Abstract
Background
Trichomonas vaginalis is a protozoan parasite that occurs in the urogenital-vaginal tract and is the primary causative agent of trichomoniasis, a common sexually transmitted disease in humans. The aggregation of this protozoan tends to destroy epithelial cells and induce pathogenesis.
Principal Findings
This study cultured T. vaginalis and human cervical epithelial cells (Z172) under the same conditions in the experiments. Following co-culturing for ten hours, the protozoans became attached to Z172, such that the cells presented a round shape and underwent shrinkage. Time-lapse recording and flow cytometry on interacted Z172 revealed that 70% had been disrupted, 18% presented a necrosis-like morphology and 8% showed signs of apoptosis. Gene expression profiling revealed in the seven inflammatory Z172 genes as well as in T. vaginalis genes that code for adhesion proteins 65 and 65-1.
Significance
These results suggest that cytopathogenic effects progress while Z172 is in contact with T. vaginalis, and the resulting morphological changes can be categorized as disruption.
Introduction
Trichomonas vaginalis, an anaerobic and flagellated parasitic protozoan, is a causative agent of trichomoniasis, one of the most common sexually transmitted disease (STD) [1]. In men, this infection is usually asymptomatic; however irritating urethritis or prostatitis occurs in a few cases. In women, the disease is associated with a wide spectrum of symptoms, ranging from a relatively asymptomatic state to severe inflammation [2]. Ten percent of infections present with a "strawberry cervix" or vagina on examination. Previous studies have reported that the presentation of T. vaginalis increases the risk of acquiring HIV [3–6]. A great deal is known about trichomoniasis; however, the pathogenic mechanisms and influences of host-parasite interactions remain largely undefined. Adhesion is believed to play an important role in the onset of infection and the T. vaginalis cytolysis of human epithelial cells is contact dependent [7–11]. Adhesion of T. vaginalis to red blood cells [10], or those of the prostate or ectocervical epithelium [11] triggers the degradation of the host cell membrane skeleton, which can lead to cytolysis.
Previous research into the molecular aspects of T. vaginalis adhesion to human cells has identified a number of adhesion molecules on the surface of the parasite, the proteins of which include AP65, AP51, AP33, and AP23 [12, 13]. Among these, AP65 is the prominent protein mediating the binding of parasites to host epithelial cells [14–17]. Little is known about the molecules binding the parasites to the host cell receptors; however, a growing body of evidence suggests that Laminin may be a target in trichomonad adhesion [18–20]. The only host cell receptor of T. vaginalis, galectin-1, has been identified on cervical epithelial cells and has been shown to bind to T. vaginalis lipoglycan (TVLG) [21].
The T. vaginalis trophozoites colonize and parasitize the vagina or prostate of infected hosts. The trophozoite divides by binary fission and, in natural infections, gives rise to a population in the lumen and on the mucosal surfaces of the urogenital tracts of humans. The trophozoite is oval and flagellated; however, the parasite develops an amoeboid morphology when adhering to epithelial cells [22]. As the parasite multiplies in it’s amoeboid stage, it attaches to the squamous epithelium in the genital tract, causing inflammation of the vagina. During menstruation, the environment of the vagina changes, resulting in an increase in the severity of clinical symptoms and the rapid growth of protozoa. The overall immune response during trichomoniasis is largely unknown and high levels of interleukin-8 (IL-8) [23] and leukotreine B4 (LTB4) have been identified in the vaginal secretions of patients symptomatic with trichomoniasis [24–27].
This study established a co-culture system to investigate the interaction of T. vaginalis with the human cervical epithelial cells, Z172, in order to gain a deeper understanding of the mechanism underlying the pathogenesis of T. vaginalis. Our aim was to reveal the alterations that occur in morphology and gene expression due to the interactions between T. vaginalis and epithelial cells.
Methods
Cell culture
Trichomonas vaginalis strain ATCC 30236 (JH31A, USA), were cultured axenically at 37°C in iron free Yeast extract, Iron-Serum (YI-S) medium [28] supplied with 2% haemoglobin and medium supplemented with 10% Nu-serum. Organisms grew to mid-log phase were used in the subsequent experiments. Human cervical epithelial cells (Z172) was culture in pH 7.2 low glucose Dulbecco's modified Eagle's medium (DMEM), which supplemented with 10% Nu-serum and 2% hemoglobin bovine at 37°C incubator in the presence of 5% CO2. After adaptation of the T. vaginalis and Z172 cells were cultured in the same culture condition (DMEM-YI-S medium (2:1, vol/vol)).
Adaptation of T. vaginalis and Z172
Trichomonas vaginalis
Addition DMEM medium in YI-S medium have been in continuous culture for 20 serial passages arrives at DMEM-YI-S medium. Medium joins the half new DMEM: YI-S-2:1 medium. Finally, T. vaginalis were cultured in the DMEM-YI-S medium (2:1, vol/vol) and supplied with 2% haemoglobin.
Z172 cell
Addition YI-S medium in DMEM medium have been in continuous culture for serial passages in the same culture condition DMEM-YI-S medium. Medium joins the half new DMEM-YI-S medium (2:1, vol/vol) and supplied with 2% haemoglobin.
Growth curves
T. vaginalis were cultured in the YI-S and DMEM-YI-S medium (2:1, vol/vol) supplied with 2% haemoglobin. Detached cells were centrifuged and the pellet was resuspended in a 0.5% trypan blue solution in sterile PBS for one min. Cells were then counted in a neubauer hemocytometer chamber, and the stained cells were considered dead. Cell counting was performed under light microscope every six hours in the duration of forty-two hours to get the numbers of alive and dead cell, which were differentiated by the trypan blue dye exclusion viability method. The number of stained cells was subtracted from the total, indicating the death ratio in each interaction condition and time.
