Abstract
INTRODUCTION
Weight loss reduces co-morbidities of obesity, but decreases bone mass.
PURPOSE
Our aims were to 1) determine if adequate dairy intake attenuates weight loss-induced bone loss; 2) evaluate the associations of endocrine, inflammatory and bone markers, anthropometric and other parameters to bone mineral density and content (BMD, BMC) pre- and post-weight loss; 3) model the contribution of these variables to post weight-loss BMD and BMC
METHODS
Overweight/obese women (BMI: 28–37 kg/m2) were enrolled in an energy reduced (−500 kcal/d; −2092 kJ/d) diet with adequate dairy (AD: 3–4 servings/d; n=25, 32.2 ± 8.8y) or low dairy (LD: ≤ 1 serving/d; n=26, 31.7 ± 8.4 y). BMD, BMC and body composition were measured by DXA. Bone markers (CTX, PYD, BAP, OC), endocrine (PTH, vitamin D, leptin, adiponectin, ghrelin, amylin, insulin, GLP-1, PAI-1, HOMA) and inflammatory markers (CRP, IL1-β, IL-6, IL-8, TNF-α, cortisol) were measured in serum or plasma. PA was assessed by accelerometry.
RESULTS
Following weight loss, AD intake resulted in significantly greater (p= 0.004) lumbar spine BMD and serum osteocalcin (p=0.004) concentration compared to LD. Pre- and post- body fat were negatively associated with hip and lumbar spine BMC (r= −0.28, p=0.04 to −0.45, p=0.001). Of note were the significant negative associations among bone markers and IL-1β, TNFα and CRP ranging from r = −0.29 (p=0.04) to r = −0.34 (p=0.01); magnitude of associations did not change with weight loss. Adiponectin was negatively related to change in osteocalcin. Factor analysis resulted in 8 pre- and post-weight loss Factors. Pre-weight loss Factors accounted for 13.7% of the total variance in pre-weight loss hip BMD; post-weight loss Factors explained 19.6% of the total variance in post-weight loss hip BMD. None of the Factors contributed to the variance in lumbar spine BMD.
CONCLUSION
AD during weight loss resulted in higher lumbar spine BMD and osteocalcin compared to LD. Significant negative associations were observed between bone and inflammatory markers suggesting inflammation suppresses bone metabolism. Using Factor Analysis, 19.6% of total variance in post-weight loss hip BMD could be explained by endocrine, immune, and anthropometric variables, but not lumbar spine BMD.
Keywords: weight loss induced bone loss, endocrine and inflammatory markers, physical activity, body composition
1.0 INTRODUCTION
Weight loss has well-established benefits for reducing co-morbidities associated with obesity [1]. However, even moderate weight loss (5 to 15%) increases bone turnover [2–7] and decreases bone mineral density (BMD) by 1 to 4% at different regional sites (mostly hip and spine) in obese and overweight premenopausal women [8–11]. Offering suitable nutritional options for weight loss diets that preserve bone mass and maintain normal bone turnover is clearly warranted. The exact mechanisms of action for weight loss induced bone loss are unknown; however, reduced calcium intake during energy restriction represents one possibility. Higher calcium and/or dairy-based weight loss diets have received attention for their potential to prevent weight loss induced bone loss. In weight loss interventions, higher calcium intake increased lumbar spine BMD [2, 12] and attenuated the increase in bone turnover [2, 6–7] in pre-and postmenopausal women. These findings were confirmed by Thorpe et al. [13] and Bowen [3] while Josse et al. [14] observed an increase in bone resorption markers in premenopausal women consuming a low dairy diet.
Another possible explanation for weight loss related bone loss may be the interaction among endocrine, inflammatory or immune processes and bone turnover. Recently Karsenty and Ferron [15] reviewed the role of the skeleton as an endocrine organ and its interaction with energy-related hormones like leptin and insulin. They suggested that bone metabolism is an energetically expensive process, which might explain why the skeleton both controls and responds to energy-related signals, e.g. leptin [16–18]. Cornish and colleagues provide an overview of this topic with foundational papers that have shown distribution of leptin receptors in a variety of tissues and the expression of the signaling form of the leptin receptor in osteoblasts, suggesting bone as a target of action [19, 20]. Similarly, receptors for adiponectin (AdipoR1, AdipoR2) have been found on both osteoblasts and osteoclasts; the implication being a direct effect of this hormone on osteoblast proliferation and inhibition of osteoclastogenesis [21, 22]. Additionally, immune responsive inflammatory cytokines may also contribute to changes in bone metabolism [23] during periods of stress or inflammation which can occur with obesity. Therefore, the purpose of the current study was to evaluate data from a controlled feeding study with 51 overweight or obese adult women consuming a reduced energy diet that included either Low Dairy (LD) (≤ 1 serving/d) or Adequate Dairy (AD) (3–4 servings/d) intake [24] 1) to determine if adequate dairy intake prevents weight loss related bone loss; 2) evaluate the associations among endocrine, inflammatory and bone markers, and anthropometric and other parameters to bone mineral density and content (BMD, BMC) pre- and post-weight loss; and 3) to explore the contribution of these variables to pre – and post- weight loss BMD using a multivariate model.
2.0 PARTICIPANTS AND METHODS
2. 1 Study Design
The study design and participant characteristics are described in detail elsewhere [24]. Briefly, overweight or obese premenopausal women (BMI 28 – 37 kg/m2) were enrolled in a 15 week controlled feeding study; all foods were provided or prepared by the Metabolic Food Laboratory at the USDA, ARS, Western Human Nutrition Research Center (WHNRC). The 15 week study was initiated with a 3 week run-in period during which women were weighed daily while consuming energy intake based on Dietary Reference Intakes [26], but adjusting caloric intake to maintain body weight; thereby establishing baseline energy requirements. A 12-week energy reduction period followed (−500 kcal/d; −2092 kJ/d). All procedures related to the study were approved by the Institutional Review Board for the Protection of Human Subjects at the University of California, Davis. All participants were informed of the study requirements and written informed consent was obtained prior to participation. The study was registered with ClinicalTrials.Gov (NCT00858312).
2.1.1 Screening and Selection
Adult females (n=51) from the weight loss study were evaluated for changes in bone mass, density, and turnover indices. Women were recruited from the faculty, staff, and student populations at UC Davis, and the greater Davis and Sacramento communities. The age criterion was 20 – 45 years. All participants were habitually low dairy consumers, ≤ 1 serving of dairy/d, and total typical calcium intake ≤ 600 mg/d. Details regarding other selection criteria have been previously published [25]. Body composition was assessed during the ‘run-in’ period using DXA to determine body fat and lean masses as well as lumbar spine and hip BMD and BMC. Participants were pair-matched based on percent body fat then assigned to LD or AD groups [24] so that at the time of enrollment the group average for percent body fat was not different between the LD and AD groups.
2.1.2 Food Intake and Compliance
The diets provided comparable levels of macronutrient and fiber (fat ~35% of total energy, carbohydrates ~49%, protein ~16%; fiber 8 – 10 g/1000 kcal). During the run-in period and the first 2 weeks of restriction 2 of the 3 meals/d were eaten at the WHNRC. For weeks 3 – 9 of intervention participants were “free living,” but all food was weighed, measured, and provided by the WHNRC metabolic kitchen staff and “packed to go” for each individual. The AD diet included 3–4 servings of milk, yogurt and cheese per day; averaging 1339 mg/d of calcium intake from all sources. The LD diet had ≤ 1 serving of dairy/d e.g. milk, yogurt or cheese with an average calcium intake of 460 mg/d calcium from all sources.
