Abstract
Objective
To present the 12-month prevalence of DSM-IV major depressive disorder (MDD) and severe MDD, examine sociodemographic correlates and comorbidity, and describe impairment and service utilization.
Method
Data are from the National Comorbidity Survey-Adolescent Supplement (NCS-A), a nationally representative survey of 10,123 adolescents aged 13 to 18 years that assesses DSM-IV disorders using the Composite International Diagnostic Interview (CIDI) Version 3.0. One parent or surrogate of each participating adolescent was also asked to complete a self-administered questionnaire.
Results
Lifetime and 12-month prevalence of MDD were 11.0% and 7.5%, respectively. The corresponding rates of severe MDD were 3.0% and 2.3%. The prevalence of MDD increased significantly across adolescence, with markedly greater increases among females than males. Most cases of MDD were associated with psychiatric comorbidity and severe role impairment, and a substantial minority reported suicidality. The prevalence of severe MDD was about a quarter of that of all MDD cases; estimates of impairment and clinical correlates were of 2- to 5-fold greater magnitude for severe versus mild/moderate depression, with markedly higher rates for suicidal thoughts and behaviors. Treatment in any form was received by the majority of adolescents with 12-month DSM-IV MDD (60.4%), but only a minority received treatment that was disorder-specific or from the mental health sector.
Conclusion
Findings underscore the important public health significance of depression among US adolescents and the urgent need to improve screening and treatment access in this population.
Keywords: adolescence, depression, epidemiology, service utilization
INTRODUCTION
Mental disorders are the leading cause of years lived with disability (YLD) worldwide, but 40.5% of this burden is uniquely attributable to major depression1. Recent estimates of the prevalence of major depression indicate that 16.6% of adults have been depressed at some point in their lifetime2. Over half of individuals who recover from a first episode of depression will have at least one additional episode in their lifetime, approximately 80% of those with a history of two episodes will experience a recurrence3, and nearly 20% of individuals with depression have episodes that last more than 24 months4. In adolescence, rates of depression increase substantially between 13 and 18 years of age, and the estimated cumulative incidence in this population approximates the adult lifetime prevalence rate2,5,6. However, despite its early onset and protracted course, only 1% of US youth are treated in an outpatient setting for depression each year7. These findings highlight adolescence as a critical developmental period for identifying high-risk individuals and preventing the incidence of this disorder.
Efforts to minimize the individual and public health burden of major depression are contingent on obtaining accurate information concerning the scope, correlates, and clinical characteristics of this condition in the general population. Ultimately, this information can be used to frame future research efforts and to set an agenda for the allocation of screening, treatment, or prevention resources. In general, such information has been lacking from nationally representative samples of adolescents. Although two recent reports provided estimates of the 12-month prevalence of major depressive disorder (MDD) among 8- to 15-year-olds (2.7%8) and among 12- to 17-year-olds (8.2%9), neither of the studies included assessment of the full range of current DSM-IV mental disorders in a comprehensive depiction of depression.
The National Comorbidity Survey-Adolescent Supplement (NCS-A) provides the opportunity to examine the full range of issues in a large, nationally representative sample of 13- to 18-year-olds, representing the critical developmental period for the onset of depression. Further, recent analyses of depression in adolescents have found that many individuals meeting DSM-IV criteria for depression have a severe, or highly impairing, form of this disorder10, but few studies have examined whether correlates vary for the severe and non-severe manifestations. This report will: (1) present the 12-month prevalence estimates of DSM-IV MDD, mild/moderate MDD, and a severe form of MDD; (2) examine sociodemographic correlates and comorbidity associated with 12-month disorders; and (3) describe impairment and service utilization rates over the past 12 months.
METHOD
Sample and Procedure
The NCS-A is a nationally representative face-to-face survey of 10,123 adolescents aged 13 to 18 in the continental United States11. The survey was administered by professional interview staff of the Institute for Social Research at the University of Michigan and conducted in a dual-frame sample that included a household subsample and a school subsample12,13. The combined NCS-A adolescent response rate was 82.9%. One biological parent or parent surrogate of each participating adolescent was mailed a self-administered questionnaire (SAQ) to collect information on adolescent mental and physical health, family, and related factors. The full SAQ was completed by 6,491 parents, and an abbreviated SAQ was completed by 1,994 parents (83.3% conditional response rate). Cases were weighted for variation in within-household probability of selection (household sub-sample) and for residual discrepancies between the sample and the US population on the basis of sociodemographic and geographic variables12,13. Recruitment and consent procedures were approved by the human subjects committees of both Harvard Medical School and the University of Michigan.
Measures
Sociodemographic Variables
Similar to previous investigations, well-established sociodemographic correlates of mental disorders and markers of environmental adversity were assessed in the NCS-A11. Age, sex, race/ethnicity, parent education, region, and urbanicity were reported by adolescents, and marital status of parents and family income were reported by parents. A poverty index ratio was calculated based on family size and the ratio of family income to the family’s poverty threshold level (≤1.5 poor, ≤3, ≤6, and >6).
