Abstract
Lipomas represent about 1 to 5% of all neoplasms of the oral cavity most commonly presenting as painless, mobile, soft, round mass. Angiolipoma, spindle cell lipoma, mylelolipoma, chondrolipoma and myxolipoma are histological variants of lipoma arising from fat tissues. Although the angiolipoma is the most common tumour in the trunk and the extrimities of young people, it occurs infrequently in the head and neck region. In this article we present clinical, radiological and histological features of a cellular infiltrative angiolipoma exicised from the buccal mucosa of a 9 months old female child.
Keywords: Cheek, infiltrative angiolipoma, lipoma
INTRODUCTION
Lipomas are the most common neoplasms arising from fat tissue. They are usually slow-growing, soft, and asymptomatic masses. Around 13% of all lipomas occur in the head and neck region, including cheek,[1,2,3,4] tongue,[5] palate,[6] parotid gland,[7] neck,[8] and larynx.[9] Lipomas are subclassified into different histological subtypes based on the appearance of the associated stroma. Angiolipoma, spindle cell lipoma, myelolipoma, chondrolipoma, and myxolipoma are some of the histological variants of lipoma reported in literature.[10] Although angiolipoma is the most common tumor in the trunk and the extremities of young people, it occurs infrequently in the head and neck region.[11]
In this case report, we present the clinical, radiological, and histological features of cellular infiltrative angiolipoma involving the buccal mucosa of an infant.
CASE REPORT
A 9-month-old female patient was brought to the Department of Oral and Maxillofacial Surgery in Buddha Institute of Dental Sciences and Hospital with complaints of a growth in the right posterior cheek region of the patient. The growth was noticed accidentally by the parents 20 days back. Clinical examination revealed a 1.5 × 1 cm soft, mobile, pedunculated mass involving the buccal mucosa adjacent to the upper right posterior alveolus [Figure 1]. The lesion was non-tender on palpation and showed no fixity to the overlying skin.
Figure 1.

Pre-op view
Contrast-enhanced computed tomography (CT) scan was suggestive of 1.7 cm, heterogeneously enhancing, fairly well marginated mixed density (predominantly hypodense) lesion on the right side of the oral cavity extending into the buccal space without underlying bony erosion or destruction [Figure 2].
Figure 2.

CT face with contrast showing the lesion
Under general anesthesia, the mass was excised through an intraoral approach and was sent for histopathologic evaluation [Figure 3].
Figure 3.
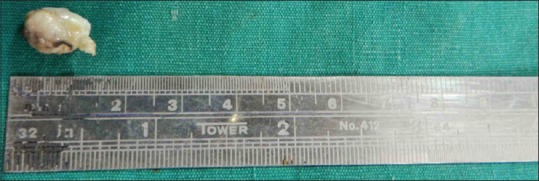
Excised tumor
H and E stained sections revealed superficial parakeratinized stratified squamous epithelium with moderate hyperplasia and intact basement membrane. The lamina propria showed well-delineated lobules of fat cells separated by anastomosing septae composed of loose fibrous connective tissue. Numerous endothelial lined spaces of varying sizes were also noted [Figure 4]. This overall histological feature were diagnostic of cellular infiltrative angiolipoma.
Figure 4.
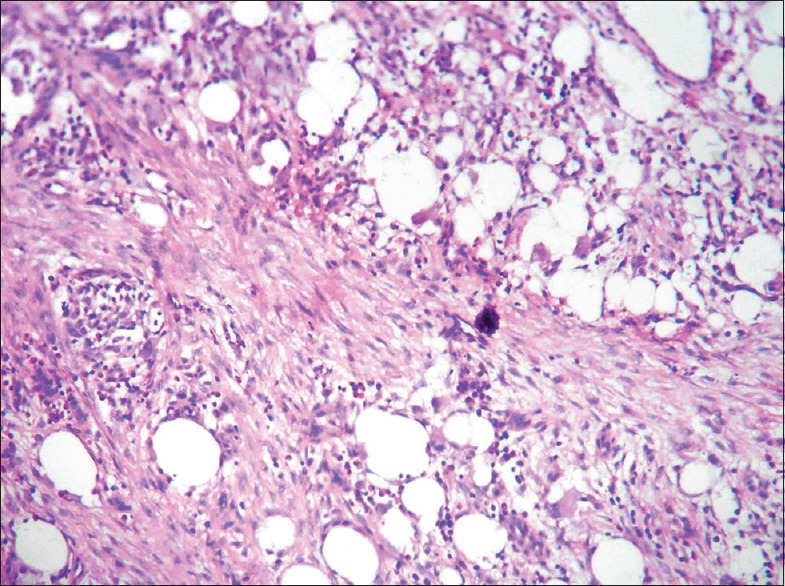
H and E stained section showing features of angiolipoma
The recovery period was uneventful. The patient is currently under follow-up for the last 1½ years with no evidence of recurrence till date [Figure 5].
Figure 5.

