Abstract
Background:
Oral cancer is one of the most common life-threatening diseases all over the world. Developing countries face several challenges to identify and remove potential risk factors. Chewing tobacco/pan masala is considered to be the most potent risk factor for oral precancerous lesions and oral cancer.
Objectives:
To investigate the relative occurrence of different oral pre-cancerous lesions and oral cancer in North India and to identify the associated risk factors.
Materials and Methods:
A hospital-based study was conducted and 471 subjects were recruited in the study. The subjects comprised patients with squamous cell carcinoma (n = 85), oral submucous fibrosis (n = 240), leukoplakia (n = 32), lichen planus (n = 15), and controls (n = 99). Statistical analysis of the data was done using Chi-square and regression analysis.
Results:
A strong correlation was observed between the presence of the chewing habit in all the oral precancerous lesions and oral cancer. Duration of the habit and intensity of habit ware also strongly correlated with the risk of oral precancerous lesions and oral cancer. Other factors such as alcohol and smoking were found to be less important in concern with oral cancer and precancerous lesions.
Keywords: Leukoplakia, lichen planus, oral cancer, oral submucous fibrosis, tobacco chewing
INTRODUCTION
India is one of the countries having the highest incidence of oral cancer in the world.[1] Lifestyle-related habits such as smoking, drinking of alcohol, chewing of tobacco/pan masala (mixture of areca nut, lime, catechu, and sweetening, coloring, and flavoring agents, with or without tobacco) and paan [betel leaf (Piper betle) with areca nut and slaked lime paste], and so on are prevalent in different parts of the world. In the South Asian region, over one-third of the tobacco consumed is smokeless.[2] Traditional forms like areca nut, betel quid, pan masala, tobacco with lime, and tooth powder containing tobacco are commonly used and the use of new products is increasing, not only among men but also among children, teenagers, women of reproductive age, and medical and dental students.[3] In India, where chewing tobacco is used with betel nuts and reverse smoking (placing the lit end in the mouth) is practiced, there is a striking incidence of oral cancer.[3] Oral cancer is related to these etiological factors from qualitative as well as quantitative points of view. A study on reverse smoking revealed that the use of tobacco in this form conferred a 5.19 times higher risk of oral precancerous lesions of the palate than did the use of chewing tobacco.[4]
Oral precancerous lesions and conditions such as oral leukoplakia and oral submucous fibrosis (OSF) have been shown to have a high rate of transformation to oral cancer.[5,6] The prevalence of OSF in India varies between 0.03 and 3.2% according to various studies.[7,8,9] Also, a higher occurrence of leukoplakia and cancer is observed in OSF patients, and tobacco is considered to be an important risk factor for oral cancer among youths.[10,11] The belt of India comprising Uttar Pradesh, Bihar, and Jharkhand witness a very high incidence of oral precancerous and cancerous lesions.[12] At the same time, the frequency of chewing tobacco/pan masala or other similar products is higher in comparison to other parts of the country.[13] Therefore, we hypothesize that chewing tobacco/pan masala or other similar products may pose a risk for precancerous oral lesions and oral cancer. The present study was conducted to understand the clinical profile of the individuals with oral precancerous lesions or oral cancer, estimate the relative prevalence of these disorders, and to test the hypothesis that chewing tobacco/pan masala are the risk factors for them.
MATERIALS AND METHODS
Study participants
A total of 1,47,983 patients were screened in the Department of Oral Pathology, King George's Medical University, Lucknow, Uttar Pradesh during 2006-2009. Of them, 471 individuals were enrolled in the study after informed consent. Among them, 99 individuals were identified as control, who had a positive history of tobacco with no oral lesions and 372 individuals having dental complaints were categorized under case with a positive history of the chewing habit as well as oral lesions. Written informed consent was taken from every patient in their own language regarding the questionnaire and intraoral examination.
Data collection
Information about chewing habits and other characterstics of the study participants was acquired using the standardized interviewer-based questionnaire. Those with the habit were questioned for the frequency of the habit in number per day and duration of the habit in years. The type of lesion in the cases was decided on the basis of careful observation of the oral cavity followed by histopathology analysis of the oral biopsies in all the cases. Ninety-nine individuals visiting the Oral Department for complaints other than oral precancerous/cancerous lesions were enrolled as controls in the study. It was made sure that the controls did not have any of the above-mentioned problems. Personal habits such as tobacco chewing/smoking/pan masala/bidi (tobacco wrapped in the leaf of Diospyros melanoxylon)/cigarette/alcohol, and so on were recorded for the controls in a manner similar to the cases.