Diagnostic Assessment
Adolescents were administered a modified version of the World Health Organization’s (WHO) Composite International Diagnostic Interview Version 3.0 (CIDI) for DSM-IV14. This instrument assesses lifetime and 12-month MDD and dysthymia, as well as a range of anxiety disorders (panic disorder, agoraphobia, social phobia, specific phobia, generalized anxiety disorder [GAD], posttraumatic stress disorder [PTSD], and separation anxiety disorder [SAD]); attention-deficit/hyperactivity disorder [ADHD]; behavior disorders (oppositional defiant disorder [ODD] and conduct disorder [CD]); and substance use disorders (alcohol abuse/dependence and drug abuse/dependence). Parents who completed the full SAQ provided information about MDD and dysthymic disorder, SAD, ADHD, ODD, and CD, whereas those completing the abbreviated SAQ reported only on ADHD. Because prior research has indicated that adolescents are the most accurate informants of their emotional symptoms15–18, only adolescent reports from the CIDI were used to assess diagnostic criteria for MDD, dysthymia, anxiety disorders, and substance use disorders, whereas only parent reports were used for diagnoses of ADHD. Information from both the parent and adolescent were combined for behavior disorders and classified as positive if either informant endorsed symptoms for diagnostic criteria15,19. For those disorders for which parent reports were used, estimation of DSM-IV disorders were based on the full SAQ.
DSM-IV Diagnosis
Definitions of all psychiatric disorders adhered to DSM-IV criteria. Diagnostic hierarchy rules were applied to all but substance use disorders. Distress and impairment criteria were embedded within each diagnostic section of the CIDI. All DSM-IV diagnoses in this report required endorsement of “moderate,” “severe,” or “very severe” levels of distress or “some,” “a lot,” or “extreme” levels of impairment.
Severe MDD
In order to minimize heterogeneity and examine correlates and treatment of more clinically significant manifestations of depression, we developed a definition of severe MDD that is based on high levels of distress and impairment. This was operationalized in the CIDI as “severe” or “very severe” distress in response to the question, “How strong were your bad feelings during those times?”, and as “a lot” or “extremely” impaired in response to one of the following questions: “How often, during those times, did you feel so bad that you could not carry out your daily activities?” or “How much did your sadness/discouragement/boredom interfere or cause problems with your school work, your job, or your relationships with family and friends?”.
Clinical features
Role impairment
Adolescents with DSM-IV 12-month MDD were administered the Sheehan Disability Scale (SDS) to assess the degree to which depression interfered with functioning in the worst month of the past year in the areas of household chores, school/work, family relationships, and social roles. The response scale ranged from 0 (no problem) to 10 (very severe). Responses were categorized into mild/moderate (0–6) and severe /very severe (7–10) impairment for each SDS domain. Overall role impairment was defined as the highest severity category that was endorsed across the four SDS domains. Respondents were also asked to estimate the number of days in the past year that they were totally unable to function because of depression (days “out-of-role”).
12-month Suicidality
In a separate section of the CIDI, adolescents were asked whether they had “…seriously thought about killing [themselves],” “made a plan for killing [themselves],” and “tried to kill themselves” in the past 12 months.
12-month Treatment
Adolescents and parents who reported adolescent MDD in the past 12 months were asked whether the adolescent received treatment for their depression (i.e., disorder-specific treatment). In the Service section of the CIDI, adolescents reported on whether they received service for emotional or behavioral problems, in what kinds of settings, and at what age they first received services for their problems. Parents responded to similar questions in the SAQ. Service use was classified as “Mental Health Specialty” if either the adolescent or parent reported using services rendered by a psychiatrist, psychologist, social worker, or family counselor in inpatient or outpatient settings (i.e., mental health clinic, drug or alcohol clinic, and admissions to hospitals and other facilities). Service use was classified as “Any Treatment” if either the adolescent or parent endorsed treatment in a mental health specialty, general medical, human services, complementary alternative medicine (CAM), juvenile justice, or school setting.
Statistical Analysis
All statistical analyses were completed using SUDAAN software (version 10) and utilized the Taylor series linearization method to take into account the complex survey design. In order to promote consistency with previous investigations of the NCS-A10, cross-tabulations were used to calculate estimates of prevalence, comorbidity, role impairment, and treatment. Age-of-onset curves were generated using the Kaplan-Meier method. Multivariate logistic regression analysis was used to examine socio-demographic correlates of prevalence and treatment. Odds Ratios were the exponentiated values of logistic regression coefficients, and 95% confidence intervals of odds ratios were calculated using design-adjusted variances.
