ABSTRACT
Purpose: To determine whether aquatic therapy in combination with land-based therapy improves patient outcomes after hip or knee arthroplasty compared with land-based therapy alone. Methods: For this systematic review, six online databases (MEDLINE, CINAHL, AMED, EMBASE, Cochrane, and PEDro) were searched from the earliest date available until September 2013. Controlled trials published in English in a peer-reviewed journal that compared aquatic therapy in combination with land-based therapy with land-based therapy alone were included; trial quality was assessed using the PEDro scale. Data were presented as standardized mean differences (SMDs), their associated 95% CIs, and meta-analyses. Results: Three small trials of moderate quality were included in the qualitative analysis. Meta-analysis of two of these studies found moderate-quality evidence that aquatic therapy in combination with land-based therapy improves functional outcomes (SMD=0.53; 95% CI, 0.03–1.03), knee range of motion (measured in knee or hip arthroplasty; SMD=0.78; 95% CI, 0.27–1.29), and edema (SMD=−0.66; 95% CI, −1.16 to −0.15) compared with land-based therapy alone. The results for improved functional outcomes were not considered clinically significant. Conclusions: It is not possible to draw confident conclusions from this review because of the small number of studies of limited quality and the modest differences found. Further studies of sound methodological quality are required to confirm the results. Economic analysis alongside randomized controlled trials is needed to examine the cost-effectiveness of these clinical outcomes.
Key Words: arthroplasty, replacement, hip; arthroplasty, replacement, knee; hydrotherapy; rehabilitation; systematic review
RÉSUMÉ
Objet: Déterminer si l'aquathérapie combinée à un traitement hors de l'eau améliore les résultats pour le patient après une arthroplastie de la hanche ou du genou par opposition à un traitement sans aquathérapie. Méthodes: Pour cet examen systématique, la recherche a été effectuée dans six bases de données en ligne (MEDLINE, CINAHL, AMED, EMBASE, Cochrane, et PEDro) à partir de la date accessible la plus éloignée jusqu'à septembre 2013. Des essais contrôlés publiés en anglais dans une revue à comité de lecture et comparant l'aquathérapie combinée à un traitement hors de l'eau au traitement sans aquathérapie ont été inclus dans l'examen; la qualité des essais a été évaluée au moyen de l'échelle PEDro. Les données ont été présentées sous forme de différences moyennes normalisées (DMN), d'intervalles de confiance (IC) connexes de 95% et de méta-analyses. Résultats: Trois petits essais de qualité modérée faisaient partie de l'analyse qualitative. La méta-analyse de deux de ces études a permis de trouver des preuves de qualité modérée que l'aquathérapie combinée à un traitement hors de l'eau améliore les résultats fonctionnels (DMN=0,53; selon un IC de 95%, 0,03–1,03), l'amplitude des mouvements du genou (mesurée dans l'arthroplastie du genou ou de la hanche) (DMN=0,78; selon un IC de 95%, 0,27–1,29), et l'œdème (DMN =−0,66; selon un IC de 95%, −1,16–−0,15) comparativement au traitement sans aquathérapie. Les données des résultats fonctionnels améliorés n'ont pas été considérées comme cliniquement significatives. Conclusions: Il n'est pas possible de tirer des conclusions fiables de cet examen en raison du petit nombre d'études de qualité limitée et des modestes différences constatées. Il faudra effectuer d'autres études de bonne qualité méthodologique pour confirmer les résultats. Parallèlement aux essais contrôlés randomisés, il faut effectuer une analyse économique pour examiner la rentabilité de ces résultats cliniques.
Mots clés : arthroplastie, remplacement, genou; arthroplastie, remplacement, hanche; hydrothérapie; réadaptation
The financial and societal burden of hip and knee arthroplasty is significant. In Canada, 47,137 hospitalisations for hip arthroplasties and 57,718 hospitalisations for knee arthroplasties occurred in the 2012–2013 fiscal year,1 representing a 16.5% increase in hip arthroplasties and a 21.5% increase in knee arthroplasties compared with the preceding 5 years. In the United States, rates of hip and knee arthroplasty have similarly risen,2 and both are expected to greatly increase by 2030 (hip arthroplasties by 174%, to 520,000 procedures, and knee arthroplasties by 673%, to 3.42 million procedures).3 Rising rates of joint-replacement surgery have resulted in increased pressure to reduce hospital length of stay and contain costs in primary health care.4
Both aquatic and land-based therapies are commonly prescribed after joint-replacement surgery.5–7 As part of rehabilitation, physiotherapists implement aquatic therapy both individually (one-on-one with a therapist) and in groups.8 Exercising in a hydrotherapy pool may enable patients to perform exercises that they would be unable to perform on land by using the hydrodynamic and hydrostatic properties of the water.9 The benefits of aquatic therapy include reduction in pain and muscle spasm through warmth, resistance to movement through turbulence and hydrostatic pressure, decreased loading of joints through buoyancy, and reduction in edema through pressure from immersion.10,11 Ideally, aquatic therapy incorporates individual assessment and clinical reasoning to formulate a treatment program appropriate to the client.8
Aquatic therapy is often combined with land-based gait education, exercise, and practice of functional tasks for patients with hip or knee arthroplasty.12 Early intensive rehabilitation with land-based therapy is associated with faster attainment of functional milestones after hip or knee arthroplasty than later rehabilitation and has become standard practice.7,13–16 A recent survey of aquatic therapy practices by the Australian Physiotherapy Association found that aquatic therapy is most commonly used in combination with land-based therapy rather than as a stand-alone treatment.17 In addition, several studies have tried to replicate clinical practice by looking at the effects of combining aquatic therapy with land-based therapy.18–24 A recent systematic review examining the effectiveness of aquatic therapy after upper and lower limb orthopaedic surgery25 reported that it was as effective as land-based therapy in reducing pain and edema and improving strength and range of motion (ROM). Studies comparing aquatic therapy with land-based therapy after hip or knee arthroplasty have demonstrated significant improvements in outcomes from both types of therapy,26,27 but whether adding aquatic therapy to land-based therapy results in even better patient outcomes is not known. This is an important clinical question, given the additional costs associated with providing aquatic therapy.
