Abstract
Penetrating facial injuries are potentially dangerous and require emergency management because of the presence of vital structures in the face and it may be life threatening especially when the injury involves airway, major blood vessels, spinal cord and cervical spines. Penetrating injuries of facial region can occur due to missile injuries, blast injuries, accidental fall on sharp objects such as sticks or glass and motor vehicle accidents etc., Indications for immediate surgical management of penetrating neck injuries include airway management and hemodynamic instability according to advanced trauma life support protocol.
Keywords: Facial injury, foreign body, wooden log, management
INTRODUCTION
Facial and neck injuries carry high risk of morbidity and mortality. The severity depends on factors including massive blood loss due to injury to the major blood vessels namely the carotid arteries and jugular veins, upper airway obstruction which can be due to edema, hematoma or emphysema that might compress the airway. The penetrating foreign body in the neck has a special apprehension because of the constellations of vital structures in the neck.[1] Early wound exploration and proper wound debridement with adequate antimicrobial coverage are the prime factors in curtailing morbidity and mortality. Irrespective of these problems, the overall mortality is relatively low, ranging from 0% to 11%.[2]
History
Penetrating facial and neck trauma has been a significant cause of injury and death for centuries. In the 16th century, Ambrose Paré performed the first documented surgical intervention for a traumatic cervical injury when he ligated the lacerated carotid artery and jugular vein of a wounded French soldier. Mandatory exploration of all wounds deep to the platysma was developed and widely practiced by military surgeons during World War II, and this practice may explain the decreased mortality rates associated with these injuries. In 1956, a landmark study by Fogelman and Stewart revealed a mortality rate was 6% in patients who underwent immediate surgical exploration and 35% mortality rate in patients who either underwent exploration in a delayed fashion or were not treated surgically.[3]
CASE REPORT
A 30 years old male patient was brought to Oral and Maxillofacial surgery casualty of Medical College Kottayam with a penetrating facial injury by a wooden log passing through the left lateral side of his face below the angle of mandible and protruding through oral cavity causing comminuted fracture of mandible after a road traffic accident. There was moderate bleeding and respiratory distress. No history of vomiting or loss of consciousness. From the history it was noted that the wooden branch was initially of length of 8 feet. In the local hospital the wooden log shortened out up to 2 feet and was then referred to Medical College Kottayam.
At the time of admission the patient complained of dyspnea and dysphasia. On examination there was significant oronasopharyngeal bleeding with no neurological deficit. Moderate trickling of blood from the entry site was noted. The blood pressure was 140/90 mmHg and the pulse rate was 110/min. The wooden log was seen protruding through his mouth [Figure 1]. The management of the patient was done by following the advanced trauma life support (ATLS) guidelines established by the American College of Surgeons, which begins with a rapid assessment of the airway, breathing, and circulation.[4] Airway management in such a patient with penetrating injury to the neck was challenging. The patient was unable to lie in supine position due to long wooden log stuck behind the neck. There was high chance of aspiration of blood and saliva. The patient was planned for tracheostomy to secure airway, since the patient was unable to lie down in the supine position due to obstruction of wooden log posteriorly. Therefore the wooden log was shortened out near close proximity to the left retromandibular region [Figure 2]. The patient was then positioned on right lateral and tracheotomy was performed under sedation and local anesthesia. General anesthesia was then administered through the tracheostome [Figure 3]. With the airway secured, breathing and circulation were evaluated and managed in the standard manner, following the ATLS protocol. The secondary survey was conducted after the patient was initially stabilized. There were no other associated injuries.
Figure 1.

Front view of patient
Figure 2.

Wooden log shortened out in right lateral position
Figure 3.