RESULTS
Lifetime and 12-month Prevalence
The lifetime and 12-month prevalence rates of DSM-IV MDD (with or without dysthymia) among US adolescents were 11.0% and 7.5%, respectively. The corresponding rates of severe MDD were 3.0% and 2.3%; the rates of mild/moderate MDD were 8.0% and 5.2%. Dysthymia affected far fewer adolescents, with lifetime and 12-month prevalence rates of 1.8% and 1.3%, respectively, and 0.9% and 0.7% for severe cases. While most cases of DSM-IV MDD assessed over the lifetime (87.5%) or over the past 12 months (86.4%) occurred without dysthymia, dysthymia almost always occurred with MDD (87.6% of all lifetime, and 90.6% of all 12-month cases).
The sociodemographic correlates of 12-month MDD are presented in Table 1. Female adolescents experienced a 2- to 3-fold risk of MDD compared to males, and a nearly 4-fold risk of severe MDD. The prevalence of MDD was strongly associated with age, generally increasing across adolescence, with rates of DSM-IV MDD being about twice as high in older compared to younger adolescents. Prevalence rates of severe MDD were 4 times higher in older compared to younger adolescents. There were no significant differences by age in rates of mild/moderate MDD, and the prevalence of MDD did not differ by other sociodemographic variables. Similar patterns were found for lifetime MDD (see tables S1 and S2, available online), and lifetime estimates of first episode of MDD yielded, a significant interaction (Wald F(1) =48.15, p<.0001) between sex and age (Figure 1).
Table 1.
Twelve-Month Prevalence Estimates and Demographic Correlates of DSM-IV, Severe, and Mild/Moderate Major Depressive Disorder (MDD; N=10,123)
| Correlates | n | DSM-IV MDD (Total) | Severe MDD | Mild/Moderate MDD | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | aOR | 95% CI | % | aOR | 95% CI | % | aOR | 95% CI | ||
| Sex | ||||||||||
| Female | 5,170 | 10.7 | 2.48 | 1.93 – 3.18 | 3.6 | 3.59 | 2.14 – 6.00 | 7.1 | 2.05 | 1.53 – 2.74 |
| Male | 4,953 | 4.6 | 1.00 | 1.0 | 1.00 | 3.5 | 1.00 | |||
| Wald χ21 | 53.7 | 25.0 | 24.9 | |||||||
| p | 0.000 | 0.000 | 0.000 | |||||||
| Age, y | ||||||||||
| 13 | 1,652 | 4.5 | 1.00 | 0.5 | 1.00 | 4.0 | 1.00 | |||
| 14 | 2,218 | 5.5 | 1.24 | 0.74 – 2.09 | 1.0 | 1.93 | 0.75 – 4.98 | 4.6 | 1.15 | 0.61 – 2.15 |
| 15 | 1,887 | 8.6 | 1.92 | 1.26 – 2.94 | 2.0 | 3.92 | 1.41 – 10.90 | 6.5 | 1.62 | 1.04 – 2.54 |
| 16 | 2,010 | 8.7 | 2.01 | 1.38 – 2.92 | 3.9 | 8.04 | 3.26 – 19.81 | 4.7 | 1.18 | 0.77 – 1.81 |
| 17 | 1,758 | 10.0 | 2.36 | 1.47 – 3.79 | 3.3 | 6.77 | 2.56 – 17.92 | 6.7 | 1.71 | 1.02 – 2.87 |
| 18 | 598 | 8.1 | 1.87 | 1.09 – 3.23 | 4.0 | 8.29 | 3.04 – 22.59 | 4.1 | 1.03 | 0.51 – 2.08 |
| Wald χ25 | 21.6 | 50.5 | 8.8 | |||||||
| p | 0.001 | 0.000 | 0.118 | |||||||
| Race/Ethnicity | ||||||||||
| Hispanics | 1,914 | 8.9 | 1.35 | 0.97 – 1.90 | 2.5 | 1.28 | 0.85 – 1.94 | 6.4 | 1.36 | 0.85 – 2.17 |
