INTRODUCTION
Sleep problems are not an inherent part of the aging process.1,2 Many older adults have good sleep quality until the end of their lives. It is critical that sleep problems are not mistaken for physiologic changes in sleep-awake patterns and sleep architecture that occur throughout the lifespan.3,4 Older adults often display an advanced circadian tendency, having an earlier bedtime and an earlier wake-up time. Sleep architecture changes include spending an increased proportion of time in stages N1 and N2 sleep (ie, the lighter stages of sleep), a decreased proportion of time in stage N3 sleep (ie, a deeper stage of sleep) and in rapid eye movement (REM) sleep. These architecture changes reflect a decrease in deep, restorative sleep and an increase in light, transitory sleep. In addition, older adults tend to spend slightly less time asleep than their younger counterparts. Although some older adults complain of poor night-time sleep or subsequent impairments in daytime functioning, others assume that their difficulties are part of the normal aging process. Therefore, a focused evaluation of sleep, specifically sleep apnea and insomnia, and related daytime functioning should be performed in every older adult in whom sleep disturbances are suspected.
SLEEP APNEA
Patients with sleep apnea show repetitive episodes of reduction (hypopnea) or absence (apnea) of airflow during sleep. There are 2 main types of sleep apnea: obstructive and central sleep apnea. In obstructive sleep apnea (OSA), the upper airway is obstructed secondary to anatomic factors, such as obesity and/or reduced activation of the dilatory muscles of the airway (eg, under the effect of alcohol or sedative drugs). In OSA, the respiratory effort persists during the episodes of hypoventilation. In contrast, central sleep apnea (CSA) is secondary to a reduced respiratory effort secondary to problems such as neurologic conditions (eg, stroke) or heart failure. Other causes of CSA include drugs or substances that depress the central nervous system (eg, opioids). Adverse effects associated with sleep apnea include hypertension, coronary artery disease, depression, car accidents, cognitive impairment, stroke, and mortality.
Diagnosis
Common symptoms of sleep apnea are daytime sleepiness, irritability, fatigue, and headache. Frail older patients may report subtle manifestations or may even be asymptomatic. Common findings at the physical examination include a crowded oral pharynx, obesity, and hypertension. However, obesity is less common in elderly patients with OSA. It is important to interview bed partners, because they can describe snoring, apnea episodes, or irritability. Sleep apnea can easily be screened for using clinical prediction rules such as the STOP-BANG questionnaire (Box 1).5 However, the gold standard for the diagnosis of sleep apnea is in-laboratory polysomnography. This test provides information regarding sleep stages, muscular activity, nasal airflow, oxygen saturation, electrocardiogram, snoring, body position, and limb movements.6 Portable monitors used at home are a simpler and more economical alternative. The concordance rates between home sleep tests and polysomnography are high, especially for moderate and severe cases of sleep apnea.
Box 1. STOP-BANG questionnaire.
Do you snore loudly (loud enough to be heard through closed doors, or for your bed partner to elbow you for snoring at night)?
Do you often feel tired, fatigued, or sleepy during the daytime (such as falling asleep while driving)?
Has anyone observed you stop breathing or choke/gasp during your sleep?
Are you or are have you been treated for high blood pressure?
Body mass index more than 35 kg/m2?
Age older than 50 year old?
Neck size (measure around Adams apple) larger than 43 cm (17 inches) for men or 41 cm (16 inches) for women?
Male gender?
Fewer than 3 “Yes” answers indicates low risk for sleep apnea.
Courtesy of www.stopbang.ca; with permission.
Sleep Apnea Severity
Sleep apnea is classified into severity levels based on the average number of hypopneas and apneas per hour during sleep (apnea hypopnea index [AHI]) as either mild (AHI 5–15), moderate (AHI 16–30), or severe (AHI>30).
