Abstract
Objective
The aim of this investigation was to assess the relationships between suicidal ideation and insomnia symptoms in Veterans misusing alcohol.
Method
Data were extracted in this retrospective chart review of Veterans referred from primary care for a behavioral health evaluation (N = 161) based on evidence of heavy drinking, drug use or another behavioral problem. Suicidal ideation (SI) was assessed using the Paykel questionnaire. Insomnia symptoms were assessed with standard diary questions in an interview format and pertained to sleep latency (SL), wake after sleep onset time (WASO), sleep quality (SQ), and habitual sleep duration (HSD). The relations between suicidal ideation and insomnia symptoms were assessed using ordinal regression analyses adjusted for socio-demographic, psychiatric and addiction-related variables.
Results
Suicidal ideation was reported in 62 (39%) of the Veterans interviewed. In a multivariable model, only inadequate SQ was associated with suicidal ideation. Short sleepers were more likely to endorse suicidal ideation and have attempted suicide in the past year. In addition, older age, inadequate financial status, and the presence of a psychiatric disorder were also significantly associated with suicidal ideation in most of the adjusted models.
Conclusion
Given their association with suicidal ideation, insomnia symptoms in Veterans misusing alcohol should prompt an assessment of underlying psychiatric and social factors.
Keywords: Veterans, Suicidal ideation, Insomnia, Sleep duration, Alcohol
1. Introduction
On average, 22 Veterans died from suicide each day during the calendar year 2010, according to recent statistics from the Department of Veterans Affairs (Kemp & Bosarte, 2012). Suicide is the tenth leading cause of death nationally (Heron, 2012). Factors associated with a higher risk of suicide in Veterans include the use of alcohol and other drugs, the presence of an underlying psychiatric disorder, and being 50–59 years old, male, White, non-Hispanic, and either married or separated (Kemp & Bosarte, 2012; Kim et al., 2012; Ribeiro et al., 2012; Roy, Lamparski, DeJong, Moore, & Linnoila, 1990).
A behavioral health factor commonly associated with suicidal risk is alcohol misuse. Because alcohol misuse is common in Veterans, with recent estimates ranging from 25 to 27% (Bradley et al., 2006; Santiago et al., 2010), its impact on suicidal risk in this population is potentially important. In a retrospective study of 324 Veterans being treated for depression and who subsequently committed suicide, alcohol abuse or dependence was a significant risk factor (Kim et al., 2012). In a large study of Norwegian conscripts with a 40-year follow-up, alcohol abuse was significantly associated with suicide, especially for those in the middle age category (more than 40 years old), as compared to the younger age group (Rossow & Amundsen, 1995). Data from a large cohort of Swedish conscripts also showed that alcohol abusers were at increased risk for attempting and completing suicide (Rossow, Romelsjo, & Leifman, 1999). Greater alcohol consumption, a higher prevalence of psychiatric and other drug use disorders, and lower socioeconomic status also have been correlated with suicidal behavior in alcohol dependent patients (Driessen et al., 1998; Preuss et al., 2002; Roy et al., 1990; Scherrer et al., 2012).
Insomnia may also contribute to risk of suicidal behavior. Self-reported insomnia (difficulty initiating or maintaining sleep and/or the report of non-restorative sleep) has been associated with suicidal ideation in military personnel, even after adjusting for psychiatric symptoms and drug and alcohol abuse (Ribeiro et al., 2012). Other studies have also demonstrated a link between insomnia and suicidal ideation or completed suicide (Bjorngaard, Bjerkeset, Romundstad, & Gunnell, 2011; McCall et al., 2010). In one study, individuals who completed suicide exhibited greater insomnia in the week preceding the suicide than matched controls (Goldstein, Bridge, & Brent, 2008). Difficulty initiating sleep and difficulty maintaining sleep have been cited as predictors of suicidal ideation and planning, while difficulty maintaining sleep has been shown to be a significant predictor of suicide attempts (Wojnar et al., 2009). Although such data suggest that insomnia may be a risk factor for suicidal ideation, attempts, and/or completion, what remains unclear is the extent to which sleep loss (decrements in total sleep time or duration) mediates the observed effects between suicidal ideation and poor sleep continuity (i.e., increased sleep latency and wake after sleep onset time). This relationship seems especially important given the finding that short sleep duration is also associated with suicidal ideation (Blasco-Fontecilla et al., 2011; Goodwin & Marusic, 2008).
Insomnia has also been associated with alcohol misuse in prior studies (Ford & Kamerow, 1989; Foster & Peters, 1999). In a recent study of alcohol dependent Veterans, those who were actively drinking and using other drugs within the past year (as compared to those without other drug use) had higher insomnia symptoms (Chakravorty et al., 2013). Higher alcohol consumption and alcohol misuse have been associated with shorter sleep duration in young adults (Chaput, McNeil, Despres, Bouchard, & Tremblay, 2012; John, Meyer, Rumpf, & Hapke, 2005; Schuckit & Bernstein, 1981). Although alcohol misuse has been associated with both suicidal ideation and insomnia individually, the direct relationship between suicidal ideation and insomnia in this population is unclear. In a recent international study of treatment-seeking, alcohol-dependent patients in Poland, the presence of insomnia symptoms was associated with suicidal ideation even after adjustment for psychiatric symptoms (Klimkiewicz et al., 2012).