| Non-Hispanic Black | 1,953 | 8.0 | 1.16 | 0.95 – 1.41 | 2.6 | 1.27 | 0.74 – 2.19 | 5.5 | 1.10 | 0.80 – 1.53 |
| Other | 622 | 8.3 | 1.26 | 0.82 – 1.94 | 3.3 | 1.71 | 1.07 – 2.75 | 5.0 | 1.06 | 0.54 – 2.05 |
| Non-Hispanic White | 5,634 | 7.1 | 1.00 | 2.1 | 1.00 | 5.0 | 1.00 | |||
| Wald χ23 | 4.4 | 5.5 | 1.8 | |||||||
| p | 0.219 | 0.141 | 0.621 | |||||||
| Poverty Index Ratio | ||||||||||
| ≤1.5 Poor | 1,717 | 8.2 | 1.04 | 0.76 – 1.44 | 2.4 | 1.07 | 0.55 – 2.06 | 5.8 | 1.03 | 0.78 – 1.38 |
| ≤3.0 | 2,023 | 6.5 | 0.82 | 0.58 – 1.17 | 2.1 | 0.93 | 0.60 – 1.43 | 4.3 | 0.79 | 0.49 – 1.26 |
| ≤6.0 | 3,101 | 7.7 | 0.99 | 0.76 – 1.30 | 2.2 | 0.96 | 0.51 – 1.81 | 5.5 | 1.01 | 0.75 – 1.35 |
| > 6.0 | 3,282 | 7.7 | 1.00 | 2.4 | 1.00 | 5.3 | 1.00 | |||
| Wald χ23 | 2.2 | 0.5 | 1.6 | |||||||
| p | 0.529 | 0.925 | 0.648 | |||||||
| Parents’ Education | ||||||||||
| Less than High School | 1,684 | 6.9 | 0.89 | 0.65 – 1.22 | 1.9 | 0.88 | 0.45 – 1.70 | 4.9 | 0.91 | 0.62 – 1.32 |
| High School Grad | 3,081 | 7.5 | 1.00 | 0.74 – 1.34 | 2.4 | 1.09 | 0.66 – 1.80 | 5.1 | 0.96 | 0.69 – 1.33 |
| Some College | 1,998 | 8.6 | 1.20 | 0.85 – 1.71 | 2.7 | 1.29 | 0.76 – 2.19 | 5.9 | 1.15 | 0.73 – 1.81 |
| College Grad | 3,360 | 7.3 | 1.00 | 2.2 | 1.00 | 5.1 | 1.00 | |||
| Wald χ23 | 4.4 | 1.7 | 1.2 | |||||||
| p | 0.225 | 0.627 | 0.747 | |||||||
| Region | ||||||||||
| Northeast | 1,868 | 9.0 | 1.25 | 0.82 – 1.92 | 1.9 | 0.60 | 0.34 – 1.07 | 7.1 | 1.74 | 1.13 – 2.68 |
| Midwest | 2,776 | 7.4 | 1.09 | 0.77 – 1.53 | 2.0 | 0.65 | 0.41 – 1.05 | 5.4 | 1.43 | 1.00 – 2.03 |
| South | 3,434 | 6.8 | 0.91 | 0.64 – 1.30 | 2.0 | 0.62 | 0.38 – 1.01 | 4.7 | 1.15 | 0.75 – 1.76 |
| West | 2,045 | 7.8 | 1.00 | 3.3 | 1.00 | 4.4 | 1.00 | |||
| Wald χ23 | 3.3 | 6.5 | 8.7 | |||||||
| p | 0.343 | 0.088 | 0.034 | |||||||
| Urbanicity | ||||||||||
| Metropolitan | 4,508 | 8.2 | 1.05 | 0.65 – 1.71 | 2.7 | 0.91 | 0.57 – 1.46 | 5.4 | 0.90 | 0.54 – 1.50 |
| Other urban | 3,304 | 6.9 | 0.94 | 0.58 – 1.52 | 2.0 | 0.92 | 0.56 – 1.50 | 4.9 | 0.85 | 0.48 – 1.50 |
| Rural | 2,311 | 7.2 | 1.00 | 1.6 | 1.00 | 5.6 | 1.00 | |||
| Wald χ22 | 1.1 | 2.9 | 0.4 | |||||||
| p | 0.587 | 0.240 | 0.834 | |||||||
| Parents’ Marital Status | ||||||||||
| Married/cohabiting | 4,602 | 7.2 | 1.00 | 2.2 | 1.00 | 5.0 | 1.00 | |||
| Previously married | 1,009 | 8.9 | 1.20 | 0.79–1.83 | 1.5 | 0.61 | 0.32–1.18 | 7.4 | 1.47 | 0.88–2.47 |
| Never married | 308 | 4.6 | 0.53 | 0.24–1.16 | 2.4 | 0.92 | 0.38–2.26 | 2.2 | 0.37 | 0.15–0.92 |
| Unknown | 4,204 | 7.7 | 0.97 | 0.71–1.34 | 2.6 | 1.0 | 0.56–1.77 | 5.1 | 0.96 | 0.72–1.29 |
| Wald χ23 | 4.4 | 3.6 | 11.4 | |||||||
| p | 0.218 | 0.308 | 0.010 | |||||||
| Total | 10,123 | 7.5 | – | – | 2.3 | – | – | 5.2 | – | – |
Note: aOR= odds ratio adjusted for adolescent sex, age, race/ethnicity and poverty index ratio; SE= standard error.
Figure 1.
