Abstract
Objective
Describe the epidemiology of healthcare-related (ie, healthcare-associated and hospital-acquired) pneumonia due to methicillin-resistant Staphylococcus aureus (MRSA) among hospitalized patients in community hospitals.
Design
Retrospective cohort study.
Setting
Twenty-four community hospitals in the southeastern United States affiliated with the Duke Infection Control Outreach Network (median size, 211 beds; range, 103–658 beds).
Methods
Adult patients with healthcare-related MRSA pneumonia admitted to study hospitals from January 1, 2008, to December 31, 2012, were identified using surveillance data. Seasonal and annual incidence rates (cases per 100,000 patient-days) were estimated using generalized estimating equation models. Characteristics of community-onset and hospital-onset cases were compared.
Results
A total of 1,048 cases of healthcare-related pneumonia due to MRSA were observed during 5,863,941 patient-days. The annual incidence rate of healthcare-related MRSA pneumonia increased from 11.3 cases per 100,000 patient-days (95% confidence interval [CI], 6.8–18.7) in 2008 to 15.5 cases per 100,000 patient-days (95% CI, 8.4–28.5) in 2012 (P = .055). The incidence rate was highest in winter months and lowest in summer months (15.4 vs 11.1 cases per 100,000 patient-days; incidence rate ratio, 1.39 [95% CI, 1.06–1.82]; P = .016). A total of 814 cases (77.7%) were community-onset healthcare-associated pneumonia cases; only 49 cases (4.7%) were ventilator-associated cases. Of 811 patients whose disposition was known, 240 (29.6%) died during hospitalization or were discharged to hospice.
Conclusions
From 2008 through 2012, the incidence of healthcare-related MRSA pneumonia among patients who were admitted to a large network of community hospitals increased, despite the decreasing incidence of invasive MRSA infections nationwide. Additional study is warranted to evaluate trends in this important and potentially modifiable public health problem.
Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most common causes of pneumonia in healthcare-exposed patients, and it accounts for more than 20% of cases of hospital-acquired pneumonia (HAP) and healthcare-associated pneumonia (HCAP).1-4 Invasive infections due to MRSA are associated with excess morbidity and mortality and high costs to the healthcare system.5 For example, in one case series, approximately 1 in 3 patients with HCAP or HAP due to MRSA died within 30 days of their infection.6
The epidemiology of severe infections caused by MRSA has changed in the last 2 decades. Although the incidence of MRSA pneumonia and other invasive infections caused by MRSA increased in the 1990s and 2000s, due in part to the emergence of a more virulent community-acquired MRSA strain,3,7 more recent data demonstrate that the incidence of serious infections due to MRSA has decreased since 2005 in numerous settings.8-12 The reason for the recent downtrend is not fully understood but may relate to a multitude of factors, including increased awareness and efforts to reduce transmission of infections in healthcare settings.12
Most data on the epidemiology of pneumonia in healthcare-exposed patients are derived from tertiary care centers, academic hospitals, and major urban settings.4,6,13 However, approximately half of US hospitalizations occur in nonteaching hospitals.14 To our knowledge, no data have been published regarding the epidemiology of MRSA pneumonia in the community hospital setting. Thus, the objective of our study was to describe the epidemiology of MRSA pneumonia among healthcare-exposed patients admitted to community hospitals.
Methods
Design and Setting
We used prospectively collected surveillance data to analyze rates of HCAP and HAP due to MRSA among patients admitted to community hospitals participating in the Duke Infection Control Outreach Network (DICON). HAP and HCAP will be collectively referred to as “healthcare-related pneumonia.” DICON is a network of community hospitals in the southeastern United States that has been described previously.15 In brief, all DICON-affiliated hospitals have active infection control and surveillance programs that collect complete and consecutive surveillance data on healthcare-associated infections (HAIs) and infections due to multidrug-resistant organisms for benchmarking and reporting purposes. Our analysis included all cases of healthcare-related pneumonia due to MRSA identified among adult (age >18 years) inpatients at 24 DICON-affiliated hospitals (median size, 211 beds; range, 103–658 beds) with complete surveillance data from January 1, 2008, to December 31, 2012.