Our primary aim in this review, therefore, was to investigate the effectiveness of aquatic therapy in combination with land-based therapy compared with land-based therapy only. Our specific objectives were to investigate whether aquatic therapy in combination with land-based therapy resulted in more reduction in impairment, activity limitations, and participation restrictions in patients after hip or knee replacement relative to land-based therapy alone.
Method
This review was prepared and reported with reference to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.28 The PRISMA guidelines encourage reviewers to report fully and transparently on how a review was planned and conducted and what its findings were. With this information, readers can clearly assess the strengths and weaknesses of a review and determine the usefulness and clinical applicability of findings.28
Search strategy
We searched the MEDLINE, CINAHL, AMED, EMBASE, Cochrane, and PEDro databases from the earliest date available through September 2013, using search terms based on the two concepts of aquatic therapy and hip or knee arthroplasty (see Appendix 1). In addition to our database searches, we tracked citations of the included articles using Google Scholar and manually searched the reference lists of the included articles.
We imported the yields from the database searches into bibliographic software (EndNote, version X7, Thompson Reuters, Philadelphia, PA). Two reviewers independently screened each item by title and abstract, using predetermined criteria; any disagreements were resolved by discussion until a consensus was reached, and we calculated agreement between reviewers as to which trials fulfilled the selection criteria using a kappa coefficient. When we could not include or exclude an article on the basis of its title and abstract, we retrieved a full-text copy and reapplied the selection criteria.
Eligibility criteria
Studies were eligible for inclusion if they met the following criteria: (1) Participants had undergone any type of hip or knee arthroplasty; (2) participants were age 18 years or older; (3) the study evaluated aquatic therapy in combination with land-based therapy; (4) the comparison group completed land-based therapy alone; (5) the study design was a controlled trial; and (6) the article was published in English. For the purposes of this review, aquatic therapy refers to any water-based therapy, including stretching, strengthening, ROM, and aerobic exercise.10 Studies were excluded if aquatic therapy as a treatment modality was compared with a non-treatment group or if aquatic therapy alone was compared with land-based therapy alone.
Data extraction
We developed a data extraction form that we used to extract data on the study participants (e.g., age, details of surgery), interventions (e.g., type, duration, frequency of intervention, when treatment began), trial setting (e.g., in-patient, outpatient), outcome measures (e.g., impairments, activity limitations, participation restrictions), and results.
We obtained full-text copies for all the included studies. Data extraction was completed by one reviewer and checked for accuracy by a second reviewer. In the case of any discrepancies, we referred back to the published article.
Quality assessment of trials and risk of bias
Two researchers independently applied the PEDro scale to rate the methodological quality of the included trials. The PEDro scale is a validated quality assessment tool for randomized controlled trials (RCTs)29 that has demonstrated moderate interrater reliability (intraclass coefficient [ICC]=0.68; 95% CI, 0.57–0.76) for clinical trials.30 Eleven items are rated as either meeting or not meeting the criteria; a maximum score of 10 is possible because the first item (eligibility criteria) is not scored. The 11 items are eligibility criteria, random allocation, concealed allocation, baseline comparability, blinding of subjects, blinding of therapists, blinding of assessors, adequate follow-up, intention-to-treat analysis, between-group comparisons, and point estimates and variability. A trial with a score of 6 or more is considered to be of high quality.31 Use of the PEDro scale (or any other numerical scale) to indicate quality of clinical trials is considered to have some limitations for assessing risk of bias in published studies. Disagreement between the reviewers was resolved through discussion to reach a consensus.
Data syntheses
We calculated standardized mean differences (SMD) and 95% CIs from post-intervention means and standard deviations; when data were not available from the original study, we contacted the corresponding author. SMD values of less than 0.2 indicate a small effect size; values of 0.2–0.5, a moderate effect size; and values of more than 0.8, a large effect size.32 We also performed a descriptive analysis to describe the characteristics of the included studies.
Our meta-analysis used a random effects model and RevMan software (Version 5.0, Cochrane Collaboration, Copenhagen). We combined data in a meta-analysis in which a minimum of two trials were clinically homogeneous. Trials were considered clinically homogeneous with each other if a common population, intervention, and outcome measure was used. Statistical heterogeneity was assessed using the I2 statistic; values of less than 25% represent low levels of heterogeneity.33,34 We calculated weighted means according to participant numbers.