Airway secure through tracheostomy
Surgical procedure
A midline lip-split incision was given till the anterior extension of the penetrating wound. Exploration was performed through existing mandibular symphysis fracture. Comminuted fracture of left body of mandible and symphysis were identified. Access was gained by swinging the mandible through the fracture symphysis [Figure 4].
Figure 4.
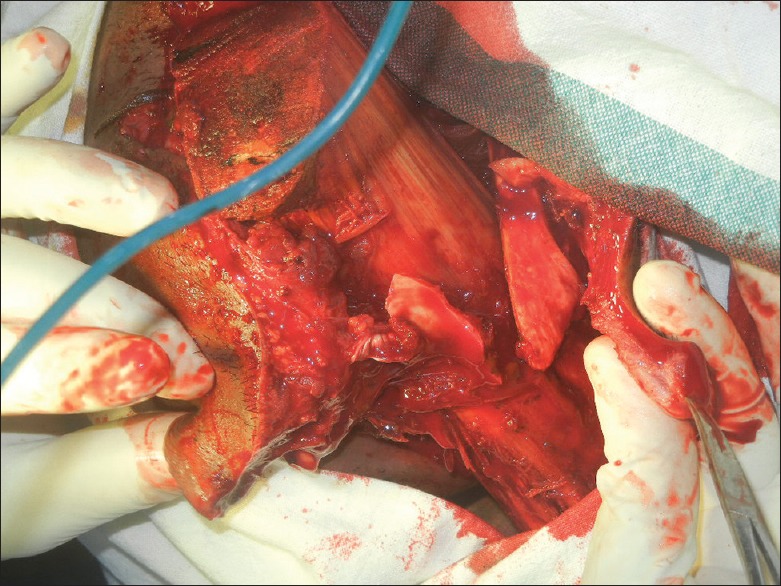
Access through mandibular swing
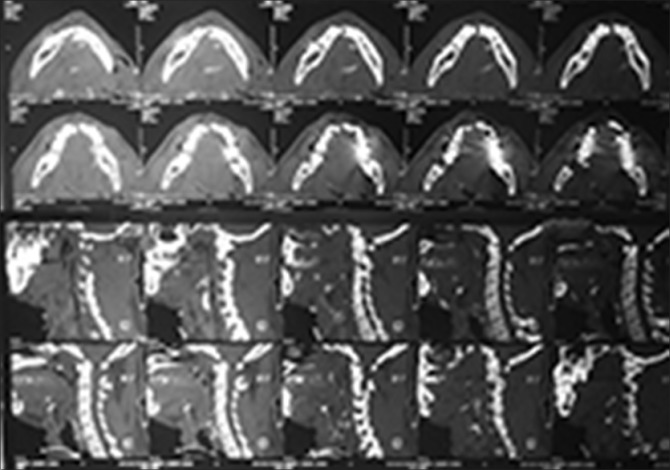
After adequate exposure the wooden log was removed in toto [Figure 5]. Lingual and facial artery were identified and ligated with 2-0 silk. No other foreign body was seen. Hemostasis was achieved and the area cleaned with betadine saline wash. There were no injury to great vessels and nerves of neck. Reduction and fixation of fracture mandible was done by stainless steel mini pates and screws [Figure 6]. Wound was then closed in layers after securing the suction drain. Post-operative CT scan of head and neck was advised to rule out head injury, cervical spine injury, other maxillofacial injury if any and foreign body. CT scan revealed that there were no associated head injury, cervical spine injury, maxillofacial injury and any other foreign body [Figure 7].
Figure 5.

Removal of wooden log
Figure 6.
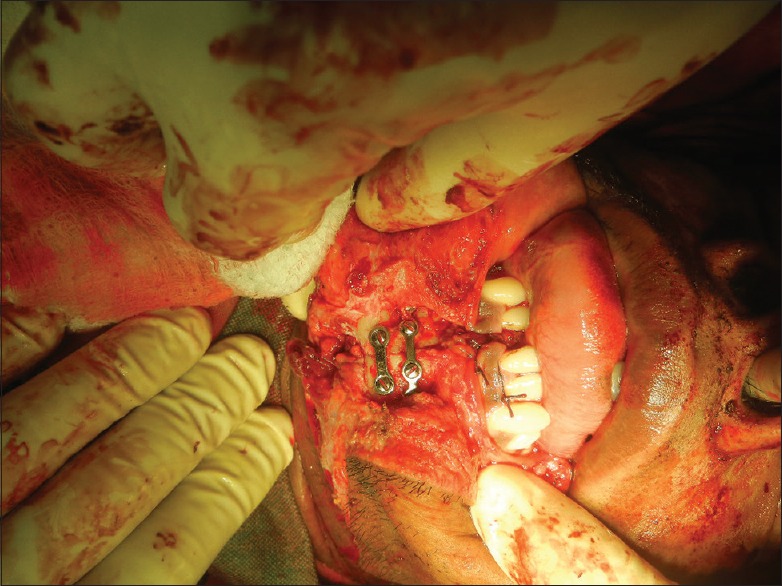
Reduction & fixation of mandible
Figure 7.
Post operative CT Mandible & C-spine
Post operative evaluation showed no injury to facial and lingual nerve. The patient had an uneventful postoperative period and was discharged on the 10th day with tracheostomy tube removed. He was followed up regularly. Review after 1 month [Figure 8] showed no functional or major aesthetic problems.
Figure 8.