2.1.3 Body Composition and Bone Measurements
Body weight was measured to the nearest 0.1 kg with women in light clothing (shoes and jewelry removed; Scale-tronix, Inc. Wheaton, IL, USA). Height was measured using a wall-mounted stadiometer (Ayrton Stadiometer, Model S100; Ayrton Corp. Prior Lake, MN, USA) and recorded to the nearest 0.1 cm. Body mass index (BMI) was calculated as kg/m2. BMD and BMC of the lumbar spine and total hip were assessed using DXA (GE Lunar, Prodigy Model; Madison, WI, USA; software version: enCORE 2006, version 10.50.086) during the run-in period (Pre) and at the end of intervention (Post). Participants were positioned on their back with feet secured to a plexiglas Λ-holder, provided by the manufacturer, to insure proper rotation of femur for the hip scan. Following the hip scan and while still positioned on the back, participant’s legs were raised onto a solid-foam block, provided by the manufacturer, to ensure that the spine was flat against the scan table for the lumbar spine scan. Lumbar vertebrae L1 – L4 were scanned, but only the average values for L2–L4 were used in the data analysis. Whole body DXA was done to assess body composition, e.g. body fat (kg, %) and lean mass (kg). Whole body scan was done positioned on the back, feet strapped together, per manufacturer’s guidelines, and hands placed flat on the table adjacent to the side of the body. Daily calibration procedures were done per manufacturer instructions. Repeated measures of instrument calibration phantom was done throughout the course of the study (11/2006 – 6/2009) and gave coefficients of variation of 0.07%, 0.01% and 0.3% for high, medium and low BMD, respectively. The CV for lumbar spine phantom L2–L4 was 0.09%; for lean and fat masses were 0.8% and 0.0%, respectively. To reduce variance in the data, DXA scans were analyzed by a single operator.
2.1.4 Assessment of Physical Activity (PA)
Women were instructed to maintain their usual physical activity throughout the study. Physical activity was monitored using an Actical physical-activity-monitoring device (Philips Electronics, Bend, OR, USA). The Actical is an omni-directional accelerometer that provides an objective and quantifiable measure of physical activity. Digital integration data acquisition incorporates intensity of movement into the activity count for sedentary, light, moderate, and vigorous levels of activity. Women were instructed to wear the Actical during all waking hours, except for bathing or swimming, for 7 days. The Actical was attached to a belt and worn over the left hip. At the end of the week, women returned the Actical to the WHNRC Physiology Support Laboratory where the data were downloaded for confirmation of the number of days of data collection, frequency, and intensity of activity sessions. One day was considered complete if the Actical contained at least 12 hours of data. If there were fewer than 5 weekdays and 2 weekend days of recorded data, the Actical was returned to the participant for additional days of data collection. PA data were collected during the run-in pre- weight loss period and every 3 weeks during intervention. PA records were analyzed for sedentary, light, moderate and vigorous and expressed in two ways as 1) energy expenditure for each level of activity and 2) time spent at each activity level, e.g. min/d or hr/d. A comparison of the run-in pre-weight loss PA data and the weeks during intervention indicated that women were compliant with instructions not to change their physical activity.
2.1.5 Analytical Assays
Blood was collected by venipuncture following an overnight fast. Serum and plasma were stored at −80° C until analyzed. Bone turnover markers were assessed in sera samples pre- and post- weight loss. The ELISA assay for bone specific alkaline phosphatase (BAP) utilized a monoclonal anti-BAP antibody coated on the strip to capture BAP in the sample (Metra BAP; Quidel Corp. San Diego, CA, USA). C terminal telopeptide of type I collagen (CTX) (Crosslaps; Nordic Bioscience Diagnostics, Denmark) was measured using two antibodies that recognize two cross linked amino acid sequences. Serum pyridinoline (PYD) was analyzed using the enzyme immunoassay for the quantitation of pyridium crosslinks kit by Metra (Quidel Corp. San Diego, CA USA). Osteocalcin was analyzed in serum using an ELISA assay (DiaSorin, Stillwater, MN, USA). Serum 25(OH)vitamin D (25(OH)D) was analyzed using a DiaSorin (Stillwater, MN, USA) 25(OH)D assay consisting of a 2 step procedure. The first step involved the rapid extraction of the 25(OH)D and other hydroxylated metabolites from serum with acetonitrile. Following extraction, treated samples were assayed using an equilibrium radioimmunoassay (RIA) procedure. The assay was based on an antibody with specificity for 25(OH)D. Serum 1,25(OH)2vitamin D (1,25(OH)2D) was analyzed using an Immunodiagnostics Systems (Fountain Hills, AZ, USA) RIA assay that is a complete assay system for the purification of 1,25(OH)2D in samples by immuno-extraction followed by quantitation by 125I. The WHNRC participates in the Vitamin D External Quality Assessment Scheme (DEQAS) and calibration standards of 25(OH)D and 1,25(OH)2D from DEQAS were analyzed in the same batch with participant samples. Intact parathyroid hormone (PTH) was analyzed using an Immulite instrument and a solid phase two site chemiluminescent enzyme labeled immunometric assay (Siemens Diagnostics; Deerfield, IL, USA).
Serum cortisol and serum high sensitivity CRP (C-reactive protein) were analyzed using an Immulite instrument and a solid phase two-site chemiluminescent enzyme labeled immunometric assay (Siemens Diagnostics, Deerfield, IL, USA). The endocrine hormones ghrelin and GLP-1 were analyzed from EDTA plasma containing a cocktail of inhibitors: whole blood was collected into EDTA vacutainers that contained the following additives: DPPIV inhibitor (dipeptidyl-peptidase IV inhibitor (Millipore, St. Charles, MO, USA) 10μl/ml whole blood), aprotinin ((G-Biosciences, St. Louis, MO, USA) 240 KIU/ml whole blood), and protease inhibitor cocktail (Sigma P2714, Sigma-Aldrich, St. Louis, MO, USA). In addition, for the ghrelin aliquot, a 1M HCl (Trace Metal Grade HCl, Fisher-Scientific, Pittsburgh, PA, USA) solution was added (100μl/ml plasma) prior to plasma storage at −80C. Ghrelin and GLP-1 were analyzed using ELISA kits (Human Ghrelin (active), EZGRA-88K, GLP-1 (active), EGLP-35K, Millipore, St. Charles, MO, USA). PAI-1 (plasminogen activator inhibitor-1) was analyzed with an ELISA kit (Technoclone Human Technozym PAI-1 Actibind ELISA TC16075, Technoclone, Vienna, Austria). Adiponectin was analyzed using a multiplex adipokine panel (Millipore HADK1-61K-A) with a Luminex reader (BioPlex, Bio-Rad, Richmond, CA, USA). Amylin was analyzed with an ELISA kit (Millipore Amylin (active) EZHA-52K). Insulin, leptin, IL-1β, IL-6, IL-8 and TNF-α were analyzed using a multiplex adipokine panel (Millipore HADK2-61K-B, St. Charles, MO, USA) with a Luminex reader (BioPlex, Bio-Rad, Richmond, CA, USA). Glucose was determined in serum using standard procedures on a clinical chemistry analyzer (Hitachi 902; Roche Diagnostics) with instrument specific reagents (Roche Diagnostics Corporation, Indianapolis, IN). HOMA, a measure of insulin resistance, was calculated using the equation HOMA-IR= (glucose × insulin)/405.
3.0 STATISTICS
Shapiro-Wilk test was used to determine normal distribution of variables and transformed as needed. Differences in pre-weight loss measurements between groups were assessed using independent t-tests or Mann-Whitney U tests if the variables could not be normalized. Analysis of covariance (ANCOVA) was used to determine if final bone markers, BMC or BMD values were significantly different by treatment group (LD, AD) after controlling for initial values. Pearson correlation coefficients were examined among body composition, BMD, BMC, PTH, vitamin D, bone, endocrine and inflammatory markers, and physical activity.