Treatment
Positive airway pressure (PAP) is the first-line therapy for patients with moderate or severe sleep apnea. PAP maintains the airway open during sleep through administration of air pressure. Some of the benefits observed with the use of PAP are improvement of sleep quality, daytime symptoms, blood pressure, ventricular ejection fraction, and cognitive function. Moreover, PAP decreases the risk of stroke, cardiovascular disease, and mortality in older patients.7,8 Continuous PAP (CPAP) is the most commonly used type of PAP. CPAP provides a fixed pressure of air during the breathing cycle. There are more advanced devices (eg, biphasic PAP or auto adjusting positive airway pressure [APAP]) that can provide different levels of pressure and may be better tolerated by some patients. Good adherence (ie, >4 hours of use per night on 70% of nights) to PAP prescription may be a challenge to older patients. Long-term adherence is best predicted by the use of PAP during the first week. There are several features of PAP machines that may improve patient compliance, such as humidifiers, ramp, and pressure relief. In addition, there are several mask options and sizes available to better fit patient preferences (eg, nasal or facial mask). In addition, concomitant psychological cognitive behavior therapy may improve adherence. For patients with obstructive apnea who reject or do not adhere to PAP therapy, oral appliances (ie, mandibular advancement devices) may be an alternative. These devices move the jaw forward in the hope of reducing airway obstruction. Other treatment alternatives (eg, nose valves and uvulopalatopharyngoplasty surgery) have not been extensively evaluated in older adults. General recommendations for older patients with sleep apnea, including those with mild sleep apnea, are avoidance of sedative drugs and alcohol, reducing weight, and controlling blood pressure.
INSOMNIA
According to the International Classification of Sleep Disorders, Third Edition,9 insomnia is defined as a subjective complaint of difficulty initiating sleep, difficulty maintaining sleep, or early morning awakenings that occur at a minimum of 3 nights per week, for 3 months, and are associated with significant daytime consequences. Examples of these daytime consequences include difficulty concentrating, mood disturbances, fatigue, and worry about sleep. On average, older adults experience insomnia symptoms for several years before receiving a formal diagnosis.10 Insomnia often occurs in association with other clinical disorders (eg, comorbid insomnia) especially in older people. Insomnia prevalence tends to be higher in older individuals with multiple physical and psychiatric conditions (60% or more), and higher among older women than among older men.3,11 The higher prevalence of insomnia among older adults is thought to be a consequence of the physical and mental health comorbidities of aging, rather than a consequence of aging itself.12 Negative consequences of insomnia in late life include decreased quality of life, risk for falls, psychological and physical difficulties, economic and social costs, risk for nursing home placement, and mortality.
Diagnosis
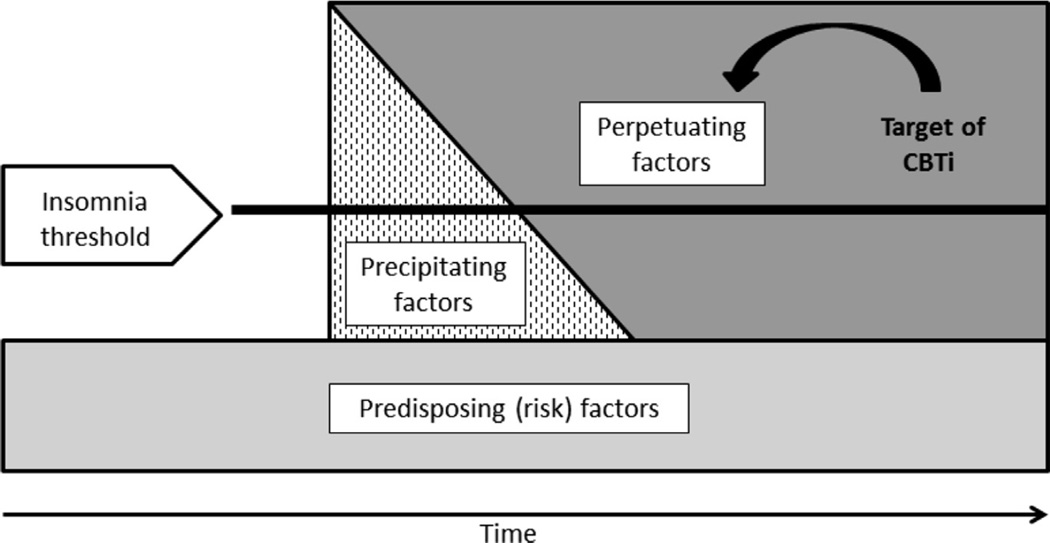