Cell proliferation assay
Z172 were cultured in the low glucose DMEM and DMEM-YI-S medium (2:1, vol/vol) with supplied with 2% haemoglobin. Z172 were seeded to 24-well polypropylene culture plate, respectively. The cultures were incubated at 37°C, 5% CO2. After overnight, the medium was replaced and 50 ul of MTT (1mg/ml) was added to each well at 37°C and 5% CO2 for 4 h. After incubation, the cultures were removed the medium and addition DMSO. The absorbance was measured on ELISA Microwell Reader at 590/630 nm. Mann-Whitney U test was used for the significant test in the study.
Viability test assay
Z172 cells were grown on 24-well of polypropylene culture plate and cultures were incubated at 37°C, 5% CO2. After parasites interaction with Z172 the medium was replaced and 50 μl of MTT (1 mg/ml) added to each well at 37°C and 5% CO2 for 4 hours. Cultures were removed the medium and addition DMSO for each sample. The absorbance was measured on ELISA Microwell Reader at 590/630 nm.
Visualze cytoskeletal rearrangements in infected cells
Using the Lipofectamine 2000 for the transfection of nucleic acids of pAcGFP1-actin vector (green fluorescent protein and cytoskeleton targeting sequence) was applied for the transfection DNA, and we for the label of actin. The DNA mixture was then incubated at room temperature for an additional 30 min to allow complex formation. Z172 cells were washed twice with phosphate-buffered saline and DMEM without serum.
Light and fluorescent
The image analysis is uses for the software of CellR (Olympus America, Inc., Melville, NY). It is used for the observation the changes of cells after T. vaginalis attacking.
Flow cytometry
The propidium iodide (PI) intercalates into the major groove of double-stranded DNA and produces a highly fluorescent adduct that can be excited at 488 nm with a broad emission centred around 600 nm. It can be used to quantitate apoptosis by flow cytometry. The system was performed according to the protocol established by Riccardi and Nicoletti [29].
RNA extraction
The total RNA of T. vaginalis and Z172 cells were extracted with TRIzol Plus RNA purification system reagent (Invitrogen) for the following experiment such as SuperArray and reverse transcription polymerase chain reaction (RT-PCR). Briefly, Z172 cells were seeded onto 10cm2 culture dish and allowed to form a monolayer for 2 days. Cells were washed with a medium mixture of DMEM-YI-S (2:1, vol/vol) without serum. Protozoa, which in the mid-logarithmic phase of growth, were added to the Z172 monolayer at Z172- T. vaginalis ratio of 1:10 and incubated at 37°C to allow for parasite adherence. Parasites were incubated with the Z172 cells within 12 hours, and non-adherent parasites were removed by aspiration. The detail procedures were processed according to the manufacturer’s protocol. The entire concentration and A260/A280 ratio of mRNA was measured with ND-1000 (NanoDrop).
Reverse transcription PCR
One step reverse transcription PCR was performed with SuperScript One-Step RT-PCR with Platinum Taq kit (Invitrogen) to investigate the gene expression of T. vaginalis of ap65 [30]、β-tubulin and ap65-1 [31]. All the cDNA was synthesized from 1 μg of total RNA of T. vaginalis and Z172. RT-PCR product separated on EtBr-stained gel after electrophoresis in 1.0–1.2% agarose. The rest procedures were processed according to the manufacturer’s protocol. Primers were listed in S1 Table.
Oligo GEArray
The Oligo GEArray Human Common Cytokines Microarray profiles (Cat. No. OHS-021) can be detected the expression of 114 important cytokine genes. Also represented are colony-stimulating factors and various growth factors (fibroblast, insulin-like, platelet-derived, transforming, and vascular endothelial). Tumor necrosis factors are included as well as other cytokine-related genes. Through a simple side-by-side hybridization experiment determine differential gene expression. The we add 5 μg aliquots of mRNA samples from Z172 cells by TrueLabeling primer and cDNA synthesis buffer and cDNA synthesis Enzyme mix (SABiosciences, USA) for cDNA synthesis. Next step for cDNA amplification were using Biotinylated-UTP and RNA polymerase buffer and RNA polymerase Enzyme. cRNA synthesis reaction and purification were using cRNA Cleanup Kit. The purified and concentrated cRNA for the experimental samples were mixed, and a hybridization mixture was prepared in GEAhyb Hybridization solution and hybridization tubes add cRNA target hybridization mix at 60°C, 5–10 rpm, in hybridization oven incubators, overnight. Chemiluminescent detection in 37°C pre-warm GEAblocking solution Q and 5X buffer at room temperature. Finally, discard buffer, repeat two times and rinse with 3 ml buffer G, invert three times and 1 ml CDP-star chemiluminescent substrate and detection by UV Photometer.
Results
Effects of adaptation of T. vaginalis and Z172 cells in co-culture medium
This study established a co-culture system to characterize the interaction between T. vaginalis and host cells. After adapting T. vaginalis from pH 5.8 to 7.2 in YIS medium, we added DMEM medium serially until reaching a volume ratio of DMEM-YIS (co-culture) medium of 2:1. No significant difference was observed in the morphology of T. vaginalis following twenty passages of adaptation (S1A and S1C Fig). To verify the effects of adaptation on the growth curve of parasites, we monitored the T. vaginalis by counting the number of cells stained with trypan blue solution in a neubauer hemocytometer chamber. The time required for the doubling of T. vaginalis were 4, 5.8, and 6.7 hours in pH5.8 YIS, pH7.2 YIS, and DMEM-YIS medium, respectively. The growth rate of T. vaginalis was slower in co-culture medium; however, the parasite density still reached 2x106 cells per ml.
