Abstract
Background
Sports-associated sudden cardiac arrests (SCAs) occur mostly during middle age. We sought to determine burden, characteristics, and outcomes of SCA during sports among middle aged residents of a large US community.
Methods and Results
SCA cases aged 35–65 years were identified in a large, prospective, population-based study (2002–2013), with systematic and comprehensive assessment of their lifetime medical history. Of the 1,247 SCA cases, 63 (5%) occurred during sports activities at a mean age of 51.1±8.8 years, yielding an incidence of 21.7 (95%CI 8.1–35.4) per million per year. The incidence varied significantly based on sex, with a higher incidence among men (RR 18.68 95%CI 2.50–139.56) for sports SCA, as compared to all other SCA (RR 2.58, 95%CI 2.12–3.13). Sports SCA was also more likely to be a witnessed event (87 vs. 53%, P<0.001), with cardiopulmonary resuscitation (44 vs. 25%, P=0.001) and ventricular fibrillation (84 vs. 51%, P<0.0001). Survival to hospital discharge was higher for sports-associated SCA (23.2 vs. 13.6%, P=0.04). Sports SCA cases presented with known pre-existing cardiac disease in 16%, ≥1 cardiovascular risk factor in 56%, and overall, 36% of cases had typical cardiovascular symptoms during the week preceding SCA.
Conclusions
Sports-associated SCA in middle age represents a relatively small proportion of the overall SCA burden, reinforcing the idea of the high benefit-low risk nature of sports activity. Especially in light of current population aging trends, our findings emphasize that targeted education could maximize both safety and acceptance of sports activity in the older athlete.
Keywords: Physical, Coronary Artery Disease, Cardiopulmonary Resuscitation, Cardiac Arrest
Introduction
Sudden Cardiac Arrest (SCA) represents a major public health issue worldwide, accounting for almost half of cardiovascular mortality.1, 2 When occurring in the setting of sports, SCA generates major societal attention and alarm, since the collapse usually occurs in a public setting, in front of many witnesses, striking those considered to be the healthiest in the community.
SCA among young competitive athletes has been extensively investigated in the United States,3, 4 allowing significant improvements in the field, notably initiation and optimization of preventive strategies.5–9 However, except for limited data on specific recreational sport activities,10, 11 there are, to the best of our knowledge, no studies evaluating SCA during sports among middle-aged subjects in any United States community. Recent European experience has emphasized that, in the community, the largest burden of sports-associated SCA results from events among middle-aged participants.12–15 A better understanding of burden (absolute as well as relative to other non-sports related SCAs) and characteristics of SCA during sports in middle-aged population is likely to inform preventive strategies.
Available information has traditionally been restricted to resuscitation variables in the immediate setting of the event. However, for a study to be meaningful from a clinical perspective a detailed evaluation of the lifetime past medical history is needed, which is particularly challenging to obtain for SCA where the majority will inevitably die in the field, and consequently the information collected by Emergency Medical Services (EMS) is often restricted to data regarding the resuscitation process. Details of the past medical history of SCA patients (especially those that cannot be resuscitated) are thus usually sparse and very rarely considered systematically. In this regard, information concerning prior cardiovascular risk factors, frequency and type of symptoms in the weeks preceding SCA during sports, have not been previously characterized.
Using a large 12-year prospective study of SCA in a northwestern US metro region, with a systematic comprehensive evaluation of the lifetime clinical history, we assessed the characteristics and outcomes of SCA during sports in middle age compared to other SCAs (not occurring during sports activity).
Methods
Setting, Definitions and Survey Methods
The Oregon Sudden Unexpected Death Study (Oregon-SUDS) is an ongoing community based prospective study of out-of-hospital SCA. Detailed methods have been published previously.16,17 Briefly, since February 1, 2002, cases of SCA in the Portland Oregon metropolitan area were identified using multiple sources that included the Emergency Medical Services (EMS) response, the Medical Examiner’s office and emergency departments of all of the 16 local hospitals. The county has a two-tiered emergency medical response system with involvement of advanced cardiac life support staffed fire engine companies as well as transporting ambulances.
A comprehensive evaluation is performed for each case of unexpected death, including analysis of the circumstances of arrest recorded by EMS personnel or the medical examiner, pre-arrest medical records, and available autopsy data. A process of in-house adjudication by three physicians is employed to determine cases meeting criteria for SCA. In the event of a disagreement regarding a specific case, the determination is based on the majority opinion. In the present analysis we included middle-aged men and women, defined as male subjects aged 35–65 years, ascertained from February 2002 to January 2013. This study was approved by the Institutional Review Boards of Cedars-Sinai Medical Center, Oregon Health and Science University and all participating hospitals.
Sudden cardiac arrest was defined as a sudden unexpected pulseless condition; if un-witnessed, subjects were included if observed alive and symptom-free within 24 hours of their sudden arrest. During the adjudication process, patients with known non-cardiac causes of arrest (e.g., trauma, overdose, pulmonary embolism, cerebrovascular accident, and terminal illness such as cancer not in remission) were excluded.1, 15 SCA during sports was defined as death occurring during sports activities or within one hour of cessation of sports activity. In most cases, the event occurred as an unexpected collapse during physical exertion. Of note, SCA occurring during physical activity but not in the setting of sports (typically SCA during sexual intercourse) was not considered as sports-associated SCA. Previous medical history was obtained from a comprehensive assessment of inpatient as well outpatient medical records/visits obtained from the hospital systems in the Portland metropolitan area.
Variables Assessed
Variables considered in the present analysis included demographics, circumstances of occurrence as well as resuscitation data. In addition to detailed information obtained from EMS, index hospital stay, and medical examiner medical records, a working group of the Oregon-SUDS collected and assessed the lifetime past medical history for both deceased patients and consent survivors, including assessment of symptoms prior to SCA.
