Abstract
We systematically reviewed the myofascial pain publications in the literature. The aim of this article is to review the methods of management and their outcome and factors associated with prognosis. The topics of interest in the diagnostic process are myofascial trigger points electromyography, jaw tracking, joint sound recorder, sonography, and vibratography, exclusion of other orofacial pain and temporomandibular disorders. Management modalities are occlusal therapy, physiotherapy, multidimensional rehabilitation antinociceptive therapy, anti-inflammatory and analgesics, muscle relaxants, stretch, and spray technique, transcutaneous electric nerve stimulation, and in severe cases botulinum toxin may be tried. The disease required interdisciplinary interaction in terms of occlusal therapy, antinociceptive therapy and physiotherapy because management of the disease may be influenced by the specialist primarily treating the patients.
Keywords: Fibromyalgia, myofascial pain, myofascial trigger points
INTRODUCTION
Bell presented the classification of temporomandibular disorders (TMD), Okeson[1] modified it. TMD include all functional disorders of the masticatory system which includes the masticatory musculature, the temporomandibular joints (TMJs) and the associated structures. Masticatory muscle disorder are protective co contraction, local muscle soreness, myofascial pain, myospasm, and centrally mediated myalgia, fibromyalgia.[2] Myofascial pain first described by Travell and Rinzler in 1952[3] as myofascial trigger point (MTrP) pain (trigger point myalgia). Laskin 1969[4] described myofascial pain dysfunction syndrome (term is broad and general) to denote any muscle disorder (not an intra capsular disorder) but it is not trigger point pain. Myofacial pain is a subtypes of fibromyalgia.[5] Han and Harrison 1997[6] described the differentiating features of myofascial pain syndrome (MPS) and fibromyalgia syndrome. Myofascial pain has been included in the tenth revision of International Statistical Classification of Diseases and Related Health problems (ICD-10) as a separate enitity M 79.1.[7] Myofascial pain may be localized or referred, with few localized trigger point and taut band, on contrary fibromyalgia is more generalized, without taut band and referred pain is less frequent. Poor sleep is more frequent with fibromyalgia.[8] Myofacial pain can also be classified as primary that are not related to other medical condition and secondary syndromes that is related with other medical condition. Primary MPSs includes myogenic headache: Chronic tension type and mixed tension-type/migraine headache, neck pain, shoulder pain, low back pain, piriformis syndrome, knee pain, ankle pain.[8] Secondary MPSs includes chronic cervical whiplash neck pain, TMJ dysfunction, secondary frozen shoulder: Impingement syndrome, rotator cuff tear, visceral pain syndromes: Nonangina chest pain, hepatic referred pain, renal/ureteral flank pain, structural anatomic variations: Scoliosis, pelvic torsions, leg length inequality, radicular pain, postlaminectomy syndrome, rheumatoid arthritis, osteoarthritis: Cervical and lumbar spondylosis, hip or shoulder osteoarthritis, Sjogren syndrome, fibromyalgia, acute trauma: Fractures, soft tissue injury, postoperative pain, hypothyroidism, chronic infection: Candidiasis, parasitic disease, Vitamin B12 deficiency. The aim of this article is to review the different treatment strategies along with etiologic and predisposing factors and their effect on treatment outcome.
MATERIALS AND METHODS
An extensive search of literature was performed on database such as MEDLINE, PubMed and Google Scholar using the keywords such as “myofascial”, “trigger points”, “myospasms”, “myofascial pain dysfunction syndrome”, “facial myalgia”, and “taut bands”. Information was also sought from related books and electronic data.
DISCUSSION
Complete etiology of MPS is complex and poorly understood. The pathophysiologic basis for the formation and persistence of taut band may be a matter of research. Predisposing factors are local factors, habits, posture, muscle strain, chilling, hypo vitaminosis of Vitamin C, Vitamin E, Vitamin B complex, decreased plasma folic acid, poor physical conditioning, fatigue, viral infections, idiopathic trigger point mechanism,[9] hyperuricaemia, increased creatinine level, oestrogen deficiency, mild iron deficiency, anaemia, and low potassium and calcium reserve, TMJ disorders, internal derangement, cervical osteoarthritis and disc disease mainly as result of reflex muscle splinting to protect the joint from aggravating movements. Some of these factors may create a vicious cycle and complement each other to propagate the disease.
