Hahn EE. Cancer survivorship and cancer rehabilitation: revitalizing the link. J Clin Oncol. 2012;30(9):904–906. doi: 10.1200/JCO.2011.37.1674. [DOI] [PubMed] [Google Scholar]
- 34.Singh S, Somers VK, Clark MM, et al. Physician diagnosis of overweight status predicts attempted and successful weight loss in patients with cardiovascular disease and central obesity. Am Heart J. 2010;160(5):934–942. doi: 10.1016/j.ahj.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hazin R, Qaddoumi I. Teleoncology: current and future applications for improving cancer care globally. Lancet Oncol. 2010;11(2):204–210. doi: 10.1016/S1470-2045(09)70288-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroenke K, Theobald D, Wu J, et al. Effect of telecare management on pain and depression in patients with cancer: a randomized trial. JAMA. 2010;304(2):163–171. doi: 10.1001/jama.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]