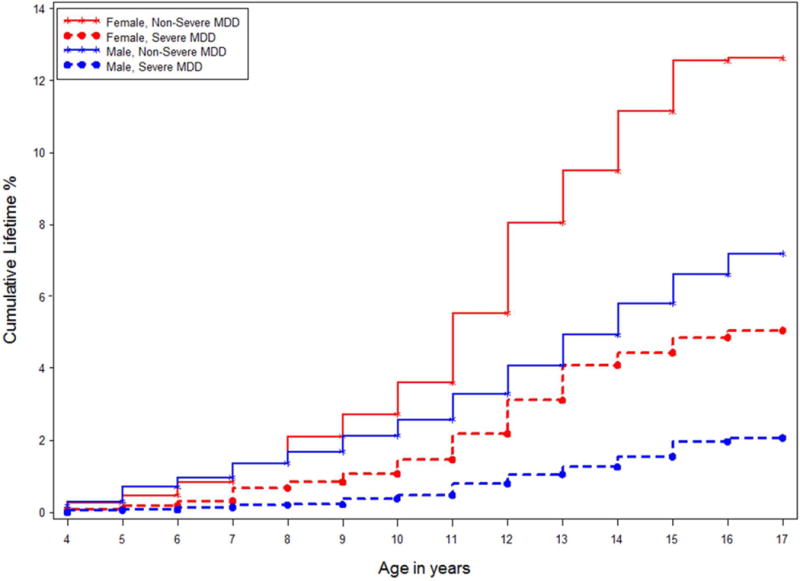
Cumulative lifetime prevalence of major depressive disorder (MDD) by sex and severity.
12-Month MDD Comorbidity
DSM-IV MDD was frequently associated with other classes of mental disorders, representing 63.7% of all 12-month cases. (Table 2- highlights that anxiety and behavioral disorders are most strongly associated with MDD, with a 4-fold increased risk for MDD compared to a 3-fold increased risk for those with ADHD or substance use disorders. Patterns of comorbidity generally did not differ by sex, with the exception that girls with MDD were at greater risk for anxiety or ADHD compared to their male counterparts. Anxiety disorders, behavioral disorders, and any disorder showed significantly stronger associations with severe MDD than with mild/moderate MDD.
Table 2.
12-Month Comorbidity of DSM-IV, Severe, and Mild/Moderate Major Depressive Disorder (MDD) With Other Classes of Mental Disorders
| DSM-IV Class of Disordera |
DSM-IV MDD (Total) |
Severe MDD | Mild/Moderate MDD | Group comparisons (Severe MDD vs. Mild/Moderate MDD) |
|||||
|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | Wald χ21 |
[p] | ||
| Anxiety Disordersd | Female | 4.09 | 2.98 – 5.61 | 5.70 | 3.99 – 8.15 | 3.54 | 2.64 – 4.75 | 2.3 | .127 |
| Male | 3.73 | 2.38 – 5.84 | 8.71 | 3.46 – 21.90 | 3.09 | 1.74 – 5.49 | 3.4 | .066 | |
| Total | 3.96 | 3.01 – 5.21 | 6.18 | 4.26 – 8.97 | 3.36 | 2.48 – 4.56 | 4.8 | .029 | |
| (Female vs. Male) Wald χ21 | 4.3 | 1.2 | 2.1 | – | – | ||||
| p | .038 | .271 | .145 | – | – | ||||
| ADHDe | Female | 2.54 | 0.83 – 7.76 | 14.10 | 3.14 – 63.36 | 1.72 | 0.62 – 4.75 | 2.4 | .124 |
| Male | 2.57 | 1.24 – 5.31 | – | – | 2.96 | 1.36 – 6.43 | 1.6 | .203 | |
| Total | 2.58 | 1.35 – 4.93 | 3.82 | 0.97 – 15.05 | 2.43 | 1.31 – 4.49 | 0.03 | .854 | |
| (Female vs. Male) Wald χ21 | 8.1 | 0.2 | 14.7 | – | – | ||||
| p | .005 | .661 | .0001 | – | – | ||||
| Behavior Disorders (ODD/CD)e | Female | 4.57 | 2.50 – 8.34 | 8.11 | 2.58 – 25.52 | 3.26 | 1.31 – 8.13 | 8.4 | .006 |
| Male | 3.62 | 1.70 – 7.68 | 19.04 | 4.88 – 74.26 | 2.51 | 1.13 – 5.58 | 5.2 | .028 | |
| Total | 4.20 | 2.25 – 7.86 | 10.33 | 4.09 – 26.10 | 3.03 | 1.43 – 6.43 | 15.9 | .0003 | |
| (Female vs. Male) Wald χ21 | 2.2 | 4.8 | 0.1 | – | – | ||||
| p | .139 | .029 | .754 | – | – | ||||
| SUDs d | Female | 3.42 | 2.05 – 5.70 | 3.81 | 2.07 – 7.02 | 3.21 | 1.73 – 5.94 | 2.3 | .128 |
| Male | 2.44 | 1.43 – 4.16 | 1.67 | 0.63 – 4.43 | 2.75 | 1.47 – 5.14 | 1.2 | .275 | |
| Total | 3.08 | 2.21 – 4.28 | 3.07 | 1.82 – 5.15 | 3.10 | 1.97 – 4.89 | 0.8 | .371 | |
| (Female vs. Male) Wald χ21 | 1.9 | 0.1 | 1.9 | – | – | ||||
| p | .171 | .730 | .166 | – | – | ||||
| Any Disorder e | Female | 4.18 | 2.63 – 6.67 | 7.63 | 4.16 – 13.99 | 3.76 | 2.24 – 6.33 | 1.6 | .208 |
| Male | 3.36 | 1.66 – 6.78 | 9.94 | 2.95 – 33.46 | 2.49 | 1.14 – 5.42 | 4.4 | .037 | |
| Total | 3.88 | 2.50 – 6.03 | 7.88 | 4.52 – 13.74 | 3.28 | 2.10 – 5.12 | 4.4 | .036 | |
| (Female vs. Male) Wald χ21 | 2.0 | 0.9 | 0.6 | – | – | ||||
| p | .154 | .343 | .448 | – | – | ||||
Note: The tests of group comparisons adjusted for sex, age, race/ethnicity, and poverty index ratio for the total groups; sex was removed for sex-specific group comparisons. Negative sign (−) denotes value was inestimable due to zero cells. ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; ODD = oppositional defiant disorder; SUD = substance use disorder.