The present study examined the association of suicidal ideation with insomnia symptoms (sleep latency, wake after sleep onset time, and sleep quality), while also accounting for the impact of sleep duration in a group of Veterans who were misusing alcohol. We hypothesized that, after adjusting for socio-demographic, psychiatric, and addiction-related covariates, suicidal ideation would be associated with insomnia symptoms (sleep latency, wake after sleep onset time, and sleep quality) and extreme sleep duration (short and long).
2. Materials and methods
2.1. Referrals
The primary care providers within the Philadelphia Veterans Affairs Medical Center healthcare system (PVAMC) referred veterans for a behavioral health evaluation. The referrals were prompted by a positive screen for at-risk drinking (i.e., score >4 on the AUDIT-C) (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998), any other substance use disorder, or another behavioral health condition (e.g. depression, PTSD, anxiety). These referrals were assessed by health technicians at the Behavioral Health Laboratory (BHL) of the PVAMC using a battery of assessments.
2.2. Behavioral Health Laboratory (BHL)
The BHL is an integrated primary care/mental health care service at the PVAMC that provides comprehensive substance use and psychiatric assessments by technicians under the supervision of psychologists, nurses and a psychiatrist. The laboratory assessments included a telephonic interview consisting of socio-demographic and psychiatric measures (Oslin et al., 2006). The interview assesses information in the following domains: baseline demographic data, Mini International Neuropsychiatric Interview (MINI) modules for mood disorders, anxiety disorders, and alcohol abuse/dependence (Sheehan et al., 1998); Patient Health Questionnaire-9 item scale (PHQ-9) (Kroenke, Spitzer, & Williams, 2001), PTSD Check List (PCL) (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996), history of past episodes of depression, current antidepressant medications, alcohol consumption, smoking, use of illicit substances, 5-item Paykel Scale for suicidal ideation (Paykel, Myers, Lindenthal, & Tanner, 1974), Blessed, Tominson, & Roth, (1968) (Katzman et al., 1983), Short Form-12 item scale (SF-12) (Ware, Kossinski, & Keller, 1998), Work Limitation Questionnaire (Lerner et al., 2001), treatment satisfaction, insomnia, social support, bodily pain and diet. If, after further evaluation, the patient is deemed at risk to attempt suicide, appropriate procedures for urgent or emergent psychiatric care are activated (Chakravorty, et al, 2013).
2.3. Subjects
For this retrospective chart review, we extracted data from the charts of 161 patients who met criteria for hazardous drinking, or the DSM-IV criteria for an alcohol use disorder (i.e., alcohol abuse, or alcohol dependence), and who completed sleep-related assessments. The study was reviewed and approved by the Institutional Review Board at the PVAMC.
2.4. Measures
All of the sleep-related assessments were conducted between March 6, 2008 and July 7, 2008 as part of a pilot study of sleep parameters that included patients referred to the BHL.
The following socio-demographic characteristics were assessed: age, gender, race (White, Black, and other), ethnicity (Hispanic descent or not), relationship status (Single, Married/Partnered), vocational status (not working, part/full time employment), and financial status (“have at least enough to get by or more”, and “cannot make ends meet”).
Suicidal ideation (assessed using the 5-item Paykel Scale (Paykel et al., 1974)) over the last year was queried as follows: 1) “Has there been a time in the last year when you thought life was not worth living?” (Not worth living), 2) “Has there been a time in the last year that you wished you were dead, for instance you would go to sleep and not wake up?” (Wished was dead), 3) “Has there been a time in the last year that you thought of taking your own life, even if you would not really do it?”(Taking own life), 4) “Has there been a time in the last year when you reached a point where you seriously considered taking your own life or perhaps made plans about how you would go about doing it?” (thoughts/plans), and 5) “In the last year, have you made an attempt on your life?” (Attempt). Responses to each of the five questions were recorded as either a “yes” or a “no”.
Insomnia and habitual sleep duration
Sleep continuity disturbance was assessed during the interview with the following questions: “How long does it usually take you to fall asleep at night?” [sleep latency (SL)], and “How long are you usually awake during the middle of the night, after initially falling asleep?” [wake after sleep onset time (WASO)]. Both items were worded to reflect standard sleep diary items (Schutte-Rodin, Broch, Buysse, Dorsey, & Sateia, 2008) and were recorded in minutes, as used previously (Chakravorty et al., 2013). Sleep quality (SQ) was assessed with a single-item comprising the sleep quality subscale from the Pittsburgh Sleep Quality Index (PSQI) (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989). This question was asked: “During the past month, how would you rate your overall sleep quality?” Responses to the question included: “very good”, “fairly good”, “fairly bad”, and “very bad,” with scores ranging from 1 to 4, respectively. This item correlates highly (r = 0.83, p < 0.001) with the global PSQI score (Buysse et al., 1989). Because the responses to this question were skewed, for the purposes of this study, overall SQ was dichotomized as “good” or “poor.” Habitual Sleep Duration (HSD) was assessed with the question: “How many hours of sleep did you usually get at night?” The responses were recorded in hours, rounded up to the nearest whole number. This question was similar to that used in prior studies (John et al., 2005; Krueger & Friedman, 2009).
Alcohol use disorder was assessed using the modules for alcohol abuse and alcohol dependence over the past 12 months from the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998).