Clinical history and examination is the gold standard in diagnosis of myofascial pain. There are great variations in the presentation of sign and symptoms among patients. Complete careful examination of musculoskeletal system, TMJ functions and disorders and dental diseases especially malocclusion, neurologic, posture, are required. Common signs of myofascial pain are MTrP (localized spot of tenderness in a nodule of palpable taut bands of contracted muscle). MTrPs may be of one of the two types: Active TrP (present in a taut band of muscle and on palpation it will give rise to jump sign) and latent TrP (nodular). It may be triggered by a change in diet or it may occur after surgery, or dental work, or after injury. It worsens with stress or may intensify with cold. It may be associated with bruxism, trauma from occlusion, and/or with jaw manipulation in any form. Pain from various MTrPs of facial region are being referred to maxillary and mandibular tooth, alveolar ridge, tongue, palate, temporal and frontal region, TMJ, Ear, pharynx, lateral surface of mandible and sometimes occiput. Other clinical features may be diffuse pain that is cyclic in nature frequently involving the head and neck area, referred pain, morning stiffness of facial muscles, local twitch response which usually improves with heat. History of emotional stress and disturbed sleep is often present.
On contrary joint related pain and dysfunction presents as a continuous or intermittent pain that is localized to the preauricular region, in and around the TMJ, and is exacerbated on jaw movements. Joint dysfunction is commonly due to mechanical interferences due to displaced disc often deformed in late stages of internal derangement. Such interferences produce the characteristic clicking sound of the TMJ. Internal derangement of TMJ may accompany the myofascial pain or vice versa. Crepitus or grating sound during jaw movements is pathognomic of temporomandibular osteoarthritis. Other diagnostic methods[10,11,12,13,14,15,16,17] like plain radiographs, computed tomography (CT) and magnetic resonance imaging (MRI) scans, electronic tests (jaw tracking, vibratography, sonography, and electromyography [EMG]) and clinical diagnostic indices (research diagnostic criteria by Dworkin and LeResche 1992[18]) can be supplemented as aids in diagnosis and research. Jaw tracking devices are machines used to study mandibular movements in patients who have craniomandibular disorders. The jaw movement parameters that are considered diagnostic include amplitude of jaw movement in all three planes of space, reproducibility or consistency of jaw movements, and velocity and smoothness of jaw trajectories. Reports have suggested that velocity of voluntary jaw movements are reduced in patients with these disorders. However, studies evaluating the reliability and accuracy of these devices have reported a high range of measurement errors. Hence studies suggest the claim of these devices having diagnostic value is not well supported by scientific evidence. EMG uses surface EMG of muscles of mastication to identify pathologic and dysfunctional conditions identified by abnormal activity of the masticatory muscles. However, investigators have opined that EMG studies cannot be taken at face value because (1) Of lack of experimental controls for age, sex, facial form, skin thickness, electrode positioning, history of bruxism or other parafunctional habits to compare the EMG findings. (2) Muscles of facial expression are a source of confounding signals when recording jaw muscles with surface electrodes. Sleep electroencephalogram (EEG) studies can be carried out in cases of suspicion of sleep disorders like obstructive sleep apnoea, behavior disorders, night bruxism etc., Sonography and vibratography may be tried to objectively measure the sound characteristics produced during jaw movements and to link these characteristic sounds to a specific pathologic state. The three pathologic states generally identified are disk displacement with reduction, disk displacement without reduction and degenerative joint disease. Studies have reported acceptable sensitivity however, the specificity is low producing many false positives. Radiological investigations (CT and MRI) are usually normal but concomitant presence of joint disturbances like internal derangement and osteoarthrosis can be ruled out using these modalities.
The natural course of myofascial pain is generally not progressive. The symptoms generally subsides over a period of time, may also recur due to the various predisposing factors that serve to maintain the disease. The main goal of management is to reduce or eliminate pain, increase mouth opening to normal and improve the quality of life. On the basis of history and clinical examination and specialized investigation, proper firm diagnosis should be made. For better and easy understanding of treatment rationale we have summarized the treatment options available in the literature into two phases and have presented an algorithm for myofascial pain management. phase I therapy includes patient education with the demonstration of an attitude of understanding and empathy. Psychological or psychiatric management should be incorporated to address the depression, anxiety, stress, poor coping skill as per the need of patient. Behavior modification through cognitive behavioral therapy should also be taken into account. Management includes physical therapy, occlusal therapy and drug therapy as mentioned in the algorithm. Refractory and unresponsive cases should be evaluated carefully from the point of view of exact cause and predisposing factors, concomitant internal derangement of TMJ and other joint diseases. Advanced diagnostics as well as opinions from the different specialties should be considered. In such cases phase II therapy may be instituted but with invariable response.
Phase I.
