Abstract
Background
Complex wounds present a substantial economic burden on healthcare systems, costing billions of dollars annually in North America alone. The prevalence of complex wounds is a significant patient and societal healthcare concern and cost-effective wound care management remains unclear. This article summarizes the cost-effectiveness of interventions for complex wound care through a systematic review of the evidence base.
Methods
We searched multiple databases (MEDLINE, EMBASE, Cochrane Library) for cost-effectiveness studies that examined adults treated for complex wounds. Two reviewers independently screened the literature, abstracted data from full-text articles, and assessed methodological quality using the Drummond 10-item methodological quality tool. Incremental cost-effectiveness ratios were reported, or, if not reported, calculated and converted to United States Dollars for the year 2013.
Results
Overall, 59 cost-effectiveness analyses were included; 71% (42 out of 59) of the included studies scored 8 or more points on the Drummond 10-item checklist tool. Based on these, 22 interventions were found to be more effective and less costly (i.e., dominant) compared to the study comparators: 9 for diabetic ulcers, 8 for venous ulcers, 3 for pressure ulcers, 1 for mixed venous and venous/arterial ulcers, and 1 for mixed complex wound types.
Conclusions
Our results can be used by decision-makers in maximizing the deployment of clinically effective and resource efficient wound care interventions. Our analysis also highlights specific treatments that are not cost-effective, thereby indicating areas of resource savings.
Please see related article: http://dx.doi.org/10.1186/s12916-015-0288-5
Electronic supplementary material
The online version of this article (doi:10.1186/s12916-015-0326-3) contains supplementary material, which is available to authorized users.
Keywords: Complex wound, Cost-benefit analysis, Cost-effectiveness analysis, Research design, Skin ulcer, Systematic review
Background
Complex wounds are those that do not heal after a period of 3 months or more [1]. These types of wounds are a significant burden on the healthcare system and result in patient and caregiver stress, economic loss, and decreased quality of life. At least 1% of individuals living in high economy countries will experience a complex wound in their lifetime [2], and over 6.5 million individuals have a complex wound in the United States alone [3]. Moreover, these types of wounds have a significant economic impact. For example, $10 billion United States dollars (USD) per year in North America is spent managing complex wounds [4], and 4% of the annual National Health Service expenditure in the United Kingdom is spent on care for patients with pressure ulcers [5].
There are three main categories of complex wounds: i) wounds resulting from chronic disease (e.g., venous insufficiency, diabetes), ii) pressure ulcers, and iii) non-healing surgical wounds [6-8]. Treatment is targeted to the type of wound. Managing complex wounds resulting from disease usually involves improving the underlying disease; for example, optimizing diabetes control for patients with diabetes [9]. A clinical assessment and history of mobility and neurological disability is often necessary to treat patients with pressure ulcers [9]. Considerations for managing surgical wound infections include previous antibiotic treatment and immune response [3].
It is estimated that the global wound care market will reach over $22 billion USD annually by 2020 [10]. Due to the burgeoning costs from the management of patients requiring complex wound care, policymakers are interested in finding cost-effective treatments. However, the cost-effectiveness of all interventions available to treat complex wounds is currently unclear. As such, we sought to elucidate cost-effective treatment strategies for complex wounds through a systematic review of cost-effectiveness analyses.
Methods
Protocol
The systematic review question was posed by members of the Toronto Central Local Health Integrated Network. In collaboration with the Toronto Central Local Health Integrated Network, our research team prepared a draft protocol that was revised to incorporate feedback from systematic review methodologists, policymakers, and clinicians with expertise in wound care (Additional file 1). Our protocol also included conducting a related project comprising an overview of systematic reviews for treating complex wounds, and these results are available in a separate publication [11].
Information sources and search strategy
On October 26, 2012, an experienced librarian conducted comprehensive literature searches in the following electronic databases from inception onwards: MEDLINE, EMBASE, and the Cochrane Library. The literature search was limited to adult patients and economic studies. The Peer Review of Electronic Search Strategies (PRESS) checklist [12] was used by another expert librarian to peer review the literature search. The search was revised, as necessary, and the final MEDLINE search is presented in Additional file 2. Full literature searches for the other databases are available upon request. The reference lists of the included studies were searched to identify additional relevant studies.
Eligibility criteria
Inclusion criteria were defined using the ‘Patients, interventions, comparators, outcomes, study designs, timeframe’ (PICOST) framework [13], as follows:
Patients
Adults aged 18 years and older experiencing complex wounds. Complex wounds included those due to chronic disease (such as diabetic foot ulcers or venous leg ulcers), pressure ulcers (such as decubitus ulcers or bed sores), and non-healing surgical wounds.
Interventions
All complex wound care interventions were included, as identified from our overview of systematic reviews [11] and outlined in Additional file 3.
Comparators
All comparators were eligible for inclusion, including any of the eligible interventions in comparison with each other or versus no treatment or placebo or usual care.
Outcomes
Cost-effectiveness (i.e., both incremental cost and incremental effectiveness) was included, where effectiveness was measured by at least one of the following outcomes: quality-adjusted life-years (QALYs), wounds healed, ulcer-free/healing time, wound size reduction/improvement, or hospitalizations (number/length of stay).
Study designs
Economic evaluations were included in which the incremental cost-effectiveness ratios (ICERs) were reported or could be derived.
Timeframe
We did not limit inclusion to year of publication.
Other limitations
We limited cost-effectiveness analyses to those based on a study with a control group, and where the data were from direct comparisons (versus a review using indirect data). Both published and unpublished studies were eligible for inclusion. Although we focused inclusion on those studies written in English, we contacted the authors of potentially relevant non-English studies to obtain the English translation.
Screening process for study selection
The team pilot-tested the pre-defined eligibility criteria using a random sample of 50 included titles and abstracts. After 90% agreement was reached, each title and abstract was screened by two team members, independently, using our Synthesi.SR tool [14]. Discrepancies were resolved by discussion or the involvement of a third reviewer. The same process was followed for screening full-text articles that were identified as being potentially relevant after screening their titles and abstracts.
Data abstraction and data collection process
The team pilot-tested data abstraction forms using a random sample of five included cost-effectiveness analyses. Subsequently, two investigators independently read each article and abstracted relevant data. Differences in abstraction were resolved by discussion or the involvement of a third reviewer. Data items included study characteristics (e.g., type of economic evaluation, time horizon, treatment interventions examined, study comparators), patient characteristics (e.g., clinical population, wound type), and cost-effectiveness results (e.g., ICERs, cost per QALY, cost per wound healed). The perspective of the economic evaluation was categorized as: patient, public payer, provider, healthcare system, or society [15].
Cost-effectiveness studies can have four possible overall results, which are often represented graphically in quadrants on a cost-effectiveness plane [16]. The possibilities for the intervention versus a comparator are: 1) more effective and less costly, which we noted as ‘dominant’; 2) more effective and more costly; 3) less effective and less costly; and 4) less effective and more costly, which we noted as ‘dominated’. The first possibility is considered to be cost-effective; whereas possibility 4 is not cost-effective. Situations 2 and 3 requires judgment by the decision-maker to interpret [17], and in such cases, the decision is often dependent on the decision-maker’s willingness to pay. For interventions that were found to be more effective yet more costly (i.e., situation 2) or less effective and less costly (situation 3), ICERs were reported or derived from both the differences in cost (i.e., incremental cost) and effectiveness (i.e., incremental effectiveness) between the study’s intervention and comparator groups using the formula:
(Cost of the intervention – Cost of the comparator) ÷ (Effectiveness of the intervention – Effectiveness of the comparator)
To assess key variables influencing the cost-effectiveness results, sensitivity analyses, level of uncertainty in the cost and benefit estimates, and incremental variabilities (i.e., the variability of the incremental cost and the variability of the incremental effectiveness), were reported.
Authors of the included cost-effectiveness analyses were contacted for data verification, as necessary. Further, multiple studies reporting the same economic data were sorted into the major publication (e.g., most recent paper or largest sample size) and companion report. Our results focus on the major publications and the companion reports were used to provide supplementary material.
Methodological quality appraisal
The methodological quality of the cost-effectiveness analyses was appraised using a 10-item tool developed by Drummond et al. (Additional file 4) [18]. The items on this tool include the appraisal of question definition, description of competing alternatives, effectiveness of the intervention, consideration of all relevant costs, measurement of costs, valuation of costs and consequences, cost adjustment/discounting, incremental analysis, uncertainty/sensitivity analysis, and discussion of study results. The Drummond score can range from 0 to 10. Each included cost-effectiveness analysis was appraised by two team members and conflicts were resolved by discussion or the involvement of a third reviewer.
Synthesis
Since the purpose of this systematic review was to summarize the cost-effectiveness of interventions for complex wound care, the results are reported descriptively. The costing data from all studies were converted to 2013 USD to increase the comparability of the economic results across cost-effectiveness studies. This process entailed first converting the currencies into USD using purchasing power parities for the particular year of the data [19,20], and then adjusting these for inflation to the year 2013 (rounded to the nearest dollar) using the consumer price index for medical care in the United States [21].
Results
Literature search and screening
The literature search identified 422 potentially relevant full-text articles after screening 6,200 titles and abstracts (Figure 1). There were 59 included cost-effectiveness analyses that fulfilled our eligibility criteria and were included [22-80], plus an additional three companion reports [81-83].
Figure 1.
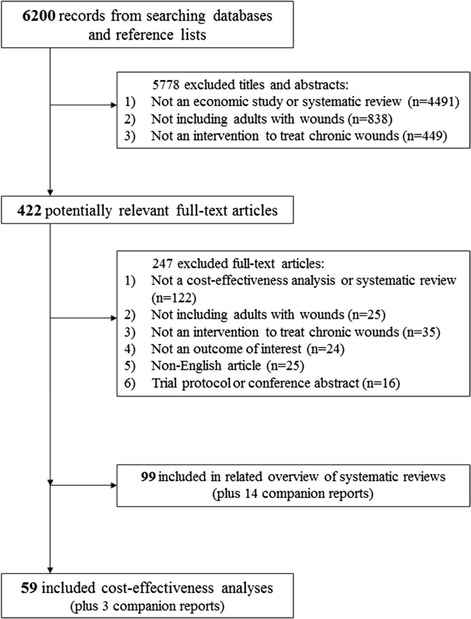
Study flow diagram.
