Abstract
This article describes the indications and technique for all-arthroscopic knotless repair of a peripheral tear to the triangular fibrocartilage complex (TFCC). The advantage of this technique is that it allows repair of the articular disk back to the fovea of the ulna without any suture knots to irritate the patient. The learning curve is steep, but once learned, this technique can be performed very quickly and is faster. There are no knots to irritate the patient, and in the author's opinion, there is quicker pain relief than with other techniques.
Keywords: arthroscopy, wrist, knotless, TFCC
Arthroscopy has continued to revolutionize the practice of orthopaedic surgery with the capability to visualize and treat intraarticular pathology. Wrist arthroscopy provides direct visualization of the cartilage surfaces, synovial tissues, and ligaments under bright light and magnified conditions. The wrist itself is complex, with eight carpal bones and multiple articular surfaces combined with intrinsic and extrinsic ligaments, including the triangular fibrocartilage complex (TFCC). Wrist arthroscopy has become a valuable adjunct to management of disorders of the TFCC.
This article reviews the indications for wrist arthroscopy in the management of peripheral ulnar-sided tears of the articular disk involving the TFCC. Many techniques have been developed for repair of ulnar-sided tears of the articular disk.1 2 3 4 5 6 These include both inside-out and outside-in techniques. While these techniques have generally been successful, they generally involve repair of the superficial layer of the articular disk and involve making a small incision with suture knots, which can irritate the soft tissues. Recently, an all-arthroscopic knotless technique has been developed for repair of peripheral ulnar-sided tears of the TFCC.3 The advantage of this technique is that it is entirely arthroscopic, utilizes a suture anchor but does not require any knots, and enables repair of both the superficial and deep layers of the articular disk, directly back down to bone.
The TFCC is a complicated soft tissue support system whose purpose is to stabilize the ulnar side of the wrist. It acts as an extension of the articular surface and both supports the proximal carpal row and stabilizes the distal radial ulnar joint. Palmer classified the components of the TFCC into the fibrocartilage articular disk, the volar and dorsal radial ulnar ligaments, and the floor of the extensor carpi ulnaris tendon sheath.7 The ulnar aspect of the articular disk has two main bundles. One bundle is joined to the ulnar styloid and the second to the fovea. Proximal limbs of the palmar and dorsal radioulnar ligaments conjoin and insert into the fovea just medial to the ulnar styloid. These structures have been previously referred to as the ligamentum subcruetum. The exact function of the superficial and deep components of the volar and dorsal radioulnar ligaments is controversial. The superficial and deep layers function independently of each other. It is felt that the ligamentum subcruetum in particular is an important structure for stability of the distal radioulnar joint.
Indications
Patients who present with ulnar-sided wrist pain, normal radiographs, and tenderness over the periphery of the TFCC are initially immobilized. Potentially, small ulnar peripheral tears of the articular disk may heal with immobilization due to the vascular blood supply. Indications for surgical intervention include persistent ulnar-sided wrist pain not relieved with conservative management for at least 3 months. Additional indications include patients with symptomatic distal radial joint instability not relieved by immobilization.
Contraindications for surgical management include patients who are minimally symptomatic despite radiographic findings, patients who have degenerative changes of either the radial carpal or distal radioulnar joint, and low-physical-demand patients who are not medically healthy enough for surgery.
Arthroscopic Knotless Peripheral TFCC Repair
The wrist is suspended with 10 pounds of traction in a traction tower. It is important to use a traction tower so that the wrist can be flexed ∼20–30 degrees. This will make easier access to the base of the ulna through the accessory 6R portal with the wrist flexed. Inflow can then be provided with the needle in either the 6U or 1–2 portal. Frequently, the 1–2 portal is utilized for inflow so that the inflow cannula will be out of the way during the arthroscopic peripheral TFCC procedure. The 3–4 portal is identified with an 18-gauge needle, and then skin is incised with the tip of a no. 11 blade. Blunt dissection is carried down with the hemostat at the level of the capsule, and the 2.7-mm arthroscope is introduced through the 3–4 portal with a blunt trocar. The radiocarpal space is evaluated. An 18-gauge needle is then used to identify the exact location of the 6R portal just distal to the articular disk. This will prevent accidental injury to the articular disk or to the articular cartilage of the lunate or triquetrum. The portal is made with blunt technique, and a probe is inserted through the 6R portal.