Anxiety disorders include agoraphobia, generalized anxiety disorder, social phobia, specific phobia, panic disorder, posttraumatic stress disorder, separation anxiety disorder; behavior disorders include CD and ODD; SUDs include alcohol and illicit drug abuse or dependence.
Entries are the percentage of respondents with lifetime MDD who also meet lifetime criteria for at least 1 of the other classes of DSM-IV disorder.
Entries are the percentage of respondents with 12-month MDD who also meet 12-month criteria for at least 1 of the other classes of DSM-IV disorders.
Reports based on adolescent Composite International Diagnostic Interview (CIDI; N=10,123).
Reports based on adolescent CIDI and parent self-administered questionnaire (SAQ; n=6,483).
Clinical and Treatment Correlates of 12-Month MDD
Table 3 presents clinical features associated with 12-month MDD. Among those with DSM-IV MDD, 63% reported significant disability in at least one domain of functioning, with 10 days out-of-role in the past 12 months. The duration of episodes was approximately 27 weeks for MDD. Nearly 30% of those with MDD reported some form of suicidality in the past year, with 10.8% reporting a suicide attempt. Compared to mild/moderate MDD, severe MDD was characterized by greater role impairment, twice as many days out-of-role, higher rates of suicide ideation and planning, and more than 3 times the suicide attempts.
Table 3.
Clinical Features Associated With 12-Month DSM-IV, Severe, and Mild/Moderate Major Depressive Disorder (MDD)
| Clinical Features | 12-Month DSM-IV MDD (Total) | 12-Month Severe MDD | 12-Month Mild/Moderate MDD | Group Comparison (Severe MDD vs. Mild/Moderate MDD) |
||||
|---|---|---|---|---|---|---|---|---|
| n=777 | n=232 | n=545 | Wald χ21 | p | ||||
| % or Mean | SE | % or Mean | SE | % or Mean | SE | |||
| Severe Role Impairmenta | 63.00 | 2.8 | 79.27 | 3.7 | 55.30 | 3.21 | 33.4 | <0001 |
| Days out of role in past 12 months | 10.05 | 1.19 | 15.84 | 2.77 | 7.24 | 1.20 | 8.2 | .004 |
| Age of onset | 12.06 | 0.17 | 12.20 | 0.27 | 12.00 | 0.18 | 0.03 | .854 |
| Duration (in weeks) | 26.79 | 3.03 | 34.92 | 6.46 | 23.23 | 2.92 | 2.0 | .154 |
| Suicidality (thought/plan/attempt) in past 12 months | 28.17 | 2.88 | 41.72 | 5.02 | 22.24 | 2.96 | 19.7 | <0001 |
| Suicidal thoughts in past 12 months | 27.34 | 3.02 | 38.97 | 5.83 | 22.24 | 2.96 | 12.3 | .001 |
| Suicide plan in past 12 months | 9.59 | 1.32 | 20.91 | 3.90 | 4.64 | 1.32 | 16.7 | <0001 |
| Suicide attempt in past 12 months | 10.80 | 2.33 | 20.71 | 3.99 | 6.45 | 2.36 | 19.7 | <0001 |
Note: The tests of group comparisons adjusted for sex, age, race/ethnicity, and poverty index ratio. SE= standard error.
Severe or very severe impairment (≥7) on any of the 4 Sheehan Disability Scale role domains (home, school/work, family, social).
