The Patient
A 20-year-old construction worker sustained a non-displaced scaphoid waist fracture in his right dominant wrist in a fall at work. The patient wants to return to work as soon as possible. Physical examination reveals pain at the anatomic snuff-box, restricted wrist movement, and decreased grip strength. He has no other associated injuries.
The Question(s)
What is the most appropriate treatment for this patient?
Current Opinion
Displaced fractures require operative treatment. On the other hand, the best treatment of non-displaced fractures is disputed. Casting for three months will predictably heal 90–95% of scaphoid waist fractures [1–3], but patient inconvenience and work restrictions when in the cast have prompted some surgeons to advocate for internal fixation with a screw.[4–8]
The Evidence
Cast Immobilization
Cast immobilization is simple, safe, and inexpensive; however, prolonged immobility can interfere with work and lifestyle, which raises socioeconomic and compliance issues.[9] Optimum management is achieved with the least cumbersome casting regimen consistent with fracture healing. Three level 1b prospective randomized studies[10] have addressed cast immobilization for non-displaced scaphoid fractures. (Table 1).
Table 1.
Casting Outcomes. Evidence of optimal casting for nondisplaced scaphoid fractures.
| Study | Purpose | Methods | Union rate (%) |
Average Time to Union |
Level of Evidence |
Authors' Conclusions |
|---|---|---|---|---|---|---|
| Gellman et al. (1989) |
To compare Above Elbow (AE) versus Below Elbow (BE) thumb-spica casts for nondisplaced fractures |
51 patients randomized into two groups: 1) AE for 6 weeks followed by BE 2) BE |
AE->BE: 28/28 (100%) BE: 21/23 (91%)†† |
AE->BE: 9.5 weeks BE: 12.7 weeks* |
Ib Prospective data with randomization and control |
6 weeks in an above-elbow thumb-spica cast followed by switch to below-elbow thumb-spica cast |
| Clay et al. (1991) |
To compare immobilization of the thumb versus leaving the thumb free down to metacarpal |
392 patients randomized into two groups: 1) Colles' cast with thumb free (C) 2) "Scaphoid" plaster cast (S) |
C: 133/148 (90%) S: 129/143 (90%)‡ |
C: 9 weeks S: 9.6 weeks |
Ib Prospective data with randomization and control |
Undisplaced waist fractures should be treated with Colles' cast with thumb free |
| Hambidge et al. (1999) |
To compare wrist flexion (F) versus wrist extension (E) with the use of a Colles' brace |
121 patients randomized into two groups: 1) Colles' with 20° flexion (F) 2) Colles'with 20° extension (E) |
F: 53/58 (91%) E: 55/63 (87%) |
Unquantified; Wrist extension at 6 months: F=61°; E=73°* |
Ib Prospective data with randomization and control |
The wrist should be positioned in slight extension to regain full extension of wrist |
p< 0.05;
Significance unquantified;
Adapted from 'Table V' by adding “Definitely united” and “Probably united” (143 + 148 = 291; patient data missing)
Gellman et al. [11] randomly assigned patients into two groups to compare above-the-elbow thumb-spica versus below-the-elbow thumb-spica casts for non-displaced scaphoid fractures. Patients who were treated initially with above-elbow thumb-spica casts for six weeks and were later switched to below-elbow thumb-spica casts had a significantly shorter time to union (9.5 weeks versus 12.7 weeks) and decreased incidence of non-union (0% versus 8.7%). It was thought that the long cast eliminates the shear forces transmitted across the fracture site by pronation and supination of the forearm.
Clay et al. [12] randomly allocated 392 scaphoid waist fractures to below-elbow casts with or without immobilization of the thumb to the interphalangeal joint. The outcomes were stratified according to fracture pattern and indicate a nonunion rate of 10% for transverse fractures regardless of the type of cast.
