Abstract
Context:
This article presents an original research conducted at Government Dental College, PGIDS, Rohtak.
Aims:
(1) To evaluate the marginal bone level changes around dental implants based on the radiological examination. (2) To evaluate the relationship of various parameters, i.e., gender, implant length, implant diameter and location of implants on the amount of bone loss around dental implants.
Materials and Methods:
An in-vivo study was undertaken to evaluate the crestal bone loss on mesial and distal aspect of implants, using standardized intra-oral periapical at the end of 6 months after placing the implants, but before prosthetically loading it.
Statistical Analysis Used:
Student's unpaired t-test.
Results:
Bone loss was measured and values were recorded immediately after implant placement and after 6 months.
Conclusions:
(1) Bone loss on mesial and distal aspects of implants was found to be same after period of 6 months. (2) Bone loss was found to be same in both 13 mm and 10 mm implants on mesial aspect, whereas on distal aspect, it was more in 10 mm implants. (3) Bone loss was found to be same in both 3.5 mm and 4.3 mm diameter implants on both mesial and distal aspects of implants. (4) Bone loss was found to be same in both maxilla and mandible on both mesial and distal aspects of implants. (5) Bone loss was found to be more in females on both mesial as well as distal aspects of implants.
Keywords: Bone loss, distal, implant, mesial
INTRODUCTION
The success of implants is dependent on meticulous pre-operative treatment planning as well as careful follow-up during the healing phase to evaluate the success of osseointegration.[1,2] Numerous studies have been conducted to establish the criteria for success and failure of osseointegration and hence for the success and failure of dental implants. Standardized periapical radiographs at regular follow-up intervals are used to detect peri-fixtural radiolucency and/or progressive marginal bone loss or “saucerization”.[3] If more than half of the bone around the implant is lost, that implant is considered to have failed.[4] Thus, the success of implant depends directly on crestal bone resorption and it is one of the major determinant factors for the post-operative success of implants.[5] According to the established criteria for the assessment of implant survival and success, marginal bone level change in 1st year should be less than 1.5 mm.[6] Smith and Zarb[7] suggested that one of the criteria for implant success was less than 0.2 mm of alveolar bone loss per year after the 1st year. However, the most active phase of bone loss during the first few months has not been studied extensively. Since bone level maintenance is one of the most important factors to be considered in implant prosthodontics, the post-operative evaluation of this bone is thus of great importance to a prosthodontist.
Aims and objectives
To evaluate the marginal bone level changes around dental implants based on radiological examination
To evaluate the relationship of various parameters, i.e., gender, implant length, implant diameter and location of implants on the amount of bone loss around dental implants and hence the success of osseointegration and thus the dental implants.
MATERIALS AND METHODS
An in-vivo study was undertaken to evaluate the crestal bone loss on the mesial and distal aspect of implants, using standardized intra-oral periapical (IOPA) radiographs at the end of 6 months after placing the implants, but before prosthetically loading it.
A total of 16 implants were placed in patients reporting to the out-patient Department of Prosthodontics and Crown and Bridge, Government Dental College, Pt. B.D. Sharma University of Health Sciences, Rohtak based on the inclusion and the exclusion criteria.
Inclusion criteria
Subjects requiring replacement of missing teeth
Patient with good oral hygiene
Adequate bone volume to accommodate an implant of appropriate dimension
Co-operative patient, willing for the surgery and proper follow-up.
Exclusion criteria
Medically compromised patients where surgery is contraindicated
Patient with poor oral hygiene
Insufficient bone quantity
Patients having any parafunctional habit
Patients suffering from periodontal diseases
Patients with history of alcohol, drug dependency, smoking and poor health.
Study was divided into following groups based on the four parameters, i.e., implant length, implant diameter, implant location and gender.
-
Based on implant length
- Group-1 (13 mm)
- Group-2 (10 mm).
-
Based on implant diameter
- Group-1 (3.5 mm)
- Group-2 (4.3 mm).
-
Based on implant location
- Group-1 (maxilla)
- Group-2 (mandible).
-
Based on gender
- Group-1 (male)
- Group-2 (female).
Detailed medical and dental history of each patient was taken. After an explanation of the proposed study criteria, including alternate treatment, potential risks and benefits, the participants were asked to sign an informed consent. Edentulous area, selected for implant placement was evaluated clinically for bucco-lingual and mesio-distal width, any undercuts, width of attached gingiva [Figures 1 and 2].
Figure 1.

Pre-operative intra-oral view in occlusion (missing 11)
Figure 2.

Pre-operative intra-oral view (missing 11)
All vital signs were checked and a complete hemogram was done to evaluate the fitness of the patient for implant placement. Complete oral prophylaxis was done before the implant placement. Pre-operative IOPA and orthopantomogram (OPG) [Figures 3 and 4] provided the necessary information regarding the available bone and distance of vital structures, i.e., maxillary sinus, floor of nasal cavity, mandibular canal from the implant site. A pre-measured 5 mm diameter ball bearing was used to calculate the magnification of OPG.
Figure 3.

Pre-operative intra-oral periapical
Figure 4.

Pre-operative orthopantomogram with 5 mm diameter ball bearing
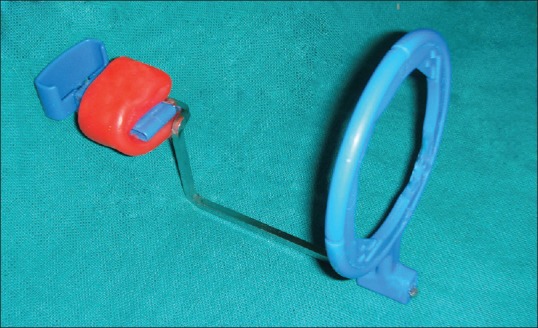
An assessment of the bone quantity at the implant site was done with the help of intra-oral periapical radiographs obtained by the long cone paralleling technique to minimize the distortion using the film holders (Rinn XCP, Dentsply) [Figures 5 and 6].
Figure 5.