The integrity of the articular disk is then inspected both visually with the arthroscope and by palpation with the probe. It is important to palpate the articular disk to evaluate the loss of tension when a peripheral tear is present. Synovitis frequently obscures the peripheral tear and needs to be débrided to appreciate the extent of the peripheral ulnar-sided tear fully.
Initially, arthroscopic knotless TFC repair was primarily designed for complete full-thickness tears of the articular disk, which involve both the superficial and deep layers. In this manner, when the articular disk was probed, the most ulnar edge of the articular disk would freely lift up from the ulnar capsule in the ulna. There was gross lack of tension to the articular disk. However, more recently, since the success of knotless TFC repair with pain relief, this technique has been, in the author's opinion, much quicker as compared with superficial repair. Superficial tears are now completed like complete full-thickness tears and the knotless technique is performed.
An accessory 6R portal is made ∼1.5 cm distal in line with an additional 6R portal. This portal is made by utilizing an 18-gauge needle inserted through the skin and aimed at the ulnar head (Fig. 1). The ulnar head should be palpated with the needle. Once the ideal location of the accessory 6R portal has been identified, the portal is made. Again, it is important to have the wrist flexed ∼20–30 degrees for easier access to the base of the ulna. The tendency is to slide off the volar aspect of the distal ulna with either the drill or the anchor. Flexing the wrist allows a more central location for insertion of the anchor, once the ideal location for the accessory 6R portal is made.
Fig. 1.

Outside view demonstrating the use of an 18-gauge needle identifying the exact location for the accessory 6R portal. This portal is made ∼1.5 cm distal to the standard 6R portal.
Only the skin is incised to protect the dorsal sensory branch of the ulnar nerve. Blunt dissection is performed with the hemostat to the level of the joint capsule.
A suture lasso (Arthrex, Naples, FL, USA) is inserted through the accessory 6R portal into the radiocarpal space (Fig. 2). The tip of the needle is easily seen with the arthroscope in the 3–4 portal, and then the lasso is passed through the periphery of the tear through the articular disk in a proximal-to-distal direction. It is very helpful to twist the lasso gently between the thumb and index finger to tease the tip of the lasso through the tough tissue of the articular disk. Both the superficial and deep layers of the articular disk are pierced through with the suture lasso. A wire suture passer is inserted through the suture lasso and retrieved through the 6R portal with a crochet hook (Figs. 3 4). An alternative method is to use a 2.0 fiber stick and pass it through the bend of the suture lasso. It has been the author's experience that it is frequently difficult for the suture to pass through the bend of the lasso. By utilizing a wire suture passer, it easily passes through the curve of the suture lasso and makes passing of the suture much easier. A 2.0 fiber wire suture (Arthrex, Naples, FL, USA) is then placed through the suture retriever and pulled distally through the suture lasso out the handle (Fig. 5). The suture lasso is then backed out of the articular disk and reinserted anterior or posterior to the previous perforation so that a horizontal mattress suture is placed (Fig. 6). It is very important that the suture lasso not be pulled out of the joint during this procedure during this step. If this happens, then soft tissue may be caught up in the suture. As the suture lasso reperforates through the articular disk, a loop of suture will be found protruding from the articular disk into the radiocarpal space. It is helpful to advance the suture lasso further into the joint and then pull back gently to make the loop of suture easily retrievable. The loop of suture is then retrieved out through the 6R portal with a crochet hook so that both limbs are exiting the 6R portal. This provides a horizontal mattress-type suture through the articular disk with permanent suture (Fig. 7).