Data Collection
During the 5-year study period, trained infection preventionists (IPs) at local hospitals prospectively identified infections due to MRSA from microbiology data. Standardized surveillance definitions were applied to determine whether patients had infection versus colonization.16 Deidentified demographic, clinical, and microbiologic data were collected and recorded in a centralized database. A subset of cases at each hospital was validated by DICON liaison IPs.
Cases of healthcare-related pneumonia due to MRSA were further classified as HAP or HCAP using the following definitions, which were adapted from existing clinical and surveillance case definitions.1,17 Cases of HAP were defined as follows: (1) symptoms of infection were not present at the time of hospital admission, and surveillance criteria for pneumonia were fulfilled more than 48 hours after admission to the hospital; or (2) the patient was transferred from another hospital, and surveillance criteria for pneumonia were fulfilled 48 hours or less after hospital admission; or (3) the patient had been discharged 48 hours or less before admission, and surveillance criteria for pneumonia were fulfilled 48 hours or less after readmission. Cases of HCAP were defined as follows: (1) surveillance criteria for pneumonia were fulfilled 48 hours or less after admission to the hospital, and the patient was discharged from the same hospital between 1 year and 48 hours earlier, was admitted from a nursing home or long-term care facility, or was receiving outpatient hemodialysis; or (2) surveillance criteria for pneumonia were fulfilled more than 48 hours after hospital admission, but the patient had symptoms of pneumonia present at the time of hospital admission and healthcare exposure as described above.
Statistical Analysis
Characteristics and outcomes of patients with HAP and HCAP were described and compared using χ2 tests for categorical variables and Wilcoxon rank sum tests for continuous variables. MRSA pneumonia incidence was calculated as number of events per 100,000 patient-days. Generalized estimating equation models using a Poisson distribution were used to estimate annual and seasonal incidence rates of MRSA infection while controlling for nonrandom clustering of outcomes within hospitals. Year and season were the independent variables in the respective models and were modeled using indicator terms. Seasons were defined by calendar month as follows: winter (December–February), spring (March–May), summer (June–August), fall (September–November). In all models, overdispersion was observed and corrected using the Pearson χ2 as the dispersion parameter. Denominator data were normalized by log transformation. One hospital was excluded from the trend analyses, because this hospital was a significant outlier (ie, the hospital's rate of healthcare-related MRSA pneumonia was greater than 3 standard deviations higher than the mean for the study hospitals). Statistical analysis was performed using SAS, version 9.3 (SAS Institute). A P value of .05 or less was considered statistically significant.
Results
Overall, 1,048 cases of healthcare-related pneumonia due to MRSA were observed during 5,863,941 patient-days at the 24 participating hospitals. The annual incidence rate (adjusted for in-hospital clustering) of healthcare-related pneumonia due to MRSA increased from 11.3 cases per 100,000 patient-days (95% confidence interval [CI], 6.8–18.7) in 2008 to a peak of 18.5 cases per 100,000 patient-days (95% CI, 10.7–32.1) in 2010 and then decreased to 15.5 cases per 100,000 patient-days (95% CI, 8.4–28.5) in 2012 (Table 1; P = .055 for linear trend). In contrast, the annual incidence rate (adjusted for in-hospital clustering) of other healthcare-related infections due to MRSA decreased from 129.3 cases per 100,000 patient-days (95% CI, 103.6–161.4) in 2008 to 103.8 cases per 100,000 patient-days (95% CI, 79.1–136.3) in 2012 (P = .056 for linear trend).