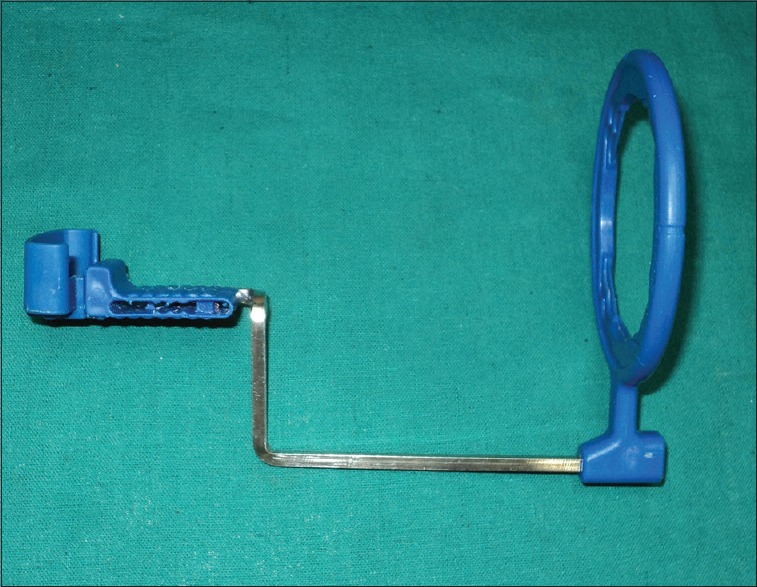
Rinn XCP film holder, Dentsply (for anterior teeth)
Figure 6.
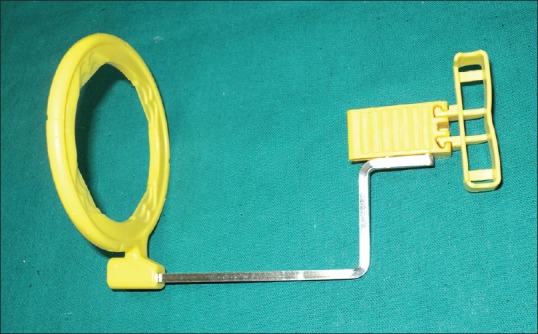
Rinn XCP film holder, Dentsply (for posterior teeth)
A customized occlusal bite jig was fabricated by attaching softened modeling wax to a film holder (Rinn XCP, Dentsply) and asking the patient to bite on this [Figures 7-10]. This jig was used for taking the standardized IOPA radiographs [Figure 11]. The jig was acrylized in heat cure acrylic and saved for use at all visits to standardize the film placement and cone angulation [Figure 12].
Figure 7.
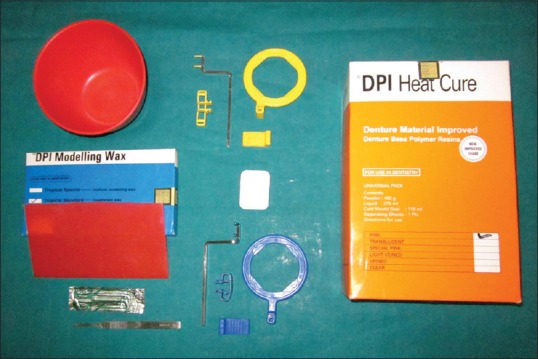
Basic armamentarium used in fabrication of custom-occlusal jig
Figure 10.
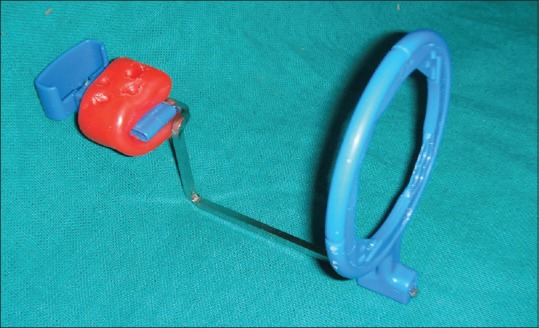
Customized occlusal bite jig
Figure 11.

Taking radiograph using customized occlusal bite jig and Rinn XCP film holder
Figure 12.

Customized occlusal bite jig acrylized in heat-cure acrylic
Figure 8.
Softened modeling wax attached to Rinn XCP film holder, Dentsply, for making customized occlusal bite jig
Figure 9.

Fabrication of customized occlusal bite jig for obtaining standardized intra-oral periapical radiographs using Rinn XCP film holder (Dentsply)
Ridge analysis was done clinically and from the prepared cast. In addition, OPG and IOPA were used to assess the height and width of the edentulous site. On the basis of clinical and radiographic findings, the implant size was selected.
Crestal incision was given for full thickness flap reflection, to expose the implant site. After marking the implant site by surgical stent, pilot drill was used, followed by twist drill, 2-caliber and final drill up to the decided depth. The implants were inserted first by using finger key, followed by cardanic ratchet key. The implants were placed at the level of alveolar crest. A cover screw was placed to close the opened implant site. The flap was closed with tight sutures to achieve water-tight closure. The patient was prescribed antibiotics and analgesics for 1 week, post-operatively.
The radiographic evaluation was performed at 0 month (immediately after the implant placement) [Figure 13] and at 6 months after the implant placement [Figure 14]. The standardized periapical radiographs obtained at 0 month and at 6 months were digitized using a computerized scanner at 600 dpi, 256 gray scales and then analyzed using UTHSCSA Image Tool (version 3.00 for Windows, University of Texas Health Science Center in San Antonio, TX, USA) which is designed to measure the distances in digital images [Figure 15]. The known implant length was used to calibrate the images in the computer software.
Figure 13.
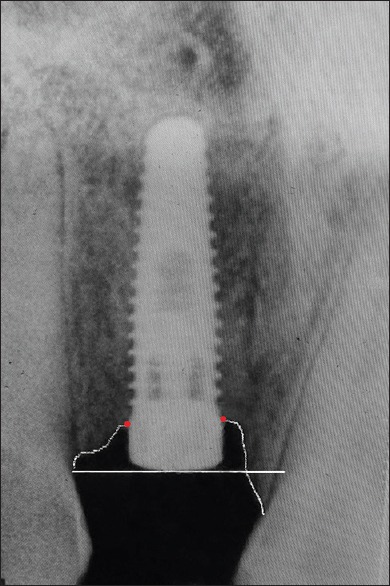
Intra-oral periapical radiograph (at 0 month)
Figure 14.
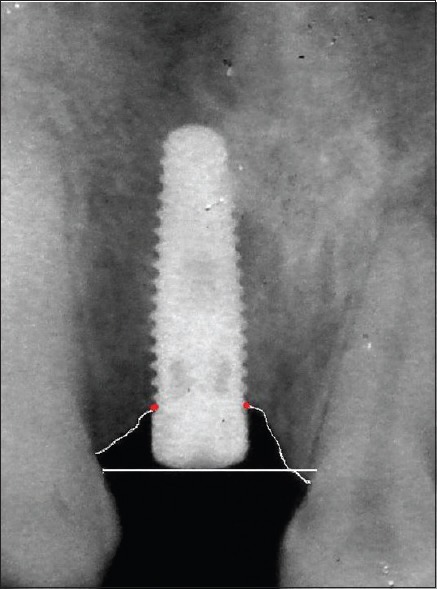
Intra-oral periapical radiograph (at 6 months)
Figure 15.
