Abstract
Aims
This study examined the association between the blood-sharing practice “flashblood” and demographic factors, HIV status, and variables associated with risky sex and drug behaviors among female injecting drug users. Flashblood is a syringe full of blood passed from someone who has just injected heroin to someone else who injects it in lieu of heroin.
Design
A cross-sectional study.
Setting
Dar es Salaam, Tanzania.
Participants
One hundred and sixty-nine female injecting drug users (IDUs) were recruited using purposive sampling for hard-to-reach populations.
Measurements
The association between flashblood use, demographic and personal characteristics and risky sex and drug use variables was analyzed by t-test and χ2 test. The association between flashblood use and residential neighborhood was mapped.
Findings
Flashblood users were more likely to: be married (p=.05), have lived in the current housing situation for a shorter time (p<.000), have been forced as a child to have sex by a family member(p=.007), inject heroin more in the last 30 days (p=.005), smoke marijuana at an earlier age (p=.04), use contaminated rinse-water (p<.03), pool money for drugs (p<.03), and share drugs (p=.00). Non-flashblood users were more likely to live with their parents (p=.003). Neighborhood flashblood use was highest near downtown and in the two next adjoining suburbs and lowest in the most distant suburbs.
Conclusions
These data indicate that more vulnerable women who are heavy users and living in shorter term housing are injecting flashblood. The practice of flashblood appears to be spreading from the inner city to the suburbs.
Keywords: substance use, women, HIV/AIDS, risk behavior, Africa
Introduction
Heroin injection has become commonplace in some East African cities since the late 1990s[1-6]. There is strong evidence that large numbers of injecting drug users (IDUs) are engaging in needle sharing and sexual behaviors known to transmit HIV. Studies conducted in Dar es Salaam, Tanzania, indicate that almost half of IDUs may be HIV-positive[7-9]. HIV infection among IDUs may potentially derail Tanzania's HIV control efforts; by 2005 HIV seroprevalence at the national level had dropped to 7%[10].
New unsafe injecting practices emerge as drug users respond to changing socioeconomic and political forces that periodically alter the amount, quality, and cost of drugs available. During 2005, a new blood-sharing practice, “flashblood,” emerged among female IDUs in Dar es Salaam[11]. Flashblood is a syringe full of blood drawn back immediately after initial injection that is passed to a companion to inject. Those practicing flashblood believe that the syringe full of about 4cm3 of such blood contains enough heroin to avoid the pains of withdrawal. Flashblood is distinct from back- or frontloading; there is an intention to inject a large amount of blood. With back- or frontloading, the presence of blood is usually minimal and a byproduct of the method of transferring drug. Female IDUs described flashblood as an altruistic practice meant to help out an IDU who failed to procure heroin herself.
The practice of flashblood emerged as the cost of heroin increased and policing of drug users activities increased[2]. More successful female IDUs, who were sex workers still able to attract customers, began accommodating women in more desperate circumstances by providing them with flashblood[11]. By 2006, the practice had spread to Zanzibar, two islands (Unguja and Pemba) off the coast of mainland Tanzania, where 9% of the male IDUs in a study (n= 200) reported using flashblood[3].
Both the use of flashblood in Tanzania and the new practice of the creation of an injection sac in the groin by young IDUs in Vietnam[12] emerged at times when IDUs felt pressure to manage their addictions more efficiently. The injection sac is a soft tissue portal to a vein created by repeatedly inserting a hypodermic needle into a specific site on the skin surface. These two innovations, flashblood in Tanzania and the injection sac in Vietnam, demonstrate the extreme lengths IDUs will use to maintain their injecting practice. Both Tanzanian and Vietnamese IDUs faced socioeconomic hardships and political pressure to limit their drug-related activities. Most of the female IDUs in Tanzania are also sex workers who have lost the social support of their families.
Personal experiences, demographic factors, and participation in other risky drug and sexual practices may predict who may be more at risk for injecting a syringe of someone else's blood. Several studies have found that experiences of sexual and physical trauma are linked to substance use[13-20]. Others have found poor social support systems and financial insecurity are linked to HIV seropositivity[21,22]. We hypothesized that vulnerable women who were the poorest and most marginalized would be the most likely to use flashblood.
HIV and HIV Services in Tanzania
Approximately 34.5 million Tanzanians live in an area roughly the size of California [23]. It is estimated that Christians and Muslims each compose 30% to 40% percent of the population and that the remaining population claims no religious affiliation or a traditional religion[24]. The multiethnic population of the economic capital, Dar es Salaam, numbered 2.5 million by 2002 with an average household size of 4.2[23].