Drinking behavior was assessed as standard alcoholic drinks consumed over the last 7days, as well as the frequency of binge drinking days (≥5 standard drinks for men and ≥4 for women on a single day) prior to the interview using the Time Line Follow-Back method (Sobell, Sobell, Leo, & Cancilla, 1988).
Psychiatric status was assessed using several modules from the MINI (Sheehan et al., 1998), including those pertaining to lifetime mania, psychosis, and panic disorder; and generalized anxiety disorder over the past 6 months. Patients were considered to have depressive disorder if they scored ≥10 on the Patient Health Questionnaire 9-item scale (PHQ-9) (“Instruction Manual: Instructions for Patient Health Questionnaire (PHQ) and GAD-7 Measures”; Kroenke et al., 2001). Patients were diagnosed with Posttraumatic Stress Disorder (PTSD) if they scored ≥50 on the PTSD checklist (PCL) (Weathers, Litz, Herman, Huska, & Keane, 1993).
Smoking was assessed with the question: “Do you currently smoke?” The responses were recorded as either a “yes” or a “no.”
Other drug use was assessed by inquiring specifically about the frequency of use of cocaine, heroin, marijuana, speed, inhalants, LSD, barbiturates, and club drugs in the past year. We coded other drug use for the past year as “yes” or “no.”
Pain was assessed with the question: “Do you have daily pain or at least weekly episodes of pain?” The responses were recorded as either “yes” or “no.” A positive response to this question was followed-up with: “how long you have had this pain?” with the responses being categorized to less than a month, 1–3months, 3–6months, 6–12months, and over a year. For the purposes of analysis, however, the presence of pain is evaluated dichotomously.
2.5. Statistical analysis
The relationship of suicidal ideation with insomnia items and sleep duration was assessed using the ordinal regression models. The ordinal regression model (Polytomous Universal Model, PLUM) is an application of the generalized linear model. It is based on the assumption that there exists a latent continuous outcome variable, and ordering into groups of this underlying continuum as an ordinal outcome variable optimally captures the data. The thresholds or constants in the model depend only on which category’s probability is being predicted, and is unaffected by the values of the independent variable. The prediction part of the model is dependent on the predictors only, and is independent of the outcome category. Thus, the model predicts a function of these values using the link function rather than predicting the actual cumulative probabilities (McCullagh & Nelder, 1989; Norusis, 2004). This analysis yields coefficients that may be positive or negative. A positive value of the coefficient with an increasing value of a predictor or covariate indicates a higher probability of being in one of the higher outcome categories.
The dependent variable in the analyses was the Paykel Scale total score (Meneese & Yutrzenka, 1990), treated as an ordinal categorical variable ranging from 0 to 4, in order of increasing severity of suicidal ideation symptoms over the last year. The independent variables were SL, WASO, SQ, HSD and covariates which have been linked with suicidal ideation and sleep-related symptoms in prior studies. The covariates included age, race, ethnicity, sex, marital status, financial status, psychiatric status (assessed with the MINI, and dichotomized as any disorder present versus absent), alcohol consumption (number of alcohol binges in the last 3 months), smoking status, illicit drug use in the past year (any use versus no use), and pain (absence or presence of pain over the past week). We evaluated the relationship of the sleep (insomnia and HSD) variables with suicidal ideation initially in an unadjusted ordinal regression analyses. Next, a series of adjusted ordinal regression models were used to examine the relations between sleep variables with suicidal ideation, adjusting for socio-demographic, psychiatric and addiction-related covariates, to evaluate for the effects of the covariates in this relationship. In a final multivariable model, all of the sleep variables, as well as the socio-demographic, psychiatric and addiction related variables were included in the model.
3. Results
3.1. Subjects
Most of the subjects were middle-aged men (which is typical of the VA population). An equal number of subjects identified themselves as either White (47.2%) or Black (46.6%), and 3% identified themselves as of Hispanic/Latino ethnicity. Thirty-five percent of the sample was married/partnered, 27.3% were working full time, and 67.7% were financially stable, see Table 1 for details. Two-thirds of the sample (65.8%) screened positive for psychiatric disorders. The subjects reported 34.42 (SD = 30.95) alcohol binges over the last 3 months. Current smokers comprised 50% the sample, and 72% of the subjects reported the use of other drugs over the last year. The presence of pain over the past week was reported by 67% of the sample (Table 2).
Table 1.
Baseline demographics for the total sample, and the sample stratified by suicidal ideation status in the past year.
| Variable | Sub-category | Total sample | Sample stratified by suicidal ideation
|
||
|---|---|---|---|---|---|
| SI− (N = 99) | SI+ (N = 62) | p | |||
| Age (years) | Mean (SD) | 51 (15) | 51 (16) | 52 (13) | 0.58 |
| Gender | Males N (%) | 151 (93%) | 93 (93%) | 58 (93%) | 0.58 |
| Race | White N (%) | 76 (47%) | 48 (48%) | 28 (45%) | 0.52 |
| Black N (%) | 75 (46%) | 44 (44%) | 31 (50%) | ||
| Others N (%) | 10 (6%) | 7 (7%) | 3 (4%) | ||
| Ethnicity | Hispanic N (%) | 5 (3%) | 3 (3%) | 2 (3%) | 1.00 |
| Marital status | Single N (%) | 104 (64%) | 63 (63%) | 41 (66%) | 0.86 |
| Married N (%) | 57 (35%) | 36 (36%) | 21 (33%) | ||
| Vocational status | Full-time N (%) | 44 (27%) | 35 (35%) | 9 (14%) | 0.74 |
| Part-time N (%) | 19 (11%) | 14 (14%) | 5 (8%) | ||
| Financial status | Can make ends meet N (%) | 109 (67%) | 80 (80%) | 29 (47%) | <0.001 |
| Cannot make ends meet N (%) | 52 (32%) | 19 (19%) | 33 (53%) | ||
SI− = absence of any suicidal ideation in the past year; SI+ = a positive response to ≥1 question on the Paykel questionnaire for suicidal ideation; financial status was assessed using the question, “have at least enough to get by or more”, and “cannot make ends meet”; SD = Standard Deviation.
