ABSTRACT
Purpose: 1) To compare the ability of functional mobility and balance assessments in discriminating fallers from non-fallers and recurrent fallers from those with fewer or no falls. 2) To compare the discriminatory accuracy of cut-off scores specific to this study sample with that of cut-off scores proposed in the literature for community-dwelling older adults. Methods: In a sample of 39 ambulatory older adults living independently in the community, fallers were identified on the basis of number of falls in the past year. Seven functional tests of mobility and balance were used to identify fallers and recurrent fallers on the basis of their fall history. Results: Discrimination of fallers from non-fallers was poor: Only a high-level balance assessment significantly discriminated these groups (p=0.0498, area under the curve [AUC]=0.68). Four assessments significantly discriminated recurrent fallers from those with fewer or no falls (ps=0.006–0.009), but their discriminatory powers were not significantly different from one another (AUCs=0.77–0.80, p>0.05). For two assessments, cutoff scores based on the study sample enhanced discriminatory accuracy relative to the literature-based cutoff scores. Conclusions: To improve fall prediction for ambulatory community-dwelling older adults, future prospective studies should consider including high-level mobility and balance assessments and targeting cutoff scores to the level of function of this relatively high-functioning population.
Key Words: aged, geriatric assessment, mobility limitation, postural balance
RÉSUMÉ
Objet : Comparer la capacité qu'ont les évaluations de la mobilité fonctionnelle et de l'équilibre d'établir une distinction entre les personnes qui chutent et les personnes qui ne chutent pas, et entre celles qui chutent fréquemment et celles qui chutent peu ou jamais; comparer la précision en matière de distinction des points de coupure propres à l'échantillon de cette étude par rapport à ceux proposés dans la littérature concernant les personnes âgées qui résident dans la collectivité. Méthodes : Dans un échantillon de 39 personnes âgées mobiles qui vivent en autonomie dans la collectivité, les personnes qui chutent ont été déterminées selon le nombre de chutes faites au cours de l'année précédente. Sept tests fonctionnels concernant la mobilité et l'équilibre ont été utilisés pour déterminer les personnes qui chutent et les personnes qui chutent fréquemment selon leurs antécédents en matière de chutes. Résultats : La distinction des personnes qui chutent des personnes qui ne chutent pas était faible: seule une évaluation avancée de l'équilibre a établi une distinction importante entre ces groupes (p=0,0498, AUC=0,68). Quatre évaluations ont établi une distinction importante entre les personnes qui chutent fréquemment par rapport à celles qui chutent peu souvent ou jamais (p=0,006 à 0,009), mais leurs puissances de distinction n'étaient pas assez différentes les unes des autres (AUC=0,77 à 0.80, p>0,05). Dans le cadre de deux évaluations, les points de coupure fondés sur l'échantillon de l'étude ont amélioré la précision en matière de distinction des points de coupure établis selon la littérature. Conclusions : Pour améliorer la prédiction des chutes chez les personnes âgées qui résident dans la collectivité, les prochaines études prospectives doivent prendre en considération l'inclusion d'évaluations avancées de la mobilité et de l'équilibre et cibler les points de coupure au niveau de cette population hautement fonctionnelle.
Mots clés : équilibre postural, évaluation gériatrique, limitation de la mobilité, vieillissement
Approximately one-third of community-dwelling older adults (aged ≥65 years) fall at least once per year, and half of this cohort experiences multiple falls.1–3 Functional mobility and balance deficits are strongly associated with a greater risk for falls,1,4 and performance-based functional assessments are widely used in clinical practice to evaluate mobility and balance deficits and predict fall risk in this population. Accurate assessment of functional mobility and balance helps to identify modifiable risk factors and ultimately guide targeted interventions to reduce falling.3
Although a variety of functional assessments are routinely used to predict falls in older adults,5 less attention has been paid to fall prediction in relatively high-functioning older adults who are ambulatory and living independently in the community (ambulatory community-dwelling older adults, or ACDOA).2,6–9 Existing reports on fall prediction among ACDOA have had conflicting results. For instance, one study reported that five balance tests—the Berg Balance Scale (BBS), timed up-and-go test (TUG), Dynamic Gait Index (DGI), Modified Clinical Tests of Sensory Interaction for Balance, and 100% Limits of Stability Test—could not predict falls in ACDOA, even when they were at risk for falls;6 however, another study reported that a combination of multiple clinical scales (balance self-report, one-leg stance, and stability limits) predicted falls in ACDOA.8 Results are difficult to compare across studies because the studies included different and, in some instances, limited functional assessments and involved predicting either fallers or recurrent fallers. For an assessment to accurately predict fall risk, it must first be able to cross-sectionally discriminate fallers from non-fallers. Therefore, our approach was to compare the ability of a wide range of functional tests to discriminate both fallers from non-fallers and recurrent fallers (i.e., those with ≥2 falls) from those with fewer or no falls in a sample of ACDOA.
Using challenging functional assessments and applying cutoff scores targeted to the level of function of an ACDOA may improve the discrimination of fallers from non-fallers. Emerging evidence has suggested that dynamic, attention-demanding, and challenging tests are needed to reveal mobility and balance deficits in higher functioning older adults,6,10,11 which indicates that including more challenging functional tests may increase the likelihood of identifying fallers among ACDOA. Some challenging assessments such as the Community Balance and Mobility (CB&M) scale have recently been validated in the population of ACDOA, but they have not been compared with other functional assessments in terms of their ability to discriminate fallers from non-fallers.10 Furthermore, the cutoff scores of functional tests that are used as thresholds to classify fall risk may need to be targeted to the functional level of ACDOA because inappropriate application of cutoff scores leads to inaccurate discrimination of fallers from non-fallers. For instance, Neuls et al.12 concluded that the routinely used literature-based BBS cutoff score cannot predict fall risk across all older adults and suggested that sample-based cutoff scores be developed that are targeted to older adults' level of function. Therefore, investigating the discriminatory ability of several functional assessments and the accuracy with which these tests discriminate fallers and recurrent fallers from non-fallers could be the first step in identifying tests to improve fall-risk prediction targeted to ACDOA's level of function.
