Abstract
Background
Few published data describe survival rates for pediatric end-stage renal disease (ESRD) patients. We aimed to describe 1-year mortality rates for US pediatric ESRD patients over a 15-year period.
Summary
In this retrospective cohort study, we used the United States Renal Data System database to identify period prevalent cohorts of patients aged younger than 19 years for each year 1995–2010. Yearly cohorts averaged approximately 1200 maintenance dialysis patients (60% hemodialysis, 40% peritoneal dialysis) and 1100 transplant recipients. Patients were followed for up to 1 year and censored at change in modality, loss to follow-up, or death. We calculated unadjusted model-based mortality rates per time at risk, within each cohort year, by treatment modality (hemodialysis, peritoneal dialysis, transplant) and patient characteristics; percentage of deaths by cause; and overall adjusted odds of mortality by characteristics and modality. Approximately 50% of patients were aged 15–18 years, 55% were male, and 45% were female. The most common causes of ESRD were congenital/reflux/obstructive causes (55%) and glomerulonephritis (30%). One-year mortality rates showed evidence of a decrease for peritoneal dialysis patients (6.03 per 100 patient-years, 1995; 2.43, 2010; P = 0.0263). Mortality rates for transplant recipients (average 0.68 per 100 patient-years) were consistently lower than rates for all dialysis patients (average 4.36 per 100 patient-years).
Key Message
One-year mortality rates differ by treatment modality in pediatric ESRD patients.
Keywords: Dialysis, end-stage renal disease, mortality, pediatrics
Introduction
In the United States, the incidence of pediatric end-stage renal disease (ESRD) increased 7.5%, from 14.6 per million population in 1995 to 15.7 in 2010 [1]. Prevalence increased 25.3%, from 71.0 per million population in 1995 to 89.0 in 2010. Of the 1395 patients aged 0 to 19 years who began renal replacement therapy in 2010, 81.4% received dialysis and 18.6% underwent kidney transplant. A US study of survival in adolescents with ESRD using United States Renal Data System (USRDS) data found improved survival rates for those undergoing kidney transplant compared with those receiving maintenance dialysis [2].
Mortality rates remain a major concern for the pediatric ESRD population. Mortality rates are higher for children undergoing kidney transplant than for children in the general population, and even higher for children receiving dialysis than for children undergoing kidney transplant [3]. A recent study reported a significant decrease in overall mortality rates over time among children initiating dialysis treatment between 1990 and 2010, but did not evaluate trends in 1-year mortality rates or compare rates across ESRD treatment groups [4]. Though 1-year mortality rates have decreased in US adults receiving maintenance dialysis [5], we were unable to find studies that examined 1-year mortality rates over time and by treatment modality for pediatric ESRD patients. Thus, in this study, we describe the trends and patterns in 1-year mortality rates and risk in the pediatric ESRD population over time (1995–2010) and by treatment modality and age group.
Subjects and Methods
Data Sources and Study Design
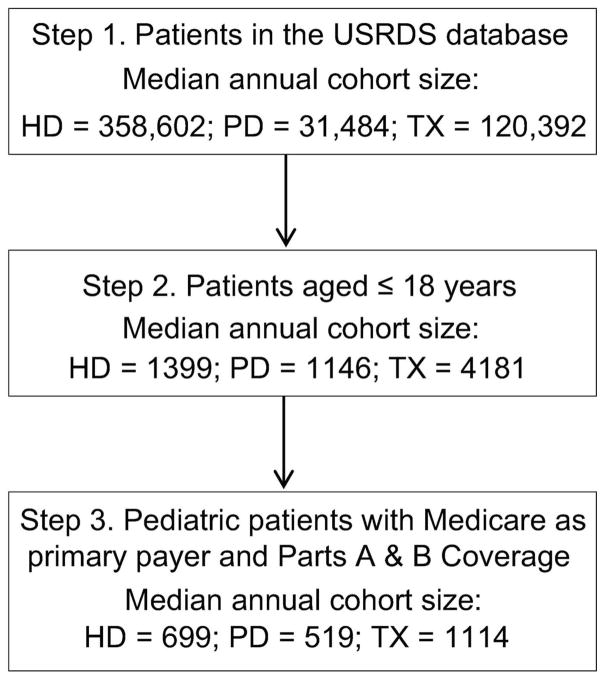
This was a retrospective cohort study using USRDS data. We created annual cohorts of period prevalent pediatric (aged < 19 years) ESRD patients for 1995–2010. Annual cohorts included patients prevalent as of January 1 and patients who were incident at any time during the year. We could not analyze incident patients separately because cohort counts were too small for stable estimates, but all adjusted results include adjustment for ESRD status (incident vs. prevalent). Eligible patients were required to have full Medicare coverage for medical and physician services. Complete Medicare claims coverage was needed to allow for censoring at changes in treatment modality (Figure 1). Patients in the dialysis cohorts may have previously undergone kidney transplant. Since new cohorts were created for each year and patients were followed for up to 1 year, patients who survived and maintained eligibility appeared in multiple cohort years. In each year, follow-up began on January 1 for prevalent patients and on the date of ESRD initiation for incident patients. Follow-up continued until the earliest date of death, change in renal replacement therapy, loss to follow-up, or end of the cohort year (December 31). Patients could be considered incident only once, but patients who were censored during the year due to a change in treatment modality may have been included (if eligible) in the prevalent cohort of the next year under their new modality.