An examination of sleep quality should be performed during routine clinical visits in older patients. Asking about sleep satisfaction and sleep-related daytime consequences may alert the provider to the necessity of a more a structured clinical interview focusing on insomnia symptoms. The clinical interview for insomnia should focus on probable predisposing factors, precipitating factors, and perpetuating factors (ie, the 3 P model, Fig. 1).13 Predisposing factors include risk factors that increase older adults’ likelihood of experiencing poor sleep, such as poor physical and mental health, family history of insomnia, or low socioeconomic status. Precipitating factors include any events that can acutely disrupt sleep, such as recent life events (eg, depressive episode, hospitalization, loss of a loved one, moving residences). Perpetuating factors are the aspects of the older adult’s daily behavior that serve to maintain poor sleep, and include all contextual, emotional, and behavioral influences.
Fig. 1.
The 3 P conceptual model of insomnia. Predisposing factors: physical and mental health, family history of insomnia, poverty, and so forth. Precipitating factors: depressive episode, hospitalization, loss of a loved one, moving, and so forth. Perpetuating factors: spending too much time in bed, not following a regular sleep schedule, and so forth. CBTi, Cognitive behavior treatment of insomnia.
Some self-report questionnaires, such as the Insomnia Severity Index14 (Box 2), have been validated in older adults. However, the retrospective recall of sleep quality necessary for these questionnaires may be difficult for older adults. A daily sleep diary can capture useful information regarding sleep timing, quantity, and quality across consecutive days. The use of a daily sleep diary is recommended in the clinical diagnosis of insomnia in late life. Polysomnography and wrist actigraphy are not indicated for the diagnosis of insomnia in older adults.
Box 2. Insomnia Severity Index.
Please rate the current (ie, last 2 weeks) severity of your insomnia problems:
Have you had difficulty falling asleep?
Have you had difficulty staying asleep?
Have you had problems waking up too early?
How satisfied/dissatisfied are you with your sleep pattern?
How noticeable to others do you think your sleep problem is in terms of impairing the quality of your life?
How worried/distressed are you about your current sleep problem?
To what extent do you consider your sleep problem to interfere with your daily functioning (eg, daytime fatigue, mood, ability to function at work/daily chores, concentration, memory)?
Five-point Likert scale (0, no problem; 4, very severe problem) possible answers for all items. Total score categories: 0 to 7, no clinically significant insomnia; 8 to 14, subthreshold insomnia; 15 to 21, moderate insomnia; 22 to 28, severe insomnia.
Courtesy of Charles M. Morin, PhD, Quebec QC; with permission.
Treatment
Insomnia should be treated with a specific and focused plan. Treatment of late-life insomnia can involve psychological strategies, pharmacologic agents, or both. In general, psychological techniques should be considered as initial treatment methods because of their strong empirical evidence, high safety in older adults, and long-term benefits. Psychological treatment approaches have outperformed pharmacologic treatment in head-to-head trials, and are also better than combined psychological/pharmacologic therapy.15,16
Psychological interventions
Psychological interventions for insomnia encompass a variety of different techniques, including sleep education, cognitive therapy, sleep hygiene, relaxation strategies, stimulus control, sleep restriction, and multicomponent treatment packages (eg, cognitive behavior treatment of insomnia [CBTi]). Sleep is largely behaviorally regulated, with a strong homeostatic biological drive and circadian component. Interventions with a foundation in behavioral theory and practice have been proved to be effective in the management of insomnia.
