Abstract
Noninvasive radionuclide imaging has the potential to identify and assess mechanisms involved in particular stages of lung injury which occur with acute respiratory distress syndrome, for example. Lung uptake of 99mTc-hexamethylpropyleneamine oxime (HMPAO) is reported to be partially dependent on the redox status of the lung tissue while 99mTc-duramycin, a new marker of cell injury, senses cell death via apoptosis and/or necrosis. Thus, we investigated changes in lung uptake of these agents in rat exposed to hyperoxia for prolonged periods, a common model of acute lung injury.
Methods
Male Sprague-Dawley rats were pre-exposed to either normoxia (21% O2) or hyperoxia (85% O2) for up to 21 days. For imaging, the rats were anesthetized, injected i.v. with either 99mTc-HMPAO or 99mTc-duramycin (37-74 MBq) and planar images were acquired using a high sensitivity modular gamma camera. Subsequently, 99mTc-macroagreggated albumin (37 MBq, diam=10-40 μm) was injected i.v., imaged, and used to define a lung region-of-interest. The lung to background ratio was used as a measure of lung uptake.
Results
Hyperoxia exposure resulted in a 74% increase in 99mTc-HMPAO lung uptake, which peaked at 7 days and persisted for the 21 days of exposure. 99mTc-duramycin lung uptake was also maximal at 7 days of exposure but decreased to near control levels by 21 days. The sustained elevation of 99mTc-HMPAO uptake suggests ongoing changes in lung redox status whereas cell death appears to have subsided by 21 days.
Conclusion
These results suggest the potential use of 99mTc-HMPAO and 99mTc-duramycin as redox and cell-death imaging biomarkers, respectively, for in vivo identification and assessment of different stages of lung injury.
Keywords: Acute lung injury, apoptosis, oxidative stress
Introduction
An essential and lifesaving treatment for hypoxemia in patients with pneumonia or acute respiratory distress syndrome is supplemental oxygen (O2) therapy. However, prolonged exposure to high concentrations of O2 can be toxic to the lungs (1,2,3). Although the mechanisms leading to pulmonary hyperoxic injury are not fully understood, there is ample evidence that the deleterious effects of high O2 are the result of increased reactive oxygen species (ROS) formation, predominantly via mitochondrial pathways (3,4).
The chronic hyperoxia rat model of lung injury mimics key functional aspects of lung O2 toxicity observed clinically (1,2,5-7). It is a well-documented acute lung injury model, especially for studies of oxidant-induced lung injury (2,5,6,8,9). Studies by Crapo et al. provide a detailed description of histologic and morphometric changes in lungs of rats exposed to 85% O2 for up to 14 days (6). For the first 72 hours of exposure, signs of histologic and/or morphometric changes are undetectable. By 5 days, there is ∼30% loss in capillary endothelial cells and cell surface, infiltration of phagocytic leukocytes and other cell types, and an increase in the thickness of air-blood barrier. By 7 days, the lungs have lost half of the capillary endothelial cells, but pleural effusion and respiratory function impairment have substantially subsided. Capillary endothelial cells that survive 7 days experience significant morphometric changes including hypertrophy, with substantially less loss of these hypertrophied endothelial cells occurring between 7 and 14 days of exposure (6). These studies suggest that there may be critical biochemical changes in these hypertrophied capillary endothelial cells and reveal that the pulmonary capillary endothelium is a primary target of lung O2 toxicity.
This sensitivity of the pulmonary capillary endothelium to oxidative stress, as well as its large surface area and close apposition to blood-borne indicators, have led us and others to develop a range of probes to evaluate the effect of chronic hyperoxia on pulmonary endothelial mitochondrial and cytosolic redox functions (3-5, 8,10-12). The utility of these probes is that their pulmonary disposition, metabolism and/or redox status is altered following injury or adaptation to hyperoxia (5, 8,12). We have developed the use of a number of redox-active probes that are lipophilic and cell permeant in their reduced form, but when oxidized to a less membrane-permeable form become trapped in the cells or sequestered in subcellular organelles (5, 8,11). The disposition of these redox probes in the lung is dependent on the redox state of lung tissue. The redox reactions may occur on either the cell surface or intracellularly with an end result that the probe is delayed on its passage through the lung vasculature, sequestered in the lung, or both (5,8,10,11). Generally these experiments have relied on inflow-outflow experiments in isolated perfused lungs using probes that are not suitable for whole animal experiments and not available in radiolabeled forms suitable for scintigraphy or SPECT (single-photon emission computed tomography) imaging. Thus the overall goal of the present study is to investigate the use of SPECT biomarker imaging in an animal model to detect and delineate particular stages of lung O2 toxicity injury as a model of human acute lung injury.
Technetium-labeled hexamethylpropyleneamineoxime (99mTc-HMPAO) is a cerebral blood flow SPECT agent that crosses the blood-brain barrier and is trapped within the brain parenchyma (13). Clinical reports in patients with brain disorders, including psychiatric and movement disorders (13 -17) and stroke (18,19), have shown that HMPAO uptake is highly influenced by not only perfusion, but also by the nature of the lesion (20,21), suggesting its utility as a biomarker of cell-type specific metabolism. In addition, increases in 99mTc-HMPAO uptake in the lung have been reported in subclinical lung injury due to chemotherapy (22), diffuse infiltrative lung disease (23), irradiation lung injury (24,25), and inhalation and smoking injuries (26-28) in humans. Of particular note is the observation that increases were observed in patients generally showing no abnormal opacity on chest radiographs or findings on pulmonary function tests (22,24,27). Thus, the development of an improved methodology for identifying early lung injury prior to evidence of structural changes or indirect measures, would be an important tool for clinicians treating critically ill patients.