Study and patient characteristics
The cost-effectiveness analyses evaluated interventions to treat venous ulcers (41%), diabetic ulcers (27%), and pressure ulcers (24%) (Table 1). The studies were published between 1988 and 2012. Most of the papers were conducted in the United Kingdom (29%) and United States (27%). Almost half (49%) reported private or mixed (private and public) funding sources of the studies, while one-third (34%) did not report a source of funding.
Table 1.
Summary characteristics of all cost-effectiveness analyses (CEAs)
| Characteristic | No. of CEAs (n = 59) | Percentage of CEAs |
|---|---|---|
| Original year of values | ||
| 1982–1996 | 15 | 25.4 |
| 1997–2000 | 19 | 32.2 |
| 2001–2005 | 10 | 16.9 |
| 2006–2010 | 15 | 25.4 |
| Year of publication | ||
| 1988–1996 | 7 | 11.9 |
| 1997–2001 | 21 | 35.6 |
| 2002–2006 | 12 | 20.3 |
| 2007–2012 | 19 | 32.2 |
| Country of conduct | ||
| Europe (17 from the UK) | 34 | 57.6 |
| North America (16 from USA) | 19 | 32.2 |
| Asia | 3 | 5.1 |
| Australia and New Zealand | 3 | 5.1 |
| Perspective | ||
| Public payer | 17 | 28.8 |
| Society | 8 | 13.6 |
| Provider | 6 | 10.2 |
| Health care system | 1 | 1.7 |
| Not reported | 27 | 45.8 |
| Efficacy study design | ||
| RCT | 44 | 74.6 |
| Observational | 9 | 15.3 |
| Systematic review of RCT | 4 | 6.8 |
| Systematic reviewa | 1 | 1.7 |
| Pseudo-RCT | 1 | 1.7 |
| Sample size b | ||
| 10–30 | 4 | 6.8 |
| 31–50 | 11 | 18.6 |
| 51–100 | 12 | 20.3 |
| 101–150 | 5 | 8.5 |
| 151–200 | 3 | 5.1 |
| 201–400 | 16 | 27.1 |
| >400 | 8 | 13.6 |
| Patient age c (years) | ||
| 50–59 | 5 | 8.5 |
| 60–69 | 20 | 33.9 |
| 70–79 | 18 | 30.5 |
| 80–89 | 8 | 13.6 |
| Not reported | 8 | 13.6 |
| Timeframe | ||
| ≤12 weeks | 28 | 47.5 |
| 13–24 weeks | 9 | 15.3 |
| >24 weeks | 22 | 37.3 |
| Funding source d | ||
| Private | 23 | 39.0 |
| Public | 10 | 16.9 |
| Mixed | 6 | 10.2 |
| Not reported | 20 | 33.9 |
| Type of wound | ||
| Venous ulcers | 24 | 40.7 |
| Diabetic ulcers | 16 | 27.1 |
| Pressure ulcers | 14 | 23.7 |
| Mixed wounds | 3 | 5.1 |
| Mixed venous and venous/arterial ulcers | 2 | 3.4 |
| Unit of effectiveness | ||
| Additional wound healed | 26 | 44.1 |
| QALY gained | 10 | 16.9 |
| Ulcer-free time (day/week/month) gained | 9 | 15.3 |
| Percentage additional reduction of ulcer (area/volume/volume per week) | 8 | 13.6 |
| Increase in healing rate | 2 | 3.4 |
| Reduction in DESIGN score | 1 | 1.7 |
| Patient-year gained | 1 | 1.7 |
| Hospital-free day gained | 1 | 1.7 |
| Foot-related hospitalization avoided | 1 | 1.7 |
| Interventions e | ||
| Dressings | 17 | 24.3 |
| Bandage | 12 | 17.1 |
| Biologics | 8 | 11.4 |
| Topical Tx | 8 | 11.4 |
| Wound care programs | 7 | 10.0 |
| Devices | 5 | 7.1 |
| Skin replacement Tx | 4 | 5.7 |
| Oral Tx | 3 | 4.3 |
| Support surfaces | 2 | 2.9 |
| Stockings | 1 | 1.4 |
| Surgery | 1 | 1.4 |
| Wound cleansing | 1 | 1.4 |
| Unspecified | 1 | 1.4 |
| Comparators e | ||
| Dressings | 17 | 24.3 |
| Bandage | 8 | 11.4 |
| No Tx | 6 | 8.6 |
| Biologics | 4 | 5.7 |
| Stockings | 2 | 2.9 |
| Support surfaces | 2 | 2.9 |
| Topical Tx | 2 | 2.9 |
| Wound care programs | 2 | 2.9 |
| Devices | 1 | 1.4 |
| Surgery | 1 | 1.4 |
| Usual care/Unspecified | 25 | 35.7 |
QALY, Quality-adjusted life-year; RCT, Randomized clinical trial; Tx, Therapy/treatment.
aNot specified if the included studies were RCTs.
bFor studies based on a review, this refers to the total sample size of the combined studies that the data were estimated from.
cAge here refers to mean age or the age used in the model.
dMixed here indicates both private and public funding.
eNumbers do not add up to 59 as some studies contributed data to more than one category.
While the majority of studies based effectiveness on a (single) randomized clinical trial (75%), only a few based effectiveness on a systematic review (9%) and 15% were based on observational studies (Tables 2, 3, 4, 5 and 6). Almost half (46%) of the economic studies included a sample size of 10 to 100 patients and the rest had a sample of >100 patients. In addition, 48% were conducted in a timeframe of 12 weeks or less, while the other studies had a duration of >12 weeks follow-up. Across the 59 economic studies, 9 different units of effectiveness were used, with the most common ones being healed wound (44%) and QALY (17%). Regarding the perspective of the cost-effectiveness analysis, almost half (46%) did not report this explicitly and 29% reported using the public payer perspective.
Table 2.
Characteristics of each cost-effectiveness analysis (CEA) for venous ulcers (n = 24)
| CEA (Original year of values) | Country (Original currency) | Perspective | Efficacy study design | Sample size | Population | Timeframe | Funding source a |
|---|---|---|---|---|---|---|---|
| Augustin 1999 (1989) [22] | Germany (DM) | Not reported | RCT | 25 | Mean 61 yrs; venous insufficiency | 24 wks | Not reported |
| DePalma 1999 (1998) [23] | USA (US$) | Not reported | RCT | 38 | Mean 61 yrs; venous insufficiency | max. 12 wks | Private |
| Glinski 1999 (1998) [24] | Poland (PLN) | Public payer | RCT | 140 | Mean 65 yrs; venous insufficiency | 24 wks | Not reported |
| Gordon 2006 (2005) [25] | Australia (AU$) | Society | RCT | 56 | Most >71 yrs; venous insufficiency | 24 wks | Not reported |
| Guest 2012 (2010) [26] | UK (£) | Public payer | Observational | 510 | Mean 80 yrs; venous insufficiency | 24 wks | Private |
| Iglesias 2006 (2004) [27] | UK (£) | Public payer | SR of RCTs | 434 | 66 yrs; venous insufficiency | 52 wks | Public |
| Iglesias 2004 (2001) [28] | UK (£) | Public payer | RCT | 387 | Mean 71 yrs; venous insufficiency | 52 wks | Public |
| Jull 2008 (2005) [29] | New Zealand (NZ$) | Public payer | RCT | 368 | Mean 68 yrs; venous insufficiency | 12 wks | Mixed |
| Junger 2008 (2007) [30] | Germany (DM) | Not reported | RCT | 39 | Mean 67 yrs; venous insufficiency | 17 wks | Private |
| Kerstein 2000 (1995) [31] | USA (US$) | Not reported | Observational | 81 | Mean 65 yrs; venous insufficiency | 3 yrs | Not reported |
| Kikta 1988 (1987) [32] | USA (US$) | Not reported | RCT | 87 | Venous insufficiency; (ages NR) | 24 wks | Not reported |
| Michaels 2009 (2007) [33] | UK(£) | Public payer | RCT | 213 | Mean 71 yrs; venous insufficiency | 12 wks | Public |
| Morrell 1998 (1995) [34] | UK (£) | Public payer | RCT | 233 | Mean 74 yrs; venous insufficiency | 52 wks | Public |
| O’Brien 2003 (2000) [35] | Ireland (€) | Public payer | RCT | 200 | Mean 72 yrs; venous insufficiency | 12 wks | Private |
| Oien 2001 (1997) [36] | Sweden (£) | Not reported | Observational | 68 | Mean 76 yrs; venous insufficiency | 12 wks | Not reported |
| Sibbald 2001 (1997) [37] | Canada (CAN$) | Society | RCT | 293 | Elderly; venous insufficiency | 13 wks | Private |
| Taylor 1998 (1987) [38] | UK (£) | Not reported | RCT | 36 | Mean 75 yrs; venous insufficiency | 12 wks | Private |
| Ukat 2003 (2002) [39] | Germany (€) | Not reported | RCT | 89 | Mean 69 yrs; venous insufficiency | 12 wks | Private |
| Watson 2011 (2007) [40] | UK (£) | Public payer | RCT | 337 | Mean 69 yrs; venous insufficiency | 52 wks | Public |
| Pham 2012 (2009) [41] | Canada (CAN$) | Society | RCT | 424 | Mean 65 yrs; venous insufficiency; most fully mobile | max. 52 wks | Public |
| Schonfeld 2000 (1996) [42] | USA(US$) | Public payer | RCT | 240 | Mean 60 yrs; venous insufficiency | 52 wks | Private |
| Simon 1996 (1993) [43] | UK (£) | Not reported | Observational | 901 | Venous insufficiency; (ages not reported) | 13 wks | Mixed |
| Carr 1999 (1998) [44] | UK (£) | Public payer | RCT | 233 | Mean 73 yrs; venous insufficiency | 52 wks | Private |
| Guest 2009 (2007) [45] | UK (£) | Public payer | RCT | 83 | Mean 71 yrs; venous insufficiency | 52 wks | Private |
RCT, Randomized clinical trial; SR, Systematic review; wks, Weeks; yrs, Years.
aMixed here indicates both private and public funding.