During 1997, the voluntary HIV testing and counseling (VCT) program began in earnest, with 73 trained counselors; by 2005 over 1200 trained counselors worked at 521 sites[25]. During 2000 increased attention to HIV/AIDS led to the creation of the Tanzanian Commission for AIDS (TACAIDS), followed by the Development of HIV/AIDS Policy in 2001 and the creation of the National Multi-Sectoral Strategic Framework (2003-2007) that resulted in the Development of a Health Sector Strategy on HIV/AIDS and a National Care and Treatment Plan, which was approved in 2003. Ninety-six care and treatment sites were created in 2004-2005 and another 104 facilities started in 2005-2006. By December 2006, 125,139 Tanzanians were enrolled in Care and Treatment Centers and 60,341 were on antiretrovirals (ARVs)[25]. By 2005 the cumulative number of reported AIDS cases in Tanzania was 205,773. Of those, 28,474 were from the Dar es Salaam Region.
Modes of transmission in sub-Saharan Africa have primarily been attributed to heterosexual contact. In Tanzania, heterosexual transmission of HIV accounted for 82% of the reported AIDS cases in 2005. Blood transfusion (1.5%) and maternal-to-child transmission (4%) explained another 5% of transmission of HIV in AIDS cases. The remaining 13% of the AIDS cases did not state the mode of transmission[25]. During 2005, 217,116 Tanzanians who had never used VCT services sought to learn their HIV status. Of those testing in health clinics 27% were HIV-positive. In contrast, 11% of those testing at sites not affiliated with a health clinic were HIV-positive. Seroprevalence was higher among women (76% vs. 16 %) [25]. At the non-health clinic VCT sites in Dar es Salaam, HIV seropositivity ranged from 7% to 18% with women testing between two to five times higher than men at each of the sites[25].
Harm reduction in Tanzania
Since the late 1990s, harm reduction strategies in Tanzania have included: 1) outreach; 2) information, education and communication; 3) risk reduction counseling; 4) HIV testing and counseling; and 5) detoxification programs[26]. VCT and the provision of antiretrovirals to those IDUs who need them are being introduced in Dar es Salaam and Zanzibar during 2008 and 2009. No opioid substitution programs are currently available to the general public. There are no needle exchange programs in Tanzania. Needle and syringe packets are sold at pharmacies for the equivalent of approximately US$0.10. Individuals are reluctant to carry needle and syringe packages because they will be targeted by police. Police do not target them at the point of purchase at a pharmacy, instead they focus on places where users congregate and inject.
One non-governmental organization (NGO) has been operating a three month detox and rehabilitation in-patient service for several years in the coastal town of Tanga that some injectors in Dar es Salaam report utilizing. Otherwise, the harm reduction measures specifically focused on IDUs are primarily government initiatives instituted by the Drug Control Commission of Tanzania in cooperation with Muhimbili National Hospital, Muhimbili University Health and Allied Sciences (MUHAS), the Tanzania Commission on AIDS, and the United States Government's Centers for Disease Control. Community-based organizations and NGOs are emerging to focus on the needs of IDUs. Several of these organizations began working together with the Tanzanian and U.S. University and community advisors to provide VCT and antiretroviral referral to IDUs during 2009 as part of a PEPFAR initiative.
At the time of data collection the harm reduction being offered by our study was VCT and referral to Muhimbili Medical Center for free detoxification. In addition, we emphasized the need to use a new needle with every injection and noted that those who did share works needed to bleach syringes to actually eliminate HIV. A pamphlet was available that detailed the bleach disinfection process.
Emerging risks and the environment
The risk of flashblood did not emerge in a vacuum. After the introduction of structural adjustment policies (SAPs) in the latter half of the 1980s, the economy was liberalized and a free market system established. Along with increasing connectedness to world markets came both licit and illicit opportunities for profit. Tanzania was first only a transit site for drug traffickers moving heroin from Asia to Europe and the U.S., then a local client base developed. As an illicit drug market developed and HIV/AIDS cases increased some of the main features of the SAPs were established. Almost overnight the Tanzanian shilling was devalued and government spending on health and education was dramatically reduced. Literacy rates dropped dramatically during the 1990s as measures for health indicators also declined. With limited educational opportunities and few job prospects, urban Tanzanian youth immersed themselves in ideas, trends and practices made increasingly available through globalization. Tanzanian hip hop, Bongo flava, is one manifestation of those connections; heroin is another. Heroin was cheap and available, education and jobs were not.
In this new millennium, many families endure extreme poverty. The AIDS crisis and increasing corruption strip families, communities and state structures of the resources needed to address basic individual needs and human rights[27-29]. Youths increasingly engaged in street life describe hunger, poverty, lack of housing and social support, and abuses ranging from neglect to sexual abuse [30,31]. Little data exists on child sexual abuse in Tanzania. One study among a relatively privileged educational sample of youths, Tanzanian university students, found 28% reported child sexual abuse[32]. Another study conducted in 11 Tanzanian regions noted child sexual abuse accounted for 29% of the types of childhood abuse[33]. Recently, a researcher comparing university students and survival sex workers found vulnerability caused by extreme deprivation to be the most likely explanation for differences in young women's childhood sexual abuse experiences[30]. The economic crisis, devastation wreaked on families by the AIDS crisis, and growing substance abuse are affecting the health of many families and youths. The limited mental health services available in the country are seeing increasing numbers of youths attempting suicide, requesting substance abuse rehabilitation, and other in- and out-patient services[27-29].
