Abstract
Background:
Meningiomas of the velum interpositum in the roof of the third ventricle are rare. Knowing from which leaflet the meningioma originates and thus its relationships with the internal cerebral and Galen veins, may help in choosing the surgical approach.
Case Description:
We report the case of a 40-year-old male with a meningioma arising from the superior leaflet of the velum interpositum. The tumor was resected successfully using the infratentorial-supracerebellar approach. Reviewing the literature, of the 22 reported cases of velum interpositum meningiomas, sufficient information regarding the precise location of the origin of the tumor was provided in 14 cases, all of which were from the inferior leaflet.
Conclusion:
We report the first case of velum interpositum meningioma arising from the superior leaflet and give a potential explanation as to why meningiomas of the velum interpositum occur more commonly on the inferior leaflet. Distinguishing from which of the two leaflets the tumor originates may influence the surgical strategy.
Keywords: Meningioma, meningiomas without dural attachment, pineal region, velum interpositum
INTRODUCTION
Meningiomas arising from the velum interpositum (VI) in the roof of the third ventricle are rare. Potentially, they may come from the upper or lower leaflet, displacing the internal cerebral veins accordingly. We describe the first case of a meningioma arising from the superior leaflet of the VI.
CASE REPORT
History and examination
A 40-year-old male consulted in June 2001 for a head trauma following alcohol consumption. His past medical history revealed long-standing alcohol abuse, smoking, and a depressive disorder with anxiety. In addition, he suffered from severe episodic headaches without nausea or vomiting. The neurological examination was entirely normal with good awareness and no focal deficit.
Imagery
The head computed tomography (CT) showed a mild left frontal contusion and a pineal region tumor. A magnetic resonance imaging (MRI) showed an isointense 1.4 cm, well delineated spherical tumor of the pineal region [Figure 1]. The lesion was homogeneously enhanced with gadolinium. There was no associated hydrocephalus and the tumor was not attached to either the falx cerebri or the tentorium cerebelli. The internal cerebral veins were pushed inferiorly by the lesion. The differential diagnosis at that time included germinoma, ependymoma, and meningioma of the VI.
Figure 1.
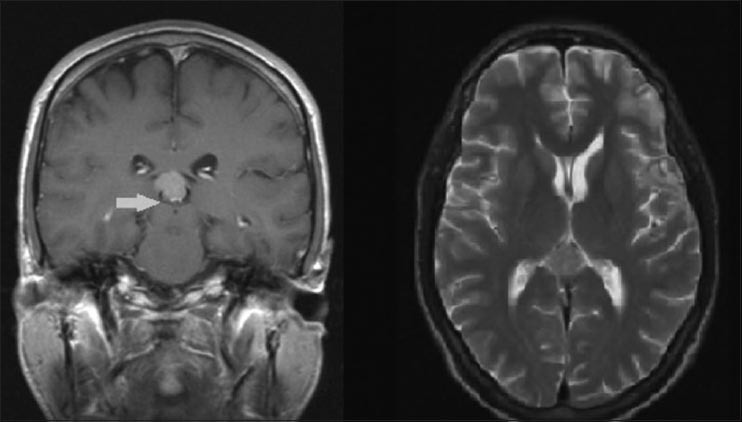
Preoperative MRI showing a well circumscribed mass in the pineal region. Right side: T2 axial section. Left side: T1 coronal section. Arrow showing the internal cerebral veins being pushed inferiorly by the tumor
Operation
Even though the relation between the severe intermittent headaches and the tumor was uncertain, given the unknown nature of the lesion, we eventually opted for surgery since the patient was young and the estimated risk was low. The tumor was successfully and completely resected via a supracerebellar infratentorial approach [Figure 2]. Intraoperatively, the tumor was displacing the pineal gland to the left and sat over the right internal cerebral vein, spanning on both sides of it. The tumor was poorly vascularized. The origin of the tumor was found to be in the superior part of the VI.
Figure 2.