We used exploratory factor analysis to examine our third objective on the contribution of endocrine and immune responses to weight loss induced bone loss. Factor analysis describes the variability among correlated variables and reduces the number of variables to a set number of “factors.” The factors represent a linear combination of potential variables plus error. The information gained from the interdependencies between variables can be used to reduce a large number of related variables in the dataset to just a few factors that account for all the variables. These factors are used to identify complex interrelationships among variables that are part of a unified concept with no a priori assumptions about the relationships among the factors. We used the Kaiser recommendation for factors using eigenvalues > 1 with varimax rotation to maximize the variance of the squared loadings of a factor on all the variables in the factor matrix; thus giving each factor a large or small loading for any particular variable. Rotational factors with coefficients closest to 1 were included in the same factor. The factor analysis reduced the number of variables, 88 variables pre- and 88 variables post-weight loss to just 8 Factors pre- and post-weight loss, respectively. Backward stepwise multiple regression analysis was used to evaluate the contribution of the 8 factors, representing the inter-relationship of endocrine, inflammatory and bone markers, body composition and physical activity variables, to pre- and post-weight loss lumbar spine and hip BMD. Probability was set at the 0.15 level of significance for inclusion in the model. This approach allowed us to ask the questions: which Factor(s) accounted for the variance in BMD before weight loss and which Factor(s) contributed to the variance in BMD after weight loss? All analyses were conducted using the SAS statistical package (version 9.2; SAS Institute Inc, Cary, NC, USA). Values reported are mean ± standard deviation (SD); significance was set at the p < 0.05 level of probability.
4.0 RESULTS
Characteristics of the women pre-weight loss are shown in Table 1. All women were premenopausal and age ranged from 19.9 to 45. 8 years. Not one of the women was osteoporotic based on their total hip and lumbar spine T scores (< 2.5) [hip range: −1.1 to 2.9; spine range: −0.9 to 3.7]. Serum BAP and osteocalcin (OC) were within reference ranges at baseline; 6.3 – 34.9 U/L and 3.8 – 11.2 ng/ml, respectively [26]. CTX and PYD ranged from 0.197 – 1.363 ng/mL and 4.5 – 28.8 ng/ml, respectively at baseline; reference ranges are 0.04 – 1.19 ng/ml and 16.0 – 37.0 ng/ml for CTX and PYD, respectively [26]. Prior to weight loss average serum values for 25(OH)D were below recommended levels (i.e. approximately 70–80 nmol/L) and ranged from 10 – 80 nmol/L; values for PTH ranged from 26 – 156 pg/ml and did not change during the intervention. Serum values for endocrine and inflammatory markers are also displayed in Table 1 and did not differ by group.
Table 1.
Physical Characteristics, Physical Activity and Bone, Endocrine, and Inflammatory Characteristics in Overweight and Obese Women Prior to a 15 Week Weight Loss Intervention
| Low Dairy (n=26) | Adequate Dairy (n=25) | Probability < 0.05 | |
|---|---|---|---|
| Age, y | 33.2 ± 8.8 | 31.7 ± 8.4 | NS |
| HT, m | 1.64 ± 0.08 | 1.65 ± 0.06 | NS |
| WT, kg | 89.2 ± 8.6 | 87.8 ± 10.1 | NS |
| BMI, kg/m2 | 32.2 ± 2.5 | 32.9 ± 2.5 | NS |
| Lean Mass, kg | 42.9 ± 5.5 | 44.1 ± 5.1 | NS |
| Body Fat, (%) | 47.6 ± 3.8 | 45.7 ± 3.6 | NS |
| Spine BMD, g/cm2 | 1.298 ± 0.112 | 1.303 ± 0.151 | NS |
| Hip BMD, g/cm2 | 1.116 ± 0.102 | 1.134 ± 0.124 | NS |
| Spine BMC, g | 54.0 ± 8.5 | 53.65 ± 10.9 | NS |
| Hip BMC, g | 34.8 ± 5.2 | 34.75 ± 4.9 | NS |
| BAP, U/L | 20.1 ± 7.5 | 20.4 ± 6.2 | NS |
| CTX, ng/ml | 0.50 ± 0.29 | 0.52 ± 0.20 | NS |
| PYD, ng/ml | 11.7 ± 5.4 | 10.9 ± 3.6 | NS |
| OC, ng/ml | 5.9 ± 0.3 | 6.7 ± 1.6 | NS |
| 25(OH)D, nmol/L | 39.0 ± 16.0 | 33.0 ± 12.5 | NS |
| PTH, pg/ml | 42.9 ± 15.5 | 44.9 ± 19.2 | NS |
| Leptin, ng/ml | 26.7 ± 21.5 | 36.5 ± 21.7 | NS |
| Adiponectin, μg/ml | 13.5 ± 8.1 | 14.2 ± 7.8 | NS |
| Ghrelin, pg/ml | 254.4 ± 137.2 | 224.3 ± 92.6 | NS |
| Amylin, pM | 9.0 ± 13.6 | 11.3 ± 27.1 | NS |
| GLP-1, pM | 3.3 ± 3.5 | 3.7 ± 5.9 | NS |
| PAI-1, U/ml | 18.7± 18.4 | 20.7 ± 15.0 | NS |
| Insulin, pg/ml | 220.5 ± 111.6 | 292.5 ± 235.1 | NS |
| Cortisol, μg/dl | 12.3 ± 4.6 | 11.6 ± 4.6 | NS |
| IL1β, pg/ml | 0.50 ± 0.5 | 0.69 ± 1.3 | NS |
| IL-6, pg/ml | 4.4 ± 5.4 | 3.1 ± 2.5 | NS |
| IL-8, pg/ml | 1.5 ± 1.0 | 1.7 ± 1.2 | NS |
| TNF-α, pg/ml | 3.1 ± 1.9 | 3.6 ± 1.7 | NS |
| CRP, mg/L | 2.5 ± 3.6 | 3.4 ± 5.0 | NS |
| Sedentary PA, hr/d | 17.8 ± 2.1 | 17.4 ± 1.5 | NS |
| Light PA, min/d | 197.0 ± 64.0 | 202.2 ± 41.6 | NS |
| Moderate PA, min/d | 134.2 ± 74.7 | 156.2 ± 57.9 | NS |
| Vigorous PA, min/d | 0.6 ± 1.7 | 3.3 ± 6.8 | NS |
Values are Mean ± SD. NS = not significant different. WT = weight; BMD = bone mineral density; BMC = bone mineral content; BAP = bone alkaline phosphatase; CTX = carboxy-terminal crosslinks; PYD = pyridinoline crosslinks; OC = osteocalcin; 25(OH)D = 25(OH)vitamin D; PTH = parathyroid hormone; GLP-1 = glucagon like peptide-1; PAI-1 = plasminogen activator inhibitor-1; IL= interleukin; TNF-α = tumor necrosis factor- alpha; CRP = c-reactive protein; PA = physical activity;
No significant differences were observed between treatment groups at baseline in physical characteristics, bone, endocrine or inflammatory parameters, nor in time spent in physical activity. As previously reported in the entire cohort containing men and women [24], body weight and fat changed significantly over time (p < 0.001), but not by treatment group. Lean body mass (LBM) did not change (▲ LBM=0.87kg ±1.49kg). We also confirmed that change in weight, fat or LBM was not different between treatment groups for this subsample of only women. Therefore, statistical control for change in body weight, fat or LBM was not necessary in further data analysis.