Stimulus control is a behavioral strategy based on classic conditioning principles that is intended to increase the response of sleep associated with the stimulus of the bed and bedroom. There is strong evidence in support of stimulus control for insomnia in late life.17,18 Sleep restriction is a behavioral strategy designed to increase the homeostatic sleep drive and strengthen the circadian signal through more closely aligning time spent in bed with time spent asleep. There is strong evidence in support of sleep restriction for insomnia in late life.17,18 Sleep education, cognitive therapy, and sleep hygiene have little empirical evidence to support their use as stand-alone treatment options for insomnia in older adults. These three techniques are most useful in combination with other psychological treatment strategies. Note that, although sleep hygiene recommendations are the most commonly used nonpharmacologic treatment approach to the management of insomnia, there is no evidence to support the use of sleep hygiene alone for insomnia management. Sleep hygiene recommendations are commonly used as the control or placebo condition in psychological intervention research. Relaxation strategies may prove beneficial alone in improving the sleep of older adults. However, like the strategies mentioned earlier, relaxation techniques may be most useful in combination with other psychological treatments.
CBTi has the strongest empirical grounding of all available behavioral treatment options for insomnia in older adults.17,18 CBTi is a combination treatment of insomnia typically consisting of stimulus control and sleep restriction, and variations of CBTi also include psychoeducation and cognitive therapy. CBTi has been shown to result in large improvements in perceived sleep in older adults with insomnia, and older adults prefer CBTi to sedative hypnotics. The typical delivery of CBTi involves one-on-one, face-to-face delivery in 4 to 6 weekly (or biweekly) sessions each lasting between 30 and 60 minutes. CBTi has been successfully delivered in as little as one or two 30-minute sessions, in group formats, and over virtual communication lines. Although commonly delivered by specially trained clinical psychologists, CBTi has been successfully administered by supervised nurse practitioners, health educators, and older adult peers. The overwhelming confluence of evidence supports CBTi as the recommended treatment of insomnia in older adults. Table 1 provides a comprehensive listing of psychological treatment options for insomnia in late life.
Table 1.
Psychological treatment approaches for insomnia in older adults
| Technique | Level of Support |
|---|---|
| Sleep education | Lowa; not an evidence-based practiceb; not a recommendationc |
| Information regarding normal sleep changes with age. Designed to normalize current sleep, improve expectations, and reduce anxiety | |
| Cognitive therapy | Lowa; not an evidence-based practiceb; not a recommendationc |
| Maladaptive thoughts, beliefs, and attitudes can negatively affect sleep. Challenging these thoughts can help promote sleep through a reduction in sleep disruptive thoughts and emotions | |
| Sleep hygiene | Lowa; not an evidence-based practiceb; not a recommendationc |
| Instruction to avoid or limit sleep disruptive substances and behaviors, including caffeine, alcohol, nicotine, exercising, and heavy meals at night | |
| Relaxation strategies | Moderatea; not an evidence-based practiceb; standard recommendationc |
| Active or passive relaxation techniques all designed to reduce physiologic or mental arousal that may be interfering with sleep | |
| Stimulus control | Stronga; not an evidence-based practiceb; standard recommendationc |
| Behavioral technique based on classic conditioning principals. Instructs individuals to limit their use of the bed to sleep and sex, and to limit the amount of time spent awake in bed | |
| Sleep restriction | Stronga; evidence-based practiceb; guideline recommendationc |
| Behavioral strategy designed to match the amount of time spent in bed with the amount of time asleep. A consistent sleep schedule and time in bed is collaboratively prescribed and adjusted as needed | |
| Multicomponent treatment packages | Stronga; evidence-based practiceb; standard recommendationc |
| Combines several individual components into a treatment package. Usually consists of stimulus control and sleep restriction. Sometimes includes sleep education, cognitive therapy, relaxation techniques, or sleep hygiene recommendations | |
Based on the authors’ critical review of empirical evidence and clinical practice with older adults.