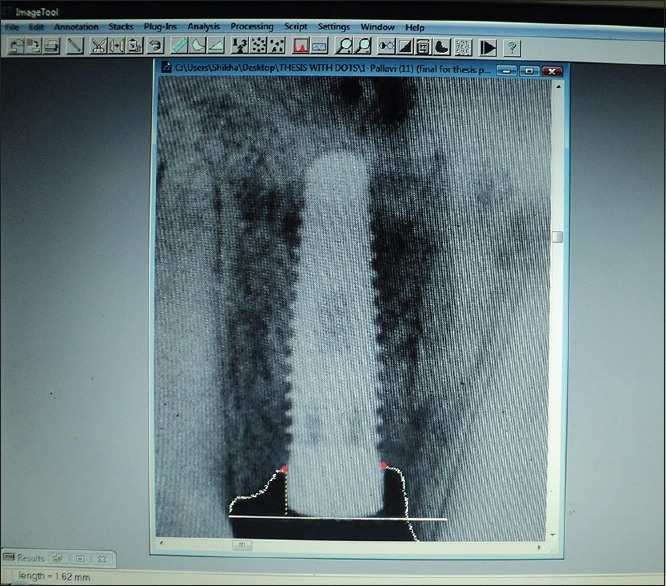
Measurement of marginal bone level from the reference line using UTHSCSA Image Tool (Version 3.00 for Windows, University of Texas Health Science Centre in San Antonio, TX, USA)
The coronal surface of the implant was taken as the reference line from which 2 perpendicular lines were dropped on the mesial and distal aspect of the implants to the first bone-to-implant contact [Figure 15]. Comparative measurements of mesial and distal crestal bone levels adjacent to implants were made to the nearest 0.1 mm. A minimum of 3 readings were made for each case and the average values were used to calculate the amount of crestal bone loss. Subtracting the bone level at 0 month from the bone level at 6 months gave the bone loss.
The results obtained were subjected to statistical analysis using Student's unpaired t-test.
RESULTS
Table 1 shows the basic details of the various parameters used in the study.
Table 1.
Basic details of the various parameters
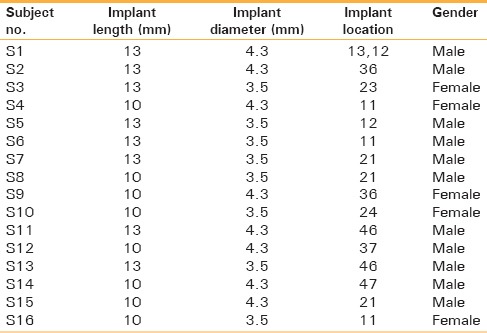
Table 2 shows the bone level measurements at 0 month and 6 months on mesial and distal aspect of implant and the calculation of bone loss.
Table 2.
Bone level measurements at 0 month and 6 months on mesial and distal aspect of implant and the calculation of bone loss
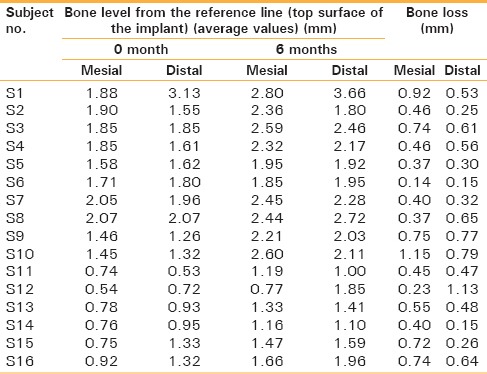
Table 3 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months. The mean bone loss on mesial aspect of implants was 0.5531 mm and on distal aspect of implants was 0.5037 mm. The P value for both mesial and distal aspect of implant was found to be statistically non-significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss on mesial and distal aspect of implant was found to be same.
Table 3.
Mean and standard deviation of bone loss on mesial and distal after 6 months
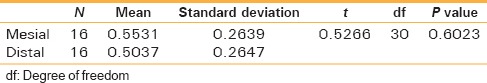
Tables 4-7 show the bone level measurements for implant length, implant diameter, implant location and gender respectively.
Table 4.
Bone level measurements for parameter-1 (implant length)
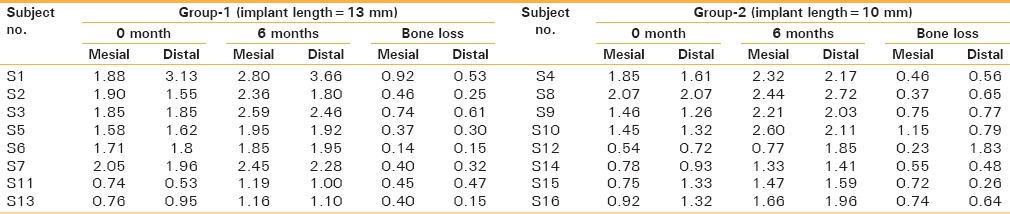
Table 7.
Bone level measurements for parameter-4 (gender)
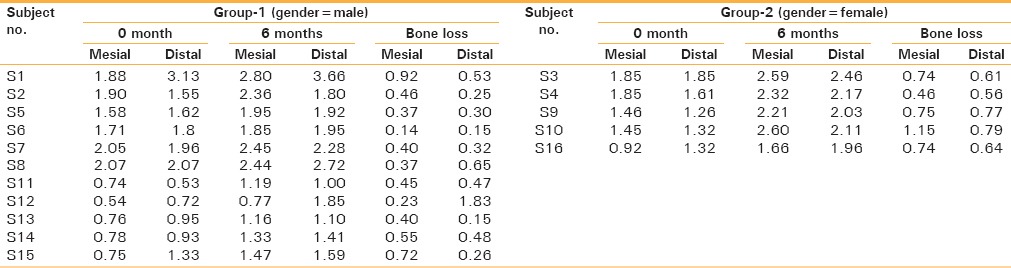
Table 5.
Bone level measurements for parameter-2 (implant diameter)
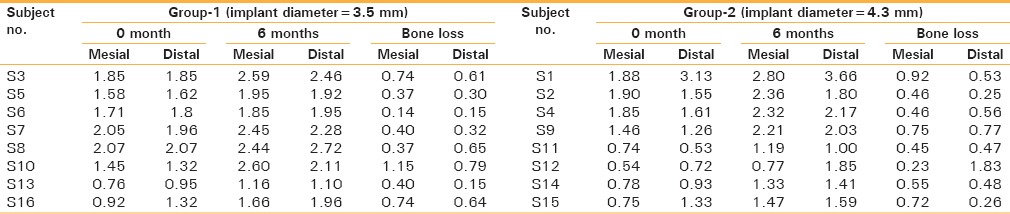
Table 6.