We examined the data from the meta-analyses for clinical significance by comparing the mean difference with data available from the literature on minimal clinically important difference (MCID). If no data on MCID were available, we substituted half the standard deviation of the control group at baseline, which is accepted as representing the MCID.35
We applied the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach36 to each meta-analysis to determine the quality of evidence across the included studies. This approach considers RCTs to be of high quality or at low risk of bias; the quality level is then downgraded to moderate, and again to low or very low, if limitations are present. In the case of our study, a one-level downgrade (e.g., from high to moderate quality) occurred when (1) the PEDro score was less than 6 for the majority of trials in the meta-analysis (a trial with a score ≥6 is considered to be of high quality31), (2) the level of statistical heterogeneity between the trials was above the low threshold (I2 ≥25%),20 or (3) the SMD had a large confidence interval (>0.8), indicating greater variability. The reasons for downgrading the evidence in each meta-analysis are provided below.
Results
Study selection
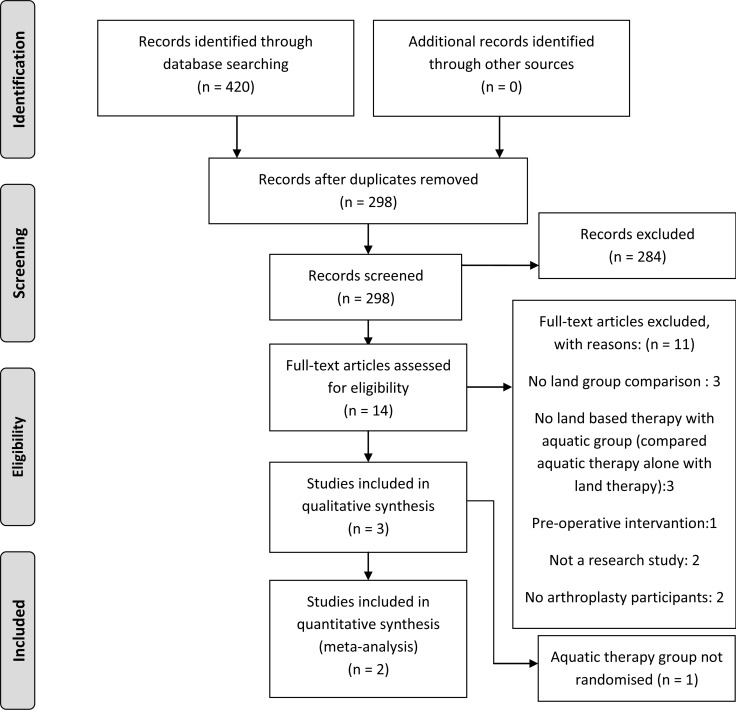
Our initial database search yielded 420 articles; reference scanning and citation tracking identified no additional articles. After removal of duplicates, we screened titles and abstracts for 298 studies. There was good agreement between reviewers (κ=0.84; 95% CI, 0.68–0.99) as to which trials did and did not fulfil selection criteria. We then retrieved full-text copies of 14 studies for further analysis. Evaluation of the full text of these 14 trials yielded a consensus to retain 3 trials13–15 for inclusion in the systematic review. Of these 3 trials, we included 213,15 in the meta-analysis; the 3rd was excluded because the aquatic therapy group was not allocated randomly14 (see Figure 1).
Figure 1.
Study selection process to identify eligible articles for inclusion in the review.
Quality of studies
All three trials included in our review were controlled trials; two13,15 were RCTs, and one14 was a controlled clinical trial. The three trials included a total of 113 participants, 63 with a total hip arthroplasty and 50 with a total knee arthroplasty. Participants' mean age was 66.5 years; 60% were women, and 48% received aquatic therapy in combination with land-based therapy (see Table 1).
Table 1.
Summary of Studies
| Aquatic:land |
|||||||
|---|---|---|---|---|---|---|---|
| Author (Date) | PEDro score |
Design | Setting | Arthroplasty type |
No. of respondents |
Sex, % male |
Mean age, y |
| McAvoy (2009)13 | 6 | RCT | Outpatient | TKA | 30 (15:15) | – | – |
| Stockton & Mengersen (2009)14 | 4 | Controlled trial | Acute inpatient | THA | 48 (21:27) | 48.0:48.0 | 65.5:62.8 |
| Rahmann, Brauer, & Nitz (2009)15 | 6 | RCT | Acute inpatient | THA:TKA (15:20) | 35 (18:17) | 56.0: 29.4 | 69.4:70.4 |
RCT=randomized controlled trial; TKA=total knee arthroplasty; THA=total hip arthroplasty.
The quality of the included trials was moderate; the mean PEDro score was 5.3 (range, 4–6) out of 10. None of the included studies was able to blind either participants or therapists to the intervention. All used intention-to-treat analysis. Two13,15 of the three studies used random allocation, concealed allocation, and blinded assessors and had adequate follow-up. There was good agreement between reviewers for individual items on the PEDro scale (κ=0.73; 95% CI, 0.48–0.98).