Table 1. Incidence Rates of Healthcare-Related Pneumonia due to Methicillin-Resistant Staphylococcus aureus, Duke Infection Control Outreach Network, 2008–2012.
| Year | Cases | Patient-days | Crude incidence ratea | Adjusted incidence rate (95% CI)a,b | Incidence rate ratio (95% CI)b |
|---|---|---|---|---|---|
| 2008 | 146 | 1,202,434 | 12.1 | 11.3 (6.8–18.7) | Ref |
| 2009 | 183 | 1,172,374 | 15.6 | 14.6 (8.3–25.7) | 1.29 (0.91, 1.83) |
| 2010 | 232 | 1,167,885 | 19.9 | 18.5 (10.7–32.1) | 1.64 (1.07, 2.53) |
| 2011 | 212 | 1,126,537 | 18.8 | 17.5 (9.6–31.9) | 1.55 (1.03, 2.33) |
| 2012 | 182 | 1,095,048 | 16.6 | 15.5 (8.4–28.5) | 1.38 (0.92, 2.07) |
Note. CI, confidence interval; Ref, reference.
Cases per 100,000 patient-days.
Point estimates and 95% CIs obtained using generalized estimating equation with Poisson distribution, adjusting for within-hospital clustering of observations.
The monthly incidence rates of healthcare-related pneumonia due to MRSA for the entire study period are shown in Figure 1. The seasonal incidence rate (adjusted for in-hospital clustering) of healthcare-related pneumonia was higher during winter (December–February) compared with summer (June–August; 15.4 vs 11.1 cases per 100,000 patient-days; incidence rate ratio [95% CI], 1.39 [1.06–1.82]; P = .016), whereas there was no significant difference in incidence rates during the other seasons of the year (Figure 2).
Figure 1.
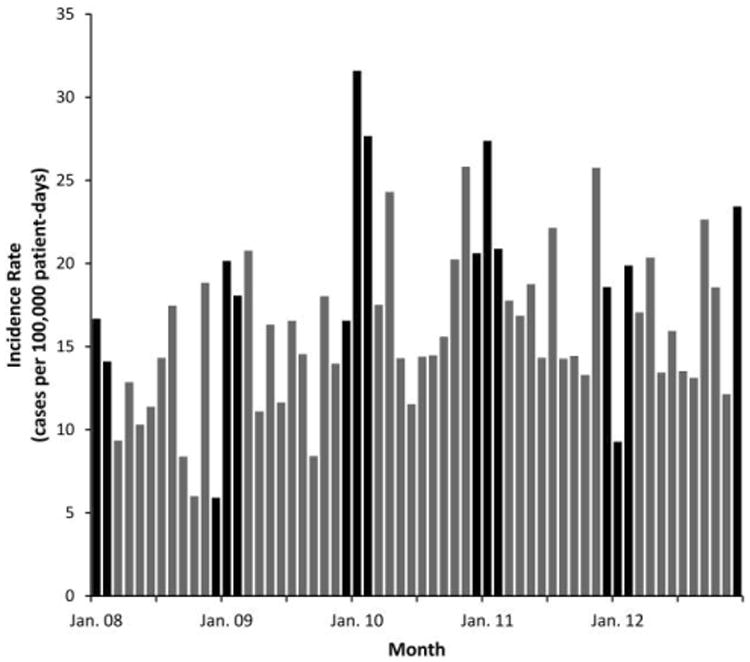
Monthly incidence rates of healthcare-related pneumonia caused by methicillin-resistant Staphylococcus aureus in patients admitted to community hospitals, Duke Infection Control Outreach Network, 2008–2012. Winter months (December–February) are highlighted in black.
Figure 2.
