Abstract
Circulating transthyretin (TTR) is a critical determinant of plasma retinol-binding protein 4 (RBP4) levels. Elevated RBP4 levels cause insulin resistance, and the lowering of RBP4 levels improves glucose homeostasis. Since lowering TTR levels increases renal clearance of RBP4, we determined whether decreasing TTR levels with antisense oligonucleotides (ASOs) improves glucose metabolism and insulin sensitivity in obesity. TTR-ASO treatment of mice with genetic or diet-induced obesity resulted in an 80–95% decrease in circulating levels of TTR and RBP4. Treatment with TTR-ASOs, but not control ASOs, decreased insulin levels by 30–60% and improved insulin sensitivity in ob/ob mice and high-fat diet–fed mice as early as after 2 weeks of treatment. The reduced insulin levels were sustained for up to 9 weeks of treatment and were associated with reduced adipose tissue inflammation. Body weight was not changed. TTR-ASO treatment decreased LDL cholesterol in high-fat diet–fed mice. The glucose infusion rate during a hyperinsulinemic-euglycemic clamp was increased by 50% in high-fat diet–fed mice treated with TTR-ASOs, demonstrating improved insulin sensitivity. This was also demonstrated by 20% greater inhibition of hepatic glucose production, a 45–60% increase of glucose uptake into skeletal and cardiac muscle, and a twofold increase in insulin signaling in muscle. These data show that decreasing circulating TTR levels or altering TTR-RBP4 binding could be a potential therapeutic approach for the treatment of type 2 diabetes.
Introduction
Type 2 diabetes is a major health concern worldwide (1) and is characterized by insulin resistance in peripheral tissues and dysregulated insulin secretion. Elevated levels of serum retinol-binding protein 4 (RBP4) cause insulin resistance and impair insulin signaling in mice (2). A mechanism for RBP4-induced insulin resistance is activation of proinflammatory pathways in adipose tissue (3,4). Similar effects occur in endothelial cells, which could impair vascular function (5). Large epidemiologic studies demonstrate that an elevated level of circulating RBP4 is a marker for prediabetes (6), metabolic syndrome (7), hypertension (8), and increased risk of coronary heart disease (9). A gain-of-function polymorphism in the RBP4 promoter is associated with an 80% increased risk of type 2 diabetes (10). Lowering RBP4 levels with an RNA oligonucleotide in rodents that were fed a high-fat diet improves metabolic syndrome and hepatic steatosis (11). Therefore, strategies are needed to lower RBP4 levels to prevent and/or treat type 2 diabetes and associated cardiovascular disease.
Transthyretin (TTR) is a transport protein for thyroxine and a binding partner for RBP4. RBP4 binding to TTR reduces the glomerular filtration rate of RBP4 and retains it in the blood (12). Thus, TTR binding is a critical determinant of serum RBP4 levels. Serum TTR levels are elevated in insulin-resistant ob/ob mice (13) and in some insulin-resistant humans (14). In insulin-resistant ob/ob mice, renal clearance of RBP4 is reduced compared with lean mice, which likely is due to the elevated serum TTR and increased serum RBP4 binding capacity (13). The synthetic retinoid fenretinide disrupts the RBP4-TTR complex, promoting the renal clearance of RBP4. Fenretinide improves insulin resistance and hepatic steatosis in rodents (2,15,16), and also improves insulin resistance in overweight humans (17). Therefore, drugs that reduce RBP4-TTR binding may lower serum RBP4 levels and improve insulin-glucose homeostasis. In fact, a human trial using fenretinide to treat insulin resistance is in progress (18).
Another approach to lowering serum RBP4 levels is to decrease serum TTR levels. Not only are serum TTR levels elevated in some humans with obesity and insulin resistance (14), but also studies (19) suggest that TTR is a marker of dyslipidemia in humans. TTR associated with chylomicrons may affect triglyceride synthesis by increasing levels of acylation-stimulating protein (20), and TTR may play a role in reverse cholesterol transport by cleaving apolipoprotein (apo)A-I (21). Thus, TTR itself may also play a role in metabolic syndrome independently of RBP4.
Antisense oligonucleotides (ASOs) provide a specific and rapid method for lowering target gene expression. ASOs are well tolerated in humans, and an ASO targeting apoB100 was recently approved by the U.S. Food and Drug Administration for the treatment of familial hypercholesterolemia (22). Since RBP4 levels are elevated in the serum of insulin-resistant, high-fat diet–fed mice and ob/ob mice, we hypothesize that TTR-ASOs would be effective in lowering serum RBP4 levels and improving insulin sensitivity in these models. We show that treatment with TTR-ASOs markedly decreases serum TTR and RBP4 levels and improves insulin-glucose homeostasis without changing body weight.
Research Design and Methods
Animals and Treatments
For studies in ob/ob mice, male C57BL/6J ob/ob mice (stock #000632) and lean littermate controls (+/+ or ob/+) were obtained from The Jackson Laboratory at 5–6 weeks of age. Mice were housed two to a cage and fed a chow diet (catalog #5008; LabDiet) ad libitum. The ob/ob mice were randomized to a treatment group based on glucose level (5 h after the removal of food) and body weight at 7 weeks of age. Mice were treated with saline solution, a control ASO (141923; Isis Pharmaceuticals), or a TTR-ASO (401723; Isis Pharmaceuticals) twice a week (12.5 mg/kg i.p.). A human TTR-ASO (304258; Isis Pharmaceuticals) was used in a subset of studies (25 mg/kg twice a week for 3.5 weeks, followed by 35 mg/kg three times per week for an additional 2.5 weeks). ASOs were resuspended in saline solution as described previously (23). Mice were weighed weekly, and body composition was determined by DEXA (Lunar PIXImus Densitometer; GE Medical Systems). All aspects of animal care were approved by the Institutional Animal Care and Use Committee of the Beth Israel Deaconess Medical Center and Harvard Medical School and by Isis Pharmaceuticals.
For studies in high-fat diet–fed mice, obesity and insulin resistance were induced in 6-week-old C57BL/6J male mice (The Jackson Laboratory) by feeding the mice a 58% high-fat diet for 3 months (catalog #12330; Research Diets). Subsequently, mice were treated with saline solution, a control ASO (141923; Isis Pharmaceuticals), or a TTR-ASO (401724; Isis Pharmaceuticals) twice a week (25 mg/kg s.c.). A lean control group was fed a chow diet (catalog #5001; Purina [Newco Distributors]) and was treated with saline solution.
Serum Chemistries and Glucose and Insulin Tolerance Tests
Plasma insulin levels were determined by ELISA (Crystal Chemistry for ob/ob mice; ALPCO Diagnostics for high-fat diet–fed mice). The glucose × insulin product was calculated by multiplying 5-h food-removed glucose and insulin values. Cholesterol measurements in high-fat diet–fed mice were determined on an AU400E Clinical Analyzer (catalog #OSR6283; Beckman Coulter). For glucose and insulin tolerance tests, ob/ob mice were fasted for 5 h and injected with glucose (1 g/kg, s.c.) or insulin (2.4 units/kg, s.c.; Humulin R; Eli Lilly), and high-fat diet–fed mice were fasted for 3.5–4 h and injected with insulin intraperitoneally.
Flow Cytometry of Surface Markers and Intracellular Cytokines
The adipose tissue stromal-vascular fraction was obtained as described previously (3) and resuspended in PBS supplemented with 2% FCS. Surface markers were stained with saturating amounts of the following fluorescent-labeled monoclonal antibodies (BioLegend) for flow cytometry: CD11c (clone N418), CD11b (clone M1/70), F4/80 (clone CI:A3–1), CD206 (clone C068C2), and CD45 (BD Horizon clone 30-F11). For intracellular cytokine staining, cells were stimulated in vitro for 5 h at 37°C in 5% CO2 with a leukocyte activation cocktail (BD Biosciences) and stained with anti–tumor necrosis factor (TNF) antibody (clone MP6-XT22; BioLegend) as described previously (3). Cells were acquired on a specially ordered five-laser LSR II Flow Cytometer (BD Biosciences) at the Beth Israel Deaconess Medical Center Flow Cytometry Core and analyzed with FlowJo software (Tree Star).