Our study used data collected as part of another larger study that included seven functional tests and a self-report of fall history.10 The first purpose of our study was to compare the ability of these functional mobility and balance assessments to discriminate both fallers from non-fallers and recurrent fallers (i.e., those with ≥2 falls) from those with one or no falls. The second purpose was to compute the discriminatory accuracy (sensitivity and specificity) of functional tests using cutoff scores specific to our study sample and compare it with that of literature-based cutoff scores. We expected the findings from this retrospective study to provide important insights for designing efficient prospective studies of fall-risk prediction for ACDOA.
Methods
Our study involved secondary analysis of data collected from a convenience sample of 40 volunteer participants recruited during a 3-year study period.10 Our study included 39 of the 40 volunteer participants from the original cohort; fall data were unavailable for 1 participant. Participants were recruited by mailing out advertisement flyers to residential, retirement, and independent living facilities as well as by talking to a group of older adults at the local wellness centre about the study's purpose and contacting them via word of mouth.
Participants
Participants were included if they were ≥65 years of age, residing independently in the community, able to walk independently without an assistive device, and able to follow verbal requests for tasks (e.g., place a foot on a 15 cm [6 in.] step in front of a chair). Potential participants were excluded from the study if they scored less than 23 on the Mini-Mental State Examination (a score that suggests cognitive impairment),13 had neurologic and orthopaedic impairments limiting balance and mobility, or had cardiorespiratory symptoms or unstable cardiovascular disease. The study was approved by the University of North Florida institutional review board for the protection of human subjects, and all participants provided informed consent.
Outcome measures
As in other retrospective reports in the literature, falls were documented as the participant's self-reported history of falls in the past year.14–17 Questions modified from the falls questionnaire of the National Health Interview Survey were used to document fall history. A fall was defined as any event that led to an unplanned, unexpected contact with a supporting surface such as the floor, the ground, a bed, or a chair;18 a faller was defined as a person who had had at least one fall in the past year, and a recurrent faller was defined as a person who had had two or more falls in the past year.
Clinical functional assessments of mobility and balance included in the study were the TUG,19,20 BBS,21,22 DGI,23 Functional Reach Test (FRT),24 Short Physical Performance Battery (SPPB),25,26 Activities-specific Balance Confidence (ABC) scale,27,28 and CB&M scale29 (Table A1 online). The first six assessments are currently used with ACDOA, and the CB&M was recently validated with ACDOA.10 All of these functional tests are performance based, except for the ABC scale, which is a self-report measure to assess balance efficacy.27 The ABC scale was included in this study because measures of self-efficacy have been shown to independently predict falls.30
Procedures
Assessments were conducted in a predetermined order; those requiring walking were conducted before the others to avoid fatigue-related bias in test performance. Two to three rest periods of as long as 10 minutes were incorporated into the testing, and participants were allowed more rest periods if needed. The CB&M, DGI, and BBS testing sessions were videotaped; the videotaped assessments were re-scored by the same physical therapist approximately 3 weeks later to evaluate intrarater reliability. To evaluate the interrater reliability of the CB&M, DGI, and BBS assessments, two physical therapists (with 25 years' and 5 years' experience, respectively), blinded to each other's scores, independently scored the videotaped assessments. The SPPB and TUG are timed assessments, and the ABC is a self-report measure; therefore, these assessments were not videotaped for the purpose of evaluating reliability.
Data analysis
We evaluated the intrarater and interrater reliability of the CB&M, DGI, and BBS using ICC2,k and ICC3,k respectively. Both intrarater reliability (ICC2,k=0.93–0.99; 95% CI, 0.89–1.0) and interrater reliability (ICC2,k=0.88–0.98; 95% CI, 0.81–0.99) were high; therefore, we used the original functional test scores for further data analyses.
Discriminating fallers from non-fallers
We used exploratory logistic regression models to investigate the likelihood of falls, using the functional tests (CB&M, BBS, FRT, TUGT, DGI, SPPB, and ABC) as single continuous predictors. Sex and age as covariates were also fitted and evaluated in the exploratory models. We created two sets of models. In the one-or-more-falls (≥1F) model, which discriminated fallers from non-fallers, the dichotomous response was “any fall” or “no fall”, in the two-or-more-falls (≥2F) model, which discriminated recurrent fallers from those with less than two falls or no falls, the dichotomous response was “≥2 falls” or “<2 falls.” The area under the curve (AUC) of a receiver operating characteristic (ROC) curve was computed to assess the discriminatory power of the functional assessments that were the significant predictors of the ≥1F and ≥2F models. Hosmer and Lemeshow31 suggested that 0.7≤AUC≤0.8 represents acceptable discriminatory power (AUC=0.50 corresponds to random classification).