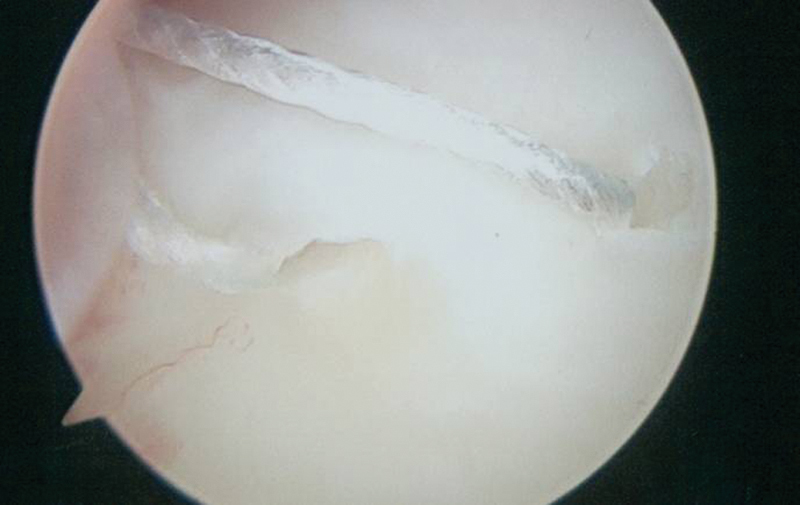
Fig. 2.
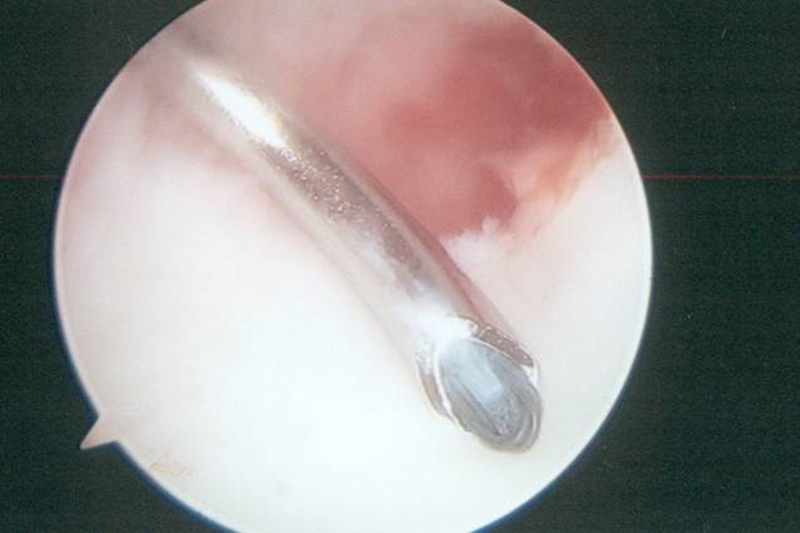
Arthroscopic view of the suture lasso being inserted through the accessory 6R portal intraarticularly into the radial carpal space.
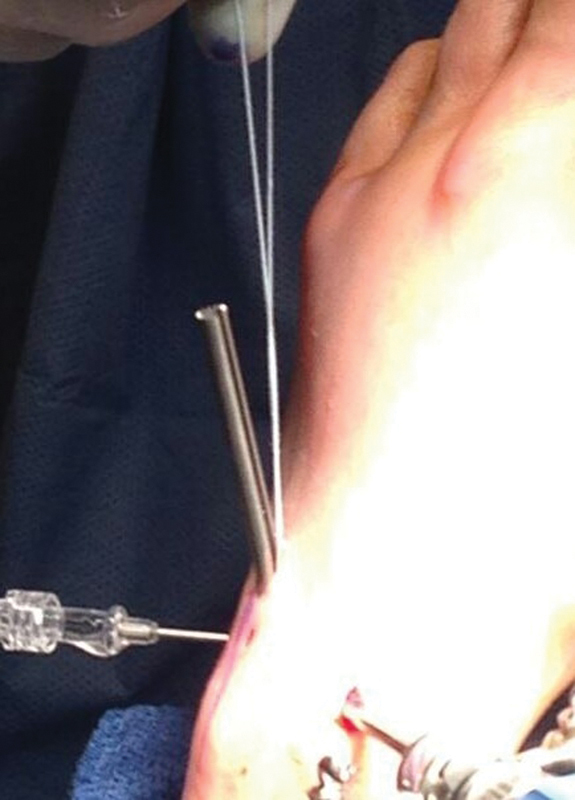
Fig. 3.