Bone level measurements for parameter-3 (implant location)
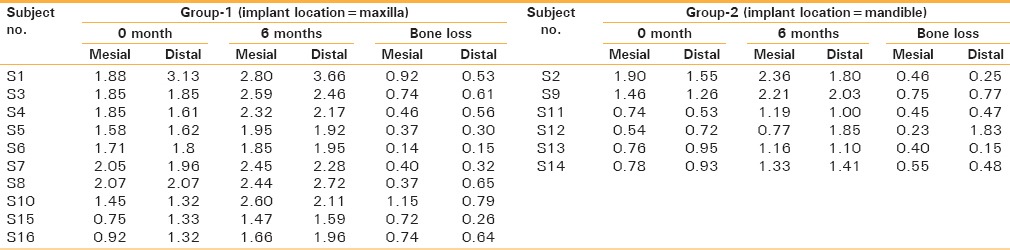
Table 8 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for 13 mm implants verses 10 mm implants. The mean bone loss on mesial aspect of implants was 0.485 mm for 13 mm implants and 0.6212 mm for 10 mm implants. Whereas the mean bone loss on distal aspect of implants was 0.3475 mm for 13 mm implants and 0.66 mm for 10 mm implants. The P value for mesial aspect of implant was found to be statistically non-significant (P < 0.05 is highly statistically significant), whereas the P value for distal aspect of implant was statistically significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be same in both 13 mm and 10 mm implants on the mesial aspect of implant whereas on distal aspect, it was more in 10 mm implants when compared with 13 mm implants [Figure 16].
Table 8.
Comparison of bone loss on mesial and distal after 6 months for group-1 (13 mm) verses group-2 (10 mm) for parameter-1 (implant length)
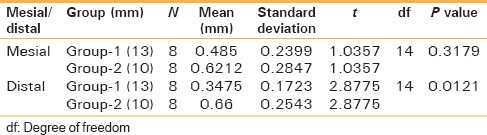
Figure 16.
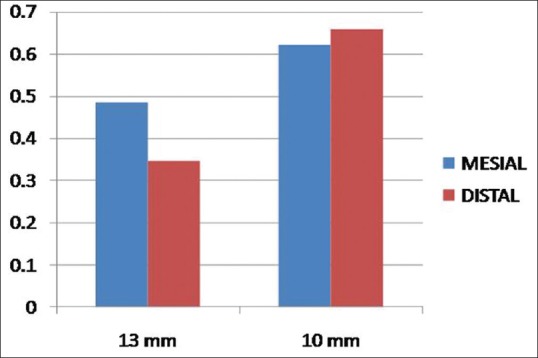
Comparison of bone loss on mesial and distal after 6 months for Group-1 (13 mm) verses Group-2 (10 mm) for parameter-1 (implant length)
Table 9 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for 3.5 mm implants verses 4.3 mm implants. The mean bone loss on mesial aspect of implants was 0.5387 mm for 3.5 mm implants and 0.5675 mm for 4.3 mm implants. Whereas the mean bone loss on distal aspect of implants was 0.4512 mm for 3.5 mm implants and 0.5562 mm for 4.3 mm implants. The P values for both mesial and distal aspects of implants were found to be non-significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be same in both 3.5 mm and 4.3 mm diameter implants on both mesial and distal aspects of implants [Figure 17].
Table 9.
Comparison of bone loss on mesial and distal after 6 months group-1 (3.5 mm) versus group-2 (4.3 mm) for parameter-2 (implant diameter)
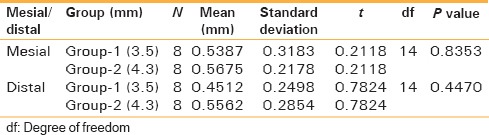
Figure 17.
Comparison of bone loss on mesial and distal after 6 months Group-1 (3.5 mm) versus Group-2 (4.3 mm) for parameter-2 (implant diameter)
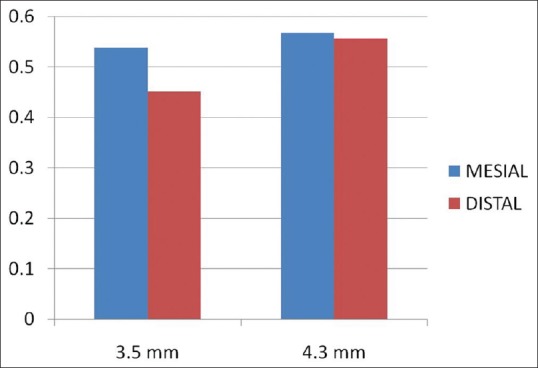
Table 10 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for maxillary implants verses mandibular implants. The mean bone loss on mesial aspect of implants was 0.601 mm for maxillary implants and 0.4733 mm for mandibular implants, whereas the mean bone loss on distal aspect of implants was 0.481 mm for maxillary implants and 0.5417 mm for mandibular implants. The P values for both mesial and the distal aspect of implant were found to be statistically non-significant significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be same in both maxilla as well as mandible on both mesial and distal aspects of implants [Figure 18].
Table 10.
Comparison of bone loss on mesial and distal after 6 months group-1 (maxilla) versus group-2 (mandible) for parameter-3 (implant location)
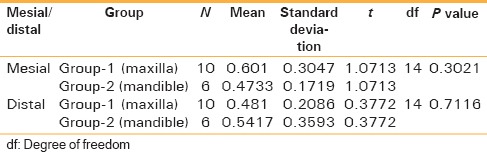
Figure 18.
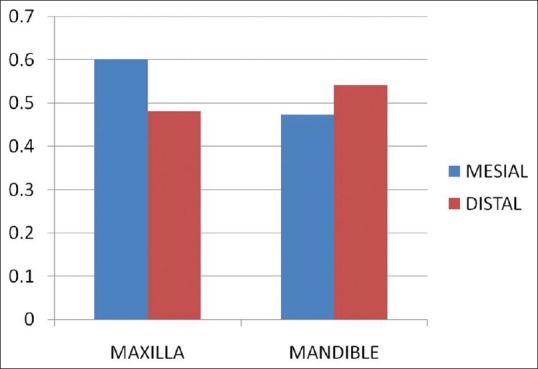
Comparison of bone loss on mesial and distal after 6 months Group-1 (maxilla) versus Group-2 (Mandible) for parameter-3 (implant location)
Table 11 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for males verses females. The mean bone loss on mesial aspect of implants was 0.4554 mm for males and 0.784 mm for females, whereas the mean bone loss on distal aspect of implants was 0.4264 mm for males and 0.644 mm for females. The P values for both mesial and the distal aspect of implant were found to be statistically significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be more in females on both mesial as well as the distal aspects of implants [Figure 19].
Table 11.
