Abstract
Objective
To compare American-Indian and Caucasian mortality rates from diabetes among tribal Contract Health Service Delivery Areas (CHSDAs) in the Great Plains Region (GPR) and describe the disparities observed.
Research design and methods
Mortality data from the National Center for Vital Statistics and Seer*STAT were used to identify diabetes as the underlying cause of death for each decedent in the GPR from 2002 to 2010. Mortality data were abstracted and aggregated for American-Indians and Caucasians for 25 reservation CHSDAs in the GPR. Rate ratios (RR) with 95% CIs were used and SEER*Stat V.8.0.4 software calculated age-adjusted diabetes mortality rates.
Results
Age-adjusted mortality rates for American-Indians were significantly higher than those for Caucasians during the 8-year period. In the GPR, American-Indians were 3.44 times more likely to die from diabetes than Caucasians. South Dakota had the highest RR (5.47 times that of Caucasians), and Iowa had the lowest RR, (1.1). Reservation CHSDA RR ranged from 1.78 to 10.25.
Conclusions
American-Indians in the GPR have higher diabetes mortality rates than Caucasians in the GPR. Mortality rates among American-Indians persist despite special programs and initiatives aimed at reducing diabetes in these populations. Effective and immediate efforts are needed to address premature diabetes mortality among American-Indians in the GPR.
Keywords: Mortality, Quantitative Methods, Native Americans
Key messages.
American-Indians are 3.44 times more likely to die from diabetes than Caucasians living in the same geographic areas, despite extensive efforts to address these disparities. American-Indians living in South Dakota have the highest mortality rates from diabetes in the Great Plains Region and the reasons for this are not clear.
Existing diabetes mortality data are available and programs such as SEER*Stat are a useful tool for hard to reach populations, such as American-Indians where small population size and a lack of tribal-specific data are common barriers.
Future research between universities and tribes should use tribal partnerships and consortia. This will help ensure researchers use methods that are appropriate for the population and culture while recognizing the unique tribal and geographic variation as they relate to diabetes mortality.
Introduction
Deaths from diabetes have increased significantly in the past two decades, impacting every state, age group, sex, and racial and ethnic group in the USA.1 However, some regions and populations carry a disproportionate burden of diabetes. Diabetes was the fourth leading cause of death among American-Indians (AIs) and Alaska Natives (ANs) between 1999 and 2010 and the seventh leading cause of death in the US population.2 Diabetes was the second leading cause of death for AIs in North Dakota, South Dakota, Iowa, and Nebraska in 2010;3 however, these rates may be 15–25% higher because death certificates often under-report diabetes as the underlying cause of death.4 To address mortality differences, public health officials, tribes, and policymakers must first document tribal-specific disparities. However, this task is often difficult to complete due to the lack of tribal-specific data, small populations, and confidentiality issues. In addition, there is a lack of substantial data and poor surveillance infrastructure in tribal communities. No known published study has examined mortality rate differences in diabetes among AIs and Caucasians residing in the same reservation areas in the Great Plains Region (GPR), (Montana, Wyoming, South Dakota, North Dakota, Iowa, and Nebraska).
Persons with diabetes often experience comorbidities such as heart disease, stroke, and kidney failure. Many patients with diabetes experience increased mortality from pneumonia and influenza.4 AIs experience more comorbidities and more severe complications from diabetes that lead to premature mortality. A recent study in South Dakota compared AI adults with diabetes and the US adult population with diabetes and found a higher prevalence of hypertension, cerebrovascular disease, lower extremity amputations, mental health disorders, and liver disease among the AI adults.5
Often, AIs experience additional risk factors for diabetes complications than other racial and ethnic groups. AIs over the age of 25 years are less likely to have a college degree or high school diploma and 77% of them have a high school diploma compared with 91% of Caucasians.6 AIs report higher rates of smoking, obesity, and unhealthy diets, all of which increase the risk of diabetes and death from diabetes.7 8 AIs also report significantly lower income than Caucasians. In 2010, the median income for AIs in the USA was $39 664 compared with $67 892 for Caucasians.9 Low income is linked with persistent poverty conditions. Lower income and persistent poverty are associated with higher mortality from all causes in the general US population.10 11
AI communities experience segregation, oppression, and discrimination, often linked to colonization,12 13 and these factors may contribute to differences in diabetes mortality and inequalities in health outcomes across tribal nations. As a racial minority, AIs may experience racial oppressions that contribute to health differences.14 AIs may experience more discrimination from healthcare providers than Caucasians15 and this may influence how they seek care, prevent or manage diabetes, and cope with complications from diabetes. Healthcare service and delivery for AIs are often described by geographic region.