Table 3.
Characteristics of each cost-effectiveness analysis (CEA) for venous and venous/arterial ulcers (n = 2)
| CEA (Original year of values) | Country (Original currency) | Perspective | Efficacy study design | Sample size | Population | Timeframe | Funding source |
|---|---|---|---|---|---|---|---|
| Dumville 2009 (2006) [46] | UK (£) | Public payer | RCT | 267 | Mean 74 yrs; venous insufficiency | 52 wks | Not reported |
| Ohlsson 1994 (1993) [47] | Sweden (SEK) | Not reported | RCT | 30 | Median 76 yrs; venous insufficiency; most female | 6 wks | Not reported |
RCT, Randomized clinical trial; WKS, Weeks; Yrs, Years.
Table 4.
Characteristics of each cost-effectiveness analysis (CEA) for diabetic ulcers (n = 16)
| CEA (Original year of values) | Country (Original currency) | Perspective | Efficacy study design | Sample size | Population | Timeframe | Funding source a |
|---|---|---|---|---|---|---|---|
| Abidia 2003 (2000) [48] | UK (£) | Not reported | RCT | 18 | Mean 71 yrs; diabetes | 52 wks | Not reported |
| Apelqvist 1996 (1993) [49] | Sweden (SEK) | Society | RCT | 41 | Included >40 yrs; diabetes | 12 wks | Mixed |
| Edmonds 1999 (1996) [50] | UK (£) | Provider | RCT | 40 | Mean 66 yrs; diabetes; foot infections | 2 wks | Private |
| Guo 2003 (2001) [51] | USA (US$) | Society | SRb | 126 | 60 yrs; diabetes | 12 yrs | Not reported |
| Habacher 2007 (2001) [52] | Austria (€) | Society | Observational | 119 | Mean 65 yrs; diabetes | 15 yrs | Not reported |
| Horswell 2003 (1999) [53] | USA (US$) | Not reported | Observational | 214 | Mean 54 yrs; diabetes; mostly African-Americans | 52 wks | Not reported |
| Jansen 2009 (2006) [54] | UK (£) | Public payer | RCT | 402 | Mean 58 yrs; diabetes | approx. 4 wks | Private |
| Jeffcoate 2009 (2007) [55] | UK (£) | Public payer | RCT | 317 | Mean 60 yrs; diabetes | 24 wks | Public |
| McKinnon 1997 (1994) [56] | USA (US$) | Provider | RCT | 90 | Mean 60 yrs; diabetes; limb-threatening foot infections | 3 wks | Private |
| Persson 2000 (1999) [57] | Sweden (US$) | Not reported | SR of RCTs | 500 | Median 60 yrs; diabetes | 52 wks | Private |
| Piaggesi 2007 (2006) [58] | Italy (€) | Not reported | RCT | 40 | Mean 60 yrs; diabetes | 12 wks | Private |
| Redekop 2003 (1999) [59] | The Nether-lands (€) | Society | RCT | 208 | Elderly; diabetes | 52 wks | Private |
| Allenet 2000 (1998) [60] | France (FF) | Society | RCT | 235 | Diabetes; (ages not reported) | 52 wks | Not reported |
| Ghatnekar 2002 (2000) [61] | France (€) | Not reported | RCT | 157 | Diabetes; (ages not reported) | 52 wks | Private |
| Ghatnekar 2001 (1999) [62] | UK(US$) | Public payer | SR of RCTs | 449 | Diabetes; (ages not reported) | 52 wks | Private |
| Hailey 2007 (2004) [63] | Canada (CAN$) | Public payer | SR of RCTs | 305 | 65 yrs; diabetes | 12 yrs | Public |
RCT, Randomized clinical trial; SR, Systematic review; wks, Weeks; yrs, Years.
aMixed here indicates both private and public funding.
bNot specified if the included studies were RCTs or not (but states they were prospective controlled clinical studies).
Table 5.
Characteristics of each cost-effectiveness analysis (CEA) for pressure ulcers (n = 14)
| CEA (Original year of values) | Country (Original currency) | Perspective | Efficacy study design | Sample size | Population | Timeframe | Funding source a |
|---|---|---|---|---|---|---|---|
| Branom 2001 (2000) [64] | USA (US$) | Not reported | RCT | 20 | Mean 72 yrs; bedridden | max. 8 wks | Not reported |
| Burgos 2000 (1998) [65] | Spain (Pta) | Not reported | RCT | 37 | Mean 80 yrs | 12 wks | Private |
| Chang 1998 (1997) [66] | Malaysia (RM) | Not reported | RCT | 34 | Mean 58 yrs | max. 8 wks | Private |
| Chuangsu-wanich 2011 (2010) [67] | Thailand (US$) | Not reported | RCT | 45 | Mean 66 yrs | 8 wks | Not reported |
| Ferrell 1995 (1992) [68] | USA (US$) | Provider | RCT | 84 | Mean 81 yrs; mostly Caucasians; most fecal incontinence | 52 wks | Mixed |
| Foglia 2012 (2010) [69] | Italy (€) | Provider | Observational | 362 | Most >80 yrs | 4.3 wks | Not reported |
| Graumlich 2003 (2001) [70] | USA (US$) | Not reported | RCT | 65 | Mean 83 yrs | 8 wks | Public |
| Muller 2001 (1998) [71] | The Netherlands (NLG) | Provider | RCT | 24 | Mean 73 yrs; all females | 12 wks | Private |
| Narayanan 2005 (2004) [72] | USA (US$) | Not reported | Observational | 976 | Most ≥80 yrs; mostly Caucasians | approx. 22 wks | |
| Payne 2009 (2007) [73] | USA (US$) | Provider | RCT | 36 | Mean 73 yrs | 4 wks | Private |
| Robson 2000 (1999) [74] | USA (US$) | Not reported | RCT | 61 | Mean 50 yrs; mostly Caucasians | 5 wks | Mixed |
| Sanada 2010 (2007) [75] | Japan (Yen) | Not reported | Observational | 105 | Mean 75 yrs | 3 wks | Not reported |
| Xakellis 1992 (1990) [76] | USA (US$) | Not reported | RCT | 39 | Mean 80 yrs | 1.4 wks | Mixed |
| Seberrn 1986 (1985) [77] | USA (US$) | Not reported | RCT | 77 | Mean 74 yrs | 8 wks | Not reported |
RCT, Randomized clinical trial; SR, Systematic review; wks, Weeks; yrs, Years.
aMixed here indicates both private and public funding.
Table 6.
Characteristics of each cost-effectiveness analysis (CEA) for mixed wound types (n = 3)
| CEA (Original year of values) | Country (Original currency) | Perspective | Efficacy study design | Sample size | Population | Timeframe | Funding source |
|---|---|---|---|---|---|---|---|
| Bale 1998 (1994) [78] | UK (£) | Not reported | RCT | 100 | Mean 76 yrs | max. 8 wks | Private |
| Terry 2009 (2008) [79] | USA (US$) | Not reported | RCT | 160 | Mean 58 yrs | 6 wks | Public |
| Vu 2007 (2000) [80] | Australia (AU$) | Health care system | Pseudo-RCT | 342 | Mean 83 yrs | 20 wks | Public |
RCT, Randomized clinical trial; wks, Weeks; Yrs, Year.
Methodological quality appraisal
Approximately 71% (42 out of 59) of the cost-effectiveness analyses had a score of 8 or higher out of a total possible score of 10 (Additional file 5, Figure 2). Using the Drummond 10-item tool [18], the key methodological shortcoming across the cost-effectiveness analyses was that only 51% (30 out of 59) had established the ‘effectiveness’ of the intervention using data from efficacy studies (i.e., systematic reviews, randomized clinical trials or observational studies) that had sufficiently large sample sizes according to the International Conference on Harmonisation guidelines for establishing efficacy [84]. Consistent methodological strengths across the cost-effectiveness analyses included a clear research question, costs and consequences measured in appropriate physical units, credibly valued costs and consequences, and discounted costs (when applicable).
Figure 2.
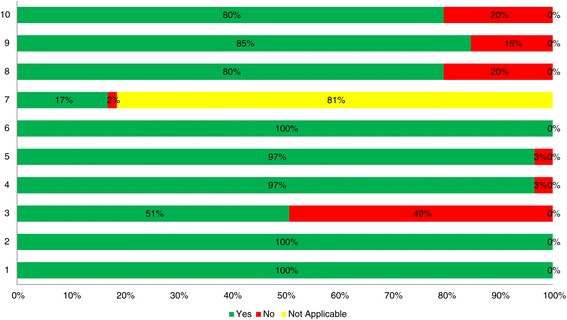
Drummond methodological quality summary results (n = 59). Items: 1. Well-defined question. 2. Competing alternatives well described. 3. Effectiveness established. 4. All important and relevant costs and consequences identified. 5. Measurement accurately performed. 6. Valuation credibility. 7. Discounting. 8. Incremental analysis performed. 9. Allowance made for uncertainty. 10. Discussion.
Cost-effectiveness results
Due to the large number of cost-effectiveness studies included and the numerous results, we have focused on dominant results in the text. However, all of the cost-effectiveness results are presented in Tables 7, 8, 9, 10 and 11 and the sensitivity analyses, level of uncertainty, and incremental variabilities are outlined in Additional file 6.
Table 7.