Post operative facial photograph of patient
DISCUSSION
Penetrating injuries of the face and neck though uncommon are potentially life threatening entity. Many cases of penetrating neck injuries that required massive surgical intervention and repair have been reported. Initial clinical presentations sometimes may not reflect the true injury that has occurred internally. A clinically superficial looking minor stab wound can have vascular or aerodigestive injury when the wound is explored.[5]
Classification of penetrating neck injuries according to Monson's criteria is a useful tool in the evaluation and treatment of penetrating neck injuries. Accordingly the lateral neck is divided into three zones:
Zone 1 extends from the clavicle to the cricoid cartilage and includes the thoracic inlet. This region contains the major vascular structures like the subclavian artery and vein, jugular vein, and common carotid artery, as well as the esophagus, thyroid, and trachea
Zone 2 extends from the cricoid to the angle of the mandible and contains the common carotid artery, internal and external carotid arteries, jugular vein, larynx, hypopharynx, and cranial nerves X, XI, and XII
Zone 3 is a small but critical area extending from the angle of the mandible to the skull base. This region contains the internal and external carotid arteries, jugular vein, lateral pharynx, and cranial nerves VII, IX, X, XI, and XII.
In the present case, the injury was on the left side in the zone 3, which has made the great vessels namely the carotid artery and jugular vein at risk. The penetrating injuries of the face and neck with such a wooden log pose a diagnostic and therapeutic dilemma. Thorough knowledge of the anatomy of the neck, physical assessment and current recommendations for diagnostic and therapeutic interventions are necessary for appropriate management.[6]
CONCLUSION
Penetrating wooden log in the facial region is an uncommon but potentially life-threatening condition. An unusual case of penetrating injury of the face and neck is presented. Diversities in the management protocol with a changing technique compel the clinician to perform a close evaluation of the patient.[7] Each maneuvre should be directed to minimize mortality and morbidity by means of timely intervention. In cases of penetrating facial injuries, observing the ATLS protocol and early exploration reduces the mortality and resulting in a favorable outcome [Figure 8].
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Hunter TB, Taljanovic MS. Foreign bodies. Radiographics. 2003;23:731–57. doi: 10.1148/rg.233025137. [DOI] [PubMed] [Google Scholar]
- 2.Nason RW, Assuras GN, Gray PR, Lipschitz J, Burns CM. Penetrating neck injuries: Analysis of experiences from a Canadian trauma centre. Can J Surg. 2001;44:122–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Fogelman MJ, Stewart RD. Penetrating wounds of the neck. Am J Surg. 1956;91:581–96. doi: 10.1016/0002-9610(56)90289-6. [DOI] [PubMed] [Google Scholar]
- 4.Marshal LF, Knowlton S, Garfin SR. 7th ed. Chicago: American College of Surgeons; 2004. American College of Surgeons Committee on Trauma Advanced Trauma Life Support Program for Doctors; p. 517. [Google Scholar]
- 5.Nabeel A, Irfan M. Near fatal fall complicated by penetrating neck injury with uneventful outcome: A case report. Bangladesh J Med Sci. 2011;10:125–8. [Google Scholar]
- 6.Singh RK, Bhandary S, Karki P. Managing a wooden foreign body in the neck. J Emerg Trauma Shock. 2009;2:191–5. doi: 10.4103/0974-2700.55340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agrawal R, Timilsina DS, Reddy NS, Ganguly SN, Tayal A. Penetrating foreign body neck: A case report. Kathmandu Univ Med J (KUMJ) 2007;5:414–6. [PubMed] [Google Scholar]