Comparison of bone loss on mesial and distal after 6 months group-1 (male) versus group-2 (female) for parameter-4 (gender)
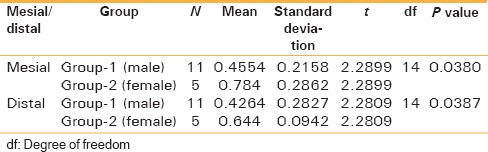
Figure 19.
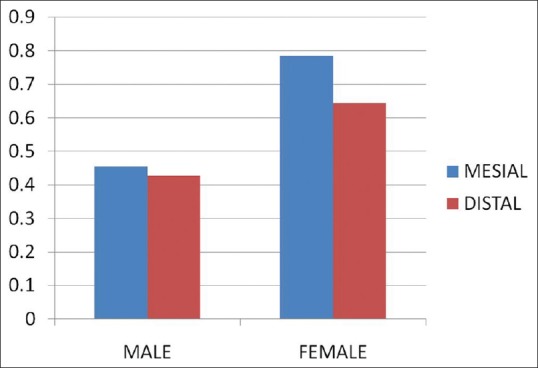
Comparison of bone loss on mesial and distal after 6 months Group-1 (male) versus Group-2 (female) for parameter-4 (gender)
DISCUSSION
The use of endosteal implant for dental rehabilitation of patients represents one of the most technologically advanced forms of dentistry available today. Endosteal implant is effective and appropriate for replacing single teeth, as well as for rehabilitating edentulous arches. The crestal bone area is usually a significant indicator of implant health, for its clinical success and longevity.
The long term preservation of crestal bone height around osseointegrated implants is often used as a primary success criterion for different implant systems. The radiographic evaluation of bone forms a very important and viable means of detecting health and stability of bone around the peri-implant hard tissue. A decrease of crestal bone level indicates that the implant is loosening its bony anchorage.[8] The pathological changes in the follow-up period always begin around the neck of implant. A study by Jung et al.[9] found that more than 50% of the total bone loss recorded in 12 months period occurred during the first 3 months. The rapid initial bone loss might be the result of periosteal elevation, surgical trauma, the preparation of the recipient bed and stress concentration from excessive tightening of the implant.[10] Various causes of greater crestal bone loss in the 1st year of implant function are surgical trauma, occlusal overload, peri-implantitis, presence of microgap, reformation of biologic width and implant crest module design.[11] A review of literature and the analysis of the results indicate that the stability of bone support for the implant is an important criterion for determining success of implants. There are many factors affecting the survival and success of implants. It has been documented that subtle changes in shape, length and width of endosseous implants could influence success rates.[12]
Various imaging options are available for the evaluation of the recipient site such as IOPA radiographs, panoramic radiographs, oblique cephalometric radiographs, computed tomography, digital subtraction radiography. Radiographs are an important tool for the assessment of bone architecture. Radiographs may be helpful in assessing stress concentration around implants, thereby obviating excessive alveolar bone loss.[13] The small changes in crestal bone levels emphasize the requirement for accurate and reproducible techniques in radiographic evaluation of the status of bone height.[14]
The standardized periapical radiographs are particularly well-suited and preferred for longitudinal assessment of implant bone loss.[15]
Rotational panoramic radiographs are not reproducible and lack sharpness, distort images and superimpose bony structures of the spine.[16] Moreover, the inconsistent magnification at each region, decreased resolution and lack of standardization of projection geometry mean there is a risk of loss of measuring precision.[15] The large area imaged with this technique is useful in initial planning of treatment which mainly includes the assessment of distance from alveolar crest to mandibular canal and mental foramen in mandible and to floor of maxillary sinus, nasal cavity and incisive canal in the maxilla.[17] The oblique cephalometric technique requires special radiographic equipment.[18]
The periapical radiographs have minimal distortion when they are well angulated applying the standardized projection geometry as described by Duckworth et al.[19] In addition, exposure dose of periapical radiography is extremely low compared to that of other modalities. The measurement value on periapical radiographs is the most reliable due to the sharpness and resolution of images obtained with the standardized periapical radiographs obtained by the long cone paralleling technique.[15] Furthermore, the standardized periapical radiographs probably provide the highest reliability and reproducibility in terms of linear measuring distance. The reproducibility of the radiographs obtained by the intra-oral bisecting angle technique is poor.[16] Therefore, the periapical radiographs are particularly well-suited for longitudinal assessment of implant bone loss.[15]
In assessing bone height in the implant region, different methods have been used: Like counting the number of threads on screw type implants, measurements by means of a computer based interactive image analysis system, measurements with the help of a magnifying glass or a digital sliding gauge.
Thus, the present study was undertaken to evaluate the “marginal bone level” changes around implants (titanium endosteal transmucosal screw type fixtures, Branemark) using the standardized periapical radiographs. These radiographs made through long cone paralleling technique with the help of radiographic film holders (Rinn XCP; Dentsply).[15,20,21,22] A customized occlusal jig[21] was fabricated by attaching modeling wax to the film holder and asking the patient to bite on this. The jig was acrylized in heat-cured acrylic and saved for use at later visits to standardize the film placement and cone angulation.[21]
The radiographs were made at 0 month, i.e., immediately after implant placement and then after 6 months, but before prosthetic loading.[23] To obtain a reproducible data, the definition of reference points in the image is most important. The most coronal point of implant was taken as the reference line because it was permanently visible and easy to locate on all radiographs. The point of bone to implant contact was chosen as the bone level.[24] The measurements were made with the help of UTHSCSA Image Tool (version 3.00 for Windows, University of Texas Health Science Center in San Antonio, TX, USA).[24] Prior to analysis, the images were calibrated geometrically based on implant length, so that the measurements record the actual distance.[25] Measurements were made at 0 month and at 6 months at the mesial and distal aspects of implants by dropping perpendiculars from the reference line to the bone level. All the radiographs showed a clear image of the implant and marginal bone. The clearly visible threads of implants indicated that the central X-ray beam has been directed perpendicular to the object and film.[26]
According to the results obtained from the above study, Table 3 shows that the mean bone loss observed on mesial aspect of implant after 6 months of implant placement was 0.5531 mm while the mean bone loss on distal aspect was 0.5037 mm. The results of this study are in accordance with those of Singh et al.[23] who found a mean bone loss of 0.6 mm on mesial and 0.9 mm on distal aspect of implant after 6 months of implant placement. Similar study conducted by Behneke et al., observed a mean bone loss of 0.8 mm between implant placement and prosthetic restoration.[27] In contrast, studies by Johansson and Ekfeldt[28] showed a mean bone loss amounting to 0.4 mm at the 1st year and annual following 0.1 mm rate on Branemark implants. Similar studies conducted by Adell et al. determined that the mean bone loss for Branemark osseointegrated implants was 1.5 mm for the 1st year.[10] Cox and Zarb reported 1.6 mm loss in the 1st year and 0.13 mm in subsequent years.[29] Studies conducted by Bryant and Zarb noted that there is no difference in crestal bone loss proximal to oral implants in the complete implant prosthesis sites of older and younger adults and a mean bone levels at loading were 1.4 mm determined in the 1st year.[30] The marginal bone loss should not be greater than 1.5 mm in the 1st year (osseointegration period) and 0.1 mm during each successive year (follow-up period).[30,31] Smith and Zarb suggested that one of the criteria for implant success was that less than 0.2 mm alveolar bone loss occurred per year after the 1st year.[7]
Hence, many authors have stated that the alveolar bone loss is around 1.2 mm during the 1st year and stabilizes to an average of 0.1 mm/year but the most active phase of bone loss during the first few months has not been studied extensively. This study evaluated the early changes in the marginal bone level around dental implants through standard intra-oral radiographs in the initial 6 months of implant placement, but before prosthetic loading.
