Abstract
Background
Two coding variants, G1 and G2, in the apolipoprotein L-1 (APOL1) gene are associated with increased incidence of ESRD in the adult African American population. These variants associate with hypertension attributed renal disease, focal segmental glomerulosclerosis and HIV associated nephropathy. We hypothesized that as a genetic disease, APOL1 nephropathy has a pediatric phenotype.
Methods
We investigated the incidence of APOL1 variants in young African Americans with hypertension or focal segmental glomerulosclerosis and a family history of end stage renal disease by conducting a case-control study of 93 pediatric and young adult African Americans with hypertension or focal segmental glomerulosclerosis to determine the association with APOL1 risk variants, G1 and G2, using custom made TaqMan based allelic discrimination assays.
Results
Forty of the 61 cases (66%) with a family history of kidney disease had two APOL-1 risk variants, significantly higher than the prevalence in the case controls and the general African American population (p < 0.001). 24/29 patients with hypertension attributed kidney disease had two APOL1 risk variants while none of nine hypertensive patients without kidney disease had more than one risk allele.
Conclusions
Although a small cohort, our findings strongly suggest for the first time that 2 APOL1 risk alleles in hypertensive young African Americans with a family history of ESRD are strongly associated with kidney disease.
Keywords: hypertension, focal segmental glomerulosclerosis, end-stage renal disease, pediatrics, APOL1, African Americans
Introduction
African Americans are four to five times more likely to develop end stage renal disease compared to European Americans and have a more rapid progression to end stage renal disease (ESRD) than the established age associated progression in the general population [1, 2]. This increased risk is independent of socioeconomic status. A familial clustering of ESRD in the African American population is well established and can be explained by the recent discovery of variants in the apolipoprotein L-1 gene on chromosome 22. The two APOL-1 risk variants consist of a missense variant labeled G1 and a 6 base pair deletion labeled G2. G1 (rs73885319) and G2 (rs71785313) have been extensively studied in the African American population. Presence of 2 risk alleles in any combination (G1/G1, G2/G2 or G1/G2) confer an increased risk of non-diabetic nephropathy with faster progression of disease and earlier initiation of renal replacement therapy[3].
Polymorphisms identified in the APOL1 gene have also been associated with an increased predisposition to focal segmental glomerulosclerosis, HIV- associated nephropathy, lupus nephritis and hypertension attributed kidney disease in the African American population [4–6]. These variants do not appear to impart the same risk on IgA nephropathy, or diabetic nephropathy [7, 8]. African Americans with sickle cell disease who had the MYH9 or APOL1 risk allele have an increased risk for renal dysfunction compared to those without these risk alleles, also supporting the role of a genetic variation at a locus close to the MYH9 gene in renal dysfunction [9, 10].
Variations in the APOL1 gene are common in the African population and absent in European Americans. The allele frequency of the G1 and G2 variants in the African Yoruba population is approximately 38% and in European Americans is 4–8% [11]. The frequency of these variants vary in the African population with G1 being more common in West Africa and rare in East Africa while the G2 variant is more uniformly distributed in Africa and is not as prevalent as G1 [12].
These coding variants confer a selective advantage to Africans with one or two copies of the risk variant in regions where sleeping sickness was endemic [12]. Research has shown that APOL1 risk allele homozygosity and compound heterozygosity (harboring 2 risk variants) are protective against the Trypanosoma brucei parasite similar to the protection offered by the sickle cell trait from malaria [12].
Case control studies have shown that patients who harbor 2 APOL1 risk alleles are at a higher risk for developing ESRD than patients who carry one or zero risk alleles [12, 13]. In a recent study of 407 African Americans with non-diabetic ESRD, enrolled in the Accelerated Mortality on Renal Replacement (ArMORR) study, subjects who harbored two APOL1 risk allele initiated dialysis up to 14 years earlier compared to subjects with no APOL1 risk allele (6). This trend has been demonstrated in other studies [13, 14].