In the U.S. between one-third and one-half of the female IDUs report experiencing child sexual abuse[17,18]. In Vancouver, 33% of female IDUs[19] and 32% of street-involved youths reported child sexual abuse[20]. The term child sexual abuse is not well defined in the literature and a range of experiences are included in its measurement complicating our understanding of the problem[18]. There is growing awareness that the association between childhood sexual abuse and high risk sexual and substance use among adolescents and adults is mediated by experiences of depression and post-traumatic stress disorder[17,18,20,34]. In this study women were asked specifically about incest. We do not know about any other experiences of child sexual abuse the study participants endured.
In this article we explore the variables related to flashblood use to determine if particular demographic, personal experiences, or risk behaviors are associated with its practice. By determining who may be at most risk of engaging in this practice, we can design evidenced-based interventions to reduce and eliminate its practice. This study was conducted among the women of Dar es Salaam, Tanzania, who created the practice of flashblood.
Methods
Study population
We conducted a cross-sectional HIV behavioral survey along with onsite VCT to understand IDUs' practices and risk behaviors in Dar es Salaam, Tanzania. One hundred sixty-nine women interviewed were asked about flashblood use and 28 (17%) reported ever using it. This paper focuses on these women's demographic data, personal experiences, and risk-taking behaviors as it examines flashblood use.
Procedures
We collected data in Dar es Salaam, Tanzania, between May 2005 and September 2006. We recruited IDUs into the study using information from key informants. We targeted neighborhoods for sampling based on interviews with drug users residing there and the information from our outreach worker who had directly observed injection drug use. The outreach worker contacted IDUs for this study and referred them for screening. Those referred were asked to contact other IDUs and refer them to the study.
IDUs were asked to participate in a brief screening questionnaire to determine their eligibility. We read the screening questionnaires and the study questionnaire to each participant. We required that participants be at least 18 years old, have injected heroin during the 48 hours before our screening, and have engaged in sex at least one time during the 30 days before screening. We confirmed reports of injection drug use by needle track markings. We did not examine body parts covered by clothing, other than extremities or neck. Of the 559 IDUs screened, 534 were eligible and agreed to participate in the study. Those not meeting eligibility criteria, included 18 who had been sexually abstinent during the last 30 days, six who had not injected during the last 48 hours, and one unwilling to undergo VCT.
IDUs eligible for the study were provided complete information about the study and asked for informed consent. Because heroin use is an illegal activity in Tanzania, IDUs are not willing to sign consent forms and do not want to carry a copy of one. Those willing to be in the study verbally consented to participate. Once consent was provided, participants went through VCT, provided a blood specimen, and were interviewed. The data collection site near the city center was in a rented duplex. Trained research assistants interviewed respondents. The interview took about one hour. Participants were provided with 3,000 Tanzanian shillings (∼$3 US), to compensate them for their time.
University committees for the protection of human subjects in the United States and Tanzania reviewed and approved all procedures and data collection forms. The Tanzania Commission for Science and Technology and the Tanzanian National Institute for Medical Research reviewed and approved the study guides and materials.
Measures
We developed the Tanzanian AIDS Prevention Project Questionnaire using items similar to those we use in our U.S. studies with drug users. We translated the questionnaire items from English into Swahili and had the Swahili version independently back-translated from Swahili into English. The investigators and translators resolved the inconsistencies in translations through detailed discussions of culturally specific meanings and the intent of the question and measure. Studies conducted in various international settings found that similar questionnaire items to those we used in the questionnaire produce responses that are both valid and reliable.
The domains we discuss in this paper include demographic and risk-related experiences and behaviors. We measured residency with parents, marital status, income, perception of being homeless, months lived in present place, and HIV seropositivity. We measured the age of first use for: alcohol, marijuana, and heroin. We asked if they were “ever forced as a child to have sex with a family member” (yes/no) and if they had ever traded sex for drugs (yes/no). We recorded the times they had injected drugs in the last 30 days and the number of times they used heroin in the last seven days. We measured the times they had used a new needle, a used needle, and the number of times they used contaminated rinse water. We also measured the times they had pooled money for drugs, the times they had shared/begged drugs, the times they injected with partner 1, in the last 30 days and the times injected with that same partner in the last 7 days.
Flashblood use was measured by the question “Have you ever injected flashblood/mixed blood?” (yes/no). Using this as the dependent variable, analyses were carried out on demographic and drug use variables in the female sample. For continuous data, analyses were by t-test and for categorical data, by χ2 test in SPSS version 15. Qualitative interviews conducted during the survey revealed that flashblood had emerged and we added it to our questionnaire. This question was added to the questionnaire during the fifth month of data collection. Of the 249 women in the data set, 68% (n=169) were asked about flashblood use and only these 169 women will be discussed in this article.