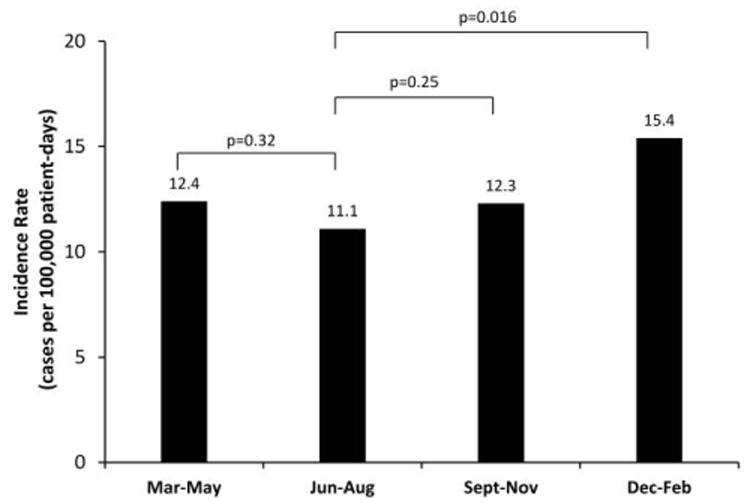
Seasonal incidence rates of healthcare-related pneumonia caused by methicillin-resistant Staphylococcus aureus in patients admitted to community hospitals, Duke Infection Control Outreach Network, 2008–2012. Incidence rate point estimates and P values obtained using generalized estimating equation with Poisson distribution, adjusting for within-hospital clustering of observations.
The median age of patients with healthcare-related pneumonia due to MRSA was 73 years (interquartile range [IQR], 61–82); 444 patients (52.6%) were male; 537 patients (51.6%) were admitted from home, and 423 patients (40.7%) were admitted from skilled nursing facilities (Table 2). Only 49 cases (4.7%) were categorized as ventilator-associated pneumonia.
Table 2. Characteristics of Patients Admitted to Community Hospitals within the Duke Infection Control Outreach Network with Healthcare-Related Pneumonia due to Methicillin-Resistant Staphylococcus aureus, 2008–2012.
| Characteristic | Total (n = 1,048) | HAP (n = 234) | HCAP (n = 814) | Pa |
|---|---|---|---|---|
| Age, years | ||||
| Median (IQR) | 73 (61–82) | 68 (58–78) | 74 (61–83) | <.001 |
| >80 | 312 (29.8) | 45 (19.2) | 267 (32.8) | <.001 |
| Sex | .093 | |||
| Female | 400 (47.4) | 89 (42.4) | 311 (49.1) | |
| Male | 444 (52.6) | 121 (57.6) | 323 (51.0) | |
| Missing | 204 | … | … | |
| Admitted from location | <.001 | |||
| Home | 537 (51.6) | 122 (53.5) | 415 (51.1) | |
| Other hospital | 64 (6.2) | 64 (28.1) | 0 (0.0) | |
| Skilled nursing facility | 423 (40.7) | 38 (16.7) | 385 (47.4) | |
| Other | 16 (1.5) | 4 (1.8) | 12 (1.5) | |
| Missing | 8 | … | … | |
| Dialysis | .50 | |||
| Yes | 54 (5.4) | 10 (4.5) | 44 (5.6) | |
| No | 951 (94.6) | 213 (95.5) | 738 (94.4) | |
| Missing | 43 | … | … | |
| Ventilator-associated pneumonia | 49 (4.7) | 45 (19.2) | 4 (0.5) | <.001 |
| Polymicrobial infectionb | 78 (7.4) | 22 (9.4) | 56 (6.9) | .20 |
Note. Data are no. (%) of patients, unless otherwise indicated. HAP, hospital-acquired pneumonia; HCAP, healthcare-associated pneumonia; IQR, interquartile range.
P value for the comparison of HAP to HCAP using Wilcoxon rank sum test (age) or Pearson χ2 test (all other variables).
More than 1 pathogen identified in respiratory specimen.
Clinical characteristics and outcomes of patients with HAP were compared with those of patients with HCAP (Tables 2 and 3). There were 234 cases of HAP (22.3%) and 814 cases of HCAP (77.7%). Patients with HCAP tended to be older: 267 patients with HCAP (32.8%) were greater than 80 years old versus 45 patients with HAP (19.2%) who were greater than 80 years old (P < .001). A total of 385 (47.4%) of the patients with MRSA HCAP were admitted from skilled nursing care facilities, whereas only 38 (16.7%) of the patients with MRSA HAP were admitted from skilled nursing care facilities (P < .001). The median number of days from positive culture to hospital discharge was 11 (IQR, 6–20) among the patients with HAP and 8 (IQR, 4–13) among the patients with HCAP (P < .001). Of the patients who had documented discharge dispositions, 76 (44.4%) of the patients with HAP died or were discharged to hospice versus 164 (25.6%) of the patients with HCAP.