Aquatic therapy
In each of the included trials, the intervention group received aquatic therapy in combination with land-based therapy, and the comparison group received land-based therapy only. Two trials provided individual (one-on-one) aquatic therapy;14,15 the other provided group sessions.13 For participants receiving both aquatic and land-based therapy, two13,15 of the three trials reported using individualised programs that were different for the land-based and aquatic therapy sessions. These two studies described their aquatic therapy programs, including progression, in detail; both used equipment in the pool. The other trial14 reported that the aquatic therapy was similar to the land-based therapy apart from being performed in the water.
Two studies conducted daily aquatic programs from the 4th postoperative day until discharge in an inpatient setting.14,15 In these studies, patients were discharged between the 5th and 11th postoperative day. The other study13 involved a 30-minute aquatic session, twice per week for 6 weeks, in an outpatient setting. None of the studies found any difference in adherence rates between the aquatic group and the land-based group. Two studies progressed participants according to ability, muscle strength, and ROM as required;13,15 the other specified altering the water depth (from waist to chest deep, or 0.5 m to 1.6 m) to either challenge or assist the participant.15
Outcome measures
Impairment
The three included studies all measured impairment-based outcomes, including edema (two studies), pain (one study), ROM of the operated joint (two studies), and muscle strength (one study; see Table 2).
Table 2.
Summary of Intervention Characteristics
| Aquatic therapy |
Land-based therapy |
Outcome |
||||||
|---|---|---|---|---|---|---|---|---|
| Author | Frequency | Duration | Delivery | Frequency | Duration | Delivery | Impairment | Activity |
| McAvoy (2009)13 | 30 min, 2×/wk |
6 wk | Group | 60 min, 2×/wk |
6 wk | Group | Edema Knee AROM & PROM Pain |
KOOS |
| Stockton & Mengersen (2009)14 |
Daily | Postoperative day 4–discharge |
1:1 | Daily | Postoperative day 1–discharge |
1:1 | – | Iowa Level of Assistance |
| Mean LOS=7.9 (SD 1.6) d |
Mean LOS=8.1 (SD 2.6) d |
|||||||
| Rahmann, Brauer, & Nitz (2009)15 |
Daily | Postoperative day 4–discharge |
1:1 | Daily | Postoperative day 1–discharge |
1:1 | Edema Knee AROM Strength: quads, hams, hip abductors |
WOMAC 10MW TUG PSFS |
| Mean LOS=7.4 (SD 1.6) d |
Mean LOS=8.3 (SD 1.9) d |
|||||||
AROM=active range of motion; PROM=passive range of motion; KOOS=Knee Injury and Osteoarthritis Outcome Score; LOS=length of stay;
WOMAC=Western Ontario and McMaster Universities Arthritis Index; 10MW=10-metre walk test; TUG=timed up-and-go test;
PSFS=Patient Specific Functional Scale.
In two studies13,15 (N=64), aquatic therapy plus land-based therapy improved the ROM of the operated knee by a statistically significant amount relative to land-based therapy only (SMD=0.78; 95% CI, 0.27–1.29; I2=0%; see Figure 2). The quality of the evidence was rated as moderate using the GRADE approach; the quality was downgraded because large confidence intervals indicated greater variability (see Table 3). The overall mean difference in ROM for both studies combined was 10.6° for both hip and knee arthroplasty, which was considered clinically significant.35 Measurements for both studies were taken with a standard plastic goniometer; a study of reliability and validity of goniometric measurements by Gogia and colleagues37 found high inter-test reliability (r=0.98; ICC=0.99) and validity (rs=0.97–0.98; ICCs=0.98–0.99).
Figure 2.
Knee range of motion
Standardised mean difference (95% CI) for the effect of aquatic physical therapy on range of motion for hip and knee arthroplasty by pooling data from two trials (n=64).
IV=inverse variance; Std=standardised.
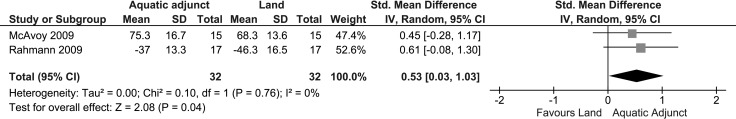
Table 3.
Quality Assessment of Meta-Analyses for Aquatic Therapy as an Adjunct versus Land-Based Therapy Alone
| Intervention | No. of trials |
No. of participants |
Outcome | SMD (95% CI), I2 | Quality of evidence (GRADE) |
|---|---|---|---|---|---|
| Activities of daily living | 213,15 | 64 | KOOS | 0.53 (0.03–1.03), 0% | Moderate* |
| Iowa Level of Assistance | |||||
| WOMAC | |||||
| ROM | 213,15 | 64 | ROM in degrees | 0.78 (0.27–1.29), 0% | Moderate* |
| Edema | 213,15 | 64 | Lower limb circumference measurement | 0.66 (0.15–1.16), 0% | Moderate* |
Reason for downgrade: large CI (>0.8).
SMD=standardized mean difference; GRADE=Grading of Recommendations Assessment, Development and Evaluation working group grades of evidence (see footnote); KOOS=Knee Injury and Osteoarthritis Outcome Score; WOMAC=Western Ontario and McMaster Universities Arthritis Index; ROM=range of motion.