Duramycin is a 19-amino acid peptide produced by streptoverticillium cinnamoneus. When labeled with 99mTc, duramycin acts as a molecular probe for phosphatidylethanolamine (PtdE), a constituent of the inner leaflet of the plasma membrane (29-31). Generally, PtdE has little presence on the surface of viable cells, but it becomes exposed with apoptosis, due to redistribution of phospholipids across the bilayer (29). Duramycin also becomes accessible to the intracellular milieu with necrosis, due to compromised plasma membrane integrity (29,30). Zhao et al. originally developed 99mTc-duramycin as a biomarker for imaging acute cell death in myocardial ischemia/reperfusion injury (30). Rat exposure to 85% O2 has been reported to result in significant loss of endothelial cells by seven days via apoptosis and/or necrosis as measured by histology (6,32). Such a loss of endothelial cells is consistent with the significant decrease in lung angiotensin converting enzyme (ACE) activity, an index of perfused vascular surface area that we have measured in lungs of rats exposed to hyperoxia and employed as a measure of change in perfused lung surface area (8). One goal of the present study is to examine the potential for early detection of oxidative injury to the pulmonary endothelium using the apoptosis/necrosis biomarker 99mTc-duramycin. Thus, the aims of this study are to determine the lung uptake of 99mTc-HMPAO and 99mTc-duramycin in the chronic hyperoxia rat model and to evaluate their potential for early detection of oxidative lung injury.
Materials and Methods
Animals
All procedures were approved by the Institutional Animal Care and Use Committees of the Zablocki Veterans Affairs Medical Center. For control animal studies, adult male Sprague-Dawley rats (Charles River, N=14, body weight = 361.8 ± 25.4 (SD) g) were exposed to room air with free access to food and water. For the hyperoxic animal studies, weight-matched rats were housed in a sealed, temperature controlled (22 ± 2 C°) Plexiglas chamber (13″×23″×12″) maintained at ∼85% O2, balance N2 for with free access to food and water and a 12 hour light/dark cycle as previously described (5,8). Bedding, food and water were changed every other day and the body weight recorded. The total gas flow was ∼3.5 L/min, while the chamber CO2 was <0.5%. The animals were then studied after 2 (N=7), 4 (N=9), 7 (N=9), 14 (N=7), and 21 (N=10) days of hyperoxia exposure.
Imaging
Control normoxic rats as well as those exposed to chronic hyperoxia were imaged as described below. The rat was anesthetized (40 – 50 mg/kg pentobarbital sodium i.p.), and the left femoral vein exposed and cannulated with PE-10 tubing attached to an injection syringe containing saline plus heparin (25 units/ml). The rat was then placed supine on an acrylic plate (4 mm) positioned directly on the face of a parallel-hole collimator (hole diameter = 2 mm, depth = 1 inch) attached to a modular miniaturized gamma camera (Radiation Sensors, LLC) with list mode electronics. Either 99mTc-HMPAO (Ceretec, GE Healthcare) or 99mTc-durmaycin (30) (37 - 74 MBq), prepared according to kit directions, was then injected via the cannula. The injected dose was calculated from the difference between the pre- and post- injection activity within the syringe using a dose calibrator. Dynamic planar images were acquired every second for the first minute and every minute thereafter for up to one hour.
Subsequently, without relocation of the animal, an injection of technetium-labeled macroaggregated albumin (18 - 37 MBq 99mTc-MAA, particle sizes of 10 – 40 μm, Cardinal Health, Wauwatosa, WI) was made via the same cannula. The 0.5 ml MAA injectate consisted of 2.5 mg of aggregated human albumin, 5.0 mg of human albumin, 0.06 mg of stannous chloride, and 1.2 mg of sodium chloride. Ninety-five percent of the 99mTc was bound to the MAA. Images were then obtained at 1 frame per minute for 15 minutes. Because more than 95% of MAA lodges in the lung in proportion to flow, 99mTc-MAA is used commonly as a pulmonary perfusion marker (33). However in these studies, the purpose of the 99mTc-MAA injection was to provide rat thorax images in which the lung boundaries could be clearly identified in the planar images. After imaging the animals were euthanized with an overdose of pentobarbital sodium.
To determine whether lung uptake of either biomarker is saturable within the amounts used in our study, four sequential injections of either 99mTc-HMPAO (∼37 MBq per injection) or 99mTc-durmaycin (∼15 MBq per injection) were administered to the same control animal, and subsequently imaged for 3 minutes after each injection.
Image Analysis
First, the boundaries of the lungs were manually outlined in the high-sensitivity 99mTc-MAA images to determine a preliminary lung region of interest (ROI). Then, since HMPAO is taken up substantially by both the liver and the lungs, the lung ROI was truncated by drawing a horizontal boundary at the widest portion of the lung resulting in a lung (ROI) free of any liver contribution. This 99mTc-MAA lung ROI mask was then superimposed on the time sequence of biomarker (99mTc-HMPAO or 99mTc-durmaycin) images yielding lung biomarker ROIs. The resulting mean intra-operator variability in lung uptake measurements was 5.6%, using four repeated measurements on five different image sets. No registration was required since the animal was maintained in the same location for both the biomarker and 99mTc-MAA imaging procedures. Background regions in the upper forelimbs were also identified in the biomarker images to provide a normalization factor. Time-activity curves depicting mean counts/sec/pixel/injected dose within the lung and forelimb-background ROIs were then acquired from the time sequence of biomarker images. The ratio of the lung and background ROI curves at each time point was calculated, and the average value over the 10 – 15 minute post-injection time interval was used as the measure of lung tissue uptake for each rat (16).