Z172 cells were also adapted from pH 7.2 DMEM to co-culture medium. Again, no difference was observed between the morphology (S1B and S1D Fig) or growth curves of Z172 cells in DMEM and the co-culture medium. Images were taken every 30 minutes using a differential interference contrast microscope to facilitate the long-term observation of Z172 cells in co-culture medium. Our results showed no effect on the growth of the cells (S2 Fig).
Appropriate ratio of parasites and Z172 cells in co-culture system for the study of pathogenesis
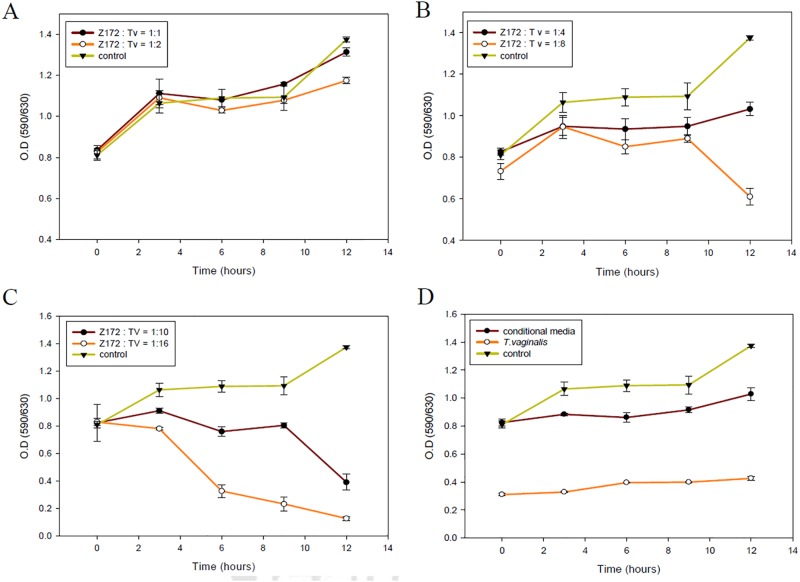
To determine the interaction level of T. vaginalis with Z172 cells, we performed a preliminary experiment using various parasite densities (1:1, 2:1, 4:1, 8:1, 10:1 and 16:1). Parasites interacting with Z172 cultures were monitored once every 2 h for the first 12 h. Our results showed that at a parasite:Z172 ratio of 1:1 or 2:1, the growth of Z172 cells remained unaffected (Fig 1A). When the parasite:Z172 ratio was increased to 4:1, 8:1, or 10:1, the growth of Z172 cells slowed slightly (Figs 1B and 2C). When the ration was increased to 16:1, cellular damage was too extensive to allow for further analysis (Fig 1C). Thus, we selected a parasite:Z172 ratio of 10:1 for subsequent experiments.
Fig 1. The cell viability of the co-cultured T. vaginalis and Z172 cells in different ratio.
The cell viabilities of Z172 cells which were co-cultured with the ratio of parasite density, 1:1 and 1:2 (A), 1:4 and 1:8 (B), 1:10 and 1:16 (C), were tested by MTT assay during 12 hours. The conditional media means that Z172 cells were cultured with the medium ever cultured T. vaginalis (D).
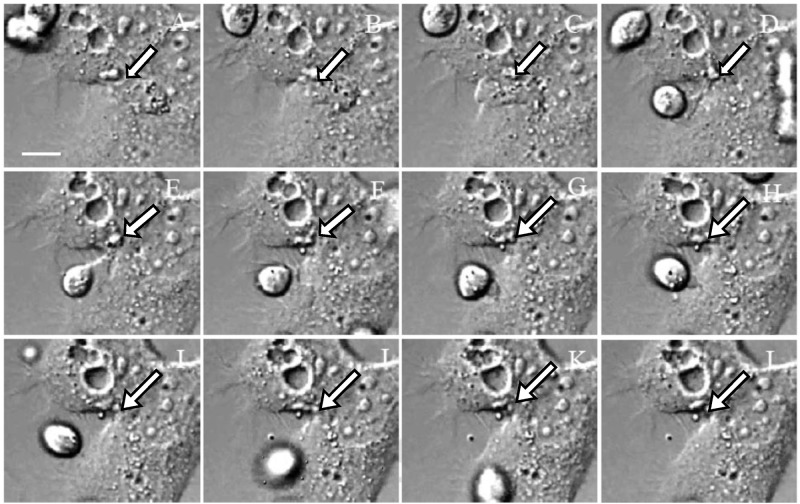
Fig 2. The light observation for the live Z172 cells imaging by time-lapse recording.
The light observation (Differential interference contrast microscopy) of the progress of Z172 cells which was transfected pAcGFP1-Actin after co-cultured with T. vaginalis in 1:10. Panel A to L were the captured images once every 30 minutes. The arrows indicate the position of the cell gap.