PCR and Western Blotting
For Western blots, the following antibodies were used in ob/ob mice: RBP4 (catalog #A0040; Dako) and TTR (catalog #A0002; Dako). The following antibodies were used in in high-fat diet–fed mice: RBP4 (catalog #210–437-C100; Alexis Biochemicals), TTR (catalog #11891–1-AP; Proteintech), pAkt473 (catalog #9271; Cell Signaling Technology), and Akt (catalog #9272; Cell Signaling Technology). Real-time PCR was performed with the ABI Prism Sequence Detector system. For studies in ob/ob mice, the following primers and probes were obtained from Applied Biosystems: TTR (Mm00443267-m1) and TBP (Mm00446971-m1). For studies in high-fat diet–fed mice, the following primer/probe set was used: TTR-forward: 5′-CGTACTGGAAGACACTTGGCATT-3′; TTR-reverse: 5′-GAGTCGTTGGCTGTGAAAACC-3′; and TTR-FAM: 5′-CCCGTTCCATGAATTCGCGGATG-3′. Targeted mRNA was normalized to total RNA as determined by RiboGreen fluorescence.
Hyperinsulinemic-Euglycemic Clamp
Three days before experiments, mice were anesthetized with isoflurane, and an indwelling catheter was inserted in the right jugular vein. A dual-tracer clamp ([3-3H]glucose infusion and 2-deoxy-d-[1-14C]glucose bolus) was performed. After an overnight fast, [3-3H]glucose (0.05 µCi/min; PerkinElmer) was infused to estimate basal whole-body glucose turnover for 2 h. Hyperinsulinemic-euglycemic clamp was performed with a primed and continuous infusion of human insulin (15 pmol/kg/min; Humulin; Eli Lilly) to raise plasma insulin levels within a physiological range (~200 pmol/L). Twenty percent glucose was infused at a variable rate to maintain glucose at basal levels (~110 mg/dL). [3-3H]glucose (0.1 µCi/min; PerkinElmer) was infused throughout the clamp to estimate insulin-stimulated whole-body glucose turnover. Insulin-stimulated glucose uptake in individual tissues was estimated by the administration of a bolus (10 µCi) of 2-deoxy-d-[1-14C]glucose (2-[14C]DG) (PerkinElmer) at 75 min after the start of the clamps. At the end of clamps, mice were killed and tissues were taken for biochemical analysis. pAkt473 and Akt were measured in samples after the clamp. Glucose concentration during clamps was determined by a glucose oxidase method on an Analox Glucose Analyzer. Plasma concentrations of tracers were determined following deproteinization of plasma samples. The radioactivity of 3H in tissue glycogen was determined by digesting samples in KOH and precipitating glycogen with ethanol. Tissue 2-[14C]DG-6-P content was determined by ion exchange chromatography to separate 2-deoxy-d-glucose (2-DG)-6-P from 2-DG.
Statistical Analysis
Data were analyzed with GraphPad using a two-tailed Student t test or ANOVA as indicated. P < 0.05 was considered to be statistically significant.
Results
TTR-ASOs Lower Expression of TTR RNA in Liver and TTR Levels in Serum in ob/ob Mice
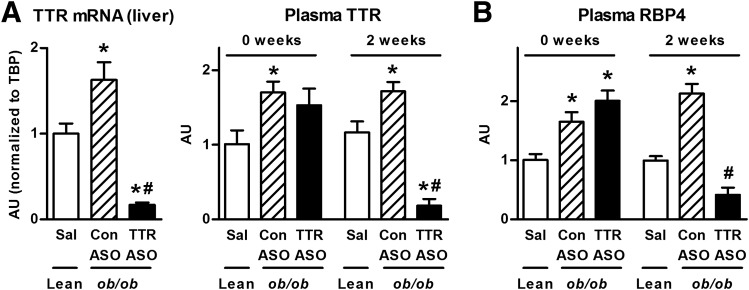
TTR expression was elevated 1.6-fold in liver of obese, insulin-resistant ob/ob mice compared with lean controls (Fig. 1A), which is consistent with previous studies (13). TTR-ASO treatment decreased TTR expression in liver by ~90% compared with control ASO treatment. Prior to ASO treatment, serum TTR and RBP4 levels were both elevated in ob/ob mice compared with lean controls (Fig. 1A and B). After 2 weeks of TTR-ASO treatment, serum TTR levels were reduced by ~90% and serum RBP4 levels by ~80% in ob/ob mice receiving TTR-ASO treatment compared with ob/ob mice receiving control ASO treatment. Because of the 80% lowering of plasma RBP4 levels, we evaluated retinoid homeostasis, which is reflected in the expression of retinoid-responsive genes such as Cyp26a1 and retinoic acid receptor β (24). The expression of these genes was not decreased in liver or adipose tissue with TTR-ASO treatment compared with control ASO treatment, suggesting normal cellular retinoid levels (data not shown). These findings are consistent with normal tissue retinoid levels in male mice with genetic knockout of TTR (25).
Figure 1.
Treatment of ob/ob mice with TTR-ASOs decreases circulating levels of TTR and RBP4. A: TTR mRNA in livers of male lean and ob/ob mice after 8 weeks of ASO treatment. Plasma TTR levels in male lean and ob/ob mice prior to ASO treatment (0 weeks) and after 2 weeks of ASO treatment. B: Plasma RBP4 levels in male lean and ob/ob mice prior to ASO treatment (0 weeks) and after 2 weeks of ASO treatment. *P < 0.05 vs. lean controls, #P < 0.05 vs. ob/ob mice treated with control ASO at the same time point by ANOVA. ASO treatment was started at 7 weeks of age. n = 8–16 per group. Data are expressed as the mean ± SEM. AU, arbitrary units; Con ASO, control ASO treatment; Sal, saline solution treatment.
TTR-ASO Treatment Improves Insulin Sensitivity in ob/ob Mice Without Altering Body Composition
TTR-ASO treatment did not alter body weight in ob/ob mice compared with control ASO treatment (Fig. 2A–C). Fat mass was increased ninefold in ob/ob mice compared with lean controls and was not altered in ob/ob mice treated with TTR-ASOs. Lean mass in ob/ob mice was not changed with TTR-ASO treatment. Food intake was increased by 1.8-fold in ob/ob mice compared with lean controls but was not affected by TTR-ASO treatment (Fig. 2D).
Figure 2.
Treatment of ob/ob mice with TTR-ASOs does not alter body weight, fat mass, or food intake. Body weight (A), fat mass (B), and lean mass (C) determined by DEXA in male lean mice and ob/ob mice treated with ASO for 2.5 and 12.5 weeks. ASO treatment was started at 7 weeks of age. D: Food intake per day in lean and ob/ob mice at 8 weeks of age. *P < 0.05 vs. lean mice by ANOVA. n = 8–16 per group. Data are expressed as the mean ± SEM. Con ASO, control ASO treatment; Sal, saline solution treatment.
