Abstract
Background Open reduction with internal fixation (ORIF) is currently the gold standard treatment of acute perilunate injuries (PLIs).
Less invasive surgery, including arthroscopic techniques, has recently emerged in the hope that results similar to those of ORIF could be obtained with less tissue disturbance.
Our purpose was to review retrospectively a series of selected PLIs treated with arthroscopic assistance over the past 10 years.
Materials and Methods Between 2004 and 2014, a total of 135 acute PLIs were surgically treated in our unit.
A total of 27 patients were treated with arthroscopic assistance, among whom 18 were reviewed clinically and radiologically.
Description of Technique After an initial closed gross reduction, radio- and midcarpal arthroscopy were performed to clean up the debris and assess the cartilaginous, bony, and ligamentous damage.
In 22 cases arthroscopy was followed by either radiolunate and lunotriquetral pinning, scapholunate ligament repair, and SL joint pinning or ORIF of a scaphoid fracture through a mini-invasive dorsal approach.
In the remaining six cases, fixation of the ligamentous and/or bony injuries was done using arthroscopy alone.
Results Arthroscopic findings are presented as well as the clinical results in a subgroup of patients. At final follow-up, visual analog scale (VAS) pain was rated 18/100 on average (minimum 0, maximum 50). If we consider only the patients without reflex sympathetic dystrophy (RSD; n = 14), the average active wrist flexion-extension was 87° (58% of the normal contralateral side) and the average grip strength was 30 kg (71% of the normal contralateral side).
Conclusions Although no statistical comparisons were made, we found that the results were similar to those of ORIF.
The results of our study suggest that the use of arthroscopy to treat selected PLIs may be a reliable adjunct either alone or in combination with a dorsal mini-open approach.
Keywords: wrist, perilunate dislocation, PLIND, scaphoid fracture, arthroscopy
Until recently, open reduction and internal fixation (ORIF) has been considered as the gold standard for treatment of acute perilunate injuries (PLIs).1 Given the extent of these devastative traumatic injuries, the clinical results of an ORIF for PLIs are very acceptable in terms of postoperative pain and residual stiffness. Long-term postoperative arthrosis is almost constant and sometimes severe.2 The number of true series with adequate follow-up is much smaller than the number of case reports,3 4 5 and we actually know little about the best treatment options of these difficult and rare injuries.
Less invasive treatments, including arthroscopic techniques, have recently emerged in the hope that results similar or better to those of ORIF could be obtained with less tissue disturbance and possibly less posttraumatic arthrosis.6
The purpose of this study is to review retrospectively a series of selected PLIs treated with arthroscopic assistance in our unit over the past 10 years.
Patients and Methods
Between 2004 and 2014, a total of 135 PLIs were surgically treated at the acute stage in our unit by the senior author or under his supervision.
A total of 27 cases were treated with arthroscopy, either alone or in conjunction with a mini-open dorsal approach.
All were closed fresh injuries from high-energy accidents. There were no polyinjured or polytrauma patients.
The delay between the injury and the treatment averaged 3 days.1 2 3 4 5 6 7
All patients but one were male. Their mean age was 33 years (range 19–67).
Only perilunate injuries not dislocated (PLIND), dorsal perilunate dislocations (PLD), and/or dorsal perilunate fracture-dislocation (PLFD) stage 1 or 2A according to our modified PLI classification7 were eligible for arthroscopic treatment.
There were 11 transscaphoid dorsal PLFDs, 12 pure ligamentous dorsal PLDs, and 4 PLINDs. The distribution of the injuries is shown in Table 1.
Table 1. Distribution of perilunate injuries and arthroscopic findings in our series of 27 wrists.