Figure 1.
Selection diagram for annual period prevalent cohorts. HD, hemodialysis; PD, peritoneal dialysis; TX, transplant.
Patient demographic and clinical characteristics included age at the beginning of follow-up (0–4, 5–9, 10–14, 15–18 years), sex, race (white, black, other), primary cause of ESRD (glomerulonephritis, congenital/reflux/obstructive, other, unknown/missing), ESRD status (incident, prevalent), and treatment modality (hemodialysis, peritoneal dialysis, transplant). Registration on a kidney transplant waiting list (yes/no) was identified from United Network for Organ Sharing data, and comorbidity status (none, ≥ 1, missing) from the Centers for Medicare & Medicaid (CMS) Medical Evidence Report (form CMS-2728). Cause-specific mortality (cardiovascular, infection, malignancy, missing, other) was determined from the CMS ESRD Death Notification (form CMS-2746); relevant codes appear in Table S1.
Patient characteristic variables were examined by cohort year, ESRD treatment modality, and age group. A chi-square test for independence was used to test for differences by group; results were considered significant at the 0.05 level.
Mortality Rates and Odds of Death
The unadjusted 1-year mortality rate per 100 patient-years was calculated for each annual cohort of period prevalent patients as: 100*(number of deaths)/(total time at risk, expressed in years). A model-based approach (Poisson regression) was used to estimate these rates and the corresponding 95% confidence intervals, so weights could be incorporated into the calculations to account for differences in exposure times. Unadjusted rates were estimated separately by ESRD treatment modality, age group, and cohort year.
To study patterns in 1-year mortality rates, we first considered unadjusted rates by ESRD treatment group, by age group, and over time, and we used the corresponding 95% confidence intervals to check for differences. Next, we tested for differences in the unadjusted rates between independent cohort groups. The annual cohorts were not independent by design, but by comparing 1995 vs. 2010, hemodialysis vs. peritoneal dialysis vs. transplant (one year at a time), and younger vs. older (one year at a time), we could test for significant differences in mortality rates between independent cohorts using a Poisson regression model.
Lastly, we modeled the adjusted odds of mortality using generalized estimating equations to fit a logistic regression model that included adjustment variables for all listed patient and clinical characteristics and cohort year (see Table 3 for a complete list of model covariates), and adjusted for patients in multiple cohort years by including a repeated effect with an exchangeable correlation structure. All analyses were performed using SAS version 9.1 (SAS Institute). All logistic regression models were fit using SAS PROC GENMOD and included an offset variable for patient follow-up time. Results were considered significant at the 0.05 level.
Table 3.