Results
The sample of 169 women had a mean age±SD of 25.6±5.5, had started using heroin at mean age 19.5±4.0, and first injected at 22.8±5.1 years: 77% were single. Most (77%) traded sex for money as their main form of income, 28% considered themselves homeless, 41% lived with their parents, 32% described themselves as Christian and 68% Muslim, and modal income category (for 31%) was 150,000-199,999 shillings (about $US 150-200) per month. Within the past 24 hours of the interview, 78% of women had traded sex for money. Data are presented in Table 1.
Table 1.
Descriptive Statistics for Female IDUs in Dar es Salaam, Tanzania (n=169)
| Variable | Mean±SD |
|---|---|
| age | 25.6±5.5 SD |
| age started using heroin | 19.5±4.0 SD |
| age first started injection | 22.8±5.1 SD |
| % | |
| single | 77% |
| traded sex for main income | 77% |
| considers self homeless | 28% |
| lives with parents | 41% |
| Christian | 32% |
| Muslim | 68% |
| Modal income 150,000-199,999 shillings ($US 150-200)/mo | 31% |
| Traded sex for money, last 24hrs | 78% |
| HIV + | 66% |
Twenty-eight (16.6%) of the 169 women had used flashblood. HIV status did not differ significantly between flashblood users and nonusers in general, over 64% of all female IDUs were positive. Flashblood users, however, were more likely to be married or cohabiting (39%) than nonusers (20%) (χ2=3.4, df=1, p=.05) and of the 11 flashblood users who were married, nine (82%) were HIV-positive, of the 17 who were not married or cohabiting, nine (53%) were HIV-positive.
Flashblood users were more likely to consider themselves homeless than non-flashblood users, but this was not statistically significant. However, where they lived and how long they had lived there were statistically significant variables. Flashblood users were more likely to live in someone else's room or house (43%) than nonusers who mostly lived with their parents (46%). Except in the case of childhood incest (χ2=8.3, df=1, p=.007), there was no difference between flashblood users and nonusers in their experiences of interpersonal violence. Flashblood users were more likely to have lived in their present abode for a far shorter time than nonusers (69 vs. 128 months), to have used heroin significantly more in the past seven and 30 days, and to have initiated use of marijuana at an earlier age (16.8 vs. 17.4 yrs). Results are in Table 2.
Table 2. Variables discriminating Flashblood users and nonusers.
| Variable Flashblood | Mean±SD No (n=141) |
Mean±SD Yes (n=28) |
sig |
|---|---|---|---|
| Months lived in present place | 117.0±128.2 | 69.2±94.1 | .000 |
| Age first used alcohol | 17.4±3.7 | 17.4 ±2.5 | .15 |
| Age first time smoked marijuana | 17.5±3.7 | 16.8±2.5 | .04 |
| Age first used heroin | 19.7±4.1 | 18.6±3.5 | .37 |
| Times injected drugs last 30 days | 89.5±21.7 | 102.6±26.9 | .005 |
| Times used heroin last 7 days | 20.7±4.9 | 24.1±6.7 | .003 |
| Risk behavior as percentage of # times injected in the last 30 days | |||
| Times used new needle | 97% | 94% | .34 |
| Times used used needle | 3% | 6% | .30 |
| Times used used rinsewater | 2% | 8% | .03 |
| Times pooled money for drugs | <1% | 3% | .03 |
| Times shared/begged drugs | <1% | 2% | .00 |
| Times injected with partner 1, last 30 days | 78% | 85% | .16 |
| Times injected with partner 1 last 7 days | 19% | 20% | .66 |
| Variable | % | % | sig |
| Married | 20% | 40% | .05 |
| Considers self homeless | 25% | 43% | .06 |
| HIV seropositive | 67% | 64% | .80 |
| Lives with parents | 46% | 14 % | .003 |
| As a child forced to have sex with family member | 21% | 46% | .007 |
| Ever trade sex for drugs | 20 % | 36% | .08 |
| Income under 150,000 shillings/month | 53% | 68% | .15 |
(all df=1)
In our examination of risk behavior as a percentage of times injected in the last 30 days, on average, flashblood users were a little more than twice as likely to have used a contaminated needle and syringe compared to non-flashblood users (3% vs. 6%) (p=.30). They were also a little more likely than nonusers to have injected with their last sexual partner (78% vs. 85%), but this was not significant either (p=.16). In terms of other blood-borne pathogen risk behaviors, the flashblood users were four times more likely to have used contaminated rinsewater than non-flashblood users (p=.03). They were also three and a half times more likely to have pooled money for drugs (p=.03) and twice as likely to have shared or begged drugs (p=.00)
All flashblood users had traded sex for money, as had 90% of the nonusers. More flashblood users had traded sex for drugs (36%) than non-flashblood users (25%), but this was not statistically significant. More Christian women (24%) than Muslim women (13%) reported flashblood use, but this was not statistically significant. Neither was there a significant difference in income categories split at the median category (150,000 shillings ∼US$150./month), between flashblood users and nonusers (χ2=2.2, df=1, p=.15).