Further analysis of the APOL1 genotype in individuals with FSGS and HIV associated nephropathy (HIVAN) revealed a significantly increased risk for disease in patients who carry two risk alleles. The estimated lifetime risk for FSGS was 4% in patients who had two APOL1risk alleles and this conferred a 17 fold increased risk of FSGS [4]. These patients developed FSGS earlier and were shown to have faster decline in renal function compared to patients with one or zero APOL1 risk allele. Patients with HIV and who have two APOL1 risk alleles have a 50% chance of developing HIV associated nephropathy and a 29 fold increased risk for HIVAN [4].
The association between the two APOL1 risk variants and African Americans with non-diabetic ESRD secondary to focal segmental glomerulosclerosis, hypertension or HIVAN has been made in adult populations [4, 8, 12, 15, 16]. The presentation of APOL1 nephropathy in the pediatric and young African American population remains unclear. The discovery of the APOL1 risk variants has shed light on the etiology of ESRD in the African American population and defining a pediatric phenotype might lead to earlier identification of at risk children and young adults and enable intervention at an earlier point than is currently practiced. We hypothesized that if APOL1 nephropathy is a genetic disease, a pediatric phenotype is likely to exist, so we set out to analyze the frequency of the APOL1 variants G1 and G2 in a pediatric and young adult African American cohort presenting with clinically diagnosed hypertension and biopsy proven FSGS who had a positive family history of ESRD in a first or second-degree relative.
Methods
The institutional review board of the Washington University in St Louis School of Medicine approved this study and informed consent was obtained from all participants. Recruitment and specimen processing were done in the Washington University Kidney Translational Research Core. The study included 117 subjects residing a single geographic region in the United States enrolled from August 2011 to June 2013 (Figure 1). Ninety three subjects presented with hypertension or FSGS, of who 61 had a family history of ESRD in a first or second degree relative, and 32 who did not have a family history of ESRD. Controls consisted of 24 healthy adult subjects with no family history of ESRD and thus ensured that they did not have ApoL1 nephropathy during childhood. Renal biopsy proven minimal change associated nephrotic syndrome was excluded from the analysis. The diagnoses of hypertension and hypertension attributed kidney disease were made by a large group of physicians by generally accepted clinical practice and not a single protocol. None of the hypertension attributed kidney disease patients had renal biopsies.
Figure 1.
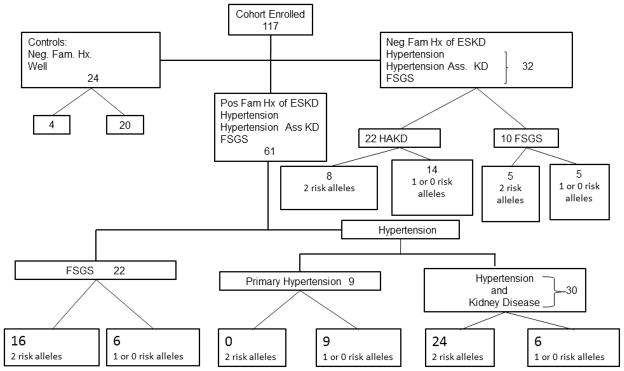
Study group breakdown of 117 subjects enrolled and the frequency of APOL1 risk alleles.
ESKD, end stage kidney disease; FSGS, focal segmental glomerulosclerosis,
Clinical data collected included demographics, physician reported diagnosis or cause of ESRD, family history of ESRD, biopsy reports where applicable, age at diagnosis, enrollment and at initiation of dialysis or transplant. Peripheral venous blood was collected from each study participant for genomic DNA extraction using the QIAamp DNA mini kit (QIAGEN Science, Maryland). DNA quality was assessed for all samples, using the ratio of absorbance at 260nm and 280nm with a Nanodrop spectrophotometer. A ratio greater than 1.7 was considered adequate.
The genotyping of APOL1 variants (rs73885319 and rs71785313) was performed on an Applied Biosystems 7900HT Fast Real-Time PCR system (7900HT Fast System) using custom TaqMan SNP Genotyping Assay for each marker with PCR primers and TaqMan FAM and VIC dye-labeled probes, which were designed according to the manufacturer’s recommendations. The genotypes were identified using the allelic discrimination plots generated by the Sequence Detection System (SDS) software version 2.3 (Applied Biosystems, Foster, CA). Allelic discrimination plots for G1 and G2 are included in the supplementary materials.