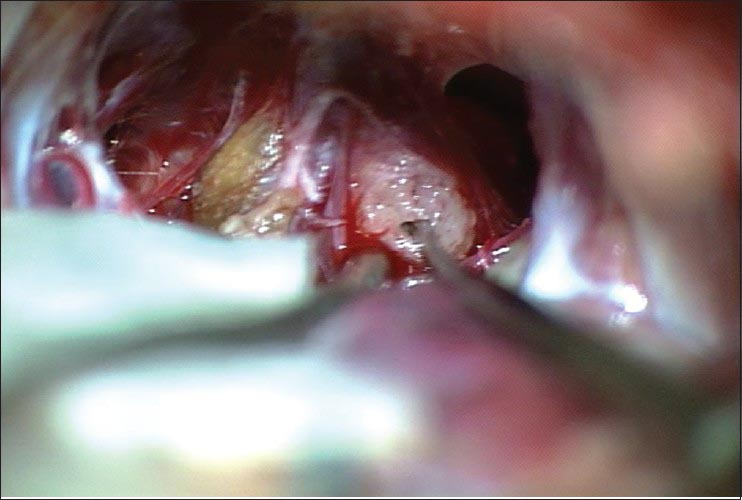
Intraoperative image showing the tumor being removed via the supracerebellar infratentorial approach
Postoperative course
The postoperative period was uneventful. Postoperative head CT scan and MRI revealed no residual tumor [Figure 3]. The patient was discharged 4 days following surgery with no neurological deficit. The pathological analysis confirmed a World Health Organization (WHO) grade I meningioma. Regular follow-up over 4 years found the patient asymptomatic and MRIs revealed no signs of recurrence.
Figure 3.
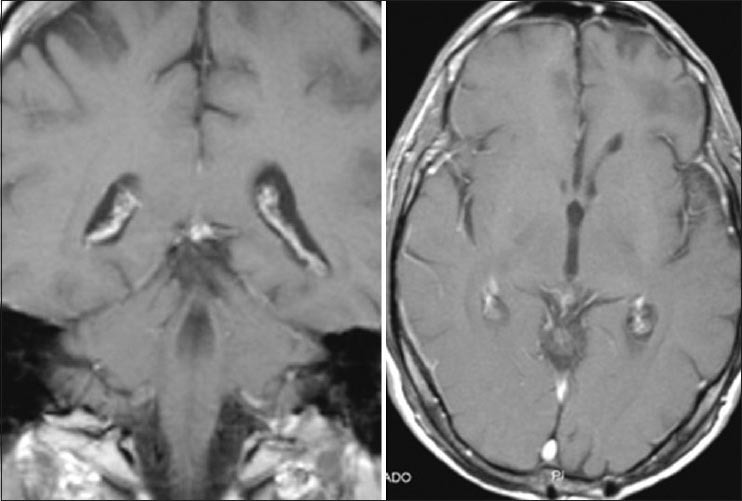
Postoperative T1 MRI sequence showing a complete macroscopic removal of the tumor. Right side: Axial section. Left side: Coronal section
DISCUSSION
Tumors arising from the pineal region represent roughly 1–4% of all intracranial neoplasms.[1,20] The variety of tumors in the pineal region depends on the cells present in that region, whether from the pineal gland itself or from the surrounding structures. Among them are meningiomas, representing 8–10% of all pineal region tumors.[20,29] Since meningiomas originate from the arachnoid's cap cells, those found in the pineal region can originate from three sites. First, they can arise at the falcotentorial junction, from the arachnoid layer, which tightly follows the dura. These are the most common.[22,23,25] However, some authors do not consider them as being “true” pineal region meningiomas since they do not originate from the region itself, but rather grow toward it.[21,29] Second, they can come from the arachnoid envelope of the gland itself, in which case they do not have a dural attachment. Finally, they can arise from the VI, also without dural attachment.[10,28] The latter two types of meningiomas without dural attachment are very rare and considered to be “true” pineal region meningiomas.
The VI consists of the potential space between the two leaflets of the tela choroidea, a double layered fold of arachnoid-pia mater in the roof of the third ventricle.[31] Traveling in the VI are the internal cerebral veins and the medial posterior choroidal arteries. The arachnoid inside the tela choroidea is divided in two layers: A ventral one, which is a direct anterior extension of the arachnoid envelope over the pineal region, and a dorsal one, which envelops the internal cerebral veins.[31]
Although some authors have stated that meningiomas coming from the VI can potentially come from either its superior or inferior leaflet; in our review of the literature, we only found cases of meningiomas arising from the inferior leaflet.
Lozier et al. reviewed all the cases of VI meningiomas up to 2003 and reported a total of 17 cases, including their own, in which there was sufficient reliable information supporting the VI as the origin of the meningiomas.[13] In the current review, one of Lauzier's rejected case was retained, judging it to provide sufficient information about the origin of the meningioma.[16] Adding cases from the literature since 2003 to the present time[17,18] and one before 2003 not considered by Lozier et al.,[14] we reached a total of 22 cases [Table 1].[3,4,5,6,7,8,9,13,14,15,16,17,18,19,22,23,24,25,26]
Table 1.