Variables included: (i) time and location of each event; (ii) clinical and demographic information (age, sex, personal history of known cardiovascular risk factors or heart disease, and any symptoms during the preceding week). Symptom assessment was derived from multiple sources, including family members at the scene of SCA, witnesses, and survivors of SCA. In addition, available hospital and outpatient medical records for all subjects were systematically analyzed for information regarding symptoms. Symptoms were categorized as absent, present or not evaluable based on the extent of information available, and the agreement of investigators. Coronary Artery Disease (CAD) was defined as ≥50% lumen stenosis on coronary angiogram prior to SCA event or identified at autopsy. In addition, subjects with past history of myocardial infarction or coronary revascularization (either surgical or percutaneous coronary intervention) were categorized as patients with CAD. History of heart failure was defined by a physician based on medical records (in-hospital and/or outpatient visit) and/or low left ventricular ejection fraction from echocardiogram, angiogram, or radionuclide multi-gated acquisition prior and unrelated to cardiac arrest; (iii) data regarding the setting and nature of sports activity at the time of the event; (iv) circumstances of collapse (during sports activity or immediately after), location type (sports facility or other area), presence of witnesses; (v) detailed information regarding resuscitation including response time (time from EMS call to their arrival on the scene), bystander cardiopulmonary resuscitation (CPR) initiation, the presenting cardiac rhythm (ventricular tachycardia/fibrillation, pulseless electrical activity or asystole), return of spontaneous circulation (defined as return of a palpable pulse in conjunction with a systolic blood pressure of >60 mmHg); (vi) survival status to hospital discharge, available in the majority of admitted cases (96%) — For survivors, neurologic status at discharge was evaluated using the Cerebral Performance Categories (CPC) score from medical records, and a comparative analysis was performed between sports-associated SCA and other SCA;14 (vii) autopsy report if available.
Statistical Analysis
This report was prepared in compliance with the STROBE checklist for observational studies.18 The objective of the study was to provide comprehensive comparisons between sports SCA and non-sports SCA, including subject characteristics and survival to hospital discharge as well as neurological outcomes. Case characteristics were reported as mean ± standard deviation, proportions, median and Interquartile Ranges (IQR), as appropriate. Comparisons between groups used χ2 test for categorical variables, Fisher Exact test when appropriate and Student’s t-test or Mann-Whitney test for continuous variables.
For calculation of incidence rates, the population was limited to Multnomah County, Oregon, the largest subset of the metro area residents (population 679,348, including 135,868 men and 133,598 women, aged 35 to 65 years, 2003 US Census Bureau data for the Multnomah County) and for the 2002–2005 period (where all SCAs were recorded). All Multnomah County residents, aged 35 to 65, were included for calculation of annual incidence rates in middle-aged men and women (calculated per year per million residents).
Predictors of survival to hospital discharge were studied among SCA cases with resuscitation attempted (N=936). Any variables in univariate analyses with a P value <0.15 were included in the multivariate modeling. The association of SCA with favorable outcome (survival to hospital discharge) was thereafter adjusted for these identified confounding factors in a single multivariable logistic regression analysis, allowing estimation of odds ratios (ORs) and their 95% confidence intervals (CIs). As a sensitivity analysis, to better appreciate the likelihood for survival when SCA occurs in the setting of sports activities, we performed additional analysis using propensity score matching.19 We calculated each subject’s propensity score as the predicted probability of having SCA during sports given the subject’s measured covariates (age, gender, history of coronary artery disease, presence of witness, bystander cardiopulmonary resuscitation, ventricular fibrillation, delay of intervention). We matched each case to the control subject (i.e., a patient who suffered a non-sports SCA) with the closest propensity score, which resulted in a dataset with 66 (33/33) SCA matched cases. All data were analyzed using STATA software version v11.0 (Lakeway Drive, TX).
Results
Patient Characteristics and Circumstances of SCA Occurrence
Between February 2002 and January 2013, there were a total of 63 subjects, middle-aged SCA cases that occurred during sports activities (Table 1), mainly during jogging (27%), basketball (17%) and cycling (14%) activities. Other sports activities included gym activities (11%), golfing (8%), volleyball (3%), tennis (3%), soccer (3%), and others (14%). Sports-associated SCA occurred during the actual sports activity in 45 cases (76%) and within the following hour in 14 (24%). More than half of the cases (58%) occurred in sports facilities such as a gym or a stadium, whereas the remainder (42%) occurred in the field (outside of sports facilities). Among the 28 sports-associated SCAs, which occurred outside of sports facilities, 18 occurred in public parks, jogging trails or other delineated areas.
Table 1.
Patient Characteristics for SCA Associated With Sports Versus Not Associated With Sports.
| Sports-Associated SCA N=63 |
Non Sports-Associated SCA N=1,184 |
P Value | |
|---|---|---|---|
| Demographic data | |||
| Age — yr | |||
| Mean±SD | 51.1±9 | 53.1±8 | 0.08 |
| 35–50 | 39 (62) | 648 (55) | 0.26 |
| 50–65 | 24 (38) | 536 (45) | |
| Timing — no. (%) | |||
| Weekend | 28 (44) | 314 (27) | 0.002 |
| Timing | <0.001 | ||
| Morning (6:00 am to 12:00 pm) | 16 (25) | 358 (30) | |
| Afternoon (12:00 pm to 6:00 pm) | 23 (37) | 268 (23) | |
| Night (6:00 pm to 06:00 am) | 7 (11) | 234 (20) | |
| Unknown | 17 (27) | 324 (27) | |
| Seasons | 0.24 | ||
| Summer | 19 (30) | 258 (22) | |
| Autumn | 14 (22) | 288 (24) | |
| Winter | 12 (19) | 340 (29) | |
| Spring | 18 (29) | 298 (25) | |
| Number of cardiovascular risk factor — no. (%) | 0.38 | ||
| None | 18 (43) | 354 (33) | |
| One | 9 (19) | 159 (15) | |
| More than one | 18 (38) | 509 (48) | |
| Type of cardiovascular risk factor — no. (%) | |||
| Diabetes mellitus | 4 (8) | 315 (28) | 0.002 |
| Dyslipidemia | 16 (33) | 290 (26) | 0.27 |
| Systemic hypertension | 19 (40) | 528 (47) | 0.28 |
| Body mass index (Kg/m2) | 29±6 | 30±8 | 0.21 |
| Smoking | 10 (31) | 451 (61) | 0.001 |
| Known heart disease — no. (%)* | 10 (16) | 358 (30) | 0.01 |
| Coronary artery disease | 5 (8) | 220 (19) | 0.03 |
| Atrial fibrillation | 3 (5) | 64 (5) | 0.82 |
| Heart failure | 3 (5) | 185 (16) | 0.02 |
| Pacemaker | 3 (5) | 56 (5) | 0.95 |
| Implantable Cardioverter Defibrillator | 0 (0) | 2 (0) | 1 |
SD denotes Standard Deviation. Percentages were calculated on the basis of the total number of known events.