| Patient number | Diagnosis (initial X-rays) | Path of transosseous trauma (initial PA views) | Degree of sagittal displacement (initial lateral views) | Scapholunate degree of dissociation (arthroscopic Dautel staging) | Type of scaphoid fracture (X-rays and arthroscopy) | Midcarpal free osteochondral fragment(s) at arthroscopy | Status of cartilage of head of capitate at arthroscopy |
|---|---|---|---|---|---|---|---|
| 1 | PLD | 2A | SLD stage 3 | — | OC fract head of capitate | ||
| 2 | PLD | 2A | SLD stage 3 | Yes | Capitate OK | ||
| 3 | PLD | 1 | SLD stage 3 | Yes | OC fract head of capitate | ||
| 4 | PLD | 1 | SLD stage 3 | — | Capitate OK | ||
| 5 | PLD | 1 | SLD stage 3 | — | Capitate OK | ||
| 6 | PLD | 1 | SLD stage 3 | Yes | OC fract head of capitate | ||
| 7 | PLD | 2A | SLD stage 3 | — | Capitate OK | ||
| 8 | PLD | 2A | SLD stage 3 | — | Capitate OK | ||
| 9 | PLD | 2A | SLD stage 3 | — | Capitate OK | ||
| 10 | PLD | 2A | SLD stage 3 | — | Capitate OK | ||
| 11 | PLD | 2A | SLD stage 3 | — | Capitate OK | ||
| 12 | PLD | 1 | SLD stage 3 | — | Capitate OK | ||
| 13 | PLFD | TS | 1 | SLD stage 2 | Waist commin | Yes | Capitate OK |
| 14 | PLFD | TS | 1 | Intact SL lig | Waist commin | Yes | Capitate OK |
| 15 | PLFD | TS | 1 | Intact SL lig | Waist commin | Yes | OC fract head of capitate |
| 16 | PLFD | TS | 1 | Intact SL lig | Waist commin | Yes | Capitate OK |
| 17 | PLFD | TS | 1 | SLD stage 2 | Waist commin | —- | OC fract head of capitate |
| 18 | PLFD | TS | 1 | Intact SL lig | Proximal pole | —- | OC fract head of capitate |
| 19 | PLFD | TS | 1 | SLD stage 2 | Waist commin | Yes | OC fract head of capitate |
| 20 | PLFD | TS | 2A | Intact SL lig | Waist commin | —- | OC fract head of capitate |
| 21 | PLFD | TS | 2A | Intact SL lig | Proximal pole | —- | Capitate OK |
| 22 | PLFD | TS | 1 | Intact SL lig | Waist commin | Yes | Capitate OK |
| 23 | PLFD | TS TT | 1 | Intact SL lig | Proximal pole | —- | Capitate OK |
| 24 | PLIND—fx | TS | Non dislocated | SLD stage 2 | Waist commin | —- | Capitate OK |
| 25 | PLIND— | Non dislocated | SLD stage 3 | — | Capitate OK | ||
| 26 | PLIND— | Non dislocated | SLD stage 3 | — | Capitate OK | ||
| 27 | PLIND—fx | TL | Non dislocated | SLD stage 1 | —- | Capitate OK |
Abbreviations: OC, osteochondral; PLD, perilunate dislocation; PLFD, perilunate fracture-dislocation; PLIND, perilunate injury, nondislocated; SL, scapholunate; SLD, scapholunate disruption; TL, translunate; TS, transscaphoid; TT, transtriquetral.
A total of 18 patients were available for clinical and radiological review at an average of 27 months of follow-up (minimum 8 months, maximum 79 months).
Outcome measurements included a visual analogue score (VAS) for pain, forearm and wrist motion measurements, and grip strength. A Modified Mayo Wrist Score (MMWS) and Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire (15 patients) were used. In addition we used the Lyon clinical electronic Excel score (Fig. 1), which generates a a graphical representation of the wrist motion using a hexagonal graph (Fig. 2).
Fig. 1.
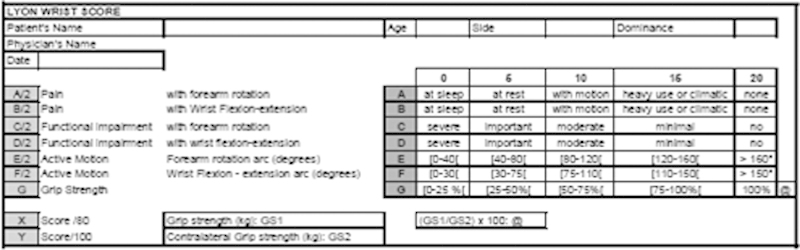
Lyon Excel electronic wrist score.
Fig. 2.
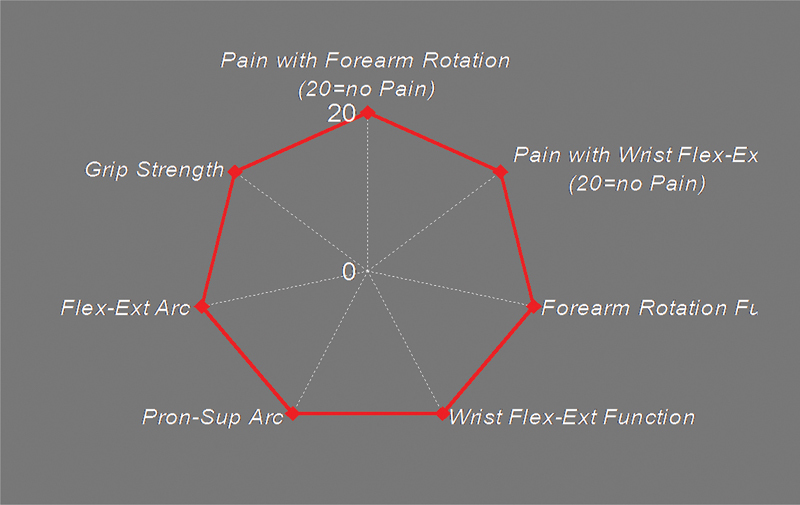
Example of a normal diamond-shaped Lyon wrist score.
Radiographic assessment consisted of standard posteroanterior (PA) and lateral wrist X-rays. Scaphoid healing was assessed when applicable.
Since our follow-up was short-term, we did not study the occurrence of posttraumatic arthritis.
Surgical Technique
Immediate closed reduction under appropriate sedation in the emergency department was successful in all 27 patients.