Discriminatory accuracy indices of sample-based versus literature-based cutoff scores
Literature-based cut-off scores are those established in the literature for ACDOAs (see Table A1). Study-sample-based cutoff scores are computed for our study sample to optimize sensitivity and specificity. The optimal cutoff score is the balance between sensitivity and specificity and indicates the point on the ROC curve that comes closest to the upper left-hand corner of the graph. We used McNemar's pairwise comparisons to compare sensitivity and specificity between literature-based and study-sample-based cutoff scores within individual assessments and compared discriminatory accuracy across assessments using the diagnostic odds ratio (DOR).32
All statistical analyses were conducted using SAS version 9.2 and JMP version 10 (SAS Institute, Cary, NC), with significance set at α=0.05.
Results
A convenience sample of 39 ACDOA (mean age 73.3 [SD 6.9] years; 13 men and 26 women) participated. Table 1 presents the characteristics of the study sample. As Table 2 shows, 61% of study participants (24/39) were fallers, 35.9% (14/39) were recurrent fallers, and 38.5% (15/39) had experienced no falls in the past year.
Table 1.
Characteristics of the Study Sample
| Characteristic |
Sample (n=39) |
Non-fallers (n=15) |
Fallers (≥1 falls; n=24) |
Recurrent fallers (≥2 falls; n=14) |
|---|---|---|---|---|
| No. | ||||
| Sex | ||||
| Male | 13 | 5 | 8 | 4 |
| Female | 26 | 10 | 16 | 10 |
| Residence | ||||
| Residential | 26 | |||
| Retirement community | 3 | |||
| Independent living facility | 10 | |||
| Comorbidities* | ||||
| Joint replacements | 6 | |||
| Vertebral impingement | 1 | |||
| Arthritis | 2 | |||
| Low BMD | 1 | |||
| Disc removal | 3 | |||
| Neck and back surgery | 1 | |||
| Diabetes | 4 | |||
| Tumour/cancer survivor | 4 | |||
| Vertigo | 2 | |||
| COPD, bronchitis | 1 | |||
| Emphysema | 2 | |||
| Controlled high BP | 9 | |||
| Pacemaker | 1 | |||
| Claudication | 1 | |||
| One eye blindness | 1 | |||
| Hypothyroid | 1 | |||
| Mean (SD) | ||||
|---|---|---|---|---|
| Age, y | 73.3 (6.9) | 73.2 (7.1) | 73.3 (6.9) | 71.6 (7.3) |
| CB&M, /96 | 47.5 (18.6) | 55.6 (20.0) | 43.1 (16.5) | 36.1 (12.7) |
| ABC, /100% | 87.76 (12.09) | 90.9 (10.2) | 85.3 (12.9) | 79.0 (13.3) |
| DGI, /24 | 19.78 (3.49) | 20.8 (3.3) | 19.2 (3.4) | 17.6 (3.4) |
| BBS, /56 | 53.13 (2.53) | 54.1 (2.2) | 52.4 (2.5) | 51.5 (2.6) |
| SPPB, /12 | 10.46 (1.62) | 10.9 (1.62) | 10.1 (1.5) | 9.7 (1.6) |
| TUGT, s | 10.36 (2.18) | 9.6 (2.1) | 10.7 (2.1) | 10.9 (2.3) |
| FRT, in. | 11.0 (2.15) | 11.1 (2.8) | 11.0 (1.5) | 11.05 (1.7) |
Some participants had more than one comorbidity.
BMD=bone mineral density; COPD=chronic obstructive pulmonary disease; BP=blood pressure; CB&M=Community Balance and Mobility Scale; ABC=Activities-Specific Balance Confidence; DGI=Dynamic Gait Index; BBS=Berg Balance Scale; SPPB=Short Physical Performance Battery; TUGT=timed up-and-go test; FRT=Functional Reach Test.
Table 2.
Fall Characteristics of the Study Sample (n=39)
| Characteristic | No. (%) of participants |
|---|---|
| History of falls per participant | |
| 0 | 15 (38.46) |
| 1 | 10 (25.64) |
| 2 | 7 (17.95) |
| 3 | 4 (10.26) |
| 4 | 1 (2.56) |
| 6 | 2 (5.13) |
| History of falls | |
| 0 | 15 (38.46) |
| ≥1 | 24 (61.54) |
| History of recurrent falls | |
| ≤1 | 25 (64.10) |
| ≥2 | 14 (35.90) |
| Reported activity/circumstance during fall | |
| Walking | |
| backwards | 1 |
| fast | 3 |
| missed a step | 1 |
| caught foot | 1 |
| outdoors | 3 |
| when dark | 1 |
| tripped | 3 |
| Stepped over an object | |
| barrier | 1 |
| irrigation system | 1 |
| newspaper | 1 |
| Surface | |
| uneven terrain | 2 |
| change in surface | 1 |
| Getting out of bed or chair | 3 |
| Not paying attention | 2 |
Functional assessments that discriminate fallers (≥1F) from non-fallers and recurrent fallers (≥2F) from those with fewer or no falls
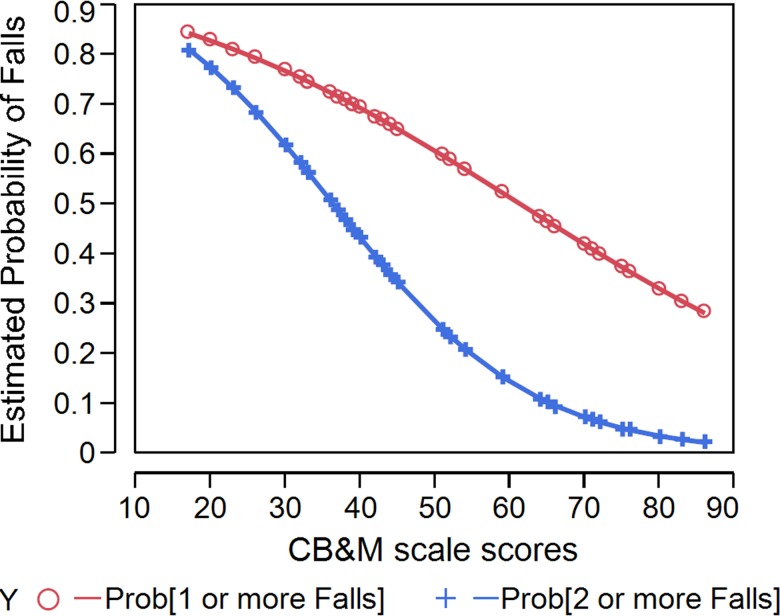
The CB&M scale discriminated participants in the ≥1F model, but the variance explained was low (p=0.049, Model R2=8%; see Table 3 and Figure 1). Four assessments discriminated participants in the ≥2F model: CB&M (p=0.009), ABC (p=0.004), DGI (p=0.006), and BBS (p=0.009), explaining low to moderate variance (Model R2=18%–22%), as shown in Table 3. Exploratory models with combinations of significant predictors and with gender and age as covariates were also tested, but none were significant. The Hosmer–Lemeshow goodness-of-fit test indicated that the logistic model was appropriate (χ2=1.86, p=0.967).