Cost-effectiveness analysis (CEA) outcomes for venous ulcers (n = 24)
| CEA (Original year of values) | Treatment vs. Comparator | ICER summary/estimate [2013 US$] | Unit of effectiveness | Incremental cost [2013 US$] | Incremental effectiveness |
|---|---|---|---|---|---|
| Augustin 1999 (1989) [22] | Hydrocolloid dressing vs. Vaseline gauze dressing | Dominant | Ulcer-free week gained | −3,362 | 1.3 |
| DePalma 1999 (1998) [23] | Thera-boot vs. Unna’s boot | Dominant | Ulcer-free week gained | −601 | 1.71 |
| Glinski 1999 (1998) [24] | Micronized purified flavonoid fraction + SC vs. SC alone | Dominanta | Additional wound healed | −714 | 0.19 |
| Gordon 2006 (2005) [25] | Community leg club vs. community home nursing | 488a | Additional wound healed | Not reported | Not reported |
| Guest 2012b (2010) [26] | NSBF vs. DBC | 18a | Percent additional reduction of ulcer area | 146 | 8 |
| Guest 2012b (2010) [26] | NSBF vs. no skin protectant | 1a | Percent additional reduction of ulcer area | 17 | 22 |
| Guest 2012b (2010) [26] | DBC vs. no skin protectant | Dominanta | Percent additional reduction of ulcer area | −129 | 14 |
| Iglesias 2006 (2004) [27] | Pentoxifylline plus compression vs. placebo plus compression | Dominanta | QALY gained | −213 | 0.01 |
| Iglesias 2004 (2001) [28] | Four-layer bandage vs. short-stretch bandage | Dominanta | QALY gained | −566 | 0.02 |
| Jull 2008 (2005) [29] | Manuka honey dressing vs. UC | Dominanta,c | Additional wound healed | −48 | 0.06 |
| Junger 2008 (2007) [30] | Low-frequency pulsed current (Dermapulse) vs. placebo | More costly & more effectived | Percent additional reduction of ulcer area | Not reported | Not reported |
| Kerstein 2000b (1995) [31] | Hydrocolloid dressing plus compression hosiery vs. Unna’s boot | Dominant | Additional wound healed | −6,748 | 0.18 |
| Kerstein 2000b (1995) [31] | Unna’s boot vs. saline gauze plus compression hosiery | More costly & more effectived | Additional wound healed | Not reported | Not reported |
| Kikta 1988 (1987) [32] | Unna’s boot vs. hydrocolloid (DuoDERM) | Dominanta | Additional wound healed | −209 | 0.32 |
| Michaels 2009 (2007) [33] | Antimicrobial silver-donating dressings vs. low-adherent dressings | 917,298a | QALY gained | 183 | 0.0002 |
| Morrell 1998 (1995) [34] | Community leg ulcer clinics using four-layer compression bandaging vs. home nursing UC | 7a | Ulcer-free week gained | 44 | 5.9 |
| O’Brien 2003 (2000) [35] | Four-layer bandage vs. UC | Dominanta | Increase in healing rate | −42 | 0.2 |
| Oien 2001 (1997) [36] | Pinch grafting in primary care vs. pinch grafting in hospital | Cost saving & same effectiveness | Additional wound healed | −14,075 | 0 |
| Sibbald 2001 (1997) [37] | Skin substitute (Apligraf) plus four-layer bandage vs. four-layer bandage only | 6095a | Additional wound healed | 457 | 0.075 |
| Taylor 1998 (1987) [38] | Four-layer high-compression bandaging vs. UC | Dominanta | Additional wound healed | −659 | 0.095 |
| Ukat 2003 (2002) [39] | Multilayer elastic bandaging (Profore) vs. short-stretch bandaging | Dominanta | Additional wound healed | −1,198 | 0.08 |
| Watson 2011 (2007) [40] | Ultrasound plus SC vs. SC alone | Dominateda | QALY gained | 371 | −0.009 |
| Pham 2012 (2009) [41] | Four-layer bandaging vs. short-stretch bandaging | 43,918a | QALY gained | 395 | 0.009 |
| Schonfeld 2000 (1996) [42] | Apligraf (Graftskin) vs. Unna’s Boot | Dominanta | Ulcer-free month gained | −13,883 | 2.85 |
| Simon 1996 (1993) [43] | Community leg ulcer clinic vs. UC clinic | Dominant | Additional wound healed | −1,826 | 0.22 |
| Carr 1999 (1998) [44] | Four-layer compression bandaging (Profore) vs. UC | Dominanta | Additional wound healed | −1,289 | 0.13 |
| Guest 2009 (2007) [45] | Amelogenin plus compression therapy vs. compression therapy only | Dominanta | QALY gained | −835 | 0.054 |
DBC, Durable barrier cream; ICER, Incremental cost-effectiveness ratio; NSBF, No sting barrier film; QALY, Quality-adjusted life-year; SC, Standard care; UC, Usual care; US$, United States dollars.
aDenotes the higher quality studies (Drummond score ≥8).
bMultiple comparisons are reported.
cICER was mostly due to an extra 3 patients hospitalized in control group… “probably due to random variation”. If remove these costs, the dominance is reversed in favor of UC.
dUnable to calculate specific ICER for these 2 studies because the data was not reported for all treatment arms or presented in a figure only but the overall result (more costly & more effective) was reported.
Table 8.
Cost-effectiveness analysis (CEA) outcomes for venous and venous/arterial ulcers (n = 2)
| CEA (Original year of values) | Treatment vs. Comparator | ICER summary/estimate [2013 US$] | Unit of effectiveness | Incremental cost [2013 US$] | Incremental effectiveness |
|---|---|---|---|---|---|
| Dumville 2009 (2006) [46] | larval therapy vs. hydrogel | 17,757a | QALY gained | 195 | 0.011 |
| Ohlsson 1994 (1993) [47] | hydrocolloid (DuoDERM) dressing vs. saline gauze | Dominanta | Additional wound healed | −588 | 0.357 |
ICER, Incremental cost-effectiveness ratio; QALY, Quality-adjusted life-year; US$, United States dollars.
aDenotes the higher quality studies (Drummond score ≥8).
Table 9.
Cost-effectiveness analysis (CEA) outcomes for diabetic ulcers (n = 16)
| CEA (Original year of values) | Treatment vs. Comparator | ICER summary/estimate [2013 US$] | Unit of effectiveness | Incremental cost [2013 US$] | Incremental effectiveness |
|---|---|---|---|---|---|
| Abidia 2003 (2000) [48] | HBOT vs. control | Dominant | Additional wound healed | −7,596 | 0.625 |
| Apelqvist 1996 (1993) [49] | Cadexomer iodine ointment vs. standard treatment | Dominanta | Additional wound healed | −119 | 0.183 |
| Edmonds 1999 (1996) [50] | Filgrastim vs. placebo | Dominanta,b | Hospital-free day gained | −7,738 | 7.5 |
| Guo 2003 (2001) [51] | HBOT + SC vs. SC alone | 3508a | QALY gained | 2,137 | 0.609 |
| Habacher 2007 (2001) [52] | Intensified treatment vs. SC | Dominanta | Patient-year gained | −7,625 | 2.97 |
| Horswell 2003 (1999) [53] | Staged management diabetes foot program vs. SC | Dominanta | Foot-related hospitalization avoided | −7,848 | 0.41 |
| Jansen 2009 (2006) [54] | Ertapenem vs. Piperacillin/Tazobactam | Dominanta | Lifetime QALY gained | −822 | 0.12 |
| Jeffcoate 2009c (2007) [55] | Hydrocolloid (Aquacel) vs. antiseptic (Inadine) | 1449a | Additional wound healed | 14 | 0.01 |
| Jeffcoate 2009c (2007) [55] | Antiseptic (Inadine) vs. non-adherent dressing | 1590a | Additional wound healed | 80 | 0.05 |
| McKinnon 1997 (1994) [56] | Ampicillin/sulbactam vs. imipenem/cilastatin | Dominanta | Hospitalization day avoided | −5,891 | 3.5 |
| Persson 2000 (1999) [57] | Becaplermin plus GWC (unspecified) vs. GWC alone | Dominanta | Ulcer-free month gained | −628 | 0.81 |
| Piaggesi 2007 (2006) [58] | Total contact casting vs. Optima Diab device | 8,578 | Additional wound healed | 858 | 0.1 |
| Redekop 2003 (1999) [59] | Apligraf (skin substitute) + GWCd vs. GWC alone | Dominanta | Ulcer-free month gained | −1,223 | 1.53 |
| Allenet 2000 (1998) [60] | Dermagraft (human dermal replacement) vs. SC | 70,961a | Additional wound healed | 12,652 | 0.178 |
| Ghatnekar 2002 (2000) [61] | Promogran dressing plus GWCe vs. GWC alone | Dominanta | Additional wound healed | −294 | 0.042 |
| Ghatnekar 2001 (1999) [62] | Becaplermin gel (containing recombinant human platelet-derived growth factor) plus GWCf vs. GWC alone | Dominanta | Ulcer-free month gained | −794 | 0.81 |
| Hailey 2007 (2004) [63] | HBOT + SC vs. SC alone | Dominant | QALY gained | −9,337 | 0.63 |
GWC, Good wound care; HBOT, Hyperbaric oxygen therapy; ICER, Incremental cost-effectiveness ratio; QALY, Quality-adjusted life-year; SC, Standard care; US$, United States dollars.
aDenotes the higher quality studies (Drummond score ≥8).
b“Patient selection may have occurred during the in-hospital stay where more control patients experienced a bad vascular condition requiring the more costly interventions”.
cMultiple comparisons are reported.
dGWC, “the best wound care available and consists mainly of offloading, debridement, and moist dressings”.
eGWC, “sharp debridement (if necessary) and wound cleansing. In the GWC alone arm, the primary dressing was saline-soaked gauze and the secondary gauze and tape”.
fGWC, “sharp debridement to remove callus, fibrin and necrotic tissue; moist saline dressing changes every 12 hours; systematic control of infection, if present; glucose control; and offloading of pressure”.
Table 10.