Traction radiographs confirmed proper gross midcarpal reduction and provided additional information about the path of the injury and the associated chip fractures.
The patient was then referred to our wrist unit.
A computed tomography (CT) scan with three-dimensional reconstructions was performed when all details of the injury could not be completely understood.
Diagnostic wrist arthroscopy using 3–4, 6-R, and midcarpal ulnar and radial portals was performed in all patients.
Dry arthroscopy with the adjunct of “automatic washout sessions” (i.e., simultaneous automatic shaver suction of a volume of fluid equal to the whole water syringe content) was used for all patients. Cartilaginous, bony and ligamentous findings were recorded (Table 1).
In seven patients, percutaneous pinning under arthroscopic control achieved stable fixation.
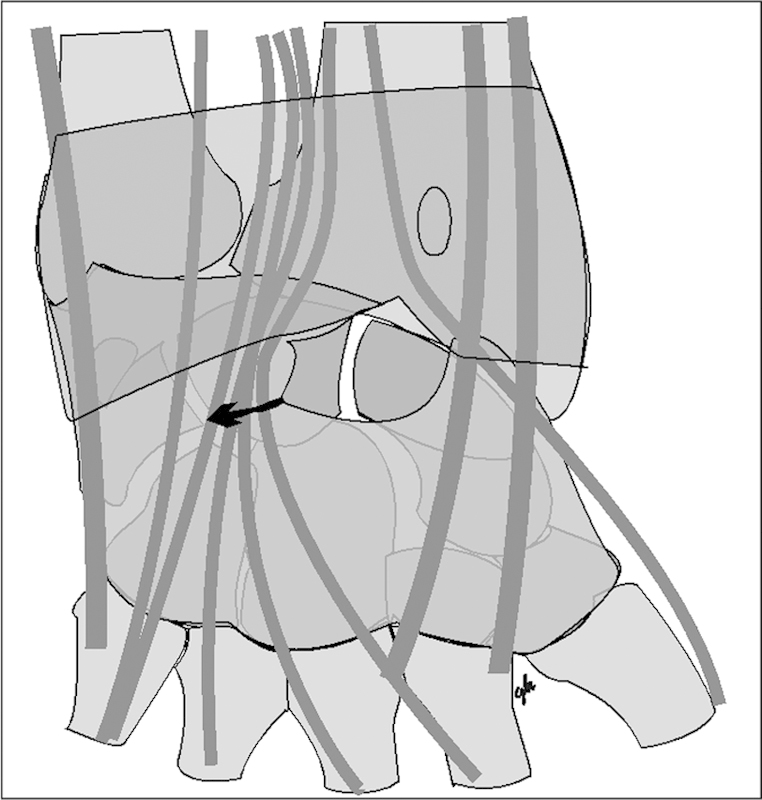
In 20 patients (12 trans-scaphoid PLFD, 6 PLD, and 3 PLIND), a combination of arthroscopy and a mini-open dorsal approach was used. The mini-invasive dorsal approach began with enlarging the 3–4 portal with a horizontal 2.5- to 3-cm skin incision (Fig. 3).
Fig. 3.

Example of the combination of four arthroscopic portals with the horizontal mini-invasive dorsal approach.
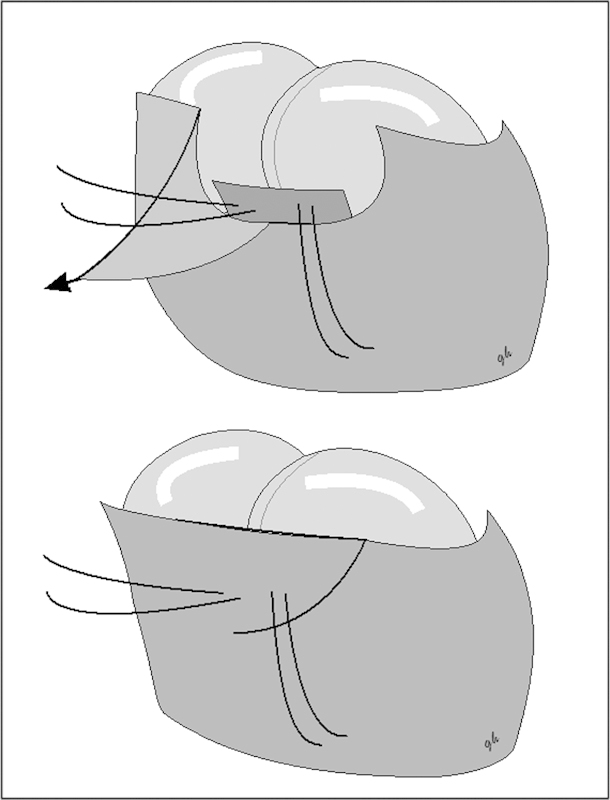
The dorsal finger extensor compartment was not opened. Only a 0.5-mm opening was made over the third compartment to facilitate access to the dorsal wrist capsule. The dorsal wrist capsule was exposed between the third and fourth compartments. A mini-v-shaped capsular incision, preserving the dorsal intercarpal ligament and exposing the scapholunate junction, was made (Fig. 4). When a scaphoid fracture was present, the proximal pole of the scaphoid was exposed along with the fracture line. Dorsal comminuted fragments were removed. An anti-rotational Kirschner wire (K-wire) was first implanted anterograde, followed by an anterograde cannulated screw, or K-wires when it was felt that compression could be deleterious (Fig. 5). The direction of the screw was as perpendicular as possible to the fracture line. Additional pinning was performed of the radiolunate (RL), lunotriquetral (LT), and scapholunate (SL) joints when necessary.