Statistical analyses
Descriptive statistics were used to find mean and standard deviations of different parameters. The variables (habits) with discrete values (yes or no) such as smoking, alcohol, and tobacco/pan masala chewing habits were analyzed for significance using the Chi-square test. Education level was classified as ‘illiterate’ and ‘literate’, where literate meant above class seven. Similarly, economic status was classified as ‘lower’ and ‘middle’. To look study the association of each habit with a particular type of malignancy, we used the Chi-square test.
Individuals with the habit of chewing any form of tobacco such as khaini, bhang, or pure tobacco, betel leaf with tobacco, chewing tobacco plus lime, mishri (burned tobacco applied to the teeth and gums), moist snuff, dry snuff, niswar (a different kind of tobacco snuff) and naas (a stronger form of niswar) with or without areca nut were considered in one group named ’tobacco chewing’, those with the habit of chewing pan masala were considered in a separate group named ‘pan masala’, and those with both the above habits were considered under the ‘mixed habits’ group. Those who drank alcohol only on special occasions such as wedding banquets, family reunions, or birthday parties were considered as ‘occasional drinkers’, those with daily use were termed as ‘regular drinkers’, and those taking alcohol regularly more than once a day were considered as ‘heavy drinkers’. Oral lesions were classified on the basis of histological evaluation as ‘oral cancer’, ‘oral submucosal fibrosis (OSF)’, ‘leukoplakia’, and ‘lichen planus’.
The continuous variables such as habit intensity and duration, smoking intensity and duration, and alcohol intensity and duration were analyzed by nominal logistic regression analysis using Minitab (version 13). Henceforth, chewing of tobacco/panmasala in any form will be termed as ‘habit’ unless specified otherwise; however, the term does not include smoking and alcohol consumption. Correlation analysis using SPSS software (version 13, SPSS, Chicago) was run to estimate the influence of economic status, locality, and education.
RESULTS
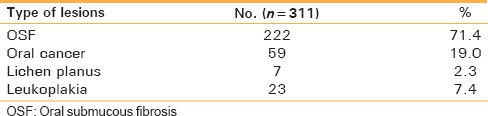
The frequency of the habits and the oral cancer or precancerous lesions is detailed in Tables 1-4. The cases included in the study belonged to the 1565-years, age group with a mean age of 37.84 years, and the controls were in the age group of 3055 with a mean age of 37.11 years. Majority of the patients (77.96%, 290 of 372) were male, whereas only 22.04% (82 of 372) were females. The control group included 65.7% (65 of 99) males and 34.3% (34 of 99) females. Most of the subjects belonged to middle (64.3%, 303 of 471) and lower (35.7%, 168 of 471) economic classes. Of 471 subjects, 84.93% (400 of 471) had some habit considered harmful for oral health, whereas only 15.07% (71 of 471) were without any habit [Table 5]. Among the individuals with habits, 33.75% (135 of 400) were tobacco chewers, 37.5% (150 of 400) were pan masala chewers and 28.75% (115 of 400) had mixed habits [Table 5]. The prevalence of smoking overall was 36.94% (174 of 471), and the prevalence was more in males (85.06%, 148 of 174) than females (14.94%, 26 of 174). The habit of drinking alcohol overall was 26.33% (124 of 471) with a higher frequency of male drinkers (85.48%, 106 of 124) in comparison to females (14.52%, 18 of 124). Of the total 372 cases with oral precancerous conditions and cancerous lesions, 22.85% (85 of 372) had oral cancer, 64.52% (240 of 372) had OSF, 8.6% (32 of 372) had leukoplakia, and only 4.03% (15 of 372) had lichen planus.
Table 1.