Neighborhood flashblood use ranged from 25% near the ferry, in the area around the harbor, to 19 to 22% in the market area where large scale heroin use first emerged (Kariakoo) and in the two next adjoining suburbs closest to town (Magomeni and Kinondoni). In Manzese, the next suburb west, adjacent to Magomeni, 17% of the female injectors used flashblood. The neighborhoods furthest from the main roads going southwest and west had the lowest numbers of flashblood users, 12% (Temeke) and 4% (Kimara) respectively (Figure 1).
Figure 1.
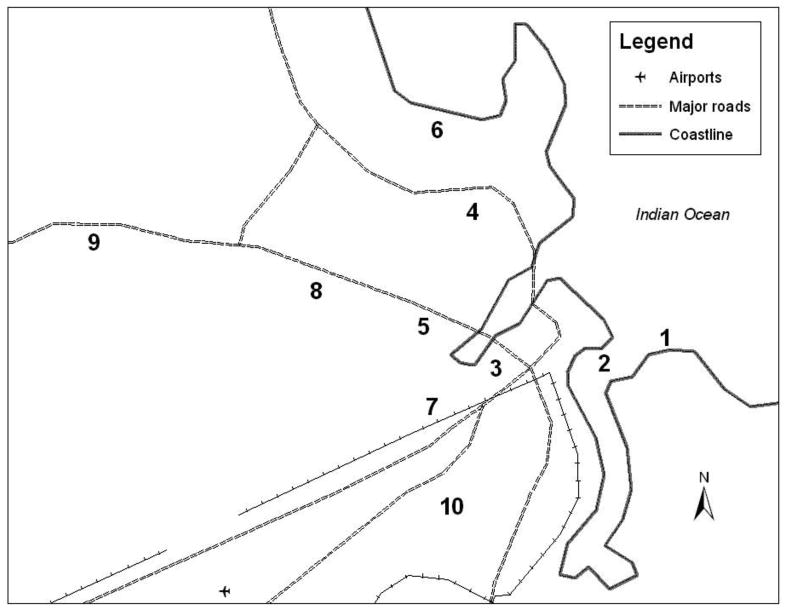
Location of Neighborhoods
1 - Harbor
2 - Kigamboni Ferry
3 - Kariakoo
4 - Kinondoni
5 - Magomeni
6 - Msasani
7 - Buguruni
8 - Manzese
9 - Kimara
10 - Temeke
Discussion
This study, while based on a relatively small sample of female IDUs in urban East Africa, offers us the first quantitative look at the phenomenon of flashblood use from Dar es Salaam, Tanzania. Our data found that 28 (17%) of the 169 women had used flashblood. Three variables significantly associated with flashblood use were indicative of vulnerability: short time in the current living arrangement, not living with their parents, and being forced to have sex by a family member. Being married or cohabiting was also significantly associated with flashblood use. Flashblood users who were married or cohabitating may have been more likely to use flashblood for several reasons. First, their partners might control and limit their money; secondly, their partner might have used her money or heroin; and third, if their partner had abandoned her or was in prison, she might have limited resources. As a married woman, whose partner was in prison or had abandoned her because of his or her own drug use, she might not initially have the same social support that other female IDUs living together do.
Not living with one's parents could indicate a break with the natal home and the loss of support that goes with estrangement from home. This estrangement and vulnerability might be associated with some women's short periods of time in their current living situation. Experiencing childhood sexual abuse is often associated with increased drug and sexual risk-taking [13-20]. Sexual abuse by a family member is especially likely to lead a young woman to leave home and the lack of social support and stable housing may lead to involvement in precarious situations and risky practices[137,14].
The younger age of initiation into marijuana use among flashblood users may be indicative of opportunity in their environment and a tendency to participate in risky behaviors. Marijuana might have also been the first substance they used to mediate depression or PTSD. Alcohol may not have mattered as much because of the influence of Islam in this community and the fact that it is less socially acceptable for women to imbibe alcohol than it is for men.
It is the heaviest heroin users, based on reported use in the past month and past week, who were most likely to use flashblood. We found no association with income and flashblood use. Flashblood users made as much money in a month as other female IDUs and this may explain why they were more likely to have used a new needle. They were more likely to have engaged in every behavior associated with injection perhaps because they injected the most heroin. The norm for female IDUs in Dar es Salaam is to inject with a new needle[5]. However, when they deplete their resources and become desperate, they resort to sharing, begging, and injecting flashblood. Flashblood users' higher heroin consumption needs put them at a greater risk of going through withdrawal when they cannot satisfy the demands of their habit.