Morphological changes in Z172 cells caused by adherence of T. vaginalis
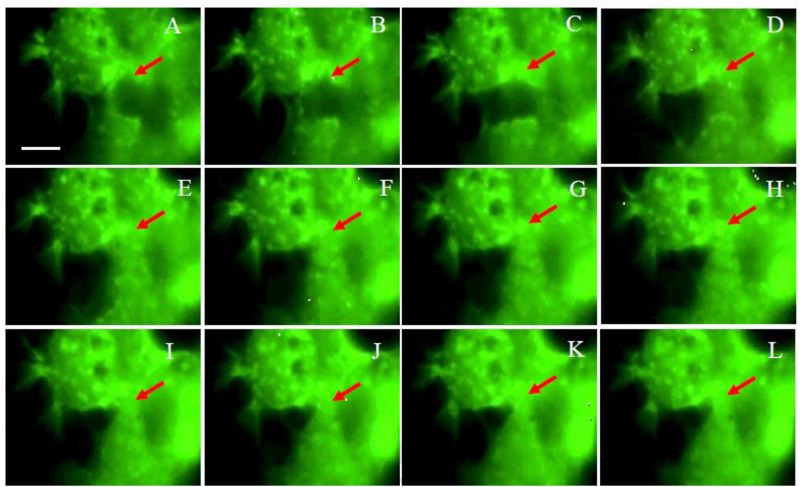
To identify the morphological changes in Z172 cells attacked by T. vaginalis, this study transfected pAcGFP-actin into Z172 cells co-cultured with parasites. Images were taken every 30 minutes using a differential interference contrast microscope to facilitate the long-term observation of Z172 cells in co-culture medium (Fig 2) and fluorescence microscope (Fig 3). These results clearly indicate that the attachment of T. vaginalis initiated damage to the Z172 cells. As incubation time was extended, the adhesion of T. vaginalis induced changes in the shape of Z172 cells and an increase in the distance between cells. These results prove once again that the cytotoxicity of T. vaginalis begins at the time of initial attachment. The adhesion of T. vaginalis induced death in the host cell as well as the destruction of the cell-cell junction, which triggered a disruption to the epithelial cells. We also prolonged the monitoring period in order to observe Z172 cells cultured with inactive T. vaginalis (S3 Fig) as well as those in parasite cultured medium (S4 Fig). The results of these experiments showed that only living T. vaginalis induced damage through contact.
Fig 3. The fluorescence observation for the live Z172 cells imaging by time-lapse recording.
The fluorescent observation of the progress of Z172 cells which was transfected pAcGFP1-Actin after co-cultured with T. vaginalis in 1:10. Panel A to L were the captured images once every 30 minutes. The arrows indicate the position of the cell gap.
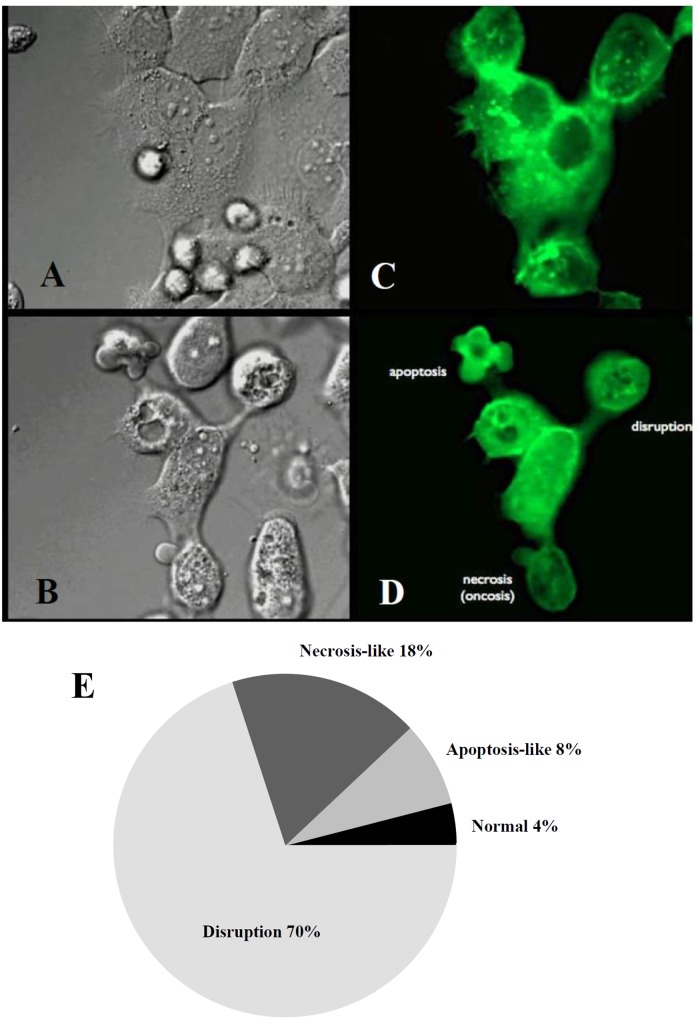
Following co-culturing with T. vaginalis for 10 hours, three types of cell morphological changes were observed in the Z172 cells: disruption, necrosis-like cell death, and apoptosis-like cell death (Fig 4B and 4D; S1–S6 Video). Time-lapse photography was used to record changes in the shape of Z172 cells in order to facilitate further analysis and statistical observation, the results of which showed that 70% of cells had undergone disruption, 18% of cells were necrosis-like, 8% of cells were apoptosis-like, and 4% of cells did not present significant morphological changes (Fig 4E). These results lead to the conclusion that after being attacked by T. vaginalis, Z172 cells shrink, become more spherical, and the gap between the cells becomes larger, but the main mode of disruption is by way of cell death.
Fig 4. The morphological change of Z172 cells after co-cultured with T. vaginalis.
Panel A and B were light observed before and after co-cultured 10 hours, Panel C and D were captured in fluorescent observation. Bar = 10 μm. The statistical results of the cell morphological changes were shown in panel E.
Cell cycle phase of Z172 cells co-cultured with T. vaginalis
This study used the PI staining of DNA to study the effects of T. vaginalis on the cell cycle phase of Z172 cells. The results were then confirmed by flow cytometry showing that most of the Z172 cells were arrested in the G0/1 phase and a small fraction in the sub-G0/1 phase. No significant differences in Z172 cell cycle phase profiles were observed after further interaction between parasites and Z172 cells (S5 Fig). This suggests that the cell damage caused by T. vaginalis is unrelated to cell cycle progression.