Quality control measures included comparing results from the TaqMan analysis with targeted exome sequencing results in 15% of participants and including duplicate samples within and between plates for 15% to confirm the accuracy of the TaqMan assay and control for genotyping errors. All these confirmed the genotypes obtained.
All statistical analyses were performed with SAS 9.2 statistical software (SAS Institute, Cary NC). We compared the allele frequency of patients and healthy controls using the Fishers exact tests. We set statistical significance at p<0.05 for all tests.
Results
Pediatric and young African American patients presenting with either hypertension or FSGS, all with a family history of ESRD, were identified as cases (Figure 1). Twenty-four healthy African American participants without a family history of ESRD were controls (Table 1). Controls were healthy African Africans who were significantly older than the cases; this selection was made to eliminate the possibility of younger controls developing significant kidney disease later in life. In addition, we also included 32 control subjects with hypertension or FSGS without a family history of ESRD. Males and females were equally represented in the cases and controls. The mean ages (SD) for the FSGS and hypertensive cases were 24.3 (7.4) and 23.6 (6.9) years, respectively. A second control group consisted of pediatric and young African American patients presenting with either hypertension or FSGS, without a family history of ESRD (Figure 1)
Table 1.
Study Participant Characteristics of cases with a family history of ESRD and Controls
| Cases (61) | Controls (24) | |
|---|---|---|
| Mean age, years | 23.1 ± 7.0 | 45.5 ± 14.9 |
| Sex (% Female) | 54 | 50 |
| Hypertension/FSGS | 39/22 | 0 |
| Onset Age (n) | ||
| < 18 years | 17 | 1 |
| 18– 35 years | 44 | 4 |
| >35 years | 0 | 19 |
| ESRD at enrollment | 40 | 0 |
FSGS, focal segmental glomerulosclerosis; ESRD, end stage renal disease
As shown in Figure 1, among 61 cases with a positive family history of ESRD, there were 39 cases of hypertension and 22 cases of FSGS. Forty (66%) of the 61 cases had two APOL-1 risk alleles (G1/G1, G1/G2 or G2/G2); a significantly higher prevalence than in the controls and the general AA population (p < 0.001). Hypertension with a positive family history of ESRD was significantly associated with the presence of two APOL1 risk alleles, p < 0.001(Table 2). FSGS with a positive family history of ESRD was also strongly associated with the presence of two APOL1 risk alleles, p < 0.001 (Table 2). The frequency of two APOL1 risk alleles in the general African American population is reported to be 10–12%. The prevalence of two APOL1 risk alleles in our controls (4/24) was not significantly different from that in the general African American population.
Table 2.
Prevalence of a two APOL1 risk alleles in cases with hypertension or FSGS and control subjects
| Cases | Controls | Odds Ratio (95% Cl) | p value | |
|---|---|---|---|---|
| Hypertension. | 39 | 24 | 8 (2.29–28) | <0.001 |
| 2-APOL-1 risk alleles | 24 (61.5%) | 4 (16.7%) | ||
| FSGS | 22 | 24 | 13.3 (3.2–55.5) | <0.001 |
| 2-APO-l risk alleles | 16 (72.7%) | 4 (16.7%) |
FSGS, focal segmental glomerulosclerosis
Among the 39 cases presenting with hypertension and a positive family history of ESRD, there were 9 cases of hypertension alone and 30 cases of hypertension attributed kidney disease (Figure 1). Of the 30 cases with hypertension attributed kidney disease, 24 (80%) had two APOL1 risk alleles (G1/G1 or G1/G2 or G2/G2); while none of the hypertensive patients who presented without kidney disease (normal GFR and no proteinuria) had more than one APOL1 risk alleles. Compared with participants with zero or one APOL1 risk allele, the presence of two APOL1 risk alleles was significantly associated to the development of ESRD among the hypertensive cohort; p< 0.001 (Table 3). During the enrollment period we found most of the cases of hypertension attributed kidney disease receiving dialysis for ESRD in Washington University affiliated clinics, while our hypertension alone group consisted of patients presenting with primary hypertension in our pediatric nephrology clinics. All of the cases of hypertension attributed kidney disease had initially presented with kidney disease and hypertension.