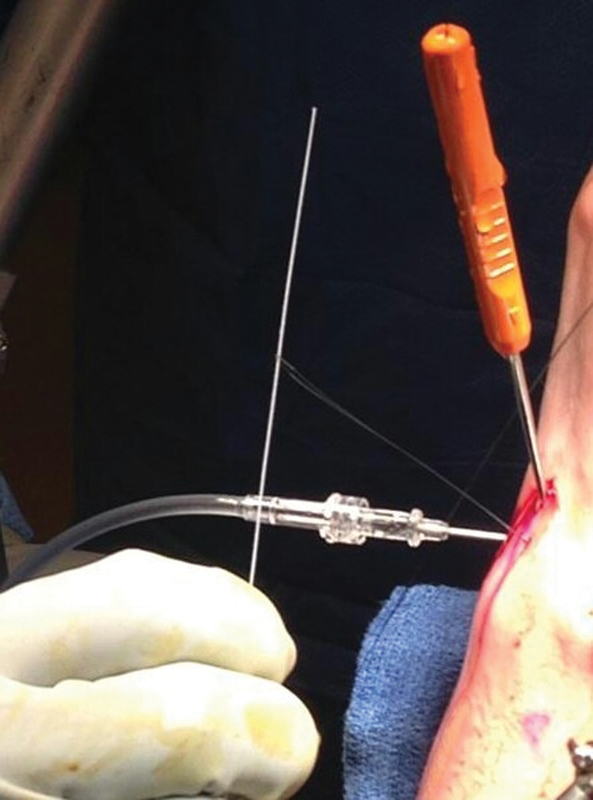
Outside view showing the wire retriever being passed through the suture lasso.
Fig. 4.

Arthroscopic view showing the crochet hook grasping the wire retriever out the standard 6R portal.
Fig. 5.
A 2.0 fiber wire suture inserted through the loop of the wire retriever and pulled distally out the handle of the suture lasso.
Fig. 6.
Arthroscopic view demonstrating repeat insertion of the suture lasso through the articular disk, leaving a loop of suture intraarticularly in the radiocarpal space.
Fig. 7.
Arthroscopic view showing both limbs of the 2.0 fiber wire being brought out the standard 6R portal, leaving a horizontal mattress suture through both layers of the articular disk.
A cannula is then inserted through the accessory 6R portal. A trocar is provided to make easier passage of the cannula through the soft tissue through the accessory 6R portal into the joint. It is important to note that the cannula has a serrated edge and a smooth edge. It will make the procedure much easier if the smooth edge of the cannula is inserted intra-articularly into the joint. In that way, the sutures will not get caught up on the rough, serrated edge during suture passage. Once the cannula is inserted through the accessory 6R portal, the crochet hook is then passed through the cannula to pull out the two suture limbs distally through the cannula. Both suture limbs should now be exiting the cannula through the accessory 6R portal (Fig. 8). The suture limbs are then passed out through the slot of the cannula so that they will not be caught up when the distal ulna is drilled with the drill bit. The cannula is then firmly placed down onto the head of the ulna through the peripheral tear of the articular disk.
Fig. 8.
Outside view demonstrating retrieval of both suture limbs out the accessory 6R portal through the slot of the cannula.
At this point, the surgeon has two options. A trocar may be inserted through the cannula and a Kirschner wire (K-wire) inserted through the trocar into the ulnar head. The position of the guide wire is checked under fluoroscopy to ensure that the insertion point of the anchor will be at the fovea of the ulna. A cannulated drill is inserted over the guide wire, and a drill hole is made in the base of the ulna as the ideal location is confirmed under fluoroscopy.