Table 3. Outcomes of Patients Admitted to Community Hospitals within the Duke Infection Control Outreach Network with Healthcare-Related Pneumonia due to Methicillin-Resistant Staphylococcus aureus, 2008–2012.
| Outcome | Total (n = 1,048) | HAP (n = 234) | HCAP (n = 814) | Pa |
|---|---|---|---|---|
| Disposition | <.001 | |||
| Death/hospice | 240 (29.6) | 76 (44.4) | 164 (25.6) | |
| Home | 247 (30.5) | 28 (16.4) | 219 (34.2) | |
| Skilled nursing facility | 288 (35.5) | 53 (31.0) | 235 (36.7) | |
| Other hospital | 36 (4.4) | 14 (8.2) | 22 (3.4) | |
| Missing | 237 | … | … | |
| LOS, days, median (IQR) | 10 (6–17) | 18 (12–31) | 9 (6–14) | <.001 |
| Days from culture to hospital discharge, median (IQR) | 8 (5–13) | 11 (6–20) | 8 (4–13) | <.001 |
Note. HAP, hospital-acquired pneumonia; HCAP, healthcare-associated pneumonia; IQR, interquartile range; LOS, length of stay.
P value for the comparison of HAP to HCAP using Wilcoxon rank sum test (LOS, days from positive culture to hospital discharge) or Pearson χ2 test (disposition).
Discussion
Our observational cohort study describes the epidemiology and characteristics of patients with healthcare-related MRSA pneumonia admitted to community hospitals in the United States. To our knowledge, longitudinal trends in incidence of healthcare-related MRSA pneumonia have not been previously examined. Furthermore, most studies of invasive MRSA infections have either used pooled data from all healthcare settings or data from tertiary care and academic centers. Our study is unique in that it describes longitudinal trends in MRSA pneumonia in an important population of patients: those seeking care in community hospitals.
Healthcare-related MRSA pneumonia continues to be prevalent in community hospitals. The incidence of healthcare-related pneumonia caused by MRSA did not decrease in our cohort over the period of our study, in contrast to other reports describing a recent decrease in the incidence of invasive MRSA infections in the United States.8-12 For example, Dantes et al12 reported that the incidence of hospital-onset invasive MRSA infections decreased by approximately 54%, and the incidence of healthcare-associated invasive MRSA infections decreased by approximately 28% in 2011 compared with 2005 in 9 major US metropolitan areas. Reasons for this discrepancy between the relatively stable incidence of healthcare-related MRSA pneumonia in community hospitals and decreasing national trends in invasive MRSA infections are unknown, but we offer 2 potential explanations. First, it may be problematic to compare trends in incidence of pneumonia to overall trends in invasive infections, as we have attempted to do. Pneumonia comprised only 15% of the total invasive MRSA infections occurring in 2011 included in the aforementioned study.12 Thus, downward trends in invasive infections observed nationally may be primarily driven by infections other than pneumonia. Second, in comparison to other sites of invasive infection, incidence of pneumonia may be influenced more by external factors (eg, circulating influenza) and therefore less responsive to interventions designed to curb the transmission of MRSA in hospital settings. Thus, interventions that have effectively decreased rates of blood-stream infection due to MRSA may not be equally effective at reducing pneumonia. Unfortunately, comparative data from tertiary care centers regarding the longitudinal trends in MRSA pneumonia among hospitalized patients are not available. Therefore, additional data regarding MRSA pneumonia incidence trends in other multicenter networks are needed to corroborate our findings.