In the GPR, AIs represent a relatively small percent of the population as a racial minority. However, AIs are an important group to study because of mounting evidence that they experience extreme health disparities and premature mortality.16–18 Similarly, in the USA, racial and ethnic minorities have poorer health than Caucasians19–21 and report higher mortality from diabetes.
The purpose of this study was to document diabetes mortality among AIs and Caucasians in the GPR and describe the differences observed. One unique contribution of this study is the use of a tribally recommended approach for calculating reservation-specific mortality rates.
Research design and methods
Description of study area
The GPR as defined for the study encompasses 6 states and 25 tribal Contract Health Service Delivery Area (CHSDA) regions: Montana, Wyoming, North Dakota, South Dakota, Nebraska, and Iowa. This does not include Minnesota or Wisconsin, which are sometimes defined as part of the GPR, because the Great Plains Tribal Chairman's Health Board and the Montana Wyoming Tribal Leaders Council were partners in this study, and they do not serve tribes in the Minnesota or Wisconsin areas. Combined, the GPR includes 6 states, 390 counties, and 7 641 494 persons, of whom 74.6% were Caucasian and 4.17% were AI.22 This study focuses on 78.8% of the population who are AI alone or Caucasian alone. Other populations in the GPR include Hispanic/Latino, Asian Pacific Islander, African-American, Native Hawaiian, and two or more races; however, the predominant racial classification in Montana, South Dakota, and North Dakota is Caucasian alone and AI alone. This study focused on these groups and observed differences.
American Indians
AIs and ANs are tribal groups in the USA and therefore are not truly ethnic minorities. The 2010 census reported that 5.2 million people identified their race as AI/AN alone or in addition to another racial category. Of these, 2.9 million identified themselves as AI/AN alone and 2.3 million people as AI/AN in combination with another race. The AI/AN population has increased 39% since 2000.6 The Bureau of Indian Affairs recognizes 566 different tribal groups and of these, 25 reservations are located in the GPR.23 In this study, AI refers to the indigenous peoples of the GPR. Few ANs reside in this region. AIs in this study were identified in the data based on death certificates.
Reservation CHSDA regions
CHSDA regions are comprised of counties located on or bordering federally recognized tribal lands (eg, §42 CFR 136.22). Approximately 57% of the AI population resides in 624 tribal CHSDA counties throughout the USA.24 In the GPR, 110 of the counties have CHSDA status. Within these CHSDA areas, health services are provided from public or private medical or hospital facilities at the expense of the Indian Health Service if funding is available. CHSDA counties are often used by researchers and federal programs to identify AI populations and subsequent county-based mortality rates by racial classification (AI vs Caucasian). For example, the Surveillance, Epidemiology, and End Results (SEER) program uses CHSDA status to classify segments of the US population by county, race, region, and disease-specific mortality.25 Reservation CHSDA regions have higher AI populations and often report less misclassification of AI status when compared with non-CHSDA counties.3 24 However, the use of reservation CHSDA counties must be approached with caution because tribes do not always feel that federally designated reservation CHSDA regions accurately represent their tribe(s) and tribal members (Giroux, personal communication, January 13, 2013). In this study, the researcher consulted with two tribal health boards in the GPR, the Northern Plains Tribal Epidemiology Center and the Montana Wyoming Tribal Leaders Council, to determine which counties should be included in tribal-specific analyses. For example, some tribes in the GPR prefer that reservation counties are used instead of CHSDA counties.3 Also, reservation CHSDA counties may overlap and therefore tribal-specific mortality rates must be interpreted with caution. Of the 118 counties included in the GPR, 20 overlap and are shared by more than one reservation CHSDA region. In this study, diabetes mortality data are based on 110 CHSDA counties and 8 additional reservation counties. Combined, this area makes up 25 reservation CHSDA regions.