Post-op view
DISCUSSION
Although lipomas are the most common soft-tissue tumors originating from the subcutaneous regions of the back, shoulder, and neck, the head and neck region is a rare site of origin. They represent about 1–5% of all neoplasms of the oral cavity and usually present as painless, soft, round, and mobile masses.
Angiolipoma is a variant of lipoma, with a prominent vascular component, constituting only 6–17% of all lipomas.[12,13] It was first described as a distinct entity by Bowen in 1912.[14] Based on studies by Gonzales-Crussi et al.,[15] angiolipoma has two histological types: Infiltrating and non-infiltrating. Non-infiltrating angiolipomas are encapsulated, and their size may vary from 1 to 4 cm. Non-infiltrating angiolipomas tend to be located on the forearms, upper arms, thighs, and anterior abdominal wall, and are more common in males than in females.
Infiltrating angiolipomas are non-capsulated tumors extending into surrounding tissues.[16] They are usually diagnosed in older patients. We reviewed the literature and to the best of our knowledge, this is the first reported case of infiltrating angiolipoma in an infant involving the buccal mucosa.
Infiltrating angiolipomas have two anatomical forms: Intermuscular and intramuscular.[3,8,17,18] Documented sites of occurrence of infiltrating angiolipoma in the head and neck are cheek, palate, neck, jaw, nose, eyelid, parotid, tongue, paranasal sinuses, and parapharynx.[4,19,20,21]
History of trauma, lipomatous differentiation by hormones during puberty, fatty degeneration of a central hemangioma, and vascular proliferation of a congenital lipoma (congenital origin) have been implicated as possible etiological factors.[8,17,18]
Angiolipomas usually present as painful or tender subcutaneous masses in young adults. Infiltrating angiolipomas can also lead to muscular pain and neural deficits.[4,12,13]
Histopathologic characteristics of angiolipomas are as follows: (1) gross evidence of tumor formation with or without a capsule; (2) microscopic evidence of 50% mature lipocytes in the tumor; and (3) microscopic evidence of angiomatous proliferation in the tumor. Although infiltrating angiolipomas are histologically similar to non-infiltrating type (proliferation of blood vessels and lipocytes), they have no identifiable capsule and there may be pleomorphism, atypia, or mitotic figures.[4,12,13]
Differential diagnosis includes hemangioma, lymphangioma, lipoma, Kaposi's sarcoma, leiomyoma, neurilemmoma, and angiosarcoma. Liposarcomas can be differentiated by the presence of embryonal adipose tissue, pleomorphism, increased number of mitosis, and metastasis. Lipomas have no predominant vascular component.[4] Presence of phleboliths in CT, pulsations, and fluctuations are helpful to rule out hemangioma. However, histopathologic evaluation is required for exclusion of leiomyoma and neurilemmoma.[22] Kaposi's sarcoma is a vascular malignancy, while lipoma is an adipose mesenchymal neoplasm. Clinically, Kaposi's sarcoma occurs as ulcerative exophytic reddish lesion, and palate, gingiva, and tongue are the most common locations.[10]
There is no evidence that angiolipomas undergo malignant transformation due to lack of atypia, pleomorphism, or mitotic figures in angiomatous or adipose tissues.[23]
Angiolipomas appears as homogenous low-intensity areas of no contrast enhancement and heterogeneous areas of extremely high enhancement. These tumors tend to show high signal intensity on T1-weighted sequences and T2-weighted fast spin echo magnetic resonance imaging (MRI) sequences. MRI is the most sensitive imaging study for excluding invasion of the neighboring structures and evaluating the resectability of the tumor.[4,20]
Treatment of angiolipomas is complete surgical excision for both infiltrating and non-infiltrating types. The infiltrating type can create difficulty in excision and, as such, the recurrence rate is high. In cases of inadequate resection, radiation therapy may be necessary.[13] Successful treatment of a giant infiltrating angiolipoma with interferon alpha also has been reported.[24] Carbon dioxide laser and liposuction may be alternative options for treatment of single and multiple angiolipomas.[9,16,23,25]
CONCLUSION
Angiolipomas are rarely seen in the head and neck region. MRI is the most sensitive imaging study. Complete surgical excision with a clear surgical margin is the treatment of choice.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Campos GM, Grandini SA, Lopes RA. Angiolipoma of the cheek. Int J Oral Surg. 1980;9:486–90. doi: 10.1016/s0300-9785(80)80082-2. [DOI] [PubMed] [Google Scholar]