Sociodemographic characteristics of the patients
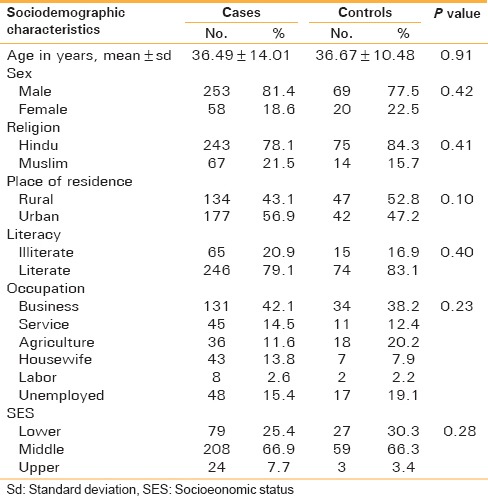
Table 4.
Risk factors for precancer and cancer
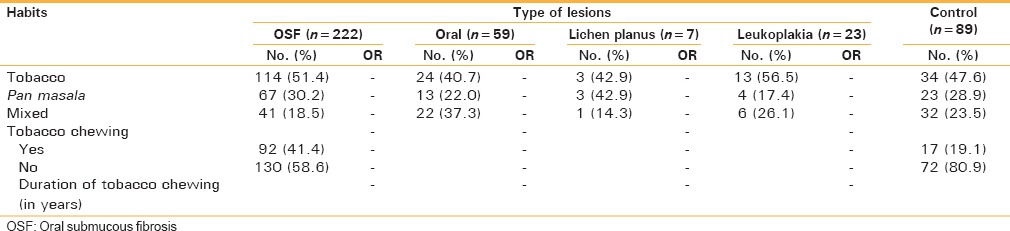
Table 5.
Dissection of habits versus oral pathologies; the values in the brackets indicate percentage
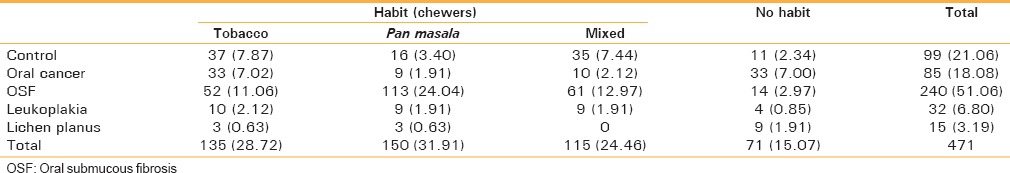
Table 2.
Tobacco habits of the patients
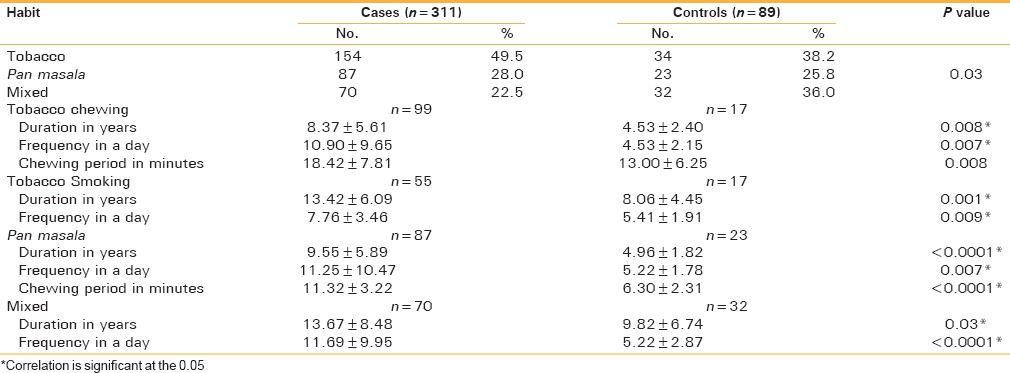
Table 3.