Table 3.
Prevalence of 2 APOL1 risk alleles in Patients with ESRD versus no ESRD among Hypertensive and FSGS cases
| Hypertension | ESRD (N= 30) | No ESRD (N= 9) | P value | Control (N= 24) | OR (95% CI) | P value |
|---|---|---|---|---|---|---|
| 2 APOL1 risk alleles versus 1 or no APOL1 risk allele | 24 (80%) | 0 | < 0.001 | 4 (16.7) | 20.0 (4.9– 80.9) | < 0.001 |
| FSGS | ESRD (N= 12) | No ESRD (N= 10) | P value | Control (N= 24) | OR (95% CI) | P value |
|---|---|---|---|---|---|---|
| 2 APOL1 risk alleles versus 1 or no APOL1 risk allele | 8 (67%) | 8 (80%) | 0.646 | 4 (16.7) | 10.0 (2.0– 50.0) | 0.007 |
FSGS, focal segmental glomerulosclerosis; ESRD, end stage renal disease
In the hypertensive cohort the presence of two APOL1 risk alleles was significantly associated to the development of ESRD compared with participants with zero or one APOL1 risk allele; p< 0.001. None of the hypertensive participants without kidney disease had two APOL1 risk alleles. Among hypertensive patients that had reached ESRD, those with two APOL1 risk alleles were found to develop ESRD 6 years earlier than those with one or no risk alleles. There was no significant difference for the age at ESRD in the FSGS cohort (Table 4).
Table 4.
Age at ESRD between different APOL1 genotypes among Participants with ESRD
| Participants with ESRD (years) | Hypertensive participants with ESRD (years) | FSGS with ESRD (years) | |
|---|---|---|---|
| G1/G1+ G1/G2+ G2/G2 | 25.5 +/− 6.4 | 26.3 +/− 5.8 | 23.1 +/− 7.9 |
| G1/WT + G2/WT + WT/WT | 21.4 +/− 5.6 | 19.7 +/− 6.2 | 24.0 +/− 3.7 |
| P value | |||
| (G1/G1+ G1/G2 + G2/G2) versus (G1/WT + G2/WT + WT/WT) | 0.076 | 0.020 | 0.841 |
ESRD, end stage renal disease; FSGS, focal segmental glomerulosclerosis
Among the 22 cases presenting with FSGS, there were 12 cases with ESRD and 10 without (Table 3). Of the 12 cases with ESRD, eight had two APOL1 risk alleles, and of the 10 without ESRD, eight had two APOL1 risk alleles, p<0.646. However, compared to controls, FSGS was strongly associated with two APOL1 risk alleles (Table 3).
There were 32 African American participants with clinically diagnosed hypertension attributed kidney disease (n= 22) or biopsy proven FSGS (n= 10) without a family history of end stage renal disease. Their age was similar to those with a positive family history, and 69% of them had end stage renal disease. Eight of 22 subjects (36%) with hypertension associated kidney disease had two APOL1 risk alleles, significantly greater than the prevalence in our controls, suggesting that even without family history of ESRD; two APOL1 risk alleles are associated with ESRD.
Discussion
Our findings demonstrate that ApoL1 nephropathy presents in the young not as a silent disease with its clinical consequences appearing later in life, nor as primary hypertension. Instead its presentation is as hypertension attributed kidney disease or as FSGS. This phenotype is similar to that reported in adult populations [3]. We did not include systemic lupus erythematosus or sickle cell anemia in our cohort, but these diseases also associate with APOL1 variants when they cause kidney disease in African Americans.