Table 2.
Suicidality, sleep continuity, psychiatric, addiction and pain characteristics in the total sample and the sample stratified by the presence or absence of suicidal ideation (past year).
| Variable | Sub-category | Total sample |
|---|---|---|
| Suicidal ideation | Not worth living N (%) | 62 (39%) |
| Wished was dead N (%) | 53 (33%) | |
| Taking own life N (%) | 33 (21%) | |
| Thoughts/plans N (%) | 20 (12%) | |
| Attempt N (%) | 5 (3%) | |
| Paykel — total score | 1 (1) |
| Variable | Sub-category | Total sample | Stratified by suicidal ideation (SI)
|
||
|---|---|---|---|---|---|
| SI− | SI+ | p | |||
| Insomnia indices | SL (minutes) mean (SD) (ICSD-2) | 67 (73) | 49 (54) | 92 (88) | <0.001 |
| WASO (minutes) mean (SD) (ICSD-2) | 81 (110) | 63 (84) | 106 (136) | 0.01 | |
| SQ | 2 (0) | 2 (0) | 3 (0) | <0.001 | |
| Habitual Sleep Duration (hours) | Total Sample mean (SD) (ICSD-2) | 5 (1) | 5 (1) | 5 (2) | 0.05 |
| Short Sleeper (N = 111) | 4 (1) | 61 (61%) | 50 (80%) | 0.23 | |
| Normal Sleeper (N = 29) | 7 (0) | 21 (21%) | 8 (12%) | ||
| Long Sleeper (N = 7) | 10 (1) | 4 (4%) | 3 (5%) | ||
| Psychiatric Diagnoses | Present N (%) | 106 (65%) | 49 (49%) | 57 (91%) | <0.001 |
| Depressive Dis | PHQ-9 ≥10 N (%) | 65 (40%) | 60 (60%) | 5 (8%) | <0.001 |
| Mania | Lifetime Prevalence N (%) | 21 (13%) | 5 (5%) | 16 (26%) | <0.001 |
| Psychosis | Lifetime Prevalence N (%) | 11 (6%) | 4 (4%) | 7 (11%) | 0.07 |
| PTSD | PCL ≥50 N (%) | 44 (27%) | 15 (15%) | 29 (47%) | 0.002 |
| GAD | Present N (%) | 50 (31%) | 15 (15%) | 35 (56%) | <0.001 |
| Panic Disorder | Present N (%) | 6 (3%) | 3 (3%) | 3 (5%) | 0.42 |
| Alcohol Use | Binges (last 3 months) (ICSD-2) | 34 (30) | 34 (31) | 33 (30) | 0.88 |
| Drinks (last 7 days) | 24 (24) | 23 (20) | 26 (28) | 0.35 | |
| Current Smokers | Yes N (%) | 82 (50%) | 48 (48%) | 34 (54%) | 0.51 |
| Drug Use (Past Yr) | Yes N (%) | 117 (72%) | 65 (65%) | 52 (83%) | 0.01 |
| Pain | Presence of pain (yes) | 108 (67%) | 63 (64%) | 45 (73%) | 0.18 |
Legend: Suicidal ideation was assessed with the Paykel questionnaire, sleep latency (SL) was assessed using the question “How long does it usually take you to fall asleep at night (in minutes)?”; wake after sleep onset time (WASO) was assessed using the question, “How long are you usually awake during the middle of the night, after initially falling asleep (in minutes)?”; sleep quality (SQ) was assessed using the question, “During the past month, how would you rate your overall sleep quality (on a scale of 1 to 4)?”; Habitual Sleep Duration (HSD) was assessed using the question, “How many hours of sleep did you usually get at night (in hours)?”. Sleep duration was further categorized into short sleeper (≤6 h a night), normal sleeper (7–8 h a night), and long sleeper (≥9 h). Psychiatric diagnoses that were assessed using the Mini International Neuropsychiatric Inventory (MINI) included the following diagnoses and evaluated for the following duration: 1) Mania — over the lifetime; 2) Psychosis — over the lifetime; 4) Panic Disorder — over the lifetime; 4) Alcohol Abuse and Alcohol Dependence — over the past year; 5) Generalized Anxiety Disorder — over the last 6 months. Depressive Disorder over the last 2 weeks was assessed using the Patient Health Questionnaire — 9-item scale; Post-traumatic Stress Disorder (PTSD) symptoms over the past month were assessed using the 17-item PTSD Check List (PCL). Alcohol consumption was assessed as standard alcoholic drinks consumed over the last 7 days, as well as the frequency of binge drinking days (≥5 standard drinks for men and ≥4 for women on a single day) prior to the interview using the Time Line Follow-Back method. Smoking Status was assessed with the question: “Do you currently smoke?” The responses were recorded as either a “yes” or a “no.” Other drug use was assessed by inquiring specifically about the frequency of use of cocaine, heroin, marijuana, speed, inhalants, LSD, barbiturates, and club drugs in the past year. We coded other drug use for the past year as “yes” or “no.” Pain was assessed with the question: “Do you have daily pain or at least weekly episodes of pain.” The responses were recorded as either “yes” or “no.”