Among consent survivors or deceased patients with medical records available (N=583, including 45 sports-associated SCA).
Of the overall number of middle-aged SCA cases in this region during the 10-year period (N=1,247), sports-associated SCA in middle age represented 5% of SCA cases in this age group, yielding an overall incidence of 21.7 (95%CI 8.1–35.4) per million per year compared to 555.0 (95%CI 541.4–568.7) for non-sports-associated SCA. The incidence varied significantly according to sex with a much higher incidence among men (vs. women) for sports-associated SCA (RR 18.68 95%CI 2.50–139.56), as opposed to all other SCA where differences were smaller (RR 2.58, 95%CI 2.12–3.13). Extrapolating to the overall population of the United States, we estimated the total number of sports-associated SCA among the 35–65 year-old age-group to be 2,269 (95%CI 772–3,773) events among men and 136 (95%CI 0–1,846) events among women per year.
The mean age of patients developing SCA during sports was 51.1±8.8 years, without significant difference between men and women (51.1±9.1 vs. 50.3±4.6 years, P=0.86). Although there was an apparent similar overall prevalence of cardiovascular risk factors (≥1 cardiovascular risk factors, 56.3 vs. 62.7%, P=0.40), sports SCA cases were less likely to present with smoking (31.3 vs. 60.8%, P=0.001) and diabetes mellitus (8.3 vs. 28.4%, P=0.002). Sports SCA cases were also less likely to have known heart disease compared to non-sports SCA (15.9 vs. 30.2%, P=0.013) (Table 1). Among the 44 middle-aged participants with possible assessment of symptoms during the week before the event, 14 (33%) presented with symptoms: typical chest pain in nine, dyspnea in four, and typical influenza-like symptoms in one. While there were significant sex differences in incidence of sports-associated SCA with higher burden in men, no significant differences were identified between men and women for clinical characteristics, circumstances and outcomes.
Bystander CPR, Advanced Life-Support and Predictors of Survival
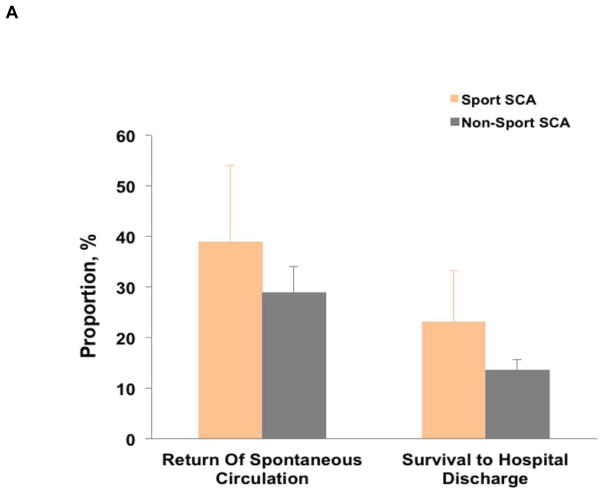
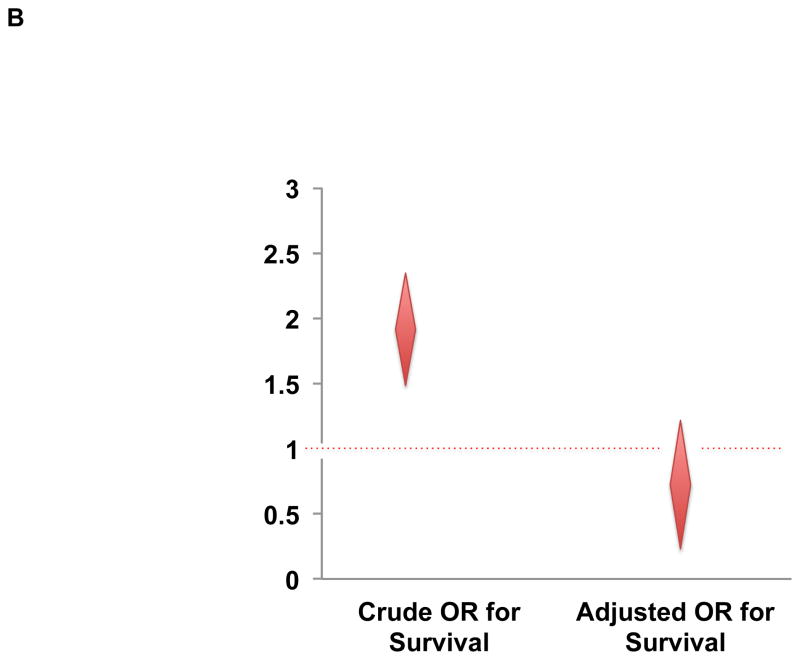
Descriptive data on resuscitation and survival after SCA, based on the association with sports, are presented in Table 2. When compared to other SCAs, SCAs during sports were characterized by a greater proportion of witnessed events (87 vs. 52%, P<0.001), bystander CPR (44 vs. 25%, P=0.001), as well as a greater likelihood of presenting with a shockable rhythm (84 vs. 51%, P<0.001). The mean response time (6.8±4 min) was very similar between both groups (P=0.99), with the proportion of patients receiving intervention within 8 min being 77% and 79% in sports SCA and non-sport SCA, respectively (P=0.44). Survival to hospital discharge was higher for sports-associated SCA (23.2%, 95%CI 11.8–34.6) compared to SCA not associated with sports (13.6%, 95%CI 11.6–15.5) (P=0.04) (Figure 1-Panel A).