Adjusted Odds of Mortality During Follow-Up for Hemodialysis and Peritoneal Dialysis Cohorts Combined and Transplant Cohorts
| Covariate | Reference | Dialysis | Transplant | ||
|---|---|---|---|---|---|
|
| |||||
| Odds Estimate (95% CI) | P | Odds Estimate (95% CI) | P | ||
| Age group, yrs. | 15–18 | ||||
| 0–4 | 4.71 (3.7–5.99) | < 0.0001 | 1.78 (1.06–3) | 0.030 | |
| 5–9 | 1.89 (1.44–2.5) | < 0.0001 | 0.66 (0.38–1.16) | 0.152 | |
| 10–14 | 1.18 (0.94–1.49) | 0.154 | 0.52 (0.31–0.86) | 0.011 | |
| Male | Female | 0.77 (0.65–0.91) | 0.002 | 0.8 (0.55–1.17) | 0.253 |
| Race Group | White | ||||
| Black | 0.98 (0.81–1.18) | 0.817 | 0.94 (0.58–1.52) | 0.786 | |
| Other | 1.1 (0.79–1.54) | 0.566 | 1.06 (0.46–2.45) | 0.883 | |
| Primary cause of ESRD | Congenital/reflux/ obstructive | ||||
| Glomerulonephritis | 0.53 (0.42–0.67) | < 0.0001 | 0.94 (0.6–1.48) | 0.790 | |
| Other | 1.22 (0.94–1.57) | 0.133 | 1.03 (0.55–1.91) | 0.937 | |
| Unknown/missing | 0.69 (0.47–1.03) | 0.069 | 0.97 (0.42–2.25) | 0.940 | |
| Dialysis type | Hemodialysis | ||||
| Peritoneal | 0.65 (0.54–0.78) | < 0.0001 | NA | NA | |
| ESRD status | Prevalent | ||||
| Incident | 0.73 (0.58–0.92) | 0.009 | 0.99 (0.24–4.03) | 0.984 | |
| Prior transplant | No | ||||
| Yes | 0.8 (0.64–1.01) | 0.057 | NA | NA | |
| Comorbid conditions | None | ||||
| ≥ 1 | 1.47 (1.22–1.76) | < 0.0001 | 1.18 (0.75–1.84) | 0.475 | |
| Missing | 0.86 (0.42–1.79) | 0.696 | 2.37 (0.97–5.8) | 0.593 | |
| Cohort year | 1995 | ||||
| 1996 | 1.01 (0.66–1.53) | 0.992 | 1.91 (0.65–5.6) | 0.241 | |
| 1997 | 0.88 (0.57–1.36) | 0.569 | 2.33 (0.83–6.57) | 0.109 | |
| 1998 | 0.78 (0.5–1.23) | 0.285 | 2.12 (0.73–6.12) | 0.167 | |
| 1999 | 1.08 (0.71–1.64) | 0.728 | 2.08 (0.71–6.12) | 0.185 | |
| 2000 | 0.68 (0.43–1.09) | 0.113 | 1.24 (0.38–4.09) | 0.725 | |
| 2001 | 0.67 (0.42–1.07) | 0.095 | 1.74 (0.56–5.35) | 0.336 | |
| 2002 | 0.58 (0.36–0.94) | 0.026 | 2.62 (0.9–7.59) | 0.077 | |
| 2003 | 1.05 (0.69–1.59) | 0.825 | 1.85 (0.6–5.71) | 0.285 | |
| 2004 | 0.52 (0.32–0.84) | 0.008 | 1.5 (0.47–4.78) | 0.493 | |
| 2005 | 0.58 (0.36–0.92) | 0.022 | 1.38 (0.43–4.38) | 0.589 | |
| 2006 | 0.72 (0.46–1.13) | 0.150 | 0.56 (0.13–2.35) | 0.427 | |
| 2007 | 0.58 (0.36–0.93) | 0.025 | 0.73 (0.19–2.76) | 0.644 | |
| 2008 | 0.54 (0.33–0.88) | 0.013 | 0.38 (0.07–1.96) | 0.247 | |
| 2009 | 0.46 (0.28–0.75) | 0.002 | 0.41 (0.08–2.14) | 0.290 | |
| 2010 | 0.43 (0.26–0.71) | 0.001 | 1.43 (0.45–4.6) | 0.545 | |
CI, confidence interval; ESRD, end-stage renal disease.
Results
Patient Characteristics
Yearly cohorts included averages of approximately 1200 maintenance dialysis patients (approximately 60% hemodialysis, 40% peritoneal dialysis; 25% incident) and 1100 transplant recipients (3.5% incident). Numbers of annual cohort patients and demographic distributions did not change dramatically over time. Hemodialysis patients differed from peritoneal dialysis patients (Table 1); they were older (average age 14.2 vs. 10.4 years) and less likely to be white (54% vs. 67%), with lower incidence of congenital/reflux/obstructive causes as primary cause of ESRD (50% vs. 58%). About 26% of hemodialysis and 17% of peritoneal dialysis patients had undergone prior kidney transplant, and a little over one-third of all dialysis patients were waitlisted for transplant. Most patients had no comorbidity, but incidence of comorbidity was higher in hemodialysis than in peritoneal dialysis or transplant patients. Transplant recipients differed from dialysis patients (Table 1); they were more likely to be white (74%) and older (10% aged 0–4 years vs. 23% of peritoneal dialysis patients), with less comorbidity (73% had none).
Table 1.