The advantage of the in vivo planar imaging approach used in this study is that the equipment required is now readily available and affordable and the experimental methods and analysis are straightforward and provide highly sensitive data. Moreover, the use of a subsequent injection of 99mTc-MAA to determine the lung boundaries, rather than the use of dual-modality imaging, is an efficient and effective approach that greatly reduces the amount of post-processing required. The use of 99mTc-MAA also provides a unique means of studying regional pulmonary perfusion in models where blood flow may be altered due to injury or disease. Finally, we acquired planar images throughout the time-course of the dynamics of 99mTc-HMPAO and 99mTc-duramycin lung uptake. Although only the steady-state values of the time-activity curves are reported here, in future studies the complete curve in conjunction with a pharmacokinetic model will be used to further investigate mechanisms involved in hyperoxic lung injury.
Results
Figure 1 shows the mean of rat body weights at the time of imaging as a percent of pre-exposure body weight. Weight loss was greatest at 7 days of exposure to 85% O2, after which the animals began to gain weight. At 21 days of exposure, body weight was significantly higher than at 7 days.
Figure 1.
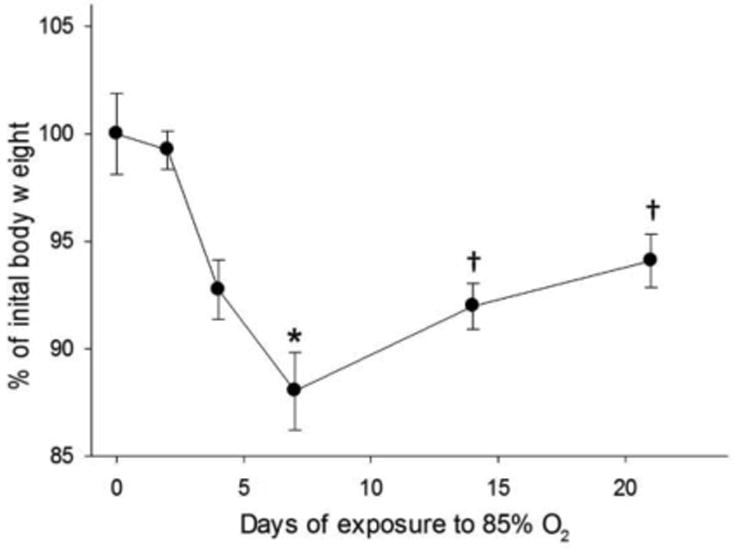
Rat body weight at time of imaging study as a percent of pre-exposure body weight. Values are mean ± SE. *Significantly different from control (normoxia), p < 0.05; † Significantly different from 7-days, p < 0.05.
A typical planar image of 99mTc-HMPAO distribution acquired ten minutes post-injection is shown in figure 2 (panel A.). Figure 2 (panel B.) is an image from the same animal following the 99mTc-MAA injection, where lung activity is sufficiently high for reliable identification of the lung boundaries. As described above, the lung ROI from the MAA image was superimposed on the corresponding 99mTc-HMPAO image, background ROIs and lung-only ROIs were drawn, and mean background and lung activity was determined.
Figure 2.
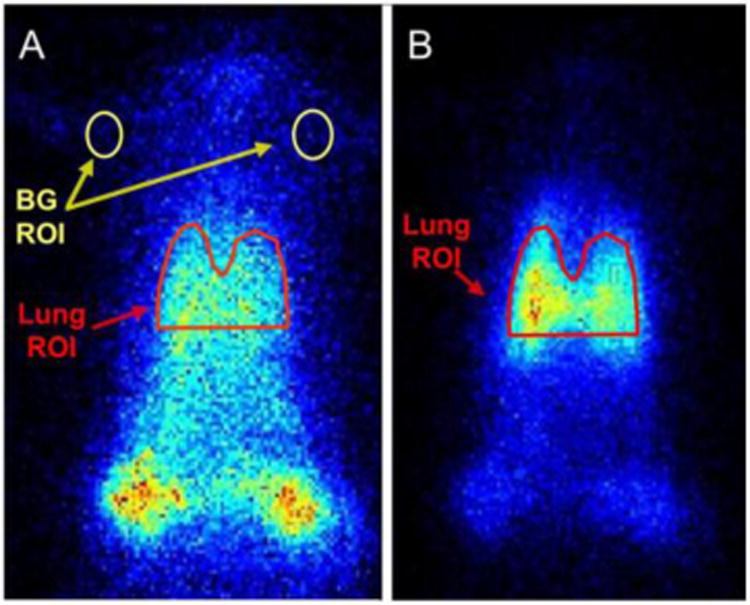
Planar images of 99mTc-HMPAO (panel A.) and 99mTc-MAA (panel B.) distribution in a control rat. A lung region-of-interest (ROI) is determined in the MAA image and used to identify a lung ROI in the HMPAO image. Background (BG) regions are identified for subsequent calculation of the lung-to-background ratio. Lung region above the horizontal boundary of the ROI is free of any liver contribution. Color indicates counts/sec/pixel/mCi injected.
The time-sequence of images acquired during repeated injections of either 99mTc-HMPAO or 99mTc-duramycin were analyzed by positioning ROIs over the upper lung and forelimb background regions and computing the difference between the mean lung and background signal at the end of each three minute acquisition. Lung minus background activity of both 99mTc-HMPAO and 99mTc-duramycin increased linearly following repeated injections in a control rat (figure 3). This linear response indicates that lung uptake of either agent is not saturating and also that incoming photons are not saturating the detection camera and/or electronics. The linearity is consistent with the lung-to-background ratio being a constant value independent of dose, so that differences in administered 99mTc-HMPAO or 99mTc-duramycin dose between animals should have no significant effect on the lung-to-background measure of uptake. Lack of saturation with each biomarker within the dose range studied is important for future experiments where it will be possible to increase the activity of each injection if necessary for adequate sensitivity and count statistics and suggests that when investigating acute responses to lung manipulations, an individual rat may serve as its own control with repeated injections. Furthermore, the protocol could be modified to include an initial injection of 99mTc-HMPAO followed by a subsequent injection of 99mTc-duramycin after waiting a sufficient amount of time for 99mTc-HMPAO in the lung to reach steady state, i.e., ∼15 minutes.