Table 2.
Setting and Outcomes of SCA Associated With Sports Versus Not Associated With Sports.
| Sports-Associated SCA N=63 |
Non Sports-Associated SCA N=1,184 |
P Value | |
|---|---|---|---|
| Public occurrence — no. (%) | 55 (90) | 242 (22) | <0.001 |
| Sudden death witnessed — no. (%) | 55 (87) | 614 (52) | <0.001 |
| Bystander CPR — no. (%) | 28 (44) | 300 (25) | 0.001 |
| First rhythm recorded on preadmission electrocardiogram — no. (%) | <0.001 | ||
| Ventricular fibrillation | 42 (84) | 437 (51) | |
| Asystole | 4 (8) | 180 (21) | |
| Pulseless electrical activity | 4 (8) | 228 (27) | |
| Undetermined | 0 (0) | 9 (1) | |
| Call-to-EMS arrival — no. (%) | |||
| Mean±SD | 6.79±4 | 6.80±4 | 0.99 |
| ≤8min | 34 (77) | 631 (79) | 0.44 |
| ROSC — no. (%) | 24 (39) | 241 (29) | 0.11 |
| Survival to hospital discharge — % (95% confidence interval) | 23.2 (11.8–34.6) | 13.6 (11.6–15.5) | 0.04 |
EMS denotes Emergency Medical Services; ROSC, Return Of Spontaneous Circulation
Percentages were calculated on the basis of the total number of known events.
Figure 1.
Panel A – Proportion of patients with return of spontaneous circulation and survival to hospital discharge, according to sudden cardiac arrest (SCA) occurring during sports or not during sports; Panel B – Odds ratio for survival to hospital discharge of Sports SCA compared to Non-Sports SCA (crude and adjusted for age, sex, initial rhythm, response time, presence of witness, bystander cardiopulmonary resuscitation, ventricular fibrillation). Error bars indicate upper 95% confidence interval.
Among overall SCAs with resuscitation attempted, variables independently (multivariate analysis) associated with survival included public location (OR 1.55, 95%CI 1.10–2.17, P=0.011), presence of witness (OR 3.22, 95%CI 1.80–5.77, P<0.0001), and initial shockable rhythm (OR 4.54, 95%CI 2.94–7.14, P<0.0001). SCA in the setting of sports activity was not associated with higher survival after adjustment for resuscitation variables (OR 0.82, 95% CI 0.36–1.82, P=0.62) (Figure 1-Panel B). From the additional sensitivity analysis, the propensity-score matched odds ratio for survival was not significantly associated with sports-SCA: OR 0.84 (95% CI 0.19–3.80, P=0.82). In addition, no significant association was observed for age (≤50 vs. >50 years) (OR 1.13, 95%CI 0.74–1.74, P=0.55) and delay in EMS response (<8min vs. ≥8min) (OR 0.96, 95%CI 0.69–1.34, P=0.83).
Etiologies of SCA could be identified in 829 cases (66%), without significant difference between the sports-associated and non sports-associated SCA (68 vs. 66%, respectively, P=0.76). The overall patterns of causes of SCA among sports and non-sports SCA are relatively similar (Figure 2), with a predominance of coronary artery disease: among the 829 cases, 36 out of 43 (84%) sports-associated SCA were associated with CAD, compared to 717 out of 786 (91%) for other SCAs. The phenotype of coronary artery disease among SCA cases, based on the setting of occurrence (sports vs. non-sports) is reported in Table 3, for overall 181 (24%) of cases with typical features of acute coronary syndrome (either on cardiac pathology or coronary angiogram). Among those subjects with known coronary artery disease (517 subjects), 140 (27%) had undergone a revascularization procedure (percutaneous coronary intervention in 46%) prior to developing SCA. Other causes of SCA included dilated cardiomyopathy (30), hypertrophic cardiomyopathy (30), congenital heart disease (6), mitral valve prolapse (3), myocarditis (3), and arrhythmogenic right ventricular dysplasia (2) (Figure 2).
Figure 2.
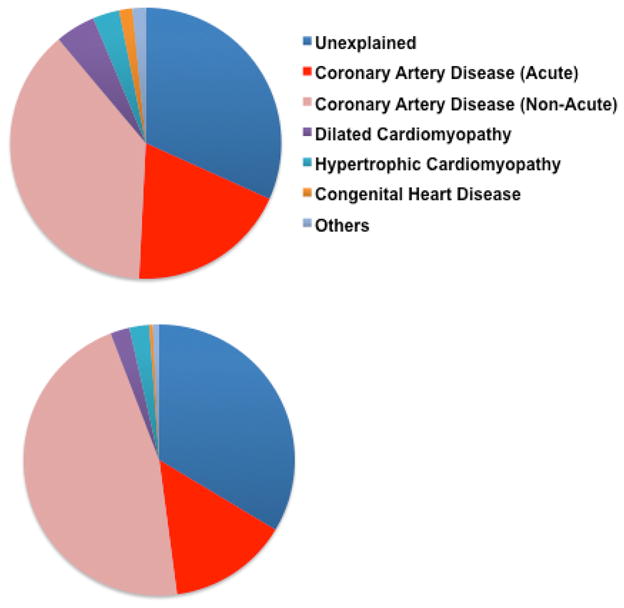
Distribution of Cardiovascular Abnormalities Associated With Sudden Cardiac Arrest (SCA) in the 1,247 Subjects, According to Sports SCA (Upper Pie, N=63) and Non-Sports SCA (Lower Pie, N=1,184).