The reservations and counties linked to tribes in the current study were identified and defined based on previous work with tribal leaders in the area3 and county designations from the 2000 US Census. Reservation CHSDA region data were used because tribal registries are not available in these areas, and reservation CHSDAs provide the most comprehensive area to measure of mortality between AIs and Caucasians in the GPR. In order to calculate reservation CHSDA region diabetes mortality rate ratios (RR) between AIs and Caucasians living in the same county, this study combined multiple counties that make up reservation CHSDAs. Tribes and reservations were designated based on federal recognition and the counties that made up reservation boundaries.3 23
Data
SEER*Stat data were used to examine diabetes as the underlying cause of death by AI versus Caucasian status from 2002 to 2010. Multiyear data were aggregated from 2002 to 2010 to limit potential instability of county rates, as suggested by a previous research report.24 The National Center for Vital Statistics National Statistics System in the USA provides coverage of deaths within the GPR by county and includes county of residence, race/ethnicity, and underlying cause of death for each decedent by year. Only individuals who self-reported one race, AI (or AN), were counted as decedents in the numerator. Population characteristics from the US Census Bureau's Population Estimates Program incorporate intercensal populations by year, county, race, sex, and age. Population characteristics were used to calcualte rates and only individuals who self-report as exclusively AI (or AN) were included in the denominator and very few ANs (<0.01%) reside in this geographic area. Deaths coded according to the International Classification of Diseases, 10th Revision (ICD-10) standards and only underlying causes of death “Diabetes Mellitus” (ICD-10: E10-E14) were used to calculate mortality rates from the SEER 2002–2010 US mortality registry.25
Diabetes mortality rates were expressed per 100 000 persons and age-adjusted to eliminate the effect of differences in age composition among AIs and Caucasians. SEER*Stat 8.0.4 software calculated age-adjusted diabetes mortality rates using the 2000 US standard population.25 Data were suppressed by SEER when <10 deaths occurred during the time period of interest. Mortality rates between AI and Caucasian populations were compared by RR with 95% CIs.
Results
The age-adjusted diabetes mortality rates among AIs residing in reservation CHSDA areas were significantly higher at 71 per 100 000 than among Caucasians residing in the same areas at 20.6 per 100 000. In the GPR, this mortality RR is 3.44 times higher among AIs than among the Caucasians. This is significantly higher than the US mortality rate for AI/ANs of 20.5 per 100 000.25 Table 1 shows differences in mortality rates by state in the GPR, with South Dakota having the highest mortality RR of any state in the region. The mortality rates among AIs were significantly higher than Caucasians for all states in the GPR with the exception of Iowa.
Table 1.
2002–2010 Diabetes mortality RR by state in the Great Plains Region
| Lower CI RR* |
Upper CI RR† |
Lower CI RR | Upper CI RR | RR p value | |||
|---|---|---|---|---|---|---|---|
| Montana | |||||||
| AI | 69.3† | 59.7 | 79.8 | 3.36‡ | 2.88 | 3.90 | 0.00 |
| Caucasian | 20.6 | 19.7 | 21.5 | ||||
| North Dakota | |||||||
| AI | 93.2† | 77.8 | 110.4 | 3.92‡ | 3.25 | 4.68 | 0.00 |
| Caucasian | 23.8 | 22.6 | 24.9 | ||||
| South Dakota | |||||||
| AI | 111.7† | 99.3 | 125.2 | 5.47‡ | 4.81 | 6.19 | 0.00 |
| Caucasian | 20.4 | 19.5 | 21.5 | ||||
| Nebraska | |||||||
| AI | 48.6† | 37.5 | 61.6 | 2.37‡ | 1.82 | 3.01 | 0.00 |
| Caucasian | 20.5 | 19.8 | 21.2 | ||||
| Iowa | |||||||
| AI | 21.9 | 14.9 | 30.4 | 1.10 | 0.758 | 1.55 | 0.60 |
| Caucasian | 19.7 | 19.2 | 20.2 | ||||
| Wyoming | |||||||
| AI | 71.3† | 52 | 94.4 | 3.1‡ | 2.23 | 4.11 | 0.00 |
| Caucasian | 23.1 | 21.8 | 24.6 | ||||
RR ALs versus Caucasians.