Treatment in any form was received by the majority of adolescents with 12-month DSM-IV MDD (60.4%). However, a much lower percentage received disorder-specific treatment (33.9%) or treatment from the mental health sector (34.9%). Disorder-specific treatment for severe MDD (44.7%) was more frequent than for mild/moderate MDD (29.4%) (Wald F(1) =7.5, p<.01), and more frequent among males (56.6%) than females (40.3%) (Wald F(1) =5.0, p<.05). Rates of disorder-specific treatment were also higher for 15- to 16-year-olds with severe MDD than for the other age groups (Wald F(2) =3.5, p<.05). Concerning sociodemographic correlates of disorder-specific treatment, services for 12-month DSM-IV MDD were less frequent for black (OR=0.08; 95% CI=0.02–0.24) and Hispanic adolescents (OR=0.23; 95% CI=0.10–0.54) as well as for those living in the Midwest (OR=0.28, 95% CI=0.12–0.66), but services were more frequent among adolescents whose parents were not married (OR=2.07; 95% CI=1.02–4.23) and who had a high school education (OR=2.51; 95% CI=1.11–5.71) or some college (OR=2.62; 95% CI=1.20–5.71). Disorder-specific treatment of severe MDD was less frequent among both black (OR=0.10; 95% CI=0.02–0.60) and Hispanic adolescents (OR=0.05; 95% CI=0.00–0.50), but more frequent among children of unmarried parents (OR=6.40; 95% CI=1.30–31.38).
DISCUSSION
When applying DSM-IV criteria, MDD was highly prevalent in this population, whether measured over the lifetime (11%) or past year (7.5%). Dysthymia affected far fewer adolescents and co-occurred with MDD in approximately 90% of cases. The increasing prevalence of MDD across adolescence was markedly greater in females than males. Most cases of MDD were associated with psychiatric comorbidity and severe role impairment, and a substantial minority of depressed adolescents reported suicidal ideation, planning, or attempts. Importantly, the majority of adolescents with MDD did not receive disorder-specific treatment, and this discrepancy was greatest for minority youth.
Several findings from this study highlight the clinical and public health need for screening, early identification, and early intervention of MDD during adolescence. First, it is notable that the prevalence of MDD is high, represents about two-thirds of the lifetime adult cases2, and is independent of most sociodemographic characteristics. These findings underscore the ubiquitous nature of this disorder in youth, suggest that a significant portion of depressive disorders have their first onset in adolescence, and support the notion of routine and universal screening during adolescence. Second, the female preponderance of depression in this study is consistent with other community-based studies6,10 and indicates that females are a particularly vulnerable subgroup that should be targeted in preventive efforts during adolescence. Third, findings that the majority of adolescents with MDD demonstrated impairment and high comorbidity with other mental conditions is indicative of a protracted clinical course and poorer treatment response20,21, thereby highlighting the importance of early intervention. The elevated prevalence of suicidal ideation, planning, and attempts in this population is of particular concern considering that suicide is the third leading cause of death among US teenagers22. Detailed findings of the prevalence, correlates, and treatment of suicidality are presented elsewhere23,24.
Of immediate concern are the more than 25% of depressed adolescents had severe MDD as indicated by high levels of distress and impairment that met the definition of severe MDD. Related clinical correlates were far greater, with considerably higher rates for suicidal thoughts and behaviors, among those with severe depression compared to those with mild/moderate depression. Comorbidity was also more prevalent among those with severe MDD. In addition to the immediate challenges of treating adolescents with acute severe symptoms of depression, severe depression has been associated with recurrence of depressive episodes, chronic health conditions, significant social and economic costs and consequences, and reduced quality of life in adults25.
Concerning service utilization, as seen in adolescents with bipolar disorder26, the majority of depressed adolescents did not receive treatment specifically for their depression, nor from the mental health sector for any emotional or behavioral problem. The finding that adolescents living in non-married families are more likely to receive treatment is unexpected, but it may reflect the need to use services to cope with associated problems and challenges. Although adolescents with severe MDD are more likely than those with less severe MDD to receive depression-specific treatment, there remain a high proportion of untreated cases of severe major depression. Despite this unmet need, instruments exist with sufficient sensitivity and specificity to be used for the screening of depression in school or primary care settings27 with subsequent referral to mental health specialties. A recent meta-analysis found that such prevention programs for youth led to moderate but significant reductions in depression symptoms and certain interventions reduced the incidence of future depressive disorder28 in particular for high-risk groups.
This report confirms the majority of estimates provided by recent national surveys of 12-month rates of MDD and treatment8,29 and by smaller community studies.30,31 However, the NCS-A provides the most comprehensive information to date concerning adolescent depression: estimates of both lifetime and 12-month prevalence, sociodemographic correlates, and comorbidity for DSM-IV MDD, mild/moderate MDD, and severe MDD in a national sample of US adolescents.
Several methodological limitations should be considered in interpreting the present findings. The cross-sectional nature of the survey limits our ability to characterize the progression of depressive disorders over time or to identify predictive risk-factors, and the assessment of lifetime disorders may be affected by retrospective recall. Follow-up of the NCS-A sample, as well as new prospective work, are needed to not only quantify these potential biases but also to examine the evolution of disorders at this vulnerable period of life. Information was acquired from only one parent, and this was based on a questionnaire and not a direct diagnostic interview. We also did not present information concerning subthreshold or minor forms of depression, entities that may affect a considerable number of adolescents and in some cases merit professional treatment. NCS-A provides a snapshot of mental health at a given time, and changes in health care after 2004 require additional attention. Nevertheless, this report provides novel information on a more severe form of this disorder that affects substantial numbers of adolescents and that is associated with considerable morbidity. The goal of minimizing the global burden of depression requires careful descriptions of its different manifestations and complex risk factors, in particular at the time of life when intervention and prevention are most needed.