Hambidge et al. [13] randomized 121 waist and distal scaphoid fractures to immobilization in either slight flexion or slight extension using a below-elbow plaster cast with the thumb free. The position of wrist immobilization did not influence the rate of nonunion, wrist flexion, grip strength, or pain, but patients immobilized in flexion had more trouble regaining extension
Cast Immobilization versus Operative Treatment
To date, six clinical trials have compared casting versus surgery for acute scaphoid fractures. They are presented here in chronological order from oldest to newest, with studies published in the same year introduced in alphabetical order, so as to remove any potential bias. The six studies in this order are: Saeden et al. (2001); Bond et al. (2001); Adolfsson et al. (2001); Dias et al. (2005 and a 2008 medium-term follow-up); McQueen et al. (2008); and Vinnars et al. (2008). (Table 2)
Table 2.
Randomized Controlled Trials comparing surgery and casting for treatment of acute scaphoid fractures.
| Study | Setting/Population | Treatment(Union rate; %) | Time to union/Return to work |
Duration of follow- up; Follow-up rate (%) |
|---|---|---|---|---|
| Saeden et al. (2001) |
Between 1984–1986 62 fractures randomized into two groups: 1) 30 treated with casting (C) 2) 32 treated with surgery(S) |
C: Short-arm cast from below the elbow to MCP joints of fingers and IP joint of thumb for 12 weeks (28/30; 93%) S: Volar approach with a Herbert screw then Colles' plaster cast for 2 weeks (31/32; 97%) |
Time to union not assessed Return to work (overall):* C: 15 weeks S:6 weeks Return to work (blue- collar workers):* C: 18 weeks S:7 weeks |
12 years (mean 11.7; range 10.2–12.8) Follow-up rate: Overall: 51/62 (82%) Casting: 26/30(87%) Surgery: 25/32 (78%) |
| Bond et al. (2001) |
Between 1997– 1998 25 fractures randomized into two groups: 1) 14 treated with casting (C) 2) 11 treated with surgery(S) |
C: Long-arm thumb-spica cast for 6 weeks then short-arm thumb-spica cast until fracture union (14/14; 100%) S: Percutaneous internal fixation with Acutrak screw then short-arm thumb-spica cast until fracture union (11/11; 100%) |
Time to union:* C: 12 weeks S:7 weeks Return to work:* C: 15 weeks S: 8 weeks |
24 months (mean: 25 months; range: 24-27 months) Follow-up rate not given |
| Adolfsson et al. (2001) |
Between 1996–1998 53 patients randomized into two groups: 1) 28 treated with casting (C) 2) 25 treated with surgery(S) |
C: Below-elbow plaster cast for 10 weeks (28/28; 100%) S: Percutaneous internal fixation with Acutrak screw then "thumb-to-elbow plaster splint" for 3 weeks (22/23; 96%) |
Time to union and Return to work not assessed |
16 weeks; Follow-up rate: Overall: 43/53 (81%) Casting: 24/28(86%) Surgery: 19/25 (76%) |
| Dias et al. (2005 and 2008) |
Between 1996–1999 88 patients randomized into two groups: 1) 44 treated with casting (C) 2) 44 treated with surgery (S) |
C: Below-elbow Colles' cast with thumb free for 8 weeks; if non-union detected at twelve weeks (10/44 [23%]) delayed fixation performed with casting for five to six weeks (42/44; 95%) S: Volar approach with Herbert screw then bulky bandage alone for 2 weeks (42/44) or bulky bandage + plaster volar splint for 6 weeks (2/44) (44/44; 100%) |
Time to union not assessed Return to work found to be roughly equal for both groups (5–6 weeks) |
2005 study: 52 weeks; 100% (Intention to treat analysis) 2008 study: 7.75 years (mean 93 months; range 73– 110 months) Follow-up rate: 71/88(81%) |
| McQueen et al. (2008) |
60 patients were randomized into two groups: 1) 30 treated with casting (C) 2) 30 treated with surgery (S) |
C: Below-elbow Colles' cast with thumb free for at least 8 weeks but no longer than 12 weeks (26/30; 87%) S: Percutaneous internal fixation with Acutrak screw using a volar approach; no post-surgical immobilization (29/30; 97%) |
Time to union:* C: 13.9 weeks S: 9.2 weeks Return to work/sports:* C: 11.4/15.5 weeks S: 3.8/6.4 weeks |
52 weeks Follow-up rate: 55/60(92%) |
| Vinnars (2008) |
Between 1992–1997 83 patients randomized into two groups: 1) 42 treated with casting (C) 2) 41 treated with surgery (S) |
C: Below-elbow cast for 6 weeks then radiographic assessment and recasting for 2–4 weeks if evidence of delayed healing (41/42; 98%) S: Various approaches with Herbert screw then dorsal plaster split with thumb free for 2 weeks then thumb-spica cast for an average of 3 weeks (41/41; 100%) |