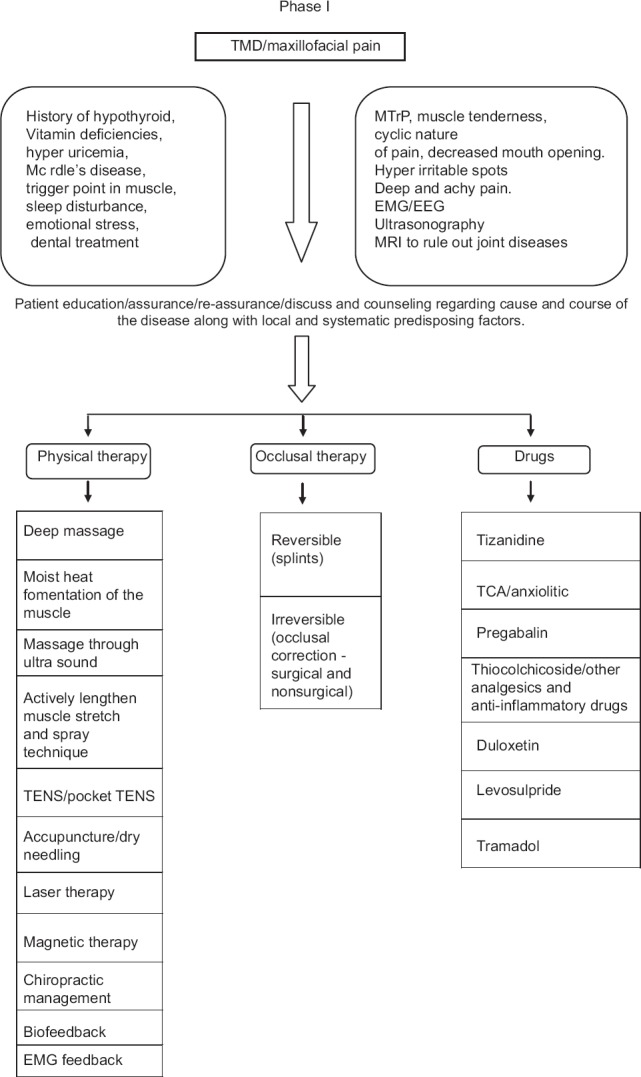
Algorithm for management of myofascial pain
Phase II.
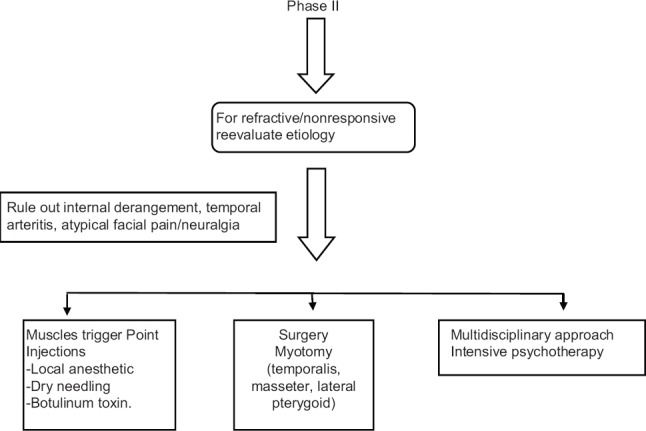
Algorithm for management of myofascial pain
Deep stroking massage is a safe and effective method applied directly to the TrP. Effectiveness of trigger point massage depends largely on ability to recognize referred pain and to trace it back to the trigger point that is causing it. TrPs are not usually at place of pain. Massage at wrong place can feel good but does not resolve the problem. Therapists should search for tenderness spots and deep stroking massage should be done with slow, rhythmic and repeated strokes in one direction. Performing a series of deep strokes across the trigger points will move the blood and and lymph fluid with accumulated waste product from the painful areas and also brings relief by activating release of painkilling endorphins.[19]
Ultrasound therapy using sound waves transmitting through sound conducting gel to the tissues leads to break down of scar tissue, relaxation of muscle and improvement in local circulation. We came across lots of research articles on use of ultra sound therapy for relieving myofascial pain. Some researchers claim that use of ultra sound in myofascial disorders is based on empirical experience and lacks firm evidence for concluding statistically significant pain improvement after ultrasound therapy.[20,21] While Majlesi and Unalan 2004[22] are in favor of use of high power ultrasound than conventional ultrasound for treating patients of acute myofascial pain. Ay et al. 2011[23] compared the effectiveness of phonophoresis using diclofenac gel and ultrasound alone in myofascial pain and conclude equal efficacy of both ultrasound and phonophoresis in reducing pain.