Figure 3.
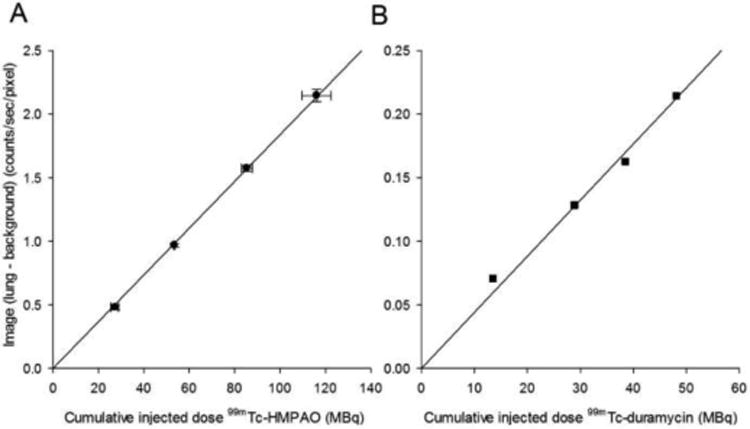
Lung (corrected for background) activity measured from images obtained following repeated biomarker injections ∼3 minutes apart in control rats. Panel A: ∼37 MBq injections of 99mTc-HMPAO, N = 2, r2= 0.99. Panel B: ∼15 MBq injections of 99mTc-duramycin, N = 1.
Figure 4 (top) shows typical 99mTc-HMPAO (panel A.) and 99mTc-duramycin (panel B.) lung and background time-activity curves obtained from images of control rats. For each biomarker, the first ∼20 seconds depict initial passage and distribution of the agent in the lung. Figure 4 (bottom) depicts the ratio of the lung-to-background curves, i.e. lung uptake, at each time point for the data in figure 4 (top).
Figure 4.
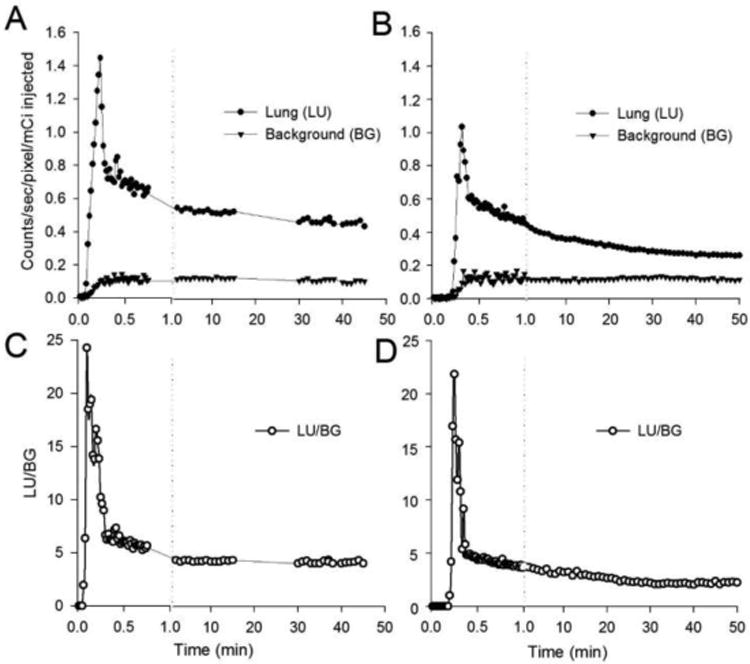
Top: Representative time-activity curves acquired from lung (circles) and background (triangles, upper forelimb) regions of 99mTc-HMPAO (panel A.) and 99mTc-duramycin (panel B.) planar images of control rats. Bottom: 99mTc-HMPAO (panel C.) and 99mTc-duramycin (panel D.) lung uptake calculated as the lung-to-background ratio for data in the top panels.
Representative images from a control (left) and 7-day hyperoxic (right) rat imaged with 99mTc-HMPAO (top) and 99mTc-duramycin (bottom) are shown in figure 5. Increased uptake of both agents can be observed in the hyperoxic rats. Summary results of lung uptake for 99mTc-HMPAO or 99mTc-duramycin for each hyperoxia treatment group as a function of the duration of hyperoxia exposure (number of days) is given in Table 1. Figure 6 shows lung uptake plotted as the percent change from control as a function of the number days of exposure. Lung uptake of both 99mTc-HMPAO and 99mTc-duramycin increased significantly up to day 7 of hyperoxia (74% and 51% respectively). Thereafter 99mTc-HMPAO uptake leveled off while 99mTc-duramycin accumulation decreased and reached its pre-exposure value by 21 days. These differences in lung uptake of 99mTc-HMPAO and 99mTc-duramycin during the course of hyperoxic lung injury may suggest cellular mechanisms involved in both initial injury and subsequent accommodation to the injury.
Figure 5.