*RR per 100 000 deaths age adjusted.
†RRs are expressed as mortality RR comparing ALs with Caucasians by state.
‡Denotes statistical significance at the p<0.0001 level.
AL, American-Indian; RR, rate ratio.
There was a variation in mortality rates from diabetes by reservation CHSDA region. The Confederated Salish and Kootenai tribes of Montana had the lowest RR, 1.78 times higher for AIs than Caucasians in the same reservation CHSDA counties, while the Sac and Fox tribes of Iowa had the highest RR, 10.25 times higher for AIs than Caucasians in the same reservation CHSDA counties. This was surprising based on the state-specific RR in table 1, where Iowa had the lowest RR (1.1) between AIs and Caucasians aggregated at the state level. However, the mortality rate for the Sac and Fox tribes of Iowa includes only those CHSDA counties within or bordering the reservation. AIs living off the reservation experience lower diabetes mortality than those living on the reservation. The Omaha tribe of Nebraska had the highest rate, 181.9 per 100 000 population, followed by the Sac and Fox tribes of Iowa. South Dakota had more reservations with rates higher than North Dakota, Montana, or Wyoming (see table 2).
Table 2.
Mortality rates* and RR by tribal CHSDA regions
| Tribe, state | #Deaths | Rate | SE | Lower CI | Upper CI | RR† | Lower CI RR | Upper CI RR | RR p value |
|---|---|---|---|---|---|---|---|---|---|
| Conf.SalishKootenai, MT | 408 | 33.0 | 7.3 | 20.3 | 50.1 | 1.78 | 1.08 | 2.74 | 0.02 |
| Ponca, NE | 2075 | 43.8 | 7.2 | 30.8 | 59.6 | 2.09 | 1.47 | 2.86 | 0.00 |
| ChippewaCree, MT | 68 | 57.0 | 16.8 | 29 | 100.5 | 2.57 | 1.23 | 4.91 | 0.01 |
| AssiniboineGrosVentre, MT | 37 | 67.0 | 19 | 35.1 | 114.3 | 3.42 | 1.49 | 7.10 | 0.00 |
| SpiritLakeDakota, ND | 96 | 93.6 | 24.3 | 52.2 | 152.9 | 3.70 | 1.94 | 6.48 | 0.00 |
| Crow, MT | 490 | 81.5 | 12.5 | 58.9 | 109 | 3.84 | 2.74 | 5.23 | 0.00 |
| TurtleMtnChippewa, ND | 76 | 122.5 | 16.7 | 91.9 | 159.1 | 4.03 | 2.094 | 7.67 | 0.00 |
| Winnebago, NE | 427 | 104.0 | 19 | 70.3 | 146.5 | 4.19 | 2.79 | 6.007 | 0.00 |
| RosebudSioux, SD | 147 | 101.4 | 13 | 77.5 | 129.8 | 4.24 | 2.94 | 5.98 | 0.00 |
| Mandan,Hidatsa, Arikara, ND | 766 | 125.6 | 15.3 | 97.4 | 158.7 | 4.68 | 3.59 | 5.99 | 0.00 |
| ShoshoneAraphoe, WY | 207 | 113.8 | 18.9 | 79.9 | 155.7 | 4.77 | 3.23 | 6.80 | 0.00 |
| AssiniboineSioux, MT | 136 | 119.1 | 21.2 | 81.3 | 166.7 | 4.92 | 3.16 | 7.34 | 0.00 |
| Blackfeet, MT | 78 | 106.7 | 16.6 | 76.7 | 143.6 | 5.13 | 3.03 | 8.51 | 0.00 |
| StandingRock, SD‡ | – | – | – | – | – | – | – | – | – |
| OgalaSioux, SD | 446 | 110.9 | 8.9 | 94.2 | 129.5 | 5.77 | 4.70 | 7.05 | 0.00 |
| CrowCreekSioux, SD§ | 120 | 148.7 | 32.3 | 92.3 | 222.3 | 5.84 | 3.45 | 9.25 | 0.00 |