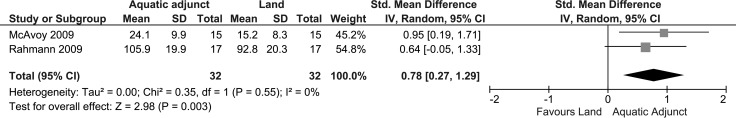
In two studies13,15 (N=64), aquatic therapy plus land-based therapy reduced edema in the operated limb by a significant amount relative to land-based therapy alone (SMD=0.66; 95% CI, 0.15–1.16; I2=0%; see Figure 3). The quality of the evidence is rated as moderate using the GRADE approach; the quality was downgraded because large CIs indicated greater variability (see Table 3). The overall mean difference in edema for both studies combined was 3.6 cm (circumference measurement), which was considered clinically significant.35
Figure 3.
Edema
Standardised mean difference (95% CI) for the effect of aquatic physical therapy on edema for hip and knee arthroplasty by pooling data from two trials (n=64).
IV=inverse variance; Std.=standardised.
One study15 of patients with hip or knee arthroplasty reported increased hip abduction strength in the aquatic therapy plus land-based therapy group (p=0.001), relative to land-based therapy alone, after 14 days. One study13 on knee arthroplasty found no significant difference in pain, as measured by the numerical pain rating scale, at 6 weeks post-treatment (p=0.68).
Activity
The three studies measured function in activities of daily living (ADLs) using patient-reported outcome measures (see Table 2). Other activity-based outcome measures used in one study15 were the 10-m walk and timed up-and-go test.
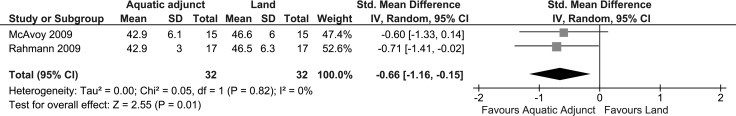
Two studies (N=64) found that compared with land-based therapy only, aquatic therapy plus land-based therapy improved ADL function by a small but significant amount (SMD=0.53; 95% CI, 0.03–1.03; I2=0%; see Figure 4). The quality of the evidence was rated as moderate using the GRADE approach; the quality was downgraded because large CIs indicated greater variability (see Table 3). The MCID for the Knee Injury and Osteoarthritis Outcome Score (KOOS)38,39 is 43 points with the sports subset of questions excluded; the mean difference in KOOS in one study13 was 51.1 for the intervention group, indicating a clinically significant change, and results for the other two studies did not appear to be clinically significant. The mean difference between intervention and comparison groups on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was 7.9, which was not considered clinically significant because the MCID for knee arthroplasty using the WOMAC is 15.40 No raw data were available to calculate the MCID of the Iowa Level of Assistance score. Overall, the difference in function was not clinically significant.
Figure 4.
Function with activities of daily living
Standardised mean difference (95% CI) for the effect of aquatic physical therapy on function for hip and knee arthroplasty by pooling data from two trials (n=64).
IV=inverse variance; Std=standardised.
Participation restrictions
One study13 measured quality of life, using the KOOS Quality of Life subscale, and found no difference between groups.
Discussion
The results of this systematic review provide moderate-quality evidence from two controlled trials that aquatic therapy in combination with land-based therapy improves function and ROM and results in more reduction in edema in adults with hip or knee replacement than land-based therapy alone. Our results complement the findings of Villalta and Peiris,25 who reported that after orthopaedic surgery, aquatic therapy improves function and is as effective as land-based therapy in terms of improving pain, edema, strength, and ROM outcomes.
The results from our meta-analyses can be considered clinically significant35 for ROM and swelling, but not for ADL function. Knee ROM has traditionally been one of the most important factors used to determine success after knee arthroplasty because many functional activities depend on it:41 Sit to stand and ascending and descending stairs requires 90°–120° of flexion, transferring in and out of a bath requires as much as 135°,42 and kneeling and squatting require about 140°–165°.43 The additional 10° in ROM for patients who received both land-based and aquatic therapy could make the difference between achieving important functional goals and not achieving them.
The overall mean difference in edema was 3.6 cm in circumference measurement at the knee. Pressure from immersion in a hydrotherapy pool combined with exercise is associated with a reduction in lower limb swelling.44 Reduction in edema is an additional benefit offered by aquatic exercise45 that is important for optimal recovery after orthopaedic surgery.46,47
More favourable results on key outcome measures (strength, ROM, and function) were obtained from the studies13,15 that described their aquatic therapy programs in detail and made use of the properties of the aquatic environment. The study14 that reported that the aquatic therapy was similar to the land-based therapy, meaning that the exercise was not adapted to the aquatic environment, did not show a statistically significant difference in function for the aquatic adjunct group. This may indicate that individualised aquatic exercises that make the most of the properties of the aquatic environment are important.8
Cost is an important factor to consider when making decisions about whether to deliver aquatic therapy in combination with land-based therapy. The cost of aquatic therapy, particularly one-to-one therapy, is high, and the additional gains in ROM, edema, and function achieved by patients may not offset the increased costs associated with aquatic therapy. The costs include those associated with setting up a hydrotherapy pool and maintaining the pool environment (or of renting a pool), as well as staffing costs. Two14,15 of the trials delivered aquatic therapy one-to-one, which is labour intensive and more costly. In these two trials, aquatic therapy was delivered beginning on postoperative day 4, which likely accounts for the use of one-to-one therapy. Although introducing aquatic therapy in the early postoperative period has been shown to be beneficial,16 one trade-off for early intervention is that a more labour-intensive model is needed. A cost–utility analysis of an 8-month aquatic training program in a community pool for women with fibromyalgia48 found that aquatic therapy added to the usual care for fibromyalgia is cost-effective in terms of both health care costs and societal costs; this suggests that a group aquatic program run in the community setting or in an existing pool may be more realistic. However, it is not yet clear whether the changes in ROM, edema, and function are significant enough to outweigh the increased cost of aquatic therapy compared with land-based therapy. To be certain about the outcome, an economic analysis alongside an RCT would be required.