Supplementary Material
Acknowledgments
This study was supported by the intramural Research Program of the NIMH (1 ZIA MH002808). The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or US government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental material cited in this article is available online.
Ms. He served as the statistical expert for this research.
Disclosure: Drs. Avenevoli, Swendsen, Burstein, Merikangas, and Ms. He report no biomedical financial interests or potential conflicts of interest.
References
- 1.WHO. The global burden of disease: 2004 update, Table A2: Burden of disease in DALYs by cause, sex and income group in WHO regions, estimates for 2004. Geneva: The World Health Organization; 2008. [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Burcusa SL, Iacono WG. Risk for recurrence in depression. Clinical psychology review. 2007;27(8):959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spijker J, de Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA. Duration of major depressive episodes in the general population: results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) The British journal of psychiatry : the journal of mental science. 2002;181:208–213. doi: 10.1192/bjp.181.3.208. [DOI] [PubMed] [Google Scholar]
- 5.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Archives of general psychiatry. 2003;60(7):709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 6.Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. Journal of abnormal psychology. 1998;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 7.Olfson M, Gameroff MJ, Marcus SC, Waslick BD. Outpatient treatment of child and adolescent depression in the United States. Archives of general psychiatry. 2003;60(12):1236–1242. doi: 10.1001/archpsyc.60.12.1236. [DOI] [PubMed] [Google Scholar]
- 8.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Results from the 2007 National Survey on Drug Use and Health: National findings. Rockville, MD: Office of Applied Studies; 2008. (DHHS Publication No SMA 08-4343, NSDUH Series H-34). [Google Scholar]
- 10.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merikangas K, Avenevoli S, Costello J, Koretz D, Kessler RC. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48(4):367–369. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Avenevoli S, Costello EJ, et al. National comorbidity survey replication adolescent supplement (NCS-A): II. Overview and design. J Am Acad Child Adolesc Psychiatry. 2009;48(4):380–385. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kessler RC, Avenevoli S, Costello EJ, et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Int J Methods Psychiatr Res. 2009;18(2):69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International journal of methods in psychiatric research. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grills AE, Ollendick TH. Issues in parent-child agreement: the case of structured diagnostic interviews. Clinical child and family psychology review. 2002;5(1):57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- 16.Foley D, Rutter M, Pickles A, et al. Informant disagreement for separation anxiety disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(4):452–460. doi: 10.1097/00004583-200404000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Foley DL, Rutter M, Angold A, et al. Making sense of informant disagreement for overanxious disorder. Journal of anxiety disorders. 2005;19(2):193–210. doi: 10.1016/j.janxdis.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 18.Jensen PS, Rubio-Stipec M, Canino G, et al. Parent and child contributions to diagnosis of mental disorder: are both informants always necessary? Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(12):1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(5):610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Hagnell O, Grasbeck A. Comorbidity of anxiety and depression in the Lundby 25-year prospective study: The pattern of subsequent episodes. In: Maser J, Cloninger C, editors. Comorbidity of Mood and Anxiety Disorders. Washington, DC: American Psychiatric Press, Inc; 1990. pp. 139–152. [Google Scholar]
- 21.Murphy J. Diagnostic comorbidity and symptom co-occurence: The Stirling County Study. Washington, D.C: American Psychiatric Press, Inc; 1990. [Google Scholar]
- 22.CDC. 10 Leading Causes of Death by Age Group, United States – 2007. Atlanta: Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 23.Husky MM, Olfson M, He JP, Nock MK, Swanson SA, Merikangas KR. Twelve-month suicidal symptoms and use of services among adolescents: results from the National Comorbidity Survey. Psychiatric services. 2012;63(10):989–996. doi: 10.1176/appi.ps.201200058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nemeroff CB. The burden of severe depression: a review of diagnostic challenges and treatment alternatives. Journal of psychiatric research. 2007;41(3–4):189–206. doi: 10.1016/j.jpsychires.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 26.Khazanov GK, Cui L, Merikangas KR, Angst J. Treatment Patterns of Youth with Bipolar Disorder: Results from the National Comorbidity Survey-Adolescent Supplement (NCS-A) J Abnorm Child Psychol. 2014 Jun 24; doi: 10.1007/s10802-014-9885-6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Williams SB, O’Connor EA, Eder M, Whitlock EP. Screening for child and adolescent depression in primary care settings: a systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2009;123(4):e716–735. doi: 10.1542/peds.2008-2415. [DOI] [PubMed] [Google Scholar]
- 28.Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. Journal of consulting and clinical psychology. 2009;77(3):486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.SAMHSA. Results from the 2012 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 30.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of general psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 31.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of abnormal psychology. 1993;102(1):133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