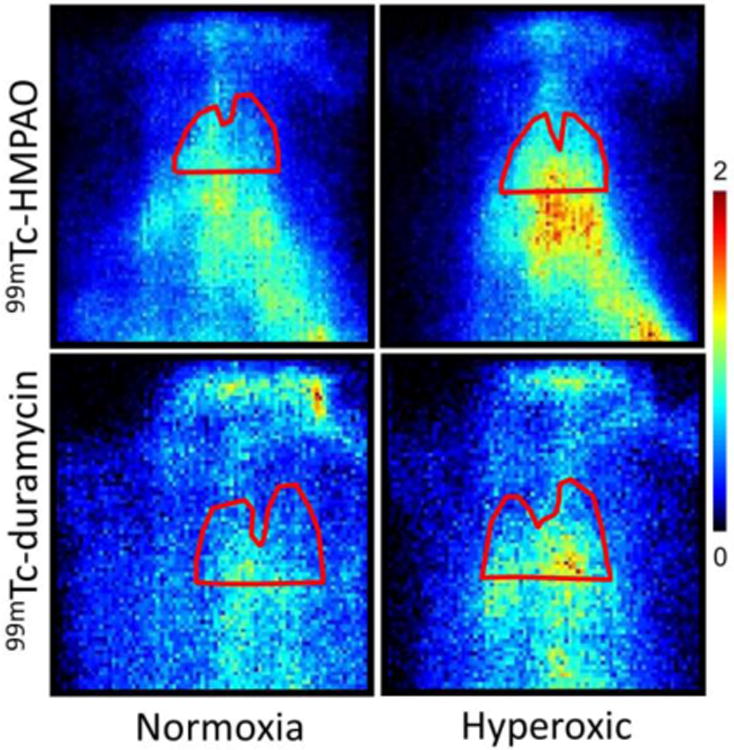
Planar images of a representative 99mTc-HMPAO (top) and 99mTc-duramycin (bottom) distribution in rats. Images were obtained from control (left, normoxia) and 7-days hyperoxic (right) rats. Lung boundaries were identified using a corresponding 99mTc-MAA image. Lung region above the horizontal boundary of the ROI is free of any liver contribution.
Table 1. Effect of Hyperoxia on Lung Uptake (LU/BG).
| Control | 2 Days | 4 Days | 7 Days | 14 Days | 21 Days | |
|---|---|---|---|---|---|---|
| 99mTc-HMPAO | 3.79 ± 0.28 | 4.56 ± 0.35 | 5.32 ± 0.30* | 6.59 ± 0.49* | 6.31 ± 0.81* | 6.55 ± 0.51* |
| N=8 | N=3 | N=4 | N=5 | N=4 | N=8 | |
|
| ||||||
| 99mTc-duramycin | 3.21 ± 0.12 | 3.37 ± 0.14 | 4.63 ± 0.12* | 4.86 ± 0.12* | 4.02 ± 0.11* | 3.35 ± 0.15 |
| N=6 | N=4 | N=5 | N=4 | N=3 | N=2 | |
All data are mean ± SE.
p < 0.05 when compared to control value.
Figure 6.
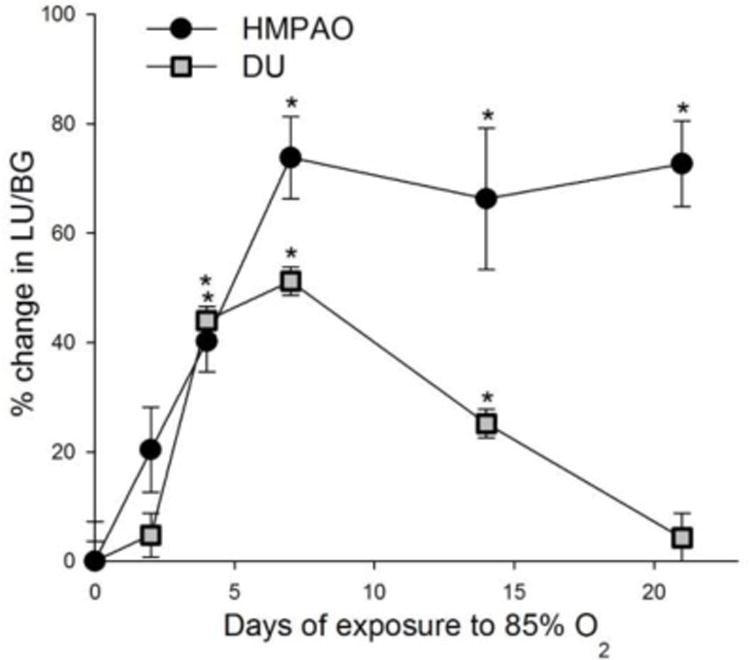
Percent increase from control (normoxia) in 99mTc-HMPAO (circles) and 99mTc-duramycin (DU, squares) lung uptake in rats exposed to 85% O2 for up to 21 days. Values are means ± SE. *Significantly different from control, p < 0.05.
Discussion
Although, there is a vast literature on histological and biochemical changes with hyperoxia lung injury (3,4,6,8), this is the first study to evaluate the progression of such lung injury in the hyperoxic rat model using noninvasive in vivo imaging of 99mTc-HMPAO or 99mTc-duramycin distribution. The hyperoxia-induced increase in 99mTc-HMPAO lung uptake measured here is consistent with previous results which also demonstrate an increase in 99mTc-HMPAO uptake in response to pulmonary oxidative stress (oxidant injury), including irradiation lung injury (22,25), inhalation injury (26,27) and cigarette smoking (28). Moreover, this is the first study to report on the pulmonary uptake of 99mTc-duramycin in an animal model of disease or injury. The observed changes in its uptake in this hyperoxia model suggest its potential utility as an in vivo marker of lung cell death.
Rat exposure to chronic hyperoxia resulted in increased lung uptake of both 99mTc-HMPAO and 99mTc-duramycin, however and most importantly, the time course of the increase was different for the two agents. 99mTc-HMPAO uptake in the lung reached a maximum by day 7 and remained elevated out to day 21. 99mTc-duramycin uptake also reached a maximum value at day 7 but then decreased at day 14 and returned to a near control level by day 21. These results are consistent with the extensive evidence that 85% O2 hyperoxic injury involves an early inflammatory phase (<7 days of exposure) characterized by significant loss of capillary endothelial cells, followed by a subsequent adaptation period (6). Thus, the pattern of uptake of these two biomarkers has the potential to identify the inflammatory phase of the injury and to provide information on biochemical and structural changes occurring within the lung over the time of exposure to high O2 levels.