Table 3.
Coronary Artery Disease Associated With Sudden Cardiac Arrest: Sports Versus Not Associated With Sports.
| Sports-Associated SCA N=63 |
Non Sports-Associated SCA N=1,184 |
P Value | |
|---|---|---|---|
| SCA with cause assessed — no. (%) | 43 (68) | 786 (66) | 0.89 |
| Frequency of CAD — no. (%) | 36 (84) | 717 (91) | 0.10 |
| Coronary presentation | 0.23 | ||
| Acute MI — no. (%) | 12 (33) | 169 (24) | |
| History of CAD — no. (%) | 3 (25) | 69 (41) | |
| No history — no. (%) | 9 (75) | 100 (59) | |
| No Acute MI — no. (%) | 24 (66) | 548 (76) | |
| History of CAD — no. (%) | 17 (71) | 428 (78) | |
| No history — no. (%) | 7 (29) | 120 (22) | |
| History of CAD — no. (%) | 20 (56) | 497 (69) | 0.08 |
| Prior revascularization | 2 (10) | 138 (28) | 0.12 |
| Surgical | 1 (5) | 74 (15) | |
| PCI | 1 (5) | 64 (13) | |
| History of angina | 0 (0) | 22 (4) | 0.99 |
| History of MI | 12 (60) | 246 (49) | 0.37 |
| Mean EF | 48.1±18 | 47.1±16 | 0.84 |
CAD denotes coronary artery disease; EF, ejection fraction of the left ventricle; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Percentages were calculated on the basis of the total number of known events.
Discussion
To the best of our knowledge, this study represents the first comprehensive assessment of SCA associated with sports activity among middle-aged participants in a US community. First, our findings emphasize that sports-associated SCA eventually represented a relatively small proportion of overall SCA in this population; a fact that is likely to encourage sports activities among middle-aged athletes, after appropriate attention to any existing musculo-skeletal limitations. Second, the comprehensive assessment of the lifetime past medical history revealed that in almost two third of cases, patients present with either a previously documented significant cardiovascular disease and/or symptoms prior to the event. This latter finding suggests that utilization of educational and general awareness approaches may further decrease sports-associated SCA burden.
Due to a disproportionate emotional and lay press response to sudden death during sports, quantification of the burden requires objective assessment . The design of our study, based on multiple sources of ascertainment, was especially useful to ensure that all cases of interest were captured. The incidence of sports-associated SCA estimated in this study is highly similar to recently reported experiences among men in Europe (from 33 to 58 per million per year).12, 13 However, by evaluating sports-associated SCA as well as overall SCAs in the same time period and geographical area, we were able to place the burden of sports-associated SCA in the context of overall SCA burden, and report that it eventually represented a small proportion of cases (one SCA out of 20). This finding suggests that in the context of SCA, the overall risk-benefit ratio is in favor of sports activity.12, 13.
In our population, the incidence ratio between men and women was 7-fold higher in sports SCA compared to non-sports SCA. Whether this reflects an intrinsic difference in pathophysiology between sexes is still speculative, but some factors merit consideration. First, men may have higher sports participation rates than women, which may contribute to the gender differences in SCA rates. Consistent with this observation, the incidence of SCA in women was transiently elevated during moderate to vigorous exertion but with a RR of only 2.38 (95% CI 1.23 to 4.60), while being almost 20-fold higher (RR 44.9, 95% CI 26.7 to 75.4) during vigorous activity among men enrolled in the Physicians’ Health Study.20, 21 Similar gender differences have also been reported in smaller retrospective studies in Finland and in the United States.22, 23 Second, the duration per sports session as well as the vigor and the method of physical activity could differ between men and women. However, in considering inherent sex differences, potential explanations could include a number of factors, such as differences in vulnerable substrate (underlying structural or electrical heart disorder), triggers and/or autonomic modulators. The age-specific prevalence of coronary heart disease is known to be lower in middle-aged women (compared to men), and a particularly low prevalence has been also observed among female victims of SCA, suggesting that women may have lower rates of sports SCA with myocardial ischemia as the primary cause.24 Another interesting factor relates to coronary plaque rupture, which has been associated with a significant proportion of sports-related acute coronary syndrome and SCA.25 Overall, women are significantly more likely to have plaque erosions (as opposed to plaque rupture) than men, potentially suggesting an inherently lower likelihood of plaque rupture in the setting of exercise in women. Sex-related differences in ventricular repolarization and vagal tone are also potential factors affecting sports SCA pathophysiology.25
Subjects that suffer SCA during sports activity are generally perceived as previously healthy individuals with the event being considered as truly “unexpected’. Our comprehensive assessment of the past medical history in these cases demonstrates that in more than half, subjects had at least one cardiovascular risk factor. However, it is important to bear in mind that the long-term benefits of regular exercise on cardiovascular health are well established,21, 26 and habitual physical activity has been demonstrated to reduce coronary heart disease events. While existence of a “sports paradox” has been recognized— vigorous activity can also acutely and transiently increase the risk of SCA and acute myocardial infarction, especially in those not habituated to exercise — overall, the long-term benefits outweigh the short-term risks related to physical activity.21 Thus, the findings from this study should in no way discourage patients with cardiovascular risk factors from engaging in regular, appropriate physical exercise within a framework of simple guiding rules from the treating physician. Whether a cautionary note needs to be raised with respect to sports in those with established coronary artery disease, is a clinical question that needs further investigation. Physical activity counseling must be tailored to the needs and circumstances of the individual, thereby increasing the likelihood of success and decreasing the risk of cardiovascular events during vigorous exercise.27–29 In this context, education of patients with recognized cardiovascular disease or risk factors regarding avoidance of extreme exercise may minimize any potential harm,23 while maximizing the acceptance of sports activity as a tool to improve cardiovascular fitness.21
Of interest, the proportion of patients with cardiovascular risk factors may appear higher when compared to the first published community-based report on SCA during sports in France (11%).12 Although differences in subjects’ characteristics may partly explain such differences, the lower rates in Europe may reflect the challenges in retrieving the detailed lifetime medical history in some studies. In addition, a significant proportion of the middle-aged subjects, who eventually died during sports activity, exhibited cardiac symptoms within a short period (one week) preceding the SCA event. Taken together, these findings suggest that careful attention to pre-existing heart disease and warning signs, along with public education and awareness in this regard may have an important place in the overall strategy to reduce SCA associated with sports activity.