Table 8 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for 13 mm implants verses 10 mm implants. The mean bone loss on mesial aspect of implants was 0.485 mm for 13 mm implants and 0.6212 mm for 10 mm implants. Whereas the mean bone loss on distal aspect of implants was 0.3475 mm for 13 mm implants and 0.66 mm for 10 mm implants. The P value for mesial aspect of implant was found to be statistically non-significant (P < 0.05 is highly statistically significant), whereas the P value for distal aspect of implant was statistically significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be same in both 13 mm and 10 mm implants on the mesial aspect of implant whereas on distal aspect, it was more in 10 mm implants when compared with 13 mm implants. The results of this study were in accordance with those reported by Naert et al.[32] who found shorter implant lengths are associated with more failure. In contrast, studies by Deporter et al.[33] and Rokn et al.[34] found similar results for both short as well as long implants.
Table 9 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for 3.5 mm implants verses 4.3 mm implants. The mean bone loss on mesial aspect of implants was 0.5387 mm for 3.5 mm implants and 0.5675 mm for 4.3 mm implants. Whereas the mean bone loss on distal aspect of implants was 0.4512 mm for 3.5 mm implants and 0.5562 mm for 4.3 mm implants. The P values for both mesial and distal aspects of implants were found to be non-significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be same in both 3.5 mm and 4.3 mm diameter implants on both mesial and distal aspects of implants. The results of this study were in accordance with study by Tawil et al.[35] who found similar values of bone loss for narrow and wide implants. According to Tamizi et al.,[36] implant diameter is a significant determinant of bone loss occurring around the implant with the risk of bone loss around a 3.5 mm diameter implant to be 5.91 folds more than a 4 mm diameter implant. Strong et al.[37] in their study have reported more risks of bone loss for implants with lower diameters compared with those with higher diameters. Scurria et al. found that implant width of less than 4.0 mm was associated with implant failure.[38]
Table 10 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for maxillary implants verses mandibular implants. The mean bone loss on mesial aspect of implants was 0.601 mm for maxillary implants and 0.4733 mm for mandibular implants, whereas the mean bone loss on distal aspect of implants was 0.481 mm for maxillary implants and 0.5417 mm for mandibular implants. The P values for both mesial and the distal aspect of implant were found to be statistically non-significant significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be same in both maxilla as well as mandible on both mesial and distal aspects of implants. The results of this study were in accordance with similar studies that reported no significant differences in the bone loss values between maxillary and mandibular implants.[20,39,40] Kumar et al.[41] studied 1183 ITI SLA implants and observed no significant difference in bone loss regarding the jaw position. Tamizi et al.[36] showed similar bone loss values for implants placed at the maxilla and mandible. On the contrary, Peñarrocha et al.[42] showed more bone loss for fixtures implanted at maxilla compared to mandibular fixtures. Pham et al.[39] in their study have reported more bone loss for maxillary implants than mandibular ones.
Table 11 shows mean values of recorded bone loss on mesial and distal aspects of implant after 6 months when compared for males verses females. The mean bone loss on mesial aspect of implants was 0.4554 mm for males and 0.784 mm for females, whereas the mean bone loss on distal aspect of implants was 0.4264 mm for males and 0.644 mm for females. The P values for both mesial and the distal aspect of implant were found to be statistically significant (P < 0.05 is highly statistically significant). Thus, in this study, the bone loss was found to be more in females on both mesial as well as the distal aspects of implants. Fartash et al. revealed no statistically significant difference between males and females. The results of this study were in contrast with those by Sverzut et al.[43] who found that men have 1.255 times greater risk of early implant failure than females.
The differences in the mean bone loss values reported by different authors may be attributed to the different implant designs, the surgeons experience, the number of studied implants, the oral hygiene status and practice in patients undergoing implant restorations, the time past from implant reception, the bone quality at the implant sites, or different measures to assess implant treatments.
The rapid bone loss in the initial months after implant placement may be because the fixtures are not loaded, so there is lack of physiologic stimulation and also there may be activities of remodeling which is a physiological change independent of loading and starts as soon as the implant is placed in bone. Pham et al. found that significantly more crestal bone loss was noted before functional loading than after the prosthesis was connected.[39]
Jung et al.[9] found that more than 50% of the total bone loss recorded in 12 months period occurred during the first 3 months. Several investigators have indicated that crestal bone loss around dental implants may be a normal occurrence as it eventually exhibits a steady state when an adequate mucosal barrier is formed by the peri-implant epithelial connective attachment. However, other views suggest that crestal bone loss may result from surgical trauma during placement of the fixtures, reflection of periosteum and preparation of implant osteotomy. The bone loss occurring post-operatively in the initial few months may also be attributed to bacterial invasion, the re-establishment of biologic width and the factors of stress concentration at the crestal region. The primary cause of bone loss around natural teeth is bacteria induced. Occlusal trauma may accelerate the process, but trauma alone is not a determining factor. The implant gingival sulcus in the partially edentulous implant patients exhibits a bacterial flora similar to that of natural teeth. Hence, a logical assumption is that the early implant bone loss is caused primarily by bacteria, with occlusal factors playing a contributing role or accelerating role. Poor oral hygiene is reported to accelerate the bone loss observed around endosteal implants.
According to the results obtained from this study, more crestal bone loss was observed with 10 mm implants when compared to the 13 mm implants. This might be due to the better primary stability obtained with longer implants (13 mm) when compared to the shorter ones (10 mm) due to increase in the surface area of long implants and thus contributing to better anchorage and bone-implant integration.
According to the results obtained from this study, more crestal bone loss was observed in females as compared with males.
In this study, the mean crestal bone loss of 0.5531 mm on mesial and 0.5037 on distal aspect of implant are within the success criteria of implant (mean crestal bone loss <1.5 mm in 1 year).
Since the sample size was relatively small, so further studies are recommended with larger sample size.