A familial clustering of ESRD has been well established in the African American population with an increased incidence in family members of patients with kidney disease [17–21]. A genetic role explains these findings and is supported by the recent identification of two variants (G1 and G2) on the last exon of the apolipoprotein L-1 gene (APOL1) in chromosome 22 observed among individuals of recent African ancestry that associate with increased risk for kidney disease [4, 12, 14]. Homozygosity for the risk alleles (G1/G1, G1/G2, or G2/G2) is strongly associated with increased disease risk [13]
The APOL1 variants have been associated with mild kidney disease, a phenotype that we specifically sought in our cohort. Freedman et al recently assessed the risk of mild kidney disease in the cohort of the Natural History of APOL1 nephropathy[15]. This cohort comprised of 826 relatives of patients with end stage renal disease. Seven hundred and eighty six participants were genotyped and multivariate analysis revealed associations between the APOL1 risk variants, proteinuria and chronic kidney disease, GFR less than 60ml/min/1.73m2 [15]. A trend was found associating quantitative albuminuria and APOL1 variants [15], but we were unable to find and enroll subjects in our cohort matching the microalbuminuric or non proteinuric CKD subjects of the cohort of the Natural History of APOL1 nephropathy. Thus, our analysis was limited to hypertension with or without kidney disease and proteinuric kidney disease, biopsy proven FSGS, in a young cohort of African American patients from a defined geographic area.
The high prevalence of two APOL1 risk alleles in our cases compared to controls allowed us to do subset analysis despite the limitations of our small cohort. Hypertension attributed kidney disease with a positive family history of kidney disease was associated with an 80% prevalence of two risk alleles while hypertension without kidney disease was not associated with two risk alleles. Furthermore, in pediatric cases with hypertension and no family history of kidney disease, the prevalence of two APOL1 risk alleles was 9% (data not shown), not different from the general population. This indicates that APOL1 risk alleles in pediatric subjects segregate with kidney disease and not just hypertension alone. Ours is the first study to evaluate the association of the APOL1 risk variants in a pediatric and young adult population, and it suggests that APOL1 nephropathy presents as a kidney disease with hypertension and not isolated hypertension.
We demonstrated a 65% prevalence of 2 APOL1 variants among our 61 cases with a positive family history, hypertension attributed kidney disease or biopsy proven FSGS. This significant association between APOL1 risk variants and hypertension attributed end stage renal disease in young African American participants compared with controls is consistent with other studies [16]. The presence of these risk variants predicted the hypertensive patients that were likely to develop end stage renal disease. The finding of a strong association with end stage renal disease among patients with hypertension attributed nephropathy and two APOL1 risk alleles lends itself to the definition of the clinical phenotype of APOL1 nephropathy and aids in the identification of hypertensive patients who have an increased risk for progressive disease. African Americans who are homozygous for the APOL1 variants have an increased lifetime risk for FSGS [4]. The presence of two risk alleles were also shown to be significantly associated with the FSGS group compared to controls in our cohort.
Hypertensive nephrosclerosis in African Americans (now generally referred to as hypertension attributed kidney disease in lieu of the discovery of ApoL1 associated risk) appears to be in the spectrum of APOL1 nephropathy along with FSGS and HIVAN, which all present histologically with some extent of glomerulosclerosis [16]. The presence of APOL1 risk alleles in the African American pediatric population might be indicative of silent kidney disease that may later present with kidney disease or failure as demonstrated in a recent study by Freedman et al [15]. However, we were unable to confirm this possibility in our cohort.
Recently, Foster et al demonstrated that two APOL1 risk alleles were significantly associated with an increased risk of chronic kidney disease [13]. In our cohort, none of the hypertensive participants without end stage renal disease possessed two APOL1 risk alleles. Also, the high frequency of the APOL1 risk alleles in the hypertensive cohort and the remarkable finding that majority of the hypertensive participants with two APOL1 risk alleles developed end stage renal disease demonstrates that hypertension in African American patients should be viewed seriously. A positive family history of end stage renal disease in a first or second-degree relative of a hypertensive African American should prompt consideration of APOL1 nephropathy.
We have not had the opportunity to perform analysis of the recently described G3 haplotype of APOL1[22], and future studies should add this analysis to our data set. The G3 haplotype has of yet to be associated with chronic kidney disease, so whether it will add to our findings of the phenotype of APOL1 nephropathy in young subjects is unknown.