Fig. 4.
Details of the mini-invasive dorsal approach including capsular opening.
Fig. 5.

Example of the use of the horizontal mini-invasive dorsal approach to fix the scaphoid fracture of a transscaphoid PLFD after arthroscopy.
In a pure ligamentous PLI, when it was felt that the dorsal interosseous SL ligament repair was better achieved through an open approach, a direct SL ligament repair was performed with one or two anchors as necessary. The suture was then drawn through the dorsal capsule to allow for a capsulodesis mattress suture after capsular closure (Figs. 6 and 7). Additional radiolunate pinning was performed as well as lunotriquetral joint pinning.
Fig. 6.
Schematic representation of the scapholunate ligament repair used in this study.
Fig. 7.

Example of the use of the horizontal mini-invasive dorsal approach to fix the scapholunate junction of a PLD after arthroscopy.
Postoperative Management
All patients were immobilized in a long-arm cast in neutral forearm rotation for 3 weeks. Then a thermoplastic short-arm cast was applied for a period depending on the injury type and its fixation. All K-wires were removed at 6 weeks. All headless scaphoid screws were left in place. When the K-wires were used for scaphoid fixation, they were not removed until 3 months. A supervised self-rehabilitation program began at 6 weeks when the injury was purely ligamentous (or ligamentous with a scaphoid fixed by a screw) and at 3 months when the scaphoid had been fixed with K-wires. Return to sports and heavy manual activities was not allowed until 4 months.
Results
Arthroscopic Findings
Arthroscopy findings are shown in Table 1. We used Dréant and Dautel's classification for scapholunate dissociation arthroscopic staging.8 In this simple midcarpal arthroscopic classification, stage 1 scapholunate dissociation means the tip of a probe can be introduced into the SL joint space, stage 2 means there is an definite SL diastasis when the probe is twisted into the SL joint space, and stage 3 means the arthroscope itself can be introduced into the SL joint space from midcarpal to radiocarpal joint. Examples of our findings are displayed in Figs. 8 9 10 11 12 13.
Fig. 8.
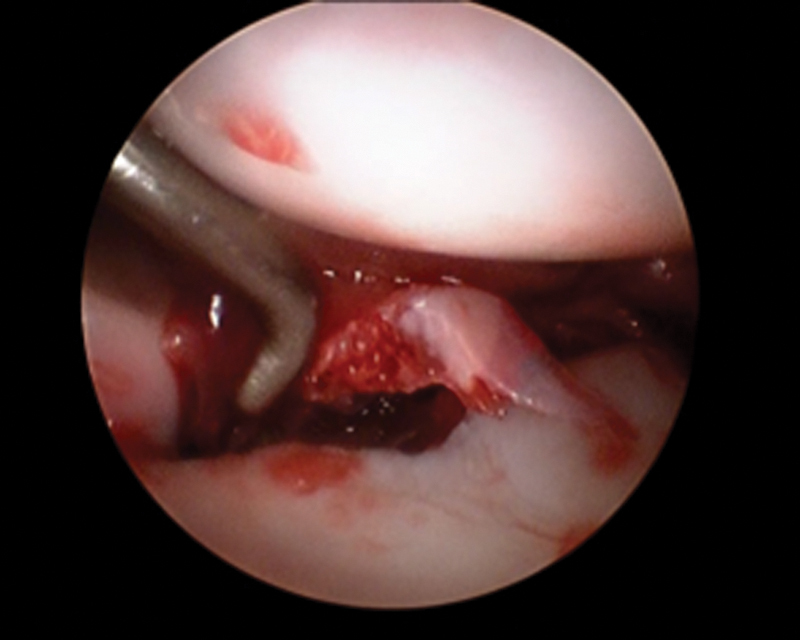
Example of a free osteochondral midcarpal fragment found at arthroscopy in a TS PLFD patient.
Fig. 9.