Prevalence of precancer and cancer lesions
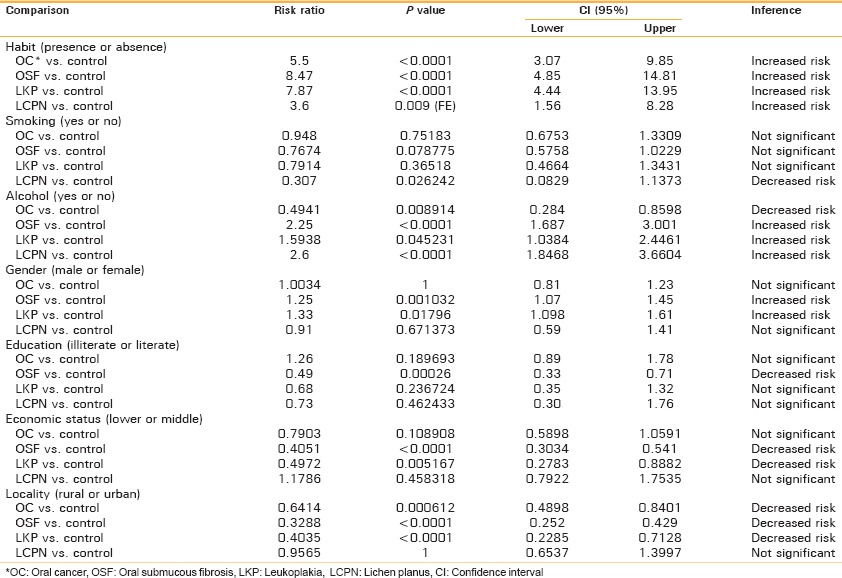
The Chi-square analysis revealed that the presence of the habit increased the risk of all kinds of precancerous and cancerous lesions [Table 6]. It was observed that the presence of the habit posed the highest risk for OSF (Risk ratio 8.47) followed by leukoplakia (RR = 7.87), oral cancer (RR = 5.5), and lichen planus (RR = 3.6). Smoking did not affect the risk of developing oral cancer, OSF, and leukoplakia; however, it was associated with a decreased risk of lichen planus (RR = 0.31). Drinking alcohol was associated with a reduced risk of oral cancer (RR = 0.49), but increased risk of OSF (RR = 2.25), leukoplakia (RR = 1.59), and lichen planus (RR = 2.6). The risk of oral cancer and lichen planus were not significantly different between male and female individuals; however, males were slightly at a higher risk of developing OSF (RR = 1.25) and leukoplakia (RR = 1.33). The risk of oral cancer, leukoplakia, and lichen planus did not differ significantly between literate and illiterate people; however, being illiterate decreased the risk of developing OSF (RR = 0.49). The risk of oral cancer and lichen planus did not differ significantly between individuals belonging to lower and middle income groups; however, the lower income group was at a lesser risk of developing OSF (RR = 0.40) and leukoplakia (RR = 0.49). The individuals belonging to rural localities were at a decreased risk of oral cancer (RR = 0.64), OSF (RR = 0.33), and leukoplakia (RR = 0.40); however, the risk of lichen planus did not differ between individuals belonging to rural and urban localities.
Table 6.
Chisquare analysis of discrete variables versus oral pathologies
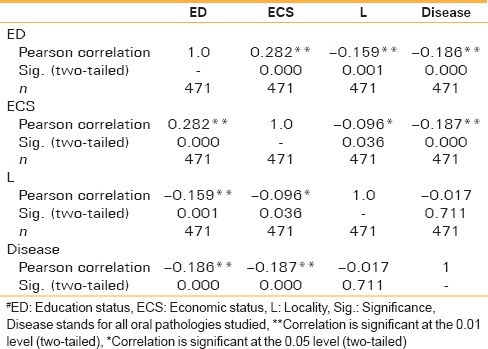
The data were analyzed by multiple regression using age, habit duration, habit intensity, smoking duration, smoking intensity, alcohol duration, and alcohol intensity as regressors. With other variables held constant, age related positively with oral cancer but negatively with OSF increasing by 0.11 for oral cancer and decreasing by 0.04 for OSF with every extra year of age [Table 7]. Habit duration was positively related to oral cancer and leukoplakia increasing by 0.01 for oral cancer and leukoplakia with every extra month of habit duration. Similarly, habit intensity positively correlated with oral cancer, OSF, and leukoplakia increasing by 0.14 for oral cancer, 0.22 for OSF, and 0.2 for leukoplakia with increase in frequency by one time per day. Smoking duration was only marginally related with oral cancer at 95% level of confidence, increasing by 0.007 with every extra month of smoking. Alcohol duration related negatively with oral cancer and leukoplakia, decreasing by 0.01 for oral cancer and leukoplakia with every extra month of the alcohol habit. None of the variables related with lichen planus. Correlation analysis showed a significant effect of locality and economic status on education [Table 8]. Also, the economic status and locality were correlated with each other.
Table 7.