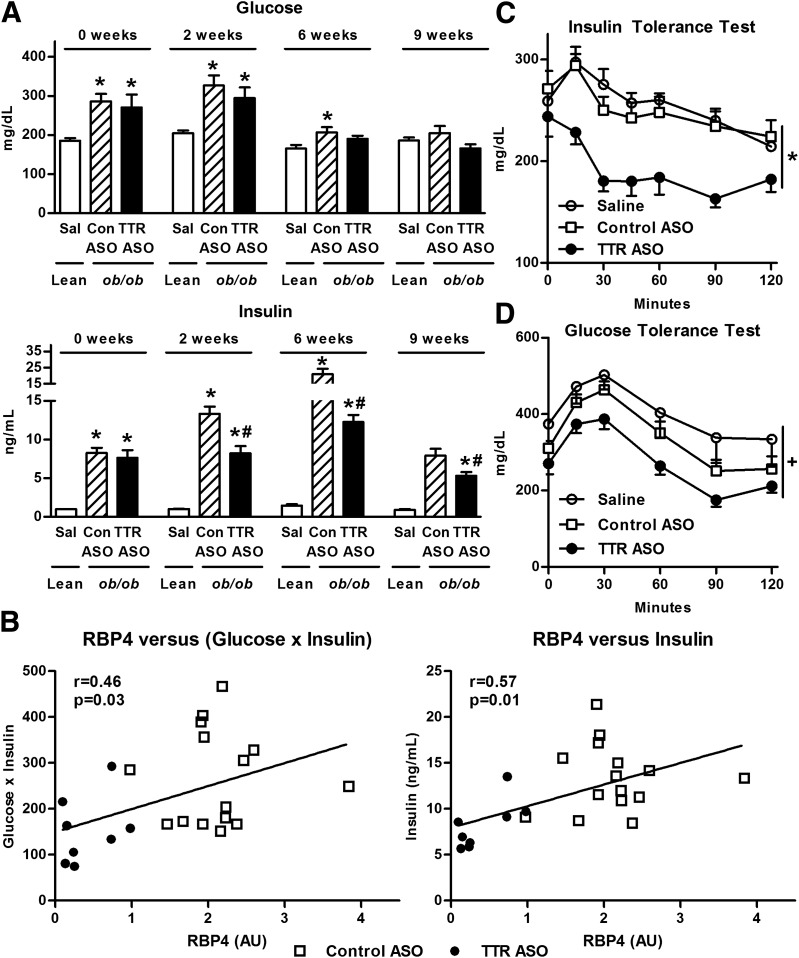
Prior to ASO treatment, at 7 weeks of age, ob/ob mice had elevated glucose levels and markedly elevated insulin levels measured 5 h after the removal of food compared with lean controls (Fig. 3A). By 16 weeks of age (after 9 weeks of ASO treatment), this hyperglycemia normalized, which was reported to occur between 12 and 16 weeks of age by The Jackson Laboratory supplier (26,27). Treatment with TTR-ASOs for 2 weeks lowered insulin levels, and the improvement was sustained at 6 and 9 weeks of ASO treatment. Insulin levels (r = 0.57, P = 0.01) and glucose-insulin product (r = 0.46, P = 0.03) correlate with serum RBP4 levels after only 2 weeks of ASO treatment (Fig. 3B). The fact that >50% of measurements of serum TTR levels in the TTR-ASO–treated mice were at or below the limit of detection made it uninformative to determine correlations with TTR. After 4 weeks of ASO treatment, ob/ob mice receiving TTR-ASO treatment had improved insulin sensitivity, as demonstrated by the results of an insulin tolerance test (Fig. 3C). Glucose tolerance also tended to be improved in the mice receiving treatment with TTR-ASOs (Fig. 3D).
Figure 3.
Treatment of ob/ob mice with TTR-ASOs improves insulin sensitivity. A: Glucose and insulin levels 5 h after the removal of food in male lean and ob/ob mice at baseline (0 weeks), and after 2, 6, and 9 weeks of ASO treatment. ASO treatment was started at 7 weeks of age. *P < 0.05 vs. lean mice, #P < 0.05 vs. ob/ob mice treated with control ASO at the same time point by ANOVA. B: Correlation of plasma RBP4 levels with insulin and glucose × insulin product in male ob/ob mice after 2 weeks of TTR-ASO treatment. Glucose and insulin levels were measured 5 h after the removal of food. C: Insulin tolerance test (2.4 units/kg s.c.) after 4 weeks of ASO treatment. *P < 0.05 for ob/ob mice treated with TTR-ASO vs. ob/ob mice treated with saline solution or control ASO by ANOVA with repeated measures for the comparison of each curve. D: Glucose tolerance test (1 mg/kg s.c.) after 3 weeks of ASO treatment. +P < 0.05 for ob/ob mice treated with TTR-ASO vs. saline solution treatment, and P = 0.09 vs. control ASO treatment by ANOVA with repeated measures for comparison of each curve. n = 8 to 16 per group. Data are expressed as the mean ± SEM. AU, arbitrary units; Con ASO, control ASO treatment; Sal, saline solution treatment.
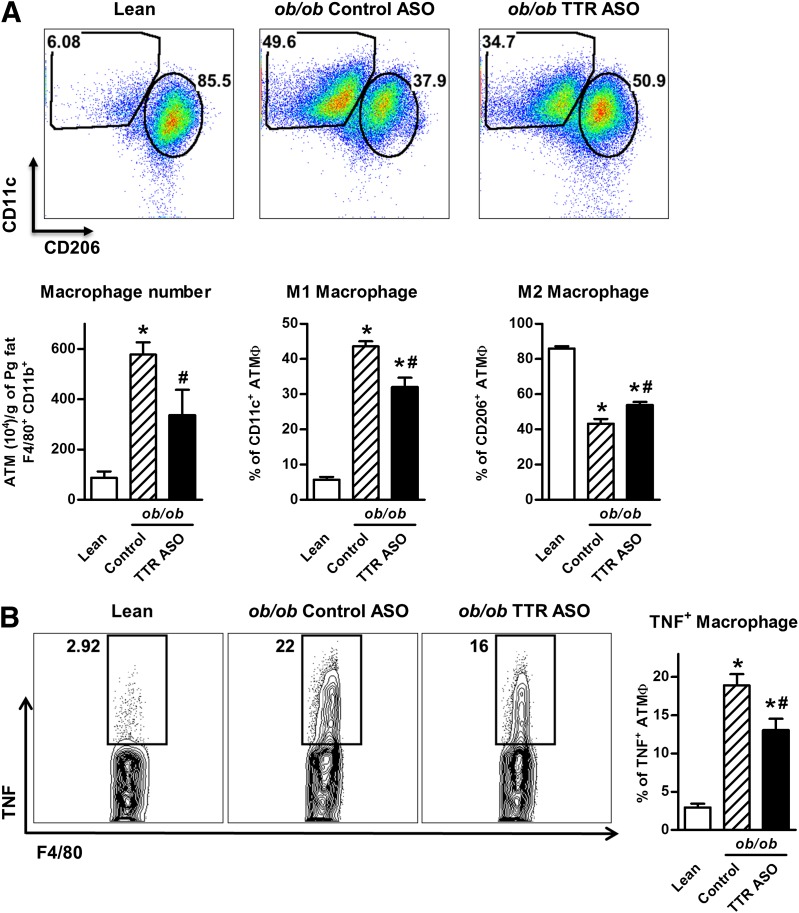
Since lowering TTR levels lowers RBP4 levels, the improved insulin sensitivity could be RBP4 dependent. One mechanism by which RBP4 induces insulin resistance is by increasing adipose tissue inflammation, involving both innate and adaptive immune responses (3). Therefore, we sought to determine whether lowering circulating TTR levels, which results in lower circulating RBP4 levels, would alter inflammation in adipose tissue (Fig. 4). As expected, in the adipose tissue of ob/ob mice, the number of macrophages and the percentage of proinflammatory M1 (CD11c+) macrophages were increased and the percentage of anti-inflammatory M2 (CD206+) macrophages was decreased compared with lean mice (Fig. 4A). Treatment with TTR-ASOs decreases the overall number of macrophages in adipose tissue and the percentage of proinflammatory M1 (CD11c+) macrophages, while increasing the percentage of anti-inflammatory M2 (CD206+) macrophages. This is accompanied by a reduction in the percentage of macrophages that produce the cytokine TNF, demonstrating anti-inflammatory effects with TTR-ASO treatment (Fig. 4B).
Figure 4.