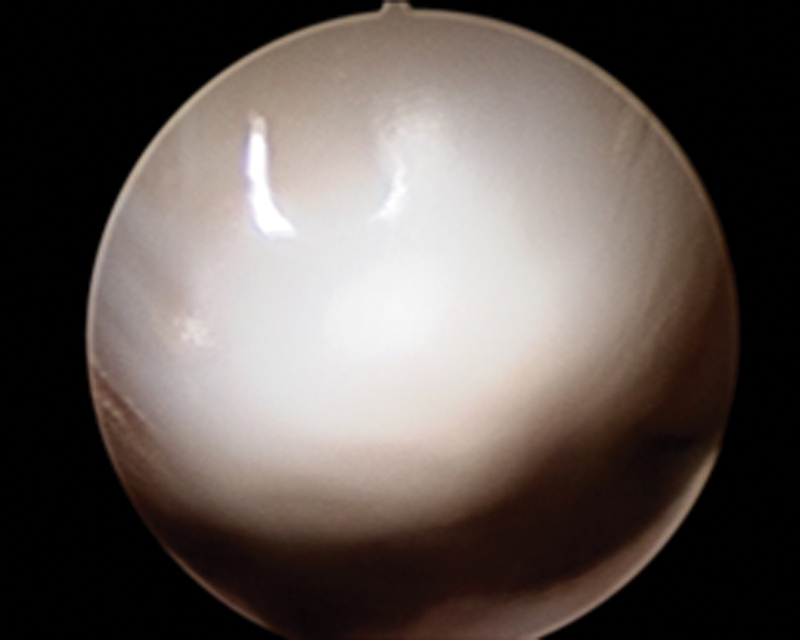
Example of normal capitate cartilage as seen during arthroscopy.
Fig. 10.
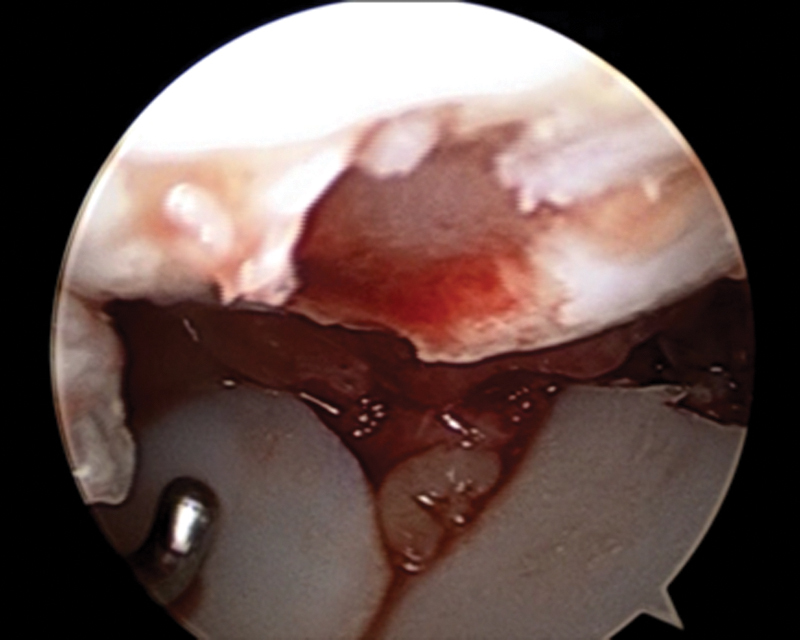
Example of a severe cartilaginous injury to the capitate as seen during arthroscopy.
Fig. 11.
Example of a comminuted waist scaphoid fracture as seen during arthroscopy.
Fig. 12.
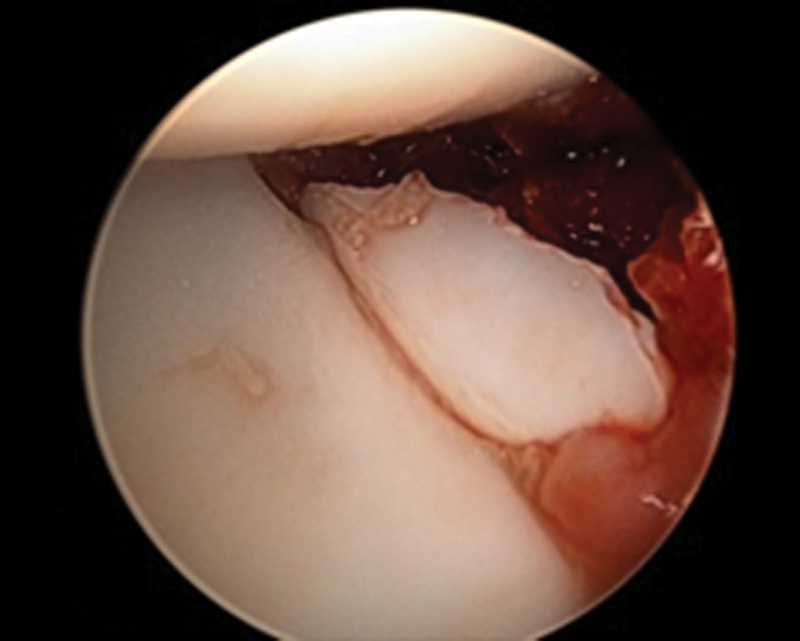
Example of an unusual proximal scaphoid fracture as seen during arthroscopy of a TS PLFD.