The mechanisms that determine the lung tissue uptake of HMPAO are still not fully understood (14,19,21,34,35). HMPAO exists in two forms, lipophilic and hydrophilic. The more membrane permeable lipo- form readily diffuses into cells where it either is sequestered in the cell by conversion to the hydro- nondiffusible form or diffuses back out to the vasculature region. The relative importance of each of these processes to lung tissue uptake of HMPAO remains an open question. Jacquier-Sarlin et al. examined HMPAO retention in several brain cell lines (35). They showed using d,l-buthionine-sulfoximine (BSO) and N-acethyl cysteine (NAC), chemical agents which decrease or increase, respectively, glutathione content, that the cellular uptake of HMPAO was dependent in part on intracellular glutathione (GSH) content and thus cell redox status (35). Our previous study demonstrated that rat exposure to 85% O2 for 7 days does increase total glutathione content (8). There is also evidence that mitochondrial damage, by reducing metabolic activity, may influence cellular uptake of HMPAO (14,23,34). Our previous studies have also demonstrated a decrease in mitochondrial complex I activity, and an increase in mitochondrial complex III and IV activity with hyperoxia exposure (5,8). In addition, studies in brain and muscle cells suggest that the extracellular environment, by modifying the amount of lipophilic HMPAO available to lung cells either by systemic uptake or conversion of the lipo- to the hydro- form of HMPAO extracellularly, may influence HMPAO cellular uptake (14, 35,-37).
Another factor that must be recognized when interpreting changes in lung uptake of HMPAO in this hyperoxia model is the significant loss of endothelial cells over the time of exposure, i.e. capillary surface area is decreased to ∼50% and 60% of the control value at 7 and 14 days of exposure, respectively (6). Although our results cannot determine the type of cells that account for the lung tissue uptake of HMPAO, the pulmonary capillary endothelium with its large surface area and direct contact with the blood must certainly play a key role in HMPAO uptake. In addition, imaging measures of uptake are dependent on both the number of cells that take up HMPAO as well as the amount of HMPAO retained within the cell. Thus at 7 days of exposure for example, given the ∼75% increase in HMPAO lung uptake reported here, and a ∼50% decrease in capillary surface, it appears that cellular uptake of HMPAO increased by a factor of 3.5 compared to control lungs.
Duramycin binds the head group of PtdE with high affinity at a molar ratio f 1:1. PtdE is available for binding in apoptotic cells because of externalization and in necrotic cells when the plasma membrane is compromised (29,31). Using cultured lymphocytes, Zhao et al. demonstrated a 32 times greater uptake of duramycin in apoptotic cells as compared to control cells (30). Previous biodistribution studies in the rat showed small but measurable uptake of duramycin in the lungs of healthy control animals (30) which is consistent with the data presented here. Duramycin uptake in lungs of hyperoxic rats increased out to 7 days of hyperoxia exposure similar to HMPAO. However, in contrast to HMPAO, duramycin uptake then decreased and was the same as that measured in control animals by 21 days of exposure. In vivo lung uptake of duramycin reported in this study likely reflects overall cell death (32). In fact, the time course of increased duramycin uptake during the hyperoxic lung injury observed here (figure 5) appears to parallel the rate of loss of endothelial cells reported previously by Crapo (9) as well as the loss of body weight of the animals in this study (figure 1). Our proposed interpretation of the above results is that out to 7 days both HMPAO and duramycin lung uptake in hyperoxic rats increase due to increases in the redox status and apoptosis/necrosis respectively. After seven days the redox status remains high due the continued high O2 exposure (high HMPAO uptake) while apoptosis/necrosis and the rate of endothelial cell loss decrease (low duramycin uptake). In essence, imaging with these two agents has the potential to distinguish both the extent and different stages of the lung injury.
In this study we opted to use in vivo planar imaging with a single modular gamma camera. The advantage of this approach over full 3D SPECT is that the equipment required is readily available and affordable and the experimental methods and analysis are straightforward. Moreover, hyperoxic lung injury is thought to be a relatively homogeneous injury throughout the lung so that SPECT would not be expected to provide any additional information about total HMPAO or duramycin retention within the lung. Nonetheless, future studies utilizing 3-dimensional SPECT will facilitate delineation of the entire lung without concern for liver contribution as well as regional analysis within the lung.
Conclusion
In this study the effect of hyperoxia on the lung uptake of radiolabeled HMPAO and duramycin was evaluated in vivo. The results suggest that the pattern of the change in biomarker uptake could be useful for differentiating the early inflammatory phase from the subsequent adapted phase of this lung injury model. This delineation is important because patients requiring high O2 come with differing tolerances of hyperoxia based upon genetics, pre-conditioning, or other factors; real-time information that would permit clinicians to determine which patients are developing O2 toxicity or tolerance could be of significant value (38). In conclusion, the results of this study demonstrate substantial uptake of these agents in both normal and injured lung tissue, suggesting their potential clinical utility as pulmonary injury biomarkers, and suggests an approach for evaluating the utility of other SPECT biomarkers for assessing lung injury.
Acknowledgments
This work was supported in part by NIH UL1RR031973 (A.V. Clough), NHLBI 24349 (A.V. Clough, S.H. Audi, and D.L. Roerig) and Department of Veterans Affairs (D.L. Roerig).
We are grateful to Dr. Ming Zhao (Northwestern University) for producing the duramycin kits.