Reported cases of velum interpositum meningiomas
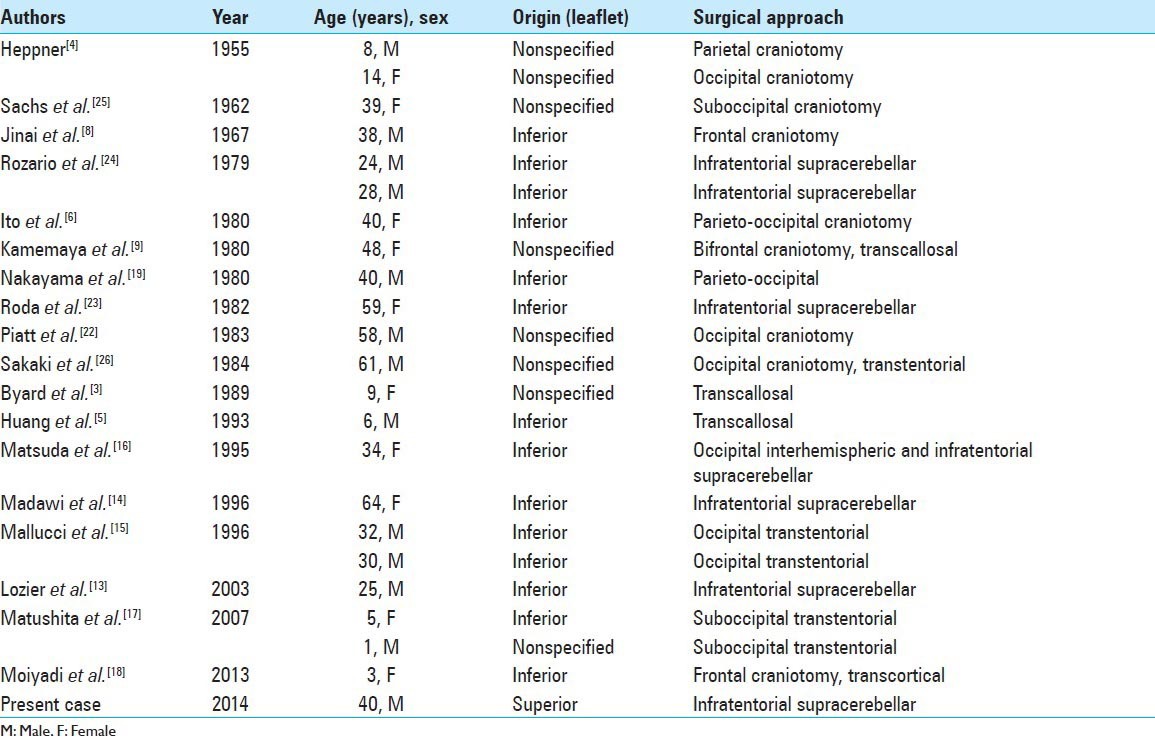
Since the location of the meningioma may have an impact on the surgical approach, in examining these 22 cases of VI meningiomas, we searched for evidence as to whether the meningioma arose from the superior or inferior layer of the VI. In fourteen cases the tumor clearly originated from the inferior leaflet as seen directly during surgery or on imagery where the internal cerebral veins were displaced superiorly. In the remaining eight cases of VI meningiomas, there was insufficient information to determine the location. Therefore, to our knowledge, there is no previously reported case of VI meningioma arising from the superior leaflet. We herein report such a case.
Even taking into consideration the eight cases with insufficient information as to location, it would appear that VI meningiomas are more commonly found on the inferior leaflet. A possible explanation could be that most meningiomas arise not from the velum itself, but from the cap cells present in the choroid plexus, which is adjacent to the inferior leaflet of the VI. Indeed, starting in the 6th week of embryogenesis, the roof of the ventricular system invaginates in order to form the choroid plexus.[27] Since the adjacent cells of the neural crest contribute to the formation of leptomeninges, some of these cells might migrate together with the choroid plexus, explaining the presence of arachnoid cells reported in normal choroid plexus stroma.[27,30] Intraventricular meningiomas are thought to arise from these arachnoid cells in the choroid plexus.[11,30] Similarly in the VI, the close vicinity of the choroid plexus in regard to the inferior leaflet could bring a significantly larger “pool” of arachnoid cells in the region that could potentially give rise to meningiomas. Also the greater blood flow in the choroid plexus could favor the growth of meningiomas in this area. In our case, the tumor was poorly vascularized. Knowing that the well-vascularized choroid plexus is attached to the inferior leaflet, it would be interesting to observe whether meningiomas of the superior leaflet are more likely to be less vascularized than those of the inferior leaflet. Noting the characteristics of the tumors according to their origin may provide new information, which, if there are differences between the two, may lead to better anticipate pitfalls during surgical resection.