Overall, only one third of witnessed SCA cases received bystander CPR indicating substantial room for improvement in public knowledge and attitudes towards basic life support.30–33 Bystander-CPR is more likely to be initiated for SCA during sports, and this may have contributed to the higher likelihood of shockable rhythms at arrival of EMS, also extending the window of opportunity for successful defibrillation.34, 35 The sports-associated SCA setting has appeal for the public and can serve as a springboard to efficiently educate the public regarding basic life support. Therefore, these findings also have potential implications for pre-hospital emergency care policy-making to promote community education in basic life support.36, 37 Although SCA during sport is associated with a higher survival,38, 39 it seems that this is mainly explained by the concomitant association with factors that have a positive impact on the resuscitation process, such as presentation with a shockable rhythm and the presence of witnesses during the SCA. Sports facilities have been identified as being particularly suitable for AED deployment,40 and where AED placement has largely been considered advisable.41 Our data further emphasize the need for systematic availability of AEDs in public sports facilities.42 However, since a good proportion of SCA occurred outside sports facilities, there is still room for improvement in public AED deployment. One potential strategy under consideration is AED placement in strategic locations such as public parks and popular jogging trails. Additionally public education to increase awareness also has an important role in improving bystander CPR. Although our data are, to the best of our knowledge, the first to address the issue related to burden and outcomes among the middle age from the general population in a large US community, with a particular efforts to provide data on past medical history, we acknowledge some limitations. Firstly, due to the extremely low incidence of SCA among women, statistical power to assess gender-related differences in sports SCA was limited. Second, we do not have access to information regarding whether or not cases of sports-associated SCA underwent regular training prior to the SCA. Regular training has been shown to reduce the incidence of SCA during sports activity.21 Third, we are not able to provide details regarding the level of exercise at the time of SCA for the entire period. Because there is no evidence to support a triggering effect of light exertion for SCA,20 it may be possible that some of SCAs occurring during sports activities were associated by chance and not related to the activity itself. Hence our use of the term ‘sports-associated’ rather than ‘sports-related’ SCA. For the SCA cases which occurred between 2002 and 2006, an estimated metabolic equivalent (MET) score, reflecting the intensity of exercise was calculated.43, 44 One MET is the amount of energy spent by a person sitting quietly. Physical activities were classified into three groups: light (<4 MET), moderate (4–6 MET), and heavy (>6 METS) sport activity. Overall, among the 30 SCA during sports activities with estimated MET available between 2002 and 2006, light exertion was observed in 14% of SCA cases, whereas moderate and vigorous were observed in 50% and 38%, respectively. Finally, specific coronary pathology examination could provide important information especially details of potential sex-specific abnormalities, but were not routinely performed by the medical examiner in Portland, Oregon.
In conclusion, the burden of sports-associated SCA among middle-aged participants is relatively low when compared to the overall SCA burden in the community. Our findings of a high prevalence of established cardiovascular disease as well as symptoms that manifested in advance of SCA highlight a prevention gap that can potentially be closed. The significant prevalence of known cardiovascular disease and prior symptoms in affected participants offers an opportunity for targeted education in order to maximize both safety and acceptance of sports activity in the middle-aged group.
Acknowledgments
We gratefully acknowledge the assistance of all Emergency Medical Services personnel (American Medical Response, Portland/Gresham fire departments), the Oregon State Medical Examiner’s office and the 16 hospitals in the Portland Oregon metro area. We thank Professor David Celermajer (Sydney Medical School, Sydney) as well as Doctor Wulfran Bougouin (Paris Sudden Death Expertise Center, Paris) for their helpful and constructive review of the paper.
Funding Sources: This work was funded in part by National Heart, Lung, and Blood Institute grants R01HL105170 and R01HL122492 to Dr. Chugh. Dr. Chugh holds the Pauline and Harold Price Chair in Cardiac Electrophysiology at the Heart Institute, Cedars-Sinai Medical Center, Los Angeles, CA. E.M. is a Visiting Faculty Scientist at the Cedars-Sinai Heart Institute funded by research grant support from the Fondation pour la Recherche Medicale, the Philip Foundation, and the French Society of Cardiology.
Footnotes
Disclosures: None.