Treatment of ob/ob mice with TTR-ASOs reduces adipose tissue inflammation. A: Flow cytometry representation of gated CD45+F4/80+CD11b+ adipose tissue macrophages expressing CD11c+ (M1 macrophage) or CD206+ (M2 macrophage) (top). Number of macrophages, percentage of inflammatory CD11c+ macrophages, and percentage of anti-inflammatory CD206+ macrophages (bottom). B: Flow cytometry representation (left) of adipose tissue macrophages expressing TNF in male lean and ob/ob mice. Percentage of TNF+ adipose tissue macrophages (right). *P < 0.05 vs. lean mice, #P < 0.05 vs. ob/ob mice treated with control ASO by ANOVA. ASO treatment was started at 7 weeks of age. n = 6–12 per group. Data are expressed as the mean ± SEM. ATM, adipose tissue macrophages; Control, combined saline and control ASO treatment; Pg fat, perigonadal fat; Sal, saline solution treatment.
Since TTR can promote insulin secretion (28), we measured glucose-stimulated insulin levels, which were not altered in ob/ob mice treated with TTR-ASO, suggesting normal secretory capacity (data not shown). Since some studies (20,21) indicate that TTR may be important in cholesterol metabolism, we measured parameters of lipid metabolism. Total cholesterol and HDL cholesterol levels were elevated in ob/ob mice and were not altered with TTR-ASO treatment (data not shown). Cholesterol efflux from macrophages to mouse serum was not different when using serum from mice treated with TTR-ASO versus serum from mice treated with control ASO (data not shown).
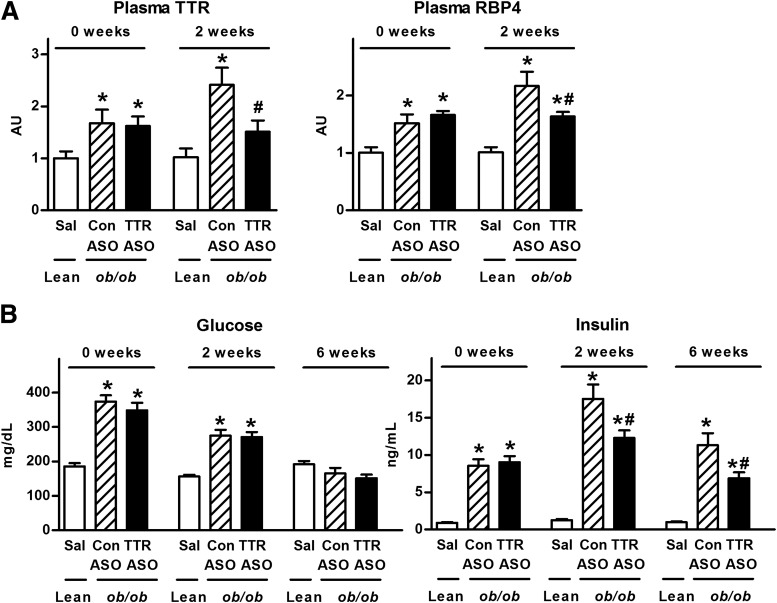
We also determined whether milder treatment that reduces TTR and RBP4 levels to physiological levels but not below them would improve insulin sensitivity. We used a human TTR-ASO that is less potent against the mouse gene. This lowered plasma TTR levels by ~40% in ob/ob mice, resulting in levels similar to those in lean mice (Fig. 5A). However, RBP4 levels were reduced by only 25%, resulting in higher levels than in lean mice. Similar to our prior cohort (Fig. 3A), ob/ob mice had elevated glucose levels at 7 weeks of age that resolved by 13 weeks of age (Fig. 5B). TTR-ASO treatment lowered insulin levels, demonstrating that a moderate reduction of TTR and RBP4 levels leads to sustained improvement of insulin sensitivity. The inhibition of gene expression achieved with ASOs made by Isis Pharmaceuticals is generally maintained for 3–4 weeks posttreatment and takes 8–10 weeks to fully reverse (29). Even with an ASO targeted against human TTR, which is less potent against mouse TTR, serum TTR levels remained decreased at 1.5 and 3 weeks after discontinuing ASO treatment and returned to baseline ob/ob levels 6 weeks after discontinuing ASO treatment (data not shown). Therefore, injecting ASOs twice a week sustains the reduction in TTR levels between doses.
Figure 5.
Reduction of TTR and RBP4 levels to physiological levels with TTR-ASOs improves insulin sensitivity. A: Plasma TTR and RBP4 levels in male lean and ob/ob mice prior to ASO treatment (0 weeks) and after 2 weeks of ASO treatment. B: Glucose and insulin levels 5 h after the removal of food in male lean and ob/ob mice at baseline (0 weeks) and after 2 and 6 weeks of ASO treatment. *P < 0.05 vs. lean mice, #P < 0.05 vs. ob/ob mice treated with control ASO at the same time point by ANOVA. ASO treatment was started at 7 weeks of age. n = 10–14 per group. Data are expressed as the mean ± SEM. AU, arbitrary units; Con ASO, control ASO treatment; Sal, saline solution treatment.
TTR-ASO Treatment Lowers TTR Levels and Improves Glucose-Insulin Homeostasis in High-Fat Diet–Fed Mice
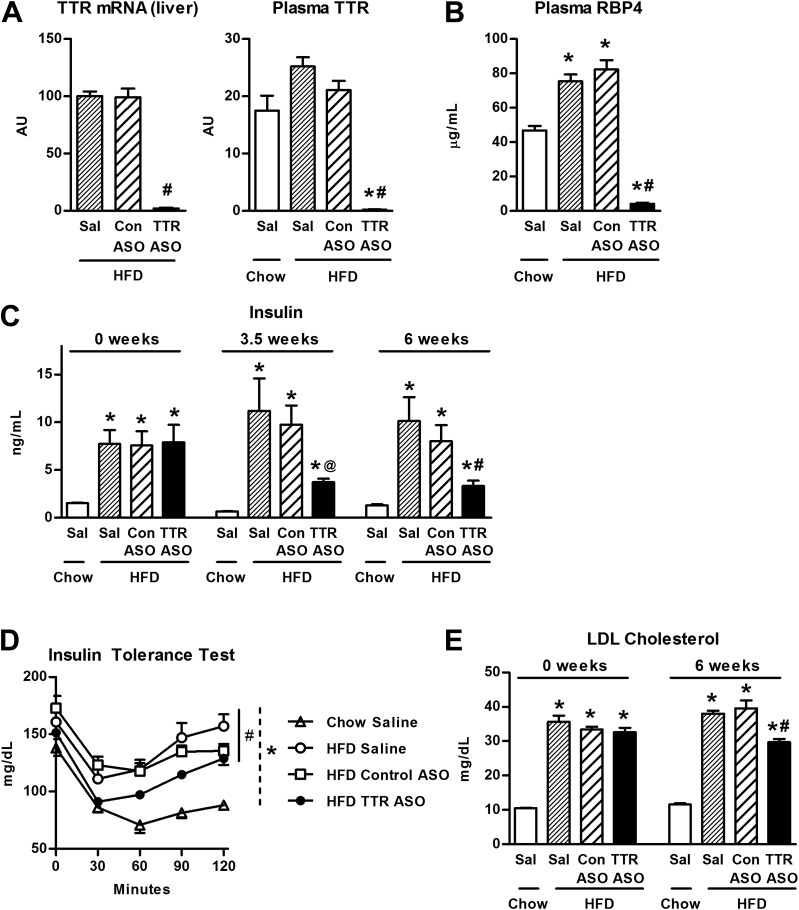
TTR-ASO treatment decreased TTR expression by 98% in liver in high-fat diet–fed mice compared with saline solution and control ASO treatment (Fig. 6A). Treatment with control ASO had no effect on circulating TTR levels in high-fat diet–fed mice. However, TTR-ASO treatment for 4 weeks decreased circulating TTR levels to undetectable levels. Circulating RBP4 levels were increased by 1.6-fold in the high-fat diet–fed mice treated with either saline solution or a control ASO compared with chow-fed controls (Fig. 6B). Reduction in TTR levels with TTR-ASO treatment was accompanied by an ~95% reduction in circulating levels of RBP4, suggesting increased RBP4 clearance by the kidney, as expected.