Transcutaneous electric nerve stimulation involves application of electrodes connected to a small battery-powered unit along the painful muscle and is a form of electroanalgesia. A low level of electrical stimulation is applied to relieve muscle tension and pain. The mechanism of the analgesia produced by TENS is explained by the gate control theory proposed by Melzack and Wall in 1965.[24] Graff-Radford et al. 1989[25] studied the effect of TENS on myofascial pain and trigger point sensitivity and observed pain reduction occurs with 100 hz, 250 ms stimulation followed by 100 hz, 50 ms. No pain reduction found in 2 hz, 250 ms. They suggested that high frequency, high intensity TENS is effective in reducing myofascial pain without having any effect on local trigger point sensitivity. Marchand et al. 1993[26] found that TENS was efficient in reducing pain intensity but not pain unpleasantness. TENS also produced a significant additive effect over repetitive treatment sessions.
Application of low level laser therapy (LLLT) has been sought in various musculoskeletal and soft tissue pain syndromes.[27] LLLT uses red and infrared light for the relief of pain, to accelerate healing and decrease inflammation. When the light source is placed against the skin, the photons penetrate several centimeters and get absorbed by the mitochondria, the energy producing part of a cell. This facilitates tissue repair and accelerates wound and tissue healing. The low intensity laser therapy is noninvasive, nontoxic and often provides a treatment alternative for patients that have not responded to other therapies. LLLT is also indicated as a noninvasive painless therapy for myofascial pain.[27] According to Ozdemir et al.[28] Laser irradiation provides analgesia by decreasing the spasm in muscle arterioles leading to increase in tissue oxygenation and active TP formation resulting into restoration of metabolic rate of the tissues with diminished energy levels. Effects on endorphin levels and gate control of pain are two another mechanisms that may cause analgesia by laser radiation as hypothesized by Ozdemir et al. By all these mechanisms it can interrupt the vicious cycle of the trigger point.[28] Simunovic[29] suggested increase in oxygen supply to hypoxic cells in trigger point areas by regulation of micro-circulation following LLLT and has reported functional recovery and decrease of spontaneous pain with LLLT on trigger points, in a study on 243 patients. Another study by Snyder-Mackler et al.[30] found an increase in skin resistance after laser therapy and suggested that effectivness was sympathetically mediated. Gur et al.[31] evaluated the efficacy of 904 nm gallium arsenide LLLT in management of chronic myofascial pain in neck and improvement in quality of life and concluded that short period application of LLLT is effective in pain relief and improves the functional ability and quality of life in patients with myofascial pain.
Biofeedback is a method of providing training to the patients to control certain involuntary bodily functions with ability to manipulate them at will such as heart rate, blood pressure, muscle tension, pain perception and skin temperature which help in providing greater control over pain and ultimately improving quality of life.[32] The three most commonly used forms of biofeedback therapy are: EMG: Which measures muscle tension; thermal biofeedback: Which measures skin temperature; neurofeedback or EEG: Which measures brain wave activity. Dalen et al. 1986[33] studied the effect of EMG biofeedback on frontalis and masseter muscle activity in the treatment of myofascial pain and concluded that biofeedback training facilitated muscular relaxation and self-regulation. Turk et al.[34] compared the effect of intraoral appliance and biofeedback for pain management in 80 patients with TMD. They found intraoral appliance to be more effective than the biofeedback treatment in reducing pain initially after treatment, but at a 6-month follow-up the intraoral appliance group significantly relapsed, especially in depression, whereas patients on biofeedback therapy maintained improvements on both pain and depression and continued to improve. They also found combined treatment approach was more effective than either of the single treatments alone.
A form of alternative medicine, namely chiropractic, is a low-tech, noninvasive technique which mainly involves mobilization, manipulation of trigger points, cryotherapy, exercises and health and lifestyle counseling. Ischemic compression is the most popular technique practiced by chiropractors. This approach is also known as Pennel's technique, Nimmo technique, trigger point therapy or acupressure. It has been used by chiropractors and other manual therapists from past four decades.[35] Although we found limited literature on its use in facial region but significant improvement in chronic cervical pain syndromes, MPS and in management of MTrPs has been seen in various studies.[36,37,38] A positive role of chiropractic care has also been demonstrated in a worsening head and neck pain in a 68-year-old female patient, resulting into improvement in quality of life.[39]
Aim of occlusal splint therapy is to establish neuromuscular harmony in the masticatory system by creating a mechanical disadvantage for parafunctional forces with removable appliances.[40] Occlusal splints allow relaxation of masticatory muscles, protect the teeth and jaws from the adverse effects of bruxism, and normalize periodontal ligament proprioception. Occlusal splints also allow repositioning of the condyles and jaws into centric relation.[40] Even small occlusal interferences can cause changes in muscle activity coordination.[41] Occlusal splints promote muscle relaxation by providing a platform for the teeth that allows for equal distribution of tooth contacts, immediate posterior tooth disclusion in all movements (with anterior guidance), and reduced stress on the joint. Neuromuscular harmony that follows provides for optimal function and comfort. Different types of splints used in occlusal splint therapy include permissive, nonpermissive, hydrostatic, and soft rubber (silicone) splints. The type of splint utilized is dependent on the diagnosis.