From a western perspective, a degree of desperation might be suggested by the fact that flashblood users were significantly more likely to have pooled money for drugs, shared or begged drugs, and shared works with others. The tendency to share all resources may be more of a cultural phenomenon demonstrating the value of sharing and building community among a highly marginalized and stigmatized group. It might also indicate some women are being driven by some compulsion to continually use. Clearly this needs to be explored in future studies.
The greater use of heroin by flashblood users might be indicative of self-medication related to depression or post-traumatic stress disorder that other authors indicate may be pathways linking childhood sexual abuse to adult drug and sexual risk-taking practices[17,20]. We do not have measures of depression or post–traumatic stress disorder that could perhaps explain more of the relationship between forced sex by a family member as a child and flashblood. Neither do we have more general data about childhood sexual abuse outside of the family. These data would have helped demonstrate similarities and differences between IDUs and other populations[17].
The link between flashblood users and the givers is another area to consider. What motivates an IDU to offer their blood? Though the practice was originally described as altruistic, the women are aware that blood-sharing practices can be lethal in the long term. While perhaps unaware of blood incompatibility issues, Tanzanian IDUs are acutely aware of the blood-borne pathogens circulating in dirty needles and syringes. Women in particular take care to use new needles to avoid acquiring any diseases. Why then are they driven to share? The most apparent explanation for givers offering their blood is the relationship between the user and giver and the culture of sharing. Many of the female IDUs live together, work together, and inject together [1]. They create new social networks of reciprocity and obligation that function to support them outside the networks of family and clan. As children Tanzanians are socialized to share. One of the first things a baby is taught once they can grasp an object is that s/he should return it[30]. Giving is a very important part of the culture. Some groups of IDUs even operate as brotherhood associations keeping track of the members of their group and tracking in a notebook the contributions that each makes to the funeral arrangements of one of their colleagues [McCurdy fieldnotes]. In the context of scarcity, poverty, and pain, the relief and gratitude associated with sharing today trumps concerns about the consequences that may follow tomorrow.
As found in earlier work about neighborhood effects and HIV, flashblood use is associated with neighborhoods[9]. The areas where IDUs have congregated for longest periods of time are where we find more flashblood users. Diffusion of innovation may partly explain why Kinondoni has the most flashblood users, since this area is known for being trendsetting and attracts those interested in fads and fashion. It had perhaps, not been long enough at the time of the study for the practice to have moved to more distant suburbs.
These data indicate women who were forced to have sex by a family member as a child, those using most heavily, and those who live in neighborhoods with longer histories of injection use who are engaging in flashblood practice. It appears that flashblood is associated with both the desperation and pains of withdrawal among heavier using female IDUs; with a community cohesion among sex workers; with the spread of risky practices from the inner city to the suburbs; and with a combination of folk wisdom and placebo effect to counter withdrawal symptoms. It could also be that some of these flashblood users are resilient women who survived childhood traumas. Their flashblood use may be a way they attempt to survive and manage mental health issues and day-today survival through self-medication. We do not know how their heroin use may be related to depression or PTSD.
The women who initially told us about flashblood during in-depth face-to-face interviews were matter of fact about the practice and explained its emergence as a survival strategy women created to help each other out. Flashblood givers and users believe there is enough heroin in the syringe of blood to help the flashblood user avoid withdrawal. After injecting flashblood, users nod off as if they have injected heroin and they do not experience withdrawal. Perhaps, for some, believing in flashblood is just one more way to manage a life where survival sex, extreme poverty, loss of family support, and violence on the street are the norm.
As drug users become more desperate they create ever more complex ways to manage their addictions and new emerging practices threaten to escalate the AIDS epidemic. Since 2005 flashblood in Tanzania and the soft tissue portal, an injection sac, among young IDUs in Hanoi, Vietnam, are innovations IDUs created in response to threats to their survival. In turn, these practices threaten to escalate the spread of HIV and other blood-borne pathogens[2,11,12]. Both innovations emerged from desperation as urban drug users maneuvered to manage addictions in the face of all attempts to repress drug use.
Dahoma et al. [3] note that flashblood is not only a coping mechanism to sustain a drug habit; it has the potential to fuel a new wave of the HIV epidemic in Tanzania. HIV prevention efforts will need to incorporate specific responses to this new phenomenon and in attempts to stop the practice of flashblood, contain its spreading use and manage its aftereffects. The factors that led to the emergence of flashblood need to be investigated and discussed so that the relationship between risky practices, the social environment, and repressive policies are better understood and negotiated. Interventions designed to reduce the practice of flashblood must address the vulnerability of the users and provide options that include treatment and the provision of social services. There is a great need for evidence-based treatment services and prevention interventions.