After controlling for initial BMD, lumbar spine BMD post-weight loss was significantly greater in the AD group compared to the LD group (p = 0.0042, Figure 1A). There was a decline of 1.4% in lumbar spine BMD for the LD group while the AD group experienced a 0.5% increase in BMD resulting in an overall difference of 2.9% between groups after weight loss. Both LD and AD experienced a small increase in osteocalcin, however, after adjusting for pre-weight loss differences, the increase in osteocalcin for AD group was significant compared to the LD. Although the LD group had a 4.1% increase in osteocalcin compared to the 1.8% increased observed in the AD group, the AD group had more variability in pre- values (standard deviation of 1.6 for AD and 0.3 for LD), therefore, the pre-weight loss covariate adjustment was more influential in the AD group (p = 0.004, Figure 1B). There were no significant differences by treatment group in hip BMD or BMC, nor in bone resorption markers (CTX, PYD), or BAP.
Figure 1.
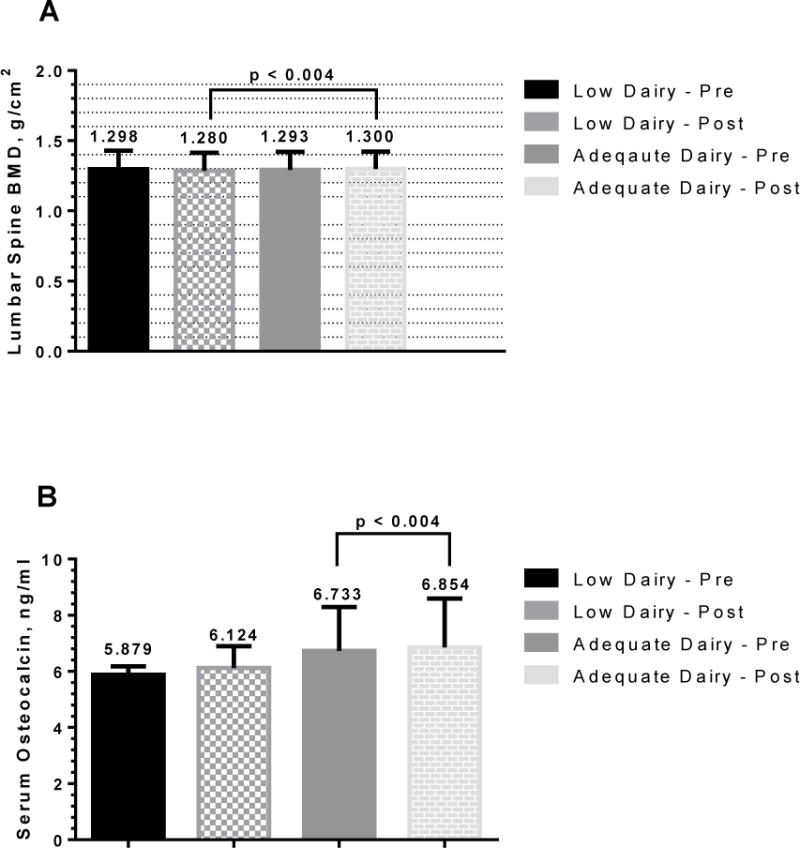
Differences in Lumbar Spine Bone Mineral Density and Serum Osteocalcin by Treatment Group Post-Weight Loss
1A: Adequate Dairy (AD) group had significantly greater lumbar spine bone mineral density compared to the Low Dairy (LD) group following weight loss and after controlling for pre-weight loss levels using ANCOVA. Values are means ± SD.
1B: Serum osteocalcin (OC) was significantly higher in the AD group compared to the LD group after weight loss and controlling for pre-weight loss levels using ANCOVA. Values are means ± SD.
Significant correlations among lumbar spine and hip BMD, BMC, body composition and endocrine variables are shown in Table 2. Pre- and post-weight loss lumbar spine and hip BMC were negatively associated with % body fat pre- and post-weight loss and change in % body fat. Leptin, pre- and post-weight loss, was positively associated with change in lumbar spine BMD. Pre- and post-weight loss HOMA were positively associated with pre- and post-weight loss hip BMD. Insulin and PAI-1 were positively related to hip BMC pre- and post-weight loss.
Table 2.
Significant Associations among Body Composition, Physical Activity, Endocrine and Bone Markers, and Lumbar Spine and Hip BMD and BMC in Fifty-one Women Pre- and Post-Weight Loss
| Pre WT, kg |
Post WT, kg |
Pre Fat % |
Post Fat % |
▲ Fat % |
Pre Leptin |
Post Leptin |
Pre HOMA |
Post HOMA |
Pre Insulin |
Post Insulin |
Pre PAI 1 |
Post PAI 1 |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ▲ Lumbar Spine BMD | 0.28 (0.05) | 0.31 (0.005) | |||||||||||
| Pre Lumbar BMC | 0.335 (0.02) | 0.28 (0.05) | −0.32 (0.02) | −0.33 (0.02) | |||||||||
| Post Lumbar Spine BMC | 0.375 (0.01) | 0.32 (0.02) | −0.28 (0.04) | −0.33 (0.02) | −0.30 (0.03) | ||||||||
| Pre Hip BMD | 0.48 (0.004) | 0.43 (0.002) | |||||||||||
| Post Hip BMD | 0.38 (0.006) | 0.35 (0.01) | |||||||||||
| Pre Hip BMC | −0.45 (0.002) | −0.45 (0.001) | −0.36 (0.01) | 0.33 (0.02) | 0.31 (0.03) | 0.28 (0.05) | |||||||
| Post Hip BMC | −0.42 (0.002) | −0.45 (0.001) | −0.35 (0.01) | 0.29 (0.04) | |||||||||
| ▲ GLP1 | 0.29 (0.04) | ||||||||||||
| AIL-1β | 0.36 (0.01) | ||||||||||||
| Pre PAI-1 | −0.30 (0.03) | ||||||||||||
| PA Light | 0.28 (0.05) | ||||||||||||
| ▲ PA Light | −0.29 (0.04) | ||||||||||||
| Post HOMA | −0.33 (0.02) | −0.28 (0.05) | |||||||||||
| Pre-BAP | 0.28 (0.04) | 0.32 (0.02) | |||||||||||
| Post BAP | 0.33 (0.02) |
Values are Pearson correlations (r) with (p values) below.
Pre = prior to weight loss; post = after weight loss; ▲= change; BMD = bone mineral density; BMC = bone mineral content; WT = weight; PAI-1 = plasminogen activator inhibitor-1.
Significant associations among endocrine and inflammatory markers, body fat and bone markers pre- and post-weight loss are displayed in Table 3. Pre- and post-weight loss adiponectin was inversely associated with change in osteocalcin while post-weight loss ghrelin and change in ghrelin were positively correlated to pre- and post-weight loss osteocalcin BAP and OC. However, pre- and post-weight loss IL-1β and TNF-α were inversely related to post-weight loss BAP. Post-weight loss TNF-α was also negative associated with post-weight loss OC. Pre-weight loss CRP was inversely related to post-weight loss CTX and change in CTX.
Table 3.
Significant Associations Among Pre- and Post Weight Loss Bone Markers and Body Composition, Endocrine and Inflammatory Markers in Fifty-one Women
| Pre Adipo- nectin |
Post Adipo- nectin |
Post HOMA |
Post Ghrelin |
▲ Ghrelin |
Pre IL-1β |
Post IL-1β |
Pre TNF-α |
Post TNF-α |
Pre CRP |
Post Fat % |
▲ Fat % |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre BAP | 0.32 (0.02) | 0.36 (0.01) | ||||||||||
| Post BAP | −0.29 (0.04) | −0.31 (0.02) | −0.29 (0.04) | −0.29 (0.04) | 0.41 (0.003) | |||||||
| ▲ BAP | ||||||||||||
| Pre OC | 0.37 (0.01) | |||||||||||
| Post OC | 0.28 (0.04) | −0.30 (0.03) | ||||||||||
| ▲ OC | −0.33 (0.02) | −0.33 (0.02) | ||||||||||
| Post CTX | −0.28 (0.04) | |||||||||||
| ▲ CTX | −0.34 (0.01) | |||||||||||
| Pre PYD | ||||||||||||
| Post PYD | 0.33 (0.02) | |||||||||||
| ▲ PYD | −0.29 (0.04) | |||||||||||
| Pre GLP-1 | −0.29 (0.04) |
Values are Pearson correlations (r) with (p values) below. Pre- = prior to weight loss; Post-after weight loss; ▲= change; BAP = bone alkaline phosphatase; CTX = carboxy-terminal collagen crosslinks; PYD = pyridinoline crosslinks; OC = osteocalcin; IL= interleukin; TNF-α = tumor necrosis factor- alpha; CRP = c-reactive protein; GLP-1 = glucagon like peptide-1.