We observed a clear seasonal trend in the incidence of healthcare-related MRSA among hospitalized patients. The incidence of infection was highest in the winter months and lowest in the summer months. This trend is consistent with the findings of Klein et al,18 who used different methodology to estimate the annual and seasonal trends in inpatient admissions for pneumonia caused by MRSA. The observed peak incidence during winter months is likely due in part to the known association between staphylococcal pneumonia and influenza.19 The greatest incidence rates were observed in January and February 2010, lagging behind the peak incidence of pandemic H1N1 influenza A activity in the US by approximately 2 months.20
Our study highlights the high mortality rate among patients hospitalized with MRSA pneumonia. Nearly 30% of patients in our study died or were discharged to hospice. Other groups have reported similar mortality rates for patients with healthcare-associated pneumonia due to MRSA.4,6 It is possible that the observed relationship between MRSA pneumonia and poor outcomes may be confounded by other factors. Still, our data suggest that, at the very least, MRSA pneumonia is a marker of severe illness and that ongoing efforts to optimize prevention and treatment of this illness are warranted.
Many infection prevention programs focus surveillance efforts on ventilator-associated pneumonia, given its associated morbidity, mortality, and costs.21-24 In our cohort, ventilator-associated pneumonia comprised only approximately 5% of all healthcare-related MRSA pneumonia cases and approximately 20% of all cases of HAP due to MRSA. Therefore, infection prevention programs that only perform surveillance for ventilator-associated pneumonia will fail to identify a large number of hospital-acquired infections and will significantly underestimate the burden of healthcare-related MRSA pneumonia at their institutions.
Our study has several limitations that may affect the generalizability of our data to patients in other settings. First, this study was performed in community hospitals in a single geographic region of the United States. However, we believe that the large number and variable size of hospitals included in this analysis strengthens our findings. Second, surveillance definitions for pneumonia are imperfect; it is possible that some patients who were included in this study did not have clinical disease and that other patients with clinical diagnoses of pneumonia were excluded from this analysis. All hospitals used the same methods and definitions for identifying healthcare-related MRSA pneumonia, and DICON liaison IPs performed case validation on a sample of cases. Finally, although we described outcomes associated with MRSA pneumonia, we were unable to assess causality or perform detailed patient-level risk factor analysis for poor outcomes related to healthcare-related MRSA pneumonia.
In summary, healthcare-related MRSA pneumonia is a serious infection associated with high mortality and is an important public health problem that warrants further study. We observed the highest incidence of healthcare-related MRSA pneumonia in winter months, peaking in 2010. In contrast to other work showing a clear decrease in the incidence of invasive MRSA infections, the incidence rate of healthcare-related MRSA pneumonia has not decreased in this network of community hospitals over a similar time period. Existing infection prevention measures that have successfully reduced the overall burden of MRSA in healthcare settings may be insufficient to prevent pneumonia due to MRSA.
Acknowledgments
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (K23AI095457 to D.J.A.).
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
Presented in part: American Thoracic Society International Conference; Philadelphia, Pennsylvania; May 17–22, 2013.