Strengths and Limitations
A strength of this review is that it was prepared according to the PRISMA guidelines.28 Another strength is that we applied the GRADE approach36 to each meta-analysis to determine the quality of evidence across included studies.
This review also has several limitations. First, the search strategy was limited to studies published in English. Second, the systematic review and meta-analyses were small, with the meta-analyses including only two trials. We urge caution in the interpretation and recommendations based on such a small sample. Finally, the evidence on participation restrictions is limited because only one study13 used a quality-of-life outcome measure.
Conclusion
It is not possible to draw confident conclusions from this review because of the small number of included studies, limited quality of the evidence, and modest between-group differences. Further studies of good quality are required to confirm the results. The quality of the evidence was rated as moderate using the GRADE approach; the quality was downgraded because of large confidence intervals, indicating greater variability. Economic analyses alongside RCTs are needed to examine the cost-effectiveness of these clinical outcomes.
Key Messages
What is already known on this topic
Aquatic therapy and land-based therapy are used after orthopaedic surgery to improve function, pain, edema, muscle strength, and joint ROM.25
What this study adds
This systematic review and meta-analysis suggests that there is currently not enough evidence to support or refute the hypothesis that aquatic therapy in combination with land-based therapy provides a clinically meaningful advantage over land-based therapy alone for rehabilitation after hip or knee replacement. Further high-quality studies are required before a conclusion can be drawn on this topic.
Appendix 1: MEDLINE Search Terms
(MH “Arthroplasty, Replacement, Hip”) OR (MH “Arthroplasty, Replacement, Knee”)
TI Knee arthroplasty OR AB Knee arthroplasty
TI knee replacement OR AB knee replacement
TI knee prosthesis OR AB knee prosthesis
TI hip arthroplasty OR AB hip arthroplasty
TI hip replacement OR AB hip replacement
TI hip prosthesis OR AB hip prosthesis
(MH “Hydrotherapy+”)
(MH “Swimming+”)
TI Aquatic *therapy OR AB Aquatic *therapy
TI Aquatic exercis* OR AB Aquatic exercis*
TI water exercis* OR AB water exercis*
TI hydrotherapy OR AB hydrotherapy
S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7
S8 OR S9 OR S10 OR S11 OR S12 OR S13
S14 AND S15
Physiotherapy Canada 2015; 67(2);133–141; doi:10.3138/ptc.2014-01
References
- 1.Canadian Institute for Health Information. Hip and knee replacements in Canada: Canadian Joint Replacement Registry 2014 annual report. Toronto: Canadian Institute for Health Information; 2014. [Google Scholar]
- 2.Kurtz S, Mowat F, Ong K, et al. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487–97. doi: 10.2106/JBJS.D.02441. http://dx.doi.org/10.2106/JBJS.D.02441. Medline:15995115. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5. doi: 10.2106/JBJS.F.00222. http://dx.doi.org/10.2106/JBJS.F.00222. Medline:17403800. [DOI] [PubMed] [Google Scholar]
- 4.Rooks DS, Huang J, Bierbaum BE, et al. Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum. 2006;55(5):700–8. doi: 10.1002/art.22223. http://dx.doi.org/10.1002/art.22223. Medline:17013852. [DOI] [PubMed] [Google Scholar]
- 5.Kim S, Losina E, Solomon DH, et al. Effectiveness of clinical pathways for total knee and total hip arthroplasty: literature review. J Arthroplasty. 2003;18(1):69–74. doi: 10.1054/arth.2003.50030. http://dx.doi.org/10.1054/arth.2003.50030. Medline:12555186. [DOI] [PubMed] [Google Scholar]
- 6.Lingard EA, Berven S, Katz JN Kinemax Outcomes Group. Management and care of patients undergoing total knee arthroplasty: variations across different health care settings. Arthritis Care Res. 2000;13(3):129–36. http://dx.doi.org/10.1002/1529-0131(200006)13:3<129::AID-ANR1>3.0.CO;2-6. Medline:14635286. [PubMed] [Google Scholar]
- 7.Munin MC, Rudy TE, Glynn NW, et al. Early inpatient rehabilitation after elective hip and knee arthroplasty. JAMA. 1998;279(11):847–52. doi: 10.1001/jama.279.11.847. http://dx.doi.org/10.1001/jama.279.11.847. Medline:9515999. [DOI] [PubMed] [Google Scholar]
- 8.Larsen J, Pryce M, Harrison J, et al. Guidelines for physiotherapists working in and/or managing hydrotherapy pools. Camberwell (VIC): Australian Physiotherapy Association; 2002. [Google Scholar]
- 9.Campion MR. Hydrotherapy: principles and practice. Oxford: Butterworth-Heinemann; 2007. [Google Scholar]