Patient Characteristics by End-Stage Renal Disease Treatment Type, All Years
| Characteristics | Treatment Type | P | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| HD | PD | Transplant | All Groups | HD vs. PD | Dialysis vs. Transplant | |
| Average annual cohort (n) | 670 | 525 | 1100 | |||
| Age group, yrs. (%) | < 0.0001 | < 0.0001 | < 0.0001 | |||
| 0–4 | 5.26 | 22.68 | 9.52 | |||
| 5–9 | 8.20 | 15.79 | 17.48 | |||
| 10–14 | 24.55 | 29.12 | 29.65 | |||
| 15–18 | 61.99 | 32.41 | 43.35 | |||
| Female (%) | 46.28 | 46.00 | 41.75 | < 0.0001 | 0.701 | < 0.0001 |
| Race (%) | < 0.0001 | < 0.0001 | < 0.0001 | |||
| White | 53.72 | 67.36 | 73.68 | |||
| Black | 39.77 | 26.14 | 20.98 | |||
| Other | 6.52 | 6.50 | 5.35 | |||
| Primary cause of ESRD (%) | < 0.0001 | < 0.0001 | < 0.0001 | |||
| Glomerulonephritis | 32.67 | 28.72 | 26.67 | |||
| Congenital/reflux/obstructive | 50.24 | 57.71 | 58.14 | |||
| Other | 9.71 | 7.40 | 9.40 | |||
| Unknown/missing | 7.37 | 6.16 | 5.79 | |||
| Incident (%) | 26.69 | 22.72 | 3.43 | < 0.0001 | < 0.0001 | < 0.0001 |
| Prior transplant (%) | 25.93 | 16.67 | NA | NA | < 0.0001 | NA |
| Wait-listed (%) | 37.09 | 33.82 | NA | NA | < 0.0001 | NA |
| Comorbidity (%) | < 0.0001 | < 0.0001 | < 0.0001 | |||
| None | 59.38 | 67.56 | 72.56 | |||
| ≥ 1 condition | 39.20 | 31.03 | 25.04 | |||
| Missing | 1.43 | 1.40 | 2.39 | |||
| Cause of death* (%) | 0.0013 | 0.121 | 0.0008 | |||
| Cardiovascular | 33.63 | 32.18 | 14.04 | |||
| Infection | 19.22 | 24.52 | 26.32 | |||
| Malignancy | 5.11 | 1.53 | 7.89 | |||
| Missing | 11.71 | 11.88 | 15.79 | |||
| Other | 30.33 | 29.89 | 35.96 | |||
During follow-up.
ESRD, end-stage renal disease; HD, hemodialysis; NA, not applicable; PD, peritoneal dialysis.
Cause of Death
Cause of death was missing for 12% of maintenance dialysis patients and 16% of transplant recipients. To create sufficient sample size to study the trend over time, causes of death were grouped into the categories listed in Table 1. Causes included in these categories are listed in Table S1. Cardiovascular disease (average 33%) was the most common cause of death among dialysis patients and infection (26%) among transplant recipients (Table 1). We found no change in the common causes over time, by groups of years, for any renal replacement therapy modality.
Trends in One-Year Mortality Rates
Outcomes by patient characteristics are shown in Table 2 and were similar for hemodialysis, peritoneal dialysis, and transplant patients. Overall, unadjusted 1-year, model-based mortality rates per 100 patient-years were lower in transplant recipients (0.7) than in dialysis patients (4.4) (Table 2). Hemodialysis and peritoneal dialysis patient mortality rates per 100 patient-years were higher for ages 0–4 and 5–9 years than for other ages, for female than for male patients, for white (4.9) than for black (3.7) patients, for patients with congenital/reflux/obstructive causes of ESRD than for those with glomerulonephritis, and for patients not waitlisted than for those who were waitlisted. Hemodialysis patient unadjusted 1-year mortality rates were higher for white than for black patients and for patients with 1 or more comorbid conditions than for those with none, but were not associated with prior kidney transplant. Peritoneal dialysis patient mortality rates did not differ notably by race or comorbidity status. Transplant recipient mortality rates were higher for ages 0–4 and 15–18 years but did not differ notably by primary cause of ESRD or comorbidity status.
Table 2.