Time to union and Return to work not assessed |
10 years (mean 10 years; range 8–13 years) Follow-up rate: Overall: 93% (75/81)† C: 35/40 (88%) S: 40/41(98%) |
p< 0.05;
2 patients died
In a study by Saeden et al., [14] 61 patients with 62 fractures were randomly allocated to receive either conservative treatment with a below elbow cast and the thumb immobilized (30 fractures) or open reduction and internal fixation using a Herbert bone screw (32 fractures). Operatively treated “blue-collar workers” took an average sick leave of 6 weeks compared to 15 weeks in casted patients. All fractures united. A 12-year follow-up the operatively treated group had a significantly higher incidence of radiographic scaphotrapezial osteoarthritis, although this finding was not correlated to patient symptoms.
Bond et al. [7] recruited 25 military personnel with non-displaced scaphoid waist fractures to be randomized to either immobilization in a long-arm cast with the thumb free or fixation with a percutaneous cannulated Acutrak screw (Acumed, Beaverton, Ore). The average time to fracture union and return time to work were shorter in those treated with screw fixation, but there were no differences in union rate, grip strength or motion at 2 year follow-up.
Adolfsson et al. [15] randomized 53 patients to either immobilization in a below-elbow plaster cast with the thumb immobilized for 10 weeks (28 patients) or percutaneous insertion of an Acutrak screw (25 patients). Operatively treated patients had significantly better motion 16 weeks after injury, but there were no differences in rate of union, time to union, final motion, or grip strength.
Dias et al. [16] randomized 88 patients to internal fixation with a Herbert screw or eight weeks immobilized in a functional below-the-elbow plaster cast with the thumb left free. The 8 and 12-week outcomes were better in the operatively treated patients, but there were no major differences detected greater than 12 weeks after injury. Union rate in the cast was 95% and with surgery was 100%. There was no difference between the two groups with respect to the time off work and ability to perform work tasks comfortably, probably because patients managed with the functional cast were advised to return to activity as soon as they wished. In the group treated surgically, there was a 30% complication rate (13/44 patients), but all the complications were minor and most were related to the scar. In a later evaluation of the patients from this trial, Dias et al. [17] noted more frequent dorsal intercalated segment instability in those treated non-operatively, but no difference in radioscaphoid osteoarthritis. They also noted that the outcomes of patients who required delayed fixation after initial non-operative treatment were comparable to the outcomes of those who had successful non-operative treatment.
McQueen et al. [18] randomized 60 patients to percutaneous fixation using a cannulated Acutrak screw (Acumed, Beaverton, Ore) (30 patients) or cast immobilization (30 patients). There was no difference in union rate and the operative group regained grip and pinch strength as well as ROM more quickly in the earlier stages of review but were not significantly different than the casting group at 1 year follow-up. Patients treated operatively returned to sports and work significantly earlier than those treated non-operatively.
Vinnars et al. [19] randomized 83 fractures to below-the-elbow scaphoid cast with the thumb included (42 patients) or operative treatment using a variety of approaches (41 patients). Ten years after the injury there were no significant differences in symptoms, motion, grip strength, or union, but many of the operatively treated patients had scaphotrapezial arthritis.
Systematic reviews of RCTs and Quasi-Randomized trials – Level II evidence
Yin et al. in 2007 [2] performed a systematic review and meta-analysis of randomized and quasi-randomized trials comparing casting and surgery f forfor treatment of non-displaced scaphoid fractures. After pooling this data, there was no significant difference in union rate or time to return to work, and any surgical benefits were noted to be transient. Complications were found to be much higher in the operatively managed group, but these complications were mostly minor.