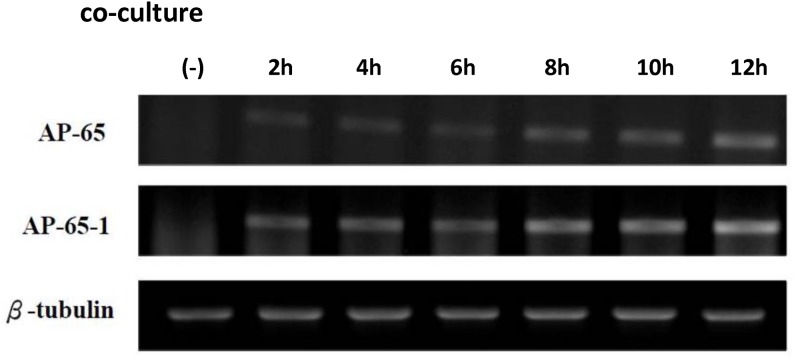
Increased RNA expression levels in T. vaginalis AP65 and AP65-1 with co-culture time
We next surveyed differences in the gene expression of parasites and host cells throughout the co-culture process. We used primers specific to ap65 and ap65-1of T. vaginalis in order to detect the RNA expression levels of the adhesion proteins by RT-PCR. Our results showed that the expression levels of ap65 and ap65-1 in T. vaginalis increased with an extension of co-culture time (Fig 5).
Fig 5. The gene expression of T. vaginalis which co-cultured with Z172 cells.
The changes of gene expression levels of T vaginalis after interacted with Z172 cells were investigated by RT-PCR. The RT-PCR products separated on EtBr-stained gel after electrophoresis in 1.0–1.2% agarose. lane 1:AP-65, lane 2:AP-65-1 and lane 3:β-Tubulin。
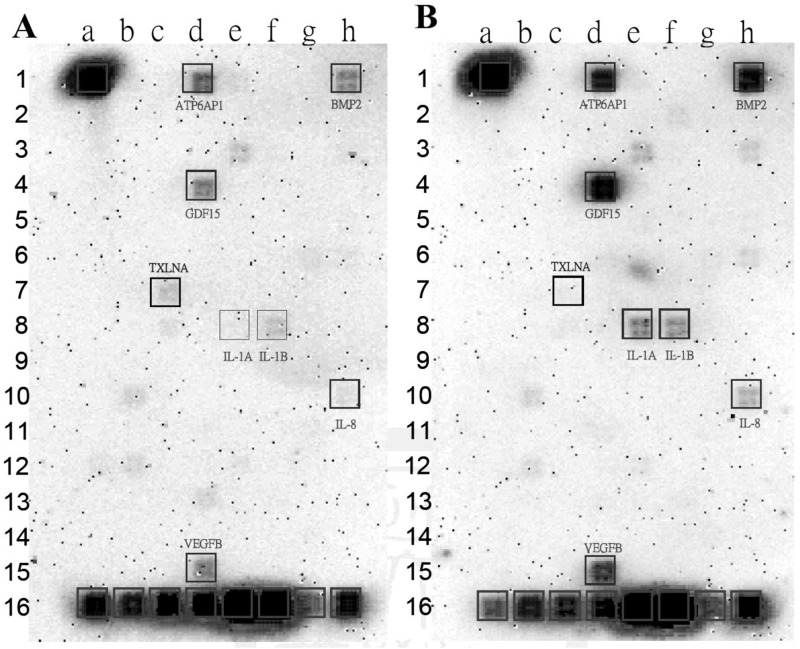
Changes in gene expression profile of co-cultured Z172 cells
In order to clarify the effects on gene expression in human cells attacked by T. vaginalis, we analyzed the gene expression profiles of Z172 cells using the Oligo GEArray Human Common Cytokines Microarray. A total of 114 important cytokine genes, colony-stimulating factors, tumor necrosis factors, various growth factors, and the other cytokine-related genes are covered by this chip. Our results revealed seven cytokine associated genes concomitant with an increase in expression levels and one associated with a decrease (Fig 6). The down-regulated gene was Taxilin-α, TXLNA (c-7) and the up-regulated genes were bone morphogenetic protein 2, BMP2 (h-1); growth differentiation factor 15, GDF 15 (d-4); IL-8, (h-10); IL-1αand IL-1β, (e-8 and f-8); ATP6AP1 (d-1); and vascular endothelial growth factor B, VEGF-β (d-15). These genes play important roles in the immune response, inflammatory response, and cell-cell signaling.
Fig 6. The cytokine genes expression profile of Z172 cells which co-cultured with T. vaginalis.
The changes of gene expression levels of Z172 cells before (A) and after interacted with T vaginalis (B) were investigated by Oligo GEArray Human Common Cytokines Microarray.
Discussion
Trichomonas vaginalis, an ancient protozoon, is the causative agent in one of the world's most common sexually infected disease, with a worldwide infection rate of 170 million annually [32]. Infection is acquired primarily through direct sexual contact although neonatal infection has also been reported [33–35]. T. vaginalis colonizes and parasites in the vagina or prostate of the infected host cause trichomonosis that can lead to severe health complications. Previous reports have shown that T. vaginalis infection results in cervical epithelial cell death via a strictly contact-dependent mechanism [11].
The importance of maintaining an intact mucosal layer is highlighted by the occurrence of pathological disorders associated with inflammatory disease, in which disruption of the epithelial barrier leads to severe inflammation of the mucosal tissue compartments [17, 36, 37]. The epithelial barrier is maintained by connections between adjoining epithelial cells, which are the first sites of contact with the host. These cells are responsible for separating potentially harmful luminal content from the underlying tissue. This function of acting as a physical barrier is accomplished by junctional complex, which comprises a plethora of membrane-associated and transmembraneous proteins organized in discreet, spatially restricted complexes [37, 38]. Our findings provide solid evidence to support claims that the damages of T. vaginalis infection to host cells and cell junctions is initiated by the attachment of live parasites and cannot be induced by the inactivated T. vaginalis or parasite cultured medium. Previous reports have shown that host cells infected by T. vaginalis presented disruption before being lysed [10, 39]. In addition to damage and disruption in the cells, we also observed in time-lapse recording apoptosis-like and necrosis-like cell death of the Z172 cells co-cultured with T. vaginalis for ten hours.