Unadjusted 1-Year Mortality Rates by End-Stage Renal Disease Treatment Group and Patient Characteristics, All Years
| Hemodialysis | Peritoneal Dialysis | Transplant | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Deaths | Patient-Years | Rate per 100 Patient-Years | Deaths | Patient-Years | Rate per 100 Patient-Years | Deaths | Patient-Years | Rate per 100 Patient-Years | |
| Overall | 333 | 7719 | 4.31 | 261 | 5776 | 4.52 | 114 | 16,767 | 0.68 |
| Age group, yrs. | |||||||||
| 0–4 | 71 | 299 | 23.78 | 109 | 1209 | 9.02 | * | * | 1.30 |
| 5–9 | 41 | 561 | 7.31 | 35 | 887 | 3.94 | 16 | 2971 | 0.54 |
| 10–14 | 70 | 1834 | 3.82 | 51 | 1704 | 2.99 | 21 | 4987 | 0.42 |
| 15–18 | 151 | 5026 | 3.00 | 66 | 1975 | 3.34 | 56 | 7200 | 0.78 |
| Sex | |||||||||
| Female | 164 | 3521 | 4.66 | 130 | 2662 | 4.88 | 52 | 6982 | 0.74 |
| Male | 169 | 4197 | 4.03 | 131 | 3114 | 4.21 | 62 | 9787 | 0.63 |
| Race | |||||||||
| White | 194 | 4001 | 4.85 | 172 | 3850 | 4.47 | 87 | 12,398 | 0.70 |
| Black | 119 | 3228 | 3.69 | 67 | 1532 | 4.37 | 21 | 3471 | 0.60 |
| Other | 20 | 489 | 4.09 | 22 | 394 | 5.58 | * | * | 0.67 |
| Primary cause of ESRD | |||||||||
| Glomerulonephritis | 57 | 2541 | 2.24 | 44 | 1700 | 2.59 | 29 | 4466 | 0.65 |
| Congenital/reflux/obstructive | 209 | 3910 | 5.35 | 176 | 3303 | 5.33 | 66 | 9753 | 0.68 |
| Other | 55 | 707 | 7.78 | 25 | 424 | 5.89 | 12 | 1583 | 0.76 |
| Unknown/missing | 12 | 560 | 2.14 | 16 | 349 | 4.59 | * | * | 0.72 |
| ESRD status | |||||||||
| Incident | 54 | 315 | 4.11 | 41 | 892 | 4.60 | * | * | 0.69 |
| Prevalent | 279 | 6404 | 4.36 | 220 | 4884 | 4.50 | 112 | 16,480 | 0.68 |
| Prior transplant | |||||||||
| No | 257 | 5256 | 4.89 | 228 | 4649 | 4.90 | NA | NA | NA |
| Yes | 76 | 2462 | 3.09 | 33 | 1126 | 2.93 | NA | NA | NA |
| Waitlisted | |||||||||
| No | 266 | 4829 | 5.51 | 209 | 3839 | 5.44 | NA | NA | NA |
| Yes | 67 | 2890 | 2.32 | 52 | 1937 | 2.68 | NA | NA | NA |
| Comorbidity | |||||||||
| None | 181 | 4735 | 3.82 | 169 | 3948 | 4.28 | 80 | 12,221 | 0.65 |
| ≥ 1 condition | 148 | 2,859 | 5.18 | 88 | 1,743 | 5.05 | 28 | 4,153 | 0.67 |
ESRD, end-stage renal disease; NA, not applicable.
Counts of fewer than 10 patients.
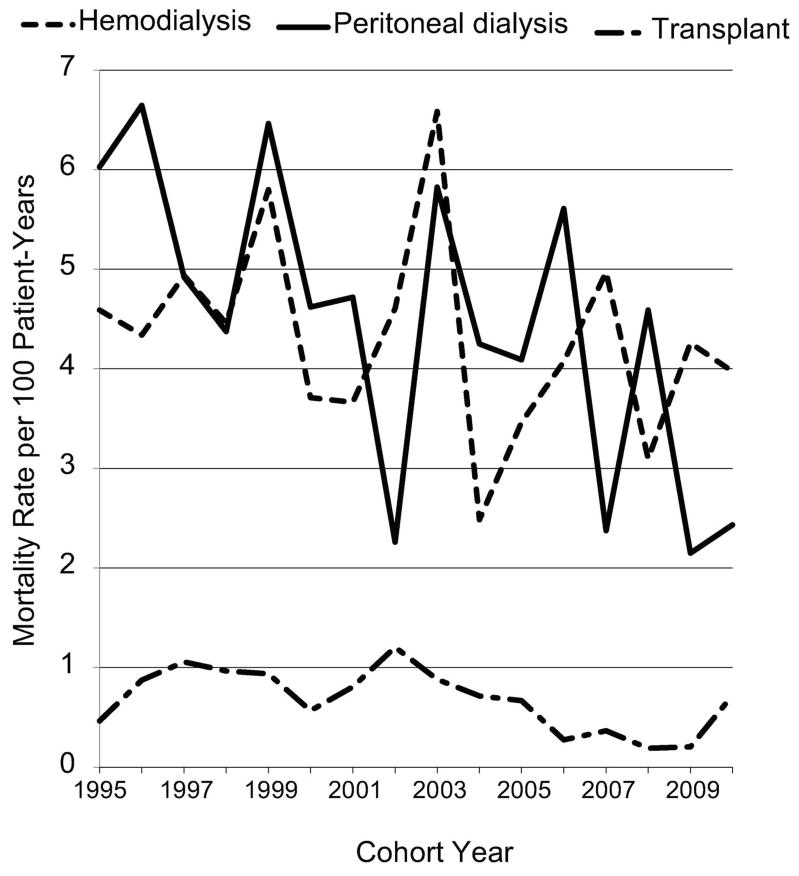
Trends in unadjusted 1-year mortality rates are shown in Figure 2 by treatment modality. Rates fluctuated from year to year in all groups. Unlike mortality rates for hemodialysis patients, rates for peritoneal dialysis patients showed evidence of a declining trend. Three of the four lowest mortality rate years (2002, 2007, 2009, 2010) were recent; rates per 100 patient-years decreased 60% from 1995 (6.03) to 2010 (2.43, P = 0.0263). For transplant recipients, mortality rates were significantly lower than for dialysis patients in all years, peaking at 1.2 per 100 patient-years in 2002 and 1.06 in 1997.