| NorthernCheyenne, MT | 81 | 114.5 | 17.7 | 82.4 | 153.6 | 5.91 | 3.49 | 9.93 | 0.00 |
| CheyenneRiverSioux, SD | 198 | 146.9 | 18.4 | 113 | 186.8 | 6.04 | 4.38 | 8.19 | 0.00 |
| SissetonWahpetonOyate, SD | 206 | 142.0 | 29.9 | 89.6 | 210.3 | 7.04 | 4.32 | 10.78 | 0.00 |
| YanktonSioux, SD | 183 | 154.3 | 30.3 | 100.7 | 223.7 | 7.05 | 4.41 | 10.66 | 0.00 |
| Omaha, NE | 151 | 181.9 | 34.8 | 120.1 | 261.3 | 9.05 | 5.68 | 13.72 | 0.00 |
| Sac&Fox, IA | 32 | 173.0 | 57.3 | 79.6 | 315.1 | 10.25 | 4.33 | 20.66 | 0.00 |
| Santee Sioux | ¶ | ¶ | |||||||
| Flandreau | ¶ | ¶ | |||||||
| Lower Brule Sioux§ | ¶ | ¶ |
*RR ALs versus Caucasians.
†Death rate per 100 000.
‡The Standing Rock tribe of South Dakota did not want tribal-specific rates published.
§GPTCHB requested that tribal county be used instead of CHSDA AI population. Surveillance Research Program, National Cancer Institute SEER*Stat software (http://www.seer.cancer.gov/seerstat) V.8.0. SEER Program (http://www.seer.cancer.gov) SEER*Stat Database: Mortality—All COD, Public-Use With County, Total U.S. for Expanded Races (2002–2010), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released July 2013. Underlying mortality data provided by NCHS (http://www.cdc.gov/nchs).
¶Less than 10 cases.
AL, American-Indian; CHSDA, Contract Health Service Delivery Area; GPTCHB, Great Plains Tribal Chairmen's Health Board; RR, rate ratio; SEER, Surveillance, Epidemiology, and End Results.
Conclusions
There was substantial variation between AIs and Caucasians in the same geographies. There was also variation between tribes and by geographies. For example, two tribes in Montana shared one county; however, one tribe's diabetes mortality RR was 5.91 compared with the other tribe's RR of 3.84. Both tribes reported higher RRs than the overall RR for Montana of 3.36; however, one tribe was significantly higher than both. In South Dakota, two tribes shared one county and their mortality RR were 5.3 and 5.8. These rates were similar to the South Dakota state ratio of 5.47.
AIs experience higher mortality from diabetes than Caucasians living in the same geographic areas, in this case reservation CHSDAs and specific states. This may be related to several risk factors and conditions described in previous reports, including low income, low education, obesity, smoking, genetic predisposition, westernization, loss of traditional foods, barriers to seeking treatment, discrimination, severe complications related to diabetes, high rates of cardiovascular disease and other comorbidities, cultural differences in diabetes based on how it is perceived and treated, and others.26–30 These individual risk factors may be magnified in certain AI populations and geographies where diabetes mortality rates are the highest.