Cost-effectiveness analysis (CEA) outcomes for pressure ulcers (n = 14)
| CEA (Original year of values) | Treatment vs. Comparator | ICER summary/estimate [2013 US$] | Unit of effectiveness | Incremental cost [2013 US$] | Incremental effectiveness |
|---|---|---|---|---|---|
| Branom 2001 (2000) [64] | Constant Force Technology mattress vs. low-air-loss mattress | Dominant | Percent additional reduction in wound volume per week | −1,435 | 0.04 |
| Burgos 2000 (1998) [65] | Collagenase ointment vs. hydrocolloid (Varihesive) dressing | 1,278 | Percent additional reduction of ulcer area | 20,825 | 16.3 |
| Chang 1998 (1997) [66] | Hydrocolloid (DuoDERM CGF) vs. saline gauze | 3 | Percent additional reduction of ulcer area | 121 | 43 |
| Chuangsu-wanich 2011 (2010) [67] | Silver mesh dressing vs. silver sulfadiazine cream | Dominant | Increase in healing rate | −1,695 | 11.89 |
| Ferrell 1995 (1992) [68] | Low-air-loss bed vs. conventional foam mattress | 58a | Ulcer-free day gained | Not reported | Not reported |
| Foglia 2012 (2010) [69] | Advanced dressings vs. simple dressings | Dominanta | Percent additional reduction of ulcer area | −132 | 6 |
| Graumlich 2003 (2001) [70] | Collagen (Medifil) vs. hydrocolloid (DuoDERM) | 63,147a | Additional wound healed | 632 | 0.01 |
| Muller 2001 (1998) [71] | Collagenase-containing ointment (Novuxol) vs. hydrocolloid (DuoDERM) dressing | Dominanta | Additional wound healed | −149 | 0.281 |
| Narayanan 2005b (2004) [72] | Initial wound stage 1: BCT (balsam Peru + hydrogenated castor oil + trypsin ointment) only vs. BCT + Others (BCT plus Other treatments) | Dominant | Additional wound healed | −5 | 0.106 |
| Narayanan 2005b (2004) [72] | Initial wound stage 1: BCT + Others vs. Others | Dominant | Additional wound healed | −10 | 0.263 |
| Narayanan 2005b (2004) [72] | Initial wound stage 2: BCT only vs. Others | Dominant | Additional wound healed | −6 | 0.16 |
| Narayanan 2005b (2004) [72] | Initial wound stage 2: BCT only vs. BCT + Others | Dominant | Additional wound healed | −7 | 0.159 |
| Narayanan 2005b (2004) [72] | Initial wound stage 2: BCT + Others vs. Others | 226,208 | Additional wound healed | 226 | 0.001 |
| Payne 2009 (2007) [73] | Polyurethane foam dressing (Allevyn Thin) vs. saline gauze | Dominant | Additional wound healed | −564 | 0.181 |
| Robson 2000b (1999) [74] | Sequential GM-CSF and bFGF vs. bFGF only | Dominant | Percent additional reduction of ulcer volume | 1,357 | −0.07 |
| Robson 2000b (1999) [74] | Sequential GM-CSF and bFGF vs. GM-CSF only | Dominant | Percent additional reduction of ulcer volume | −848 | 1 |
| Robson 2000b (1999) [74] | Placebo vs. sequential GM-CSF and bFGF | 735 | Percent additional reduction of ulcer volume | 2,205 | 3 |
| Sanada 2010 (2007) [75] | New incentive system vs. non-introduced control | Dominant | reduction in DESIGN score | −16 | 4.1 |
| Xakellis 1992 (1990) [76] | Hydrocolloid (DuoDERM) vs. gauze | Dominanta | ulcer-free day gained | −25 | 2 |
| Sebern 1986b (1985) [77] | Grade II PrU: MVP vs. gauze | Dominanta | percent additional reduction of ulcer area | −1,925 | 48 |
| Sebern 1986b (1985) [77] | Grade III PrU: MVP vs. gauze | 9a | percent additional reduction of ulcer area | 217 | 23 |
BCT, Balsam Peru plus hydrogenated castor oil plus trypsin ointment; bFGF, Basic fibroblast growth factor; GM-CSF, Granulocyte-macrophage/colony-stimulating factor; ICER, Incremental cost-effectiveness ratio; MVP, Moisture vapor permeable dressing; PrU, Pressure ulcer; QALY, Quality-adjusted life-year; US$, United States dollars.
aDenotes the higher quality studies (Drummond score ≥8).
bMultiple comparisons are reported.
Table 11.
Cost-effectiveness analysis (CEA) outcomes for mixed wound types (n = 3)
| CEA (Original year of values) | Treatment vs. Comparator | ICER summary/estimate [2013 US$] | Unit of effectiveness | Incremental cost [2013 US$] | Incremental effectiveness |
|---|---|---|---|---|---|
| Bale 1998 (1994) [78] | Hydrocellular (Allevyn) dressing vs. hydrocolloid (Granuflex) dressing | 26 | Additional wound healed | 3 | 0.13 |
| Terry 2009 (2008) [79] | Telemedicine plus WCS consults vs. WCS consults only | Dominateda | Additional wound healed | 2,085 | −0.249 |
| Vu 2007 (2000) [80] | Multidisciplinary wound care team vs. UC | Dominantb | Additional wound healed | −346 | 0.092 |
ICER, Incremental cost-effectiveness ratio; UC, Usual care; US$, United States dollars; WCS, Wound care specialist.
a“Disproportionate distribution, by chance, in group A [telemedicine plus WCS consults] of large non-healing surgical wounds and large, numerous pressure ulcers”.
bDenotes the higher quality study (Drummond score ≥8).
Venous ulcers
Twenty-four cost-effectiveness analyses examined interventions for venous ulcers (Table 7) [22-45,83]. Sixteen studies found the interventions were dominant (i.e., more effective and less costly) [22-24,26-29,31,32,35,38,42-45], and 12 of these were studies with a Drummond score ≥8 [24,26-29,32,35,38,39,42,44,45]. These included Apligraf (Graftskin) vs. Unna’s Boot [42], Unna’s boot vs. hydrocolloid (DuoDERM) [32], micronized purified flavonoid fraction plus usual care vs. usual care alone [24], durable barrier cream vs. no skin protectant [26], pentoxifylline plus compression vs. placebo plus compression [27], Manuka honey dressing vs. usual care [29], amelogenin plus compression therapy vs. compression therapy only [45], and four-layer compression bandaging vs. usual care [35,38,44]. Although four-layer compression bandaging vs. short-stretch compression bandaging was found to be dominant in two studies [28,39]], this intervention was more effective and more costly in another economic evaluation [41].
Dominant interventions from four studies scoring <8 on the Drummond tool [22,23,31,43] included hydrocolloid dressing vs. Vaseline gauze dressing [22], hydrocolloid dressing plus compression hosiery vs. Unna’s boot [31], Thera-boot vs. Unna’s boot [23], and community leg ulcer clinic vs. usual care clinic [43].
Mixed venous and venous/arterial ulcers
Two cost-effectiveness analyses evaluated interventions for mixed venous and venous/arterial ulcers (Table 8) [46,47]. Only one study found an intervention to be dominant (and had a Drummond score ≥8); hydrocolloid (DuoDERM) dressing was dominant compared to saline gauze [47].
Diabetic ulcers
Sixteen cost-effectiveness analyses examined interventions for diabetic ulcers (Table 9) [48-63]. Twelve studies found the interventions were dominant [48-50,52-54,56,57,59,61-63], and 10 of these were studies with a Drummond score ≥8 [49,50,52-54,56,57,59,61,62]. These included becaplermin gel (containing recombinant human platelet-derived growth factor) plus good wound care (GWC) vs. GWC alone (note: the various GWC definitions used are outlined in Table 9) [57,62], cadexomer iodine ointment vs. usual care [49], filgrastim vs. placebo [50], intensified treatment vs. usual care [52], staged management diabetes foot program vs. usual care [53], ertapenem vs. piperacillin/tazobactam [54], ampicillin/sulbactam vs. imipenem/cilastatin [56], Apligraf (skin substitute) plus GWC vs. GWC alone [59], and promogran dressing plus GWC vs. GWC alone [61]. Hyperbaric oxygen therapy plus usual care vs. usual care alone was found to be dominant in one study [63], yet was more effective and more costly in another economic evaluation [51].
Dominant interventions from studies scoring <8 on the Drummond tool included hyperbaric oxygen therapy vs. control [48], and hyperbaric oxygen therapy plus standard care vs. standard care alone [63].
Pressure ulcers
Fourteen cost-effectiveness analyses evaluated pressure ulcer interventions (Table 10) [64-77]. Ten studies found the interventions were dominant [64,67,69,71-77], and four of these were studies with a Drummond score ≥8 [69,71,76,77]. These included moisture vapor permeable dressing vs. gauze [for grade II pressure ulcers] [77], advanced dressings vs. simple dressings [69], and hydrocolloid (DuoDERM) vs. gauze [76]. Collagenase-containing ointment (Novuxol) vs. hydrocolloid (DuoDERM) dressing was found to be dominant in one study [71], while collagen (Medifil) vs. hydrocolloid (DuoDERM) was more effective and more costly in another cost-effectiveness analysis [70].
The following interventions were dominant in six studies with a Drummond score <8: constant force technology mattress vs. low-air-loss mattress [64], silver mesh dressing vs. silver sulfadiazine cream [67], balsam Peru plus hydrogenated castor oil plus trypsin ointment vs. balsam Peru plus hydrogenated castor oil plus trypsin ointment plus other treatment (unspecified) for stage 1 and 2 wounds [72], balsam Peru plus hydrogenated castor oil plus trypsin ointment plus other treatment (unspecified) vs. other treatment (unspecified) for stage 1 wounds [72], balsam Peru plus hydrogenated castor oil plus trypsin ointment vs. other treatment (unspecified) for stage 2 wounds [72], polyurethane foam dressing vs. saline gauze [73], sequential granulocyte-macrophage/colony-stimulating factor and basic fibroblast growth factor vs. basic fibroblast growth factor alone [74], sequential granulocyte-macrophage/colony-stimulating factor and basic fibroblast growth factor vs. granulocyte-macrophage/colony-stimulating factor alone [74], and new hospital incentive system vs. non-introduced control [75].
Mixed wound types
Three cost-effectiveness analyses evaluated mixed complex wound types (Table 11) [78-80]. One study with a Drummond score ≥8 found that a multidisciplinary wound care team was dominant compared to usual care [80].
Discussion
We conducted a comprehensive systematic review to summarize the cost-effectiveness of interventions for complex wound care including data from 59 cost-effectiveness analyses. These economic studies examined numerous interventions and comparators and used different outcomes to assess effectiveness. In a few situations, the intervention considered in one cost-effectiveness analysis comprised the comparator in another cost-effectiveness analysis. Therefore, cost-effectiveness results are presented as comparisons of one treatment option relative to another.