Cost Analysis
Three groups have performed an economic analysis to ascertain the role of surgery and casting for the management of scaphoid fractures.
Davis and Chung [6] performed a cost-utility analysis of open reduction and internal fixation (ORIF) versus cast immobilization for acute non-displaced mid-waist scaphoid fractures. They used a decision analytic model to measure differences in quality of life and cost and used a web-based questionnaire to determine patient preferences. Direct costs were determined by Medicare payments and income loss was computed using average U.S. hourly wages obtained from the U.S. Bureau of Labor Statistics. They concluded that ORIF offered more quality-adjusted life-years and is less costly than casting ($7940 versus $13,851 per patient) because of a longer period of lost productivity with casting. These figures were calculated with the assumption that time off work would be about 0.17 (8.8 weeks) for surgery and 0.33 years (17.2 weeks) for casting. These probabilities were obtained from a wide variety of studies with various casting and surgical methods. When only considering direct costs incurred by Medicare reimbursement, casting was less costly than ORIF ($605 vs. $1747). As noted by the authors, the cost-utility analysis overestimates the indirect cost associated surgery because not all patients require absence from work during the entire duration of recovery.
Arora et al. [8] allocated patients to cast and surgery treatment groups, although there was no mention of randomization, therefore bringing into question the internal validity of the study. The group found a significant difference in immobilization time between the surgical and cast group (11 days versus 76 days) and a significantly shorter time off work (8 days vs. 55 days). However, the benefits of shorter time off work were balanced by the higher direct costs of surgery as suggested by the similar overall costs of surgery and casting. The authors reported a 19% complication rate (4/21 patients) with the operation, including one non-union, one superficial wound infection, and two instances of complex regional pain syndrome treated with physiotherapy and oral analgesics. Unfortunately, the costs of complications were not factored into the data.
In the trial of Vinnars et al. [20], total hospital costs were significantly lower with cast treatment than with surgery, and manual workers as a group had a longer time off work than non-manual workers (84 versus 16 days). Casting resulted in a substantially longer time off work in manual workers than surgical treatment (100 days versus 61 days) but resulted in no difference in time off work for non-manual workers.
Initially, surgery is more expensive than cast immobilization. Nevertheless, in a young working individual whose labor is hand-intensive, these early expenses can be offset by the gains in recovery time that will predictably reduce worker’s compensation costs. Therefore, if a patient is clearly dependent on hand function for income, surgery should be offered from a cost-savings point of view. In workers who can accomplish tasks with a cast or whose income is not intimately tied to immediate recovery of hand function, cast immobilization should be the treatment of choice based on economic rationales.
Shortcomings of the Evidence
Current best evidence does not confer clear-cut support for the use of either cast immobilization or surgery. Even among the six randomized controlled trials, the authors’ conclusions varied when considering patient age, occupation, surgical technique employed, type of cast used, costs, and short-term, medium-term, and long-term results. The rate of bone union for both procedures is greater than 90%, and detection of any significant differences between the two treatment options will likely require a high powered, multi-center clinical trial.
The Future
The next step in informing the debate between operative and non-operative treatment for non-displaced scaphoid waist fractures would be a large, multi-center clinical trial to address union rate, cost, and patient-rated outcomes (for example, patient satisfaction).