Nominal logistic regression for continuous variables versus risk of oral pathologies
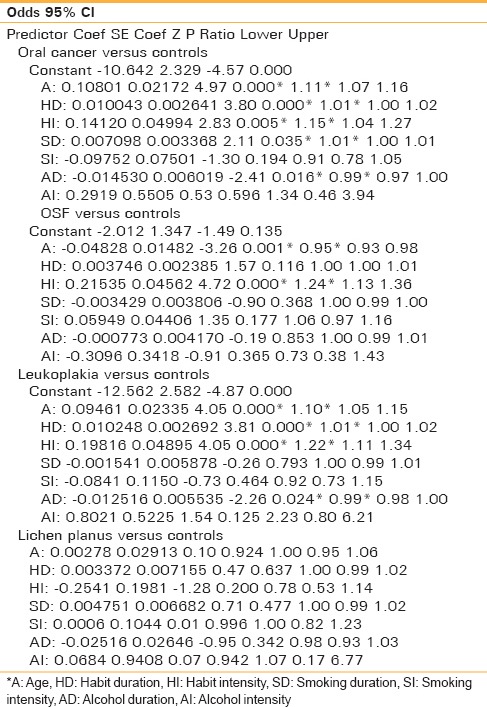
Table 8.
Correlations between the variables and diseases
DISCUSSION
The habit posed the maximum risk for OSF, which justifies the highest prevalence of OSF in this region of the country. The risk was an interplay of habit duration and intensity. These habits are very addicting and the users often continue chewing tobacco/pan masala over several years. The length of chewing duration also increases the number of times one chews. There are users in this part of the country who chew tobacco/pan masala continuously during waking hours. The use of smokeless tobacco (Pan Parag, zarda, etc.) is on the rise in North India and especially in Uttar Pradesh. Considering the impact of habit duration and intensity, it is not surprising to see a high incidence of oral cancer and OSF in this region.[14]
Among other factors which could modify the risk of oral lesions, alcohol appeared to increase the risk of OSF, leukoplakia, and lichen planus but not oral cancer. It is difficult to explain why alcohol should increase the risk of oral precancerous lesions but not oral cancer. Males were at a higher risk of developing OSF and leukoplakia; however, the risk of cancer was not significantly different between the two genders. This difference could be related to the difference in habit frequency between male and female individuals, diet, or other physiological factors. Smoking duration was only marginally related with oral cancer at 95% level of confidence, increasing by 0.007 with every extra month of smoking. A relatively lesser impact of smoking maybe due to the indirect and relatively shorter duration of contact with tobacco in the oral cavity in comparison to the habit of tobacco chewing. Alcohol duration related negatively with oral cancer and leukoplakia, decreasing by 0.01 for oral cancer and leukoplakia with every extra month of the alcohol habit; however, the mechanism of the same remains beyond understanding. It is possible that smoking and alcohol are greater risk factors in the presence of other habits such as chewing tobacco/pan masala but do not seriously affect the risk of oral lesions by themselves. None of the variables related with lichen planus, indicating that other factors could be responsible for this disorder.
The risk of oral cancer, leukoplakia, and lichen planus did not differ between literate and illiterate people; however, being illiterate decreased the risk of developing OSF (RR = 0.49). We had believed that illiterate people maybe more addicted and at a higher risk; however, the data shows that there is a very high frequency of educated chewers who are at an equal risk. We had also believed that economically poor people maybe at an increased risk due to lesser awareness. However, the figures were very surprising as the risk of oral cancer and lichen planus did not differ between individuals belonging to lower and middle income groups, and surprisingly the lower income group was at a lesser risk of developing OSF (RR = 0.40) and leukoplakia (RR = 0.49). Similarly, the individuals belonging to the rural locality were at a decreased risk of oral cancer (RR = 0.64), OSF (RR = 0.33), and leukoplakia (RR = 0.40). All the above factors taken together indicate that education and urbanization have not significantly reduced the use of these products and the risk associated. The effect of locality and economic status on other factors could be due to their strong association with education status.