Our discovery will add to the present knowledge of APOL1 nephropathy and will help with earlier identification of at risk patients. While it is premature to advocate for universal screening of African American children, screening might be an option in the future when interventions are developed to effectively treat patients and prevent progression to end stage renal disease. This might lead to the development of targets for therapy given the significant health and economic burden of APOL1 nephropathy in the African American population. A longitudinal study to evaluate disease progression is paramount and would go a long way in providing insight and addressing some of the unanswered questions pertaining to APOL1 nephropathy in the young.
Besides the inherent weakness produced by the small size of the reported cohort, the selection bias introduced by the decision to focus on components of our practice where we considered risk to be feasible introduced a selection bias. However, the finding of no more than the prevalence of ApoL1 in the general African-American population in our patients with primary limits the importance of this selection bias.
In conclusion, we demonstrated for the first time the phenotype of APOL1 nephropathy in a young adult African American population is kidney disease, not hypertension. We found that 2 APOL1 risk alleles in young African Americans with a family history of ESRD were significantly associated with hypertension attributed kidney disease and FSGS and not primary hypertension in a young African American cohort including pediatric age subjects. Although a small cohort, our findings strongly suggest that APOL1 nephropathy presents with kidney diseases known to associate with ApoL1 risk alleles and not primary hypertension in patients with a positive family history of ESRD.
Acknowledgments
Sources of Support: This work was supported by a Genzyme (Sanofi) fellowship grant (EA) and the National Institutes of Health (NIH) George M. O’Brien Center for Kidney Disease Research (P30-DK079333) and CTSA-ICTS tissue procurement and molecular phenotyping and center for biomedical informatics cores (NCRR UL1 RR024992) to Washington University, Children Discovery Institute grants MDII2009177 (S.J.).
We would like to acknowledge the assistance of Mary Hoffmann: Clinical Research Coordinator, Kidney Translational Research Core (KTRC), Washington University School of Medicine, Masato Hoshi: Senior Scientist, Jain Lab, Washington University School of Medicine, and Jie Zheng Division of Biostatistics, Washington University School of Medicine.
Footnotes
Disclosures:
The authors have no relevant financial disclosures
References
- 1.Coresh J, Byrd-Holt D, Astor BC, Briggs JP, Eggers PW, Lacher DA, Hostetter TH. Chronic Kidney Disease Awareness, Prevalence, and Trends among U.S. Adults, 1999 to 2000. J Am Soc Nephrol. 2005;16:180–188. doi: 10.1681/ASN.2004070539. [DOI] [PubMed] [Google Scholar]
- 2.Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Herzog C, Ishani A, Johansen K, Kasiske B, Kutner N, Liu J, St Peter W, Ding S, Guo H, Kats A, Lamb K, Li S, Li S, Roberts T, Skeans M, Snyder J, Solid C, Thompson B, Weinhandl E, Xiong H, Yusuf A, Zaun D, Arko C, Chen S-C, Daniels F, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L. US Renal Data System 2012 Annual Data Report. Am J Kid Dis. 2013;61:A7. doi: 10.1053/j.ajkd.