In myofacial pain identification of the etiology that causes the activation of trigger points is important from the point of view of treatment. The localized pain in the muscle is due to accumulation of lactic acid, serotonin, histamine, kinins, and prostaglandins due to long standing muscle contraction. This accumulation of chemicals leads to the increased motor or sympathetic activity and in turn leads to the increased pain. Trigger point injections includes normal saline, local anesthesia and botulinum toxin A may be given.[42,43,44,45] Trigger point injection disrupt the trigger point mechanically as well as chemically resulting in relaxation and legthening of muscle fiber. Injected solution may cause vasodilation of the area, dilution of the chemicals which are deposited in the muscle and removal of the accumulated chemicals through diffusion. But there is no strong evidence in favor of trigger point injection and ultrasonic guided trigger point injections are seem to be more effective and efficacy of peripheral nerve block is yet to be need more exploration.
As myofacial pain commonly result of clinical states like increased muscle tension, muscle spasm, spasticity and trigger point formation therefore the role of muscle relaxants in relieving pain is found to be beneficial and repeatedly being investigated. Tizanidine is the one most frequently used centrally acting muscle relaxant having alpha-2-adrenergic agonist properties, which decrease the muscle spasm, and is thought to prevent release of excitatory amino acids by suppressing polysynaptic excitation of spinal cord interneurons. Tizanidine should be administered initially at bed time owing to its sedative effect with gradual dose increment from an initial dose of 2 to 4 mg at bedtime up to the maximum of 8 mg 3 times/day. The bedtime dose can provide an analgesic effect as well as improve quality of sleep. Malanga et al.[46] studied the effect of tizanidine in treatment of myofascial pain in 29 patients. Subjects were titrated up to 12 mg of tizanidine over 3 weeks and maintained for 2 weeks. Pain intensity and disability decreased significantly (P < 0.001) with improvement in pressure threshold and sleep quality and suggested it to be used as first line drug for myofascial pain. Commonly reported side effects are daytime drowsiness, hypotension, weakness, and dry mouth. Less commonly reported side effects of tizanidine are palpitations, bradycardia, dizziness, headache, nausea, elevated liver enzymes. Liver function enzymes are recommended to be monitored closely during the treatment. Thiocolchicoside is another agent that functions as an anti-inflammatory and analgesic, as well as a muscle relaxant. It exhibits selective affinity for the inhibitory gamma-aminobutyric acid and glycinergic receptors. It has an agonistic action at the spinal-strychnine-sensitive receptors that could mediate its myorelaxant effect.[47] In a single blind phase IV clinical study on the efficacy of topical thiocolchicoside in the treatment of myofascial pain, it was found that ointment form may be a good alternative, particularly in patients who cannot receive injections.[48]
Since stress and psychiatric disorders are one of the factors predisposing to myofascial pain therefore antidepressant medications has been considered for pain control in such patients. It has also been seen that patients of myofascial pain frequently suffered from sleep disturbance. Studies have shown a reciprocal relationship between sleep disturbance and pain. Hence tricyclic antidepressants (TCA's) are also group of drugs included by many clinicians in the prescription given to patients of myofascial pain. TCA's have a more predictably positive effect on sleep continuity and slow-wave sleep than do the popular selective serotonin reuptake inhibitors. One more reason suggested in favor of antidepressant drugs is that there is evidence of antidepressant analgesia independent of their effects on depression.[49] Although exact mechanism of pain relief is not known but it has been suggested that TCAs work on central serotonergic and noradrenergic signals, which affect central pain pathways.[50] We found a literature in which study was done, on 33 nondepressed patients having chronic tension-type headache, to investigate whether the analgesic effect of amitriptyline (TCA) is caused by a reduction of muscle pain or by a general reduction of pain sensitivity.