Current Concepts
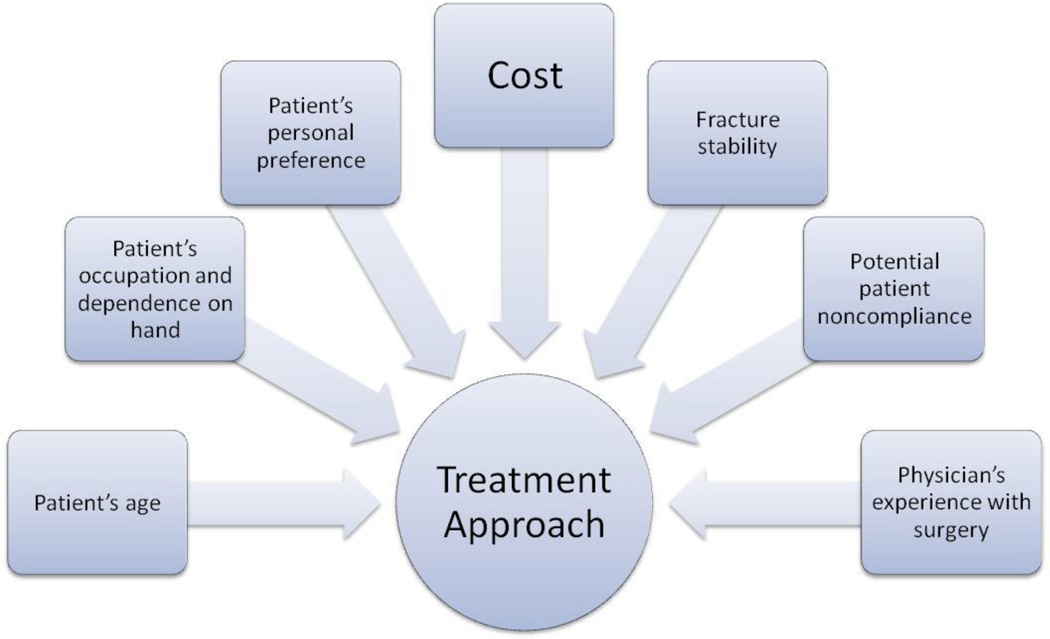
Both casting and surgery are reliable treatments for non-displaced scaphoid waist fractures, and the outcomes are comparable. Cast immobilization with the thumb free is less disabling and does not seem to prolong healing time or impair recovery. The cost effectiveness of operative treatment is debatable and, at best, favorable only in certain circumstances. The best approach to a patient with an acute non-displaced scaphoid waist fracture is to combine consideration of the individual’s unique circumstances with a well-reasoned algorithm.(Figure 1)
Figure 1.
Combining patient and physician factors with a focus on costs to arrive at the proper treatment approach.
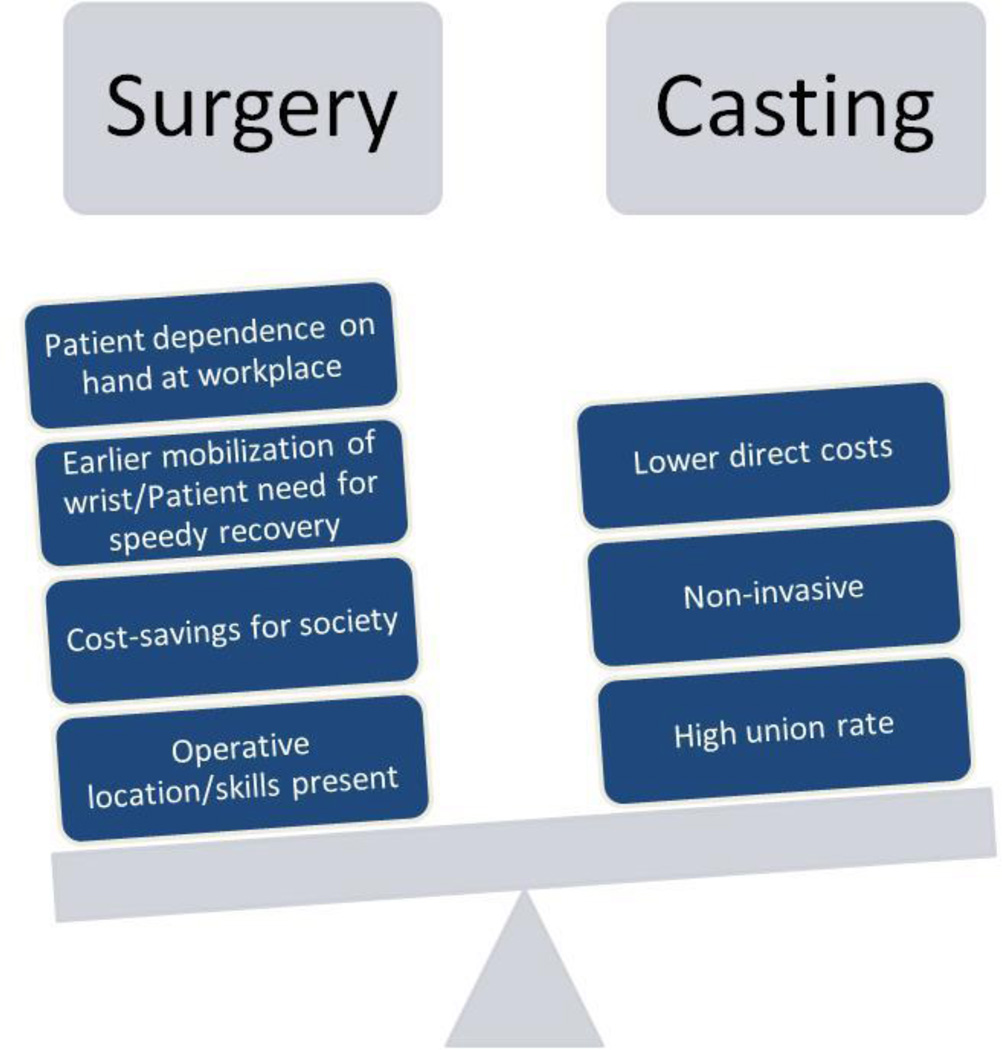
The intent of an economic analysis is to evaluate the impact of a treatment on society. Given a particular set of preconditions, surgery was found to be the dominant approach when viewed from the U.S. at large.[6] However, each clinician must carefully consider the needs of an individual patient that may tip the balance in favor of one treatment approach versus another. (Figure 2) Ultimately, patient needs and preferences appear to be the dominant factor in selecting treatment. I make use of a treatment algorithm similar to the “aggressive-conservative” approach advanced by Dias et al. [16, 17]. For a patient who requires earlier use of the hand because of work or sports participation, I will perform screw fixation using a limited 3 cm dorsal incision. For a patient who is averse to surgery or for whom earlier hand use is not a preference, I will fit a short-arm fiberglass cast that leaves the thumb free up to the metacarpophalangeal joint with the wrist in 20° of extension for 8 weeks. If fracture union is uncertain after 8 weeks, I image with a CT scan to look for signs of healing. If a gap is visualized, I offer operative treatment.
Figure 2.
Consideration of all factors in the hypothetical case tips the balance in favor of surgery.
Acknowledgements
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Kevin C. Chung).
References