Many approaches have been described to treat pineal region meningiomas such as the suboccipital transtenorial, supracerbellar infratentorial and posterior interhemispheric approaches.[2,10,12,13] One important factor in considering the choice of approach is the relationship between the tumor and the deep cerebral veins. Usually meningiomas arising below the internal cerebral veins are approached via a supracerebellar infratentorial approach, while those arising above the major veins are approached via a posterior interhemispheric approach.[13] However, in our case where the meningioma was above the internal cerebral veins, because of its moderate size, we were able to successfully approach it from below using a supracerebellar infratentorial approach.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2015/6/4/132/155703
Contributor Information
Pierre-Olivier Champagne, Email: pierre-olivier.champagne@umontreal.ca.
Michel W. Bojanowski, Email: michel.bojanowski.chum@ssss.gouv.qc.ca.
REFERENCES
- 1.Araki C, Kayoto MD. Meningiomas in the pineal region: A report of two cases, removed by operation. Arch Jpn Chir. 1937;14:1181–92. [Google Scholar]
- 2.Bassiouni H, Asgari S, König HJ, Stolke D. Meningiomas of the falcotentorial junction: Selection of the surgical approach according to the tumor type. Surg Neurol. 2008;69:339–49. doi: 10.1016/j.surneu.2007.02.029. [DOI] [PubMed] [Google Scholar]
- 3.Byard RW, Bourne AJ, Clark B, Hanieh A. Clinicopathological and radiological features of two cases of intraventricular meningioma in childhood. Pediatr Neurosci. 1989;15:260–4. doi: 10.1159/000120478. [DOI] [PubMed] [Google Scholar]
- 4.Heppner F. Uber Meningeome des 3 Ventrikels. Acta Neurochir. 1954;4:55–67. doi: 10.1007/BF01413617. [DOI] [PubMed] [Google Scholar]
- 5.Huang PP, Doyle WK, Abbott IR. Atypical meningioma of the third ventricle in a 6-year-old boy. Neurosurgery. 1993;33:312–5. doi: 10.1227/00006123-199308000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Ito J, Kadekaru T, Hayano M, Kurita I, Okada K, Yoshida Y. Meningioma in the tela choroidea of the third ventricle: CT and angiographic correlations. Neuroradiology. 1981;21:207–11. doi: 10.1007/BF00367342. [DOI] [PubMed] [Google Scholar]
- 7.Ito J, Kadekaru T, Hayano M, Kurita I, Okada K, Yoshida Y. Meningioma originating and developing in the tela choroidea of the third ventricle. Its CT and angiographic findings (author's transl) Neurol Med Chir. 1980;20:1081–94. doi: 10.2176/nmc.20.1081. [DOI] [PubMed] [Google Scholar]
- 8.Jinnai D, Mogami H, Ioku M, Kamikawa K, Murakawa J. Case of meningioma of the third ventricle. No To Shinkei. 1967;19:1263–8. [PubMed] [Google Scholar]
- 9.Kameyama M, Seki H, Ogawa A, Yoshimoto T. A giant meningioma of the third ventricle (author's transl) Neurol Med Chir. 1980;20:1055–60. doi: 10.2176/nmc.20.1055. [DOI] [PubMed] [Google Scholar]
- 10.Konovalov AN, Spallone A, Pitzkhelauri DI. Meningioma of the pineal region: A surgical series of 10 cases. J Neurosurg. 1996;85:586–90. doi: 10.3171/jns.1996.85.4.0586. [DOI] [PubMed] [Google Scholar]
- 11.Landenheim JC. Illinois: Charles C Thomas; 1963. Choroid Plexus Meningiomas of the Lateral Ventricle; p. 5. [Google Scholar]
- 12.Li Y, Zhao G, Wang H, Zhu W, Qu L, Li Y, et al. Use of 3D-computed tomography angiography for planning the surgical removal of pineal region meningiomas using Poppen's approach: A report of ten cases and a literature review. World J Surg Oncol. 2011;9:64. doi: 10.1186/1477-7819-9-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lozier AP, Bruce JN. Meningiomas of the velum interpositum: Surgical considerations. Neurosurg Focus. 2003;15:E11. doi: 10.3171/foc.2003.15.1.11. [DOI] [PubMed] [Google Scholar]