Figure 6.
Treatment of high-fat diet–fed mice with TTR-ASOs decreases circulating TTR and RBP4 levels, and improves insulin sensitivity. A: TTR mRNA in liver in male mice fed a high-fat diet after 4 weeks of ASO treatment. Plasma TTR levels in male chow-fed and high-fat diet–fed mice. *P < 0.05 vs. chow-fed mice, #P < 0.05 vs. high-fat diet–fed mice treated with saline solution or control ASO by ANOVA. B: Plasma RBP4 levels in male chow-fed and high-fat diet–fed mice after 3 weeks of ASO treatment. *P < 0.05 vs. chow-fed mice, #P < 0.05 vs. high-fat diet–fed mice treated with saline solution or control ASO by ANOVA. C: Fed insulin levels in male chow-fed and high-fat diet–fed mice prior to ASO treatment (0 weeks) and after 3.5 and 6 weeks of ASO treatment. *P < 0.05 vs. chow-fed mice, @P < 0.05 vs. high-fat diet–fed mice treated with control ASO, #P < 0.05 high-fat diet–fed mice treated with saline solution or control ASO by t test. D: Insulin tolerance test (0.4 units/kg) after 6.5 weeks of ASO treatment. *P < 0.05 for chow-fed vs. high-fat diet–fed mice treated with saline solution, control ASO, or TTR-ASO by ANOVA with repeated measures for comparison of each curve. #P < 0.05 for high-fat diet–fed mice treated with TTR-ASO vs. control ASO, P = 0.056 vs. saline solution by ANOVA with repeated measures for comparison of each curve. E: Fed LDL cholesterol levels in male chow-fed and high-fat diet–fed mice prior to ASO treatment (0 weeks) and after 6 weeks of ASO treatment. *P < 0.05 vs. chow-fed mice, #P < 0.05 vs. high-fat diet–fed mice treated with saline solution or control ASO by ANOVA. n = 4–5 per group (A); n = 6–9 per group (B–E). Data are expressed as the mean ± SEM. AU, arbitrary units; Con ASO, control ASO treatment; HFD, high-fat diet; Sal, saline solution treatment.
TTR-ASO treatment for up to 6 weeks did not alter body weight or food intake in high-fat diet–fed mice (data not shown). Untreated high-fat diet–fed mice had fivefold elevated insulin levels compared with chow-fed mice (Fig. 6C). TTR-ASO treatment for either 3.5 or 6 weeks reduced insulin levels by 60% compared with saline solution and control ASO treatment. Corresponding fed glucose levels were unchanged with TTR-ASO treatment when insulin levels were lowered, indicating improved insulin sensitivity (data not shown). This was directly demonstrated by the results of an insulin tolerance test (Fig. 6D).
As mentioned above, studies (20,21) suggest that TTR may be involved in cholesterol metabolism. High-fat diet–fed mice had elevated levels of total cholesterol, HDL cholesterol, and LDL cholesterol compared with chow-fed mice (data not shown). TTR-ASO treatment for 6 weeks reduced LDL cholesterol levels compared with saline solution and control ASO treatment (Fig. 6E), but did not alter HDL cholesterol levels (data not shown).
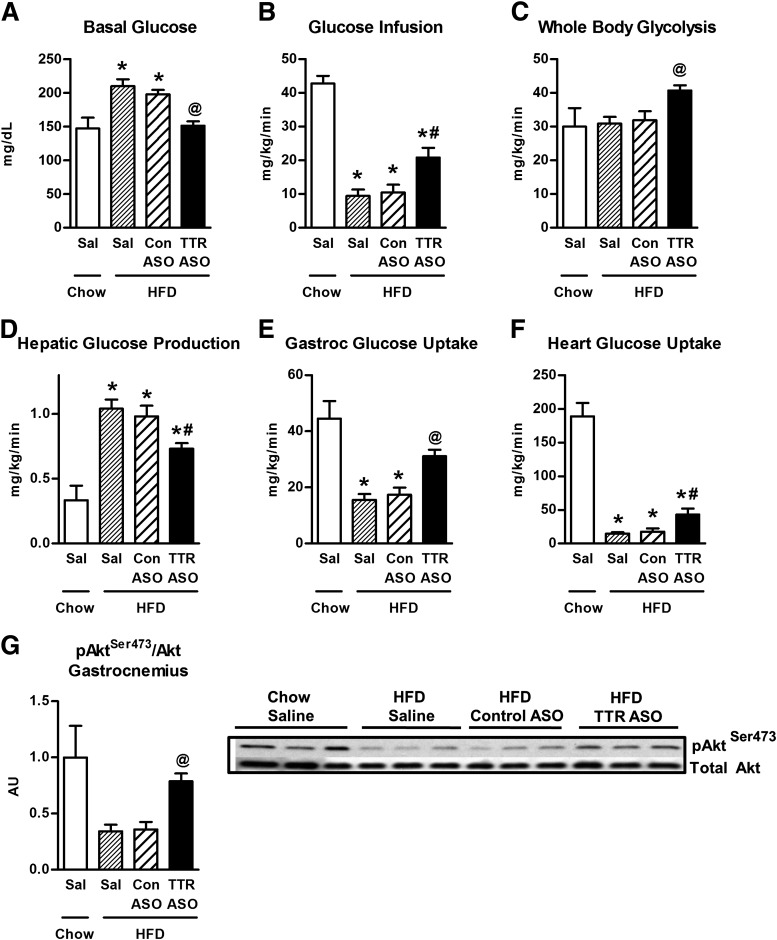
TTR-ASO Treatment Improves Insulin-Glucose Homeostasis During Hyperinsulinemic-Euglycemic Clamp
To evaluate which tissues may contribute to the increased insulin sensitivity with TTR-ASO treatment, a hyperinsulinemic-euglycemic clamp study was performed in the high-fat diet–fed mice and chow-fed lean controls. Prior to the clamp, the basal glucose level was higher in high-fat diet–fed mice compared with chow-fed mice. TTR-ASO treatment decreased basal glucose levels compared with saline and control ASO treatment (Fig. 7A). During the clamp, glucose was maintained at the same level in all groups (data not shown). The glucose infusion rate was decreased by 75% in high-fat diet–fed mice compared with chow-fed controls, indicating insulin resistance with the high-fat diet (Fig. 7B). TTR-ASO treatment of high-fat diet–fed mice increased the glucose infusion rate by 50% compared with treatment with saline solution or a control ASO, demonstrating improved insulin sensitivity. Increased insulin sensitivity was also shown by a 30% increase in whole-body glycolysis in high-fat diet–fed mice treated with TTR-ASO compared with saline solution or control ASO (Fig. 7C). Basal hepatic glucose production was not different with TTR-ASO treatment (data not shown). Hepatic glucose production in the presence of insulin was 80% higher in high-fat diet–fed mice treated with saline solution or control ASO compared with chow-fed mice (Fig. 7D). TTR-ASO treatment of high-fat diet–fed mice reduced hepatic glucose production by 20%, indicating improved hepatic insulin sensitivity. Glucose uptake into skeletal and cardiac muscle was decreased in high-fat diet–fed mice treated with saline solution or a control ASO compared with chow diet–fed mice (Fig. 7E and F). TTR-ASO treatment increased glucose uptake into gastrocnemius muscle by 44%, and into heart by 59%, compared with saline or control ASO treatment, demonstrating increased insulin sensitivity in skeletal and cardiac muscle. Glucose uptake into white adipose tissue was decreased with a high-fat diet compared with a chow diet and was not changed with TTR-ASO treatment (data not shown). Consistent with the improved insulin sensitivity in skeletal muscle, TTR-ASO treatment increased Akt phosphorylation by twofold in gastrocnemius muscle in high-fat diet–fed mice compared with mice treated with saline solution or a control ASO (Fig. 7G).