- 2.Sánchez Aniceto G, Salván Saez R, García Peńin A. Angiolipoma of the cheek: Report of a case. J Oral Maxillofac Surg. 1990;48:512–5. doi: 10.1016/0278-2391(90)90243-u. [DOI] [PubMed] [Google Scholar]
- 3.Ali MH, el-Zuebi F. Angiolipoma of the cheek: Report of a case. J Oral Maxillofac Surg. 1996;54:213–5. doi: 10.1016/s0278-2391(96)90450-4. [DOI] [PubMed] [Google Scholar]
- 4.Alvi A, Garner C, Thomas W. Angiolipoma of the head and neck. J Otolaryngol. 1998;27:100–3. [PubMed] [Google Scholar]
- 5.Brahney CP, Aria AA, Koval MH, Najjar TA. Angiolipoma of the tongue: Report of case and review of literature. J Oral Surg. 1981;39:451–3. [PubMed] [Google Scholar]
- 6.Flaggert JJ, III, Heldt LV, Keaton WM. Angiolipoma of the palate. Report of a case. Oral Surg Oral Med Oral Pathol. 1986;61:333–6. doi: 10.1016/0030-4220(86)90412-3. [DOI] [PubMed] [Google Scholar]
- 7.Reilly JS, Kelly DR, Royal SA. Angiolipoma of the parotid: Case report and review. Laryngoscope. 1988;98:818–21. doi: 10.1288/00005537-198808000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Saydam L, Bozkurt MK, Ugur MB, Ozcelik T, Kutluay L. Angiolipoma of the neck: A case report. Ear Nose Throat J. 2005;84:375–7. [PubMed] [Google Scholar]
- 9.Mesollela M, Di Martino M, Laguardia M, Galera F, Galli V. Angiolipoma of the larynx. Otolaryngol Head Neck Surg. 2007;136:142–3. doi: 10.1016/j.otohns.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Williams TP, Stewart JC. Soft tissue cysts and benign neoplasms. In: Fonseca RJ, editor. Oral and Maxillofacial Surgery. Philadelphia: WB Saunders; 2000. pp. 127–51. [Google Scholar]
- 11.Altug HA, Sahin S, Sencimen M, Dogan N, Erdogan O. Non-infiltrating angiolipoma of the cheek: A case report and review of the literature. J Oral Sci. 2009;51:137–9. doi: 10.2334/josnusd.51.137. [DOI] [PubMed] [Google Scholar]
- 12.Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 1960;82:924–31. doi: 10.1001/archderm.1960.01580060078011. [DOI] [PubMed] [Google Scholar]
- 13.Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974;34:720–7. doi: 10.1002/1097-0142(197409)34:3<720::aid-cncr2820340331>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 14.Bowen JT. Multiple subcutaneous hemangiomas, together with multiple lipomas, occurring in enormous numbers in an otherwise healthy, muscular subject. Am J Med Sci. 1912;144:189–92. [Google Scholar]
- 15.Gonzales-Crussi F, Enneking WF, Arean VM. Infiltrating angiolipoma. J Bone Joint Surg Am. 1966;48:1111–24. [PubMed] [Google Scholar]
- 16.Kanter WR, Wolfort FG. Multiple familial angiolipomatosis: Treatment of liposuction. Ann Plast Surg. 1988;20:277–9. doi: 10.1097/00000637-198803000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Enzinger FM, Weiss SW. Benign lipomatous tumours. In: Enzinger FM, Weiss SW, editors. Soft Tissue Tumours. 3rd ed. St Louis: CV Mosby; 1995. pp. 381–2. [Google Scholar]
- 18.El-Monem MH, Gaafar AH, Magdy EA. Lipomas of the head and neck: Presentation variability and diagnostic work-up. J Laryngol Otol. 2006;120:47–55. doi: 10.1017/S0022215105004597. [DOI] [PubMed] [Google Scholar]
- 19.Pfannenstiel TJ, Boseley M, Roach L. A case of paranasal sinus angiolipoma. Laryngoscope. 2003;113:1080–1. doi: 10.1097/00005537-200306000-00031. [DOI] [PubMed] [Google Scholar]
- 20.Alobid I, Benítez P, Berenguer J, Bernal-Sprekelsen M, Mullol J. Parapharyngeal angiolipoma causing obstructive sleep apnoea syndrome. Acta Otolaryngol. 2004;124:210–2. doi: 10.1080/00016480310015722. [DOI] [PubMed] [Google Scholar]
- 21.Reilly JS, Kelly DR, Royal SA. Angiolipoma of the parotid: Case report and review. Laryngoscope. 1988;98:818–21. doi: 10.1288/00005537-198808000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Altuğ HA, Büyüksoy V, Okçu KM, Doğan N. Hemangiomas of the head and neck with phleboliths: Clinical features, diagnostic imaging, and treatment of three cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e60–4. doi: 10.1016/j.tripleo.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Hamakawa H, Hino H, Sumida T, Tanioka H. Infiltrating angiolipoma of the cheek: A case report and a review of the literature. J Oral Maxillofac Surg. 2000;58:674–7. doi: 10.1016/s0278-2391(00)90166-6. [DOI] [PubMed] [Google Scholar]
- 24.Akyüz C, Emir S, Büyükpamukçu M, Büyükpamukçu N, Cağlar M, Kale G, et al. Successful treatment with interferon alfa in infiltrating angiolipoma: A case presenting with Kasabach-Merritt syndrome. Arch Dis Child. 2003;88:67–8. doi: 10.1136/adc.88.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaneko T, Tokushige H, Kimura N, Moriya S, Toda K. The treatment of multiple angiolipomas by liposuction surgery. J Dermatol Surg Oncol. 1994;20:690–2. doi: 10.1111/j.1524-4725.1994.tb00455.x. [DOI] [PubMed] [Google Scholar]