Table 3.
Results of Multivariate Logistic Regression on Functional Mobility and Balance Outcomes Discriminating Fallers (One or More Falls) and Recurrent Fallers (Two or More Falls)
| Parameter | β | χ2 | Model R2 | p-value | OR* |
|---|---|---|---|---|---|
| One or more falls (≥1F model) – Faller | |||||
| CB&M | 0.0380 | 3.85 | 0.085 | 0.049† | 1.038 |
| ABC | 0.0430 | 1.86 | 0.041 | 0.172 | 1.0448 |
| DGI | 0.1480 | 1.95 | 0.041 | 0.162 | 1.1601 |
| BBS | 0.3120 | 3.65 | 0.082 | 0.065 | 1.3669 |
| SPPB | 0.3410 | 1.98 | 0.044 | 0.158 | 1.4069 |
| TUG | −0.2570 | 2.33 | 0.049 | 0.127 | 0.7727 |
| FRT | 0.0260 | 0.03 | 0.000 | 0.861 | 1.0271 |
| Two or more falls (≥2F) – Recurrent faller | |||||
| CB&M | −0.075 | 6.66 | 0.206 | 0.009‡ | 0.927 |
| ABC | −0.109 | 7.99 | 0.226 | 0.004‡ | 0.896 |
| DGI | −0.327 | 7.56 | 0.187 | 0.006‡ | 0.720 |
| BBS | −0.455 | 6.77 | 0.181 | 0.009‡ | 0.634 |
| SPPB | −0.418 | 3.51 | 0.075 | 0.060 | 0.658 |
| TUG | 0.192 | 1.45 | 0.029 | 0.229 | 1.212 |
| FRT | −.0306 | 0.04 | 0.000 | 0.843 | 0.969 |
Unadjusted for age and sex.
p<0.05.
p<0.01.
CB&M=Community Balance and Mobility Scale; ABC=Activities-Specific Balance Confidence; DGI=Dynamic Gait Index; BBS=Berg Balance Scale; SPPB=Short Physical Performance Battery; TUGT=timed up-and-go test; FRT=Functional Reach Test.
Figure 1.
Logistic predictions of the faller (≥1 falls) and recurrent faller (≥2 falls) models in the past year, using the CB&M scale as the predictor assessment. In both models, the probability of falling decreases as CB&M scale scores increase; the slope of the prediction is better for the recurrent fallers.
CB&M=Community Balance and Mobility Scale.
The discriminatory power of the CB&M scale was low for the ≥1F model (AUC=0.68; 95% CI, 0.4978–0.8688; see Figure A1 online). The discriminatory powers of the significant assessments (CB&M, ABC, DGI, and BBS) were greater (AUCs=0.77–0.80) in the ≥2F model than in the ≥1F model, but the AUC indices were not statistically different from one another for the four significant predictors of the ≥2F model (Figure A2 online).