Based on evidence from 42 cost-effectiveness studies with a Drummond score ≥8, 22 intervention comparisons were dominant (Additional file 7). For venous ulcers, these were four-layer compression bandaging vs. usual care, skin replacement vs. Unna’s Boot, Unna’s boot vs. hydrocolloid, micronized purified flavonoid fraction plus usual care vs. usual care, durable barrier cream vs. no skin protectant, pentoxifylline plus compression vs. placebo plus compression, Manuka honey dressing vs. usual care, and amelogenin plus compression therapy vs. compression therapy only. For mixed venous and venous/arterial ulcers, only hydrocolloid dressing vs. saline gauze was dominant according to high quality cost-effectiveness analyses. For diabetic ulcers, cadexomer iodine ointment vs. usual care, filgrastim vs. placebo, intensified treatment vs. usual care, staged management diabetes foot program vs. usual care, ertapenem vs. piperacillin/tazobactam, ampicillin/sulbactam vs. imipenem/cilastatin, skin replacement plus GWC vs. GWC alone, promogran dressing plus GWC vs. GWC alone, and becaplermin gel (containing recombinant human platelet-derived growth factor) plus GWC vs. GWC alone were dominant. For pressure ulcers, moisture vapor permeable dressing vs. gauze, advanced dressings vs. simple dressings, and hydrocolloid vs. gauze were dominant. Finally, for mixed wound types, multidisciplinary wound care team was dominant vs. usual care.
Our results highlight a need for a future network meta-analysis given the numerous interventions and comparators available. Network meta-analysis is a statistical technique that can be used to combine direct evidence of effectiveness from head-to-head studies and indirect evidence of the relative benefits of interventions versus a common comparator (usually placebo). This powerful statistical approach can also be used to select the best treatment option available from a ranking of all treatments. An attractive property of network meta-analysis is that it allows researchers and health economists the opportunity to use the ranking analysis to generate a de novo cost-effectiveness analysis more efficiently. Another potential future study is to conduct a systematic review of clinical practice guidelines on complex wounds, and compare the interventions recommended in these with those found to be cost-effective in our review.
The major methodological quality limitation found in the included cost-effectiveness analyses was that the majority did not adequately establish the effectiveness of the wound care intervention using data from systematic reviews, randomized clinical trials, or observational studies that had sufficiently large sample sizes. Moreover, many of the included economic studies did not report on uncertainty of the cost-effectiveness estimates, incremental variabilities, or sensitivity analyses, thereby further limiting the utility of those results. Further, many of the cost-effectiveness analyses did not assess long-term cost-effectiveness, and the choice of timeframe for an economic evaluation might significantly affect the cost-effectiveness results. Given the chronic nature of many types of wounds, economic modeling of a longer time horizon would provide a clearer picture in many circumstances. As an example, an intervention might be more effective yet more costly in the first 2 months of usage but it might be cost saving over a 1 year or longer timeframe due to overall fewer additional interventions required. Furthermore, most of the cost-effectiveness studies did not include information on patient-reported quality of life, which is a major limitation of this literature.
The majority of the included economic studies were from European countries and 16 were from the United States. When trying to apply the cost-effectiveness results to a country-specific context, several factors need to be assessed such as the perspective of the economic evaluation (e.g., public payer, healthcare provider), the type of healthcare system (e.g., publicly-funded healthcare), the local practice of medicine, and local costs.
There are a few limitations related to our systematic review process worth noting. Due to resource constraints, we only included studies written in English. However, we contacted authors of non-English studies to obtain the English translations. In addition, although we contacted authors to share their unpublished data, only published literature was identified for inclusion. Finally, due to the numerous number of cost-effectiveness analyses included, we focused reporting on those with dominant results and a score ≥8 on the Drummond tool in the main text. We note that this is an arbitrary cut-off, and there is not an agreed upon method to provide a summary score on this tool. However, all of our results for all studies are presented in the tables and appendices despite dominance and score on the Drummond tool.
Conclusions
We conducted a comprehensive systematic review of cost-effectiveness studies for interventions to treat adult patients with complex wounds. Our results can be used by decision-makers to assist in maximizing the deployment of clinically effective and resource efficient wound care interventions. Our analysis also highlights specific treatments that are not cost-effective, thus indicating areas for potential improvements in efficiency. A network meta-analysis and de novo cost-effectiveness analysis will likely bring additional clarity to the field, as some of the findings were conflicting.
Acknowledgements
We thank the Toronto Central Local Health Integrated Network (TC LHIN) for their generous funding. ACT is funded by Canadian Institutes for Health Research/Drug Safety and Effectiveness Network (CIHR/DSEN) New Investigator Award in Knowledge Synthesis. SES is funded by a CIHR Tier 1 Research Chair in Knowledge Translation. We thank Dr. James Mahoney and Chris Shumway from the TC LHIN who provided invaluable feedback on our original report. We thank Laure Perrier for conducting the literature searches, and Afshin Vafaei, Alana Harrington, Charlotte Wilson, and John Ivory for screening articles. We also thank Inthuja Selvaratnam and Wasifa Zarin for formatting the report and references, and Judy Tran for obtaining the full-text articles.
Abbreviations
- GWC
Good wound care
- ICER
Incremental cost-effectiveness ratio
- QALY
Quality-adjusted life-year
- USD
United States dollar
Additional files
Wound care protocol. Outlines the protocol used in the systematic review.
MEDLINE search strategy. Lists MEDLINE search terms.
Classification of wound care interventions. Lists the wound care interventions in each classification.
Drummond’s 10-item checklist tool used for cost-effectiveness analyses quality appraisal. Provides the descriptions of the 10 items in Drummond’s 10-item checklist tool.
Cost-effectiveness analysis methodological quality appraisal results. Lists the quality appraisal results for the 59 included cost-effectiveness analyses.
Cost-effectiveness analyses sensitivity analysis, uncertainty of results and incremental variabilities. Outlines the sensitivity analyses, level of uncertainty, and incremental variabilities for the cost-effectiveness analyses results.
Summary of the less costly and more effective interventions for studies with a Drummond score ≥8. Lists 42 cost-effectiveness studies with a Drummond score ≥8.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ACT conceived the study, helped obtain funding for the study, screened articles, analyzed the data, interpreted the results, and wrote the manuscript. EC coordinated the study, peer reviewed the MEDLINE search, screened articles, abstracted data, appraised quality, cleaned the data, converted the costs, analyzed the data, generated tables, interpreted the results, and helped write the manuscript. WI abstracted data, appraised quality, and edited the manuscript. PAK screened articles, abstracted data, scanned reference lists, and edited the manuscript. GS screened articles, abstracted data, appraised quality, and edited the manuscript. JA helped coordinate the review, screened articles, and edited the manuscript. JSH provided economic guidance and edited the manuscript. SES conceived and designed the study, obtained the funding, interpreted the results, and edited the manuscript. All authors read and approved the final manuscript.
Contributor Information
Andrea C Tricco, Email: triccoa@smh.ca.
Elise Cogo, Email: cogoe@smh.ca.
Wanrudee Isaranuwatchai, Email: isaranuwatcw@smh.ca.
Paul A Khan, Email: khanp@smh.ca.
Geetha Sanmugalingham, Email: geetha.sanmugalingham@alumni.utoronto.ca.
Jesmin Antony, Email: antonyj@smh.ca.
Jeffrey S Hoch, Email: hochj@smh.ca.
Sharon E Straus, Email: sharon.straus@utoronto.ca.
References
- 1.Mustoe TA, O’Shaughnessy K, Kloeters O. Chronic wound pathogenesis and current treatment strategies: a unifying hypothesis. Plast Reconstr Surg. 2006;117:35S–41. doi: 10.1097/01.prs.0000225431.63010.1b. [DOI] [PubMed] [Google Scholar]
- 2.Gottrup F. A specialized wound-healing center concept: importance of a multidisciplinary department structure and surgical treatment facilities in the treatment of chronic wounds. Am J Surg. 2004;187:38S–43. doi: 10.1016/S0002-9610(03)00303-9. [DOI] [PubMed] [Google Scholar]
- 3.Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009;17:763–71. doi: 10.1111/j.1524-475X.2009.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swanson L. Solving stubborn-wound problem could save millions, team says. CMAJ. 1999;160:556. [PMC free article] [PubMed] [Google Scholar]
- 5.Miller PS. In economics as well as medicine prevention is better than cure. Age Ageing. 2004;33:217–8. doi: 10.1093/ageing/afh085. [DOI] [PubMed] [Google Scholar]
- 6.Canadian Association of Wound Care. Best practice articles. http://cawc.net/index.php/resources/resources/clinical-practice/.
- 7.Jull AB, Rodgers A, Walker N. Honey as a topical treatment for wounds. Cochrane Database Syst Rev. 2008;4 doi: 10.1002/14651858.CD005083.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Lazarus GS, Cooper DM, Knighton DR, Percoraro RE, Rodeheaver G, Robson MC. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 1994;2:165–70. doi: 10.1046/j.1524-475X.1994.20305.x. [DOI] [PubMed] [Google Scholar]
- 9.Werdin F, Tennenhaus M, Schaller HE, Rennekampff HO. Evidence-based management strategies for treatment of chronic wounds. Eplasty. 2009;9:e19. [PMC free article] [PubMed] [Google Scholar]
- 10.Global Industry Analysts. Advanced wound care: a global strategic business report. http://www.marketresearch.com/Global-Industry-Analysts-v1039/Advanced-Wound-Care-8102385/.
- 11.Tricco A, Antony J, Vafaei A, Khan PA, Cogo E, Wilson C, et al. Seeking effective interventions to treat complex wounds: an overview of systematic reviews. BMC Med. 2015, DOI: 10.1186/s12916-015-0288-5. [DOI] [PMC free article] [PubMed]
- 12.Sampson M, McGowan J, Cogo E, Grimshaw J, Moher D, Lefebvre C. An evidence-based practice guideline for the peer review of electronic search strategies. J Clin Epidemiol. 2009;62:944–52. doi: 10.1016/j.jclinepi.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 13.Stone PW. Popping the (PICO) question in research and evidence-based practice. Appl Nurs Res. 2002;15:197–8. doi: 10.1053/apnr.2002.34181. [DOI] [PubMed] [Google Scholar]
- 14.Newton D. Synthesi.SR. http://knowledgetranslation.ca/sysrev/login.php.