[50] In the study it was found that amitriptyline elicits its analgesic effect in chronic myofascial pain by reducing the transmission of painful stimuli from myofascial tissues rather than by reducing overall pain sensitivity. They suggested that this effect was caused by a segmental reduction of central sensitization in combination with a peripheral antinociceptive action.[51] Certain adverse effects of TCA's that should be given consideration during treatment include anticholinergic effects, such as dizziness, orthostatic hypotension, sedation, and problems with micturition. Higher doses are associated with an increased risk of sudden death owing to cardiac arrhythmias; a 75 mg daily dose of amitriptyline is generally accepted as “cardio-safe”.[52]
Individualized treatment is required for the treatment of MPS. Initial focus is on analgesics and anti-inflammatory, physiotherapy, occlusal therapy, TENS, deep massage, laser therapy, acupuncture, biofeedback. Recurrent and refractory cases should be properly reevaluated from the point of view of etiology, organic and psychogenic cause, internal derangement of TMJ and should be managed accordingly. Vicious cycle of pain should be interrupted with the judicious use of analgesics, anti-inflammatory, sedatives and antidepressants/TENS. Botox therapy may be considered. Physical exercises along with yoga and pranayam may also be tried.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Okeson JP. 6th ed. Mosby, Inc; 2008. Management of Temporomandibular Disorders and Occlusion. [Google Scholar]
- 2.Costen JB. A syndrome of ear and sinus symptoms based on disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol. 1934;43:1–15. doi: 10.1177/000348949710601002. [DOI] [PubMed] [Google Scholar]
- 3.Travell JG, Rinzler SH. The myofascial genesis of pain. Postgrad Med. 1952;11:425–34. doi: 10.1080/00325481.1952.11694280. [DOI] [PubMed] [Google Scholar]
- 4.Laskin DN. Etiology of the pain dysfunction syndrome. J Am Dent Assoc. 1969;79:147–53. doi: 10.14219/jada.archive.1969.0234. [DOI] [PubMed] [Google Scholar]
- 5.Gray RJ, Davies SJ, Quayle AA. A clinical approach to temporomandibular disorders 1. Classification and functional anatomy. Br Dent J. 1994;176:429–35. doi: 10.1038/sj.bdj.4808473. [DOI] [PubMed] [Google Scholar]
- 6.Han SC, Harrison P. Myofascial pain syndrome and trigger-point management. Reg Anesth. 1997;22:89–101. doi: 10.1016/s1098-7339(06)80062-3. [DOI] [PubMed] [Google Scholar]
- 7.ICD version 2007: World Health Organization Online Resource. Available from: http://apps.who.int/classifications/apps/icd/icd10online/
- 8.Turk DC. Psychosocial and behavioral assessment of patients with temporomandibular disorders: Diagnostic and treatment implications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:65–71. doi: 10.1016/s1079-2104(97)90093-7. [DOI] [PubMed] [Google Scholar]
- 9.Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: Towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9:613–33. doi: 10.1016/j.ejpain.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Laskin DM, Greene CS, Hylander WL. Chicago, IL: Quintessence Pub; 2006. Temporomandibular Disorders: An Evidence-Based Approach to Diagnosis and Treatment; p. xii. 548. [Google Scholar]
- 11.Lund JP, Widmer CG, Feine JS. Validity of diagnostic and monitoring tests used for temporomandibular disorders. J Dent Res. 1995;74:1133–43. doi: 10.1177/00220345950740041501. [DOI] [PubMed] [Google Scholar]
- 12.Mohl ND, Lund JP, Widmer CG, McCall WD., Jr Devices for the diagnosis and treatment of temporomandibular disorders. Part II: Electromyography and sonography. J Prosthet Dent. 1990;63:332–6. doi: 10.1016/0022-3913(90)90207-s. [DOI] [PubMed] [Google Scholar]
- 13.Mohl ND, McCall WD, Jr, Lund JP, Plesh O. Devices for the diagnosis and treatment of temporomandibular disorders. Part I: Introduction, scientific evidence, and jaw tracking. J Prosthet Dent. 1990;63:198–201. doi: 10.1016/0022-3913(90)90106-m. [DOI] [PubMed] [Google Scholar]
- 14.Mohl ND, Ohrbach RK, Crow HC, Gross AJ. Devices for the diagnosis and treatment of temporomandibular disorders. Part III: Thermography, ultrasound, electrical stimulation, and electromyographic biofeedback. J Prosthet Dent. 1990;63:472–7. doi: 10.1016/0022-3913(90)90240-d. [DOI] [PubMed] [Google Scholar]