Figure 2.
Unadjusted 1-year mortality rates over time, by end-stage renal disease treatment group.
Adjusted Odds of Mortality
For maintenance dialysis patients, mortality risk was significantly increased for ages 0–4 vs. 15–18 years, for patients with congenital/reflux/obstructive causes of ESRD vs. glomerulonephritis, for hemodialysis patients, for prevalent patients, and for patients with one or more comorbid condition vs. those with none (Table 3). Mortality risk was significantly lower for years 2002, 2004, 2005, and 2007–2010 compared with 1995. For transplant recipients, the only significant variations in the odds of mortality occurred by age; odds were higher for ages 0–4 years and lower for ages 10–14 years, compared with ages 15–18 years.
Discussion
We studied mortality rates among cohorts of pediatric maintenance dialysis patients and kidney transplant recipients in each year from 1995 through 2010. An important finding is that 1-year mortality rates for pediatric dialysis patients have not consistently declined over time, though we did observe evidence of a modest decline for peritoneal dialysis patients. Average annual mortality rates for hemodialysis and peritoneal dialysis patients were almost identical at about 4.3 per 100 patient-years (over all 15 years studied), and were consistently about 6 times higher than average rates for transplant recipients. Using a model for the adjusted odds of mortality, we found that odds of yearly survival were better for older patients, male patients, and patients with glomerulonephritis as primary cause of ESRD compared with congenital/reflux/obstructive causes. We also found that race had no effect on odds of survival within the cohort year.
This study provides important updates and new insights compared with prior studies evaluating mortality rates in pediatric ESRD populations. Ferris et al [2] similarly used USRDS data from 1978 through 2002 to evaluate survival trends in incident adolescent (aged 12–19 years) patients with ESRD, and found improved survival for kidney transplant vs. maintenance dialysis patients. Our study extends the analysis to younger patients, incident and prevalent patients, and mortality risk by dialysis modality. Our study design differs from the design of a study by Mitsnefes et al [4] of mortality risk for children treated with dialysis. That study grouped incident patients aged younger than 21 years who started dialysis between 1990 and 2010 into 5-year calendar increments. All patients were followed until December 2010 unless censored by transplant or death. Patients in the 1990–1994 cohort were followed more than twice as long as patients in the 2005–2010 cohort. In contrast, we studied 1-year mortality rates using annual point prevalent cohorts of patients aged younger than 19 years with up to 1 year of follow-up for each cohort. In addition, Mitsnefes et al [4] excluded a sizable proportion of maintenance dialysis patients who had undergone prior transplant, and we included these patients.
We observed that the mortality rate was higher for peritoneal dialysis patients than for hemodialysis patients during the earlier years analyzed and lower in the later years, hence the evidence of decline in mortality rates for peritoneal dialysis patients while rates for hemodialysis patients remained constant. Among patients aged younger than 10 years, mortality rates were lower for peritoneal dialysis than for hemodialysis patients, but this difference was not apparent among patients aged 15–18 years. This is consistent with findings from Mitsnefes et al [4], who demonstrated decreased mortality risk in peritoneal dialysis vs. hemodialysis patients aged younger than 5 years, but not in children aged older than 5 years.