Figure 7.
Treatment of high-fat diet–fed mice with TTR-ASOs improves insulin-glucose homeostasis during hyperinsulinemic-euglycemic clamp. A: Glucose levels prior to hyperinsulinemic-euglycemic clamp in chow-fed and in high-fat diet–fed mice receiving saline solution, control ASO, or TTR-ASO. Six-week-old C57BL/6J male mice were fed a high-fat diet for 3 months and treated with saline solution or ASO for 4 weeks. B–F: Glucose infusion rate during clamp, whole-body glycolysis, hepatic glucose production, glucose uptake in skeletal muscle, and glucose uptake in cardiac muscle during clamp in the presence of insulin. G: pAkt473/Akt in gastrocnemius muscle. *P < 0.05 vs. chow-fed mice, #P < 0.05 vs. all other groups, @P < 0.05 vs. high-fat diet–fed mice treated with saline solution or control ASO. A, B, and E, by ANOVA. C, D, F, and G, by t test comparing individual groups. n = 6–7 per group for A–F; n = 3 per group for G. Data are expressed as the mean ± SEM. AU, arbitrary units; Con ASO, control ASO treatment; Gastroc, gastrocnemius muscle; HFD, high-fat diet; Sal, saline solution treatment.
Discussion
Since elevated circulating levels of RBP4 cause insulin resistance and TTR is a critical determinant of circulating RBP4 levels, we sought to determine whether lowering TTR levels improved insulin resistance. Other approaches to lowering RBP4 levels, which improves metabolic parameters in rodents, include treatment with RNA oligonucleotides (11) and the synthetic retinoid fenretinide (2,15,16). Although both TTR-ASO and fenretinide lower RBP4 levels by promoting its renal excretion, fenretinide may have additional effects due to the displacement of extracellular and intracellular retinoids (30) and the inhibition of enzymes such as β-carotene monooxygenase (31). Fenretinide can also affect signaling pathways (32) and basic cellular processes, including apoptosis (33). Therefore, since fenretinide may have side effects related or unrelated to altered retinoid homeostasis, it is important to develop different treatment approaches to reduce RBP4-TTR binding or lower TTR levels. Lowering circulating TTR levels could improve metabolic syndrome by reducing circulating levels of RBP4 or by RBP4-independent effects (20,21).
Serum TTR levels are elevated by an average of 1.2-fold and as much as twofold in some individuals with insulin resistance (14), and this elevation could contribute to the increased RBP4 levels in these people. TTR levels are elevated in ob/ob mice but not in high-fat diet–fed mice (13). We found that TTR-ASO treatment decreases circulating levels of TTR and RBP4, and improves insulin sensitivity in genetic and dietary models of insulin resistance without changing body weight. Therefore, even insulin-resistant individuals without elevated TTR levels may benefit from the lowering of TTR levels. In both ob/ob mice and high-fat diet–fed mice, TTR-ASO treatment lowered circulating levels of TTR to below those in lean control mice (Figs. 1A and 6A) and also decreased circulating RBP4 levels (Figs. 1B and 6B). Therefore, treatment with TTR-ASOs is an effective means to lower circulating levels of TTR and RBP4 in genetic and diet-induced obesity.
Treatment with TTR-ASO improved insulin sensitivity, as demonstrated by decreased circulating insulin levels (Figs. 3A and 6C), improved insulin tolerance (Figs. 3C and 6D), enhanced glucose disposal on hyperinsulinemic-euglycemic clamp (Fig. 7B), and increased insulin signaling (Fig. 7G). In addition to enhanced glucose disposal, the clamp demonstrated improved suppression of hepatic glucose production, and augmented insulin-stimulated glucose uptake in skeletal and cardiac muscle (Fig. 7D–F). This was accompanied by enhanced insulin signaling in muscle (Fig. 7G). The improvement in insulin sensitivity coincided with the decrease in TTR as early as 2 weeks after initiating TTR-ASO treatment and was sustained for 9 weeks of treatment.
Three different ASOs were effective in decreasing TTR levels and improving insulin sensitivity. Even with the one ASO that achieved a modest reduction in TTR levels, insulin sensitivity was still improved (Fig. 5A and B). We also found that TTR-ASO treatment of high-fat diet–fed mice lowered LDL cholesterol levels. This suggests that lowering TTR levels could be an effective treatment for insulin resistance and metabolic syndrome associated with obesity. The resultant increased insulin sensitivity that we observed with TTR-ASOs could be due to decreased TTR levels or to the fact that reducing TTR levels lowers RBP4 levels. Elevated RBP4 levels cause insulin resistance by increasing adipose tissue inflammation (3). We show that TTR-ASO treatment reduces adipose tissue inflammation, which could be due to the reduced circulating RBP4 levels (Fig. 4).
TTR-ASO treatment could be a feasible approach to treating insulin resistance since the safety of ASOs has been shown in clinical studies in humans (34). ASOs targeting apoB100 are approved for the treatment of familial hypercholesterolemia (22). Furthermore, TTR-ASO treatment has been used in phase 3 clinical trials for TTR-associated amyloidosis (35) in which mutations in TTR destabilize the TTR tetramer and induce the formation of amyloid fibrils in tissues. In these trials, insulin resistance was not studied because of debilitating neurologic symptoms in some patients. However, these studies support the conclusion that TTR-ASOs effectively lower plasma TTR levels and are safe in humans.
TTR binding to retinol-RBP4 is critical to maintaining circulating RBP4 and retinol levels. TTR-ASO treatment lowers circulating RBP4 levels by 80–95%, which could potentially alter retinoid homeostasis. Mice with genetic knockout of TTR have only ~5% of wild-type circulating RBP4 and retinol levels, but they are fertile, viable, and do not show symptoms of vitamin A deficiency (36). These mice have normal dark-adapted electroretinogram responses as early as 3 weeks of age, and they are sustained throughout life (37) along with normal retinal morphology (38). Therefore, it is unlikely that treatment with TTR-ASO would lead to night blindness. Even animals with complete knockout of RBP4 have normal dark-adapted electroretinogram responses starting at 8 weeks of age and acquire normal visual function (37).
It is also unlikely that treatment with TTR-ASOs would lead to accelerated vitamin A deficiency since TTR knockout mice on a vitamin A–deficient diet do not develop vitamin A deficiency faster than wild-type mice. This suggests that TTR knockout mice can use stored retinol (36). Furthermore, retinol levels are normal in liver and other tissues of male TTR knockout mice (25). In our studies, the normal levels of the retinoid-responsive genes Cyp26a1 and retinoic acid receptor β (24) indicate normal retinoid status. However, the potential developmental effects of lowering TTR levels in the presence of vitamin A deficiency deserve consideration.
Since TTR is a carrier protein for thyroid hormone, the potential effects of lowering TTR levels on thyroid status are important. In humans, thyroxine-binding globulin, and not TTR, is the main thyroid hormone-binding protein. Individuals with mutations in TTR are euthyroid, because free thyroid hormone levels are maintained (39,40). In rodents, TTR is the major thyroid hormone carrier protein. However, TTR knockout mice are euthyroid and have normal free thyroid hormone levels (41,42). Their euthyroid status is further demonstrated by their normal thyroid-stimulating hormone dynamics and normal deiodinase activity in liver and brain (41,42). These rodent studies indicate that even when TTR is the major thyroid hormone transport protein, its absence does not alter thyroid function. Therefore, lowering TTR levels with ASOs should not affect thyroid function in mice, and furthermore in humans in whom TTR is a minor thyroid-binding protein accounting for ~15% of circulating thyroid hormone (43).