- 15.Lund JP, Lavigne G, Feine JS, Goulet JP, Chaytor DV, Sessle BJ, et al. The use of electronic devices in the diagnosis and treatment of temporomandibular disorders. J Can Dent Assoc. 1989;55:749–50. [PubMed] [Google Scholar]
- 16.Eversole LR, Machado L. Temporomandibular joint internal derangements and associated neuromuscular disorders. J Am Dent Assoc. 1985;110:69–79. doi: 10.14219/jada.archive.1985.0283. [DOI] [PubMed] [Google Scholar]
- 17.Laskin DM, Block S. Diagnosis and treatment of myofacial pain-dysfunction (MPD) syndrome. J Prosthet Dent. 1986;56:75–84. doi: 10.1016/0022-3913(86)90287-8. [DOI] [PubMed] [Google Scholar]
- 18.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–55. [PubMed] [Google Scholar]
- 19.Davies C. 2nd ed. Oakland, California: Published by New Harbinger Publication Inc; 2004. The Trigger Point Therapy Workbook; pp. 47–74. [Google Scholar]
- 20.Gam AN, Johannsen F. Ultrasound therapy in musculoskeletal disorders: A meta-analysis. Pain. 1995;63:85–91. doi: 10.1016/0304-3959(95)00018-N. [DOI] [PubMed] [Google Scholar]
- 21.Gam AN, Warming S, Larsen LH, Jensen B, Høydalsmo O, Allon I, et al. Treatment of myofascial trigger-points with ultrasound combined with massage and exercise – a randomised controlled trial. Pain. 1998;77:73–9. doi: 10.1016/S0304-3959(98)00084-0. [DOI] [PubMed] [Google Scholar]
- 22.Majlesi J, Unalan H. High-power pain threshold ultrasound technique in the treatment of active myofascial trigger points: A randomized, double-blind, case-control study. Arch Phys Med Rehabil. 2004;85:833–6. doi: 10.1016/j.apmr.2003.07.023. [DOI] [PubMed] [Google Scholar]
- 23.Ay S, Dogan SK, Evcik D, Baser OC. Comparison the efficacy of phonophoresis and ultrasound therapy in myofascial pain syndrome. Rheumatol Int. 2011;31:1203–8. doi: 10.1007/s00296-010-1419-0. [DOI] [PubMed] [Google Scholar]
- 24.Melzack R, Wall PD. Pain mechanisms: A new theory. Science. 1965;150:971–9. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 25.Graff-Radford SB, Reeves JL, Baker RL, Chiu D. Effects of transcutaneous electrical nerve stimulation on myofascial pain and trigger point sensitivity. Pain. 1989;37:1–5. doi: 10.1016/0304-3959(89)90146-2. [DOI] [PubMed] [Google Scholar]
- 26.Marchand S, Charest J, Li J, Chenard JR, Lavignolle B, Laurencelle L. Is TENS purely a placebo effect? A controlled study on chronic low back pain. Pain. 1993;54:99–106. doi: 10.1016/0304-3959(93)90104-W. [DOI] [PubMed] [Google Scholar]
- 27.Beckerman H, de Bie RA, Bouter LM, De Cuyper HJ, Oostendorp RA. The efficacy of laser therapy for musculoskeletal and skin disorders: A criteria-based meta-analysis of randomized clinical trials. Phys Ther. 1992;72:483–91. doi: 10.1093/ptj/72.7.483. [DOI] [PubMed] [Google Scholar]
- 28.Ozdemir F, Birtane M, Kokino S. The clinical efficacy of low-power laser therapy on pain and function in cervical osteoarthritis. Clin Rheumatol. 2001;20:181–4. doi: 10.1007/s100670170061. [DOI] [PubMed] [Google Scholar]
- 29.Simunovic Z. Low level laser therapy with trigger points technique: A clinical study on 243 patients. J Clin Laser Med Surg. 1996;14:163–7. doi: 10.1089/clm.1996.14.163. [DOI] [PubMed] [Google Scholar]
- 30.Snyder-Mackler L, Barry AJ, Perkins AI, Soucek MD. Effects of helium-neon laser irradiation on skin resistance and pain in patients with trigger points in the neck or back. Phys Ther. 1989;69:336–41. doi: 10.1093/ptj/69.5.336. [DOI] [PubMed] [Google Scholar]
- 31.Gur A, Sarac AJ, Cevik R, Altindag O, Sarac S. Efficacy of 904 nm gallium arsenide low level laser therapy in the management of chronic myofascial pain in the neck: A double-blind and randomize-controlled trial. Lasers Surg Med. 2004;35:229–35. doi: 10.1002/lsm.20082. [DOI] [PubMed] [Google Scholar]
- 32.deCharms RC, Maeda F, Glover GH, Ludlow D, Pauly JM, Soneji D, et al. Control over brain activation and pain learned by using real-time functional MRI. Proc Natl Acad Sci U S A. 2005;102:18626–31. doi: 10.1073/pnas.0505210102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dalen K, Ellertsen B, Espelid I, Grønningsaeter AG. EMG feedback in the treatment of myofascial pain dysfunction syndrome. Acta Odontol Scand. 1986;44:279–84. doi: 10.3109/00016358609004734. [DOI] [PubMed] [Google Scholar]