According to the Centre for Disease Control and Prevention (CDC), chewing tobacco 78 times a day may be equivalent to smoking 30-40 cigarettes per day. An increased incidence of squamous cell (oral cancer) and verrucous carcinomas of the oral cavity and pharynx has been found in patients who are used to chewing tobacco.[15,16] Sawyer et al.(1992) also reported an increased risk with increase in the frequency and duration of the habit.[17] Though the nicotine content of chewing tobacco is lower than that in the smoking form, it is said to have an increased carcinogenic potential because it remains in contact with the oral mucosa for longer periods of time.[17] Tobacco-specific N-nitrosamines, present in higher concentrations in smokeless tobacco, are readily extracted by saliva; the absorption is further enhanced in alkaline environments.[18,19] These factors are known to influence the formation and yields/levels of toxic chemicals in tobacco chewers and smokers.[20] Tobacco contains N-nitroso compounds, well-known carcinogens, which play a key role in the malignant transformation in the oral cavity.[21]
In a nutshell, our results show that the habit of chewing tobacco/pan masala is a very strong risk factor for oral cancer and related lesions. It is not only the duration for which one had been consuming, the number of times one consumes everyday is also strongly related with oral cancer and related lesions. It maybe merely a false impression that educated people chew less and are at a lesser risk. The percentage of chewers does not differ much between illiterates and literates, and the habit was less of a risk factor in the rural or economically poor people. A very strong correlation of tobacco/pan masala chewing with OSF explains a very high incidence of this precancerous lesion in this part of the country. A more serious threat is the introduction of several new mixtures of chewing tobacco/pan masala which are increasing by the day. Often, these mixtures have more than one kind of hazardous content mixed in them, which may result in the exposure to several different toxic substances at the same time, making it the most dangerous form of the habit. We need to review the policies governing the contents, sale, and use of these mixtures, and to educate the educated and uneducated people about the hazardous effects these habits may have.
CONCLUSION
Oral malignancies continue to burden the clinical and economic dimensions of health care around the world. The Indian subcontinent accounts for one-third of the world burden.
Use of tobacco use and alcohol are known risk factors for cancers of the oral cavity. In India, 57% of all men and 11% of women between 15 and 49 years of age use some form of tobacco. About 800,000 deaths occur every year in India directly as a result of cardiovascular diseases, chronic obstructive lung diseases, and tobacco-related cancers.[22] If current smoking patterns persist, tobacco is set to cause about one-third of all deaths. Use of tobacco continues to have a personal impact on individuals as well as having an impact on public health. Hence, the reason that cancers of the oral cavity occupy a strategic position in the health-care systems is that an early detection of these lesions is theoretically possible and practically useful. Such early detection is generally associated with a high expectation of the prevention of deformity, relapse, and mortality.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gupta PC, Ray CS. Smokeless tobacco and health in India and South Asia. Respirology. 2003;8:419–31. doi: 10.1046/j.1440-1843.2003.00507.x. [DOI] [PubMed] [Google Scholar]
- 2.Hamada GS, Bos AJ, Kasuga H, Hirayama T. Comparative epidemiology of oral cancer in Brazil and India. Tokai J Exp Clin Med. 1991;16:63–72. [PubMed] [Google Scholar]
- 3.Khandekar SP, Bagdey PS, Tiwari RR. Oral Cancer and Some Epidemiological Factors: A Hospital Based Study. Ind J Comm Med. 2006;31:157–9. [Google Scholar]