Because BMD is the clinical measure of osteoporosis and used to assess risk of fracture, we focused our exploratory factor analysis on factors that contribute to hip and lumbar spine BMD pre- and post-weight loss only. The rotation factor patterns with factor scoring coefficients are shown in Table 4. Eighty-eight variables were offered into the factor analysis for separate pre- and post-weight loss Factor determinations. Collectively the pre-and post-weight loss variables were reduced to 8 Factors (Table 4). Pre- and post-weight loss Factor 1 consisted of physical activity variables while Factor 2 primarily included inflammatory variables. Bone metabolism variables appeared in Factor 3 pre- weight loss and Factor 4 post-weight loss. Factors 5–8 pre- and post-weight loss consisted primarily of combinations of endocrine variables. Each Factor was then offered in a backward stepwise multiple regression analysis to determine which Factors accounted for variance in hip and spine BMD pre- and post-weight loss. This approach allowed us to answer the questions 1) which Factors were important to hip and spine BMD during weight stable conditions (pre-weight loss) and 2) which Factors, if any, changed with weight loss? Results from the regression analysis are displayed in Table 5. No factors were significant contributors to the variance in lumbar spine BMD either pre- or post-weight loss. Factors contributing to the variance in hip BMD pre-weight loss were Factors 2 (TNF-α, IL-1β, IL-8) and 5 (cortisol, PYD, % Body Fat); accounting for 13.7% of the total variance. Post-weight loss factors included Factors 2 (TNF-α, IL-1β, IL-8, Leptin, PYD) and 3 (insulin, cortisol, PAI-1, % Body Fat) accounting for 19.6% of the total variance.
Table 4.
Rotated Factor Patterns with Scoring Coefficients for Endocrine, Inflammatory, Bone, Body Composition and Physical Activity Variables in Fifty-one Women
| Pre- Weight Loss | |||||||
|---|---|---|---|---|---|---|---|
| Factor 1 Coefficient | Factor 2 Coefficient | Factor 3 Coefficient | Factor 4 Coefficient | Factor 5 Coefficient | Factor 6 Coefficient | Factor 7 Coefficient | Factor 8 Coefficient |
| PA Time Vigorous 0.2405 | TNF-α 0.30719 | OC 0.31806 | PA Time Moderate 0.36924 | Cortisol 0.41126 | GLP-1 0.41588 | PAI-1 0.45154 | Zn 0.42053 |
| EE Vigorous PA 0.23229 | IL-1β 0.29187 | CTX 0.30615 | PA Time Light 0.30095 | PYD −0.27042 | Amylin 0.39110 | Insulin 0.33779 | HOMA 0.18495 |
| EE Light PA 0.17658 | IL8 0.28412 | BAP 0.25313 | % Body Fat −0.33979 | IL-6 0.27682 | CRP 0.3230 | Leptin 0.20301 | |
| EE Moderate PA −0.16208 | Weight 0.24594 | Vitamin D 0.17456 | Ghrelin −0.30707 | ||||
| PA Time Sedentary −0.17759 | Treatment 0.16320 | Adiponecti n −0.12052 | |||||
| Post-weight Loss | |||||||
| Factor 1 Coefficients | Factor 2 Coefficients | Factor 3 Coefficients | Factor 4 Coefficients | Factor 5 Coefficients | Factor 6 Coefficients | Factor 7 Coefficients | Factor 8 Coefficients |
| PA Time Moderate 0.26216 | TNF-α 0.27703 | Insulin 0.27489 | CTX 0.32357 | Vitamin D 0.35081 | EE Light PA 0.46317 | Ghrelin 0.35672 | GLP-1 0.41821 |
| PA Time Light 0.22930 | IL-8 0.28909 | Cortisol 0.25060 | OC 0.28665 | Zn −0.21032 | EE Moderate PA 0.45688 | CRP 0.29149 | Amylin 0.40734 |
| EE Light PA 0.16995 | IL-1β 0.26014 | PAI-1 0.25538 | BAP 0.21178 | HOMA −0.25126 | Weight −0.33347 | Adiponectin −0.3250 | |
| PA Time Vigorous 0.16456 | Leptin −0.13816 | % Body Fat −0.21899 | IL-6 0.19688 | ||||
| PA Time Sedentary −0.27666 | PYD −0.15984 | Treatment 0.11977 | |||||
PA physical activity; EE energy expenditure; TNF-α tumor necrosis factor- alpha; ILinterleukin; Zn zinc, OC osteocalcin; CTX carboxy-terminal crosslinks; BAP bone alkaline phosphatase; PYD pyridinoline crosslinks; GLP-1 glucagon like peptide-1; PAI-1 plasminogen activator inhibitor-1; CRP c-reactive protein;.
Table 5.
Regression Models for Hip Bone Mineral Density in Fifty-one Women Using Factor Variables Pre- and Post- Weight Loss.
| Pre-Weight Loss Hip BMD (n=51) | ||
|---|---|---|
| Parameter | Regression Coefficient | Probability > F |
| Intercept | 1.13586 | |
| Factor 2 | 0.02867 | 0.0684 |
| Factor 5 | 0.03128 | 0.0475 |
| Model R2 | 0.1369 | |
| Post- Weight Loss Hip BMD (n=51) | ||
|---|---|---|
| Parameter | Regression Coefficient | Probability > F |
| Intercept | 1.13274 | |
| Factor 2 | 0.02913 | 0.0611 |
| Factor 3 | 0.04243 | 0.0075 |
| Model R2 | 0.1965 | |
Factor 2: Tumor Necrosis Factor α, Interleukin (IL)-1β, IL-8.
Factor 5: Cortisol, PYD = pyridinoline cross-links, %Body Fat
Factor 2: Tumor Necrosis Factor α, Interleukin (IL) -1β, IL-8, Leptin, PYD- pyridinoline cross-links
Factor 3: Insulin, Cortisol, PIA-1 – plasminogen activation inhibitor-1, %Body Fat.
Significance was set at the p = 0.15 level of probability for inclusion in the model
5.0 DISCUSSION
We conducted a post-hoc analysis of data from a controlled feeding trial with overweight and obese women and evaluated the influence of dairy foods to attenuate weight loss induced bone loss. We also used correlational analysis and exploratory factor analysis to examine the inter-relationships among endocrine, inflammatory and bone markers, and anthropometric and other parameters on BMD and BMC. The present study demonstrated that a meal plan with adequate dairy resulted in greater BMD at the lumbar spine following weight loss compared to the LD meal plan. We also found that bone formation was greater in the AD group following weight loss compared to the LD group, while bone resorption did not change. Consistent with our results, Josse et al. [14] showed that exercise combined with a high protein (30%) and high dairy diet (6–7 servings/d) (HPHD) protected against an increase in bone resorption markers compared to weight loss with an adequate protein, low dairy diet (APLD). Thorpe et al. [13] found that a diet providing 30% protein (1.4 g/kg of weight) and 3 servings of dairy preserved bone compared to a diet with approximately 15% protein (0.8 g/kg of protein) and 2 servings of dairy. Our findings support the inclusion of dairy foods in a weight reduction program as a strategy to maintain bone health.