References
- 1.Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 2.Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(6):3854–3862. doi: 10.1378/chest.128.6.3854. [DOI] [PubMed] [Google Scholar]
- 3.Rubinstein E, Kollef MH, Nathwani D. Pneumonia caused by methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008;46(suppl 5):S378–S385. doi: 10.1086/533594. [DOI] [PubMed] [Google Scholar]
- 4.Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568–3573. doi: 10.1128/AAC.00851-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shorr AF, Haque N, Taneja C, et al. Clinical and economic outcomes for patients with health care-associated Staphylococcus aureus pneumonia. J Clin Microbiol. 2010;48(9):3258–3262. doi: 10.1128/JCM.02529-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tadros M, Williams V, Coleman BL, et al. Epidemiology and outcome of pneumonia caused by methicillin-resistant Staphylococcus aureus (MRSA) in Canadian hospitals. PLoS One. 2013;8(9):e75171. doi: 10.1371/journal.pone.0075171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fagon JY, Maillet JM, Novara A. Hospital-acquired pneumonia: methicillin resistance and intensive care unit admission. Am J Med. 1998;104(5A):17S–23S. doi: 10.1016/s0002-9343(98)00151-x. [DOI] [PubMed] [Google Scholar]
- 8.Burton DC, Edwards JR, Horan TC, Jernigan JA, Fridkin SK. Methicillin-resistant Staphylococcus aureus central line-associated bloodstream infections in US intensive care units, 1997–2007. JAMA. 2009;301(7):727–736. doi: 10.1001/jama.2009.153. [DOI] [PubMed] [Google Scholar]
- 9.Jain R, Kralovic SM, Evans ME, et al. Veterans affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med. 2011;364(15):1419–1430. doi: 10.1056/NEJMoa1007474. [DOI] [PubMed] [Google Scholar]
- 10.Kallen AJ, Mu Y, Bulens S, et al. Health care-associated invasive MRSA infections, 2005–2008. JAMA. 2010;304(6):641–648. doi: 10.1001/jama.2010.1115. [DOI] [PubMed] [Google Scholar]
- 11.Landrum ML, Neumann C, Cook C, et al. Epidemiology of Staphylococcus aureus blood and skin and soft tissue infections in the US military health system, 2005–2010. JAMA. 2012;308(1):50–59. doi: 10.1001/jama.2012.7139. [DOI] [PubMed] [Google Scholar]
- 12.Dantes R, Mu Y, Belflower R, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med. 2013;173(21):1970–1978. doi: 10.1001/jamainternmed.2013.10423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carratala J, Mykietiuk A, Fernandez-Sabe N, et al. Health care-associated pneumonia requiring hospital admission: epidemiology, antibiotic therapy, and clinical outcomes. Arch Intern Med. 2007;167(13):1393–1399. doi: 10.1001/archinte.167.13.1393. [DOI] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality. HCUPnet. [Accessed March 8, 2014]; http://hcupnet.ahrq.gov.
- 15.Anderson DJ, Miller BA, Chen LF, et al. The network approach for prevention of healthcare-associated infections: long-term effect of participation in the Duke Infection Control Outreach Network. Infect Control Hosp Epidemiol. 2011;32(4):315–322. doi: 10.1086/658940. [DOI] [PubMed] [Google Scholar]
- 16.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Klevens RM, Morrison MA, Nadle J, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298(15):1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- 18.Klein EY, Sun L, Smith DL, Laxminarayan R. The changing epidemiology of methicillin-resistant Staphylococcus aureus in the United States: a national observational study. Am J Epidemiol. 2013;177(7):666–674. doi: 10.1093/aje/kws273. [DOI] [PubMed] [Google Scholar]
- 19.Kallen AJ, Brunkard J, Moore Z, et al. Staphylococcus aureus community-acquired pneumonia during the 2006 to 2007 influenza season. Ann Emerg Med. 2009;53(3):358–365. doi: 10.1016/j.annemergmed.2008.04.027. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. FluView: 2009-2010 influenza season summary. [Accessed March 8, 2014]; http://www.cdc.gov/flu/weekly/weeklyarchives2009-2010/09-10summary.htm.
- 21.Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- 22.Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C. Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med. 1993;94(3):281–288. doi: 10.1016/0002-9343(93)90060-3. [DOI] [PubMed] [Google Scholar]
- 23.Rello J, Ollendorf DA, Oster G, et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest. 2002;122(6):2115–2121. doi: 10.1378/chest.122.6.2115. [DOI] [PubMed] [Google Scholar]
- 24.Venditti M, Falcone M, Corrao S, Licata G, Serra P. Outcomes of patients hospitalized with community-acquired, health care–associated, and hospital-acquired pneumonia. Ann Intern Med. 2009;150(1):19–26. doi: 10.7326/0003-4819-150-1-200901060-00005. [DOI] [PubMed] [Google Scholar]