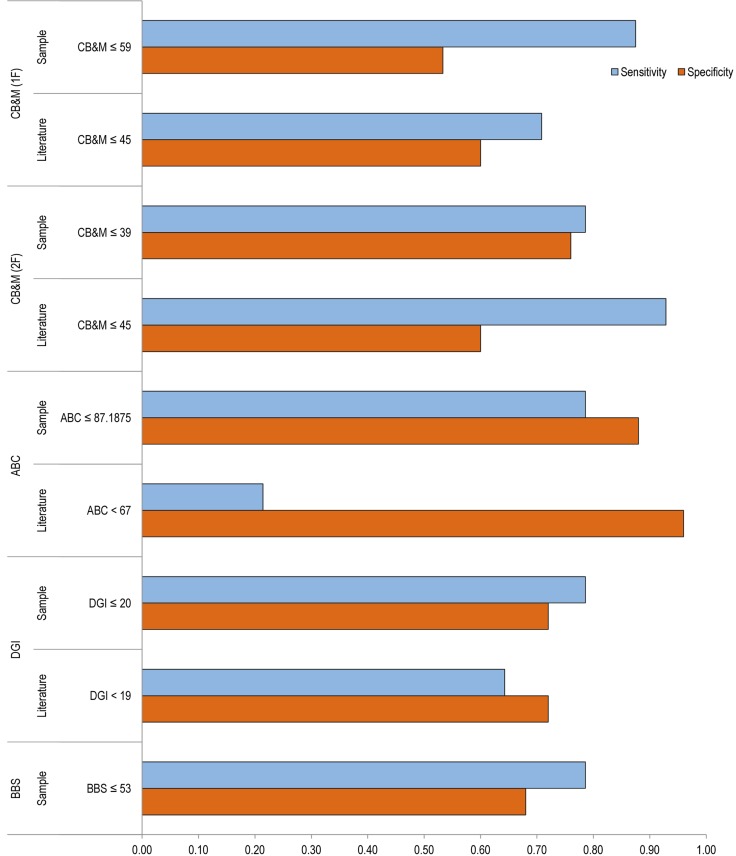
Sensitivity, specificity, and diagnostic odds ratios of cutoff scores for the significant assessments of the ≥1 F and ≥2 F models
Using study-sample-based cutoff scores improved sensitivity and DORs for all assessments (except the CB&M for the ≥2F model) relative to the literature-based cutoff scores, but the effect on specificity was not uniform (see Table 4 and Figure 2). The sample-based cutoff of ≤59 for the CB&M had significantly (p=0.045) higher sensitivity than the literature-based cutoff score of ≤45 for the ≥1F model; similarly, the sample-based cutoff of ≤87 for the ABC had significantly (p=0.025) higher sensitivity than the literature-based cutoff of ≤67 (see Table 4 and Figure 2). An exception was the literature-based cutoff of ≤45 for the CB&M, which had significantly (p=0.045) higher sensitivity than the sample-based cutoff of ≤39 for the ≥2F model. No other pairwise comparisons for sensitivity and specificity were significantly different from each other (see Table 4). The study-sample-based cutoff score of ≤87 for the ABC had the highest DOR at 26.89, followed by the CB&M cutoff score of ≤45, with a DOR of 19.50 for the ≥2F model (see Table 4).
Table 4.
Accuracy Indices of Literature-Based and Sample-Based Cutoff Scores of the Significant Discriminators of the Faller (One or More Falls) and Recurrent Faller (Two or More Falls) Model
| Measure and cutoff score type | Cutoff score (≤) | Sensitivity (TPR) | Specificity (TNR) | DOR | PR |
|---|---|---|---|---|---|
| One or more falls (≥1F) | |||||
| CB&M | |||||
| Lit. | 45 | 0.71 | 0.60 | 3.64 | 0.62 |
| Sample | 59 | 0.88* | 0.53 | 8.00 | 0.62 |
| Two or more falls (≥2F) | |||||
| CB&M | |||||
| Lit. | 45 | 0.93* | 0.60 | 19.50 | 0.36 |
| Sample | 39 | 0.79 | 0.76 | 11.61 | 0.36 |
| ABC | |||||
| Lit. | 67 | 0.21 | 0.96 | 6.55 | 0.36 |
| Sample | 87 | 0.79* | 0.88 | 26.89 | 0.36 |
| DGI | |||||
| Lit. | 19 | 0.64 | 0.72 | 4.63 | 0.36 |
| Sample | 20 | 0.79 | 0.72 | 9.43 | 0.36 |
| BBS | |||||
| Lit. | 45 | N/A† | N/A† | N/A† | N/A† |
| Sample | 53 | 0.79 | 0.68 | 7.79 | 0.36 |
Statistically significant difference in sensitivity and specificity between literature-based and sample-based cut-off scores within an assessment.
No participants below the literature-based cut-off score (BBS<45).
TPR=true positive ratio; TNR=true negative ratio; DOR=diagnostic odds ratio; PR=prevalence; Lit.=literature-based cut-off score; sample=sample-based cut-off score; CB&M=Community Balance and Mobility Scale; ABC=Activities-Specific Balance Confidence; DGI=Dynamic Gait Index; BBS=Berg Balance Scale; N/A=not applicable.
Figure 2.
Sensitivity and specificity of the literature-based and sample-based cutoff scores for the outcomes that significantly discriminated fallers and recurrent fallers.
Discussion
Our study has three main findings. First, the CB&M scale discriminated fallers (≥1F) from non-fallers. Second, four functional assessments—the CB&M, ABC, DGI, and BBS—discriminated recurrent fallers (≥2F) from those with fewer or no falls. Third, cutoff scores computed for the study sample improved discriminatory accuracy relative to literature-based cutoff scores for two assessments. These findings should be considered preliminary in the area of fall-risk prediction until prospective studies can further validate our results.
The proportion of falls in our study sample was higher than some reports in the literature: 61% of participants in our study reported at least one fall in the past year; 30% of community-dwelling older adults in the literature experienced one or more falls in a year.1–3 Moreover, 25% of participants in our study sample fell once, and 35% fell on two or more occasions, whereas other retrospective studies have reported 19% experiencing one fall and 14% experiencing two or more falls.33
There may be several reasons for the high proportion of falls in our sample. First, we recruited ACDOA who volunteered to participate in the study, as opposed to using a random sample. Second, risk for any fall may have been higher for this group because individuals were participating at their usual level of functioning, which exposed them to more situations that could result in a fall.8 Third, our small sample size may have skewed the percentages, overestimating the proportion of fallers. It is interesting that our reported fall rates are similar to those of some other studies in the literature, such as that of Sai and colleagues,34 who reported the incidence of falls in their community-dwelling sample to be around 62.5%. As suggested earlier,8 comparison with other studies on fall rates may be difficult because of the variability in methods of reporting fall events (self-report vs. identified by a professional), study designs used for data collection (retrospective vs. prospective), and participants' level of function.