Criteria for an intervention to be considered evidence-based include 50% of the outcome measures showing significant treatment effects with between-group effect sizes of at least 0.20.17
American Academy of Sleep Medicine practice parameters.18
Pharmacotherapy
Medication treatment of late-life insomnia should be used in the minority of patients; however, sedative hypnotic medications are the most commonly prescribed treatment approach for insomnia in older patients. Older adults are more than twice as likely as younger adults to be prescribed medication treatment of insomnia,19 which is particularly concerning given the increased risk for drug side effects, drug interactions, tolerance and dependence, and lack of empirical evidence supporting long-term use in older patients. In general, short-term pharmacotherapy may be indicated in situations of acute insomnia. In older adults with chronic insomnia, sedative hypnotics should be used with great caution. When the decision is made to prescribe a sedative hypnotic to an older patient, the smallest effective dose with the lowest risk of adverse effects should be prescribed for the shortest duration of time.
The commonly used sedative hypnotic medications can be broadly grouped into 3 categories: (1) short, intermediate, and long-acting benzodiazepines; (2) nonbenzodiaze-pines or z-drugs; and (3) sedating antidepressants. In general, long-acting benzodiazepines should not be used with older adults because of increased risks of daytime sedation, falls, and confusion. Short-acting or intermediate-acting benzodiazepines are preferable for patients with a primary complaint of sleep maintenance difficulties. The nonbenzodiazepines have a shorter duration of action than the benzodiazepines and are thought to carry a lower side effect profile; however, there is a limited amount of evidence pertaining directly to the use of most nonbenzodiazepines specifically in older patients with comorbid insomnia. Sedating antidepressants (eg, trazodone, tricyclics) are often used off-label for their sedative hypnotic effects, although little empirical evidence supports the use of sedating antidepressants as hypnotic agents in older adults. In addition, agents with anticholinergic side effects should be avoided (eg, diphenhydramine).
Differential Diagnosis of Sleep Apnea and Insomnia
Differential diagnosis for sleep apnea and insomnia includes distinguishing these two common sleep disorders from other sleep disturbances in late life. Less common sleep disorders in older adults include:
Circadian rhythm sleep disorders: older people commonly experience an advanced sleep phase (ie, an early bedtime and early morning awakening). Sleep logs can be used for making a diagnosis and for monitoring treatment response. Wrist actigraphy or polysomnography is indicated when the diagnosis is unclear or another sleep disorder is suspected.
REM behavior disorder (RBD): patients act out dreams with forceful movements and behaviors during sleep secondary to a lack of the normal muscle atonia present during REM sleep. They may injure themselves or their bed partners. RBD is rare in the general population, but has been associated with dementia, multiple system atrophy, and Parkinson disease. Polysomnography is required to confirm the diagnosis and to rule out other conditions.
Restless legs syndrome (RLS): RLS is an uncontrollable urge to move the legs, commonly caused by an uncomfortable sensation in the legs. The symptoms start during periods of rest (especially at night) and are partially or entirely relieved with movement. RLS is diagnosed clinically based on symptoms.
SUMMARY/FUTURE CONSIDERATIONS
Sleep problems are frequent, but underexplored in older adults. Sleep apnea and insomnia are particularly important sleep problems in older adults. Both sleep apnea and insomnia are associated with serious negative physical, mental, and social consequences. Methods for recognition of these disorders are effective, and safe treatment options are available. Improving the adherence to PAP therapy and reducing the use of sedative drugs are important goals to address in clinical practice and future research with older adults.
KEY POINTS.
Older adults frequently have sleep problems, such as sleep apnea and insomnia. These problems are often unrecognized and undertreated.
Obstructive sleep apnea (OSA) has been associated with hypertension, coronary artery disease, depression, car accidents, cognitive impairment, stroke, and mortality.
Positive airway pressure therapy effectively treats OSA.
Insomnia carries many negative unwanted consequences in older adults. Psychological techniques have been shown to be effective and should be considered as the first-line therapy for older adults with insomnia.