CONCLUSIONS
Within the limitations of the study, the following conclusions were drawn:
The mean marginal bone loss after 6 months of implant placement was 0.5531 mm on mesial and 0.5037 mm on distal aspect of implant
There were no statistically significant differences between the marginal bone loss on mesial compared with the distal aspect of implant after 6 months of implant placement. Thus, the bone loss on mesial and distal aspects of implants was found to be same after a period of 6 months
The mean marginal bone loss for 13 mm implants was 0.485 mm on mesial and 0.3475 mm on distal aspect of implant. Whereas, the mean marginal bone loss for 10 mm implants was 0.6212 mm on mesial and 0.66 mm on distal aspect of implant. Thus, in this study, the bone loss was found to be same in both 13 mm and 10 mm implants on the mesial aspect of implant whereas on distal aspect, it was more in 10 mm implants when compared with 13 mm implants
The mean marginal bone loss for 3.5 mm implants was 0.5387 mm on mesial and 0.4512 mm on distal aspect of implant. Whereas, the mean marginal bone loss for 4.3 mm implants was 0.5675 mm on mesial and 0.5562 mm on distal aspect of implant. Thus, in this study, the bone loss was found to be same in both 3.5 mm and 4.3 mm diameter implants on both mesial and distal aspects of implants
The mean marginal bone loss for implants placed in maxilla was 0.601 mm on mesial and 0.481 mm on distal aspect of implant. Whereas, the mean marginal bone loss for implants placed in mandible was 0.4733 mm on mesial and 0.5417 mm on distal aspect of implant. Thus, in this study, the bone loss was found to be same in both maxilla as well as mandible on both mesial and distal aspects of implants
The mean marginal bone loss for implants placed in males was 0.4554 mm on mesial and 0.4264 mm on distal aspect of implant. Whereas, the mean marginal bone loss for implants placed in females was 0.784 mm on mesial and 0.644 mm on distal aspect of implant. Thus, in this study, the bone loss was found to be more in females on both mesial as well as the distal aspects of implants.
Clinical significances
Thus, some amount of post-operative crestal bone loss is inevitable but efforts should always be made to minimize the post-operative crestal bone loss for the clinical success and longevity of implants. Based on the results obtained from this study, following measures may be recommended to minimize the post-operative crestal bone loss during the initial months of healing but before prosthetic loading.
Implants may be selected with longer length, if bone quantity permits
Surgical trauma should be minimized during preparation of implant osteotomy site and implant placement
Patients should be encouraged for meticulous oral hygiene maintenance in the post-operative period
A regular follow-up is required to evaluate the osseointegration and the crestal bone levels in order to evaluate the clinical success and longevity of implants.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Branemark PI. Introduction to osseointegration. In: Branemark PI, Zarb GA, Albrektsson T, editors. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago: Quintessence Publ; 1985. pp. 11–76. [Google Scholar]
- 2.Ashley ET, Covington LL, Bishop BG, Breault LG. Ailing and failing endosseous dental implants: A literature review. J Contemp Dent Pract. 2003;4:35–50. [PubMed] [Google Scholar]
- 3.Lavstedt S, Bolin A, Henrikson CO. Proximal alveolar bone loss in a longitudinal radiographic investigation. II. A 10-year follow-up study of an epidemiologic material. Acta Odontol Scand. 1986;44:199–205. doi: 10.3109/00016358608997721. [DOI] [PubMed] [Google Scholar]
- 4.Bergman B. Evaluation of the results of treatment with osseointegrated implants by the Swedish National Board of Health and Welfare. J Prosthet Dent. 1983;50:114–5. doi: 10.1016/0022-3913(83)90176-2. [DOI] [PubMed] [Google Scholar]
- 5.Akdeniz BG, Oksan T, Kovanlikaya I, Genç I. Evaluation of bone height and bone density by computed tomography and panoramic radiography for implant recipient sites. J Oral Implantol. 2000;26:114–9. doi: 10.1563/1548-1336(2000)026<0114:EOBHAB>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 7.Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62:567–72. doi: 10.1016/0022-3913(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 8.Kwon JY, Kim YS, Kim CW. Assessing changes of peri-implant bone using digital subtraction radiography. J Korean Acad Prosthodont. 2001;39:273–80. [Google Scholar]
- 9.Jung YC, Han CH, Lee KW. A 1-year radiographic evaluation of marginal bone around dental implants. Int J Oral Maxillofac Implants. 1996;11:811–8. [PubMed] [Google Scholar]
- 10.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 11.Hosseinzadeh A, Savabi O, Nassiri F. Average annual crestal bone loss of ITI implants following the first year of loading. J Res Med Sci. 2006;11:146–50. [Google Scholar]
- 12.Misch CE. 2nd ed. St. Louis: Elsevier; 1999. Contemporary Implant Dentistry; p. 54. [Google Scholar]
- 13.Misch CE. Implant success or failure: Clinical assessment. In: Misch CE, editor. Contemporary Implant Dentistry. St. Louis: Mosby; 1992. pp. 29–42. [Google Scholar]
- 14.Shulman LB. Surgical considerations in implant dentistry. J Dent Educ. 1988;52:712–20. [PubMed] [Google Scholar]
- 15.Wakoh M, Harada T, Otonari T, Otonari-Yamamoto M, Ohkubo M, Kousuge Y, et al. Reliability of linear distance measurement for dental implant length with standardized periapical radiographs. Bull Tokyo Dent Coll. 2006;47:105–15. doi: 10.2209/tdcpublication.47.105. [DOI] [PubMed] [Google Scholar]
- 16.Meijer HJ, Steen WH, Bosman F. A comparison of methods to assess marginal bone height around endosseous implants. J Clin Periodontol. 1993;20:250–3. doi: 10.1111/j.1600-051x.1993.tb00353.x. [DOI] [PubMed] [Google Scholar]
- 17.Lindh C, Petersson A. Radiologic examination for location of the mandibular canal: A comparison between panoramic radiography and conventional tomography. Int J Oral Maxillofac Implants. 1989;4:249–53. [PubMed] [Google Scholar]