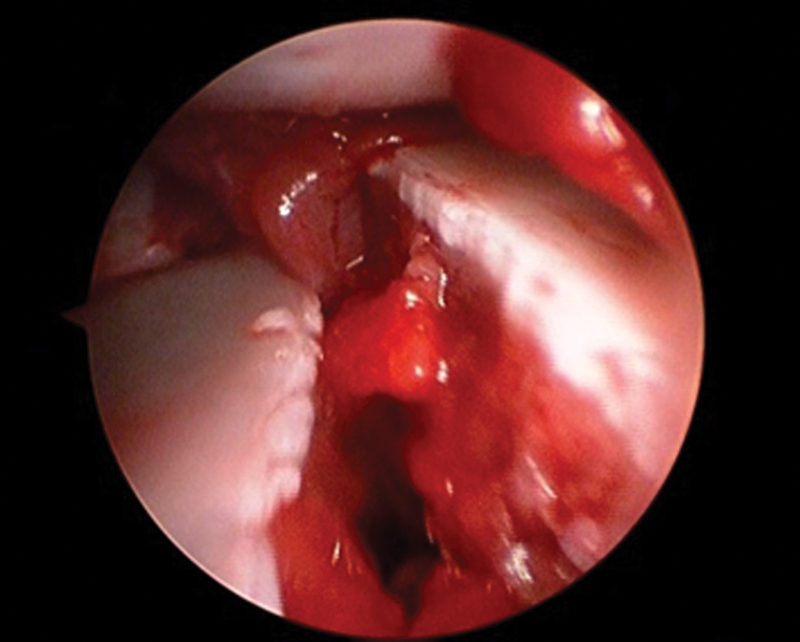
Fig. 13.
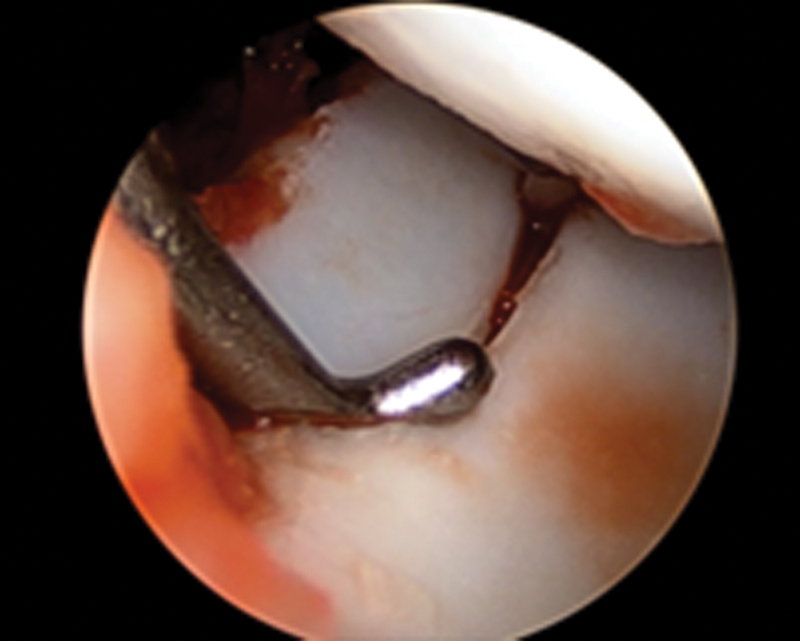
Example of the combination of a scaphoid fracture and scapholunate dissociation as seen during arthroscopy in a TS PLFD.
Clinical and Radiological Outcomes
A total of four patients developed reflex sympathetic dystrophy (RSD). No other complications were observed.
At final follow-up, VAS pain was rated 18/100 on average (minimum 0, maximum 5). The average wrist flexion was 39° (range 15–70°). The average wrist extension was 41° (range 10–60°). The average arc of active wrist flexion-extension was 80°, which was 53% of the normal contralateral side. The average grip strength was 29 kg (range 12–55 kg) which was 69% of the contralateral side. If we consider only the patients without RSD (n = 14), the average wrist active wrist flexion-extension was 87° (58% of the normal contralateral side) and the average grip strength was 30 kg (71% of the normal contralateral side).
The average MMWS was 71 (range 50–90). A total of seven good, six fair, and five poor were observed. A total of three of the poor results displayed RSD during their postoperative period. Two case examples are displayed in Figs. 14 15 16 17 18 19 20.
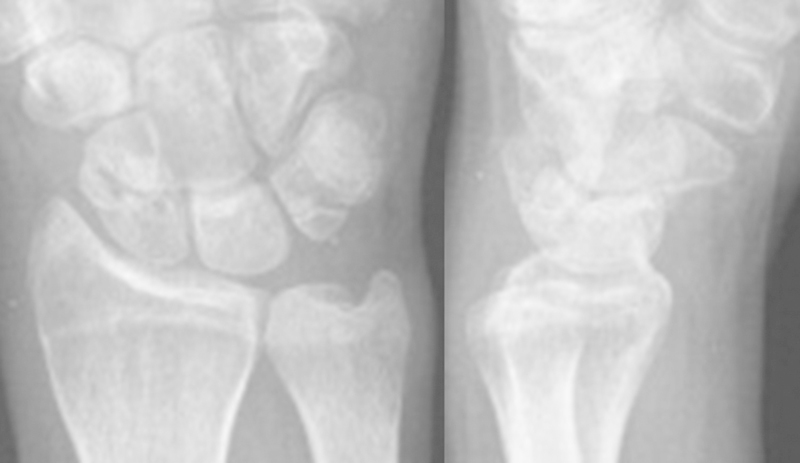
Fig. 14.