Alternatively, it is the author's recommendation that if the surgeon feels comfortable, the fovea of the ulna may be drilled once the cannula is in ideal position. Again, the tendency is for the cannula to slip off volarly. Once the cannula is inserted through the accessory 6R portal and is stable onto the distal aspect of the ulna, the ulna is drilled.
It is of vital importance that once the ulna is drilled, the cannula be kept in the same position. Generally, the assistant controls the cannula so that it does not move after drilling of the distal ulna. The 2.0 fiber wire suture limbs are than inserted through the mini push lock anchor (Arthrex, Naples, FL), and the anchor is advanced down the cannula to the drill hole (Fig. 9). It is helpful to have the slot of the cannula aimed toward the wrist arthroscope so that it can easily be seen. In that manner, as the anchor is being placed down the cannula, the sutures can be definitely identified reducing back through the slot into the cannula as the anchor is being advanced (Fig. 10). The anchor is then advanced into the drill hole and the sutures are tensioned. Once the sutures are tensioned, the anchor is advanced into the distal ulna. Following insertion of the anchor into the bone, a gentle attempt is made to remove the insertion handle. If the anchor is correctly inserted into the drill hole, there will be resistance to this. If there is resistance, the anchor has been correctly inserted into the head of the ulna. The insertion handle is then twisted counterclockwise off the anchor and removed. The 2.0 fiber wire sutures are than cut with a small upbiter through the 6R portal and are removed through the accessory 6R portal. This procedure repairs both layers of the articular disk back down to bone with an all-arthroscopic knotless technique.
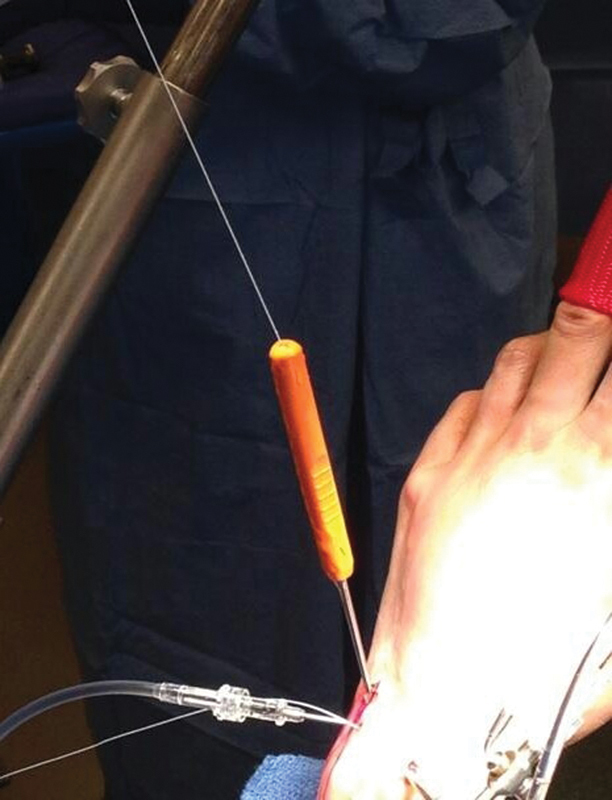
Fig. 9.

Outside view demonstrating suture of the mini push lock anchor being inserted through the cannula into the fovea of the ulna.