Patterns in mortality rates differed for hemodialysis and peritoneal dialysis patients, but an explanation was not apparent from the covariates we studied. Although hemodialysis patients were older, overall odds of mortality were highest for younger patients. Glomerulonephritis was the leading cause of ESRD for hemodialysis patients, and was associated with lower odds of 1-year mortality. Although we observed a significant difference in the racial distribution of hemodialysis and peritoneal dialysis patients, we did not find race to be a significant risk factor for mortality. Possibly, overall health differs by treatment modality, and only the healthiest ESRD patients were started on peritoneal dialysis in recent years.
Despite our findings that death rates remained constant (hemodialysis) or slightly decreased (peritoneal dialysis), mortality rates for pediatric dialysis patients remain extremely high. We found that mortality rates for pediatric dialysis patients were significantly higher than rates for pediatric transplant recipients in all years studied (average rates, 4.4 per 100 patient-years for dialysis patients, 0.7 for transplant recipients). The most recent National Vital Statistics Report [6] provides death rates per 100,000 patient-years for the general pediatric population in 2009; rates were 26.1, 12.2, 15.7, and 53.5 per 100,000 patient-years for ages 1–4, 5–9, 10–14, and 15–19 years, respectively. Extrapolating mortality rates from our 2009 data to the same scale gives rates of 3394 per 100,000 patient-years for pediatric (aged 0–18 years) maintenance dialysis patients and 203 per 100,000 patient-years for pediatric (aged 0–19) transplant recipients. Clearly, mortality rates for pediatric ESRD patients are much higher than for the general pediatric population, and the population is growing (a 7.8% overall increase in pediatric ESRD patients) [1]. Of concern, 1-year mortality rates remained largely unchanged for the past 15 years in children undergoing maintenance hemodialysis despite technical advances in pediatric dialysis therapy over that time [7]. Kidney transplant is associated with marked reduction in mortality risk and with improved growth, neurodevelopment, and quality of life [2;3;8–10]. One strategy to reduce mortality in pediatric dialysis patients is earlier transplant.
Another previous study found a cardiac death rate in children with ESRD 1000 times that in the general population [11]. In our study, cardiovascular disease was the most common cause of death for dialysis patients and the second most common cause for transplant recipients. We demonstrated that cardiovascular mortality rates remained unchanged over the past 15 years. Significantly increased cardiovascular disease risk in the pediatric ESRD population compared with the general pediatric population is well known [12]. However, at-risk children do not appear to be receiving the cardiovascular disease care that they require. Our recent study of pediatric maintenance hemodialysis patients demonstrated that only one-third had received an echocardiogram, the gold standard for diagnosis of cardiac disease [13]. Another recent study evaluated cardiovascular risk assessment in pediatric chronic kidney disease, dialysis, and kidney transplant patients at the time of transition to adult nephrology care [14]. Only 58% of cardiovascular risk factor assessments were documented, including echocardiogram, smoking assessment, family history of cardiovascular disease, lipid profile, and physical activity assessment.
This study’s limitations are as follows: First, generalizability is limited to pediatric patients with Medicare as primary payer. This requirement had the greatest impact on the number of available transplant patients since many pediatric transplant patients are not fully covered by Medicare and lose Medicare eligibility after 3 years. Second, as this was an observational study using Medicare claims data, all information was limited to claims and no observed relationships can be considered causal. Third, the factors used to assign treatment modality were not available for this study and are likely non-random. Children who could undergo preemptive transplant were able to avoid a period of dialysis. Selection of dialysis modality for potentially sicker or high-risk patients was likely individualized to fit the needs of the patient and family. Maintenance peritoneal dialysis is the modality most commonly prescribed for infants and small children [15]. Fourth, as we chose to consider incident and prevalent patients together to increase patient counts, we could not draw conclusions about differences between these groups. The number of incident patients (and number of deaths within that group) was small enough that (1) these patients could not be analyzed separately and (2) the combined rates (incident and prevalent together) were very similar to rates for prevalent patients alone. Combining incident and prevalent patients also produced annual cohorts that were not independent, since patients who met inclusion requirements for multiple years were in multiple cohorts. However, these period prevalent cohorts are still useful for understanding the current state of pediatric ESRD mortality. Our results describe the annual 1-year mortality rates for all available patients, in each year. Fifth, our study cohort included only patients with both Part A and Part B Medicare coverage. All patients had Part A coverage. The effect of lack of Part B coverage on mortality in pediatric ESRD patients is unknown.
In conclusion, we found that 1-year mortality rates among pediatric dialysis patients have not changed dramatically over the past 15 years; rates for hemodialysis patients remained relatively constant and rates for peritoneal dialysis patients showed evidence of a slight decline. However, 1-year mortality rates were significantly higher for pediatric maintenance dialysis patients than for pediatric kidney transplant recipients, and 1-year mortality rates for all pediatric ESRD patients were much higher than for the general pediatric population. Further improvement in dialysis procedures, early transplant, and cardiovascular disease evaluation, prevention and treatment are needed for this population.