Case #1: initial radiographs.
Fig. 15.
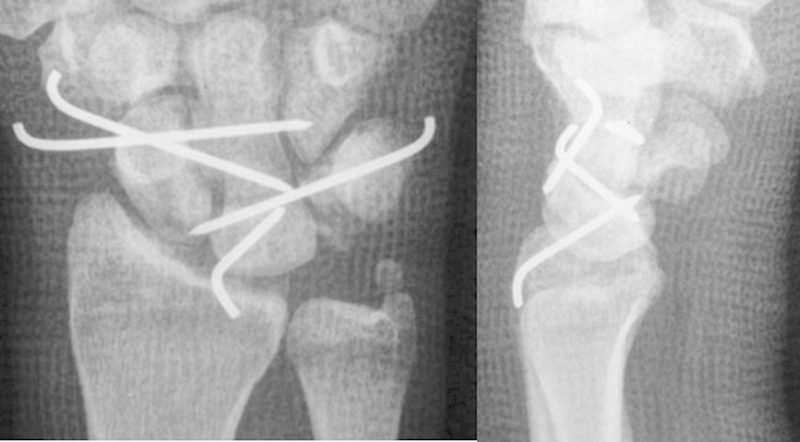
Case #1: K-wire fixation.
Fig. 16.

Case #1: result at 6-years follow-up.
Fig. 17.

Case #1: result at 6-years follow-up, ulnar deviation.
Fig. 18.

Case #16: initial radiographs.
Fig. 19.
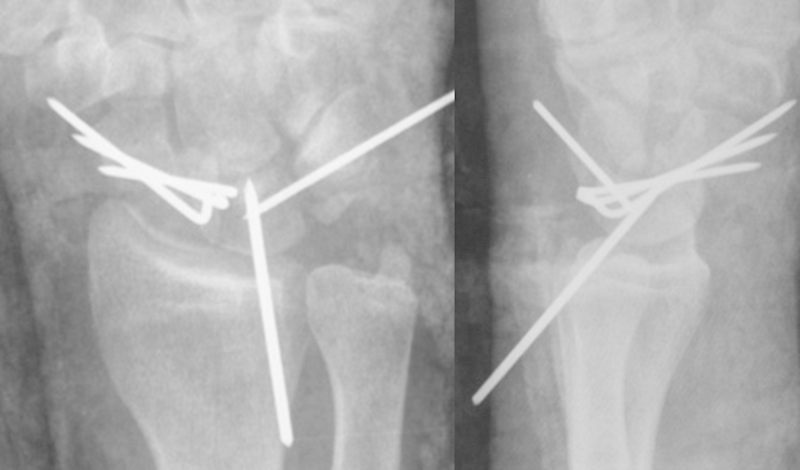
Case #16: K-wire fixation.
Fig. 20.
Case #16: result at 6-months follow-up.
The average QuickDASH, available in 15 patients, was 31 (range 0–59). The Lyon score diamond-shaped chart provided a visual idea of the clinical result (Fig. 21).
Fig. 21.
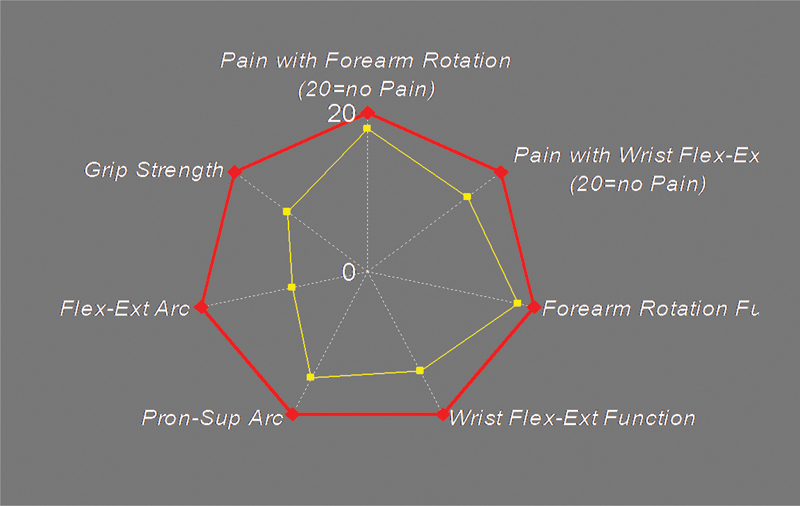
Results of our series of 18 patients as shown with a diamond-shaped Lyon wrist score.