- 1.Dias J, Brenkel I, Finlay D. Patterns of union in fractures of the waist of the scaphoid. J Bone Joint Surg Br. 1989;71(2):307–310. doi: 10.1302/0301-620X.71B2.2925752. [DOI] [PubMed] [Google Scholar]
- 2.Yin Z, Zhang J, Kan S, Wang P. Treatment of acute scaphoid fractures: systematic review and meta-analysis. Clin Orthop Relat Res. 2007;460:142–151. doi: 10.1097/BLO.0b013e31803d359a. [DOI] [PubMed] [Google Scholar]
- 3.Leslie I, Dickson R. The fractured carpal scaphoid. Natural history and factors influencing outcome. J Bone Joint Surg Br. 1981;63-B(2):225–230. doi: 10.1302/0301-620X.63B2.7217146. [DOI] [PubMed] [Google Scholar]
- 4.Slade J, III, Geissler W, Gutow A, Merrell G. Percutaneous internal fixation of selected scaphoid nonunions with an arthroscopically assisted dorsal approach. J Bone Joint Surg Am. 2003;85-A(Suppl 4):20–32. doi: 10.2106/00004623-200300004-00003. [DOI] [PubMed] [Google Scholar]
- 5.Rettig M, Kozin S, Cooney W. Open reduction and internal fixation of acute displaced scaphoid waist fractures. J Hand Surg [Am] 2001;26(2):271–276. doi: 10.1053/jhsu.2001.21524. [DOI] [PubMed] [Google Scholar]
- 6.Davis E, Chung K, Kotsis S, Lau F, Vijan S. A cost/utility analysis of open reduction and internal fixation versus cast immobilization for acute nondisplaced mid-waist scaphoid fractures. Plast Reconstr Surg. 2006;117(4):1223–1235. doi: 10.1097/01.prs.0000201461.71055.83. [DOI] [PubMed] [Google Scholar]
- 7.Bond C, Shin A, McBride M, Dao K. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83-A(4):483–488. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Arora R, et al. Fixation of nondisplaced scaphoid fractures: making treatment cost effective. Prospective controlled trial. Arch Orthop Trauma Surg. 2007;127(1):39–46. doi: 10.1007/s00402-006-0229-z. [DOI] [PubMed] [Google Scholar]
- 9.Kawamura K, Chung K. Treatment of scaphoid fractures and nonunions. J Hand Surg [Am] 2008;33(6):988–997. doi: 10.1016/j.jhsa.2008.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centre for Evidence-Based Medicine. Levels of Evidence. Available at: http://www.cebm.net/index.aspx?o=1025. [Last accessed: November 30, 2008].