Supplementary Material
Acknowledgments
This study was performed under Contract No. HHSN267200715002C (National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland). The data reported have been supplied by the United States Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government. The authors thank Chronic Disease Research Group colleagues Beth Forrest for regulatory assistance, Delaney Berrini, BS, for manuscript preparation and submission assistance, and Nan Booth, MSW, MPH, ELS, for manuscript editing.
Footnotes
The authors have no conflicts of interest with the study’s subject matter.
Reference List
- 1.U.S. Renal Data System. USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States. 2012. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2012. [Google Scholar]
- 2.Ferris ME, Gipson DS, Kimmel PL, Eggers PW. Trends in treatment and outcomes of survival of adolescents initiating end-stage renal disease care in the United States of America. Pediatr Nephrol. 2006;21:1020–1026. doi: 10.1007/s00467-006-0059-9. [DOI] [PubMed] [Google Scholar]
- 3.McDonald SP, Craig JC. Long-term survival of children with end-stage renal disease. N Engl J Med. 2004;350:2654–2662. doi: 10.1056/NEJMoa031643. [DOI] [PubMed] [Google Scholar]
- 4.Mitsnefes MM, Laskin BL, Dahhou M, Zhang X, Foster BJ. Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990–2010. JAMA. 2013;309:1921–1929. doi: 10.1001/jama.2013.4208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins AJ, Foley RN, Gilbertson DT, Chen SC. The state of chronic kidney disease, ESRD, and morbidity and mortality in the first year of dialysis. Clin J Am Soc Nephrol. 2009;4(Suppl 1):S5–S11. doi: 10.2215/CJN.05980809. [DOI] [PubMed] [Google Scholar]
- 6.National Vital Statistics Report. [Accessed September 12, 2014];Deaths: Leading Causes for 2009. 61(7) Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_07.pdf. [PubMed] [Google Scholar]
- 7.Sebestyen JF, Warady BA. Advances in pediatric renal replacement therapy. Adv Chronic Kidney Dis. 2011;18:376–383. doi: 10.1053/j.ackd.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Fine RN, Martz K, Stablein D. What have 20 years of data from the North American Pediatric Renal Transplant Cooperative Study taught us about growth following renal transplantation in infants, children, and adolescents with end-stage renal disease? Pediatr Nephrol. 2010;25:739–746. doi: 10.1007/s00467-009-1387-3. [DOI] [PubMed] [Google Scholar]
- 9.Davis ID, Chang PN, Nevins TE. Successful renal transplantation accelerates development in young uremic children. Pediatrics. 1990;86:594–600. [PubMed] [Google Scholar]
- 10.Goldstein SL, Rosburg NM, Warady BA, Seikaly M, McDonald R, Limbers C, Varni JW. Pediatric end-stage renal disease health-related quality of life differs by modality: a PedsQL ESRD analysis. Pediatr Nephrol. 2009;24:1553–1560. doi: 10.1007/s00467-009-1174-1. [DOI] [PubMed] [Google Scholar]
- 11.Parekh RS, Carroll CE, Wolfe RA, Port FK. Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr. 2002;141:191–197. doi: 10.1067/mpd.2002.125910. [DOI] [PubMed] [Google Scholar]
- 12.Chavers BM, Li S, Collins AJ, Herzog CA. Cardiovascular disease in pediatric chronic dialysis patients. Kidney Int. 2002;62:648–653. doi: 10.1046/j.1523-1755.2002.00472.x. [DOI] [PubMed] [Google Scholar]
- 13.Chavers BM, Solid CA, Sinaiko A, Daniels FX, Chen SC, Collins AJ, Frankenfield DL, Herzog CA. Diagnosis of cardiac disease in pediatric end-stage renal disease. Nephrol Dial Transplant. 2011;26:1640–1645. doi: 10.1093/ndt/gfq591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hooper DK, Williams JC, Carle AC, Amaral S, Chand DH, Ferris ME, Patel HP, Licht C, Barletta GM, Zitterman V, Mitsnefes M, Patel UD. The quality of cardiovascular disease care for adolescents with kidney disease: a Midwest Pediatric Nephrology Consortium study. Pediatr Nephrol. 2013;28:939–949. doi: 10.1007/s00467-013-2419-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Warady BA, Neu AM, Schaefer F. Optimal care of the infant, child, and adolescent on dialysis: 2014 update. Am J Kidney Dis. 2014;64:128–142. doi: 10.1053/j.ajkd.2014.01.430. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.