Our study included assessment of both fallers and recurrent fallers. This is important, because even a single fall (injurious or non-injurious) may lead to fear of falling, resulting in a decrease in physical activity.30 Moreover, a history of even a single fall increases a person's risk of admission to a long-term facility threefold compared with that of someone with no history of falling.35 Therefore, early identification of those at risk of falling may be helpful in initiating fall-prevention efforts sooner. A relatively high-functioning population such as the ACDOA in our sample may require more challenging assessments to reveal subtle balance deficits.6,11 The CB&M scale was recently validated for ACDOA as a challenging assessment because it did not show a ceiling in detection of balance and mobility deficits, unlike other functional assessments.10 The CB&M scale includes a range of challenging assessment items, including more difficult and complex activities that may create cognitive–motor interference (e.g., sequencing movement components and multi-tasking).
Although the CB&M scale was the only assessment that discriminated fallers from non-fallers in our study, as a predictor of the ≥1F model it was only marginally significant, and it demonstrated low discriminatory power (AUC=0.68) and a low DOR in the ≥2F model. Together, these findings suggest that in our study sample, even the most challenging assessment did not accurately discriminate fallers from non-fallers. Therefore, we suggest creating a battery of assessment items using some activities from the CB&M scale (especially those that create cognitive–motor interference) and developing other challenging activities (such as negotiating obstacles under secondary cognitive demands) to improve early fall prediction in ACDOA. Emerging evidence has suggested that the interplay between motor and cognitive systems to maintain postural support and balance is affected in older adults.36 Therefore, assessing functional performance of challenging and complex activities that create cognitive–motor interference may be key to unmasking balance deficits in ACDOA, whose motor and cognitive performance may appear unremarkable in isolation. Furthermore, the literature linking reactive balance control (e.g., reactive and compensatory stepping) to falls remains unexploited in clinical assessment tools.37 We suggest that challenging activities that target reactive balance control may improve fall-risk assessment in ACDOA.
Recurrent fallers were identified by four significant predictors (CB&M, ABC, DGI, and BBS), supporting earlier findings that recurrent fallers are more easily identified than fallers.3,34 Two of these assessments (ABC, DGI) have been shown to have minimal ceiling effects (≤10%).10 In contrast, the three functional assessments (TUG, FRT, and SPPB) that could not discriminate even recurrent fallers from those with fewer or no falls may have been too easy for this relatively high-functioning population; future prospective fall-prediction studies should be cautious when including functional assessments that are not targeted to the level of function of ACDOA. Nonetheless, because our study used a retrospective design, our results are only the first step in supporting the use of challenging assessments for fall prediction in ACDOA.
Although our study found four functional assessments that discriminated recurrent fallers from those with fewer or no falls, investigation of their sensitivity and specificity showed that discriminatory cutoff scores targeted to ACDOA enhanced sensitivity in some clinical assessments relative to direct application of literature-based cutoff scores. Whereas the sample-based cutoff score of ≤59 for the CB&M enhanced sensitivity in identifying fallers, the literature-based cutoff score of ≤4510 was more accurate in identifying recurrent fallers. Furthermore, the sample-based cutoff score of ≤87% for the ABC accurately identified recurrent fallers in our sample, and this cutoff score significantly increased sensitivity and DOR relative to the literature-based cutoff score without much loss in specificity.
Although none of the other functional assessments achieved statistical significance, the cutoff scores on the BBS and DGI assessment may need to be re-examined to better suit ACDOA. For instance, all participants in our study scored above the suggested cutoff of <45 for the BBS,15 demonstrating the BBS's reduced discriminatory ability in this population. Similarly, the sample-based cutoff score of ≤20 for the DGI increased sensitivity (although not to the threshold of statistical significance) and DOR, which suggests a modest improvement in discriminatory accuracy. It is important to note that the suggested cutoff scores shown to improve sensitivity in our study sample are not representative of all ACDOA and need to be further validated using larger prospective samples. Nonetheless, our method of re-examining cutoff scores to improve sensitivity of functional assessments to identify fallers is promising and highlights the need for prospective studies to establish multiple thresholds based on level of function.
Limitations
Our study has several limitations. First, fall risk was identified retrospectively. In a retrospective study design, evaluation of exposure (mobility and balance deficits) takes place after the outcome (falls) has occurred; therefore, it is not possible to establish a temporal link between falling and test scores, and it is difficult to determine whether the poor function caused the fall or whether the fall resulted in the poor mobility and balance function. Prospective observation of falls as the diagnostic gold standard is essential to validate our findings.
Second, our study used a small convenience sample whose characteristics may not be generalizable to the large population of ACDOA; a larger random sample is needed to further validate the results. Third, our method of evaluating discriminatory accuracy has some limitations. Some literature-based cutoff scores were derived from prospective studies; using prospective cutoff scores to determine the accuracy of retrospective fall events may limit the conclusions derived from our observed results. Last, falls are multi-factorial, and a thorough assessment of fall risk should include evaluation of other relevant factors such as vision, medications, cognitive impairment, sensation, and concomitant medical problems. Therefore, future models for predicting fall risk should reflect the multi-factorial nature of falls.
Key Messages
What is already known on this topic
Functional assessments of mobility and balance have been used to predict fall risk and identify modifiable targets for interventions to reduce falling in older adults. Although several functional tests are used to predict fall risk in older adults, more research is needed on predicting the fall risk of ambulatory older adults living independently in the community. Results from some existing studies have suggested that current functional assessments do not accurately predict fall risk in this relatively high-functioning older adult population.