Epithelial cells act in a manner similar to that of a connector in a host-microbe communications network, building signal transduction connections between luminal microbes and the host. The epithelial cells act as sensors for the microbes and as providers of signal to immune cells to activate inflammatory and immune responses. The infection accompanied by the release of cytokines and chemokines is caused by inflammation of one of the causes. The array results in this study showed an increase in the expression of seven cytokine-associated genes following infection with T. vaginalis in Z172. In these cytokines, IL-8 is known to govern polymorphonuclear leukocytes localization and function. Shaio reported the interleukin-8 response to infection with T. vaginalis in human monocyte and neutrophils [40, 41]. In T. vaginalis-infected human ectocervical cells, parasites as well as exosomes were shown to specifically modulate IL-8 [42]. Interestingly, Twu et al. reported that T. vaginalis produces and secretes exosomes capable of promoting parasite:parasite communication and host cell colonization, as well as mediating the immune response of host cells [42]. In this study, we did not observe any effects of Z172 with the medium with which parasites were cultured. We propose the following explanations: Either the release of exosomes must be induced or the concentration of exosomes is too low to induce any visible effects.
Previous reports have shown that Entamoeba histolytica co-cultured with human intestinal epithelial cells increase the expression and secretion of chemoattractant and proinflammatory cytokines, including IL-8, GROα, GM-CSF, IL-lα, and IL-6 [43]. We also found that proinflammatory cytokines, IL-1α and IL-1β, are induced after the attachment of T. vaginalis. The secretion of IL-1β into surrounding interstitial fluid and blood during inflammation mediates a wide range of proinflammatory activities. IL-1β has been shown to cause a significant increase in intestinal tight junction permeability [44]. Wang et al. reported that VEGF could induce tight junction disassembly and alter the distribution of actin filaments in microvessel endothelial cells in the brain by reducing ZO-1 and occludin located at tight junctions [23].
We also found that VEGF-β is induced in human ectocervical cells infected with T. vaginalis. According to these results, it is reasonable to assume that the disruption of host cell pathogenesis may be caused by these cytokines. Another cytokine which increased expression level, BMP-2 is a member of the TGF-β superfamily, playing an important role in the embryonic development, suppression of the immune response, and differentiation and proliferation of tissues and cells. In mature colonic epithelial cells, it acts as a tumor suppressor capable of promoting apoptosis [45]. We propose that the death of Z172 not caused by infection, but hyperimmunization of cytokines.
In summary, we hypothesize that the morphological and gene expression of Z172 is altered to form cytokines and a complex signaling cascade in response to trichomonal adherence. During the parasite and host cell interaction, T. vaginalis as well as Z172 cells stimulate each other to induce the differential expression of genes. Contact-dependent changes in cytotoxicity of human cervical cells are important in the pathogenesis of human cervical disease and may also be an effective target for the development of new drugs.
Supporting Information
The T. vaginalis and Z172 cells were adapted respectively from the original medium, the YI-S medium (panel A) and the DMEM medium (panel B), into the co-culture medium, DMEM:YI-S (2:1, vol/vol) medium (panel C and D). The adapted T. vaginalis and Z172 cells were co-cultured in DMEM:YI-S medium (panel E). Bar = 20μm.
(TIFF)
Panel A to T were the captured images once every 30 minutes. Bar = 20μm.
(TIFF)
Panel A to T were the captured images once every 30 minutes. Bar = 20μm.
(TIFF)
Panel A to T were the captured images once every 30 minutes. Bar = 20μm.
(TIFF)
The propidium iodide (PI) was used to stain the DNA and look for the sub-diploid to quantitate apoptosis by flow cytometry.
(TIFF)
(DOCX)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was supported by the Ministry of Education, Taiwan, R. O. C. The Aim for the Top University Project to the National Cheng Kung University (NCKU). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Schwebke JR, Burgess D. Trichomoniasis. Clinical microbiology reviews. 2004;17(4):794–803, table of contents. 10.1128/CMR.17.4.794-803.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Akira S. [Innate immunity and allergic diseases]. Arerugi = [Allergy]. 2002;51(4):352–6. . [PubMed] [Google Scholar]
- 3. Mason PR, Fiori PL, Cappuccinelli P, Rappelli P, Gregson S. Seroepidemiology of Trichomonas vaginalis in rural women in Zimbabwe and patterns of association with HIV infection. Epidemiology and infection. 2005;133(2):315–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mavedzenge SN, Pol BV, Cheng H, Montgomery ET, Blanchard K, de Bruyn G, et al. Epidemiological synergy of Trichomonas vaginalis and HIV in Zimbabwean and South African women. Sexually transmitted diseases. 2010;37(7):460–6. 10.1097/OLQ.0b013e3181cfcc4b . [DOI] [PubMed] [Google Scholar]
- 5. McClelland RS, Sangare L, Hassan WM, Lavreys L, Mandaliya K, Kiarie J, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. The Journal of infectious diseases. 2007;195(5):698–702. 10.1086/511278 . [DOI] [PubMed] [Google Scholar]