References
- 1.Capellier G, Maupoil V, Boussat S, Laurent E, Neidhardt A. Oxygen toxicity and tolerance. Minerva Anestesiol. 1999;65:388–392. [PubMed] [Google Scholar]
- 2.Fisher AB, Beers MF. Hyperoxia and acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2008;295:L1066. doi: 10.1152/ajplung.90486.2008. author reply L1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher AB, Forman HJ, Glass M. Mechanisms of pulmonary oxygen toxicity. Lung. 1984;162:255–259. doi: 10.1007/BF02715655. [DOI] [PubMed] [Google Scholar]
- 4.Brueckl C, Kaestle S, Kerem A, et al. Hyperoxia-induced Reactive Oxygen Species Formation in Pulmonary Capillary Endothelial Cells in situ. Am J Respir Cell Mol Biol. 2006;34(4):453–463. doi: 10.1165/rcmb.2005-0223OC. [DOI] [PubMed] [Google Scholar]
- 5.Audi SH, Merker MP, Krenz GS, Ahuja T, Roerig DL, Bongard RD. Coenzyme Q1 redox metabolism during passage through the rat pulmonary circulation and the effect of hyperoxia. J Appl Physiol. 2008;105:1114–1126. doi: 10.1152/japplphysiol.00177.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crapo JD, Barry BE, Foscue HA, Shelburne J. Structural and biochemical changes in rat lungs occurring during exposures to lethal and adaptive doses of oxygen. Am Rev Respir Dis. 1980;122:123–143. doi: 10.1164/arrd.1980.122.1.123. [DOI] [PubMed] [Google Scholar]
- 7.Matute-Bello G, Frevert CW, Martin TR. Animal models of acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2008;295:L379–L399. doi: 10.1152/ajplung.00010.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gan Z, Roerig DL, Clough AV, Audi SH. Differential responses of targeted lung redox enzymes to rat exposure to 60 or 85% oxygen. J Appl Physiol. 2011;111:95–107. doi: 10.1152/japplphysiol.01451.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramakrishna M, Gan Z, Clough AV, Molthen RC, Roerig DL, Audi SH. Distribution of capillary transit times in isolated lungs of oxygen-tolerant rats. Ann Biomed Eng. 2010;38:3449–3465. doi: 10.1007/s10439-010-0092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Audi SH, Olson LE, Bongard RD, Roerig DL, Schulte ML, Dawson CA. Toluidine blue O and methylene blue as endothelial redox probes in the intact lung. Am J Physiol Heart Circ Physiol. 2000;278:H137–H150. doi: 10.1152/ajpheart.2000.278.1.H137. [DOI] [PubMed] [Google Scholar]
- 11.Audi SH, Bongard RD, Dawson CA, Siegel D, Roerig DL, Merker MP. Duroquinone reduction during passage through the pulmonary circulation. Am J Physiol (Lung Cell Mol Physiol) 2003;285:L1116–L1131. doi: 10.1152/ajplung.00185.2003. [DOI] [PubMed] [Google Scholar]
- 12.Audi SH, Bongard RD, Krenz GS, et al. Effect of chronic hyperoxic exposure on duroquinone reduction in adult rat lungs. Am J Physiol Lung Cell Mol Physiol. 2005;289:L788–797. doi: 10.1152/ajplung.00064.2005. [DOI] [PubMed] [Google Scholar]
- 13.Catafau AM. Brain SPECT in clinical practice Part I: Perfusion. J Nucl Med. 2001;42:259–271. [PubMed] [Google Scholar]
- 14.Gardner A, Pagani M, Beier H, Jacobsson H, Larsson S, Hallstrom T. 99mTc-HMPAO distribution at SPECT is associated with succinate-cytochrome c reductase (SCR) activity in subjects with psychiatric disorders. Nucl Med Biol. 2004;31:277–282. doi: 10.1016/S0969-8051(03)00130-6. [DOI] [PubMed] [Google Scholar]
- 15.Habert MO, Horn JF, Sarazin M, et al. Brain perfusion SPECT with an automated quantitative tool can identify prodromal Alzheimer's disease among patients with mild cognitive impairment. Neurobiol Aging. 2011;32:15–23. doi: 10.1016/j.neurobiolaging.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 16.Kaya GC, Ertay T, Tuna B, et al. Technetium-99m hexamethylpropylene amine oxime lung scintigraphy findings in low-dose amiodarone therapy. Lung. 2006;184:57–61. doi: 10.1007/s00408-005-2562-3. [DOI] [PubMed] [Google Scholar]
- 17.Nobili F, Koulibaly PM, Rodriguez G, et al. 99mTc-HMPAO and 99mTc-ECD brain uptake correlates of verbal memory in Alzheimer's disease. Q J Nucl Med Mol Imaging. 2007;51:357–363. [PubMed] [Google Scholar]
- 18.Eicker SO, Turowski B, Heiroth HJ, Steiger HJ, Hänggi D. A comparative study of perfusion CT and 99m Tc-HMPAO SPECT measurement to assess cerebrovascular reserve capacity in patients with internal carotid artery occlusion. Eur J Med Res. 2011;16:484–490. doi: 10.1186/2047-783X-16-11-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oku N, Kashiwagi K, Hatazawa J. Nuclear neuroimaging in acute and subacute ischemic stroke. Ann Nucl Med. 2010;24:629–638. doi: 10.1007/s12149-010-0421-7. [DOI] [PubMed] [Google Scholar]
- 20.Andersen AR, Friberg H, Knudsen KBM, et al. Extraction of [99mTc]-d,l-HM-PAO across the blood-brain barrier. J Cereb Blood Flow Metab. 1988;1:S44–S51. doi: 10.1038/jcbfm.1988.32. [DOI] [PubMed] [Google Scholar]