Comparison of the phenotype of TTR-ASO treatment in adult mice with that of TTR knockout mice is of interest. Studies (44) reported no alterations of glucose tolerance, glycemia, or lipid levels in chow-fed TTR knockout mice on a wild-type background. In addition, TTR knockout in ob/ob mice did not alter basal glucose or insulin levels, but glucose tolerance tests were not performed (45). Furthermore, there are no reports of insulin tolerance testing, euglycemic clamp, insulin signaling, or other in-depth metabolic characterization of TTR knockout mice on either genotype and no data on a high-fat diet. The phenotypes could be different because peripherally administered ASOs target gene expression primarily in liver and fat (46,47) and would not affect TTR expression in other tissues. TTR is also expressed in choroid plexus (48) and pancreatic islets. TTR synthesized by the choroid plexus regulates insulin-like growth factor receptor 1 in the central nervous system (49), and TTR in pancreatic α-cells may regulate glucagon expression (50). TTR in the tissues that are not targeted by peripheral ASO treatment could have important metabolic effects, which may make the phenotype different in TTR knockout mice compared with mice treated with TTR-ASOs.
RBP4 levels are elevated in most, although not all, insulin-resistant people, and elevated RBP4 levels are a marker for metabolic syndrome (6–8). Lowering RBP4 levels improves glucose homeostasis in both obese and lean rodents (2,11,15,16) and may mediate some or all of the beneficial effects of lowering plasma TTR levels in insulin-resistant mice. Our studies demonstrate that lowering TTR levels with TTR-ASO treatment in mice with genetic or diet-induced obesity is an effective approach for improving insulin sensitivity. This improvement, which we observed as early as 2 weeks following ASO treatment, demonstrates that TTR plays an important role in glucose homeostasis either directly or indirectly by regulating RBP4 levels. Since plasma levels of RBP4 are elevated in most insulin-resistant humans, they are likely to benefit from the lowering of TTR levels regardless of whether the TTR level is elevated because RBP4 levels will also be reduced. Thus, lowering TTR levels is a promising approach to the treatment of insulin resistance.
Article Information
Acknowledgments. The authors thank Daniel Rader and Dawn Marchadier at the University of Pennsylvania for plasma cholesterol and cholesterol efflux measurements in ob/ob mice. The authors also thank William S. Blaner at Columbia University for helpful discussion.
Funding. This work was supported by National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases grants K08-DK-84344 (to L.Z.), RR37-DK-43051 and P30-DK-57521 (to B.B.K.), and T32-DK-07516 (to B.B.K. and L.Z.). A.C. was supported by São Paulo Research Foundation (FAPESP) grant 2014/02218-6.
Duality of Interest. O.D.P. and B.B.K. are inventors who are listed on a patent related to RBP4. S.B., S.F.M., P.M., S.G., and B.P.M. are employees of Isis Pharmaceuticals Inc. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. L.Z. helped to design the studies, perform the experiments, and write and review the manuscript. S.B. helped to design the studies and review the manuscript. O.D.P., S.F.M., P.M.M.-V., A.C., P.M., and S.G. performed the experiments and helped to review the manuscript. B.P.M. contributed to the discussion and edited the manuscript. B.B.K. helped to design the studies and to write and review the manuscript. L.Z. and S.B. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 69th Scientific Sessions of the American Diabetes Association, New Orleans, LA, 5–9 June 2009.
References
- 1.Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. Lancet Diabetes Endocrinol 2014;2:56–64 [DOI] [PubMed] [Google Scholar]
- 2.Yang Q, Graham TE, Mody N, et al. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature 2005;436:356–362 [DOI] [PubMed] [Google Scholar]
- 3.Moraes-Vieira PM, Yore MM, Dwyer PM, Syed I, Aryal P, Kahn BB. RBP4 activates antigen-presenting cells, leading to adipose tissue inflammation and systemic insulin resistance. Cell Metab 2014;19:512–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norseen J, Hosooka T, Hammarstedt A, et al. Retinol-binding protein 4 inhibits insulin signaling in adipocytes by inducing proinflammatory cytokines in macrophages through a c-Jun N-terminal kinase- and toll-like receptor 4-dependent and retinol-independent mechanism. Mol Cell Biol 2012;32:2010–2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farjo KM, Farjo RA, Halsey S, Moiseyev G, Ma JX. Retinol-binding protein 4 induces inflammation in human endothelial cells by an NADPH oxidase- and nuclear factor kappa B-dependent and retinol-independent mechanism. Mol Cell Biol 2012;32:5103–5115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meisinger C, Rückert IM, Rathmann W, et al. Retinol-binding protein 4 is associated with prediabetes in adults from the general population: the Cooperative Health Research in the Region of Augsburg (KORA) F4 Study. Diabetes Care 2011;34:1648–1650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qi Q, Yu Z, Ye X, et al. Elevated retinol-binding protein 4 levels are associated with metabolic syndrome in Chinese people. J Clin Endocrinol Metab 2007;92:4827–4834 [DOI] [PubMed] [Google Scholar]
- 8.Solini A, Santini E, Madec S, Rossi C, Muscelli E. Retinol-binding protein-4 in women with untreated essential hypertension. Am J Hypertens 2009;22:1001–1006 [DOI] [PubMed] [Google Scholar]
- 9.Sun Q, Kiernan UA, Shi L, et al. Plasma retinol-binding protein 4 (RBP4) levels and risk of coronary heart disease: a prospective analysis among women in the nurses’ health study. Circulation 2013;127:1938–1947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Hoek M, Dehghan A, Zillikens MC, Hofman A, Witteman JC, Sijbrands EJ. An RBP4 promoter polymorphism increases risk of type 2 diabetes. Diabetologia 2008;51:1423–1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan Y, Sun LQ, Kamal MA, Wang X, Seale JP, Qu X. Suppression of retinol-binding protein 4 with RNA oligonucleotide prevents high-fat diet-induced metabolic syndrome and non-alcoholic fatty liver disease in mice. Biochim Biophys Acta 2011;1811:1045–1053 [DOI] [PubMed] [Google Scholar]
- 12.van Bennekum AM, Wei S, Gamble MV, et al. Biochemical basis for depressed serum retinol levels in transthyretin-deficient mice. J Biol Chem 2001;276:1107–1113 [DOI] [PubMed] [Google Scholar]
- 13.Mody N, Graham TE, Tsuji Y, Yang Q, Kahn BB. Decreased clearance of serum retinol-binding protein and elevated levels of transthyretin in insulin-resistant ob/ob mice. Am J Physiol Endocrinol Metab 2008;294:E785–E793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klöting N, Graham TE, Berndt J, et al. Serum retinol-binding protein is more highly expressed in visceral than in subcutaneous adipose tissue and is a marker of intra-abdominal fat mass. Cell Metab 2007;6:79–87 [DOI] [PubMed] [Google Scholar]
- 15.Preitner F, Mody N, Graham TE, Peroni OD, Kahn BB. Long-term Fenretinide treatment prevents high-fat diet-induced obesity, insulin resistance, and hepatic steatosis. Am J Physiol Endocrinol Metab 2009;297:E1420–E1429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koh IU, Jun HS, Choi JS, et al. Fenretinide ameliorates insulin resistance and fatty liver in obese mice. Biol Pharm Bull 2012;35:369–375 [DOI] [PubMed] [Google Scholar]