Acknowledgments
This work was supported by UCLA Claude D. Pepper Older Americans Independence Center (NIA 5P30 AG028748); NIH/NCATS UCLA CTSI (UL1TR000124); the VA Advanced Geriatrics Fellowship Program; the Geriatric Research, Education, and Clinical Center (GRECC); and the VA Greater Los Angeles Healthcare System.
REFERENCES
- 1.Foley DJ, Monjan AA, Brown SL, et al. Sleep complaints among elderly persons - an epidemiological study of 3 communities. Sleep. 1995;18:425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 2.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment: prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 3.Morgan K. Sleep and aging. In: Lichstein K, Morin C, editors. Treatment of late-life insomnia. Thousand Oaks (CA): Sage Publications; 2000. pp. 3–36. [Google Scholar]
- 4.Floyd JA, Medler SM, Ager JW, et al. Age-related changes in initiation and maintenance of sleep: A meta-analysis. Res Nurs Health. 2000;23:106–117. doi: 10.1002/(sici)1098-240x(200004)23:2<106::aid-nur3>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 5.Chung F, Yegneswaran B, Liao P, et al. STOP Questionnaire: a tool to screen for obstructive sleep apnea. Anesthesiology. 2008;108:812–821. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 6.Epstein LJ, Kristo D, Strollo PJ, Jr, et al. Clinical guidelines for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;15:263–276. [PMC free article] [PubMed] [Google Scholar]
- 7.Campos-Rodriguez F, Pena-Grinan N, Reyes-Nuñez N, et al. Mortality in obstructive sleep apnea-hypopnea patients treated with positive airway pressure. Chest. 2005;128:624–633. doi: 10.1378/chest.128.2.624. [DOI] [PubMed] [Google Scholar]
- 8.Giles TL, Lasserson TJ, Smith BJ, et al. Continuous positive airway pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;(25) doi: 10.1002/14651858.CD001106.pub2. CD001106. [DOI] [PubMed] [Google Scholar]
- 9.Diagnostic Classification Steering Committee TMJC. International classification of sleep disorders. 3rd edition. Rochester (NY): American Academy of Sleep Medicine; 2014. [Google Scholar]
- 10.Dzierzewski JM, O’Brien E, Kay DB, et al. Tackling sleeplessness: psychological treatment options for insomnia in older adults. Nat Sci Sleep. 2010;2:47–61. doi: 10.2147/NSS.S7064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ford DE, Kamerow DB. Epidemiological study of the sleep disturbances and psychiatric disorders. JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 12.Vitiello MV, Moe KE, Prinz PN. Sleep complaints cosegregate with illness in older adults: clinical research informed by and informing epidemiological studies of sleep. J Psychosom Res. 2002;53:555–559. doi: 10.1016/s0022-3999(02)00435-x. [DOI] [PubMed] [Google Scholar]
- 13.Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10:541–453. [PubMed] [Google Scholar]
- 14.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 15.Morin CM, Colecchi C, Stone J, et al. Behavioral and pharmacological therapies for late life insomnia: a randomized controlled trial. JAMA. 1999;281:991–999. doi: 10.1001/jama.281.11.991. [DOI] [PubMed] [Google Scholar]
- 16.Sivertsen B, Omvik S, Pallesen S, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults. JAMA. 2006;295:2851–2858. doi: 10.1001/jama.295.24.2851. [DOI] [PubMed] [Google Scholar]
- 17.McCurry SM, Logsdon RG, Teri L, et al. Evidence-based psychological treatments for insomnia in older adults. Psychol Aging. 2007;22:18–27. doi: 10.1037/0882-7974.22.1.18. [DOI] [PubMed] [Google Scholar]
- 18.Morgenthaler T, Kramer M, Alessi CA, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29:1415–1419. [PubMed] [Google Scholar]
- 19.Stewart R, Besset A, Bebbington P, et al. Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep. 2006;29:1391–1397. doi: 10.1093/sleep/29.11.1391. [DOI] [PubMed] [Google Scholar]