- 6. Van Der Pol B, Kwok C, Pierre-Louis B, Rinaldi A, Salata RA, Chen PL, et al. Trichomonas vaginalis infection and human immunodeficiency virus acquisition in African women. The Journal of infectious diseases. 2008;197(4):548–54. 10.1086/526496 . [DOI] [PubMed] [Google Scholar]
- 7. Krieger JN, Ravdin JI, Rein MF. Contact-dependent cytopathogenic mechanisms of Trichomonas vaginalis. Infection and immunity. 1985;50(3):778–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pindak FF, Mora de Pindak M, Gardner WA Jr. Contact-independent cytotoxicity of Trichomonas vaginalis. Genitourinary medicine. 1993;69(1):35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fiori PL, Rappelli P, Addis MF, Sechi A, Cappuccinelli P. Trichomonas vaginalis haemolysis: pH regulates a contact-independent mechanism based on pore-forming proteins. Microbial pathogenesis. 1996;20(2):109–18. 10.1006/mpat.1996.0010 . [DOI] [PubMed] [Google Scholar]
- 10. Fiori PL, Rappelli P, Addis MF, Mannu F, Cappuccinelli P. Contact-dependent disruption of the host cell membrane skeleton induced by Trichomonas vaginalis. Infection and immunity. 1997;65(12):5142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lustig G, Ryan CM, Secor WE, Johnson PJ. Trichomonas vaginalis contact-dependent cytolysis of epithelial cells. Infection and immunity. 2013;81(5):1411–9. 10.1128/IAI.01244-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Arroyo R, Engbring J, Alderete JF. Molecular basis of host epithelial cell recognition by Trichomonas vaginalis. Molecular microbiology. 1992;6(7):853–62. . [DOI] [PubMed] [Google Scholar]
- 13. Alvarez-Sanchez ME, Avila-Gonzalez L, Becerril-Garcia C, Fattel-Facenda LV, Ortega-Lopez J, Arroyo R. A novel cysteine proteinase (CP65) of Trichomonas vaginalis involved in cytotoxicity. Microbial pathogenesis. 2000;28(4):193–202. 10.1006/mpat.1999.0336 . [DOI] [PubMed] [Google Scholar]
- 14. Kucknoor AS, Mundodi V, Alderete JF. Adherence to human vaginal epithelial cells signals for increased expression of Trichomonas vaginalis genes. Infection and immunity. 2005;73(10):6472–8. 10.1128/IAI.73.10.6472-6478.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kucknoor AS, Mundodi V, Alderete JF. Heterologous expression in Tritrichomonas foetus of functional Trichomonas vaginalis AP65 adhesin. BMC molecular biology. 2005;6:5 10.1186/1471-2199-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garcia AF, Alderete J. Characterization of the Trichomonas vaginalis surface-associated AP65 and binding domain interacting with trichomonads and host cells. BMC microbiology. 2007;7:116 10.1186/1471-2180-7-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kucknoor AS, Mundodi V, Alderete JF. The proteins secreted by Trichomonas vaginalis and vaginal epithelial cell response to secreted and episomally expressed AP65. Cellular microbiology. 2007;9(11):2586–97. 10.1111/j.1462-5822.2007.00979.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Crouch ML, Alderete JF. Trichomonas vaginalis interactions with fibronectin and laminin. Microbiology. 1999;145 (Pt 10):2835–43. . [DOI] [PubMed] [Google Scholar]
- 19. Silva Filho FC, Ortega-Lopez J, Arroyo R. YIGSR is the preferential laminin-1 residing adhesion sequence for Trichomonas vaginalis. Experimental parasitology. 1998;88(3):240–2. 10.1006/expr.1998.4227 . [DOI] [PubMed] [Google Scholar]
- 20. Benchimol M, Batista C, De Souza W. Fibronectin- and laminin-mediated endocytic activity in the parasitic protozoa Trichomonas vaginalis and Tritrichomonas foetus. Journal of submicroscopic cytology and pathology. 1990;22(1):39–45. . [PubMed] [Google Scholar]
- 21. Okumura CY, Baum LG, Johnson PJ. Galectin-1 on cervical epithelial cells is a receptor for the sexually transmitted human parasite Trichomonas vaginalis. Cellular microbiology. 2008;10(10):2078–90. 10.1111/j.1462-5822.2008.01190.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Heath JP. Behaviour and pathogenicity of Trichomonas vaginalis in epithelial cell cultures: a study by light and scanning electron microscopy. The British journal of venereal diseases. 1981;57(2):106–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ryu JS, Kang JH, Jung SY, Shin MH, Kim JM, Park H, et al. Production of interleukin-8 by human neutrophils stimulated with Trichomonas vaginalis. Infection and immunity. 2004;72(3):1326–32. Epub 2004/02/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nam YH, Min D, Park SJ, Kim KA, Lee YA, Shin MH. NF-kappaB and CREB are involved in IL-8 production of human neutrophils induced by Trichomonas vaginalis-derived secretory products. The Korean journal of parasitology. 2011;49(3):291–4. 10.3347/kjp.2011.49.3.291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nam YH, Min D, Kim HP, Song KJ, Kim KA, Lee YA, et al. Leukotriene B4 receptor BLT-mediated phosphorylation of NF-kappaB and CREB is involved in IL-8 production in human mast cells induced by Trichomonas vaginalis-derived secretory products. Microbes and infection / Institut Pasteur. 2011;13(14–15):1211–20. 10.1016/j.micinf.2011.07.006 . [DOI] [PubMed] [Google Scholar]
- 26. Shaio MF, Lin PR. Influence of humoral immunity on leukotriene B4 production by neutrophils in response to Trichomonas vaginalis stimulation. Parasite immunology. 1995;17(3):127–33. . [DOI] [PubMed] [Google Scholar]
- 27. Shaio MF, Lin PR, Lee CS, Hou SC, Tang P, Yang KD. A novel neutrophil-activating factor released by Trichomonas vaginalis. Infection and immunity. 1992;60(11):4475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Diamond LS, Clark CG, Cunnick CC. YI-S, a casein-free medium for axenic cultivation of Entamoeba histolytica, related Entamoeba, Giardia intestinalis and Trichomonas vaginalis. The Journal of eukaryotic microbiology. 1995;42(3):277–8. . [DOI] [PubMed] [Google Scholar]