Bone loss during weight loss has not been consistently reported in premenopausal women [2, 9, 13, 14] as compared to studies in postmenopausal women [27–29]. Differences across studies in premenopausal women may be due to the skeletal site examined, the degree of weight loss, the intake of calcium and/or protein, and the methods used to assess bone status. The intake of calcium prior to weight loss may also be a critical factor that influences the outcome seen in different studies, but pre-intervention dairy and/or calcium intake levels generally are not reported. Because participants in our study were low calcium and low dairy consumers at recruitment (≤ 600 mg/d and ≤ 1 serving/d, respectively), changes may have been more easily detectable. The low level of calcium intake as a selection criterion was representative of the intake in the U.S. population, ~640 mg/d in women aged 18 to 50 years old [30].
There has been much debate regarding the cause of weight loss-induced bone loss. Unloading of the skeleton, as a result of weight loss, has been suggested as a cause for the observed decrease in bone mass (mechanostat theory) [31]. However, the mechostat theory cannot explain the difference in bone loss observed between our treatment groups because both LD and AD groups lost the same amount of weight. A third explanation may be interactions among bone, body composition, endocrine, and inflammatory systems. Interactions among these systems exist throughout development as bone marrow mesenchymal cells are the origin for adipocytes and osteoblasts, linking adipocyte related endocrinology with bone formation. Hematopoietic stem cells are the origin for osteoclast and immune cells thus linking inflammatory processes with bone resorption. Therefore, weight loss induced changes in body composition and endocrine or inflammatory markers and their interactions with bone physiology may represent a plausible explanation for weight loss induced bone loss. We examined the interrelationships among these systems using exploratory factor analysis to understand their contribution to bone before and after weight loss.
Cornish and colleagues [19] demonstrated a leptin dose-response in osteoblast-like cell number and detected measurable levels in mRNA for leptin receptor in the cells. Research conducted by Bartell et al. [32] further demonstrated the role of leptin in bone formation using leptin deficient ob/ob mice. Additionally, Reimer, LaMothe and Zernike [33] demonstrated in leptin receptor deficient obese rats that tibia, but not vertebrae, were significantly shorter and achieved greater load, displacement and stress at the proportional limit compared to lean rats; suggesting leptin may affect axial and appendicular bone differently. Adiponectin also has been shown to have in vitro and in vivo effects on bone. Williams et al. [34] investigated the effect of adiponectin on primary cultures of osteoblastic and osteoclastic cells (rat and human cells) and in adiponectin deficient mice. A 50% increase was observed in osteoblastogenesis at 10 μg/ml and reduced osteoclastogenesis at a concentration of 1μg/ml and greater. In adiponectin knockout mice (AdKO) a 30% increase in trabecular volume and trabecular number was observed. Williams et al. concluded that adiponectin stimulated osteoblast growth, inhibited osteoclastogenesis and may act as an indirect effect through action of insulin or growth factor. Insulin receptors, expressed on osteoblasts, also play a role in bone metabolism and respond to exogenous insulin by increasing anabolic markers of bone [36]. Basu and colleagues [37] investigated the effects of insulin on osteocalcin and bone metabolism in 14 research volunteers using a 7 hr. euglycemic clamp procedure with matched levels of growth hormone and glucagon. Samples were collected at low, intermediate and high dose insulin infusions. Serum P1NP, a marker of bone formation, was significantly lower at the end of the intermediate dose of insulin, but not different from the low and high insulin dose. They did not observe changes in circulating osteocalcin across any of the insulin concentrations nor did CTX or OPG differ at the intermediate or high insulin dose compared to the low dose. Although acute changes in serum insulin levels did not affect bone metabolism, insulin sensitivity, assessed as glucose infusion rate and glucose rate of disappearance (Rd) were positively correlated with CTX. This suggests that increased insulin sensitivity is associated with increased bone resorption. Costa and co-workers [38] demonstrated an effect of ghrelin on human osteoblasts; cell proliferation increased 2-fold. However, ghrelin had no effect on osteoblast differentiation and apoptosis. They further examined the effects of ghrelin on osteoclast differentiation and activity in mature rat osteoclasts and observed a 30% increase in the number of excavated osteoclast. These studies provide clear evidence of the interrelationship among endocrine hormones, osteoblasts, osteoclasts and bone metabolism.
Results from human studies are confounded by the age, sex, weight, and type of methodology for BMD assessment and, therefore, inconsistent results have been reported. The InCHIANTI study [18] examined the relationship of adiponectin to total, trabecular and cortical BMD (quantitative CT of tibia) in a large group of men and women (320M, 271F; 29 – 97 yr). For women, there was a negative association between adiponectin and anthropometric variables, total BMD, and trabecular and cortical BMD. This is similar to our negative association between adiponectin and osteocalcin. Iida et al. [39] evaluated the relationships among circulating levels of leptin and adiponectin with lumbar spine BMD and femoral and distal forearm BMD in 111 Japanese women 40 – 80 yrs. There was no correlation between leptin and BMD (contrary to our findings), but adiponectin was significantly and negatively related to lumbar spine and femoral BMD in premenopausal women. They concluded that the influence of adiponectin on BMD may be different at different skeletal sights. Sherk and colleagues [40] had similar findings when comparing leptin to BMD in pre- and postmenopausal women and also concluded that the relationship between leptin and BMD may be age dependent. Jürimäe and co-workers [41] also investigated the role of leptin, adiponectin and ghrelin on BMD in healthy postmenopausal women and found that the correlative associations between circulating levels of these hormones and BMD were mediated by body composition parameters. In our study we observed a significant inverse relationship between adiponectin and the change on osteocalcin. We did not observe any correlation between adiponectin and BMD or BMC at either lumbar spine or hip sites.
Because overweight and obesity may contribute to increased inflammation, we also examined the associations among inflammatory markers and bone metabolism during weight loss. We found that pre- and post-weight loss IL-1β and TNF-α were negatively associated with post-weight loss BAP and post-weight loss TNF-α was also inversely related to osteocalcin. These results support the hypothesis that both prior to and following weight loss, inflammatory processes in overweight and obese women may be detrimental to bone metabolism by suppressing bone formation activity not elevating one resorption; as may be commonly believed. This is consistent with previous studies [23].
Although other studies exist that have examined the relationships among adipokines, inflammatory markers, BMD, BMC and bone turnover, they tend to be observational studies with older adults, individuals with diabetes or other health related issues. Our study was unique in that we examined inter-relationships among biomarkers of endocrine, immune and bone systems, along with anthropometric and other parameters on BMD and BMC pre- and post-weight loss using an exploratory factor analysis. Regression models were constructed to assess the contribution of endocrine and inflammatory markers, anthropometric and other parameters to total variance in bone metabolism in vivo before and after weight loss. We demonstrated that for pre- and post- weight loss in overweight and obese women ~14% and 20%, respectively of the variance in hip BMD was accounted for a combination of inflammatory and bone metabolism markers plus body composition. Future animal models and human clinical trials should attempt to further elucidate the contribution of endocrine, inflammatory and phenotypic factors, e.g. body composition, physical activity, etc. to changes in bone metabolism.
Our study had several limitations. First, it was designed as a weight loss study, therefore, the power calculation was done to detect a change in weight and body fat, not bone. However, the controlled feeding aspect of the study did allow for the detection of significant changes with this cohort. Additionally, a longer study (6 months or more), with more time points would have been beneficial. It is possible that after 3 months of weight loss, the bone turnover cycle was not complete, and our observations must be taken with caution. We also note that the greater BMD detected in the lumbar spine of those in the AD group may not be physiologically important, but may be artifacts due to the technical limitations of DXA scans. Indeed, Van Loan et al. [42] reported that during weight loss, bone edge detection is modified due to the decrease in fat mass around the bone. However, we do not believe this to be the case because both groups lost an equal amount of weight and fat during the intervention. Furthermore, the observed increase in lumbar spine BMD in the AD group is supported by greater serum OC concentration.