- 18.Steen WH. Errors in oblique cephalometric radiographic projections of the edentulous mandible. Part I: Geometric errors. J Prosthet Dent. 1984;51:411–8. doi: 10.1016/0022-3913(84)90233-6. [DOI] [PubMed] [Google Scholar]
- 19.Duckworth JE, Judy PF, Goodson JM, Socransky SS. A method for the geometric and densitometric standardization of intraoral radiographs. J Periodontol. 1983;54:435–40. doi: 10.1902/jop.1983.54.7.435. [DOI] [PubMed] [Google Scholar]
- 20.Boronat A, Peńarrocha M, Carrillo C, Marti E. Marginal bone loss in dental implants subjected to early loading (6 to 8 weeks postplacement) with a retrospective short-term follow-up. J Oral Maxillofac Surg. 2008;66:246–50. doi: 10.1016/j.joms.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 21.Rao W, Benzi R. Single mandibular first molar implants with flapless guided surgery and immediate function: Preliminary clinical and radiographic results of a prospective study. J Prosthet Dent. 2007;97(6 Suppl):S3–14. doi: 10.1016/S0022-3913(07)60003-1. [DOI] [PubMed] [Google Scholar]
- 22.Kan JY, Rungcharassaeng K, Liddelow G, Henry P, Goodacre CJ. Periimplant tissue response following immediate provisional restoration of scalloped implants in the esthetic zone: A one-year pilot prospective multicenter study. J Prosthet Dent. 2007;97(6 Suppl):S109–18. doi: 10.1016/S0022-3913(07)60014-6. [DOI] [PubMed] [Google Scholar]
- 23.Singh P, Garge HG, Parmar VS, Viswambaran M, Goswami MM. Evaluation of implant stability and crestal bone loss around the implant prior to prosthetic loading: A six month study. J Indian Prosthodont Soc. 2006;6:33–7. [Google Scholar]
- 24.Shin YK, Han CH, Heo SJ, Kim S, Chun HJ. Radiographic evaluation of marginal bone level around implants with different neck designs after 1 year. Int J Oral Maxillofac Implants. 2006;21:789–94. [PubMed] [Google Scholar]
- 25.Galli F, Capelli M, Zuffetti F, Testori T, Esposito M. Immediate non-occlusal vs. early loading of dental implants in partially edentulous patients: A multicentre randomized clinical trial. Peri-implant bone and soft-tissue levels. Clin Oral Implants Res. 2008;19:546–52. doi: 10.1111/j.1600-0501.2008.01530.x. [DOI] [PubMed] [Google Scholar]
- 26.Siepenkothen T. Clinical performance and radiographic evaluation of a novel single-piece implant in a private practice over a mean of seventeen months. J Prosthet Dent. 2007;97(6 Suppl):S69–78. doi: 10.1016/S0022-3913(07)60010-9. [DOI] [PubMed] [Google Scholar]
- 27.Behneke A, Behneke N, d’Hoedt B, Wagner W. Hard and soft tissue reactions to ITI screw implants: 3-year longitudinal results of a prospective study. Int J Oral Maxillofac Implants. 1997;12:749–57. [PubMed] [Google Scholar]
- 28.Johansson LA, Ekfeldt A. Implant-supported fixed partial prostheses: A retrospective study. Int J Prosthodont. 2003;16:172–6. [PubMed] [Google Scholar]
- 29.Cox JF, Zarb GA. The longitudinal clinical efficacy of osseointegrated dental implants: A 3-year report. Int J Oral Maxillofac Implants. 1987;2:91–100. [PubMed] [Google Scholar]
- 30.Bryant SR, Zarb GA. Crestal bone loss proximal to oral implants in older and younger adults. J Prosthet Dent. 2003;89:589–97. doi: 10.1016/s0022-3913(03)00199-9. [DOI] [PubMed] [Google Scholar]
- 31.Weber HP, Buser D, Fiorellini JP, Williams RC. Radiographic evaluation of crestal bone levels adjacent to nonsubmerged titanium implants. Clin Oral Implants Res. 1992;3:181–8. doi: 10.1034/j.1600-0501.1992.030405.x. [DOI] [PubMed] [Google Scholar]
- 32.Naert I, Koutsikakis G, Duyck J, Quirynen M, Jacobs R, van Steenberghe D. Biologic outcome of implant-supported restorations in the treatment of partial edentulism. Part I: A longitudinal clinical evaluation. Clin Oral Implants Res. 2002;13:381–9. doi: 10.1034/j.1600-0501.2002.130406.x. [DOI] [PubMed] [Google Scholar]
- 33.Deporter D, Pilliar RM, Todescan R, Watson P, Pharoah M. Managing the posterior mandible of partially edentulous patients with short, porous-surfaced dental implants: Early data from a clinical trial. Int J Oral Maxillofac Implants. 2001;16:653–8. [PubMed] [Google Scholar]
- 34.Rokn AR, Noorani H, Afzalifar R. Evaluation of survival rate and bone loss of implants with various lengths. J Dent. 2006;3:153–8. [Google Scholar]
- 35.Tawil G, Mawla M, Gottlow J. Clinical and radiographic evaluation of the 5-mm diameter regular-platform Brånemark fixture: 2-to 5-year follow-up. Clin Implant Dent Relat Res. 2002;4:16–26. doi: 10.1111/j.1708-8208.2002.tb00147.x. [DOI] [PubMed] [Google Scholar]
- 36.Tamizi M, Ghanavati F, Radvar M, Rahmani MA. Comparison of bone healing around nonsubmerged and submerged implants in Maestro system of Biohorizon technology. J Dent Sch Shahid Beheshti Univ Med Sci. 2005;23:18–27. [Google Scholar]
- 37.Strong JT, Misch CE, Bidez MW, Nalluri P. Functional surface area: Thread form parameter optimization for implant body design. Compend Contin Educ Dent. 1998;19:4–9. [Google Scholar]
- 38.Scurria MS, Shugars DA, Hayden WJ, Felton DA. General dentists’ patterns of restoring endodontically treated teeth. J Am Dent Assoc. 1995;126:775–9. doi: 10.14219/jada.archive.1995.0273. [DOI] [PubMed] [Google Scholar]
- 39.Pham AN, Fiorellini JP, Paquette D, Williams RC, Weber HP. Longitudinal radiographic study of crestal bone levels adjacent to non-submerged dental implants. J Oral Implantol. 1994;20:26–34. [PubMed] [Google Scholar]
- 40.Carlsson GE, Lindquist LW, Jemt T. Long-term marginal periimplant bone loss in edentulous patients. Int J Prosthodont. 2000;13:295–302. [PubMed] [Google Scholar]
- 41.Kumar A, Jaffin RA, Berman C. The effect of smoking on achieving osseointegration of surface-modified implants: A clinical report. Int J Oral Maxillofac Implants. 2002;17:816–9. [PubMed] [Google Scholar]
- 42.Peñarrocha M, Palomar M, Sanchis JM, Guarinos J, Balaguer J. Radiologic study of marginal bone loss around 108 dental implants and its relationship to smoking, implant location, and morphology. Int J Oral Maxillofac Implants. 2004;19:861–7. [PubMed] [Google Scholar]
- 43.Sverzut AT, Stabile GA, de Moraes M, Mazzonetto R, Moreira RW. The influence of tobacco on early dental implant failure. J Oral Maxillofac Surg. 2008;66:1004–9. doi: 10.1016/j.joms.2008.01.032. [DOI] [PubMed] [Google Scholar]