- 34.Turk DC, Zaki HS, Rudy TE. Effects of intraoral appliance and biofeedback/stress management alone and in combination in treating pain and depression in patients with temporomandibular disorders. J Prosthet Dent. 1993;70:158–64. doi: 10.1016/0022-3913(93)90012-d. [DOI] [PubMed] [Google Scholar]
- 35.Chapman-Smith DA, Cleveland CS., 3rd . International status, standards, and education of the chiropractic profession. In: Haldeman S, Dagenais S, Budgell B, et al., editors. Principles and Practice of Chiropractic. 3rd ed. New York: McGraw-Hill; 2005. pp. 111–34. [Google Scholar]
- 36.Missaghi B. Sternocleidomastoid syndrome: A case study. J Can Chiropr Assoc. 2004;48:201–5. [PMC free article] [PubMed] [Google Scholar]
- 37.Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: A systematic review of the literature. J Manipulative Physiol Ther. 2009;32:14–24. doi: 10.1016/j.jmpt.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 38.Schroeder J, Kaplan L, Fischer DJ, Skelly AC. The outcomes of manipulation or mobilization therapy compared with physical therapy or exercise for neck pain: A systematic review. Evid Based Spine Care J. 2013;4:30–41. doi: 10.1055/s-0033-1341605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodine RJ, Aker P. Trigeminal neuralgia and chiropractic care: A case report. J Can Chiropr Assoc. 2010;54:177–86. [PMC free article] [PubMed] [Google Scholar]
- 40.Dylina TJ. A common-sense approach to splint therapy. J Prosthet Dent. 2001;86:539–45. doi: 10.1067/mpr.2001.118878. [DOI] [PubMed] [Google Scholar]
- 41.Bakke M, Møller E. Distortion of maximal elevator activity by unilateral premature tooth contact. Scand J Dent Res. 1980;88:67–75. doi: 10.1111/j.1600-0722.1980.tb00722.x. [DOI] [PubMed] [Google Scholar]
- 42.Wong CS, Wong SH. A new look at trigger point injections. Anesthesiol Res Pract 2012. 2012 doi: 10.1155/2012/492452. 492452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hong CZ, Hsueh TC. Difference in pain relief after trigger point injections in myofascial pain patients with and without fibromyalgia. Arch Phys Med Rehabil. 1996;77:1161–6. doi: 10.1016/s0003-9993(96)90141-0. [DOI] [PubMed] [Google Scholar]
- 44.Ferrante FM, Bearn L, Rothrock R, King L. Evidence against trigger point injection technique for the treatment of cervicothoracic myofascial pain with botulinum toxin type A. Anesthesiology. 2005;103:377–83. doi: 10.1097/00000542-200508000-00021. [DOI] [PubMed] [Google Scholar]
- 45.Zhou JY, Wang D. An update on botulinum toxin A injections of trigger points for myofascial pain. Curr Pain Headache Rep. 2014;18:386. doi: 10.1007/s11916-013-0386-z. [DOI] [PubMed] [Google Scholar]
- 46.Malanga GA, Gwynn MW, Smith R, Miller D. Tizanidine is effective in the treatment of myofascial pain syndrome. Pain Physician. 2002;5:422–32. [PubMed] [Google Scholar]
- 47.Carta M, Murru L, Botta P, Talani G, Sechi G, De Riu P, et al. The muscle relaxant thiocolchicoside is an antagonist of GABAA receptor function in the central nervous system. Neuropharmacology. 2006;51:805–15. doi: 10.1016/j.neuropharm.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 48.Ketenci A, Basat H, Esmaeilzadeh S. The efficacy of topical thiocolchicoside (Muscoril) in the treatment of acute cervical myofascial pain syndrome: A single-blind, randomized, prospective, phase IV clinical study. Agri. 2009;21:95–103. [PubMed] [Google Scholar]
- 49.Sullivan MD, Robinson JP. Antidepressant and anticonvulsant medication for chronic pain. Phys Med Rehabil Clin N Am. 2006;17:381–400. doi: 10.1016/j.pmr.2005.12.006. vi. [DOI] [PubMed] [Google Scholar]
- 50.Botney M, Fields HL. Amitriptyline potentiates morphine analgesia by a direct action on the central nervous system. Ann Neurol. 1983;13:160–4. doi: 10.1002/ana.410130209. [DOI] [PubMed] [Google Scholar]
- 51.Bendtsen L, Jensen R. Amitriptyline reduces myofascial tenderness in patients with chronic tension-type headache. Cephalalgia. 2000;20:603–10. doi: 10.1046/j.1468-2982.2000.00087.x. [DOI] [PubMed] [Google Scholar]
- 52.Sindrup SH, Otto M, Finnerup NB, Jensen TS. Antidepressants in the treatment of neuropathic pain. Basic Clin Pharmacol Toxicol. 2005;96:399–409. doi: 10.1111/j.1742-7843.2005.pto_96696601.x. [DOI] [PubMed] [Google Scholar]