- 21.Inoue K, Nakagawa M, Goto R, et al. Regional differences between 99mTc-ECD and 99mTc-HMPAO SPET in perfusion changes with age and gender in healthy adults. Eur J Nucl Med Mol Imaging. 2003;30:1489–1497. doi: 10.1007/s00259-003-1234-x. [DOI] [PubMed] [Google Scholar]
- 22.Liu FY, Shian YC, Huang WT, Kao CH. Usefulness of technetium-99m hexamethylpropylene amine oxime lung scan to detect sub-clinical lung injury of patients with breast cancer after chemotherapy. Anticancer Res. 2003;23:3505–3507. [PubMed] [Google Scholar]
- 23.Hang LW, Shiau YC, Hsu WH, Tsai JJ, Yeh JJ, Kao A. Increased lung uptake of technetium-99m hexamethylpropylene amine oxime in diffuse infiltrative lung disease. Respiration. 2003;70:479–83. doi: 10.1159/000074203. [DOI] [PubMed] [Google Scholar]
- 24.Suga K, Uchisako H, Nishigauchi K, et al. Technetium-99m-HMPAO as a marker of chemical and irradiation lung injury: experimental and clinical investigations. J Nucl Med. 1994;35:1520–7. [PubMed] [Google Scholar]
- 25.Kuo SJ, Yang KT, Chen DR. Objective and noninvasive detection of sub-clinical lung injury in breast cancer patients after radiotherapy. Eur J Surg Oncol. 2005;31:954–957. doi: 10.1016/j.ejso.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Hung CJ, Liu FY, Shaiu YC, Kao A, Lin CC, Lee CC. Assessing transient pulmonary injury induced by volatile anesthetics by increased lung uptake of technetium-99m hexamethylpropylene amine oxime. Lung. 2003;181:1–7. doi: 10.1007/s00408-002-0109-4. [DOI] [PubMed] [Google Scholar]
- 27.Shiau YC, Liu FY, Tsai JJ, Wang JJ, Ho ST, Kao A. Usefulness of technetium-99m hexamethylpropylene amine oxime lung scan to detect inhalation lung injury of patients with pulmonary symptoms/signs but negative chest radiograph and pulmonary function test findings after a fire accident--a preliminary report. Ann Nucl Med. 2003;17:435–438. doi: 10.1007/BF03006430. [DOI] [PubMed] [Google Scholar]
- 28.Shih WJ, Rehm SR, Grunwald F, et al. Lung uptake of Tc-99m HMPAO in cigarette smokers expressed by lung/liver activity ratio. Clin Nucl Med. 1993;18:227–30. doi: 10.1097/00003072-199303000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Emoto K, Toyama-Sorimachi N, Karasuyama H, Inoue K, Umeda M. Exposure of phosphatidylethanolamine on the surface of apoptotic cells. Exp Cell Res. 1997;232:430–434. doi: 10.1006/excr.1997.3521. [DOI] [PubMed] [Google Scholar]
- 30.Zhao M, Li Z, Bugenhangen S. 99mTc-labeled duramycin as a novel phosphatidylethanolamine-binding molecular probe. J Nucl Med. 2008;49:1345–1352. doi: 10.2967/jnumed.107.048603. [DOI] [PubMed] [Google Scholar]
- 31.Zhao M. Lantibiotics as probes for phosphatidylethanolamine. Amino Acids. 2011;41:1071–1079. doi: 10.1007/s00726-009-0386-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mantell LL, Horowitz S, Davis JM, Kazzaz JA. Hyperoxia-induced cell death in the lung--the correlation of apoptosis, necrosis, and inflammation. Ann NY Acad Sci. 1999;887:171–180. doi: 10.1111/j.1749-6632.1999.tb07931.x. [DOI] [PubMed] [Google Scholar]
- 33.Bajc M, Neilly JB, Miniati M, Schuemichen C, Meignan M, Jonson B EANM Committee. EANM guidelines for ventilation/perfusion scintigraphy: Part 1. Pulmonary imaging with ventilation/perfusion single photon emission tomography. Eur J Nucl Med Mol Imaging. 2009;36:1356–70. doi: 10.1007/s00259-009-1170-5. [DOI] [PubMed] [Google Scholar]
- 34.Fujibayahsi Y, Taniudhi H, Waki A, Yokoyama A, Ishii Y, Yonekura Y. Intracellular mechanism of 99mTc-d,l-HMPAO in vitro: A basic approach for understanding the hyperfixation mechanism in damaged brain. Nucl Med Biol. 1998;25:375–378. doi: 10.1016/s0969-8051(97)00221-7. [DOI] [PubMed] [Google Scholar]
- 35.Jacquier-Sarlin MR, Polla BS, Slosman DO. Cellular basis of ECD brain retention. J Nucl Med. 1996;37:1694–1697. [PubMed] [Google Scholar]
- 36.Sasaki T, Toyama H, Oda K, Ogihara-Umeda I, Nishigori H, Senda M. Assessment of antioxidative ability in brain: Tc-99m-meso-HMPAO as an imaging agent for glutathione localization. J Nucl Med. 1996;37:1698–1701. [PubMed] [Google Scholar]
- 37.Shimura N, Musya A, Hashimoto T, Kojima S, Kuboder A, Sasaki T. Usefulness of (99m)Tc-d,l-HMPAO for estimation of GSH content in tumor tissues. Nucl Med Biol. 2000;27:577–580. doi: 10.1016/s0969-8051(00)00131-1. [DOI] [PubMed] [Google Scholar]
- 38.Phua J, Badia JR, Adhikari NK, et al. Has mortality from acute respiratory distress syndrome decreased over time?: A systematic review. Am J Respir Crit Care Med. 2009;179:220–227. doi: 10.1164/rccm.200805-722OC. [DOI] [PubMed] [Google Scholar]