3.2. Suicidal ideation
Approximately one-third of the subjects (38.5%) endorsed the presence of suicidal ideation over the past year (Table 2). The most common suicidal symptoms endorsed were “not worth living” in 39%, and “wished was dead” in 33%. The least common symptom reported was a suicide attempt in the past year (3%).
3.3. Sleep
The subjects reported the following insomnia symptoms: a mean SL of 67.58 (SD = 73.50) minutes, mean WASO of 81.61 (SD = 110.70) minutes, and mean SQ of 2.70 (0.95). Subjects reported being short sleepers on average, with a HSD of 5.54 (SD = 1.84) hours (Table 2).
3.4. Association between suicidal ideation, insomnia, sleep duration and covariates
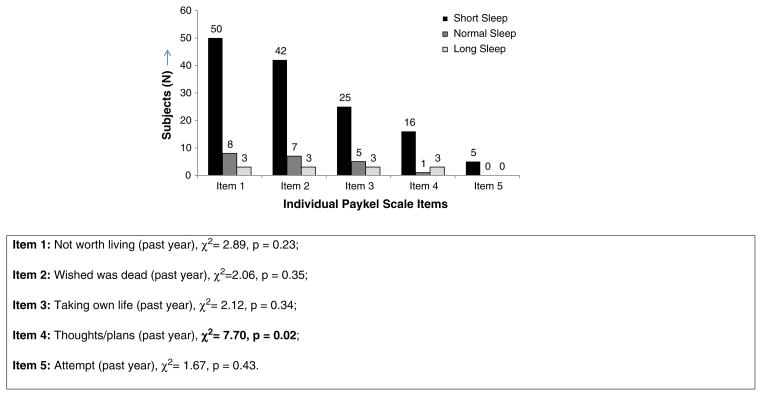
Subjects that reported the presence of suicidal ideation over the past year had significantly more financial problems, more insomnia symptoms, shorter sleep duration, and a higher prevalence of psychiatric disorders and drug use in the past year, and pain symptoms in the past week. Although they reported lower alcohol binges in the past three months, these differences were not significant (Table 2 and Fig. 1).
Fig. 1.
The total number of subjects who endorsed the five suicidal ideation symptoms over the last year (on the Paykel Scale) across the sleep duration categories. Item 1: Not worth living (past year), χ2=2.89, p=0.23; Item 2: Wished was dead (past year), χ2=2.06, p=0.35; Item 3: Taking own life (past year), χ2=2.12, p=0.34; Item 4: Thoughts/plans (past year), χ2= 7.70, p = 0.02; Item 5: Attempt (past year), χ2 = 1.67, p = 0.43.
Sleep duration was assessed using the question, “How many hours of sleep did you usually get at night”, with the responses being recorded as hours a night. Short sleep duration (short sleep) was assessed as those reporting a habitual sleep duration of ≤6 hours a night; normal sleep duration (normal sleep) was assessed as those reporting sleeping 7–8 hours a night; long sleep duration (long sleep) was assessed as those reporting a nocturnal sleep duration of ≥9 hours.
3.5. Univariate analyses
In separate models adjusted for socio-demographic variables, SL, WASO, and a poor SQ were all positively associated with suicidal ideation. HSD was associated with suicidal ideation only in the unadjusted model; however no such relationship was seen in the adjusted model. The covariates that were also associated with suicidal ideation in these models included inadequate finances (all p < 0.001), and the presence of a psychiatric disorder (all p < 0.001); age was also a significant covariate in most of these models (p<0.05) with the exception of WASO (p=0.06).
3.6. Multivariable analysis
In the final model including all sleep indices and covariates, poor sleep quality was the only sleep variable associated with suicidal ideation (Table 3). Other variables seen to be positively associated with suicidal ideation included older age (p = 0.02), inadequate finances (p < 0.001), and the presence of psychiatric disorders (p = 0.001). A non-significant trend was seen for WASO and HSD. No relationship was seen to exist between SL and suicidal ideation.
Table 3.