References
- 1.Fishman GI, Chugh SS, Dimarco JP, Albert CM, Anderson ME, Bonow RO, Buxton AE, Chen PS, Estes M, Jouven X, Kwong R, Lathrop DA, Mascette AM, Nerbonne JM, O’Rourke B, Page RL, Roden DM, Rosenbaum DS, Sotoodehnia N, Trayanova NA, Zheng ZJ. Sudden cardiac death prediction and prevention: report from a National Heart, Lung, and Blood Institute and Heart Rhythm Society Workshop. Circulation. 2010;122:2335–2348. doi: 10.1161/CIRCULATIONAHA.110.976092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of Sudden Cardiac Death in National Collegiate Athletic Association Athletes. Circulation. 2011;123:1594–1600. doi: 10.1161/CIRCULATIONAHA.110.004622. [DOI] [PubMed] [Google Scholar]
- 4.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119:1085–1092. doi: 10.1161/CIRCULATIONAHA.108.804617. [DOI] [PubMed] [Google Scholar]
- 5.Drezner JA, Levine BD, Vetter VL. Reframing the debate: Screening athletes to prevent sudden cardiac death. Heart Rhythm. 2013;10:454–455. doi: 10.1016/j.hrthm.2012.12.037. [DOI] [PubMed] [Google Scholar]
- 6.Drezner JA. Contemporary approaches to the identification of athletes at risk for sudden cardiac death. Curr Opin Cardiol. 2008;23:494–501. doi: 10.1097/HCO.0b013e32830b3624. [DOI] [PubMed] [Google Scholar]
- 7.Uberoi A, Stein R, Perez MV, Freeman J, Wheeler M, Dewey F, Peidro R, Hadley D, Drezner J, Sharma S, Pelliccia A, Corrado D, Niebauer J, Estes NAM, Ashley E, Froelicher V. Interpretation of the Electrocardiogram of Young Athletes. Circulation. 2011;124:746–757. doi: 10.1161/CIRCULATIONAHA.110.013078. [DOI] [PubMed] [Google Scholar]
- 8.Kaltman JR, Thompson PD, Lantos J, Berul CI, Botkin J, Cohen JT, Cook NR, Corrado D, Drezner J, Frick KD, Goldman S, Hlatky M, Kannankeril PJ, Leslie L, Priori S, Saul JP, Shapiro-Mendoza CK, Siscovick D, Vetter VL, Boineau R, Burns KM, Friedman RA. Screening for Sudden Cardiac Death in the Young: Report From a National Heart, Lung, and Blood Institute Working Group. Circulation. 2011;123:1911–1918. doi: 10.1161/CIRCULATIONAHA.110.017228. [DOI] [PubMed] [Google Scholar]
- 9.Drezner JA. Detect, manage, inform: a paradigm shift in the care of athletes with cardiac disorders? Br J Sports Med. 2013;47:4–5. doi: 10.1136/bjsports-2012-091963. [DOI] [PubMed] [Google Scholar]
- 10.Thompson PD, Funk EJ, Carleton RA, Sturner WQ. Incidence of death during jogging in Rhode Island from 1975 through 1980. JAMA. 1982;247:2535–2538. [PubMed] [Google Scholar]
- 11.Harris KM, Henry JT, Rohman E, Haas TS, Maron BJ. Sudden death during the triathlon. JAMA. 2010;303:1255–1257. doi: 10.1001/jama.2010.368. [DOI] [PubMed] [Google Scholar]
- 12.Marijon E, Tafflet M, Celermajer DS, Dumas F, Perier MC, Mustafic H, Toussaint JF, Desnos M, Rieu M, Benameur N, Le Heuzey JY, Empana JP, Jouven X. Sports-related sudden death in the general population. Circulation. 2011;124:672–681. doi: 10.1161/CIRCULATIONAHA.110.008979. [DOI] [PubMed] [Google Scholar]
- 13.Berdowski J, de Beus MF, Blom M, Bardai A, Bots ML, Doevendans PA, Grobbee DE, Tan HL, Tijssen JG, Koster RW, Mosterd A. Exercise-related out-of-hospital cardiac arrest in the general population: incidence and prognosis. Eur Heart J. 2013;34:3616–3623. doi: 10.1093/eurheartj/eht401. [DOI] [PubMed] [Google Scholar]
- 14.Marijon E, Bougouin W, Perier MC, Celermajer DS, Jouven X. Incidence of sports-related sudden death in France by specific sports and sex. JAMA. 2013;310:642–643. doi: 10.1001/jama.2013.8711. [DOI] [PubMed] [Google Scholar]
- 15.Marijon E, Bougouin W, Celermajer DS, Périer MC, Dumas F, Benameur N, Karam N, Lamhaut L, Tafflet M, Mustafic H, de Deus NM, Le Heuzey JY, Desnos M, Avillach P, Spaulding C, Cariou A, Prugger C, Empana JP, Jouven X. Characteristics and outcomes of sudden cardiac arrest during sports in women. Circ Arrhythm Electrophysiol. 2013;6:1185–1191. doi: 10.1161/CIRCEP.113.000651. [DOI] [PubMed] [Google Scholar]
- 16.Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, Ilias N, Vickers C, Dogra V, Daya M, Kron J, Zheng ZJ, Mensah G, McAnulty J. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 17.Reddy PR, Reinier K, Singh T, Mariani R, Gunson K, Jui J, Chugh SS. Physical activity as a trigger of sudden cardiac arrest: the Oregon Sudden Unexpected Death Study. Int J Cardiol. 2009;131:345–349. doi: 10.1016/j.ijcard.2007.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vandenbroucke JP. The making of STROBE. Epidemiology. 2007;18:797–799. doi: 10.1097/EDE.0b013e318157725d. [DOI] [PubMed] [Google Scholar]
- 19.Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whang W, Manson JE, Hu FB, Chae CU, Rexrode KM, Willett WC, Stampfer MJ, Albert CM. Physical exertion, exercise, and sudden cardiac death in women. JAMA. 2006;295:1399–1403. doi: 10.1001/jama.295.12.1399. [DOI] [PubMed] [Google Scholar]
- 21.Albert CM, Mittleman MA, Chae CU, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343:1355–1361. doi: 10.1056/NEJM200011093431902. [DOI] [PubMed] [Google Scholar]
- 22.Vuori I. The cardiovascular risks of physical activity. Acta Med Scand Suppl. 1986;711:205–214. doi: 10.1111/j.0954-6820.1986.tb08951.x. [DOI] [PubMed] [Google Scholar]
- 23.Siscovick DS. Exercise and its role in sudden cardiac death. Cardiol Clin. 1997;15:467–472. doi: 10.1016/s0733-8651(05)70352-0. [DOI] [PubMed] [Google Scholar]