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 3.Parsa A, Kao WHL, Xie D, Astor BC, Li M, Hsu C-Y, Feldman HI, Parekh RS, Kusek JW, Greene TH, Fink JC, Anderson AH, Choi MJ, Wright JT, Lash JP, Freedman BI, Ojo A, Winkler CA, Raj DS, Kopp JB, He J, Jensvold NG, Tao K, Lipkowitz MS, Appel LJ. APOL1 Risk Variants, Race, and Progression of Chronic Kidney Disease. N Engl J Med. 2013;369:2183–2196. doi: 10.1056/NEJMoa1310345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kopp JB, Nelson GW, Sampath K, Johnson RC, Genovese G, An P, Friedman D, Briggs W, Dart R, Korbet S, Mokrzycki MH, Kimmel PL, Limou S, Ahuja TS, Berns JS, Fryc J, Simon EE, Smith MC, Trachtman H, Michel DM, Schelling JR, Vlahov D, Pollak M, Winkler CA. APOL1 Genetic Variants in Focal Segmental Glomerulosclerosis and HIV-Associated Nephropathy. J Am Soc Nephrol. 2011;22:2129–2137. doi: 10.1681/ASN.2011040388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freedman B, Murea M. Target Organ Damage in African American Hypertension: Role of APOL1. Curr Hypertens Rep. 2012;14:21–28. doi: 10.1007/s11906-011-0237-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman BI, Langefeld CD, Andringa KK, Croker JA, Williams AH, Garner NE, Birmingham DJ, Hebert LA, Hicks PJ, Segal MS, Edberg JC, Brown EE, Alarcón GS, Costenbader KH, Comeau ME, Criswell LA, Harley JB, James JA, Kamen DL, Lim SS, Merrill JT, Sivils KL, Niewold TB, Patel NM, Petri M, Ramsey-Goldman R, Reveille JD, Salmon JE, Tsao BP, Gibson KL, Byers JR, Vinnikova AK, Lea JP, Julian BA, Kimberly RP on behalf of the Lupus Nephritis–End-Stage Renal Disease C. End-Stage Renal Disease in African Americans With Lupus Nephritis Is Associated With APOL1. Arthritis Rheumatol. 2014;66:390–396. doi: 10.1002/art.38220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin CP, Adrianto I, Lessard CJ, Kelly JA, Kaufman KM, Guthridge JM, Freedman BI, Anaya JM, Alarcon-Riquelme ME, Pons-Estel BA, Martin J, Glenn S, Adler A, Bae SC, Park SY, Bang SY, Song YW, Boackle SA, Brown EE, Edberg JC, Alarcon GS, Petri MA, Criswell LA, Ramsey-Goldman R, Reveille JD, Vila LM, Gilkeson GS, Kamen DL, Ziegler J, Jacob CO, Rasmussen A, James JA, Kimberly RP, Merrill JT, Niewold TB, Scofield RH, Stevens AM, Tsao BP, Vyse TJ, Langefeld CD, Moser KL, Harley JB, Gaffney PM, Montgomery CG. Role of MYH9 and APOL1 in African and non-African populations with lupus nephritis. Genes Immun. 2012;13:232–238. doi: 10.1038/gene.2011.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papeta N, Kiryluk K, Patel A, Sterken R, Kacak N, Snyder HJ, Imus PH, Mhatre AN, Lawani AK, Julian BA, Wyatt RJ, Novak J, Wyatt CM, Ross MJ, Winston JA, Klotman ME, Cohen DJ, Appel GB, D’Agati VD, Klotman PE, Gharavi AG. APOL1 Variants Increase Risk for FSGS and HIVAN but Not IgA Nephropathy. J Am Soc Nephrol. 2011;22:1991–1996. doi: 10.1681/ASN.2011040434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashley-Koch AE, Okocha EC, Garrett ME, Soldano K, De Castro LM, Jonassaint JC, Orringer EP, Eckman JR, Telen MJ. MYH9 and APOL1 are both associated with sickle cell disease nephropathy. Br J Haematol. 2011;155:386–394. doi: 10.1111/j.1365-2141.2011.08832.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hicks PJ, Langefeld CD, Lu L, Bleyer AJ, Divers J, Nachman PH, Derebail VK, Bowden DW, Freedman BI. Sickle cell trait is not independently associated with susceptibility to end-stage renal disease in African Americans. Kidney Int. 2011;80:1339–1343. doi: 10.1038/ki.2011.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanji Z, Powe CE, Wenger JB, Huang C, Ankers E, Sullivan DA, Collerone G, Powe NR, Tonelli M, Bhan I, Bernhardy AJ, DiBartolo S, Friedman D, Genovese G, Pollak MR, Thadhani R. Genetic Variation in APOL1 Associates with Younger Age at Hemodialysis Initiation. J Am Soc Nephrol. 