Acknowledgments
This study was supported by a grant from the National Institute on Drug Abuse, “Tanzania AIDS Prevention Project” NIDA R21 DA19394. This publication was supported (in part) by the Baylor-UTHouston Center for AIDS Research (CFAR), an NIH funded program (AI036211). We thank Stella Mujaya, Samuel Kiore, Mary Anderson Mbwambo, Brown Emmanuel, Doris Msuali, Charles Msumari, Samuel Mduma, Dr. Sandra Timpson, and Dr. John Atkinson for their assistance in data collection, management, and analysis. We thank Patrick Courtney for his assistance creating the map and legend.
References
- 1.McCurdy S, Williams ML, Kilonzo GP, Ross MW, Leshabari MT. Heroin and HIV risk in Dar es Salaam, Tanzania: Youth hangouts, mageto and injecting practices. AIDS Care. 2005;17:S65–S76. doi: 10.1080/09540120500120930. [DOI] [PubMed] [Google Scholar]
- 2.McCurdy S, Kilonzo GP, Williams M, Kaaya S. Harm reduction in Tanzania: An urgent need for multisectoral intervention [editorial] Int J Drug Policy. 2007;18:155–159. doi: 10.1016/j.drugpo.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Dahoma MJU, Salim AA, Abdool R, Othman AA, Makame H, Ali AS, Abdalla A, et al. HIV and substance abuse: The dual epidemics challenging Zanzibar. Afr J Drug Alcohol Stud. 2006;5:129–138. URL: http://www.crisanet.org/ajdas_vol5_num2.html. [Google Scholar]
- 4.Beckerleg S, Hundt GL. The characteristics and recent growth of heroin injecting in a Kenyan coastal town. Addict Res Theory. 2004;12:41–54. doi: 10.1080/16066350410001646605. [DOI] [Google Scholar]
- 5.Deveau C, Levine B, Beckerleg S. Heroin use in Kenya and findings from a community based outreach programme to reduce the spread of HIV/AIDS. Afr J Drug Alcohol Stud. 2006;5:95–107. URL: http://www.crisanet.org/ajdas_vol5_num2.html. [Google Scholar]
- 6.Reid S. Injection drug use, unsafe medical injections, and HIV in Africa: a systematic review. Harm Reduct J. 2009;6:24. doi: 10.1186/1477-7517-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Timpson S, McCurdy S, Leshabari MT, Kilonzo G, Atkinson J, Msami A, Williams ML. Substance abuse, HIV risk and HIV/AIDS in Tanzania. Afr J Drug Alcohol Stud. 2006;5:157–169. URL: http://www.crisanet.org/ajdas_vol5_num2.html. [Google Scholar]
- 8.Williams M, McCurdy S, Atkinson J, Kilonzo G, Leshabari MT, Ross M. Differences in HIV risk behaviors by gender in a sample of Tanzanian injection drug users. AIDS Behav. 2007;11:137–44. doi: 10.1007/s10461-006-9102-x. [DOI] [PubMed] [Google Scholar]
- 9.McCurdy S, Ross M, Kilonzo G, Leshabari MT, Williams M. HIV/AIDS and injection drug use in the neighborhoods of Dar es Salaam, Tanzania. Drug Alcohol Depend. 2006;82:s23–s27. doi: 10.1016/S0376-8716(06)80004-9. [DOI] [PubMed] [Google Scholar]
- 10.National AIDS Control Programme. HIV/AIDS/STI Surveillance Report, January-December 2005, Report No 20, issued March 2007. United Republic of Tanzania, Ministry of Health and Social Welfare; Tanzania Mainland: [Google Scholar]
- 11.McCurdy SA, Williams ML, Ross MW, Kilonzo GP, Leshabari MT. New injecting practice increases HIV risk among drug users in Tanzania. BMJ. 2005;331:778. doi: 10.1136/bmj.331.7519.778-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clatts MC, Giang LM, Goldsamt LA, Yi H. Novel heroin injection practices: Implications for transmission of HIV and other bloodborne pathogens. Am J Prev Med. 2007;32:s226–s233. doi: 10.1016/j.amepre.2007.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dickson-Gomez J, Bodnar G, Gueverra A, Rodriguez K, Gaborit M. Childhood sexual abuse and HIV risk among crack-using commercial sex workers in San Salvador, El Salvador: a qualitative analysis. Med Anthropol Q. 2006;20:545–574. doi: 10.1525/maq.2006.20.4.545. [DOI] [PubMed] [Google Scholar]
- 14.Medrano MA, Zule WA, Hatch J, Desmond DP. Prevalence of childhood trauma in a community sample of substance-abusing women. Am J Drug Alcohol Abuse. 1999;25:449–462. doi: 10.1081/ada-100101872. [DOI] [PubMed] [Google Scholar]
- 15.Simoni JM, Sehgal S, Walters KL. Triangle of risk: Urban American Indian women's sexual trauma, injection drug use, and HIV sexual risk behaviors. AIDS Behav. 2004;8:33–45. doi: 10.1023/b:aibe.0000017524.40093.6b. [DOI] [PubMed] [Google Scholar]