What this study adds
The Community Balance and Mobility (CB&M) scale identified both fallers and recurrent fallers on the basis of their fall history in a sample of ambulatory community-dwelling older adults, providing preliminary support for the inclusion of a challenging assessment such as the CB&M for fall risk prediction in an ambulatory cohort. Of the seven assessments included in the study, four (CB&M, ABC, DGI, and BBS) discriminated recurrent fallers from those with fewer or no falls. Study-sample-based cutoff scores enhanced sensitivity of discrimination relative to literature-based cutoff scores for two clinical assessments, which suggests that prospective study designs should evaluate cutoff scores targeted to the level of ambulatory older adults to improve sensitivity of functional assessments.
Supplementary Material
Physiotherapy Canada 2015; 67(2);184–193; doi:10.3138/ptc.2014-19
References
- 1.O'Loughlin JL, Robitaille Y, Boivin JF, et al. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. Medline:8452142. [DOI] [PubMed] [Google Scholar]
- 2.Gates S, Smith LA, Fisher JD, et al. Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults. J Rehabil Res Dev. 2008;45(8):1105–16. http://dx.doi.org/10.1682/JRRD.2008.04.0057. Medline:19235113. [PubMed] [Google Scholar]
- 3.Stel VS, Smit JH, Pluijm SMF, et al. Balance and mobility performance as treatable risk factors for recurrent falling in older persons. J Clin Epidemiol. 2003;56(7):659–68. doi: 10.1016/s0895-4356(03)00082-9. http://dx.doi.org/10.1016/S0895-4356(03)00082-9. Medline:12921935. [DOI] [PubMed] [Google Scholar]
- 4.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7. doi: 10.1056/NEJM198812293192604. http://dx.doi.org/10.1056/NEJM198812293192604. Medline:3205267. [DOI] [PubMed] [Google Scholar]
- 5.Perell KL, Nelson A, Goldman RL, et al. Fall risk assessment measures: an analytic review. J Gerontol A Biol Sci Med Sci. 2001;56(12):M761–6. doi: 10.1093/gerona/56.12.m761. http://dx.doi.org/10.1093/gerona/56.12.M761. Medline:11723150. [DOI] [PubMed] [Google Scholar]
- 6.Boulgarides LK, McGinty SM, Willett JA, et al. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83(4):328–39. Medline:12665404. [PubMed] [Google Scholar]
- 7.Laessoe U, Hoeck HC, Simonsen O, et al. Fall risk in an active elderly population—can it be assessed? J Negat Results Biomed. 2007;6(1):2. doi: 10.1186/1477-5751-6-2. http://dx.doi.org/10.1186/1477-5751-6-2. Medline:17257414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muir SW, Berg K, Chesworth B, et al. Balance impairment as a risk factor for falls in community-dwelling older adults who are high functioning: a prospective study. Phys Ther. 2010;90(3):338–47. doi: 10.2522/ptj.20090163. http://dx.doi.org/10.2522/ptj.20090163. Medline:20056721. [DOI] [PubMed] [Google Scholar]
- 9.O'Brien K, Pickles B, Culham E. Clinical measures of balance in community-dwelling elderly female fallers and non-fallers. Physiother Can. 1998;50(3):212–21. [Google Scholar]
- 10.Balasubramanian CK. The Community Balance and Mobility Scale alleviates the ceiling effects observed in the currently used gait and balance assessments for the community-dwelling older adults. J Geriatr Phys Ther. doi: 10.1519/JPT.0000000000000024. Epub 2014 Jun 19. http://dx.doi.org/10.1519/JPT.0000000000000024. Medline:24949849. [DOI] [PubMed] [Google Scholar]
- 11.Pardasaney PK, Latham NK, Jette AM, et al. Sensitivity to change and responsiveness of four balance measures for community-dwelling older adults. Phys Ther. 2012;92(3):388–97. doi: 10.2522/ptj.20100398. http://dx.doi.org/10.2522/ptj.20100398. Medline:22114200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neuls PD, Clark TL, Van Heuklon NC, et al. Usefulness of the Berg Balance Scale to predict falls in the elderly. J Geriatr Phys Ther. 2011;34(1):3–10. doi: 10.1097/JPT.0b013e3181ff2b0e. Medline:21937886. [DOI] [PubMed] [Google Scholar]
- 13.Bean JF, Kiely DK, LaRose S, et al. Which impairments are most associated with high mobility performance in older adults? Implications for a rehabilitation prescription. Arch Phys Med Rehabil. 2008;89(12):2278–84. doi: 10.1016/j.apmr.2008.04.029. http://dx.doi.org/10.1016/j.apmr.2008.04.029. Medline:19061739. [DOI] [PubMed] [Google Scholar]
- 14.Dibble LE, Christensen J, Ballard DJ, et al. Diagnosis of fall risk in Parkinson disease: an analysis of individual and collective clinical balance test interpretation. Phys Ther. 2008;88(3):323–32. doi: 10.2522/ptj.20070082. http://dx.doi.org/10.2522/ptj.20070082. Medline:18187494. [DOI] [PubMed] [Google Scholar]
- 15.Shumway-Cook A, Baldwin M, Polissar NL, et al. Predicting the probability for falls in community-dwelling older adults. Phys Ther. 1997;77(8):812–9. doi: 10.1093/ptj/77.8.812. Medline:9256869. [DOI] [PubMed] [Google Scholar]