The associations between suicidal ideation and insomnia symptoms, sleep duration, and covariates (socio-demographic, psychiatric, addiction, and pain variables).a
| Variable | Estimate | [95% CI] | p |
|---|---|---|---|
| Habitual sleep duration | 0.12 | [−0.04, 0.29] | 0.14 |
| Sleep latency | 0.002 | [−0.002, 0.006] | 0.28 |
| Wake after sleep onset | 0.002 | [−0.001, 0.004] | 0.14 |
| Sleep quality (poor) | 0.88 | [0.09, 1.67] | 0.02 |
| Age | 0.02 | [0.003, 0.049] | 0.02 |
| Sex (male) | −0.30 | [−1.38, 0.77] | 0.58 |
| Race (White) | 0.20 | [−0.37, 0.78] | 0.48 |
| Partner status (partnered) | −0.21 | [−0.83, 0.40] | 0.49 |
| Financial (cannot make ends meet) | 1.21 | [0.65, 1.76] | <0.001 |
| Psychiatric status (present) | 1.76 | [0.73, 2.79] | 0.001 |
| Alcohol binges (past 3 months) | 0.003 | [−0.005, 0.012] | 0.44 |
| Smoking status (smoker) | 0.01 | [−0.56 0.58] | 0.96 |
| Drugs (used in the past year) | 0.39 | [−0.36, 1.16] | 0.30 |
| Pain (present in the past week) | −0.30 | [−0.94, 0.33] | 0.35 |
Estimate = coefficient, CI = Confidence Interval; Habitual Sleep Duration was assessed with the question, “How many hours of sleep did you usually get at night (in hours)?”, Sleep latency was assessed with the question, “How long does it usually take you to fall asleep at night (in minutes)”; wake after sleep onset time was assessed with the question, “How long are you usually awake during the middle of the night, after initially falling asleep?”; sleep quality was assessed with the question, “During the past month, how would you rate your overall sleep quality?” with responses ranging from very good–very bad; partner status was dichotomously, as whether subject was in either single or in married/non-married relationship; financial status was assessed dichotomously as whether subject could make ends meet (or not); psychiatric status was assessed dichotomously for the absence or presence of psychiatric disorder/s (lifetime diagnosis of mania, psychosis or panic disorder on the MINI (Mini International Neuropsychiatric Inventory)); presence of generalized anxiety disorder symptoms in the last 6 months on the MINI; a score of ≥10 on the Patient Health Questionnaire (PHQ-9) for depressive disorder; and a score of ≥ 50 on the PTSD Checklist for Post-Traumatic Stress Disorder (PTSD); smoking status was assessed using the question, “Do you currently smoke?” The responses were recorded as either a “yes” or a “no”; Other drug use was assessed by inquiring specifically about the frequency of use of cocaine, heroin, marijuana, speed, inhalants, LSD, barbiturates, and club drugs in the past year. We coded other drug use for the past year as “Yes” or “No.” Pain was assessed with the question: “Do you have daily pain or at least weekly episodes of pain.” The responses were recorded as either “yes” or “no.”
Model χ2 = 64.70, p < 0.001, pseudo R2 = 0.35.
4. Discussion
In this preliminary study of Veterans misusing alcohol, we evaluated the relations between suicidal ideation and insomnia symptoms and habitual sleep duration. Veterans with short sleep duration were more likely to endorse all five suicidal ideation symptoms over the last year, in comparison to those with normal and long sleep duration. Additionally, all three hallmark insomnia symptoms: difficulty falling asleep, difficulty maintaining sleep, and a poor sleep quality, were associated with higher levels of suicidal ideation after adjusting for socio-demographics, psychiatric and addiction related covariates. Other significant predictors of suicidal ideation over the past year were the presence of psychiatric symptoms and the patient’s financial status. In an adjusted model including all three insomnia symptoms, inadequate sleep quality was still significantly associated with higher suicidal ideation.
The association found between insomnia symptoms and suicidal ideation is consistent with prior literature in community-dwelling population (Bjorngaard et al., 2011; Goldstein et al., 2008), Veteran (Ribeiro et al., 2012), and alcohol-misusing populations (Klimkiewicz et al., 2012; Rossow & Amundsen, 1995). Difficulty falling asleep and difficulty maintaining sleep can result in extended periods of time being awake at night and thus a greater amount of time available for rumination, frustration, and catastrophic thinking. Additionally, the physiological aspect of reduced frontal activation during night hours, which decreases executive function, thought inhibition, and emotional regulation (Durmer & Dinges, 2005) may confer additional risk. These factors, taken together, provide the pressure and opportunity for irrational cognition and thoughts.
Those with short sleep duration were more likely to endorse all the suicidal ideation symptoms. It is to be noted that all five respondents who attempted suicide in the past year endorsed having short sleep duration. These findings are consistent with prior literature showing that short sleep duration is associated with suicidal ideation (Goodwin & Marusic, 2008), and extends the literature from a nationally representative sample (Goodwin & Marusic, 2008) and hospitalized patients (Blasco-Fontecilla et al., 2011) to a population of Veterans misusing alcohol. Controlling for HSD, suicidal ideation also was significantly associated with financial difficulties and underlying psychiatric symptoms, as suggested previously (Grandner & Drummond, 2007; Grandner, Patel, Gehrman, Perlis, & Pack, 2010; Meltzer et al., 2011).
In the final multivariable analysis including all sleep variables and covariates, poor sleep quality was the only significant insomnia symptom associated with suicidal ideation, with a trend towards significance for WASO and HSD. It may be possible that sleep quality assesses a domain different from the other insomnia symptoms, for example daytime tiredness (Harvey, Stinson, Whitaker, Moskovitz, & Virk, 2008), which may be magnified with the psychiatric symptoms and alcohol consumption. The lack of an association of suicidal ideation with WASO and SL may have been due, in part, to the inadequate sample size. In addition, some of our selected covariates that were associated with suicidal ideation in this final model included increasing age, inadequate finances and the presence of psychiatric disorders. Increasing age is an established risk factor for suicide especially in Veterans and in those abusing alcohol (Kemp & Bosarte, 2012; Rossow & Amundsen, 1995). Inadequate finances have been associated with suicidal ideation in prior studies involving non-Veteran and Veteran subjects (Mavandadi, Rook, Newsom, & Oslin, 2013; Meltzer et al., 2011).