Possible explanations for increased mortality among AIs in the GPR may be related to the higher prevalence of diabetes in the GPR and the presence of more risk factors associated with diabetes and premature mortality often found in reservation CHSDA areas. For example, the estimated prevalence of diabetes among all residents living in reservation CHSDAs in the GPR is 8.20% compared with 7.46% of non-CHSDAs in the GPR.26 Among reservation CHSDAs in the GPR, 20.73% report limited food access compared with 14.76% of non-CHSDAs.31 Smoking is a behavioral risk factor that contributes to premature mortality and among tribal CHSDAs, the rates are higher, 21.07% compared with 18.40%.32 Poverty is another contributing factor and differences between non-CHSDAs and tribal CHSDAs are pronounced where persistent poverty and persistent child poverty is less than 1% in non-CHSDAs, but 18.35% of tribal CHSDAs experience persistent poverty and 24.77% of tribal CHSDAs have persistent child poverty33 (figure 1).
Figure 1.
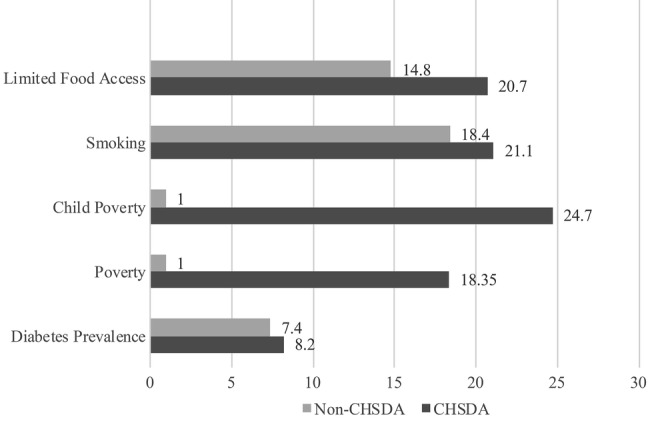
Characteristics of reservation and non-reservation counties.26–29
To address these differences based on tribe and geography, future studies could examine tribal-specific factors and geographies associated with lower diabetes mortality. This line of research could examine diabetes disparities using a strength-based approach, where tribes with lower mortality rates are involved in assessing the individual-level and population-level characteristics that may be protective against diabetes and subsequent mortality. Examining differences using social determinants of health framework might provide insights into the environment, conditions, and modifiable risk factors associated with diabetes disparities.19 34
By documenting mortality rate differences based on state, region, and tribal area, this study underscores the need for effective tribe-specific public health initiatives, policies, and interventions. First, immediate efforts might focus on communicating and describing the extent of disparities with tribal leaders and community members. Knowledge of great documented disparities in diabetes mortality might compel federal funding agencies, community health programs, the Indian Health Service, and families to take action. Second, tribes in the GPR might consider sharing best practices and lessons learned from previous diabetes prevention and interventions. For example, the variation of diabetes mortality in the GPR among AIs shows that some tribes have significantly lower mortality rates than others. Finally, since every tribe has a unique culture, history, language, and geography, differences in diabetes mortality must be addressed through the lens of the tribal population experiencing them, with assistance from public health professionals, policymakers, and tribal leaders.3 15 17 Higher rates of diabetes mortality among AIs living in reservation CHSDAs may be related to oppression and discrimination.14 15 Documenting and understanding risk factors as they relate to diabetes mortality may inform future interventions aimed at alleviating disparities reported in this study.
This study has some limitations and several strengths. Accurately reporting and assessing diabetes mortality in all populations including AIs can be challenging, given that death certificates may be incomplete, inaccurate, or under-report AI status.16 Another challenge with reporting and estimating diabetes deaths stems from the complications and comorbidities associated with diabetes.20 For example, the majority of diabetes-related deaths report the underlying cause of death as cardiovascular disease and a contributing cause of death as diabetes. In this study, only the underlying cause of death as diabetes was examined, and the contributing cause of death was not. These limitations are balanced by several strengths including these: tribally recommended design; the secondary data source used provides an efficient approach to improved understanding about disparities in diabetes mortality by tribe and region. The tribally recommended design used to identify reservation CHSDA regions was shared with the lead author by the Northern Plains Tribal Epidemiology Center, informed by tribal leaders and tribal health directors. Next, the lead author extracted the data and compiled the results. Results were shared with the tribal consortiums as a first step in documenting diabetes disparities. In the coming months, the lead author will present the results of this study to tribes in the GPR while supporting future efforts and programs aimed at eliminating differences in diabetes mortality. Tribes and public health officials agree that documenting disparities to show that they exist is the first of many steps in achieving health equity for all, including AIs.