- 14.Madawi AA, Crockard HA, Stevens JM. Pineal region meningioma without dural attachment. Br J Neurosurg. 1996;10:305–7. doi: 10.1080/02688699650040197. [DOI] [PubMed] [Google Scholar]
- 15.Mallucci CL, Obukhov S. Successful removal of large pineal region meningiomas: Two case reports. Surg Neurol. 1995;44:562–6. doi: 10.1016/0090-3019(95)00220-0. [DOI] [PubMed] [Google Scholar]
- 16.Matsuda Y, Inagawa T. Surgical removal of pineal region meningioma--three case reports. Neurol Med Chir (Tokyo) 1995;35:594–7. doi: 10.2176/nmc.35.594. [DOI] [PubMed] [Google Scholar]
- 17.Matushita H, Pinto FC, Plese JP. Meningiomas of pineal region in children. Arq Neuropsiquiatr. 2007;65:1000–6. doi: 10.1590/s0004-282x2007000600016. [DOI] [PubMed] [Google Scholar]
- 18.Moiyadi AV, Shetty P. Giant velum interpositum meningioma in a child. Indian J Med Paediatr Oncol. 2012;33:173–5. doi: 10.4103/0971-5851.103147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakayama K, Miyasaka Y, Ohwada T, Yada K. Meningioma in the pineal region—report of a case and review of the literature (author's transl) Neurol Med Chir. 1980;20:265–71. [PubMed] [Google Scholar]
- 20.Obrador S, Soto M, Gutierrez-Diaz JA. Surgical management of tumors of the pineal region. Acta Neurochir (Wien) 1976;34:159–71. doi: 10.1007/BF01405870. [DOI] [PubMed] [Google Scholar]
- 21.Okami N, Kawamata T, Hori T, Takakura K. Surgical treatment of falcotentorial meningioma. J Clin Neurosci. 2001;8(Suppl 1):15–8. doi: 10.1054/jocn.2001.0870. [DOI] [PubMed] [Google Scholar]
- 22.Piatt JH, Jr, Campbell GA. Pineal region meningioma: Report of two cases and literature review. Neurosurgery. 1983;12:369–76. doi: 10.1227/00006123-198304000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Roda JM, Perez-Higuras A, Oliver B, Alvarez MP, Blazquez MG. Pineal region meningiomas without dural attachment. Surg Neurol. 1882;17:147–51. doi: 10.1016/s0090-3019(82)80044-x. [DOI] [PubMed] [Google Scholar]
- 24.Rozario R, Adelman L, Prager RJ, Stein BM. Meningiomas of the pineal region and third ventricle. Neurosurgery. 1979;5:489–5. doi: 10.1227/00006123-197910000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Sachs E, Jr, Avman N, Fisher RG. Meningiomas of pineal region and posterior part of 3 rd ventricle. J Neurosurg. 1962;19:325–31. doi: 10.3171/jns.1962.19.4.0325. [DOI] [PubMed] [Google Scholar]
- 26.Sakaki S, Shiraishi T, Takeda S, Matsuoka K, Sadamoto K. Occlusion of the great vein of Galen associated with a huge meningioma in the pineal region. Case report. J Neurosurg. 1984;61:1136–40. doi: 10.3171/jns.1984.61.6.1136. [DOI] [PubMed] [Google Scholar]
- 27.Shuangshoti S, Netsky MG. Histogenesis of choroid plexus in man. Am J Anat. 1966;118:283–316. doi: 10.1002/aja.1001180114. [DOI] [PubMed] [Google Scholar]
- 28.Songtao Q, Xi-an Z, Jun F, Guanglong Huang, Jun P, Binghui Q. Anatomical study of the arachnoid envelope over the pineal region. Neurosurgery. 2011;68(1 Suppl Operative):7–15. doi: 10.1227/NEU.0b013e3182059e10. [DOI] [PubMed] [Google Scholar]
- 29.Stein BM, Bruce JN, Fetell MR, Wilkins RH, Rengachary SS, editors. 1st edition. Vol. 41. New York: McGraw-Hill; 1990. Surgical approaches to pineal tumors In: Neurosurgery update; pp. 489–98. [Google Scholar]
- 30.Wajima D, Iida J, Nishi N. Third ventricular meningioma-case report. Neurol Med Chir (Tokyo) 2011;51:75–8. doi: 10.2176/nmc.51.75. [DOI] [PubMed] [Google Scholar]
- 31.Zhang XA, Qi S, Fan J, Huang G, Peng J, Xu J. The distribution of arachnoid membrane within the velum interpositum. Acta Neurochir (Wien) 2012;154:1711–5. doi: 10.1007/s00701-012-1436-8. [DOI] [PubMed] [Google Scholar]