The limitations associated with this study included the following: the retrospective, observational nature of the study; the subjective insomnia assessments assessed only the habitual nature of SL, WASO and HSD; the lack of additional data on substance use and disorders; the lack of a comparison group to assess for variability in the risk factors and the small sample size. It is to be noted, however, that insomnia is commonly assessed using subjective measures (Schutte-Rodin et al., 2008). In spite of the presence of these limitations, this study is amongst the first to assess for the relationship between suicidal ideation and insomnia in a primary care sample of Veterans misusing alcohol. Future research studies should expand on these findings by including larger samples that are more generalizable, and evaluate the effects on sleep of combined alcohol and other drug use, with or without the use of objective sleep measures. From a clinical standpoint, insomnia symptoms in Veterans misusing alcohol should trigger an evaluation for suicidal ideation, especially if they have psychosocial problems.
HIGHLIGHTS.
Suicidal ideation was associated with insomnia symptoms in Veterans misusing alcohol.
Suicidal ideation was not associated with habitual sleep duration.
In the final model, suicidal ideation was only associated with the sleep quality.
In Veterans misusing alcohol, insomnia should prompt a psychiatric assessment.
Acknowledgments
Role of funding sources
The VISN-4 MIRECC of the Philadelphia Veterans Affairs Medical Center supported this study. The authors (SC, SM, DO) received salary support from the Department of Veterans Affairs. Dr. Grandner received a grant support from the National Institutes of Health (1K23HL110216-01, 1R21ES022931-01).
The authors would like to thank Dr. Henry Kranzler and Dr. Holly Shue for their advice relating to the preparation of this manuscript. The content of this publication does not represent the views of the Department of Veterans Affairs, the United States Government, or any of the affiliated institutions. The authors (SC, SM, ES, and DO) received salary support from the Department of Veterans Affairs.
Footnotes
Disclaimers
The content of the publication does not represent the views of the Department of Veterans Affairs, the United States Government, or any of the affiliated institutions.
Contributors
Drs, Chakravorty, Grandner, Mavandadi, Perlis and Oslin designed the study. Drs. Chakravorty, and Grandner conducted the literature review. Drs. Chakravorty and Mavandadi conducted the data analyses. Dr. Chakravorty wrote the first draft of the manuscript and all authors contributed to and have approved of the final manuscript.
Conflict of interest
None of the authors have any actual or potential conflict of interest with this manuscript.
References
- Bjorngaard JH, Bjerkeset O, Romundstad P, Gunnell D. Sleeping problems and suicide in 75,000 Norwegian adults: A 20 year follow-up of the HUNT I study. Sleep. 2011;34:1155–1159. doi: 10.5665/SLEEP.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blasco-Fontecilla H, Alegria AA, Lopez-Castroman J, Legido-Gil T, Saiz-Ruiz J, de Leon J, et al. Short self-reported sleep duration and suicidal behavior: A cross-sectional study. Journal of Affective Disorders. 2011;133:239–246. doi: 10.1016/j.jad.2011.04.003. [DOI] [PubMed] [Google Scholar]
- Blessed G, Tominson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral gray matter. British Journal of Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. The American Journal of Managed Care. 2006;12:597–606. [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Chakravorty S, Grandner MA, Kranzler HR, Mavandadi S, Kling MA, Perlis ML, et al. Insomnia in alcohol dependence: Predictors of symptoms in a sample of veterans referred from primary care. The American Journal on Addictions/American Academy of Psychiatrists in Alcoholism and Addictions. 2013;22:266–270. doi: 10.1111/j.1521-0391.2012.12009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, McNeil J, Despres JP, Bouchard C, Tremblay A. Short sleep duration is associated with greater alcohol consumption in adults. Appetite. 2012;59:650–655. doi: 10.1016/j.appet.2012.07.012. [DOI] [PubMed] [Google Scholar]
- Driessen M, Veltrup C, Weber J, John U, Wetterling T, Dilling H. Psychiatric co-morbidity, suicidal behaviour and suicidal ideation in alcoholics seeking treatment. Addiction. 1998;93:889–894. doi: 10.1046/j.1360-0443.1998.93688910.x. [DOI] [PubMed] [Google Scholar]
- Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Seminars in Neurology. 2005;25:117–129. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA: The Journal of the American Medical Association. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Foster JH, Peters TJ. Impaired sleep in alcohol misusers and dependent alcoholics and the impact upon outcome. Alcoholism, Clinical and Experimental Research. 1999;23:1044–1051. [PubMed] [Google Scholar]
- Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. Journal of Consulting and Clinical Psychology. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31:1097–1101. [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Medicine Reviews. 2007;11:341–360. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: Bridging the gap between laboratory and epidemiological studies. Sleep Medicine Reviews. 2010;14:239–247. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H. The subjective meaning of sleep quality: A comparison of individuals with and without insomnia. Sleep. 2008;31:383–393. doi: 10.1093/sleep/31.3.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron M. Deaths: Leading causes for 2008. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2012;60:1–94. [PubMed] [Google Scholar]
- Instruction Manual. Instructions for Patient Health Questionnaire (PHQ) and GAD-7 Measures. http://www.phqscreeners.com/instructions/instructions.pdf.