In summary, this study adds to the literature a clear picture of the geographic and tribal-specific disparities in the GPR that have not been published previously. Researchers, public health professionals, clinicians, community members, and policymakers working in partnership with and in communities must take immediate action through multifaceted strategies to reduce disparities that lead to early mortality among AIs. The time to do this is now. These results are a call to further action to address these severe tribal disparities.
Footnotes
Contributors: AK conducted the analysis, wrote the manuscript, and is responsible for the intellectual content. JG, MS, and BA were responsible for the intellectual content and critical review. DW, RB, and SM reviewed and edited the manuscript. AK is the guarantor.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data used for this publication are available through the National Cancer Institute's cancer related databases and Surveillance Epidemiology and End Results program. Tribal-specific methods used to define tribal CHSDA regions are available on request.
References
- 1.Centers for Disease Control. Behavioral Risk Factor Surveillance System: diabetes prevalence and trends data. http://apps.nccd.cdc.gov/brfss/ (accessed 1 Jan 2014).
- 2.Centers for Disease Control. National Center for Health Statistics: leading causes of deaths and numbers of deaths, by sex, race, and Hispanic origin United States, 1980 and 2010. http://www.cdc.gov/nchs/hus/contents2012.htm#022 (accessed 27 Feb 2014).
- 3.Giroux J, Maschino A. Cause of death mortality among Great Plains tribes: Report for the Great Plains Tribal Chairman's Health Board. Rapid City, SD, 2013. [Google Scholar]
- 4.Centers for Disease Control. National Diabetes Fact Sheet: national estimates and general information on diabetes and prediabetes in the US, 2011 Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, 2011. [Google Scholar]
- 5.O'Connell J, Yi R, Wilson C et al. . Racial disparities in health status A comparison of the morbidity among American Indian and US adults with diabetes. Diabetes Care 2010;33:1463–70. 10.2337/dc09-1652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United States Census Bureau. Overview of race and Hispanic origin 2010. Department of Commerce Economic and Statistics Administration, 2012:6–7. [Google Scholar]
- 7.National Heart Lung and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute, 1998:2010. [Google Scholar]
- 8.Jernigan VB, Duran B, Ahn D et al. . Changing patterns in health behaviors and risk factors related to cardiovascular disease among American Indians and Alaska Natives. Am J Public Health 2010;100:677–83. 10.2105/AJPH.2009.164285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Census Bureau. Small area income and poverty estimates 2012.
- 10.Saydah SH, Imperatore G, Beckles GL. Socioeconomic status and mortality: contribution of health care access and psychological distress among U.S. adults with diagnosed diabetes. Diabetes Care 2013;36:49–55. 10.2337/dc11-1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castor ML, Smyser MS, Taualii MM et al. . A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties. Am J Public Health 2006;96:1478–84. 10.2105/AJPH.2004.053942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King M, Smith A, Gracey M. Indigenous health part 2: the underlying causes of the health gap. Lancet 2009;374:76–85. 10.1016/S0140-6736(09)60827-8 [DOI] [PubMed] [Google Scholar]
- 13.Wilson AC, Yellow Bird M. For indigenous eyes only: a decolonization handbook. Santa Fe, N.M: School of American Research, c2005, 2005. [Google Scholar]
- 14.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 2001;30:668–77. 10.1093/ije/30.4.668 [DOI] [PubMed] [Google Scholar]