- 16.Lundin-Olsson L, Jensen J, Nyberg L, et al. Predicting falls in residential care by a risk assessment tool, staff judgement, and history of falls. Aging Clin Exp Res. 2003;15(1):51–9. doi: 10.1007/BF03324480. http://dx.doi.org/10.1007/BF03324480. Medline:12841419. [DOI] [PubMed] [Google Scholar]
- 17.Barker AL, Nitz JC, Low Choy NL, et al. Measuring fall risk and predicting who will fall: clinimetric properties of four fall risk assessment tools for residential aged care. J Gerontol A Biol Sci Med Sci. 2009;64(8):916–24. doi: 10.1093/gerona/glp041. http://dx.doi.org/10.1093/gerona/glp041. Medline:19414508. [DOI] [PubMed] [Google Scholar]
- 18.Bogle Thorbahn LD, Newton RA. Use of the Berg Balance Test to predict falls in elderly persons. Phys Ther. 1996;76(6):576–83; discussion 584–5. doi: 10.1093/ptj/76.6.576. Medline:8650273. [DOI] [PubMed] [Google Scholar]
- 19.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. Medline:10960937. [PubMed] [Google Scholar]
- 20.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. Medline:1991946. [DOI] [PubMed] [Google Scholar]
- 21.Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27(1):27–36. Medline:7792547. [PubMed] [Google Scholar]
- 22.Muir SW, Berg K, Chesworth B, et al. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449–59. doi: 10.2522/ptj.20070251. http://dx.doi.org/10.2522/ptj.20070251. Medline:18218822. [DOI] [PubMed] [Google Scholar]
- 23.Shumway-Cook A, Baldwin M, Polissar NL, et al. Predicting the probability for falls in community-dwelling older adults. Phys Ther. 1997;77(8):812–9. doi: 10.1093/ptj/77.8.812. Medline:9256869. [DOI] [PubMed] [Google Scholar]
- 24.Duncan PW, Studenski S, Chandler J, et al. Functional reach: predictive validity in a sample of elderly male veterans. J Gerontol. 1992;47(3):M93–8. doi: 10.1093/geronj/47.3.m93. http://dx.doi.org/10.1093/geronj/47.3.M93. Medline:1573190. [DOI] [PubMed] [Google Scholar]
- 25.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. http://dx.doi.org/10.1093/geronj/49.2.M85. Medline:8126356. [DOI] [PubMed] [Google Scholar]
- 26.Rikli R, Jones CJ. Senior Fitness Test manual. Champaign, IL: Human Kinetics; 2001. [Google Scholar]
- 27.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–34. doi: 10.1093/gerona/50a.1.m28. http://dx.doi.org/10.1093/gerona/50A.1.M28. Medline:7814786. [DOI] [PubMed] [Google Scholar]
- 28.Lajoie Y, Gallagher SP. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg Balance Scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38(1):11–26. doi: 10.1016/s0167-4943(03)00082-7. http://dx.doi.org/10.1016/S0167-4943(03)00082-7. Medline:14599700. [DOI] [PubMed] [Google Scholar]
- 29.Howe JA, Inness EL, Venturini A, et al. The Community Balance and Mobility Scale—a balance measure for individuals with traumatic brain injury. Clin Rehabil. 2006;20(10):885–95. doi: 10.1177/0269215506072183. Medline:17008340. [DOI] [PubMed] [Google Scholar]
- 30.Scheffer AC, Schuurmans MJ, van Dijk N, et al. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37(1):19–24. doi: 10.1093/ageing/afm169. http://dx.doi.org/10.1093/ageing/afm169. Medline:18194967. [DOI] [PubMed] [Google Scholar]
- 31.Hosmer DW, Lemeshow S. Applied logistic regression. New York: Wiley; 2000. http://dx.doi.org/10.1002/0471722146. [Google Scholar]
- 32.Glas AS, Lijmer JG, Prins MH, et al. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56(11):1129–35. doi: 10.1016/s0895-4356(03)00177-x. http://dx.doi.org/10.1016/S0895-4356(03)00177-X. Medline:14615004. [DOI] [PubMed] [Google Scholar]
- 33.Lord SR, Ward JA, Williams P, et al. An epidemiological study of falls in older community-dwelling women: the Randwick falls and fractures study. Aust J Public Health. 1993;17(3):240–5. doi: 10.1111/j.1753-6405.1993.tb00143.x. http://dx.doi.org/10.1111/j.1753-6405.1993.tb00143.x. Medline:8286498. [DOI] [PubMed] [Google Scholar]
- 34.Sai AJ, Gallagher JC, Smith LM, et al. Fall predictors in the community dwelling elderly: a cross sectional and prospective cohort study. J Musculoskelet Neuronal Interact. 2010;10(2):142–50. Medline:20516631. [PubMed] [Google Scholar]
- 35.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–84. doi: 10.1056/NEJM199710303371806. http://dx.doi.org/10.1056/NEJM199710303371806. Medline:9345078. [DOI] [PubMed] [Google Scholar]
- 36.Pichierri G, Wolf P, Murer K, et al. Cognitive and cognitive-motor interventions affecting physical functioning: a systematic review. BMC Geriatr. 2011;11(1):29. doi: 10.1186/1471-2318-11-29. http://dx.doi.org/10.1186/1471-2318-11-29. Medline:21651800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maki BE, McIlroy WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age Ageing. 2006;35(Suppl 2):ii12–8. doi: 10.1093/ageing/afl078. http://dx.doi.org/10.1093/ageing/afl078. Medline:16926197. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.