- 24.Albert CM, McGovern BA, Newell JB, Ruskin JN. Sex differences in cardiac arrest survivors. Circulation. 1996;93:1170–1176. doi: 10.1161/01.cir.93.6.1170. [DOI] [PubMed] [Google Scholar]
- 25.Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125:620–637. doi: 10.1161/CIRCULATIONAHA.111.023838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, 3rd, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 27.Thompson PD, Franklin BA, Balady GJ, Blair SN, Corrado D, Estes NA, 3rd, Fulton JE, Gordon NF, Haskell WL, Link MS, Maron BJ, Mittleman MA, Pelliccia A, Wenger NK, Willich SN, Costa F American Heart Association Council on Nutrition PA, Metabolism, American Heart Association Council on Clinical C and American College of Sports M. Exercise and acute cardiovascular events placing the risks into perspective: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation. 2007;115:2358–2368. doi: 10.1161/CIRCULATIONAHA.107.181485. [DOI] [PubMed] [Google Scholar]
- 28.Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, Coke LA, Fleg JL, Forman DE, Gerber TC, Gulati M, Madan K, Rhodes J, Thompson PD, Williams MA, Stroke N American Heart Association Exercise CR, Prevention Committee of the Council on Clinical Cardiology CoNPA, Metabolism CoC, Council on E and Prevention. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128:873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 29.Koller A, Shephard RJ, Balady GJ. Exercise as cardiovascular therapy. Circulation. 2000;101:E164. doi: 10.1161/01.cir.101.14.e164. [DOI] [PubMed] [Google Scholar]
- 30.Schober P, van Dehn FB, Bierens JJ, Loer SA, Schwarte LA. Public access defibrillation: time to access the public. Ann Emerg Med. 2011;58:240–247. doi: 10.1016/j.annemergmed.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 31.Bobrow BJ, Vadeboncoeur TF, Spaite DW, Potts J, Denninghoff K, Chikani V, Brazil PR, Ramsey B, Abella BS. The effectiveness of ultrabrief and brief educational videos for training lay responders in hands-only cardiopulmonary resuscitation: implications for the future of citizen cardiopulmonary resuscitation training. Circ Cardiovasc Qual Outcomes. 2011;4:220–226. doi: 10.1161/CIRCOUTCOMES.110.959353. [DOI] [PubMed] [Google Scholar]
- 32.Marijon E, Bougouin W, Celermajer DS, Perier MC, Benameur N, Lamhaut L, Karam N, Dumas F, Tafflet M, Prugger C, Mustafic H, Rifler JP, Desnos M, Le Heuzey JY, Spaulding CM, Avillach P, Cariou A, Empana JP, Jouven X. Major regional disparities in outcomes after sudden cardiac arrest during sports. Eur Heart J. 2013;34:3632–3640. doi: 10.1093/eurheartj/eht282. [DOI] [PubMed] [Google Scholar]
- 33.Sasson C, Meischke H, Abella BS, Berg RA, Bobrow BJ, Chan PS, Root ED, Heisler M, Levy JH, Link M, Masoudi F, Ong M, Sayre MR, Rumsfeld JS, Rea TD. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–1350. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
- 34.Herlitz J, Ekstrom L, Wennerblom B, Axelsson A, Bang A, Holmberg S. Effect of bystander initiated cardiopulmonary resuscitation on ventricular fibrillation and survival after witnessed cardiac arrest outside hospital. Br Heart J. 1994;72:408–412. doi: 10.1136/hrt.72.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bobrow BJ, Clark LL, Ewy GA, Chikani V, Sanders AB, Berg RA, Richman PB, Kern KB. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299:1158–1165. doi: 10.1001/jama.299.10.1158. [DOI] [PubMed] [Google Scholar]
- 36.Drezner JA, Rao AL, Heistand J, Bloomingdale MK, Harmon KG. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009;120:518–525. doi: 10.1161/CIRCULATIONAHA.109.855890. [DOI] [PubMed] [Google Scholar]
- 37.Drezner JA. Preparing for sudden cardiac arrest--the essential role of automated external defibrillators in athletic medicine: a critical review. Br J Sports Med. 2009;43:702–707. doi: 10.1136/bjsm.2008.054890. [DOI] [PubMed] [Google Scholar]
- 38.Drezner JA, Rogers KJ. Sudden cardiac arrest in intercollegiate athletes: detailed analysis and outcomes of resuscitation in nine cases. Heart Rhythm. 2006;3:755–759. doi: 10.1016/j.hrthm.2006.03.023. [DOI] [PubMed] [Google Scholar]
- 39.Drezner JA, Chun JSDY, Harmon KG, Derminer L. Survival trends in the United States following exercise-related sudden cardiac arrest in the youth: 2000–2006. Heart Rhythm. 2008;5:794–799. doi: 10.1016/j.hrthm.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 40.American College of Sports Medicine and American Heart Association joint position statement: automated external defibrillators in health/fitness facilities. Med Sci Sports Exerc. 2002;34:561–564. doi: 10.1097/00005768-200203000-00027. [DOI] [PubMed] [Google Scholar]
- 41.Drezner JA, Courson RW, Roberts WO, Mosesso VN, Jr, Link MS, Maron BJ. Inter-association task force recommendations on emergency preparedness and management of sudden cardiac arrest in high school and college athletic programs: a consensus statement. Heart Rhythm. 2007;4:549–565. doi: 10.1016/j.hrthm.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 42.Drezner JA, Asif IM, Harmon KG. Automated external defibrillators in health and fitness facilities. Phys Sportsmed. 2011;39:114–118. doi: 10.3810/psm.2011.05.1901. [DOI] [PubMed] [Google Scholar]
- 43.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 44.Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329:1677–1683. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]