- 15.Gonzales KL, Harding AK, Lambert WE et al. . Perceived experiences of discrimination in health care: a barrier for cancer screening among American Indian women with Type 2 diabetes. Womens Health Issues 2013;23:e61–7. 10.1016/j.whi.2012.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gohdes D, Oser CS, Harwell TS et al. . Diabetes in Montana's Indians: the epidemiology of diabetes in the Indians of the Northern Plains and Canada. Curr Diab Rep 2004;4:224–9. 10.1007/s11892-004-0028-2 [DOI] [PubMed] [Google Scholar]
- 17.Christensen M, Kightlinger L. Premature mortality patterns among American Indians in South Dakota, 2000–2010. Am J Prev Med 2013;44:465–71. 10.1016/j.amepre.2013.01.014 [DOI] [PubMed] [Google Scholar]
- 18.Geiger HJ, Borchelt G. Racial and ethnic disparities in US health care. Lancet 2003;362:1674 10.1016/S0140-6736(03)14806-4 [DOI] [PubMed] [Google Scholar]
- 19.Marmot M. Social determinants of health inequalities. Lancet 2005;365:1099–104. 10.1016/S0140-6736(05)74234-3 [DOI] [PubMed] [Google Scholar]
- 20.Morewitz SJ. Chronic diseases and health care: new trends in diabetes, arthritis, osteoporosis, fibromyalgia, low back pain, cardiovascular disease, and cancer. Springer, 2006. [Google Scholar]
- 21.Centers for Disease Control and Prevention. Health disparities experienced by racial/ethnic minority populations. MMWR Morb Mortal Wkly Rep 2004;53:755. [Google Scholar]
- 22.United States Department of the Interior. Who we are. Indian Affairs, 2013. [Google Scholar]
- 23.United States Census Bureau. Montana, Wyoming, South Dakota, North Dakota County Query 2010.
- 24.Espey DK, Wiggins CL, Jim MA et al. . Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer 2008;113(S5):1120–30. 10.1002/cncr.23724 [DOI] [PubMed] [Google Scholar]
- 25.National Cancer Institute. Surveillance Epidemiology and End Results. Bethesda, MD: SEER*Stat software, 2002–2010. [Google Scholar]
- 26.Cobb N, Paisano RE. Patterns of cancer mortality among Native Americans. Cancer 1998;83:2377–83. [DOI] [PubMed] [Google Scholar]
- 27.Whiting D, Unwin N, Roglic G. Diabetes: equity and social determinants. Equity, social determinants and public health programmes, 2010:77. [Google Scholar]
- 28.Moy E, Smith CR, Johansson P et al. . Gaps in data for American Indians and Alaska natives in the national healthcare disparities report. Am Indian Alsk Native Ment Health Res 2006;13:52–69. 10.5820/aian.1301.2006.52 [DOI] [PubMed] [Google Scholar]
- 29.United States Congress. A way out of the diabetes crisis in Indian country and beyond hearing before the Committee on Indian Affairs, United States Senate, One Hundred Eleventh Congress, second session, June 30, 2010. U.S. G.P.O. http://purl.fdlp.gov/GPO/gpo2845 (accessed 1 Jul 2013) 30.
- 30.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: prevalence and trends data 2004, diabetes, obesity, physical inactivity. http://www.cdc.gov/brfss/annual_data/annual_2004.htm (accessed 1 Jan 2014).
- 31.United States Department of Agriculture. Food access. Food Environment Atlas Data: United States Department of Agriculture, 2006. http://www.ers.usda.gov/data-products/food-environment-atlas.aspx#.UtbHK7Sad60 (accessed 1 Sep 2013). [Google Scholar]
- 32.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: prevalence and trends data 2005, smoking. http://www.cdc.gov/brfss/annual_data/annual_2005.htm (accessed 1 Jan 2014).
- 33.United States Department of Agriculture. Nonmetro persistent poverty counties, 1990. http://www.ers.usda.gov/data-products/county-typology-codes.aspx#.UtQJ87TMpZk (accessed 1 Dec 2013).
- 34.Mitchell FM. Reframing diabetes in American Indian communities: a social determinants of health perspective. Health Soc Work 2012;37:71–9. 10.1093/hsw/hls013 [DOI] [PubMed] [Google Scholar]