- John U, Meyer C, Rumpf HJ, Hapke U. Relationships of psychiatric disorders with sleep duration in an adult general population sample. Journal of Psychiatric Research. 2005;39:577–583. doi: 10.1016/j.jpsychires.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short Orientation–Memory–Concentration Test of cognitive impairment. The American Journal of Psychiatry. 1983;140:734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- Kemp J, Bosarte R. DoV Affairs, editor. Suicide Data Report 2012. Department of Veterans Affairs; 2012. [Google Scholar]
- Kim HM, Smith EG, Ganoczy D, Walters H, Stano CM, Ilgen MA, et al. Predictors of suicide in patient charts among patients with depression in the Veterans Health Administration health system: Importance of prescription drug and alcohol abuse. The Journal of Clinical Psychiatry. 2012;73:e1269–e1275. doi: 10.4088/JCP.12m07658. [DOI] [PubMed] [Google Scholar]
- Klimkiewicz A, Bohnert AS, Jakubczyk A, Ilgen MA, Wojnar M, Brower K. The association between insomnia and suicidal thoughts in adults treated for alcohol dependence in Poland. Drug and Alcohol Dependence. 2012;122:160–163. doi: 10.1016/j.drugalcdep.2011.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Willaims JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger PM, Friedman EM. Sleep duration in the United States: A cross-sectional population-based study. American Journal of Epidemiology. 2009;169:1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner D, Amick BC, III, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Medical Care. 2001;39:72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- Mavandadi S, Rook KS, Newsom JT, Oslin DW. Suicidal ideation and social exchanges among at-risk veterans referred for a behavioral health assessment. Social Psychiatry and Psychiatric Epidemiology. 2013;48:233–243. doi: 10.1007/s00127-012-0534-5. [DOI] [PubMed] [Google Scholar]
- McCall WV, Blocker JN, D’Agostino R, Jr, Kimball J, Boggs N, Lasater B, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Medicine. 2010;11:822–827. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. 2. London: Chapman and Hall/CRC; 1989. [Google Scholar]
- Meltzer H, Bebbington P, Brugha T, Jenkins R, McManus S, Dennis MS. Personal debt and suicidal ideation. Psychological Medicine. 2011;41:771–778. doi: 10.1017/S0033291710001261. [DOI] [PubMed] [Google Scholar]
- Meneese WB, Yutrzenka BA. Correlates of suicidal ideation among rural adolescents. Suicide & Life-Threatening Behavior. 1990;20:206–212. [PubMed] [Google Scholar]
- Norusis M. SPSS 13.0 Advanced Statistical Procedures Companion. Upper Saddle-River, NJ: Prentice Hall, Inc; 2004. [Google Scholar]
- Oslin DW, Ross J, Sayers S, Murphy J, Kane V, Katz IR. Screening, assessment and management of depression in VA primary care clinics. The Behavioral Health Laboratory. Journal of General Internal Medicine. 2006;21:46–50. doi: 10.1111/j.1525-1497.2005.0267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paykel ES, Myers JK, Lindenthal JJ, Tanner J. Suicidal feelings in the general population: A prevalence study. The British Journal of Psychiatry: The Journal of Mental Science. 1974;124:460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- Preuss UW, Schuckit MA, Smith TL, Danko GP, Buckman K, Bierut L, et al. Comparison of 3190 alcohol-dependent individuals with and without suicide attempts. Alcoholism, Clinical and Experimental Research. 2002;26:471–477. [PubMed] [Google Scholar]
- Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. Journal of Affective Disorders. 2012;136:743–750. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- Rossow I, Amundsen A. Alcohol abuse and suicide: A 40-year prospective study of Norwegian conscripts. Addiction. 1995;90:685–691. doi: 10.1046/j.1360-0443.1995.9056859.x. [DOI] [PubMed] [Google Scholar]
- Rossow I, Romelsjo A, Leifman H. Alcohol abuse and suicidal behaviour in young and middle aged men: Differentiating between attempted and completed suicide. Addiction. 1999;94:1199–1207. doi: 10.1046/j.1360-0443.1999.948119910.x. [DOI] [PubMed] [Google Scholar]
- Roy A, Lamparski D, DeJong J, Moore V, Linnoila M. Characteristics of alcoholics who attempt suicide. The American Journal of Psychiatry. 1990;147:761–765. doi: 10.1176/ajp.147.6.761. [DOI] [PubMed] [Google Scholar]
- Santiago PN, Wilk JE, Milliken CS, Castro CA, Engel CC, Hoge CW. Screening for alcohol misuse and alcohol-related behaviors among combat veterans. Psychiatric Services. 2010;61:575–581. doi: 10.1176/ps.2010.61.6.575. [DOI] [PubMed] [Google Scholar]
- Scherrer JF, Grant JD, Agrawal A, Madden PA, Fu Q, Jacob T, et al. Suicidal behavior, smoking, and familial vulnerability. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2012;14:415–424. doi: 10.1093/ntr/ntr230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Bernstein LI. Sleep time and drinking history: A hypothesis. The American Journal of Psychiatry. 1981;138:528–530. doi: 10.1176/ajp.138.4.528. [DOI] [PubMed] [Google Scholar]
- Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine. 2008;4:487–504. [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.) The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. (quiz 34–57) [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. British Journal of Addiction. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Ware J, Kossinski M, Keller S. How to Score the SF-12 (R) Physical and Mental Health Summary Scores. 3. Lincoln, RI: Quality Metric Incorporated; 1998. [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. Journal of Psychiatric Research. 2009;43:526–531. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]