- 15.Centers for Disease Control and Prevention. Public health economics and tools. http://www.cdc.gov/stltpublichealth/pheconomics/.
- 16.Black WC. The CE, plane: a graphic representation of cost-effectiveness. Med Decis Making. 1990;10:212–4. doi: 10.1177/0272989X9001000308. [DOI] [PubMed] [Google Scholar]
- 17.Government of Ontario. Ontario guidelines for economic analysis of pharmaceutical products: interpretation of cost-effectiveness ratios. http://www.health.gov.on.ca/english/providers/pub/drugs/economic/econ_ratios.html.
- 18.Drummond MF. Methods for the economic evaluation of health care programmes. 3. Oxford, New York: Oxford University Press; 2005. [Google Scholar]
- 19.OECD. StatExtracts, PPPs and exchange rates. http://stats.oecd.org/Index.aspx?datasetcode=SNA_TABLE4.
- 20.Economy Watch. Implied PPP conversion rate data for year 1997, all countries. http://www.economywatch.com/economic-statistics/economic-indicators/Implied_PPP_Conversion_Rate/1997/.
- 21.US Bureau of Labor Statistics. Consumer price index – all urban consumers (current series). http://data.bls.gov/pdq/querytool.jsp?survey=cu.
- 22.Augustin M, Siegel A, Heuser A, Vanscheidt W. Chronic leg ulcers: cost evaluation of two treatment strategies. J Dermatolog Treat. 1999;10:S21–5. [Google Scholar]
- 23.DePalma RG, Kowallek D, Spence RK, Caprini JA, Nehler MR, Jensen J, et al. Comparison of costs and healing rates of two forms of compression in treating venous ulcers. Vasc Surg. 1999;33:683–90. doi: 10.1177/153857449903300617. [DOI] [Google Scholar]
- 24.Glinski W, Chodynicka B, Roszkiewicz J, Bogdanowski T, Lecewicz-Torun B, Kaszuba A, et al. The beneficial augmentative effect of micronised purified flavonoid fraction (MPFF) on the healing of leg ulcers: An open, multicentre, controlled, randomised study. Phlebology. 1999;14:151–7. doi: 10.1007/s005239970005. [DOI] [Google Scholar]
- 25.Gordon L, Edwards H, Courtney M, Finlayson K, Shuter P, Lindsay E. A cost-effectiveness analysis of two community models of care for patients with venous leg ulcers. J Wound Care. 2006;15:348–53. doi: 10.12968/jowc.2006.15.8.26942. [DOI] [PubMed] [Google Scholar]
- 26.Guest JF, Taylor RR, Vowden K, Vowden P. Relative cost-effectiveness of a skin protectant in managing venous leg ulcers in the UK. J Wound Care. 2012;21:389–94. doi: 10.12968/jowc.2012.21.8.389. [DOI] [PubMed] [Google Scholar]
- 27.Iglesias CP, Claxton K. Comprehensive decision-analytic model and Bayesian value-of-information analysis: pentoxifylline in the treatment of chronic venous leg ulcers. Pharmacoeconomics. 2006;24:465–78. doi: 10.2165/00019053-200624050-00005. [DOI] [PubMed] [Google Scholar]
- 28.Iglesias CP, Nelson EA, Cullum N, Torgerson DJ, VenUS I Collaborators Economic analysis of VenUS I, a randomized trial of two bandages for treating venous leg ulcers. Br J Surg. 2004;91:1300–6. doi: 10.1002/bjs.4755. [DOI] [PubMed] [Google Scholar]
- 29.Jull A, Walker N, Parag V, Molan P, Rodgers A. Randomized clinical trial of honey‐impregnated dressings for venous leg ulcers. Br J Surg. 2008;95:175–82. doi: 10.1002/bjs.6059. [DOI] [PubMed] [Google Scholar]
- 30.Junger M, Arnold A, Zuder D, Stahl HW, Heising S. Local therapy and treatment costs of chronic, venous leg ulcers with electrical stimulation (Dermapulse): a prospective, placebo controlled, double blind trial. Wound Repair Regen. 2008;16:480–7. doi: 10.1111/j.1524-475X.2008.00393.x. [DOI] [PubMed] [Google Scholar]
- 31.Kerstein MD, Gahtan V. Outcomes of venous ulcer care: results of a longitudinal study. Ostomy Wound Manage. 2000;46:22–6. [PubMed] [Google Scholar]
- 32.Kikta MJ, Schuler JJ, Meyer JP, Durham JR, Eldrup-Jorgensen J, Schwarcz TH, et al. A prospective, randomized trial of Unna’s boots versus hydroactive dressing in the treatment of venous stasis ulcers. J Vasc Surg. 1988;7:478–83. doi: 10.1016/0741-5214(88)90466-1. [DOI] [PubMed] [Google Scholar]
- 33.Michaels JA, Campbell WB, King BM, Macintyre J, Palfreyman SJ, Shackley P, et al. A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial. Health Technol Assess. 2009;13:1–114. doi: 10.3310/hta13560. [DOI] [PubMed] [Google Scholar]
- 34.Morrell CJ, Walters SJ, Dixon S, Collins KA, Brereton LM, Peters J, et al. Cost effectiveness of community leg ulcer clinics: randomised controlled trial. BMJ. 1998;316:1487–91. doi: 10.1136/bmj.316.7143.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Brien JF, Grace PA, Perry IJ, Hannigan A, Clarke Moloney M, Burke PE. Randomized clinical trial and economic analysis of four-layer compression bandaging for venous ulcers. Br J Surg. 2003;90:794–8. doi: 10.1002/bjs.4167. [DOI] [PubMed] [Google Scholar]
- 36.Oien RF, Hakansson A, Ahnlide I, Bjellerup M, Hansen BU, Borgquist L. Pinch grafting in hospital and primary care: a cost analysis. J Wound Care. 2001;10:164–9. doi: 10.12968/jowc.2001.10.5.26082. [DOI] [PubMed] [Google Scholar]
- 37.Sibbald RG, Torrance GW, Walker V, Attard C, MacNeil P. Cost-effectiveness of Apligraf in the treatment of venous leg ulcers. Ostomy Wound Manage. 2001;47:36–46. [PubMed] [Google Scholar]
- 38.Taylor AD, Taylor RJ, Marcuson RW. Prospective comparison of healing rates and therapy costs for conventional and four-layer high-compression bandaging treatments of venous leg ulcers. Phlebology. 1998;13:20–4. [Google Scholar]
- 39.Ukat A, Konig M, Vanscheidt W, Munter KC. Short-stretch versus multilayer compression for venous leg ulcers: a comparison of healing rates. J Wound Care. 2003;12:139–43. doi: 10.12968/jowc.2003.12.4.26490. [DOI] [PubMed] [Google Scholar]
- 40.Watson JM, Kang’ombe AR, Soares MO, Chuang LH, Worthy G, Bland JM, et al. VenUS III: a randomised controlled trial of therapeutic ultrasound in the management of venous leg ulcers. Health Technol Assess. 2011;15:1–192. doi: 10.3310/hta15130. [DOI] [PubMed] [Google Scholar]
- 41.Pham B, Harrison MB, Chen MH, Carley ME. Cost-effectiveness of compression technologies for evidence-informed leg ulcer care: results from the Canadian Bandaging Trial. BMC Health Serv Res. 2012;12:346–53. doi: 10.1186/1472-6963-12-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schonfeld WH, Villa KF, Fastenau JM, Mazonson PD, Falanga V. An economic assessment of Apligraf (Graftskin) for the treatment of hard-to-heal venous leg ulcers. Wound Repair Regen. 2000;8:251–7. doi: 10.1046/j.1524-475x.2000.00251.x. [DOI] [PubMed] [Google Scholar]
- 43.Simon DA, Freak L, Kinsella A, Walsh J, Lane C, Groarke L, et al. Community leg ulcer clinics: a comparative study in two health authorities. BMJ. 1996;312:1648–51. doi: 10.1136/bmj.312.7047.1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carr L, Phillips Z, Posnett J. Comparative cost-effectiveness of four-layer bandaging in the treatment of venous leg ulceration. J Wound Care. 1999;8:243–8. doi: 10.12968/jowc.1999.8.5.26361. [DOI] [PubMed] [Google Scholar]
- 45.Guest JF, Nagy E, Sladkevicius E, Vowden P, Price P. Modelling the relative cost-effectiveness of amelogenin in non-healing venous leg ulcers. J Wound Care. 2009;18:216. doi: 10.12968/jowc.2009.18.5.42176. [DOI] [PubMed] [Google Scholar]
- 46.Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al. VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers. Health Technol Assess. 2009;13:1–182. doi: 10.3310/hta13550. [DOI] [PubMed] [Google Scholar]
- 47.Ohlsson P, Larsson K, Lindholm C, Moller M. A cost-effectiveness study of leg ulcer treatment in primary care. Comparison of saline-gauze and hydrocolloid treatment in a prospective, randomized study. Scand J Prim Health Care. 1994;14:295–9. doi: 10.3109/02813439409029256. [DOI] [PubMed] [Google Scholar]
- 48.Abidia A, Laden G, Kuhan G, Johnson BF, Wilkinson AR, Renwick PM, et al. The role of hyperbaric oxygen therapy in ischaemic diabetic lower extremity ulcers: a double-blind randomised-controlled trial. Eur J Vasc Endovasc Surg. 2003;25:513–8. doi: 10.1053/ejvs.2002.1911. [DOI] [PubMed] [Google Scholar]
- 49.Apelqvist J, Ragnarson TG. Cavity foot ulcers in diabetic patients: a comparative study of cadexomer iodine ointment and standard treatment. An economic analysis alongside a clinical trial. Acta Derm Venereol. 1996;76:231–5. doi: 10.2340/0001555576231235. [DOI] [PubMed] [Google Scholar]
- 50.Edmonds M, Gough A, Solovera J, Standaert B. Filgrastim in the treatment of infected diabetic foot ulcers. Retrospective cost analysis of a phase II randomised clinical trial. Clin Drug Investig. 1999;17:275–86. doi: 10.2165/00044011-199917040-00003. [DOI] [Google Scholar]