- 10.Bartels EM, Lund H, Hagen KB, et al. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Db Syst Rev. 2007;(4) doi: 10.1002/14651858.CD005523.pub2. Medline:17943863. [DOI] [PubMed] [Google Scholar]
- 11.Batterham SI, Heywood S, Keating JL. Systematic review and meta-analysis comparing land and aquatic exercise for people with hip or knee arthritis on function, mobility and other health outcomes. BMC Musculoskelet Disord. 2011;12(1):123. doi: 10.1186/1471-2474-12-123. http://dx.doi.org/10.1186/1471-2474-12-123. Medline:21635746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naylor J, Harmer A, Fransen M, et al. Status of physiotherapy rehabilitation after total knee replacement in Australia. Physiother Res Int. 2006;11(1):35–47. doi: 10.1002/pri.40. http://dx.doi.org/10.1002/pri.40. Medline:16594314. [DOI] [PubMed] [Google Scholar]
- 13.McAvoy R. Research report: aquatic and land based therapy vs. land therapy on the outcome of total knee arthroplasty: a pilot randomized clinical trial. J Aquatic Phys Ther. 2009;17(1):8–15. [Google Scholar]
- 14.Stockton KA, Mengersen KA. Effect of multiple physiotherapy sessions on functional outcomes in the initial postoperative period after primary total hip replacement: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(10):1652–7. doi: 10.1016/j.apmr.2009.04.012. http://dx.doi.org/10.1016/j.apmr.2009.04.012. Medline:19801052. [DOI] [PubMed] [Google Scholar]
- 15.Rahmann AE, Brauer SG, Nitz JC. A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(5):745–55. doi: 10.1016/j.apmr.2008.12.011. http://dx.doi.org/10.1016/j.apmr.2008.12.011. Medline:19406293. [DOI] [PubMed] [Google Scholar]
- 16.Liebs TR, Herzberg W, Rüther W, et al. Multicenter Arthroplasty Aftercare Project. Multicenter randomized controlled trial comparing early versus late aquatic therapy after total hip or knee arthroplasty. Arch Phys Med Rehabil. 2012;93(2):192–9. doi: 10.1016/j.apmr.2011.09.011. http://dx.doi.org/10.1016/j.apmr.2011.09.011. Medline:22196125. [DOI] [PubMed] [Google Scholar]
- 17.Australian Physiotherapy Association. Australian Physiotherapy Association survey of aquatic physiotherapy practice. Camberwell (VIC): Australian Physiotherapy Association; forthcoming. [Google Scholar]
- 18.Brady B, Redfern J, MacDougal G, et al. The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: a feasibility study. Physiother Res Int. 2008;13(3):153–61. doi: 10.1002/pri.403. http://dx.doi.org/10.1002/pri.403. Medline:18548557. [DOI] [PubMed] [Google Scholar]
- 19.Hidding A, van der Linden S, Gielen X, et al. Continuation of group physical therapy is necessary in ankylosing spondylitis: results of a randomized controlled trial. Arthritis Care Res. 1994;7(2):90–6. doi: 10.1002/art.1790070208. http://dx.doi.org/10.1002/art.1790070208. Medline:7857999. [DOI] [PubMed] [Google Scholar]
- 20.Geytenbeek J. Evidence for effective hydrotherapy. Physiotherapy. 2002;88(9):514–29. http://dx.doi.org/10.1016/S0031-9406(05)60134-4. [Google Scholar]
- 21.Green J, McKenna F, Redfern EJ, et al. Home exercises are as effective as outpatient hydrotherapy for osteoarthritis of the hip. Br J Rheumatol. 1993;32(9):812–5. doi: 10.1093/rheumatology/32.9.812. http://dx.doi.org/10.1093/rheumatology/32.9.812. Medline:8369892. [DOI] [PubMed] [Google Scholar]
- 22.Mannerkorpi K, Nyberg B, Ahlmén M, et al. Pool exercise combined with an education program for patients with fibromyalgia syndrome: a prospective, randomized study. J Rheumatol. 2000;27(10):2473–81. Medline:11036846. [PubMed] [Google Scholar]
- 23.Peterson C. Exercise in 94°F water for a patient with multiple sclerosis. Phys Ther. 2001;81(4):1049–58. Medline:11276186. [PubMed] [Google Scholar]
- 24.Sherry DD, Wallace CA, Kelley C, et al. Short- and long-term outcomes of children with complex regional pain syndrome type I treated with exercise therapy. Clin J Pain. 1999;15(3):218–23. doi: 10.1097/00002508-199909000-00009. http://dx.doi.org/10.1097/00002508-199909000-00009. Medline:10524475. [DOI] [PubMed] [Google Scholar]
- 25.Villalta EM, Peiris CL. Early aquatic physical therapy improves function and does not increase risk of wound-related adverse events for adults after orthopedic surgery: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2013;94(1):138–48. doi: 10.1016/j.apmr.2012.07.020. http://dx.doi.org/10.1016/j.apmr.2012.07.020. Medline:22878230. [DOI] [PubMed] [Google Scholar]
- 26.Harmer AR, Naylor JM, Crosbie J, et al. Land-based versus water-based rehabilitation following total knee replacement: a randomized, single-blind trial. Arthritis Rheum. 2009;61(2):184–91. doi: 10.1002/art.24420. http://dx.doi.org/10.1002/art.24420. Medline:19177536. [DOI] [PubMed] [Google Scholar]