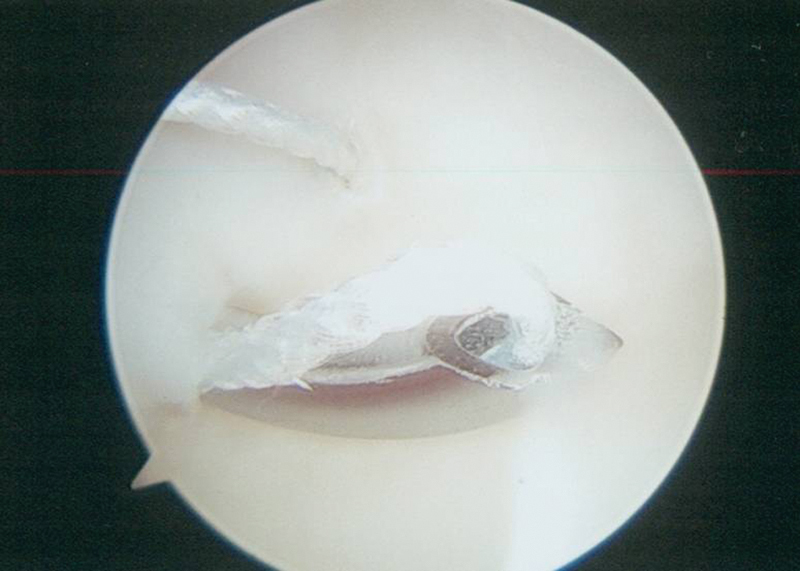
Fig. 10.

Arthroscopic view demonstrating the mini push lock anchor being inserted through the drill hole into the fovea of the ulna.
The wrist is then immobilized in slight supination in an above-elbow splint for ∼3–4 weeks. A removable wrist splint is then used for an additional 3 weeks. Digital range of motion exercises are initiated immediately. Range-of-motion and strengthening exercises of the forearm and wrist are started at approximately 7 weeks. Most patients are discharged at approximately 3 months postoperatively.
Discussion
There are several reasons for the surgeon to have in his or her armamentarium to address peripheral ulnar-sided tears of the articular disk. First, this technique enables repair of both layers of the articular disk directly back to bone with permanent suture. This provides a very strong construct to the repair. Second, utilizing an anchor allows a completely knotless repair. There are no suture knots to irritate the soft tissues, a frequent complication with previous techniques. Third, by being entirely arthroscopic, there is less soft tissue dissection, and it is felt that patients have less postoperative pain compared with previous techniques. Fourth, because of the use of permanent sutures, it is felt that patients may be immobilized for less time and range-of-motion programs may be initiated sooner than when biodegradable suture is used. It is acknowledged that there is a steep learning curve with this technique. However, multiple modifications have been made over the past year or two to decrease the arthroscopic steps to make the procedure easier. Once the steep learning curve has been addressed, the procedure can easily be done in ∼10–15 minutes.
Footnotes
Conflict of Interest The author recieves royalties from Arthrex.
References
- 1.de Araujo W, Poehling G G, Kuzma G R. New Tuohy needle technique for triangular fibrocartilage complex repair: preliminary studies. Arthroscopy. 1996;12(6):699–703. doi: 10.1016/s0749-8063(96)90173-5. [DOI] [PubMed] [Google Scholar]
- 2.Estrella E P Hung L K Ho P C Tse W L Arthroscopic repair of triangular fibrocartilage complex tears Arthroscopy 2007237729–737., 737.e1 [DOI] [PubMed] [Google Scholar]
- 3.Geissler W B. Arthroscopic knotless peripheral triangular fibrocartilage repair. J Hand Surg Am. 2012;37(2):350–355. doi: 10.1016/j.jhsa.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 4.Ruch D S, Anderson S R, Ritter M R. Biomechanical comparison of transosseous and capsular repair of peripheral triangular fibrocartilage tears. Arthroscopy. 2003;19(4):391–396. doi: 10.1053/jars.2003.50137. [DOI] [PubMed] [Google Scholar]
- 5.Ruch D S, Papadonikolakis A. Arthroscopically assisted repair of peripheral triangular fibrocartilage complex tears: factors affecting outcome. Arthroscopy. 2005;21(9):1126–1130. doi: 10.1016/j.arthro.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 6.Whipple T L, Geissler W B. Arthroscopic management of wrist triangular fibrocartilage complex injuries in the athlete. Orthopedics. 1993;16(9):1061–1067. doi: 10.3928/0147-7447-19930901-16. [DOI] [PubMed] [Google Scholar]
- 7.Palmer A K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(4):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]