A normal carpal alignment was observed in all 18 patients at follow-up. All scaphoid fractures healed uneventfully.
Discussion
It should be noted that PLIs are rare and severe high-energy injuries, and there are cases with irreparable lesions that must be treated at the acute stage with palliative methods such as proximal row carpectomy. Thus, by definition, a single treatment, such as ORIF, cannot work for all types of PLIs.
The first case report of arthroscopic treatment for perilunate dislocation was published by Savoie in 1995.9 Since then there have been some small series confirming the feasibility of this particular treatment.6
The purpose of the present study was to review retrospectively a series of selected PLIs treated with arthroscopic assistance over the past 10 years. In an attempt to reproduce the good results of ORIF reliably, we used pure arthroscopic surgery only in selected cases. Due to the almost ubiquitous comminution of the scaphoid fractures in PLI, with highly unstable fragments that could lead to suboptimal fixation, we preferred to use an anterograde ORIF.
This study has limitations. It is a retrospective short-term study and could not provide comparative information. However, it is doubtful that a true comparative study could apply to PLI treatment, since not all PLIs are equal regarding the extent of their pathology.
During the same 10-year period, other treatments including immediate palliative treatments (emergency proximal row carpectomies, for example, in the most severe cases) were used in our whole population of PLIs.
In 2002 we reported on 13 dorsal TS PLFDs treated with ORIF through a dorsal approach and reviewed at an average of 8 years follow-up.3 The MMWS averaged 79%. All scaphoid fractures healed. The postoperative wrist flexion-extension arc averaged 112°. Grip strength averaged 79% of the opposite side.
Knoll4 reported on 25 dorsal TS PLFDs treated with ORIF through a dorsal approach and reviewed at an average of 8 years follow-up. They found similar results with a 100% fusion rate of the scaphoid. The postoperative wrist flexion-extension arc averaged 114°. Grip strength averaged 80% of the opposite side.
Trumble5 reported on 22 dorsal PLDs treated with ORIF through combined volar and dorsal approaches with SL ligament repair and stabilization with intraosseous wiring technique. The postoperative wrist flexion-extension arc averaged 106°. Grip strength averaged 77% of the opposite side.
In 2005 Park6 reported on three cases of acute PLI treated with arthroscopy alone. The postoperative wrist flexion-extension arc averaged 107°. Grip strength averaged 85% of the opposite side. In 2012 Kim and Park reported on 20 patients with PLIs treated with arthroscopy alone and reviewed at an average of 31 months follow-up. The postoperative wrist flexion-extension arc averaged 104°. Grip strength averaged 78% of the opposite side. There were 15 TS PLFDs. Two of them went on to nonunion, suggesting that classic ORIF may be more reliable than arthroscopic scaphoid fixation in these highly unstable injuries. This is why we currently prefer to combine arthroscopy and a mini-invasive dorsal approach.
In the present series all scaphoids healed uneventfully. The VAS pain averaged 18/100, which was very acceptable given the extent of the injury. The postoperative wrist flexion-extension arc averaged 80°. This was not better than what was observed after ORIF in the literature. Grip strength averaged 69% of the opposite side, which again was not better than after ORIF. It was the surgeon's opinion, however, that the short-term follow-up period after mini-invasive surgery was more comfortable, with less pain and an earlier rehabilitation.
Acknowledgments
We thank Mireille Orjollet for her help in the preparation of the manuscript.
Footnotes
Conflict of Interest None
References
- 1.Herzberg G. Perilunate and axial carpal dislocations and fracture-dislocations. J Hand Surg Am. 2008;33(9):1659–1668. doi: 10.1016/j.jhsa.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 2.Forli A, Courvoisier A, Wimsey S, Corcella D, Moutet F. Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up. J Hand Surg Am. 2010;35(1):62–68. doi: 10.1016/j.jhsa.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg [Br] 2002;27(6):498–502. doi: 10.1054/jhsb.2002.0774. [DOI] [PubMed] [Google Scholar]
- 4.Knoll V D, Allan C, Trumble T E. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg Am. 2005;30(6):1145–1152. doi: 10.1016/j.jhsa.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am. 2004;29(3):412–417. doi: 10.1016/j.jhsa.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Park M J, Ahn J H. Arthroscopically assisted reduction and percutaneous fixation of dorsal perilunate dislocations and fracture-dislocations. Arthroscopy. 2005;21(9):1153. doi: 10.1016/j.arthro.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 7.Herzberg G. Perilunate injuries, non dislocated (PLIND) J Wrist Surg. 2013;2(4):337–345. doi: 10.1055/s-0033-1358548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dréant N, Dautel G. Elaboration d'un score de sévérité arthroscopique pour les instabilités scapholunaires. Chir Main. 2003;22(2):90–94. doi: 10.1016/s1297-3203(03)00018-0. [DOI] [PubMed] [Google Scholar]
- 9.Savoie F H III, Grondel R J. Arthroscopy for carpal instability. Orthop Clin North Am. 1995;26(4):731–738. [PubMed] [Google Scholar]