- 51.Guo S, Counte MA, Gillespie KN, Schmitz H. Cost-effectiveness of adjunctive hyperbaric oxygen in the treatment of diabetic ulcers. Int J Technol Assess Health Care. 2003;19:731–7. doi: 10.1017/s0266462303000710. [DOI] [PubMed] [Google Scholar]
- 52.Habacher W, Rakovac I, Gorzer E, Haas W, Gfrerer RJ, Wach P, et al. A model to analyse costs and benefit of intensified diabetic foot care in Austria. Eur J Vasc Endovasc Surg. 2007;13:906–12. doi: 10.1111/j.1365-2753.2006.00770.x. [DOI] [PubMed] [Google Scholar]
- 53.Horswell RL, Birke JA, Patout CA., Jr A staged management diabetes foot program versus standard care: a 1-year cost and utilization comparison in a state public hospital system. Arch Phys Med Rehabil. 2003;84:1743–6. doi: 10.1016/S0003-9993(03)00477-5. [DOI] [PubMed] [Google Scholar]
- 54.Jansen JP, Kumar R, Carmeli Y. Accounting for the development of antibacterial resistance in the cost effectiveness of ertapenem versus piperacillintazobactam in the treatment of diabetic foot infections in the UK. Pharmacoeconomics. 2009;27:1045–56. doi: 10.2165/11310080-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 55.Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al. Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes. Health Technol Assess. 2009;13:1–86. doi: 10.3310/hta13540. [DOI] [PubMed] [Google Scholar]
- 56.McKinnon PS, Paladino JA, Grayson ML, Gibbons GW, Karchmer AW. Cost-effectiveness of ampicillin/sulbactam versus imipenem/cilastatin in the treatment of limb-threatening foot infections in diabetic patients. Clin Infect Dis. 1997;24:57–63. doi: 10.1093/clinids/24.1.57. [DOI] [PubMed] [Google Scholar]
- 57.Persson U, Willis M, Odegaard K, Apelqvist J. The cost-effectiveness of treating diabetic lower extremity ulcers with becaplermin (Regranex): a core model with an application using Swedish cost data. Value Health. 2000;3:39–46. doi: 10.1046/j.1524-4733.2000.36027.x. [DOI] [PubMed] [Google Scholar]
- 58.Piaggesi A, Macchiarini S, Rizzo L, Palumbo F, Tedeschi A, Nobili LA, et al. An off-the-shelf instant contact casting device for the management of diabetic foot ulcers: a randomized prospective trial versus traditional fiberglass cast. Diabetes Care. 2007;30:586–90. doi: 10.2337/dc06-1750. [DOI] [PubMed] [Google Scholar]
- 59.Redekop WK, McDonnel J, Verboom P, Lovas K, Kalo Z. The cost-effectiveness of Apligraf treatment of diabetic foot ulcers. Pharmacoeconomics. 2003;21:1171–83. doi: 10.2165/00019053-200321160-00003. [DOI] [PubMed] [Google Scholar]
- 60.Allenet B, Paree F, Lebrun T, Carr L, Posnett J, Martinin J, et al. Cost-effectiveness modelling of Dermagraft for the treatment of diabetic foot ulcers in the French context. Diabetes Metab. 2000;26:125–32. [PubMed] [Google Scholar]
- 61.Ghatnekar O, Willis M, Persson U. Cost-effectiveness of treating deep diabetic foot ulcers with Promogram in four European countries. J Wound Care. 2002;11:70–4. doi: 10.12968/jowc.2002.11.2.26675. [DOI] [PubMed] [Google Scholar]
- 62.Ghatnekar O, Persson U, Willis M, Odegaard K. Cost effectiveness of becaplermin in the treatment of diabetic foot ulcers in four European countries. Pharmacoeconomics. 2001;19:767–78. doi: 10.2165/00019053-200119070-00005. [DOI] [PubMed] [Google Scholar]
- 63.Hailey D, Jacobs P, Perry DC, Chuck A, Morrison A, Boudreau R. Adjunctive hyperbaric oxygen therapy for diabetic foot ulcer: an economic analysis. Canadian Agency for Drugs and Technologies in Health. 2007;75:1–19. [Google Scholar]
- 64.Branom R, Rappl LM. Constant force technology versus low-air-loss therapy in the treatment of pressure ulcers. Ostomy Wound Manage. 2001;47:38–46. [PubMed] [Google Scholar]
- 65.Burgos A, Gimenez J, Moreno E, Lamberto E, Utrera M, Urraca EM, et al. Cost, efficacy, efficiency and tolerability of collagenase ointment versus hydrocolloid occlusive dressing in the treatment of pressure ulcers. A comparative, randomised, multicentre study. Clin Drug Investig. 2000;19:357–65. doi: 10.2165/00044011-200019050-00006. [DOI] [Google Scholar]
- 66.Chang KW, Alsagoff S, Ong KT, Sim PH. Pressure ulcers–randomised controlled trial comparing hydrocolloid and saline gauze dressings. Med J Malaysia. 1998;53:428–31. [PubMed] [Google Scholar]
- 67.Chuangsuwanich A, Charnsanti O, Lohsiriwat V, Kangwanpoom C, Thong-In N. The efficacy of silver mesh dressing compared with silver sulfadiazine cream for the treatment of pressure ulcers. J Med Assoc Thai. 2011;94:559–65. [PubMed] [Google Scholar]
- 68.Ferrell BA, Keeler E, Siu AL, Ahn SH, Osterweil D. Cost-effectiveness of low-air-loss beds for treatment of pressure ulcers. J Gerontol A Biol Sci Med Sci. 1995;50:M141–6. doi: 10.1093/gerona/50A.3.M141. [DOI] [PubMed] [Google Scholar]
- 69.Foglia E, Restelli U, Napoletano AM, Coclite D, Porazzi E, Bonfanti M, et al. Pressure ulcers management: an economic evaluation. J Prev Med Hyg. 2012;53:30–6. [PubMed] [Google Scholar]
- 70.Graumlich JF, Blough LS, McLaughlin RG, Milbrandt JC, Calderon CL, Agha SA, et al. Healing pressure ulcers with collagen or hydrocolloid: a randomized, controlled trial. J Am Geriatr Soc. 2003;51:147–54. doi: 10.1046/j.1532-5415.2003.51051.x. [DOI] [PubMed] [Google Scholar]
- 71.Muller E, van Leen MW, Bergemann R. Economic evaluation of collagenase-containing ointment and hydrocolloid dressing in the treatment of pressure ulcers. Pharmacoeconomics. 2001;19:1209–16. doi: 10.2165/00019053-200119120-00003. [DOI] [PubMed] [Google Scholar]
- 72.Narayanan S, Van Vleet J, Strunk B, Ross RN, Gray M. Comparison of pressure ulcer treatments in long-term care facilities: clinical outcomes and impact on cost. J Wound Ostomy Continence Nurs. 2005;32:163–70. doi: 10.1097/00152192-200505000-00004. [DOI] [PubMed] [Google Scholar]
- 73.Payne WG, Posnett J, Alvarez O, Brown-Etris M, Jameson G, Wolcott R, et al. A prospective, randomized clinical trial to assess the cost-effectiveness of a modern foam dressing versus a traditional saline gauze dressing in the treatment of stage II pressure ulcers. Ostomy Wound Manage. 2009;55:50–5. [PubMed] [Google Scholar]
- 74.Robson MC, Hill DP, Smith PD, Wang X, Meyer-Siegler K, Ko F, et al. Sequential cytokine therapy for pressure ulcers: clinical and mechanistic response. Ann Surg. 2000;231:600–11. doi: 10.1097/00000658-200004000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sanada H, Nakagami G, Mizokami Y, Minami Y, Yamamoto A, Oe M, et al. Evaluating the effect of the new incentive system for high-risk pressure ulcer patients on wound healing and cost-effectiveness: a cohort study. Int J Nurs Stud. 2010;47:279–86. doi: 10.1016/j.ijnurstu.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 76.Xakellis GC, Chrischilles EA. Hydrocolloid versus saline-gauze dressings in treating pressure ulcers: a cost-effectiveness analysis. Arch Phys Med Rehabil. 1992;73:463–9. [PubMed] [Google Scholar]
- 77.Sebern MD. Pressure ulcer management in home health care: efficacy and cost effectiveness of moisture vapor permeable dressing. Arch Phys Med Rehabil. 1986;67:726–9. doi: 10.1016/0003-9993(86)90004-3. [DOI] [PubMed] [Google Scholar]
- 78.Bale S, Hagelstein S, Banks V, Harding KG. Costs of dressings in the community. J Wound Care. 1998;7:327–30. doi: 10.12968/jowc.1998.7.7.327. [DOI] [PubMed] [Google Scholar]
- 79.Terry M, Halstead LS, O’Hare P, Gaskill C, Ho PS, Obecny J, et al. Feasibility study of home care wound management using telemedicine. Adv Skin Wound Care. 2009;22:358–64. doi: 10.1097/01.ASW.0000358638.38161.6b. [DOI] [PubMed] [Google Scholar]
- 80.Vu T, Harris A, Duncan G, Sussman G. Cost-effectiveness of multidisciplinary wound care in nursing homes: a pseudo-randomized pragmatic cluster trial. Fam Pract. 2007;24:372–9. doi: 10.1093/fampra/cmm024. [DOI] [PubMed] [Google Scholar]
- 81.Sebern MD. Cost and efficacy of pressure ulcer management in a metropolitan visiting nurse association. Decubitus. 1989;2:58–9. [PubMed] [Google Scholar]
- 82.Chuck AW, Hailey D, Jacobs P, Perry DC. Cost-effectiveness and budget impact of adjunctive hyperbaric oxygen therapy for diabetic foot ulcers. Int J Technol Assess Health Care. 2008;24:178–83. doi: 10.1017/S0266462308080252. [DOI] [PubMed] [Google Scholar]
- 83.Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, VenUS Team. VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers. Health Technol Assess. 2004;8:iii. 1-105. [DOI] [PubMed]
- 84.International Conference on Harmonisation (ICH) of Technical Requirements for the Registration of Pharmaceuticals for Human Use. Guidance E9: Statistical Principles for Clinical Trials. Rockville, MD: ICH; 1998.