- 16.Wilsnack SC, Vogeltanz ND, Klassen AD, Harris R. Childhood sexual abuse and women's substance abuse: National survey findings. J Stud Alcohol. 1997;58:264–271. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]
- 17.Plotzker R, Metzger D, Holmes W. Childhood sexual and physical abuse histories, PTSD, depression and HIV risk outcomes in women injecting drug users: A potential mediating pathway. Am J Addict. 2007;16:431–438. doi: 10.1080/10550490701643161. [DOI] [PubMed] [Google Scholar]
- 18.Senn T, Carey M, Vanable P. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: Evidence from controlled studies, methodological critique, and suggestions for research. Clin Psychol Rev. 2008;28:711–735. doi: 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braitstein P, Li K, Tydall M, Spittal P, O'Shaughnessy M, Schilder A, Johnston C, Hogg R, Schechter M. Sexual violence among a cohort of injection drug users. Soc Sci Med. 2003;57:561–569. doi: 10.1016/s0277-9536(02)00403-3. [DOI] [PubMed] [Google Scholar]
- 20.Stolz J, Shannon K, Kerr T, Zhang R, Montaner J, Wood E. Associations between childhood maltreatment and sex work in a cohort of drug-using youth. Soc Sci Med. 2007;65:1214–1221. doi: 10.1016/j.socscimed.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Metsch LR, McCoy CB, McCoy HV, Shultz J, Inciardi J, Wolfe H, et al. Social influences: Living arrangements of drug using women at risk for HIV infection. Women Health. 1998;27:123–136. doi: 10.1300/J013v27n01_08. [DOI] [PubMed] [Google Scholar]
- 22.Humphrey JH, Nathoo KJ, Hargrove JW, Iliff PJ, Mutasa KE, Moulton LH, et al. HIV-1 and HIV-2 prevalence and associated risk factors among postnatal women in Harare, Zimbabwe. Epidemiol Infect. 2007;135(6):933–42. doi: 10.1017/S0950268806007709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sensa ya watu na makazi ya mwaka 2002. Tanzania Sensa 2002. [8 March 2010]. Available at: http://www.tanzania.go.tz/sensa/dsm.htm.
- 24.Bureau of Democracy, Human Rights, and Labor, 2007. International Religious Freedom Report 2007. [15 September 2008]. at: http://www.state.gov/g/drl/rls/irf/2007/90124.htm.
- 25.National AIDS Control Programme. National guidelines for voluntary counseling and testing. United Republic of Tanzania, Ministry of Health and Social Welfare; Tanzania Mainland: 2005. [Google Scholar]
- 26.United Republic of Tanzania. Five years Drug Control Master Plan in the United Development of Tanzania. 2001 [Google Scholar]
- 27.Ndosi N. The Challenges of Psychiatry Amidst Economic Deprivation and Social Change in Dar es Salaam City, Tanzania. In: Heggenhougen K, Lugalla J, editors. Social Change and Health in Tanzania. Dar es Salaam, Tanzania: Dar es Salaam University Press; 2005. pp. 196–208. [Google Scholar]
- 28.Kilonzo G, Simmons N. Development of Mental Health Services in Tanzania: A Reappraisal for the Future. In: Heggenhougen K, Lugalla J, editors. Social Change and Health in Tanzania. Dar es Salaam, Tanzania: Dar es Salaam University Press; 2005. pp. 209–226. [Google Scholar]
- 29.Ndosi N, Waziri M. The Nature of Parasuicide in Dar es Salaam. In: Heggenhougen K, Lugalla J, editors. Social Change and Health in Tanzania. Dar es Salaam, Tanzania: Dar es Salaam University Press; 2005. pp. 227–240. [Google Scholar]
- 30.Bali TA. Dissertation. Storrs (CT): University of Connecticut; 2008. Changing Contexts of Deference to Elders, Children's Rights and Sexual Exploitation of Children in Tanzania. [Google Scholar]
- 31.Lugalla J, Mbwambo J. Street Children and Street Life in Urban Tanzania: The Culture of Surviving and Its Implications for Children's Health. In: Heggenhougen K, Lugalla J, editors. Social Change and Health in Tanzania. Dar es Salaam, Tanzania: Dar es Salaam University Press; 2005. pp. 69–90. [Google Scholar]
- 32.McCrann D, Lalor K, Kataboro JK. Child Sexual Abuse among University Students in Tanzania. Child Abuse Negl. 2006;30(12):1343–1351. doi: 10.1016/j.chiabu.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 33.United Republic of Tanzania. “Plus 5” Review of the Special Session on Children and World Fit For Children Plan of Action. National Report on WFFC+5. 2006 [Google Scholar]
- 34.Volkow N, Li T. Drugs and alcohol: Treating and preventing abuse, addiction and their medical consequences. Pharmacol Ther. 2005;108:3–17. doi: 10.1016/j.pharmthera.2005.06.021. [DOI] [PubMed] [Google Scholar]