- 11.Gellman H, Caputo R, Carter V, Aboulafia A, McKay M. Comparison of short and long thumb-spica casts for non-displaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989;71(3):354–357. [PubMed] [Google Scholar]
- 12.Clay N, Dias J, Costigan P, Gregg P, Barton N. Need the thumb be immobilised in scaphoid fractures? A randomised prospective trial. J Bone Joint Surg Br. 1991;73(5):828–832. doi: 10.1302/0301-620X.73B5.1894676. [DOI] [PubMed] [Google Scholar]
- 13.Hambidge J, et al. Acute fractures of the scaphoid. Treatment by cast immobilisation with the wrist in flexion or extension? J Bone Joint Surg Br. 1999;81(1):91–92. doi: 10.1302/0301-620x.81b1.9367. [DOI] [PubMed] [Google Scholar]
- 14.Saeden B, Tornkvist H, Ponzer S, Hoglund M. Fracture of the carpal scaphoid. A prospective, randomised 12-year follow-up comparing operative and conservative treatment. J Bone Joint Surg Br. 2001;83(2):230–234. doi: 10.1302/0301-620x.83b2.11197. [DOI] [PubMed] [Google Scholar]
- 15.Adolfsson L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilisation for undisplaced scaphoid waist fractures. J Hand Surg [Br] 2001;26(3):192–195. doi: 10.1054/jhsb.2001.0558. [DOI] [PubMed] [Google Scholar]
- 16.Dias J, Wildin C, Bhowal B, Thompson J. Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am. 2005;87(10):2160–2168. doi: 10.2106/JBJS.D.02305. [DOI] [PubMed] [Google Scholar]
- 17.Dias J, Dhukaram V, Abhinav A, Bhowal B, Wildin C. Clinical and radiological outcome of cast immobilisation versus surgical treatment of acute scaphoid fractures at a mean follow-up of 93 months. J Bone Joint Surg Br. 2008;90(7):899–905. doi: 10.1302/0301-620X.90B7.20371. [DOI] [PubMed] [Google Scholar]
- 18.McQueen M, Gelbke M, Wakefield A, Will E, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008;90(1):66–71. doi: 10.1302/0301-620X.90B1.19767. [DOI] [PubMed] [Google Scholar]
- 19.Vinnars B, Pietreanu M, Bodestedt A, af Ekenstam F, Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures. A randomized clinical trial. J Bone Joint Surg Am. 2008;90(6):1176–1185. doi: 10.2106/JBJS.G.00673. [DOI] [PubMed] [Google Scholar]
- 20.Vinnars B, Ekenstam F, Gerdin B. Comparison of direct and indirect costs of internal fixation and cast treatment in acute scaphoid fractures: a randomized trial involving 52 patients. Acta Orthop. 2007;78(5):672–679. doi: 10.1080/17453670710014383. [DOI] [PubMed] [Google Scholar]