- 29. Lin WC, Li SC, Lin WC, Shin JW, Hu SN, Yu XM, et al. Identification of microRNA in the protist Trichomonas vaginalis. Genomics. 2009;93(5):487–93. Epub 2009/05/16. 10.1016/j.ygeno.2009.01.004 . [DOI] [PubMed] [Google Scholar]
- 30. Madico G, Quinn TC, Rompalo A, McKee KT Jr., Gaydos CA. Diagnosis of Trichomonas vaginalis infection by PCR using vaginal swab samples. Journal of clinical microbiology. 1998;36(11):3205–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ong SJ, Hsu HM, Liu HW, Chu CH, Tai JH. Multifarious transcriptional regulation of adhesion protein gene ap65-1 by a novel Myb1 protein in the protozoan parasite Trichomonas vaginalis. Eukaryotic cell. 2006;5(2):391–9. 10.1128/EC.5.2.391-399.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Carlton JM, Hirt RP, Silva JC, Delcher AL, Schatz M, Zhao Q, et al. Draft genome sequence of the sexually transmitted pathogen Trichomonas vaginalis. Science. 2007;315(5809):207–12. 10.1126/science.1132894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Danesh IS, Stephen JM, Gorbach J. Neonatal Trichomonas vaginalis infection. The Journal of emergency medicine. 1995;13(1):51–4. Epub 1995/01/01. . [DOI] [PubMed] [Google Scholar]
- 34. Kerekes A, Tege A, Szarka K, Temesvari P. [Neonatal respiratory insufficiency caused by maternal infection with trichomonas vaginalis]. Orvosi hetilap. 2000;141(33):1821–2. Epub 2000/09/09. . [PubMed] [Google Scholar]
- 35. Trintis J, Epie N, Boss R, Riedel S. Neonatal Trichomonas vaginalis infection: a case report and review of literature. International journal of STD & AIDS. 2010;21(8):606–7. Epub 2010/10/27. 10.1258/ijsa.2010.010174 . [DOI] [PubMed] [Google Scholar]
- 36. Fichorova RN, Trifonova RT, Gilbert RO, Costello CE, Hayes GR, Lucas JJ, et al. Trichomonas vaginalis lipophosphoglycan triggers a selective upregulation of cytokines by human female reproductive tract epithelial cells. Infection and immunity. 2006;74(10):5773–9. 10.1128/IAI.00631-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kucknoor A, Mundodi V, Alderete JF. Trichomonas vaginalis adherence mediates differential gene expression in human vaginal epithelial cells. Cellular microbiology. 2005;7(6):887–97. 10.1111/j.1462-5822.2005.00522.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Koch S, Nusrat A. Dynamic regulation of epithelial cell fate and barrier function by intercellular junctions. Annals of the New York Academy of Sciences. 2009;1165:220–7. 10.1111/j.1749-6632.2009.04025.x . [DOI] [PubMed] [Google Scholar]
- 39. Guenthner PC, Secor WE, Dezzutti CS. Trichomonas vaginalis-induced epithelial monolayer disruption and human immunodeficiency virus type 1 (HIV-1) replication: implications for the sexual transmission of HIV-1. Infection and immunity. 2005;73(7):4155–60. 10.1128/IAI.73.7.4155-4160.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Shaio MF, Lin PR, Liu JY, Tang KD. Monocyte-derived interleukin-8 involved in the recruitment of neutrophils induced by Trichomonas vaginalis infection. The Journal of infectious diseases. 1994;170(6):1638–40. . [DOI] [PubMed] [Google Scholar]
- 41. Shaio MF, Lin PR, Liu JY, Yang KD. Generation of interleukin-8 from human monocytes in response to Trichomonas vaginalis stimulation. Infection and immunity. 1995;63(10):3864–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Twu O, de Miguel N, Lustig G, Stevens GC, Vashisht AA, Wohlschlegel JA, et al. Trichomonas vaginalis exosomes deliver cargo to host cells and mediate hostratioparasite interactions. PLoS pathogens. 2013;9(7):e1003482 10.1371/journal.ppat.1003482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Eckmann L, Reed SL, Smith JR, Kagnoff MF. Entamoeba histolytica trophozoites induce an inflammatory cytokine response by cultured human cells through the paracrine action of cytolytically released interleukin-1 alpha. The Journal of clinical investigation. 1995;96(3):1269–79. 10.1172/JCI118161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Al-Sadi RM, Ma TY. IL-1beta causes an increase in intestinal epithelial tight junction permeability. Journal of immunology. 2007;178(7):4641–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hardwick JC, Van Den Brink GR, Bleuming SA, Ballester I, Van Den Brande JM, Keller JJ, et al. Bone morphogenetic protein 2 is expressed by, and acts upon, mature epithelial cells in the colon. Gastroenterology. 2004;126(1):111–21. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The T. vaginalis and Z172 cells were adapted respectively from the original medium, the YI-S medium (panel A) and the DMEM medium (panel B), into the co-culture medium, DMEM:YI-S (2:1, vol/vol) medium (panel C and D). The adapted T. vaginalis and Z172 cells were co-cultured in DMEM:YI-S medium (panel E). Bar = 20μm.
(TIFF)
Panel A to T were the captured images once every 30 minutes. Bar = 20μm.
(TIFF)
Panel A to T were the captured images once every 30 minutes. Bar = 20μm.
(TIFF)
Panel A to T were the captured images once every 30 minutes. Bar = 20μm.
(TIFF)
The propidium iodide (PI) was used to stain the DNA and look for the sub-diploid to quantitate apoptosis by flow cytometry.
(TIFF)
(DOCX)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
The observation of the progress of Z172 cells which co-cultured with T. vaginalis.
(MOV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.