- 4.Hebert JR, Gupta PC, Bhonsle RB, Mehta H, Zheng W, Sanderson M, et al. Dietary exposures and oral precancerous lesions in Srikakulam District, Andhra Pradesh, India. Public Health Nutr. 2002;5:303–12. doi: 10.1079/PHN2002249. [DOI] [PubMed] [Google Scholar]
- 5.Murti PR, Bhonsle RB, Pindborg JJ, Daftary DK, Gupta PC, Mehta FS. Malignant transformation rate in oral submucous fibrosis over a 17 year period. Community Dent Oral Epidemiol. 1985;13:340–1. doi: 10.1111/j.1600-0528.1985.tb00468.x. [DOI] [PubMed] [Google Scholar]
- 6.Pindborg JJ, Murti PR, Bhonsle RB, Gupta PC, Daftary DK, Mehta FS. Oral submucous fibrosis as a precancerous condition. Scand J Dent Res. 1984;92:224–9. doi: 10.1111/j.1600-0722.1984.tb00883.x. [DOI] [PubMed] [Google Scholar]
- 7.Mehta FS, Gupta PC, Daftary DK, Pindborg JJ, Choksi SK. An epidemiological study of oral cancer and precancerous condition among 101,761 villagers in Maharashtra, India. Int J Cancer. 1972;10:134–41. doi: 10.1002/ijc.2910100118. [DOI] [PubMed] [Google Scholar]
- 8.Pindborg JJ, Chawla TN, Mishra RK, Nagpaul RK, Gupta VK. Frequency of oral carcinoma, leukoplakia, leukokeratosis, leukoedema, sub mucous fibrosis and lichen planus in 10,000 Indians in Lucknow, Uttar Pradesh India; Preliminary Report. J Dent Res. 1965;44:61. doi: 10.1177/00220345650440032901. [DOI] [PubMed] [Google Scholar]
- 9.Pindborg JJ, Mehta FS, Gupta PC, Daftary DK. Prevalence of Oral sub mucous Fibrosis among 50,915 Indian villagers. Br J Cancer. 1968;22:646–54. doi: 10.1038/bjc.1968.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta PC, Sinor PN, Bhonsle RB, Pawar VS, Mehta HC. Oral Sub mucous Fibrosis in India: A new epidemic? Natl Med J Ind. 1998;11:113–6. [PubMed] [Google Scholar]
- 11.Gupta PC, Ray CS. Tobacco and youth in the South East Asian region. Indian J Cancer. 2002;39:1–33. [PubMed] [Google Scholar]
- 12.Saran S, Agrawal GN. Cancer pattern in Central U.P. Indian J Cancer. 1984;21:133–6. [PubMed] [Google Scholar]
- 13.Wakefield M, Morley C, Horan JK, Cummings KM. The cigarette pack as image: New evidence from tobacco industry documents. Tob Control. 2002;11(Supp l):173–80. doi: 10.1136/tc.11.suppl_1.i73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehrotra R, Singh M, Kumar D, Pandey AN, Gupta RK, Sinha US. Age specific incidence rate and pathological spectrum of oral cancer in Allahabad. Indian J Med Sci. 2003;57:400–4. [PubMed] [Google Scholar]
- 15.Fant RV, Henningfield JE, Nelson RA, Pickworth WB. Pharmacokinetics and pharmacodynamics of moist snuff in humans. Tob Control. 1999;8:387–92. doi: 10.1136/tc.8.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah N, Sharma PP. Role of chewing and smoking habits in the etiology of oral submucous fibrosis: A case control study. J Oral Pathol Med. 1998;27:475–9. doi: 10.1111/j.1600-0714.1998.tb01915.x. [DOI] [PubMed] [Google Scholar]
- 17.Sawyer DR, Wood NK. Oral cancer: Etiology, recognition and management. Dent Clin North Am. 1992;36:919–44. [PubMed] [Google Scholar]
- 18.Main JH, Lecavalier DR. Smokeless tobacco and oral disease: A review. J Can Dent Assoc. 1988;54:586–91. [PubMed] [Google Scholar]
- 19.Lindqvist R, Lendahls L, Tollbom O, Aberg H, Håkansson A. Smoking during Pregnancy: Comparison of self-reports and cotinine levels in 496 women. Acta Obstet Gynecol Scand. 2002;81:240–4. doi: 10.1034/j.1600-0412.2002.810309.x. [DOI] [PubMed] [Google Scholar]
- 20.Maher R, Lee AJ, Warnakulasuriya KA, Lewis JA, Johnson NW. Role of areca nut in the causation of oral submucous fibrosis: A case control study in Pakistan. J Oral Pathol Med. 1994;23:65–9. doi: 10.1111/j.1600-0714.1994.tb00258.x. [DOI] [PubMed] [Google Scholar]
- 21.Patel BP, Rawal UM, Shah PM, Prajapati JA, Rawal RM, Dave TK, et al. Study of tobacco habits and alterations in Patel enzymatic antioxidant system in oral cancer. Oncology. 2005;68:511–9. doi: 10.1159/000086995. [DOI] [PubMed] [Google Scholar]
- 22.Sankaranarayan R, Masuyer E, Swaminathan R, Ferley J, Whelan S. Head and neck cancer: A global perspective on epidemiology and prognosis. Anticancer Res. 1998;18:4779–86. [PubMed] [Google Scholar]