2011;22:2091–2097. doi: 10.1681/ASN.2010121234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Genovese G, Friedman DJ, Ross MD, Lecordier L, Uzureau P, Freedman BI, Bowden DW, Langefeld CD, Oleksyk TK, Uscinski Knob AL, Bernhardy AJ, Hicks PJ, Nelson GW, Vanhollebeke B, Winkler CA, Kopp JB, Pays E, Pollak MR. Association of Trypanolytic ApoL1 Variants with Kidney Disease in African Americans. Science. 2010;329:841–845. doi: 10.1126/science.1193032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster MC, Coresh J, Fornage M, Astor BC, Grams M, Franceschini N, Boerwinkle E, Parekh RS, Kao WHL. APOL1 Variants Associate with Increased Risk of CKD among African Americans. J Am Soc Nephrol. 2013;24:2585–2491. doi: 10.1681/ASN.2013010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tzur S, Rosset S, Shemer R, Yudkovsky G, Selig S, Tarekegn A, Bekele E, Bradman N, Wasser W, Behar D, Skorecki K. Missense mutations in the APOL1 gene are highly associated with end stage kidney disease risk previously attributed to the MYH9 gene. Hum Genet. 2010;128:345–350. doi: 10.1007/s00439-010-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freedman BI, Langefeld CD, Turner J, Nunez M, High KP, Spainhour M, Hicks PJ, Bowden DW, Reeves-Daniel AM, Murea M, Rocco MV, Divers J. Association of APOL1 variants with mild kidney disease in the first-degree relatives of African American patients with non-diabetic end-stage renal disease. Kidney Int. 2012;82:805–811. doi: 10.1038/ki.2012.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lipkowitz MS, Freedman BI, Langefeld CD, Comeau ME, Bowden DW, Kao WHL, Astor BC, Bottinger EP, Iyengar SK, Klotman PE, Freedman RG, Zhang W, Parekh RS, Choi MJ, Nelson GW, Winkler CA, Kopp JB. Apolipoprotein L1 gene variants associate with hypertension-attributed nephropathy and the rate of kidney function decline in African Americans. Kidney Int. 2013;83:114–120. doi: 10.1038/ki.2012.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferguson R, Grim CE, Opgenorth TJ. A familail risk of chronic renal failure among blacks on dialysis. J Clin Epidemiol. 1988;41:1189–1196. doi: 10.1016/0895-4356(88)90023-6. [DOI] [PubMed] [Google Scholar]
- 18.Freedman BI, Tuttle AB, Spray BJ. Familial predisposition to nephropathy in African-Americans with non-insulin-dependent diabetes mellitus. Am J Kidney Dis. 1995;25:710–713. doi: 10.1016/0272-6386(95)90546-4. [DOI] [PubMed] [Google Scholar]
- 19.Freedman BI, Spray BJ, Tuttle AB, Buckalew VM., JR The familial risk of end-stage renal disease in Africian-americans. Am J Kidney Dis. 1993;21:387–393. doi: 10.1016/s0272-6386(12)80266-6. [DOI] [PubMed] [Google Scholar]
- 20.Bergman S, Key BO, Kirk KA, Warnock DG, Rostant SG. Kidney disease in the first-degree relatives of African-americans with hypertensive end-stage renal disease. Am J Kidney Dis. 1996;27:341–346. doi: 10.1016/s0272-6386(96)90356-x. [DOI] [PubMed] [Google Scholar]
- 21.Whittle JC, Whelton PK, Seidler AJ, Klag MJ. Does racial variation in risk factors explain black-white differences in the incidence of hypertensive end-stage renal disease? Arch Intern Med. 1991;151:1359–1364. [PubMed] [Google Scholar]
- 22.Ko W-Y, Rajan P, Gomez F, Scheinfeldt L, An P, Winkler CA, Froment A, Nyambo Thomas B, Omar Sabah A, Wambebe C, Ranciaro A, Hirbo Jibril B, Tishkoff Sarah A. Identifying Darwinian Selection Acting on Different Human APOL1 Variants among Diverse African Populations. Am J Hum Genet. 2013;93:54–66. doi: 10.1016/j.ajhg.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]