- 17.Johansson H, Gandini S, Guerrieri-Gonzaga A, et al. Effect of fenretinide and low-dose tamoxifen on insulin sensitivity in premenopausal women at high risk for breast cancer. Cancer Res 2008;68:9512–9518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veterans Medical Research Foundation. A randomized, double-blind study of the effects of fenretinide administered in subjects with obesity. ClinicalTrials.gov Identifier: NCT00546455 [Internet], 2007. San Diego, CA, University of California, San Diego. Available from http://clinicaltrials.gov/ct2/show/study/NCT00546455. Accessed 15 March 2014
- 19.Yoshida A, Matsutani Y, Fukuchi Y, Saito K, Naito M. Analysis of the factors contributing to serum retinol binding protein and transthyretin levels in Japanese adults. J Atheroscler Thromb 2006;13:209–215 [DOI] [PubMed] [Google Scholar]
- 20.Scantlebury T, Maslowska M, Cianflone K. Chylomicron-specific enhancement of acylation stimulating protein and precursor protein C3 production in differentiated human adipocytes. J Biol Chem 1998;273:20903–20909 [DOI] [PubMed] [Google Scholar]
- 21.Liz MA, Gomes CM, Saraiva MJ, Sousa MM. ApoA-I cleaved by transthyretin has reduced ability to promote cholesterol efflux and increased amyloidogenicity. J Lipid Res 2007;48:2385–2395 [DOI] [PubMed] [Google Scholar]
- 22.U.S. Food and Drug Administration. FDA news release: FDA approves new orphan drug Kynamro to treat inherited cholesterol disorder [Internet], 2013. Available from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm337195.htm. Accessed 15 March 2014
- 23.Zinker BA, Rondinone CM, Trevillyan JM, et al. PTP1B antisense oligonucleotide lowers PTP1B protein, normalizes blood glucose, and improves insulin sensitivity in diabetic mice. Proc Natl Acad Sci USA 2002;99:11357–11362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wongsiriroj N, Jiang H, Piantedosi R, et al. Genetic dissection of retinoid esterification and accumulation in the liver and adipose tissue. J Lipid Res 2014;55:104–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wei S, Episkopou V, Piantedosi R, et al. Studies on the metabolism of retinol and retinol-binding protein in transthyretin-deficient mice produced by homologous recombination. J Biol Chem 1995;270:866–870 [DOI] [PubMed] [Google Scholar]
- 26.The Jackson Laboratory. Variation in the severity and duration of hyperglycemia in the C57BL/6J-ob/ob (obese) mouse [article online], 1992. Available from http://jaxmice.jax.org/jaxnotes/archive/451b.html. Accessed 15 March 2014
- 27.Coleman DL, Hummel KP. The influence of genetic background on the expression of the obese (Ob) gene in the mouse. Diabetologia 1973;9:287–293 [DOI] [PubMed] [Google Scholar]
- 28.Refai E, Dekki N, Yang SN, et al. Transthyretin constitutes a functional component in pancreatic beta-cell stimulus-secretion coupling. Proc Natl Acad Sci USA 2005;102:17020–17025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Geary RS, Yu RZ, Siwkowski A, Levin AA. Pharmacokinetic/pharmacodynamic properties of phosphorothioate 2K-O-(2-methoxyethyl)-modified antisense oligonucleotides in animals and man. In Antisense Drug Technology: Principles, Strategies, and Applications. 2nd Ed. London, CRC Press—Taylor & Francis Group. 2008, p. 305–326 [Google Scholar]
- 30.Takahashi N, Sausville EA, Breitman TR. N-(4-hydroxyphenyl)retinamide (Fenretinide) in combination with retinoic acid enhances differentiation and retinoylation of proteins. Clin Cancer Res 1995;1:637–642 [PubMed] [Google Scholar]
- 31.Poliakov E, Gubin A, Laird J, Gentleman S, Salomon RG, Redmond TM. The mechanism of fenretinide (4-HPR) inhibition of β-carotene monooxygenase 1. New suspect for the visual side effects of fenretinide. Adv Exp Med Biol 2012;723:167–174 [DOI] [PubMed] [Google Scholar]
- 32.Bikman BT, Guan Y, Shui G, et al. Fenretinide prevents lipid-induced insulin resistance by blocking ceramide biosynthesis. J Biol Chem 2012;287:17426–17437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hail N Jr, Lotan R. Mitochondrial permeability transition is a central coordinating event in N-(4-hydroxyphenyl)retinamide-induced apoptosis. Cancer Epidemiol Biomarkers Prev 2000;9:1293–1301 [PubMed] [Google Scholar]
- 34.Ackermann EJ, Guo S, Booten S, et al. Clinical development of an antisense therapy for the treatment of transthyretin-associated polyneuropathy. Amyloid 2012;19(Suppl. 1):43–44 [DOI] [PubMed] [Google Scholar]
- 35.Isis Pharmaceuticals. Drugs in development: pipeline [Internet], 2014. Available from http://www.isispharm.com/Pipeline/index.htm. Accessed 15 March 2014
- 36.Episkopou V, Maeda S, Nishiguchi S, et al. Disruption of the transthyretin gene results in mice with depressed levels of plasma retinol and thyroid hormone. Proc Natl Acad Sci USA 1993;90:2375–2379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quadro L, Blaner WS, Salchow DJ, et al. Impaired retinal function and vitamin A availability in mice lacking retinol-binding protein. EMBO J 1999;18:4633–4644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bui BV, Armitage JA, Fletcher EL, Richardson SJ, Schreiber G, Vingrys AJ. Retinal anatomy and function of the transthyretin null mouse. Exp Eye Res 2001;73:651–659 [DOI] [PubMed] [Google Scholar]
- 39.Moses AC, Rosen HN, Moller DE, et al. A point mutation in transthyretin increases affinity for thyroxine and produces euthyroid hyperthyroxinemia. J Clin Invest 1990;86:2025–2033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moses AC, Lawlor J, Haddow J, Jackson IM. Familial euthyroid hyperthyroxinemia resulting from increased thyroxine binding to thyroxine-binding prealbumin. N Engl J Med 1982;306:966–969 [DOI] [PubMed] [Google Scholar]
- 41.Palha JA, Hays MT, Morreale de Escobar G, Episkopou V, Gottesman ME, Saraiva MJ. Transthyretin is not essential for thyroxine to reach the brain and other tissues in transthyretin-null mice. Am J Physiol 1997;272:E485–E493 [DOI] [PubMed] [Google Scholar]
- 42.Palha JA, Episkopou V, Maeda S, Shimada K, Gottesman ME, Saraiva MJ. Thyroid hormone metabolism in a transthyretin-null mouse strain. J Biol Chem 1994;269:33135–33139 [PubMed] [Google Scholar]
- 43.Woeber KA, Ingbar SH. The contribution of thyroxine-binding prealbumin to the binding of thyroxine in human serum, as assessed by immunoadsorption. J Clin Invest 1968;47:1710–1721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marques F, Sousa JC, Oliveira P, Oliveira HC, Palha JA. The absence of transthyretin does not impair regulation of lipid and glucose metabolism. Horm Metab Res 2007;39:529–533 [DOI] [PubMed] [Google Scholar]
- 45.Rendenbach C, Ganswindt S, Seitz S, et al. Increased expression of transthyretin in leptin-deficient ob/ob mice is not causative for their major phenotypic abnormalities. J Neuroendocrinol 2013;25:14–22 [DOI] [PubMed] [Google Scholar]
- 46.Bennett CF, Swayze EE. RNA targeting therapeutics: molecular mechanisms of antisense oligonucleotides as a therapeutic platform. Annu Rev Pharmacol Toxicol 2010;50:259–293 [DOI] [PubMed] [Google Scholar]
- 47.Erion DM, Yonemitsu S, Nie Y, et al. SirT1 knockdown in liver decreases basal hepatic glucose production and increases hepatic insulin responsiveness in diabetic rats. Proc Natl Acad Sci U S A 2009;106:11288–11293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Benson MD, Smith RA, Hung G, et al. Suppression of choroid plexus transthyretin levels by antisense oligonucleotide treatment. Amyloid 2010;17:43–49 [DOI] [PubMed] [Google Scholar]
- 49.Vieira M, Gomes JR, Saraiva MJ. Transthyretin induces insulin-like growth factor I nuclear translocation regulating its levels in the hippocampus. Mol Neurobiol. 2 August 2014. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Su Y, Jono H, Misumi Y, et al. Novel function of transthyretin in pancreatic alpha cells. FEBS Lett 2012;586:4215–4222 [DOI] [PubMed] [Google Scholar]