CONCLUSION
We have shown that a diet with 3–4 servings/d of dairy foods and adequate calcium intake resulted in greater lumbar spine BMD and increased bone formation during a controlled energy restricted weight loss period; supporting the positive effect of including dairy in a weight loss diet. Additionally, our use of exploratory factor analysis to examine interactions among endocrine, immune and bone systems with anthropometric and other parameters serves as hypothesis generating results. Although cellular studies and animal models clearly demonstrate the interaction among bone, endocrine and immune systems, in vivo human studies provide no consistent results. Clearly further research is needed to examine the interaction among these systems under defined conditions with pre-planned selection criteria for age, sex, race, BMI, etc. that will help elucidate the role of the skeleton in human physiological systems.
Highlights.
Adequate dairy intake increased lumbar spine BMD following weight loss.
Energy related hormones were positively related to hip and lumbar spine BMD.
Inflammatory markers were inversely related to markers of bone metabolism.
We modeled the contribution of endocrine and inflammatory markers to BMD.
Acknowledgments
This study would not have been possible without the efforts of a team of individuals starting with the research volunteers, the WHNRC Metabolic Food Lab, human studies support, and physiology and analytical laboratory staff members and the support of Ms. Janet Peerson, statistician. Additional support was provided by the UC Davis Clinical and Translational Science Center (CTSC) nursing staff for blood draws and radiology technicians for the intra-abdominal adipose tissue CT scan and analysis. Major funding for the project was provided by the National Dairy Council and administered by the Dairy Research Foundation. Funds were also provided by the Dairy Council of California and the United States Department of Agriculture (USDA), Agriculture Research Service (ARS) intramural project 5306-51520-007-00D, and the Clinical and Translational Science Center of the University of California, Davis, grant number UL1 RR024146 from the National Center for Medical Research. The contents of this manuscript are the sole responsibility of the authors and do not represent the official view of National Center for Research Resources (NCRR), National Institute of Health (NIH), or USDA. The United States Department of Agriculture is an equal opportunity provider and employer.
Authors Adams, Keim and Van Loan have received grant funding from the National Dairy Council administered by the Dairy Research Institute and the Dairy Council of California. No other income, fees for consulting, expert testimony, employment, ownership interest from an organization that may gain or lose financially from the work being presented.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authorship Contribution
MAL ECS, LRW, SHA, NLK and MVL contributed to conception and design, acquisition of data, data analysis and interpretation, and manuscript preparation.
ERG, BCP, GUS, MW contributed to acquisition, analysis and interpretation of data, participated in manuscript preparation and critical revisions.
Conflict of Interest Disclosure
All authors state they have no additional conflicts of interest to disclose.
References
- 1.NIH Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68:899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 2.Shapses SA, Von Thun NL, Heymsfield SB, Ricci TA, Ospina M, Pierson RN, Jr, Stahl T. Bone turnover and density in obese premenopausal women during moderate weight loss and calcium supplementation. J Bone Miner Res. 2011;16:1329–1336. doi: 10.1359/jbmr.2001.16.7.1329. [DOI] [PubMed] [Google Scholar]
- 3.Bowen J, Noakes M, Clifto PM. A high dairy protein, high calcium diet minimizes bone turnover in overweight adults during weight loss. J Nutr. 2004;134:568–573. doi: 10.1093/jn/134.3.568. [DOI] [PubMed] [Google Scholar]
- 4.Rector RS, Loethen J, Ruebel M, Thomas TR, Hinton PS. Serum markers of bone turnover are increased by modest weight loss with or without weight bearing exercise in overweight premenopausal women. Appl Physiol Nutr Metab. 2009;34:933–941. doi: 10.1139/H09-098. [DOI] [PubMed] [Google Scholar]
- 5.Jensen LB, Kollerup G, Quaade F, Sørensen OH. Bone mineral changes in obese women during a moderate weight loss with and without calcium supplementation. J Bone Miner Res. 2001;16:141–147. doi: 10.1359/jbmr.2001.16.1.141. [DOI] [PubMed] [Google Scholar]
- 6.Ricci TA, Chowdhury HA, Heymsfield SB, Stahl T, Pierson RN, Jr, Shapses SA. Calcium supplementation suppresses bone turnover during weight reduction in postmenopausal women. J Bone Miner Res. 1998;13:1045–1050. doi: 10.1359/jbmr.1998.13.6.1045. [DOI] [PubMed] [Google Scholar]
- 7.Riedt CS, Cifuentes M, Stahl T, Chowdhury HA, Schlussel Y, Shapses SA. Overweight postmenopausal women lose bone with moderate weight reduction and 1g/day calcium intake. J Bone Miner Res. 2005;20:455–463. doi: 10.1359/JBMR.041132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramsdale SJ, Bassey EJ. Changes in bone mineral density associated with dietary induced loss of body mass in young women. Clin Sci (Lond) 1994;87:343–348. doi: 10.1042/cs0870343. [DOI] [PubMed] [Google Scholar]
- 9.Salamone LM, Cauley JA, Black DM, SimkinSilverman L, Lang W, Gregg E, Palermo L, Epstein RS, Kuller LH, Wing R. Effect of a lifestyle intervention on bone mineral density in premenopausal women: a randomized trial. Am J Clin Nutr. 1999;70:97–103. doi: 10.1093/ajcn/70.1.97. [DOI] [PubMed] [Google Scholar]
- 10.Fogelholm GM, Sievänen HT, KukkonenHarjula TK, Pasanen ME. Bone mineral density during reduction, maintenance and regain of body weight in premenopausal, obese women. Osteoporos Int. 2001;12:199–206. doi: 10.1007/s001980170130. [DOI] [PubMed] [Google Scholar]
- 11.Pritchard JE, Nowson CA, Wark JD. Bone loss accompanying diet induced or exercise -induced weight loss: a randomised controlled study. Int J Obes Relat Metab Disord. 1996;20:513–520. [PubMed] [Google Scholar]
- 12.Riedt CS, Schlussel Y, von Thun N, AmbiaSobhan H, Stahl T, Field MP, Sherrell RM, Shapses SA. Premenopausal overweight women do not lose bone during moderate weight loss with adequate or higher calcium intake. Am J Clin Nutr. 2007;85:972–980. doi: 10.1093/ajcn/85.4.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thorpe MP, Jacobson EH, Layman DK, He X, Kris-Etherton PM, Evans EM. A diet high in protein, dairy, and calcium attenuates bone loss over twelve months of weight loss and maintenance relative to a conventional high carbohydrate diet in adults. J Nutr. 2008;138:1096–1100. doi: 10.1093/jn/138.6.1096. [DOI] [PubMed] [Google Scholar]
- 14.Josse AR, Atkinson SA, Tarnpolsky MA, Phillips SM. Diets higher in dairy foods and dietary protein support bone health during diet and exercise induced weight loss in overweight and obese premenopausal women. J Clin Endocrin Metab. 2012;97:251–260. doi: 10.1210/jc.2011-2165. [DOI] [PubMed] [Google Scholar]