- 27.Jakovljevic M, Vauhnik R. Aquatic exercises versus land based exercises for elderly patients after a total hip replacement. Zdrav Vestn. 2011;80(4):240–5. [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007. http://dx.doi.org/10.1016/j.ijsu.2010.02.007. Medline:20171303. [DOI] [PubMed] [Google Scholar]
- 29.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–33. doi: 10.1016/s0004-9514(09)70043-1. http://dx.doi.org/10.1016/S0004-9514(09)70043-1. Medline:19463084. [DOI] [PubMed] [Google Scholar]
- 30.Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21. Medline:12882612. [PubMed] [Google Scholar]
- 31.Maher CG. A systematic review of workplace interventions to prevent low back pain. Aust J Physiother. 2000;46(4):259–69. doi: 10.1016/s0004-9514(14)60287-7. http://dx.doi.org/10.1016/S0004-9514(14)60287-7. Medline:11676811. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J. Statistical power analysis for the behavioural sciences. 2nd ed. Hillsdale (NJ): Erlbaum; 1988. [Google Scholar]
- 33.Greenhalgh T. How to read a paper: papers that summarise other papers (systematic reviews and meta-analyses) BMJ. 1997;315(7109):672–5. doi: 10.1136/bmj.315.7109.672. http://dx.doi.org/10.1136/bmj.315.7109.672. Medline:9310574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. http://dx.doi.org/10.1136/bmj.327.7414.557. Medline:12958120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92. doi: 10.1097/01.MLR.0000062554.74615.4C. http://dx.doi.org/10.1097/01.MLR.0000062554.74615.4C. Medline:12719681. [DOI] [PubMed] [Google Scholar]
- 36.Atkins D, Best D, Briss PA, et al. GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490–4. doi: 10.1136/bmj.328.7454.1490. http://dx.doi.org/10.1136/bmj.328.7454.1490. Medline:15205295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gogia PP, Braatz JH, Rose SJ, et al. Reliability and validity of goniometric measurements at the knee. Phys Ther. 1987;67(2):192–5. doi: 10.1093/ptj/67.2.192. Medline:3809242. [DOI] [PubMed] [Google Scholar]
- 38.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1(1):64. doi: 10.1186/1477-7525-1-64. http://dx.doi.org/10.1186/1477-7525-1-64. Medline:14613558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Collins NJ, Misra D, Felson DT, et al. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS) Arthritis Care Res (Hoboken) 2011;63(S11):S208–28. doi: 10.1002/acr.20632. http://dx.doi.org/10.1002/acr.20632. Medline:22588746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Escobar A, Quintana JM, Bilbao A, et al. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage. 2007;15(3):273–80. doi: 10.1016/j.joca.2006.09.001. http://dx.doi.org/10.1016/j.joca.2006.09.001. Medline:17052924. [DOI] [PubMed] [Google Scholar]
- 41.Murphy M, Journeaux S, Russell T. High-flexion total knee arthroplasty: a systematic review. Int Orthop. 2009;33(4):887–93. doi: 10.1007/s00264-009-0774-5. http://dx.doi.org/10.1007/s00264-009-0774-5. Medline:19352655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rowe PJ, Myles CM, Walker C, et al. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture. 2000;12(2):143–55. doi: 10.1016/s0966-6362(00)00060-6. http://dx.doi.org/10.1016/S0966-6362(00)00060-6. Medline:10998612. [DOI] [PubMed] [Google Scholar]
- 43.Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24(3):191–8. doi: 10.1097/00004356-200109000-00004. http://dx.doi.org/10.1097/00004356-200109000-00004. Medline:11560234. [DOI] [PubMed] [Google Scholar]
- 44.Hartmann S, Huch R. Response of pregnancy leg edema to a single immersion exercise session. Acta Obstet Gynecol Scand. 2005;84(12):1150–3. doi: 10.1111/j.0001-6349.2005.00829.x. http://dx.doi.org/10.1080/j.0001-6349.2005.00829.x. Medline:16305699. [DOI] [PubMed] [Google Scholar]
- 45.Tidhar D, Drouin J, Shimony A. Aqua lymphatic therapy in managing lower extremity lymphedema. J Support Oncol. 2007;5(4):179–83. Medline:17500505. [PubMed] [Google Scholar]
- 46.Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25(2):337–57. doi: 10.1016/j.csm.2005.12.008. http://dx.doi.org/10.1016/j.csm.2005.12.008. Medline:16638496. [DOI] [PubMed] [Google Scholar]
- 47.Shelbourne KD. Invited commentary. J Orthop Sports Phys Ther. 2005;35(2):61–2. [Google Scholar]
- 48.Gusi N, Tomas-Carus P. Cost-utility of an 8-month aquatic training for women with fibromyalgia: a randomized controlled trial. Arthritis Res Ther. 2008;10(1):R24. doi: 10.1186/ar2377. http://dx.doi.org/10.1186/ar2377. Medline:18294367. [DOI] [PMC free article] [PubMed] [Google Scholar]