- 15.Karsentry G, Ferron M. The contribution of bone to whole-organism physiology. Nature. 2012;481:314–320. doi: 10.1038/nature10763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cornish J, Costa JL, Naot D. The bone-fat relationship: Laboratory studies. IBMS BoneKey. 2009 Sep 6;:311–322. doi:19.1138/20090395. [Google Scholar]
- 17.Gimble JM. Leptin’s balancing act between bone and fat. J Bone & Miner Res. 2011;26:1694–1697. doi: 10.1002/jbmr.445. [DOI] [PubMed] [Google Scholar]
- 18.Napoli N, Pedone C, Pozzilli P, Lauretani F, Ferucci L, Incalzi RA. Adiponetic and bone mass density: The InCHIANTI study. Bone. 2010;47:1001–1005. doi: 10.1016/j.bone.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cornish J, Callon KE, Baya U, Lin C, Naot D, Hill BL, Grey AB, Broom N, Myers DE, Nicholson GC, Reid IR. Leptin directly regulates bone cell function in vitro and reduces bone fragility in vivo. J Endocrinol. 2002;175:405–415. doi: 10.1677/joe.0.1750405. [DOI] [PubMed] [Google Scholar]
- 20.Holloway WR, Collier FM, Aitken CJ, Myers DE, Hodge JM, Malakellis M, Gough TJ, Collier GR, Nicholson GC. Leptin inhibits osteoclast generation. J Bone Miner Res. 2002;17:200–209. doi: 10.1359/jbmr.2002.17.2.200. [DOI] [PubMed] [Google Scholar]
- 21.Berner HS, Lyngstadaas SP, Spahr A, Monjo M, Thommesen L, Drevon CA, Syversen U, Reseland JE. Adiponectin and its receptors are expressed I\n bone-forming cells. Bone. 2004;35:842–849. doi: 10.1016/j.bone.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 22.Oshima K, Nampei A, Matsuda M, Iwaki M, Fukuhara A, Hashimoto J, Yoshikawa H, Shimomura I. Adiponectin increases bone mass by suppressing osteoclast and activating osteoblast. Biochem Biophys Res Commun. 2005;331:520–526. doi: 10.1016/j.bbrc.2005.03.210. [DOI] [PubMed] [Google Scholar]
- 23.Baker-LePain JC, Nakamura MC, Lane NE. Effects of inflammation on bone: an update. Curr Opin Rheumat. 2011;23:389–395. doi: 10.1097/BOR.0b013e3283474dbe. [DOI] [PubMed] [Google Scholar]
- 24.Van Loan MD, Keim NL, Adams SH, Souza E, Woodhouse L, Bremmer A, Spurlock M, Burnett D, Gertz ER, Piccolo B, Witbracht M, Thomas A. Does the inclusion of dairy foods in a moderate energy restricted diet enhance central fat, weight, and intra-abdominal adipose tissue losses in overweight and obese adults? A controlled feeding study. J Obes. 2011 doi: 10.1155/2011/989657. ID 989657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes: Recommended Intakes for Individuals. USDA National Agriculture Library; 2002. [Google Scholar]
- 26.Glover SJ, Garnero P, Naylor K, Rogers A, Eastell R. Establishing a reference range for bone turnover markers in young, healthy women. Bone. 2008;42:623–630. doi: 10.1016/j.bone.2007.12.218. [DOI] [PubMed] [Google Scholar]
- 27.Villareal DT, Shah K, Banks MR, Sinacore DR, Klein S S. Effect of weight loss and exercise therapy on bone metabolism and mass in obese older adults: a one year randomized controlled trial. J Clin Endocrinol Metab. 2008;93:2181–2187. doi: 10.1210/jc.2007-1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cifuentes M, Riedt CS, Brolin RE, Field MP, Sherrell RM, Shapses SA. Weight loss and calcium intake influence calcium absorption in overweight postmenopausal women. Am J Clin Nutr. 2004;80:123–130. doi: 10.1093/ajcn/80.1.123. 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ricci TA, Heymsfield SB, Pierson RN, Jr, Stahl T, Chowdhury HA, Shapses SA. Moderate energy restriction increases bone resorption in obese postmenopausal women. Am J Clin Nutr. 2001;73:347–352. doi: 10.1093/ajcn/73.2.347. [DOI] [PubMed] [Google Scholar]
- 30.US Department of Agriculture 1994–1996 Continuing Survey of Food Intakes by Individuals and 1994–1996 Diet and Health Knowledge Survey. National Technical Information Service; Springfield, VA: 1998. [Google Scholar]
- 31.Frost H. Bone “mass” and the “mechanostat”: a proposal. Anat Rec. 1987;219:19. doi: 10.1002/ar.1092190104. [DOI] [PubMed] [Google Scholar]
- 32.Bartell SM, Rayalam S, Ambati S, Gaddam DR, Hartzell DL, Hamrick M, She J-X, Della-Fera MA, Baile CA. Central (ICV) leptin injection increase bone formation, bone mineral density, muscle mass, serum IGF-1, and the expression of osteogenic genes in leptin-deficient ob/ob mice. J Bone Miner Res. 2011;26:1710–1720. doi: 10.1002/jbmr.406. [DOI] [PubMed] [Google Scholar]
- 33.Reimer RA, LaMothe JM, Zernicke RE. Leptin deficiency and its effects in tibial and vertebral bone mechanical properties in mature genetically lean and obese JCR:LA-corpulent rats. J Obesity. 2012 doi: 10.1155/2012/650193. Article ID: 650193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams GA, Wang Y, Callon KE, Watson M, Lin J-M, Lam JBB, Costa JL, Orpe A, Broom N, Naot D, Reid IR, Cornish J. In Vitro and in vivo effects of adiponectin on bone. Endocrinol. 2009;150:3603–3610. doi: 10.1210/en.2008-1639. [DOI] [PubMed] [Google Scholar]
- 35.Irwin R, Lin HV, Motyl KJ, McCabe LR. Normal bone density obtained in the absence of insulin receptor expression in bone. Endocrinol. 2006;147:5760–5767. doi: 10.1210/en.2006-0700. [DOI] [PubMed] [Google Scholar]
- 36.Fulzele K, Riddle RC, DiGirolamo DJ, Cao X, Wan C, Chen D, Faugere MC, Aja S, Hussain MA, Brüning JC, Clemens TL. Insulin receptor signaling in osteoblasts regulates postnatal bone acquisition and body composition. Cell. 2010;142:309–319. doi: 10.1016/j.cell.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basu R, Petersn J, Rizza R, Khosla S. Effects of physiological variations in circulating insulin levels on bone turnover in humans. J Clin Endocrinol. 2001 doi: 10.2010/jc.2010-2877. [Epub 16 Feb] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Costa JL, Naot D, Lin J-M, Watson M, Callon KE, Reid IR, Grey AB, Cornish J. Ghrelin is an osteoblast mitogen and increases osteoclastic bone resorption in vitro. Internat J Peptides. 2011 doi: 10.1155/2011/605193. Article ID 605193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iida T, Domoto T, Takigawa A, Nakamura S, Kato Y, Togo M, Chikamura C, Harada T, Ishizaki F, Ono Y. Relationship among blood leptin and adiponectin levels, fat mass, and bone mineral density in Japanese pre- and postmenopausal women. Hiroshima J Med Sci. 2011;60:71–78. [PubMed] [Google Scholar]
- 40.Sherk VD, Malone SP, Bemben MG, Knehans AW, Palmer IJ, Bemben DA. Leptin, fat mass, and bone mineral density in healthy pre- and postmenopausal women. J Clin Densit. 2001;14:321–325. doi: 10.1016/j.jocd.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 41.Jürimäe J, Jürimäe T, Leppil A, Kum T. The influence of ghrelin, adiponectin, and leptin on bone mineral density in healthy postmenopausal women. J Bone Miner Metab. 2008;26:618–623. doi: 10.1007/s000774-0861-5. [DOI] [PubMed] [Google Scholar]
- 42.Van Loan MD, Johnson HL, Barbieri TF. Effect of weight loss on bone mineral content and bone mineral density in obese women. Am J Clin Nutr. 1998;67:734738. doi: 10.1093/ajcn/67.4.734. [DOI] [PubMed] [Google Scholar]


